Computer-Based 3D Simulation Method in Dental Occlusion Education: Student Response and Learning Effect
Abstract
1. Introduction
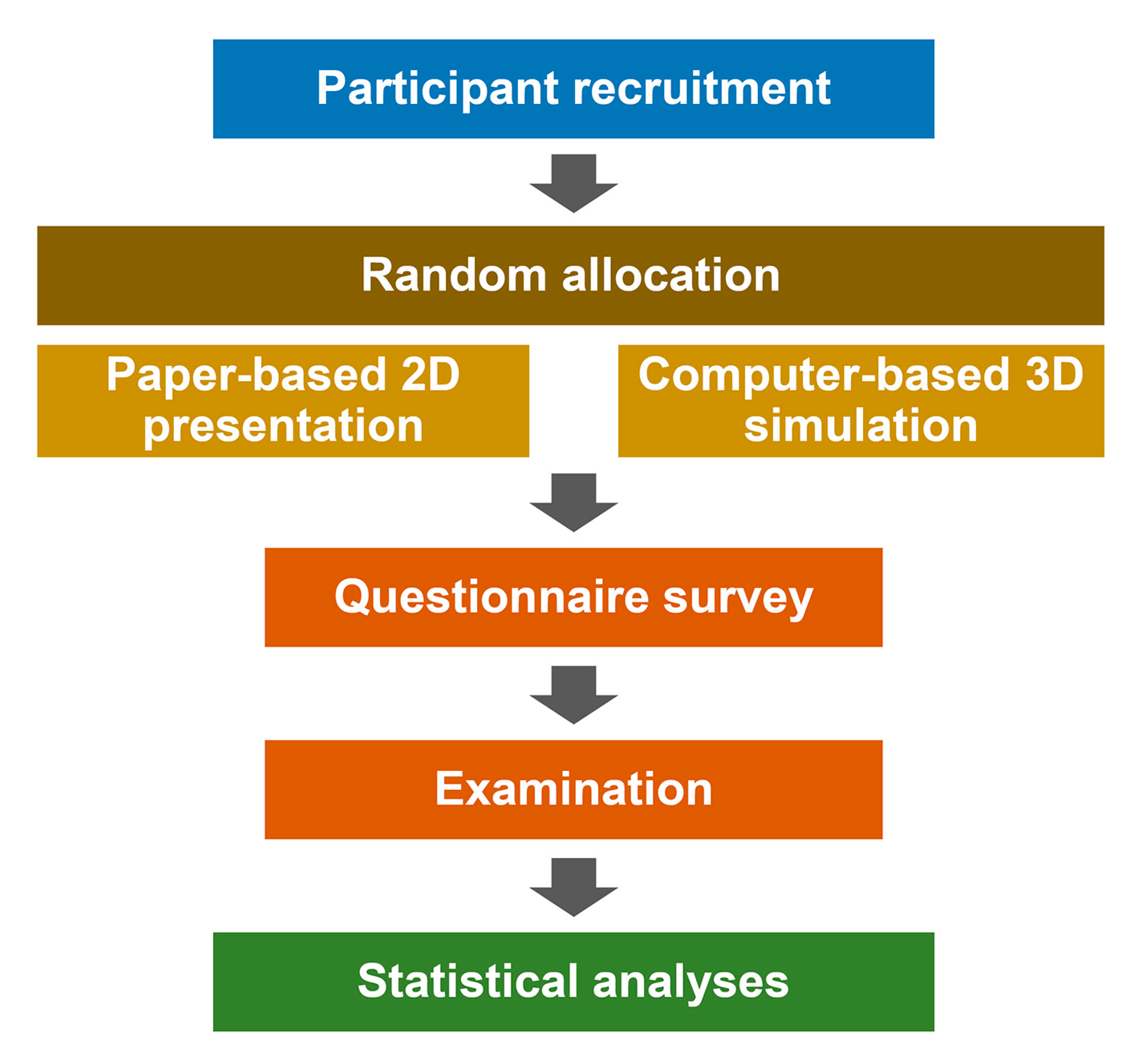
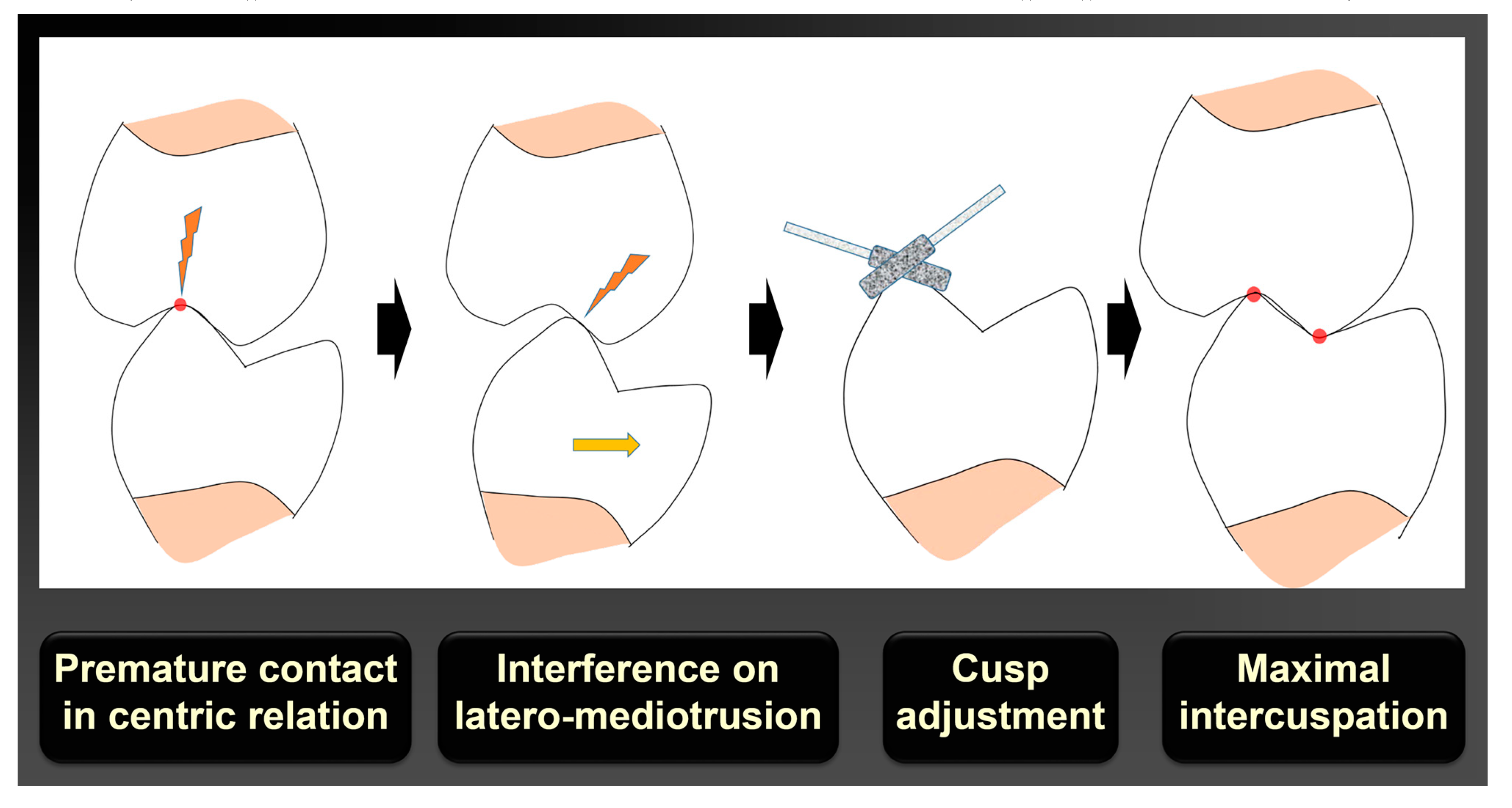
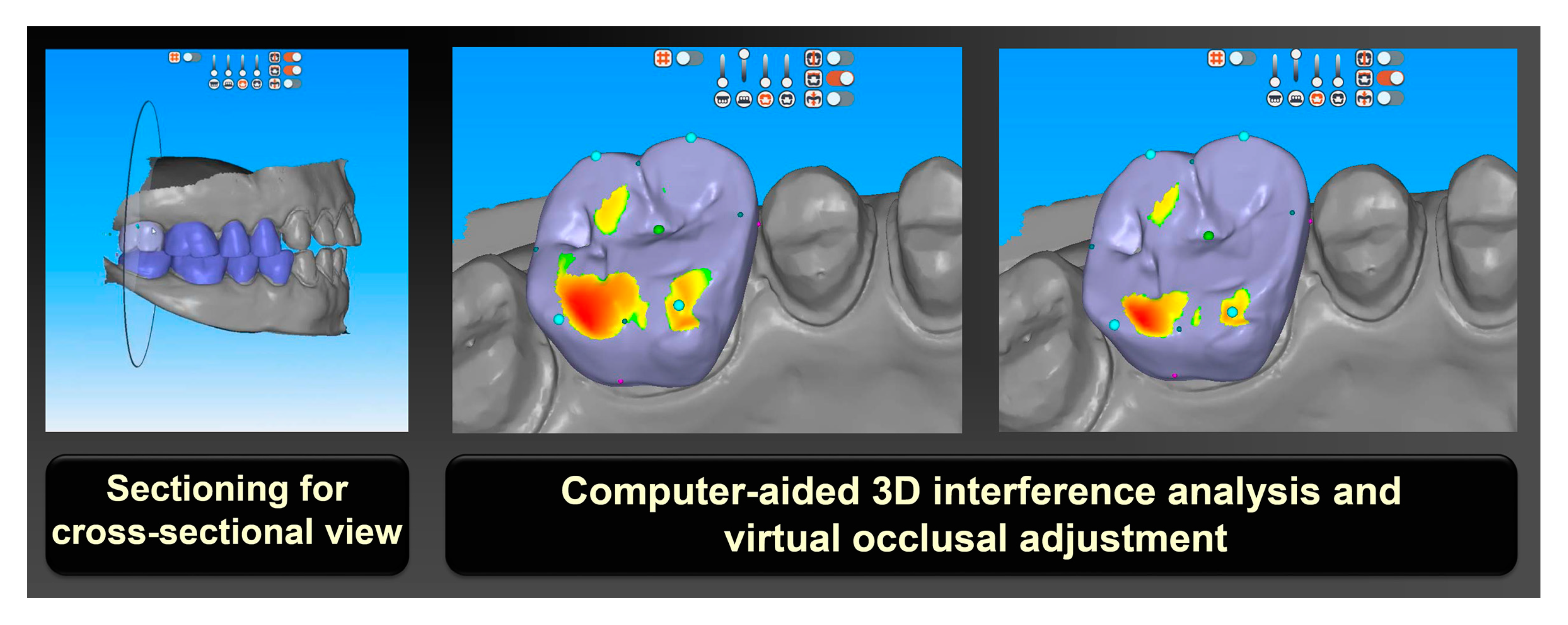
2. Materials and Methods
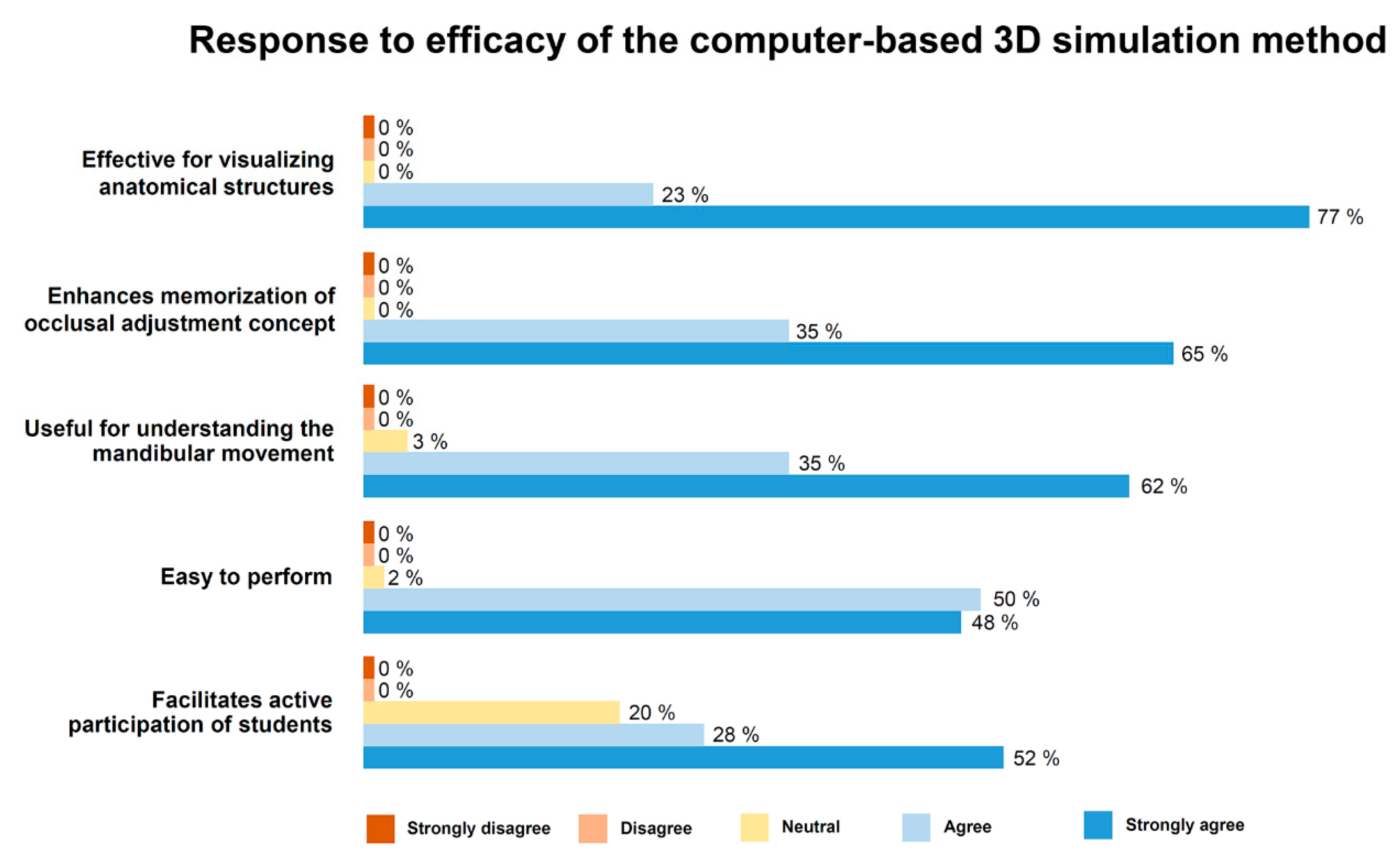
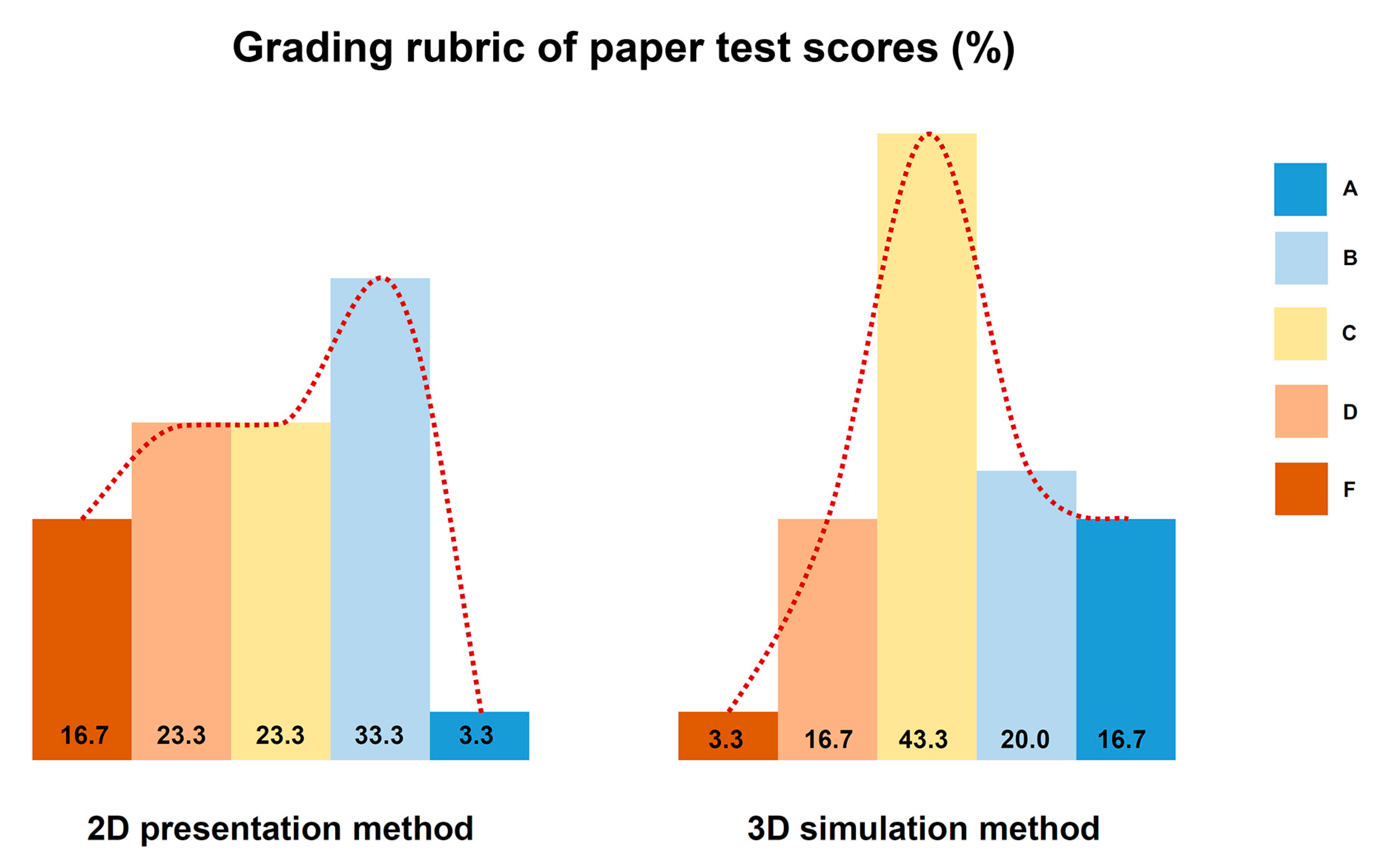
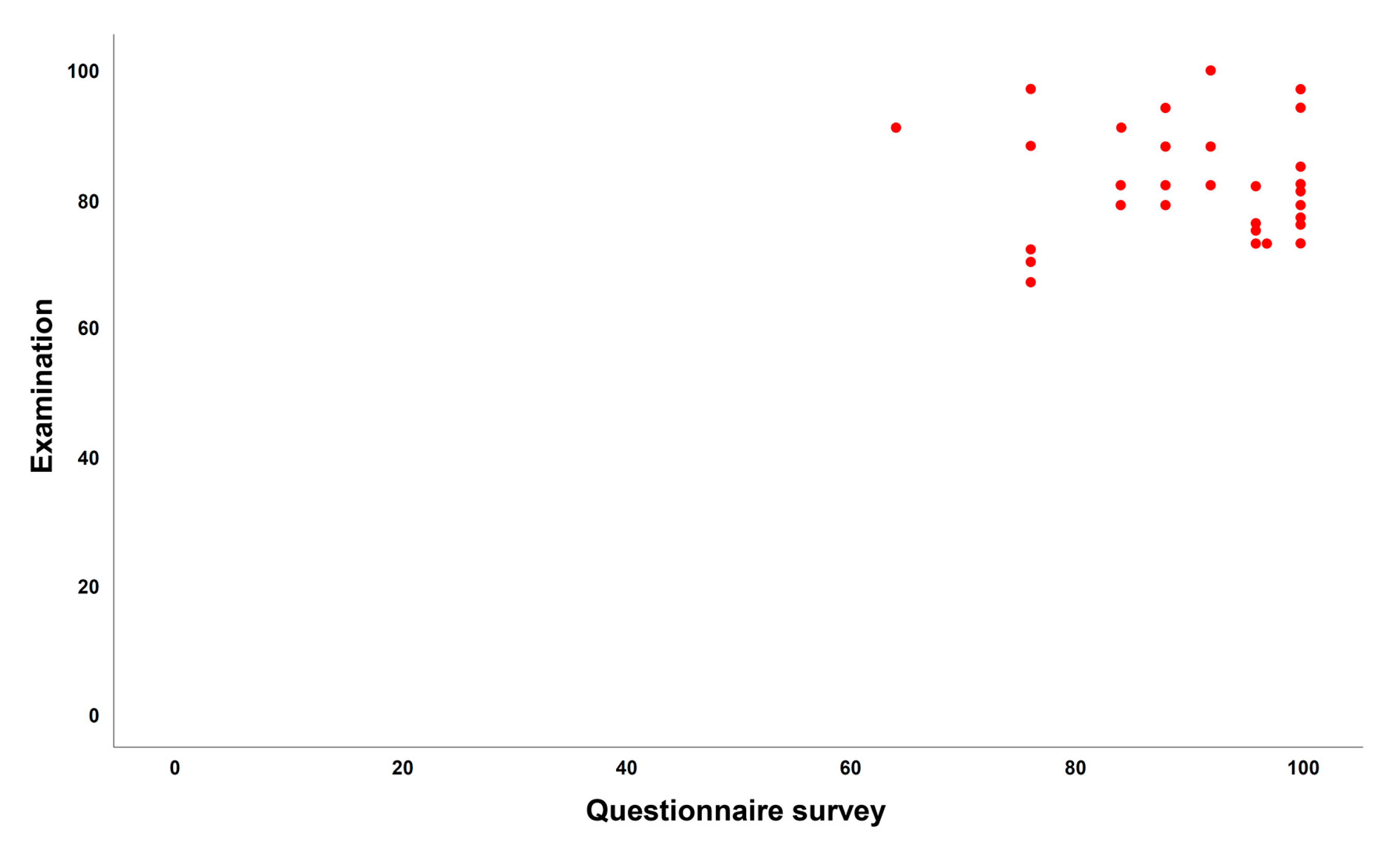
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Clark, J.R.; Evans, R.D. Functional occlusion: I. A review. J. Orthod. 2001, 28, 76–81. [Google Scholar] [CrossRef]
- Clark, G.T.; Adler, R.C. A critical evaluation of occlusal therapy: Occlusal adjustment procedures. J. Am. Dent. Assoc. 1985, 110, 743–750. [Google Scholar] [CrossRef]
- McCullock, A.J. Making occlusion work: I. Terminology, occlusal assessment and recording. Dent. Update 2003, 30, 150–157. [Google Scholar] [CrossRef][Green Version]
- Dawson, P.E. Evaluation, Diagnosis, and Treatment of Occlusal Problems; C.V. Mosby: St. Louis, MO, USA, 1988. [Google Scholar]
- Bakke, M. Mandibular elevator muscle: Physiology, action and effect of dental occlusion. Scand. J. Dent. Res. 1993, 101, 314–331. [Google Scholar] [CrossRef]
- Bando, E.; Nishigawa, K.; Nakano, M.; Takeuchi, H.; Shigemoto, S.; Okura, K.; Satsuma, T.; Yamamoto, T. Current status of researches on jaw movement and occlusion for clinical application. Jpn Dent. Sci. Rev. 2009, 45, 83–97. [Google Scholar] [CrossRef]
- O’Carroll, E. The teaching of occlusion in undergraduate dental schools in the UK and Ireland. Br. Dent. J. 2019, 227, 512–517. [Google Scholar] [CrossRef]
- Lee, D.J.; Wiens, J.P.; Ference, J.; Donatelli, D.; Smith, R.M.; Dye, B.D.; Obrez, A.; Lang, L.A. Assessment of occlusion curriculum in predoctoral dental education: Report from ACP Task Force on Occlusion Education. J. Prosthodont. 2012, 21, 578–587. [Google Scholar] [CrossRef]
- Truntzer, J.; Lynch, A.; Kruse, D.; Prislin, M. Musculoskeletal education: An assessment of the clinical confidence of medical students. Perspect. Med. Educ. 2014, 3, 238–244. [Google Scholar] [CrossRef]
- Jwayyed, S.; Stiffler, K.; Wilber, S.; Southern, A.; Weigand, J.; Bare, R.; Gerson, L. Technology-assisted education in graduate medical education: A review of the literature. J. Emerg. Med. 2011, 4, 1145–1157. [Google Scholar] [CrossRef]
- Frizziero, L.; Santi, G.M.; Liverani, A.; Napolitano, F.; Papaleo, P.; Maredi, E.; di gennaro, G.; Zarantonello, P.; Stallone, S.; Stilli, S.; et al. Computer-Aided Surgical Simulation for Correcting Complex Limb Deformities in Children. Appl. Sci. 2020, 10, 5181. [Google Scholar] [CrossRef]
- Buchanan, J.A. Experience with virtual reality-based technology in teaching restorative dental procedures. J. Dent. Educ. 2004, 68, 1258–1265. [Google Scholar] [CrossRef] [PubMed]
- Eve, E.J.; Koo, S.; Alshihri, A.A.; Cormier, J.; Kozhenikov, M.; Donoff, R.B.; Karimbux, N.Y. Performance of dental students versus prosthodontics residents on a 3D immersive haptic simulator. J. Dent. Educ. 2014, 78, 630–637. [Google Scholar] [CrossRef] [PubMed]
- Jasinevicius, T.R.; Landers, M.; Nelson, S.; Urbankova, A. An evaluation of two dental simulation systems: Virtual reality versus contemporary non-computer-assisted. J. Dent. Educ. 2004, 68, 1151–1162. [Google Scholar] [CrossRef] [PubMed]
- Pohlenz, P.; Gröbe, A.; Petersik, A.; von Sternberg, N.; Pflesser, B.; Pommert, A.; Höhne, K.H.; Tiede, U.; Springer, I.; Heiland, M. Virtual dental surgery as a new educational tool in dental school. J. Craniomaxillofac. Surg. 2010, 38, 560–564. [Google Scholar] [CrossRef]
- Urbankova, A. Impact of computerized dental simulation training on preclinical operative dentistry examination scores. J. Dent. Educ. 2010, 74, 402–409. [Google Scholar] [CrossRef]
- Zitzmann, N.; Matthisson, L.; Ohla, H.; Joda, T. Digital Undergraduate Education in Dentistry: A Systematic Review. Int. J. Environ. Res. Public. Health 2020, 17, 3269. [Google Scholar] [CrossRef]
- Kwon, C. The Effect of the Degree of Anxiety of Learners during the Use of VR on the Flow and Learning Effect. Appl. Sci. 2020, 10, 4932. [Google Scholar] [CrossRef]
- Van Helvoort, D.; Stobbe, E.; Benning, R.; Otgaar, H.; Ven, V. Physical exploration of a virtual reality environment: Effects on spatiotemporal associative recognition of episodic memory. Mem. Cogn. 2020, 48, 691–703. [Google Scholar] [CrossRef]
- Balzer, L.B.; Petersen, M.L.; van der Laan, M.J.; Consortium, T.S. Adaptive pair-matching in randomized trials with unbiased and efficient effect estimation. Stat. Med. 2015, 34, 999–1011. [Google Scholar] [CrossRef]
- Wiens, J. Fundamentals of Occlusion, 1st ed.; American College of Prosthodontists: Chicago, IL, USA, 2015. [Google Scholar]
- Alwin, D.; Krosnick, J. The Reliability of Survey Attitude Measurement. Sociol. Methods Res. 1991, 20, 139–181. [Google Scholar] [CrossRef]
- Husain, H.; Bais, B.; Hussain, A.; Samad, S. How to Construct Open Ended Questions. Procedia Soc. Behav. Sci. 2012, 60, 456–462. [Google Scholar] [CrossRef]
- Schuman, H.; Presser, S. The Open and Closed Question. Am. Sociol. Rev. 1979, 44, 692–712. [Google Scholar] [CrossRef]
- Anderson, L. A critique of grading: Policies, practices, and technical matters. Educ. Policy Anal. Arch. 2018, 26, 49. [Google Scholar] [CrossRef]
- Jofré, J.; Fuentes, J.; Conrady, Y.; Michel, M.; Quintana, P.; Asenjo-Lobos, C. Improving Dental Students Fine Motor Skills by Visualization and Mental Imagery: A Pilot Randomized Clinical Trial. Int. J. Odontostomat. 2019, 13, 69–74. [Google Scholar] [CrossRef]
- Steinert, Y.; Snell, L.S. Interactive lecturing: Strategies for increasing participation in large group presentations. Med. Teach. 2009, 21, 37–42. [Google Scholar]
- Siddiq, F.; Scherer, R.; Tondeur, J. Teachers’ emphasis on developing students’ digital information and communication skills (TEDDICS): A new construct in 21st century education. Comput. Educ. 2016, 92-93, 1–14. [Google Scholar] [CrossRef]
- Singh, R.; Gupta, N.; Singh, G. Learning style and teaching methodology preferences of dental students. J. Anat. Soc. India 2017, 65, 179–186. [Google Scholar] [CrossRef]
- De Boer, I.R.; Wesselink, P.R.; Vervoorn, J.M. Student performance and appreciation using 3D vs. 2D vision in a virtual learning environment. Eur. J. Dent. Educ. 2016, 20, 142–147. [Google Scholar] [CrossRef]
- Perry, S.; Bridges, S.M.; Burrow, M.F. A review of the use of simulation in dental education. Simul. Healthc. 2015, 10, 31–37. [Google Scholar] [CrossRef]
- Rao, A.; Tait, I.; Alijani, A. Systematic review and meta-analysis of the role of mental training in the acquisition of technical skills in surgery. Am. J. Sur. 2015, 210, 545–553. [Google Scholar] [CrossRef]
- Sobierajewicz, J.; Szarkiewicz, S.; Przekoracka-Krawczyk, A.; Jaśkowski, W.; Lubbe, R. To What Extent Can Motor Imagery Replace Motor Execution While Learning a Fine Motor Skill? Cogn. Psychol. 2016, 12, 179–192. [Google Scholar] [CrossRef] [PubMed]
| 2D Presentation Method | 3D Simulation Method | |
|---|---|---|
| Material | book, paper sheet, 2D figures | computer, software, 3D graphic models |
| Contents | descriptive | descriptive, manipulative, analytic |
| Visuospatial information | static | dynamic |
| Teaching method | teacher-centered | student-centered |
| Cost for facility | low | moderate to high |
| Learning method | observation | virtual practice |
| Recommend group size | NS | small to medium |
| Preparation | NS | learning how to operate software |
| Question | Teaching Method | P | |
|---|---|---|---|
| 2D Presentation | 3D Simulation | ||
| Centric | 77.0 ± 9.5 | 82.6 ± 10.3 | 0.034 |
| Eccentric | 66.0 ± 16.7 | 70.3 ± 22.6 | 0.403 |
| Whole | 72.9 ± 10.0 | 78.0 ± 11.0 | 0.064 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mai, H.Y.; Mai, H.-N.; Lee, D.-H. Computer-Based 3D Simulation Method in Dental Occlusion Education: Student Response and Learning Effect. Appl. Sci. 2020, 10, 6073. https://doi.org/10.3390/app10176073
Mai HY, Mai H-N, Lee D-H. Computer-Based 3D Simulation Method in Dental Occlusion Education: Student Response and Learning Effect. Applied Sciences. 2020; 10(17):6073. https://doi.org/10.3390/app10176073
Chicago/Turabian StyleMai, Hai Yen, Hang-Nga Mai, and Du-Hyeong Lee. 2020. "Computer-Based 3D Simulation Method in Dental Occlusion Education: Student Response and Learning Effect" Applied Sciences 10, no. 17: 6073. https://doi.org/10.3390/app10176073
APA StyleMai, H. Y., Mai, H.-N., & Lee, D.-H. (2020). Computer-Based 3D Simulation Method in Dental Occlusion Education: Student Response and Learning Effect. Applied Sciences, 10(17), 6073. https://doi.org/10.3390/app10176073





