Effects of Achilles Tendon Moment Arm Length on Insertional Achilles Tendinopathy
Abstract
1. Introduction
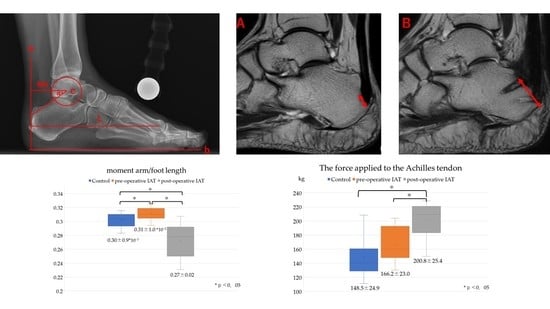
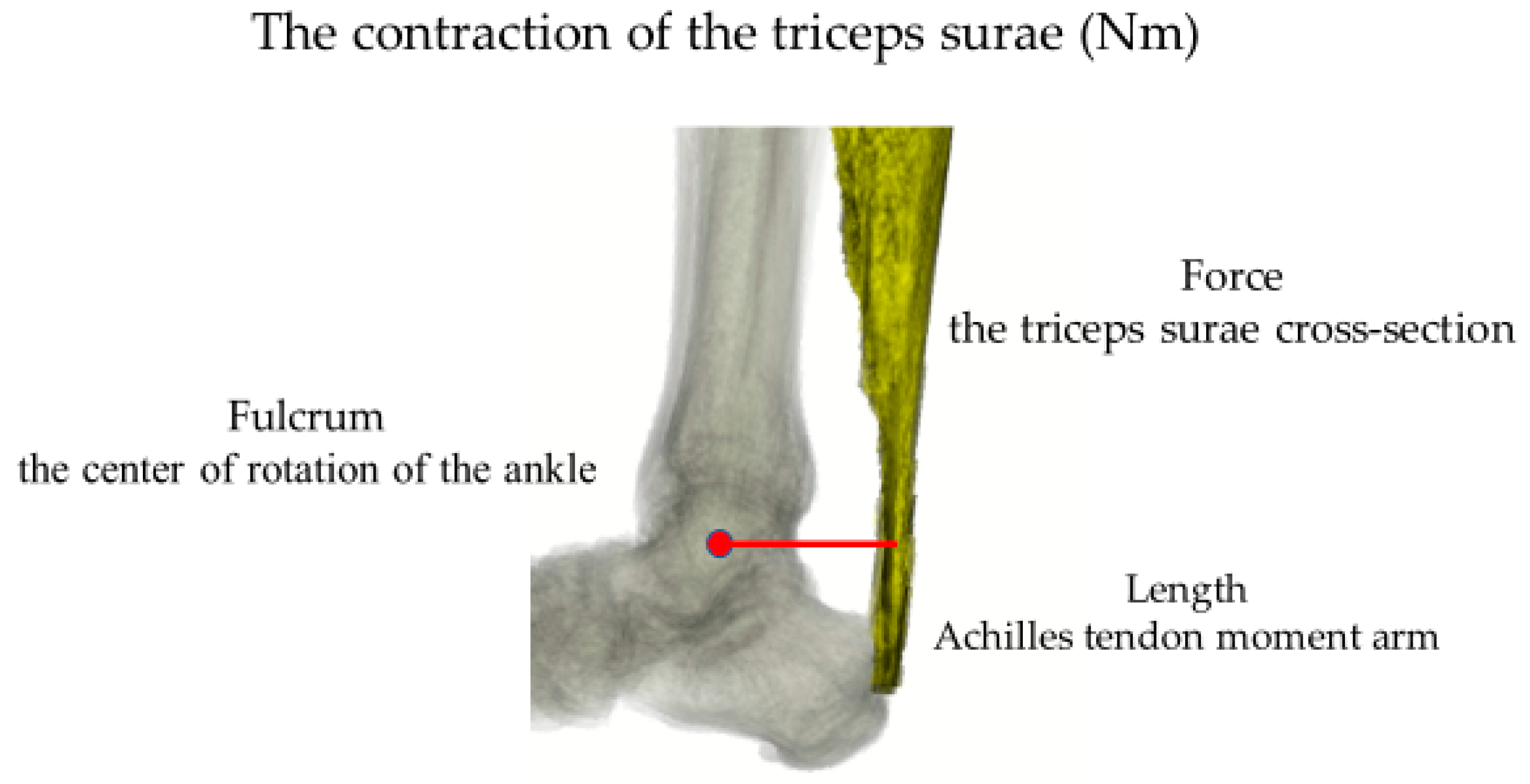
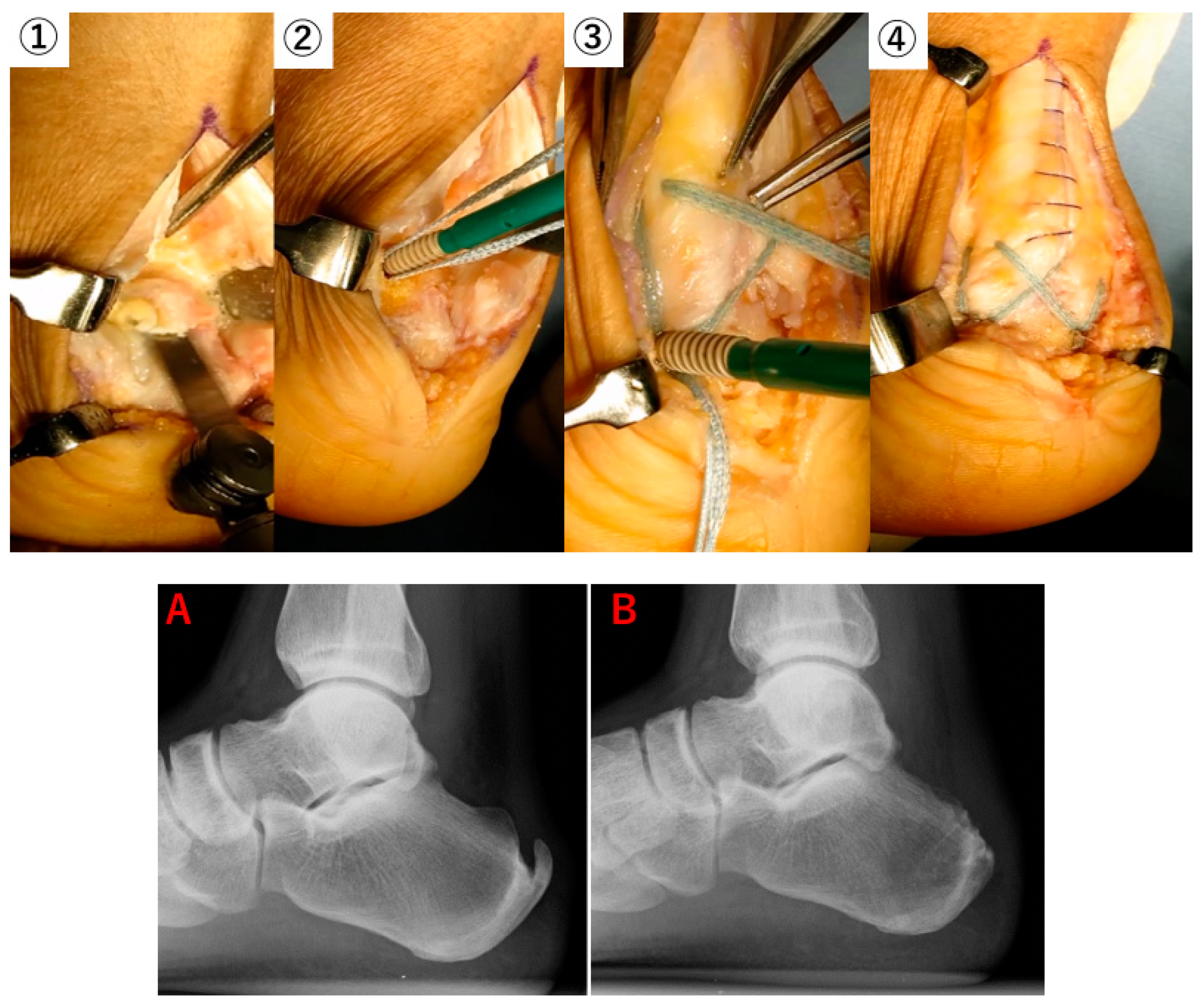
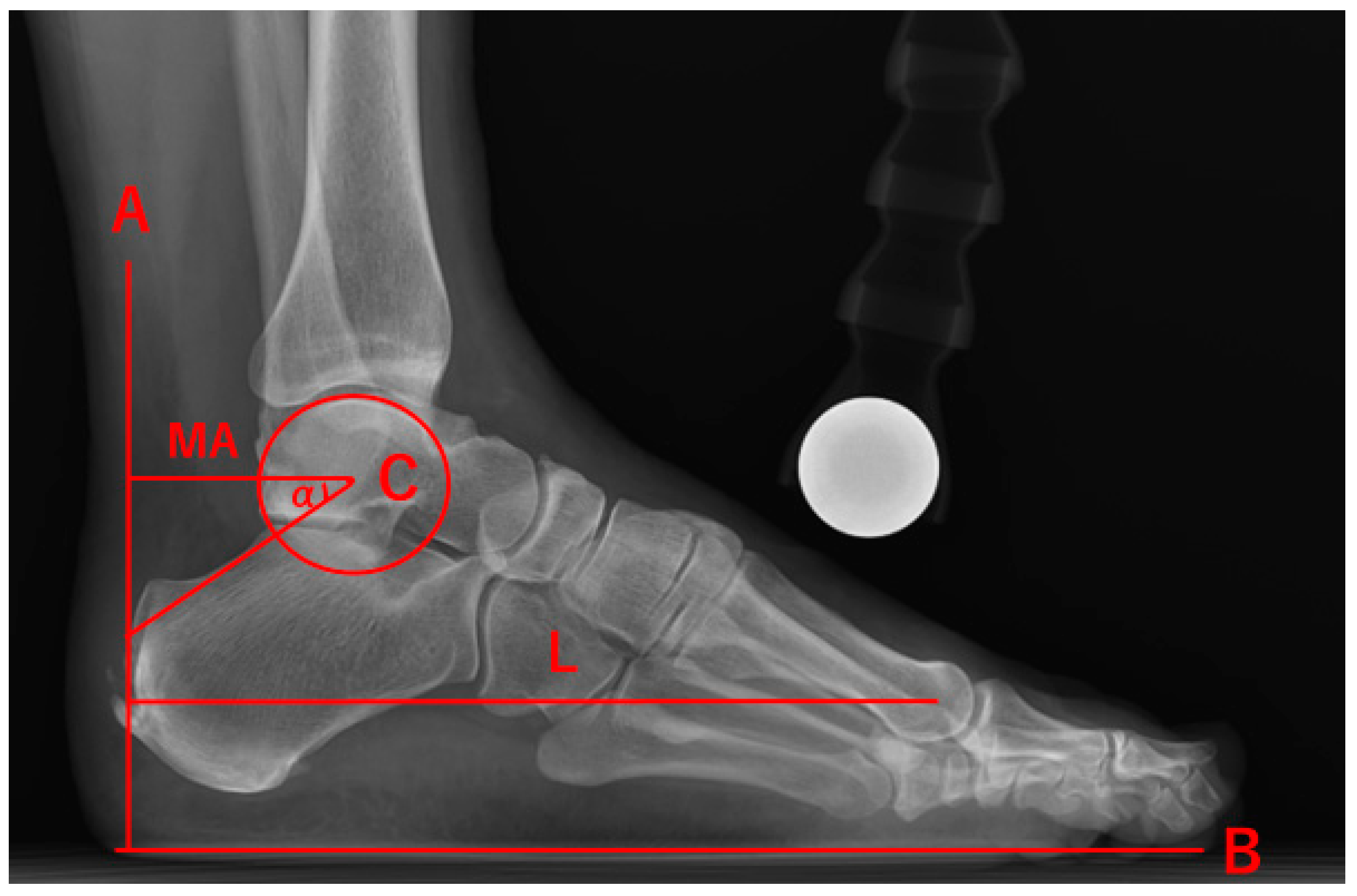
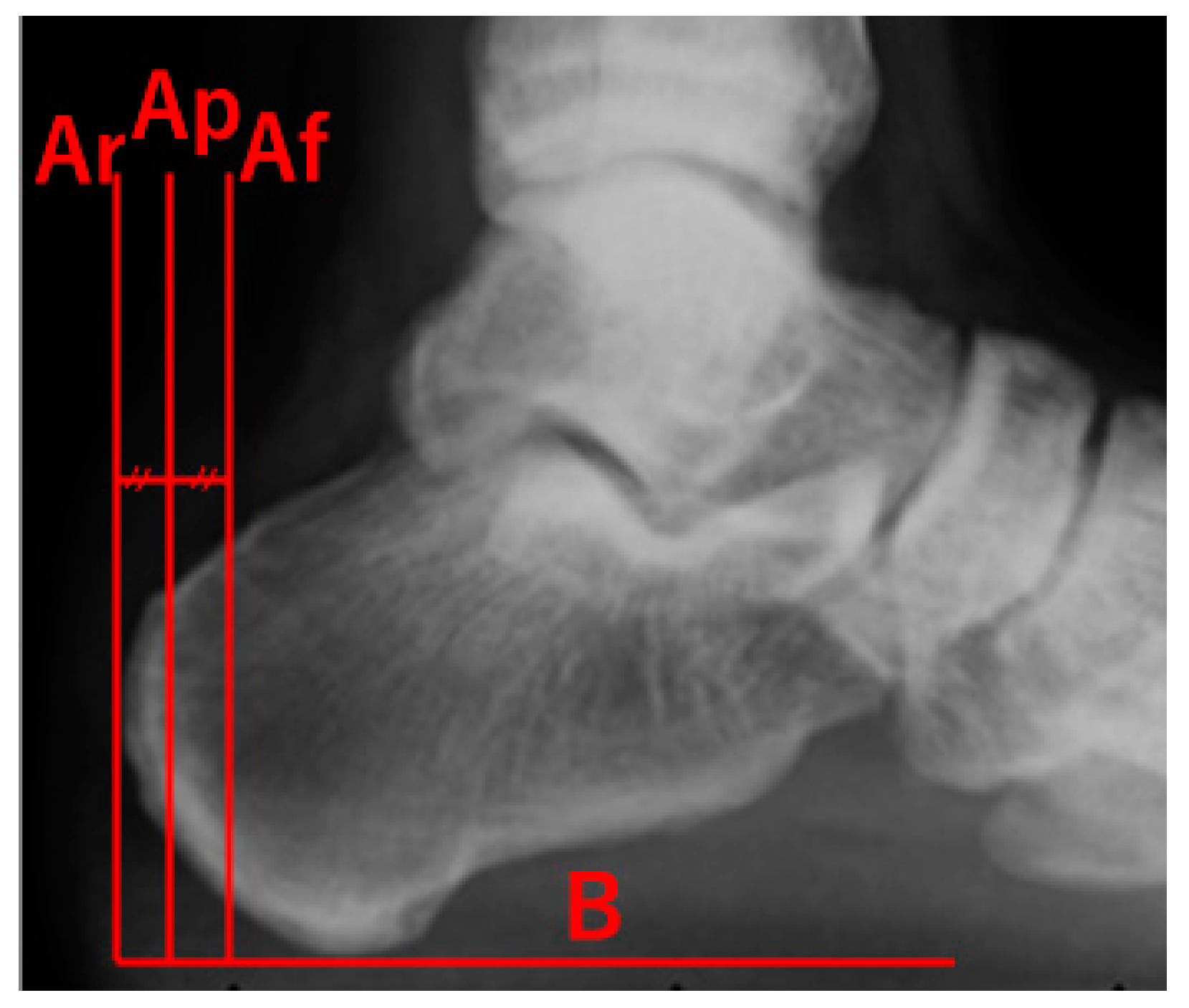
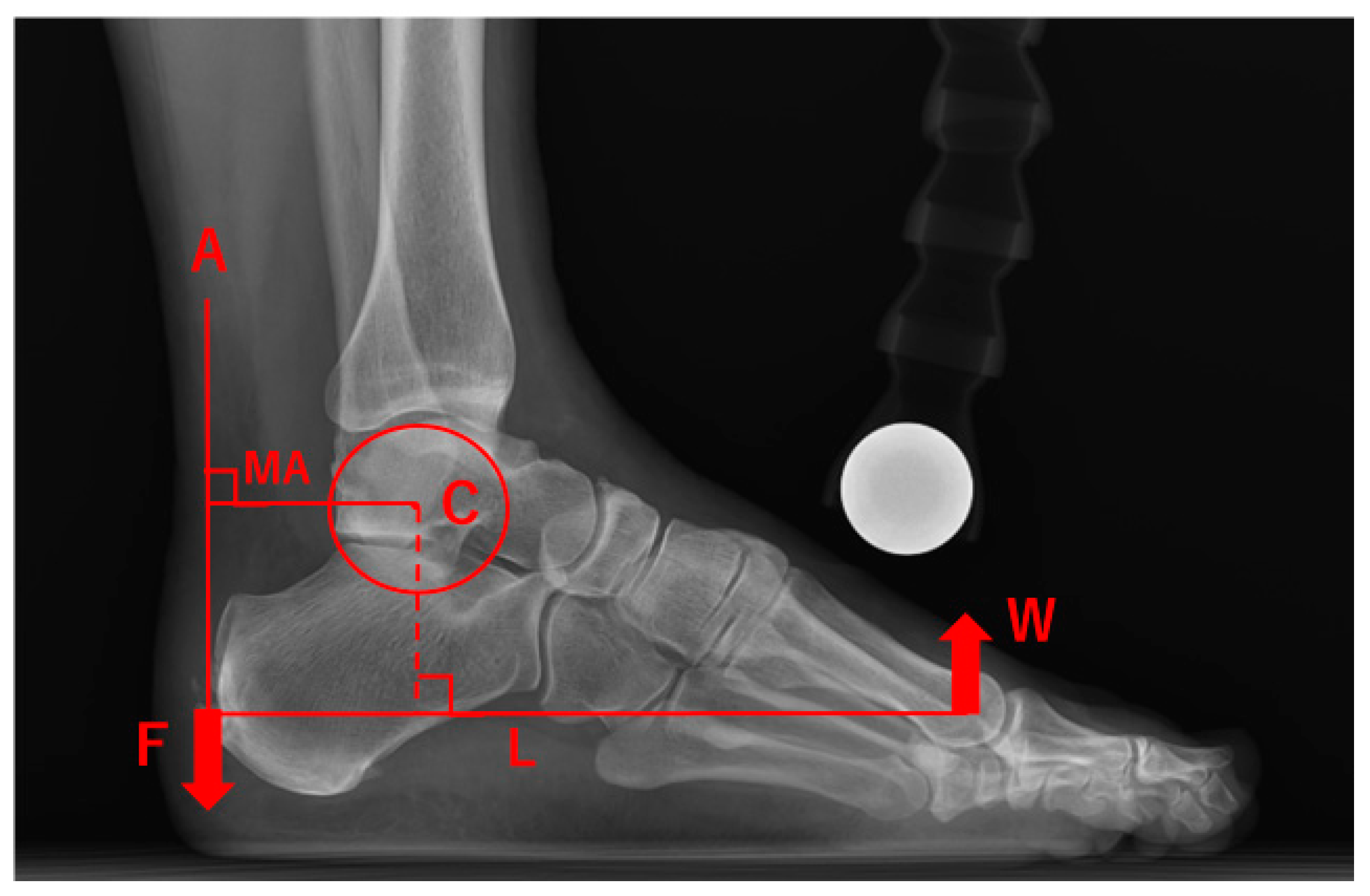
2. Materials and Methods
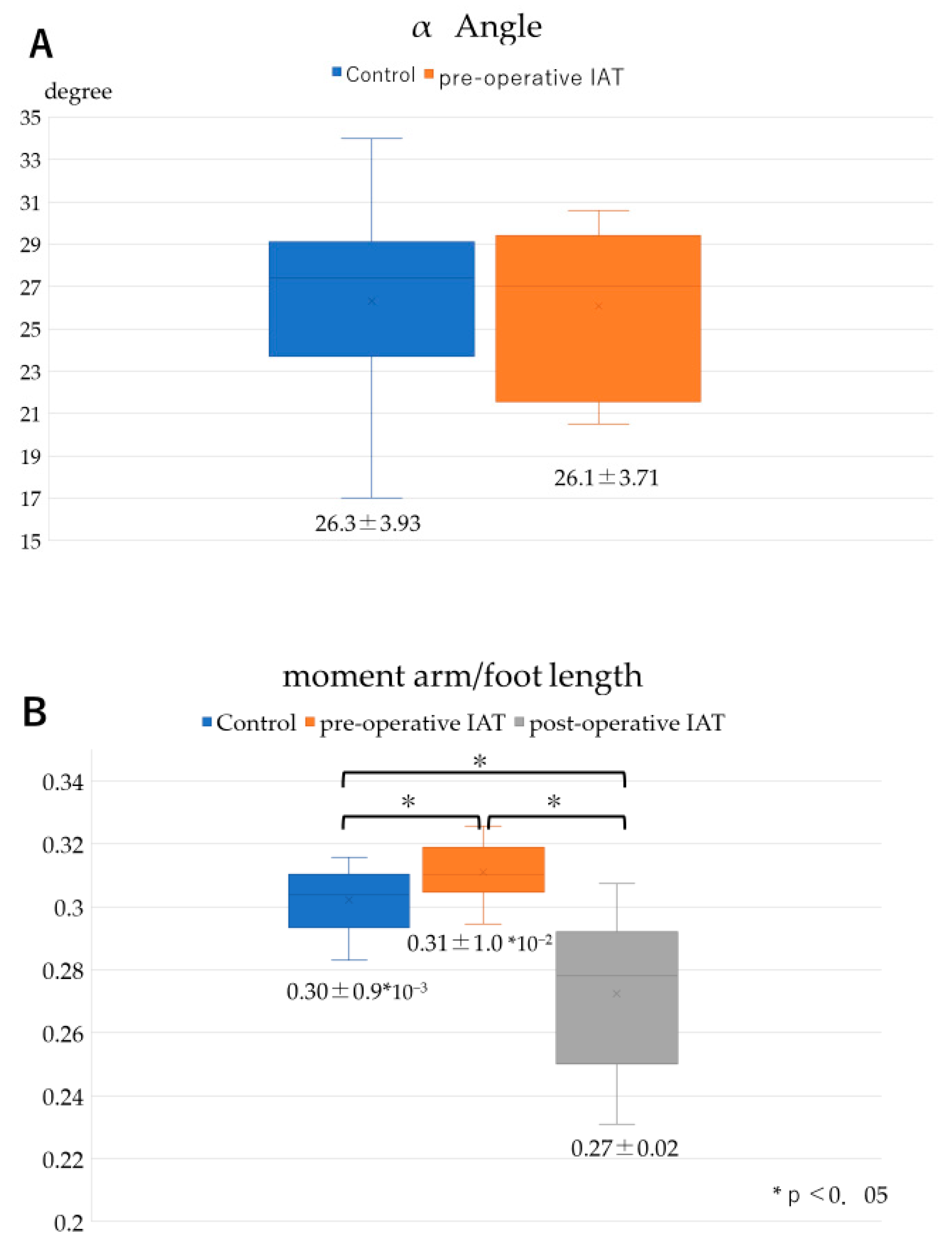
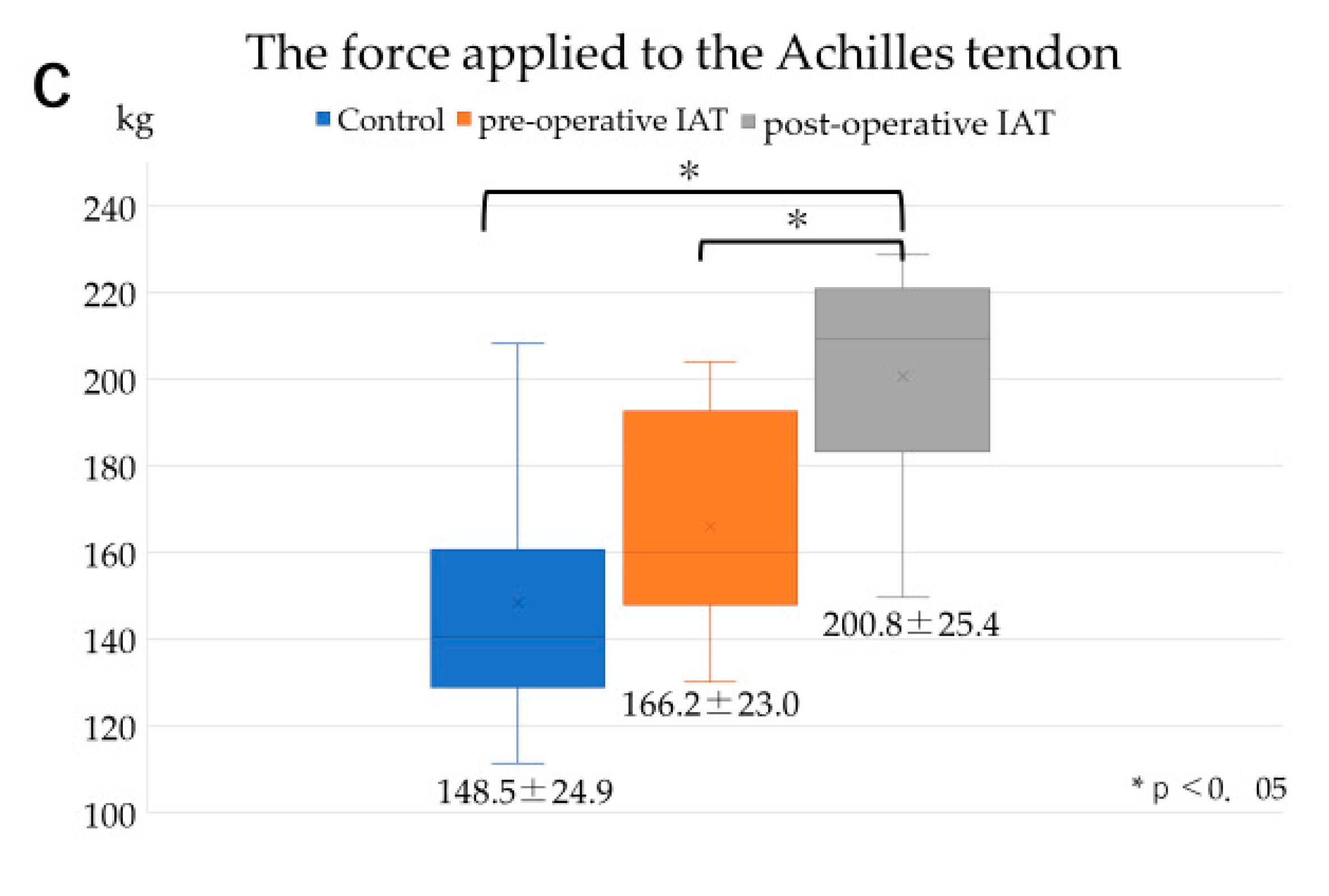
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Dayton, P. Anatomic, Vascular, and Mechanical Overview of the Achilles Tendon. Clin. Podiatr. Med. Surg. 2017, 34, 107–113. [Google Scholar] [CrossRef]
- Carbone, V.; Fluit, R.; Pelilaan, P.; van der Krogt, M.M.; Janssen, D.; Damsgaard, M.; Vigneron, L.; Feilkas, T.; Koopman, H.F.J.M.; Verdonschot, N. TLEM 2.0-A comprehensive musculoskeletal geometry dataset for subject-specific modeling of the lower extremity. J. Biomech. 2015, 48, 734–774. [Google Scholar] [CrossRef]
- Klein Horsman, M.D.; Koopman, H.F.J.M.; van der Helm, F.C.T.; Poliacu Prose, L.; Veeger, H.E.J. Morphological muscle and joint parameters for musculoskeletal modeling of the lower extremity. Clin. Biomech. 2007, 22, 239–247. [Google Scholar] [CrossRef]
- Klein, P.; Mattys, S.; Rooze, M. Moment arm length variations of selected muscles acting on talocrural and subtalar joints during movement: An in vitro study. J. Biomech. 1996, 29, 21–30. [Google Scholar] [CrossRef]
- Fath, F.; Blazevich, A.J.; Waugh, C.M.; Miller, S.C.; Korff, T. Direct comparison of in vivo Achilles tendon moment arms obtained from ultrasound and MR scans. J. Appl. Physiol. 2010, 109, 1644–1652. [Google Scholar] [CrossRef] [PubMed]
- Maganaris, C.N. Imaging-based estimates of moment arm length in intact human muscle-tendons. Eur. J. Appl. Phsyol. 2004, 91, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Olzewski, K.; Dick, T.J.; Wakeling, J.M. Achilles tendon moment arms: The importance of measuring at constant tendon load when using the tendon excursion method. J. Biomech. 2015, 48, 1206–1209. [Google Scholar] [CrossRef] [PubMed]
- Csapo, R.; Hodgson, J.; Kinugasa, R.; Edgerton, V.R.; Sinha, S.; Edgerton, V.R.; Sinha, S. Ankle morphology amplifies calcaneus movement relative to triceps surae muscle shortening. J. Appl. Physiol. 2013, 115, 468–473. [Google Scholar] [CrossRef]
- Manal, K.; Cowder, J.D.; Buchanan, T.S. Subject-specific measures of Achilles tendon moment arm using ultrasound and video-based motion capture. Physiol. Rep. 2013, 1, e00139. [Google Scholar] [CrossRef]
- Manja, D.; Zwicky, L.; Horn, T.; Hintermann, B. The effect of foot type on the Achilles tendon moment arm and biomechanics. Foot 2019, 38, 91–94. [Google Scholar] [CrossRef]
- Rufai, A.; Ralphs, J.R.; Benjamin, M. Structure and histopathology of the insertional region of the human Achilles tendon. J. Orthop. Res. 1995, 13, 585–593. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, M.; Kumai, T.; Milz, S.; Boszczyk, B.M.; Boszczyk, A.A.; Ralphs, J.R. The skeletal attachment of tendons-tendon ‘entheses’. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 2002, 133, 931–945. [Google Scholar] [CrossRef]
- Baxter, J.R.; Piazza, S.J. Plantar flexor moment arm and muscle volume predict torque-generating capacity in young men. J. Appl. Physio. 2014, 116, 538–544. [Google Scholar] [CrossRef]
- Kunimasa, Y.; Sano, K.; Oda, T.; Nicol, C.; Komi, P.V.; Locatelli, E.; Ito, A.; Ishikawa, M. Specific muscle-tendon architecture in elite Kenyan distance runners. Scand. J. Med. Sci. Sports 2014, 24, e269–e274. [Google Scholar] [CrossRef]
- Irwin, T.A. Current concepts review: Insertional Achilles tendinopathy. Foot Ankle Int. 2010, 31, 933–939. [Google Scholar] [CrossRef] [PubMed]
- Chimenti, R.L.; Cychosz, C.C.; Hall, M.M.; Phisitkul, P. Current concepts review Update: Insertional Achilles tendinopathy. Foot Ankle Int. 2017, 38, 1160–1169. [Google Scholar] [CrossRef]
- McGravey, W.C.; Palumbo, R.C.; Baxter, D.E.; Leibman, B.D. Insertional Achilles Tendinosis: Surgical Treatment through a Central Tendon Splitting Approach. Foot Ankle Int. 2002, 23, 19–25. [Google Scholar] [CrossRef]
- Blazevich, A.J.; Coleman, D.R.; Horne, S.; Cannavan, D. Anatomical predictors of maximum isometric and concentric knee extensor moment. Eur. J. Appl. Physiol. 2009, 105, 869–878. [Google Scholar] [CrossRef]
- Carrier, D.R.; Heglund, N.C.; Earls, K.D. Variable Gearing During Locomotion in the Human Musculoskeletal System. Science 1994, 265, 651–653. [Google Scholar] [CrossRef]
- Magnaris, C.N.; Balizopolos, V.; Sargeant, A.J. In vivo measurement-based estimations of the human Achilles tendon moment arm. Eur. J. Appl. Physiol. 2000, 83, 363–369. [Google Scholar] [CrossRef]
- Rasske, K.; Thelen, D.G.; Prahz, J.R. Variation in the human Achilles tendon moment arm during walking. Comput. Method Biomech. Biomed. Engin. 2017, 20, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Lyman, J.; Weinhold, P.S.; Almekinders, L.C. Strain behavior of the distal Achilles tendon: Implications for insertional Achilles tendinopathy. Am. J. Sports Med. 2004, 32, 457–461. [Google Scholar] [CrossRef] [PubMed]
- Andrew, G.; Jonathan, S. Comparison of Achilles tendon loading between male and female recreational runners. J. Hum. Kinet. 2014, 44, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Willy, R.W.; Halsey, L.; Hayek, A.; Johnson, H.; Willson, J.D. Patellofemoral joint and Achilles tendon loads during overground and treadmill running. J. Orthop. Sports Phys. Ther. 2016, 46, 664–672. [Google Scholar] [CrossRef]
- Farris, D.J.; Buckeridge, E.; Trewartha, G.; McGuigan, M.P. The effects of orthotic heel lifts on Achilles tendon force and strain during running. J. Appl. Biomech. 2012, 28, 511–519. [Google Scholar] [CrossRef]
- Franz, J.R.; Slane, L.C.; Rasske, K.; Thelen, D.G. Non-uniform in vivo deformations of the human Achilles tendon during walking. Gait Posture 2015, 41, 192–197. [Google Scholar] [CrossRef]
- Frankewycz, B.; Penz, A.; Weber, J.; da Silva, N.P.; Freimoser, F.; Bell, R.; Nerlich, M.; Jung, E.M.; Docheva, D.; Pfeifer, C.G. Achilles tendon elastic properties remain decreased in long term after rupture. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 2080–2087. [Google Scholar] [CrossRef]
- Fahlstrom, M.; Jonsson, P.; Lorentzon, R.; Alfredson, H. Chronic Achilles tendon pain treated with eccentric calf-muscle training. Knee Surg. Sports Traumatol. Arthrosc. 2003, 11, 327–333. [Google Scholar] [CrossRef]
- Rompe, J.D.; Furia, J.; Maffuli, N. Eccentric loading versus eccentric loading plus shock-wave treatment for midportion Achilles tendinopathy: A randomized controlled trial. Am. J. Sports Med. 2009, 37, 463–470. [Google Scholar] [CrossRef]
- Perlman, M.D. Enlargement of the entire posterior aspect of the calcaneus: Treatment with the Keck and Kelly calcaneal osteotomy. J. Foot Surg. 1992, 31, 424–433. [Google Scholar]
- Greenhagen, R.M.; Shinabarger, A.B.; Pearson, K.T.; Burns, P.R. Intermediate and long-term outcomes of the suture bridge technique for the management of insertional Achilles tendinopathy. Foot Ankle Spec. 2013, 6, 185–190. [Google Scholar] [CrossRef] [PubMed]


| IAT | Control | p Value | |
|---|---|---|---|
| n | 10 feet (8 people) | 15 feet (15 people) | |
| Sex | Male: 4 Female: 4 | Male: 8 Female: 7 | |
| Age, y | 55.5 ± 14.4 | 37.4 ± 16.2 | |
| Height, cm | 164 ± 13.3 | 163 ± 7.44 | >0.05 |
| Body weight, kg | 73.5 ± 11.0 | 64.5 ± 12.1 | >0.05 |
| BMI, kg/m2 | 27.7 ± 4.58 | 24.3 ± 4.83 | >0.05 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miyamoto, T.; Shinohara, Y.; Matsui, T.; Kurokawa, H.; Taniguchi, A.; Kumai, T.; Tanaka, Y. Effects of Achilles Tendon Moment Arm Length on Insertional Achilles Tendinopathy. Appl. Sci. 2020, 10, 6631. https://doi.org/10.3390/app10196631
Miyamoto T, Shinohara Y, Matsui T, Kurokawa H, Taniguchi A, Kumai T, Tanaka Y. Effects of Achilles Tendon Moment Arm Length on Insertional Achilles Tendinopathy. Applied Sciences. 2020; 10(19):6631. https://doi.org/10.3390/app10196631
Chicago/Turabian StyleMiyamoto, Takuma, Yasushi Shinohara, Tomohiro Matsui, Hiroaki Kurokawa, Akira Taniguchi, Tsukasa Kumai, and Yasuhito Tanaka. 2020. "Effects of Achilles Tendon Moment Arm Length on Insertional Achilles Tendinopathy" Applied Sciences 10, no. 19: 6631. https://doi.org/10.3390/app10196631
APA StyleMiyamoto, T., Shinohara, Y., Matsui, T., Kurokawa, H., Taniguchi, A., Kumai, T., & Tanaka, Y. (2020). Effects of Achilles Tendon Moment Arm Length on Insertional Achilles Tendinopathy. Applied Sciences, 10(19), 6631. https://doi.org/10.3390/app10196631