Biomechanical Evaluation of the Effects of Implant Neck Wall Thickness and Abutment Screw Size: A 3D Nonlinear Finite Element Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Finite Element (FE) Model Generation
2.2. Nonlinear FE Simulation
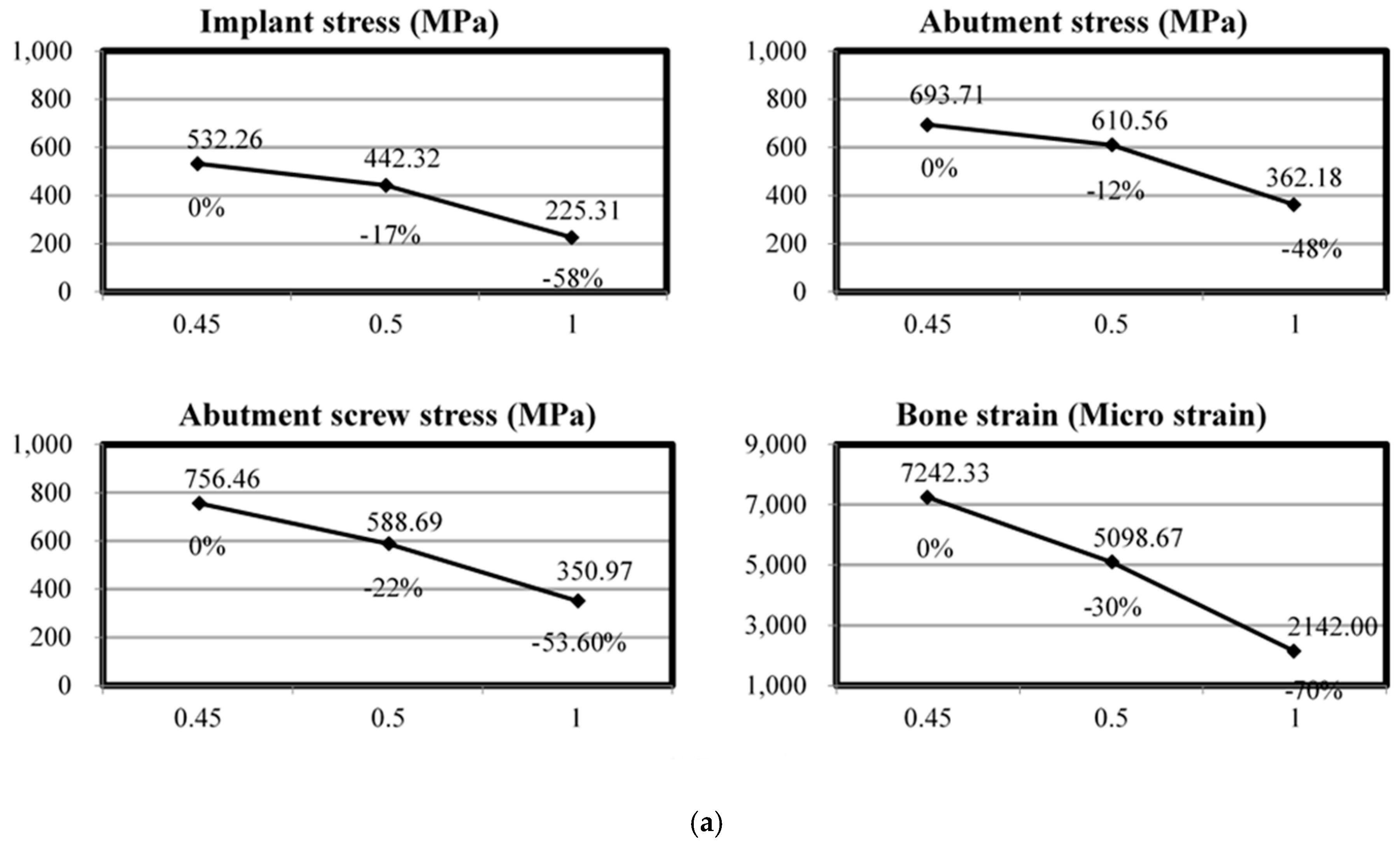
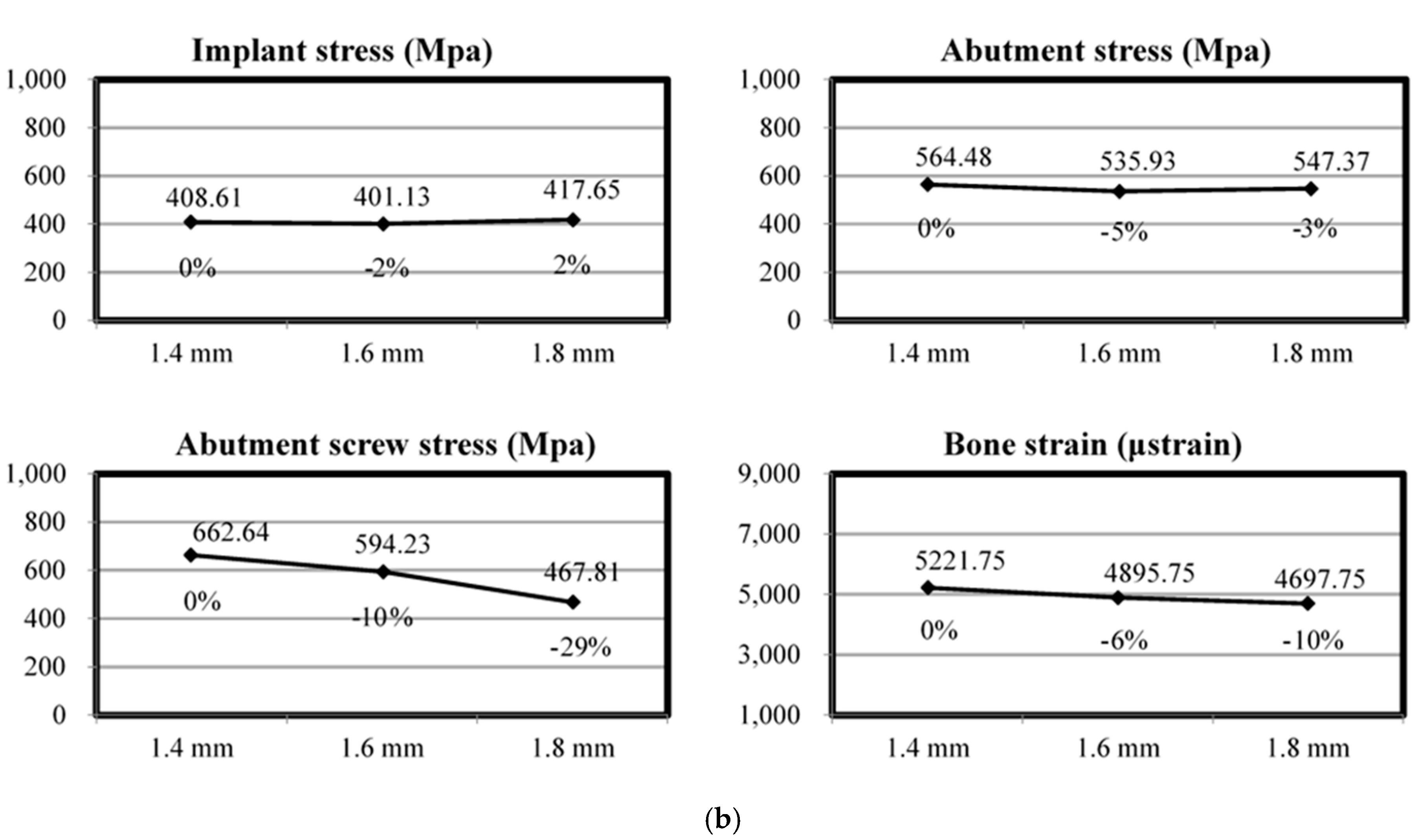
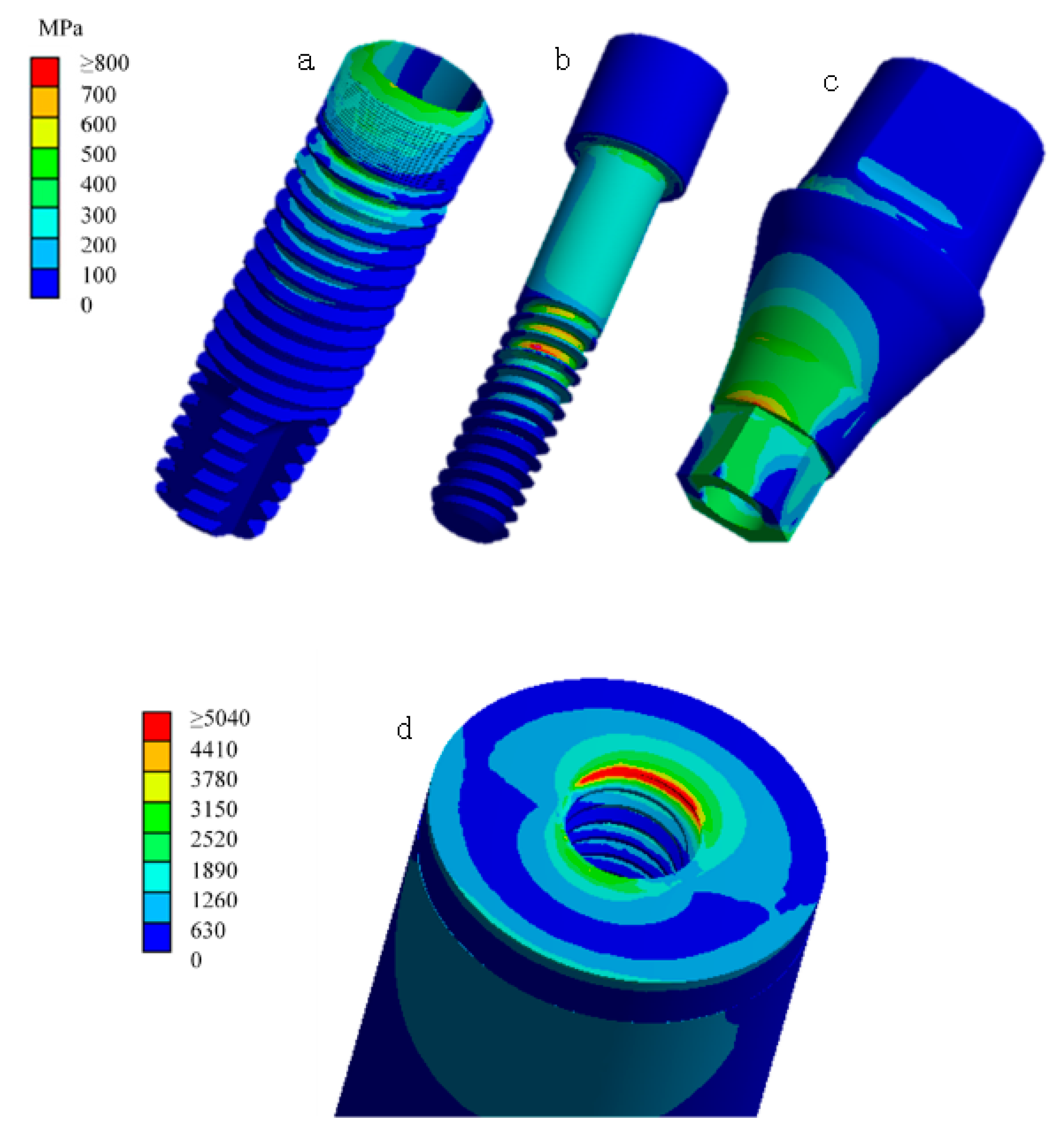
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Data Availability Statement
References
- Sahin, S.; Cehreli, M.C.; Yalcin, E. The influence of functional forces on the biomechanics of implant supported proethses-a review. J. Dent. 2002, 30, 271–282. [Google Scholar] [CrossRef]
- Tada, S.; Stegaroiu, R.; Kitamurs, E.; Miyakawa, O.; Kusakari, H. Influence of implant design and bone quality on stress/strain distribution in bone around implants: A 3-dimensional finite element analysis. Int. J. Oral Maxillofac. Implants 2003, 18, 357–368. [Google Scholar] [PubMed]
- Lin, C.L.; Wang, J.C.; Ramp, L.C.; Liu, P.-R. Biomechanical response of implant systems placed in the maxillary posterior region under various conditions of angulation, bone density, and loading. Int. J. Oral Maxillofac. Implants 2008, 23, 57–64. [Google Scholar]
- Ugurel, C.S.; Steiner, M.; Isik-Ozkol, G.; Kutay, O.; Kern, M. Mechanical resistance of screwless morse taper and screw-retained implant-abutment connections. Clin. Oral Implants Res. 2015, 26, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Caricasulo, R.; Malchiodi, L.; Ghensi, P.; Fantozzi, G.; Cucchi, A. The influence of implant-abutment connection to peri-implant bone loss: A systematic review and meta-analysis. Clin. Implant Dent. Relat. Res. 2018, 20, 653–664. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.C.; Lee, J.; Kim, S.; Koo, K.-T.; Kim, H.-Y.; Luke Yeo, I.-S. Influence of implant-abutment connection structure on peri-implant bone level in a second molar: A 1-year randomized controlled trial. J. Adv. Prosthodont. 2019, 11, 147–154. [Google Scholar] [CrossRef]
- Swami, V.; Vijayaraghavan, V.; Swami, V. Current trends to measure implant stability. J. Indian Prosthodont. Soc. 2016, 16, 124–130. [Google Scholar] [CrossRef]
- Brunski, J.B. Biomechanical factors affecting the bone-dental implant interface. Clin. Mater. 1992, 10, 153–201. [Google Scholar] [CrossRef]
- Lin, C.L.; Lin, Y.H.; Chang, S.H. Multi-factorial analysis of variables influencing the bone loss of an implant placed in the maxilla: Prediction using FEA and SED bone remodeling algorithm. J. Biomech. 2010, 43, 644–651. [Google Scholar] [CrossRef]
- Albrektsson, T.; Dahlin, C.; Jemt, T.; Sennerby, L.; Turri, A.; Wennerberg, A. Is marginal bone loss around oral implants the result of a provoked foreign body reaction? Clin. Implant Dent. Relat. Res. 2014, 16, 155–165. [Google Scholar] [CrossRef]
- Baffone, G.M.; Botticelli, D.; Pantani, F.; Cardoso, L.C.; Schweikert, M.T.; Lang, N.P. Influence of various implant platform configurations on peri-implant tissue dimensions: An experimental study in dog. Clin. Oral Implants Res. 2011, 22, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Bateli, M.; Att, W.; Strub, J.R. Implant neck configurations for preservation of marginal bone level: A systematic review. Int. J. Oral Maxillofac. Implants 2011, 26, 290–303. [Google Scholar]
- Nishioka, R.S.; de Vasconcellos, L.G.; de Melo Nishioka, G.N. Comparative strain gauge analysis of external and internal hexagon, Morse taper, and influence of straight and offset implant configuration. Implant Dent. 2011, 20, e24–e32. [Google Scholar] [CrossRef] [PubMed]
- Peñarrocha-Diago, M.A.; Flichy-Fernández, A.J.; Alonso-González, R.; Peñarrocha-Oltra, D.; Balaguer-Martínez, J.; Peñarrocha-Diago, M. Influence of implant neck design and implant-abutment connection type on peri-implant health. Radiological study. Clin. Oral Implants Res. 2013, 24, 1192–1200. [Google Scholar] [CrossRef]
- Pozzi, A.; Agliardi, E.; Tallarico, M.; Barlattani, A. Clinical and radiological outcomes of two implants with different prosthetic interfaces and neck configurations: Randomized, controlled, split-mouth clinical trial. Clin. Implant Dent. Relat. Res. 2014, 16, 96–106. [Google Scholar] [CrossRef]
- Lin, M.I.; Shen, Y.W.; Huang, H.L.; Hsu, J.-T.; Fuh, L.-J. A retrospective study of implant-abutment connections on crestal bone level. J. Dent. Res. 2013, 92, 202S–207S. [Google Scholar] [CrossRef]
- Lin, C.L.; Chang, S.H.; Chang, W.J.; Kuo, Y.C. Factorial analysis of variables influencing mechanical characteristics of a single tooth implant placed in the maxilla using finite element analysis and the statistics-based Taguchi method. Eur. J. Oral Sci. 2007, 115, 408–416. [Google Scholar] [CrossRef]
- Bozkaya, D.; Müftü, S. Mechanics of the tapered interference fit in dental implants. J. Biomech. 2003, 36, 1649–1658. [Google Scholar] [CrossRef]
- Saidin, S.; Abdul Kadir, M.R.; Sulaiman, E.; Abu Kasim, N.H. Effects of different implant-abutment connections on micromotion and stress distribution: Prediction of microgap formation. J. Dent. 2012, 40, 467–474. [Google Scholar] [CrossRef]
- Bozkaya, D.; Müftü, S. Mechanics of the taper integrated screwed-in (TIS) abutments used in dental implants. J. Biomech. 2005, 38, 87–97. [Google Scholar] [CrossRef]
- Yi, Y.; Koak, J.Y.; Kim, S.K.; Lee, S.J.; Heo, S.J. Comparison of implant component fractures in external and internal type: A 12-year retrospective study. J. Adv. Prosthodont. 2018, 10, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Mao, Z.; Yi, D.; Cao, G. Influence of sizes of abutments and fixation screws on dental implant system: A non-linear finite element analysis. Biomed. Tech. 2017, 62, 357–364. [Google Scholar] [CrossRef] [PubMed]
- ISO 14801:2016. Dentistry—Implants—Dynamic Loading Test for Endosseous Dental Implants; ISO: Geneve, Switzerland, 2016. [Google Scholar]
- Lin, C.L.; Wang, J.C.; Kuo, Y.C. Numerical simulation on the biomechanical interactions of tooth/implant-supported system under various occlusal forces with rigid/non-rigid connections. J. Biomech. 2006, 39, 453–463. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.L.; Wang, J.C. Nonlinear finite element analysis of a splinted implant with various connectors and occlusal forces. Int. J. Oral Maxillofac. Implants 2003, 18, 331–340. [Google Scholar] [PubMed]
- Lin, C.L.; Kuo, Y.C.; Lin, T.S. Effects of dental implant length and bone quality on biomechanical responses in bone around implants: A 3-D non-linear finite element analysis. Biomed. Eng. Appl. Basis Commun. 2005, 17, 44–49. [Google Scholar] [CrossRef]
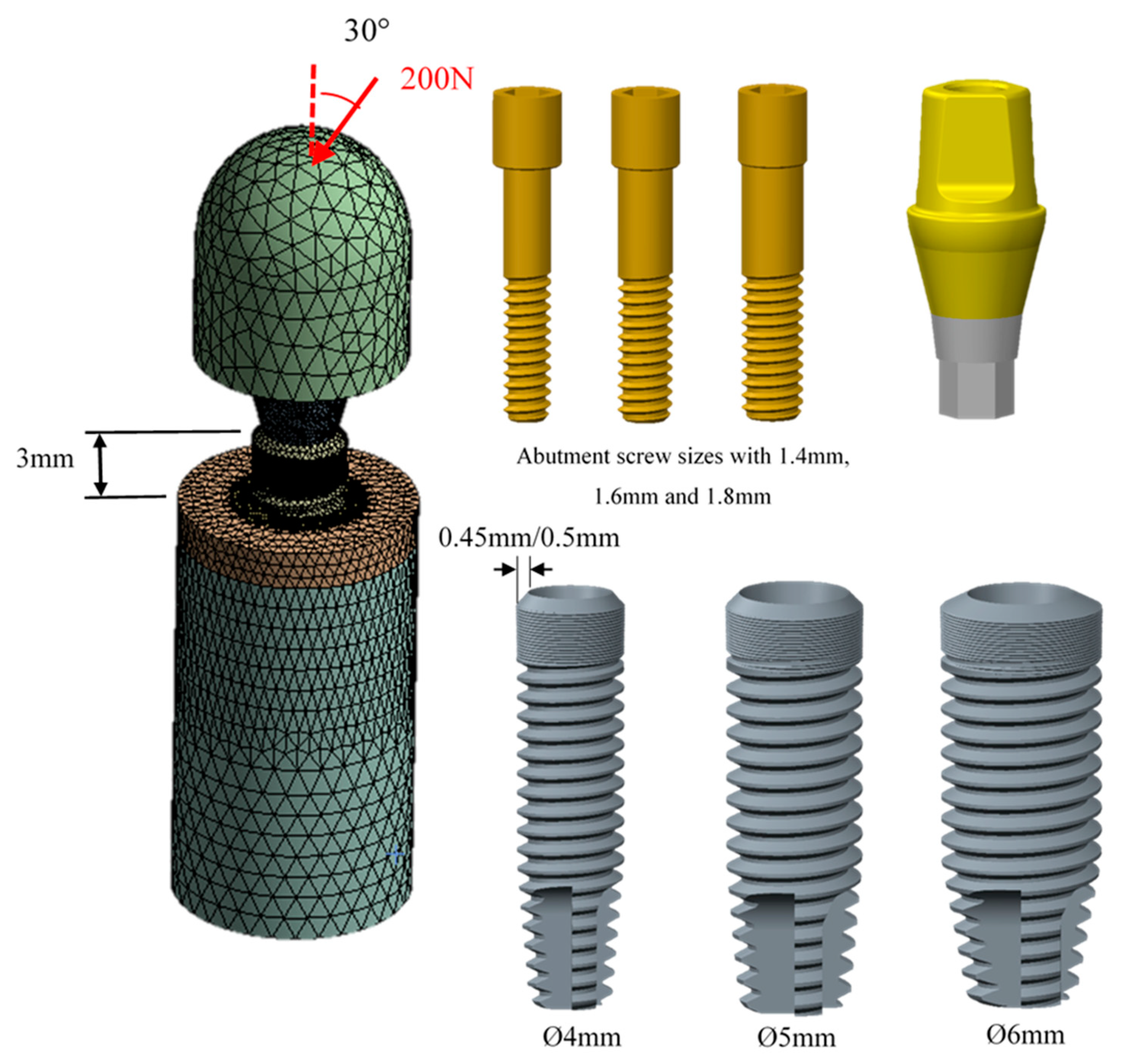
| Diameter of Implant (D) (mm) | Thickness of Implant Neck (t) (mm) | Diameter of Abutment Screw (d) (mm) | Node Number | Element Number | Illustration of Implant Designed |
| Ø4.00 | 0.45 | Ø 1.40 | 442424 | 296904 | 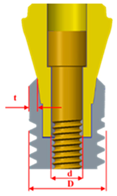 |
| Ø 1.60 | 475068 | 319867 | |||
| Ø 1.80 | 507375 | 342558 | |||
| Ø4.00 | 0.50 | Ø 1.40 | 440134 | 294937 | |
| Ø 1.60 | 472225 | 317487 | |||
| Ø 1.80 | 472896 | 317988 | |||
| Ø5.00 | 0.50 | Ø 1.40 | 543691 | 369648 | |
| Ø 1.60 | 576516 | 392682 | |||
| Ø 1.80 | 606135 | 413360 | |||
| Ø6.00 | 1.00 | Ø 1.40 | 580837 | 395051 | |
| Ø 1.60 | 614518 | 418713 | |||
| Ø 1.80 | 643244 | 438669 |
| Material | Young’s Modulus (GPa) | Poisson’s Ratio |
| Cortical bone | 13.7 | 0.3 |
| Cancellous bone | 1.37 | 0.3 |
| Implant (Ti grade 4) | 105 | 0.3 |
| Abutment (Ti6Al4V) | 110 | 0.35 |
| Abutment screw (Ti6Al4V) | 110 | 0.35 |
| Loading device | 193 | 0.26 |
| Diameter of Implant (mm) | Diameter of Abutment Screw (mm) | Neck Thickness of Implant (mm) | Maximum of Equivalent Stress of Abutment Screw (MPa) | Maximum of Equivalent Stress of Abutment (MPa) | Maximum of Equivalent Stress of Implant (MPa) | Maximum of Principle Strain of Cortical Bone (μstrain) |
| 4 | 1.4 | 0.45 | 876.35 | 726.62 | 536.24 | 8149 |
| 4 | 1.6 | 0.45 | 723.25 | 655.70 | 512.84 | 7053 |
| 4 | 1.8 | 0.45 | 669.79 | 698.81 | 547.70 | 6525 |
| 4 | 1.4 | 0.50 | 725.08 | 820.32 | 556.47 | 7301 |
| 4 | 1.6 | 0.50 | 709.62 | 780.36 | 542.49 | 7048 |
| 4 | 1.8 | 0.50 | 434.73 | 735.41 | 578.34 | 7022 |
| 5 | 1.4 | 0.50 | 633.19 | 359.40 | 327.29 | 3241 |
| 5 | 1.6 | 0.50 | 608.49 | 345.75 | 324.51 | 3327 |
| 5 | 1.8 | 0.50 | 465.29 | 382.16 | 307.73 | 3169 |
| 6 | 1.4 | 1.00 | 415.93 | 351.56 | 214.42 | 2196 |
| 6 | 1.6 | 1.00 | 335.55 | 361.90 | 224.69 | 2155 |
| 6 | 1.8 | 1.00 | 301.44 | 373.09 | 236.83 | 2075 |
| Implant Stress | Abutment Stress | Abutment Screw Stress | Bone Strain | |
| Implant neck wall thickness | <0.001 | 0.039 | 0.002 | 0.002 |
| Abutment screw size | <0.001 | 0.961 | 0.960 | 0.817 |
| Implant neck wall thickness * Abutment screw size | 0.021 | 0.999 | 0.998 | 0.977 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeng, M.-D.; Lin, Y.-S.; Lin, C.-L. Biomechanical Evaluation of the Effects of Implant Neck Wall Thickness and Abutment Screw Size: A 3D Nonlinear Finite Element Analysis. Appl. Sci. 2020, 10, 3471. https://doi.org/10.3390/app10103471
Jeng M-D, Lin Y-S, Lin C-L. Biomechanical Evaluation of the Effects of Implant Neck Wall Thickness and Abutment Screw Size: A 3D Nonlinear Finite Element Analysis. Applied Sciences. 2020; 10(10):3471. https://doi.org/10.3390/app10103471
Chicago/Turabian StyleJeng, Ming-Dih, Yang-Sung Lin, and Chun-Li Lin. 2020. "Biomechanical Evaluation of the Effects of Implant Neck Wall Thickness and Abutment Screw Size: A 3D Nonlinear Finite Element Analysis" Applied Sciences 10, no. 10: 3471. https://doi.org/10.3390/app10103471
APA StyleJeng, M.-D., Lin, Y.-S., & Lin, C.-L. (2020). Biomechanical Evaluation of the Effects of Implant Neck Wall Thickness and Abutment Screw Size: A 3D Nonlinear Finite Element Analysis. Applied Sciences, 10(10), 3471. https://doi.org/10.3390/app10103471






