Abstract
The COVID-19 (coronavirus disease) pandemic has had a significant impact on the healthcare delivery system worldwide. Many pre-pandemic norms, standards, and methods of providing medical services in most medical facilities had to be changed and re-evaluated. Many of them will likely stay changed and will probably never be provided in the same way in post-pandemic reality. The COVID-19 crisis is still ongoing and some sources say that we should be prepared for a third wave of the pandemic. The scope of the analysis conducted in this publication is related to the healthcare sector, including services and Polish healthcare professionals’ work quality during the COVID-19 crisis. The research gap, the basis for conducting new research, is the lack of clarified results analysing the quality assurance of healthcare workers during the COVID-19 pandemic. It is necessary to ask about healthcare professionals’ rate of personal protective equipment quality in Polish medical facilities. The result of cluster analysis will help us to know what the clusters for variables on quality assurance of protection measures for healthcare workers are. The research was carried out using a questionnaire survey on a sample of 21 medical personnel in Polish hospitals. The main findings of this publication are problems with information flow between staff and staff managers and determining appropriate zones. The quality of the personal protective equipment offered by medical facilities’ management and their availability is at an appropriate level. The publication aims to analyse the level of quality assurance of health care worker protection measures in the example of Silesian voivodeships in Poland during the COVID-19 pandemic.
1. Introduction
In times of a COVID-19 outbreak, it is important to ensure that the quality of health care services is adequate to enable the proper execution of medical procedures. For medical staff to carry out their tasks in this regard, the employer must provide them with adequate protective measures to enable them to carry out the procedures used for COVID-19 patients.
The provision of high-quality protection measures for health workers is also important because, in a pandemic, health facilities are often a significant source of COVID-19 transmission, and their inadequate organization may not only fail to contain the pandemic, but may even contribute to the spread of the virus (Dixon 2021; Howells et al. 2021; Deloitte 2021). For this reason, the issue of investigating the level of quality assurance of health worker protection measures is not only scientifically important, but also very important for social reasons. Based on the analysis of the international publication databases (Austin and Kachalia 2020; Fitzsimons 2021; European Union 2020a, 2020b; Roder-DeWan 2020; Belasen et al. 2020; Shirazi et al. 2020). There is a research gap in the analysis of the quality assurance of protective measures for health workers during the COVID-19 pandemic. This publication aims to analyse the level of quality assurance of health care worker protection measures, with the example of Silesian voivodeships in Poland during the COVID-19 pandemic.
This publication poses two research questions:
- What are the clusters for the variables on quality assurance of protection measures for health workers during the COVID-19 pandemic?
- How do healthcare workers rate the implementation of quality assurance of protection measures by the employer?
2. Literature Review
The COVID-19 pandemic has had a significant impact on the whole world, including societies in different countries, but people who most have to deal with this disease are healthcare workers and medical facilities’ staff (Gajdzik and Wolniak 2021). From a psychological point of view, this group of people is especially vulnerable to mental stress, which is associated with a sense of anxiety, insecurity, as well as a sense of resignation and acceleration of burnout (Aleinikov et al. 2020; Atlani-Duault et al. 2020). In the case of the COVID-19 pandemic, the level of the personal protective equipment of healthcare workers has significant importance on the healthcare system stability of entire countries (Hon et al. 2008). The pandemic highlighted strong and weak sides of healthcare systems in different countries all over the world (Austin and Kachalia 2020). One of the major strengths is the healthcare professionals’ dedication to fighting the disease, to provide the best care for patients (Howells et al. 2021; Austin and Kachalia 2020; Roder-DeWan 2020; Gallagher et al. 2020). Nevertheless, assessing the quality of healthcare provided during the pandemic is a difficult and complex issue. The one aspect of quality assessment is patients’ satisfaction (Wolniak and Skotnicka-Zasadzień 2018; Ferreira and Borges 2020; Pacana et al. 2014). On the other hand, a lack of medical staff and an emergency, that forces medical facilities to follow slightly different procedures and work differently than in ordinary cases, make what previously were considered as factors that guarantee patient satisfaction take on a different meaning, or in extreme situations may even be marginalized (Belasen et al. 2020; Shirazi et al. 2020; Teng et al. 2020). The other point of view connected to patients’ satisfaction in COVID-19 pandemic times was introduced in the year 2020 as a result of research conducted by Shirazi et al., which investigated patients and customers satisfaction in private clinics and hospitals in Iran. The results clearly showed that hospitals which once worked well are losing their efficiency during the COVID-19 crisis, caused by the health conditions of medical staff (Shirazi et al. 2020; Shreffler et al. 2020). One of the key factors, which directly impacts healthcare providing quality, is the physical and mental health of professionals working in hospitals and other medical facilities over the world (Howells et al. 2021; Austin and Kachalia 2020; Shirazi et al. 2020; Teng et al. 2020; Shreffler et al. 2020; Wolniak and Skotnicka-Zasadzień 2012). The COVID-19 crisis sped up organizational and procedural changes and developed an approach to protective equipment usage, its limitation, and issues, which were not very significant in the “pre-Covid” world (Fitzsimons 2021). According to research conducted in 2020 by Adams and Walls, Sars-CoV-2 (Severe acute respiratory syndrome coronavirus 2) disease caused 22 deaths among 3000 healthcare workers in China. According to the Centres for Disease Control and Prevention (CDC), the best way to limit Coronavirus transmission is using barrier precautions, environmental hygiene, and practicing overall sound hygiene (Adams and Walls 2020; World Health Organisation 2014, 2020). However, 2014 WHO “Infection Prevention and Control of Epidemic- and Pandemic-Prone Acute Respiratory Infections in Health Care” guidelines suggest that the incidence of transmission respiratory diseases, which are caused by viruses, depend on (World Health Organisation 2014, 2020):
- changes in human behaviour and demographics;
- technology impact and its development;
- industry;
- economic growth and development;
- commerce travels;
- microbial adaptation and change;
- poor implementation of public health measures;
- domestic, wild animals, and birds in environments in which people are living.
It is worth noting that, the above-mentioned factors relate to various possibilities of transmitting infectious diseases of the respiratory system, not only the COVID-19. However, it can be concluded that some of them are common to most infectious diseases of the human respiratory system, including the COVID-19 now (Wolniak and Skotnicka-Zasadzień 2012; World Health Organisation 2014; Qiu et al. 2020; Morawska and Milton 2020; Mick and Murphy 2020; Beam et al. 2011). World Health Organization (WHO) guidelines from the year 2020 and the Centres for Disease Control and Preventions recommend the use of personal protective equipment by healthcare professionals during every instance contact with every patient, who may be potentially infected. To minimize the risk of virus transmission and infection during treating patients with Covid-19, the Centres for Disease Control (CDC) and WHO suggest treating listed below precautions with a special priority (Shreffler et al. 2020; Adams and Walls 2020; Qiu et al. 2020; Morawska and Milton 2020; Mick and Murphy 2020; Beam et al. 2011; CDC 2020):
- gloves;
- gown;
- masks (especially N95);
- eyewear;
- face shield or Powered Air Purifying Respirator (PAPR);
- disinfecting hands;
- decontaminating (if there is a possibility) parts of protective equipment;
- decontaminating surfaces;
- decontaminating items which have contact with patients and medical staff;
- using also masks for patients;
- waste management; prevention of needle sticks or sharps injuries.
Unfortunately, especially in pandemic times, the availability of personal protective equipment is more and more limited (Diptanu et al. 2020; Boškoski et al. 2020). It is necessary to take a question about the usage of personal protective equipment, its efficiency, and safety-providing quality. The research connected to this issue was conducted by Hedge. The results were introduced in the year 2020. The experiment consisted of testing the effectiveness of various personal protective equipment for healthcare workers, they were highly exposed to factors causing infectious and viral diseases. Additionally, this study also consisted of testing the effectiveness of modified personal protective equipment. Researchers found that some differentiation in the way of personal protective equipment’s parts can lead to an improvement in safety level. For example, The contamination risk can be decreased by a sealed gown and glove combination. They can be removed together and also covers wrists areas. Another example can be a tight-fitting gown around the neck, wrist area, and hands. For the additional comfort of use, decontamination, and safety, the added tabs to facilitate doffing of masks, can be added. The main results, which showed what parts of protective equipment provide the best safety level and the fact about full body-covering suit (Hegde 2020) showed:
- The more of body parts are covered the better protection is ensured. However, the comfort of donning and doffing is less than in the case of multiple-parts personal protective equipment;
- Protective suits are most uncomfortable to wear and for removing parts of equipment, but provides the best safety level;
- Long gowns and aprons also provide best safety level.
The next issue, which is connected to personal protective equipment used in the work of healthcare workers, and the real level of safety and probability of risk minimalization, is their approach to using this equipment (Kang et al. 2017; Rowan and Laffey 2020; Rowan and Laffey 2021). There are barriers and limitations in personal protective equipment usage among healthcare workers. There are few major following limitations of Personal protective equipment (PPE) usage (Rowan and Laffey 2020): Time-consumable activity:
- (1)
- Time-consumable activity:
There are numerous situations in which medical staff do not have so much time (especially in emergency cases) to wear full protection suits, which consist of numerous parts. Some medical staff (rather not in pandemic times) say: One question to patient and I must wear all this stuff”. The next aspect is that the time of wearing equipment is sometimes the same as the time it takes to complete the task (Kang et al. 2017; Rowan and Laffey 2020, 2021).
- (2)
- Lack of comfort and cumbersomeness:
Protective equipment sometimes makes it harder to handle some kind of medical device. Additionally, Powered Air Purifying Respirator (PAPR) is big and in connection with gowns, aprons, suits can also be annoying for the wearer or even make moving around impossible. Discomfort after wearing these parts can also occur. (Hegde 2020; Kang et al. 2017; Rowan and Laffey 2020, 2021).
- (3)
- Lack of training:
Issues connected to knowledge about procedures of donning personal protective equipment, lack of experience in equipment usage, sometimes the difficulty in wearing more than 1 layer occurs (Kang et al. 2017; Narayane et al. 2020).
- (4)
- Doubts about the effectiveness of personal protective equipment:
Some medical staff has concerns that the equipment they use is the real barrier for viruses, etc. Some people pay attention to the fact, that while doffing equipment they “feel contaminated” (fear of contact with the outer layers of gowns, masks, etc.) (Hegde 2020; Kang et al. 2017; Rowan and Laffey 2020; Narayane et al. 2020; Meng et al. 2020).
- (5)
- Different problems with equipment:
The obvious problem (especially during a pandemic) is the limitation of personal protective equipment, most parts of it are not decontaminating such as surgical masks, n95 masks, gloves, etc. Some of the stuff can be reused, but the limited number of times, i.e., Gowns can be decontaminated, but not indefinitely, Powered Air Purifying Respirator (PAPR) equipment needs electricity (often battery pack) to run (Boškoski et al. 2020; Hegde 2020; Kang et al. 2017; Rowan and Laffey 2021; Meng et al. 2020).
- (6)
- Other problematic factors such discomfort caused by high outside temperature, laziness, etc. (Kang et al. 2017; Kim and Choi 2016; Verbeek et al. 2020):
The good practice and idea of dealing with personal protective equipment and the contaminated or potentially contaminated area were introduced in the publication “Radiology department strategies to protect radiologic technologists against COVID-19: Experience from Wuhan” (Kim and Choi 2016). In the publication, environmental modifications in the radiology department in one of Wu-Han city hospitals were presented. A very interesting conception of decreasing the risk of healthcare workers’ infection is setting up three areas: clean, potentially contaminated, and contaminated. Each area is separated by a buffer room. Additionally, passages for patients and medical personnel were separated to avoid cross-infection of patients and medical staff (Kim and Choi 2016). The new order of putting on and doffing personal protective equipment parts was also “reinvented”. Particular attention was also paid to air purifiers, UV lamps, and personal hygiene before leaving home from work (Kim and Choi 2016).
However, the particular attention to personal protective equipment in times of a pandemic is not only good practice and duty of medical personnel, but of all people living in society and having contact with other people. According to CDC, COVID-19 can be transmitted in the following ways (Beam et al. 2011; Zhao et al. 2020; Phan et al. 2020; Zhu 2020; Brlek et al. 2020; Shen et al. 2020):
- Contact—when the infection is transmitted through direct contact with an infected person or contaminated surface (touching, handshakes, etc.);
- Droplet transmission—infecting during exposure to the virus-containing respiratory droplets, which are exhaled by an infected person. The virus transmission occurs when somebody is close to an infected person or people, within about nearly 180 cm;
- Airborne transmission—infection spread through exposure to the virus-containing respiratory droplets and particles exhaled by an infectious person. The virus transmission can occur when somebody is close to an infected person, within about 6 feet.
The different researches in connection to quality and patients’ satisfactions were conducted in numerous positions, introduced in the “literature review” section. One of the most interesting is the influence of COVID-19 on the quality of private hospitals in India, the result was the fact that COVID-19 is the factor that decreases the level of healthcare quality (Shirazi et al. 2020). Another point of view on medical services quality and providing healthcare is a study on low-income countries. Studies and observations showed that in Tanzanian hospitals, a long time before the COVID-19 outbreak (2018), correct hand hygiene was observed 6.9% of the time, reusable equipment disinfected 4.8% of the time, gloves appropriately used for 74.8% of indications, and waste correctly managed in 43.3% of cases (Roder-DeWan 2020). The other case is the fact that working in personal protective equipment can be burdensome for healthcare workers and cause discomfort, even after taking off. Research conducted in Wuhan hospitals showed that long-term wearing and working in protective equipment can cause: discomfort; dizziness or palpitation; chest distress or dyspnea; nausea or vomiting; micturition desire; retroauricular pain (mask pressure-related); thirst or dry throat. Most healthcare workers complained about retroauricular pain (Branovački et al. 2021). Similar methodology approach to COVID-19 and issues connected with were presented in the publication “Clustering analysis of countries using the COVID-19 cases dataset”.
3. Methodology
The research presented in this article presents the implementation of quality assurance of personal protective equipment for medical personnel. The research was carried out using a questionnaire survey on a sample of 21—medical personnel in Polish hospitals located in the Silesian Voivodeship. As a result of the expert analysis, 20 variables affecting the implementation of quality assurance of personal protective equipment for health care workers were identified.
Z1: The employees are regularly and scrupulously informed about the possibility of the occurrence of infections with infectious or viral diseases among both patients and hospital employees;
Z2: Employees are trained and informed (should also be reminded) about the behaviour and scope of special precautions in epidemic conditions;
Z3: Parking spaces and driveways for ambulance vehicles are marked;
Z4: Parking spaces and driveways for ambulances bringing patients with suspected infectious or viral disease should be marked, secured, and separated;
Z5: There is a secure point on the hospital premises where patients with suspected infectious or viral illness can be admitted;
Z6: It is ensured that parking spaces designated for ambulance vehicles are not occupied by unauthorized persons;
Z7: The hospital emergency room and entrances to the hospital are equipped with personnel and equipment to measure the temperature of persons entering the premises;
Z8: The hospital emergency room and all other wards of the hospital have guidelines and procedures for individual application for each employee in the event of contact with a patient or a person with suspected infectious or viral disease;
Z9: The Hospital’s toilets and showers are separate for employees and patients;
Z10: The hospital has hand disinfection points for people entering and leaving the building;
Z11: The hospital has separate hand disinfection points for employees;
Z12: The hospital has separate hand disinfection facilities for staff in particularly aseptic-sensitive areas;
Z13: The hospital authorities provide an individual set of handwashing and disinfecting liquids for each employee;
Z14: Hospital authorities ensure access to individual items of personal protection such as gloves, masks, visors, protective goggles, aprons for employees;
Z15: The hospital authorities provide a full set of individual protective clothing for each employee;
Z16: The hospital has a place for decontamination of protective suits and their reusable elements;
Z17: The hospital provides the possibility of decontamination of protective suits, change of elements such as protective masks, visors, gloves, aprons to each employee in a situation when such a need is identified or by safety regulations and hospital procedures;
Z18: Flat surfaces and those exposed to direct contact with persons with potentially infectious or viral diseases are disinfected regularly;
Z19: Disinfection of medical equipment in direct contact with both patients and hospital staff is carried out after each contact with a patient;
Z20: Hospital employees are protected from contact with persons potentially ill with infectious or viral diseases by limiting visits to the hospital and applying guidelines for the stay of patients in individual hospital departments.
The research was conducted in the last quarter of 2020, individual variables were assessed on a 7-point scale.
Cluster analysis was used to analyse the relationships between the studied variables. Cluster analysis is a method of unsupervised learning (Thrun 2018). It is a method that groups elements into relatively homogeneous classes. The basis for clustering in most algorithms is the similarity between elements—expressed by a similarity function (metric). Agglomerative procedures were used in the analysis, which creates a similarity matrix of classified objects and then, in subsequent steps, combines the most similar objects into clusters (Wolniak et al. 2019; Murtagh and Legendre 2011).
Euclidean distances were used in the analysis. Euclidean distances are expressed by the formula:
where: x = (x1, …, xp) and y = (y1 …, yp).
In cluster analysis, it is not necessary to fulfil the assumptions of linearity and normality of the variables. However, it requires the assumption of the absence of collinearity between variables, as collinearity makes it difficult to assess the “true” impact of individual variables. Ward’s method was chosen to combine the ties, as the collected data fulfil the conditions allowing for its application (Ward 1963). This method uses an analysis of variance approach to estimate the distance between clusters. In short, the method aims to minimize the sum of squares of deviations of any two clusters that can be formed at each stage (Omran et al. 2007; Pacana et al. 2020; Xia et al. 2020; Zarikas et al. 2020). STATISTICA 12 (Statistica is an advanced analytics software package originally developed by StatSoft) software was used for the calculations.
4. Results
Table 1 and Figure 1 show the results of the assessment of the level of quality assurance of personal protective equipment of the surveyed health workers.

Table 1.
The quality of services level assessment.
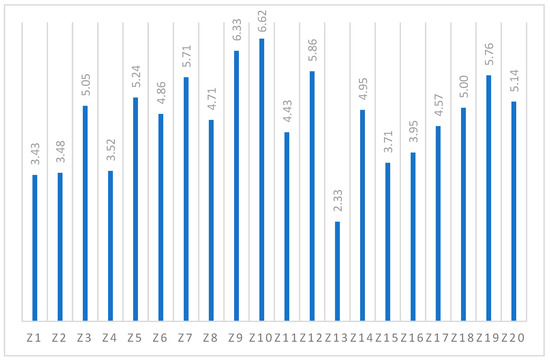
Figure 1.
Level of quality assurance of health measures. Source: Author’s own research.
From the data collected, the highest-rated variables include:
- ▪
- Hand disinfection points for people entering and leaving the building—a score of 6.62;
- ▪
- The hospital’s toilets and showers are located separately for staff and patients—a score of 6.33;
- ▪
- The hospital has separate hand disinfection points for staff in particularly aseptic areas—rating 5.86;
- ▪
- The hospital’s emergency room and entrances to the hospital are equipped with staff and equipment to measure the temperature of persons entering the facility—rating 5.71.
The main shortcomings in the provision of protection measures by employers to health workers include:
- ▪
- The hospital authorities provide an individual set of handwashing and disinfecting liquids for each employee—rating 2.33;
- ▪
- Employees are regularly and scrupulously informed and the possibility of infectious or viral disease cases among patients and hospital staff—rating 3.43;
- ▪
- Employees are trained and informed about the behaviour and scope of special precautions in epidemic conditions—rating 3.48.
As mentioned in the methodological part, the agglomeration method—Ward’s cluster analysis—was used to group the variables. Figure 2 shows the performed cluster analysis for the studied 20 variables. The study shows that 4 clusters can be distinguished:
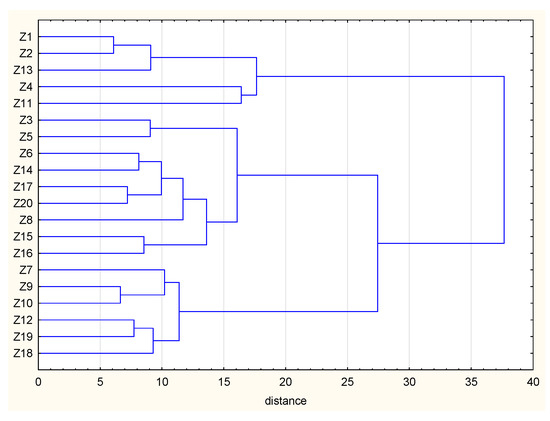
Figure 2.
Cluster analysis for quality assurance variables of health worker protection measures.
- Cluster 1 consists of 3 variables—The variables that make up the focus relate to regularly informing staff of the possibility of cases of infection; training and informing staff on the use of precautions in epidemic conditions and the provision by the hospital authorities of an individual set of hand washing and disinfecting liquids for each staff member. The cluster was named—information flow;
- Cluster 2 consist of 2 variables—clear signage, security and separation of parking areas and ramps for ambulances bringing patients with suspected COVID-19 and separate hand disinfection points for staff. Cluster named—separation of COVID-19 risk areas;
- Cluster 3 consist of 9 variables—These consist of issues relating to: signposting of ambulance parking areas and driveways; a secure point within the hospital where a patient with suspected COVID-19 can be admitted; ensuring that parking areas designated for ambulance vehicles are not occupied by unauthorised persons; ensuring access to individual personal protective items for staff; being able to decontaminate protective outfits for staff and replace them; protecting hospital staff from contact with people potentially ill with viral diseases by limiting hospital visits and applying guidelines; the hospital has guidelines and procedures in place for individual use by each staff member in the event of contact with a patient or person with a suspected infectious disease. The cluster was named—adherence to COVID-19 procedures.
- Cluster 4 consists of the 6 variables—the hospital is equipped to measure the temperature of people entering; hospital toilets and showers are separate for staff and patients; the hospital has hand disinfection points for people entering and leaving; the hospital has separate disinfection points for staff; disinfection of medical equipment in contact with patients and staff is carried out after each patient contact; flat surfaces and those exposed to direct contact with people suspected of having COVID-19 are disinfected regularly. The cluster was named—ensuring adequate disinfection. Figure 3 shows different clusters.
 Figure 3. Clusters identified in quality assurance variables of health worker protection.
Figure 3. Clusters identified in quality assurance variables of health worker protection.
5. Discussion and Conclusions
In this research, cluster analysis was used for group countries due to the time and increase in infections of COVID-19. The conclusions are drawn from the cluster analysis also apply to the healthcare system. Authors concluded that countries at a sub-level of economic development, population, etc., with similar COVID-19 infections increase can be considered as similarly burdened with too high demands on health systems. Additionally, in this paper, the algorithms, which can be used for clustering groups according to the increase in the number of infections and is based on Euclidean distance was presented (Mulenga and Marbán 2020). The other publication, which also uses cluster analysis, is online math learning in Zambia during the COVID-19 pandemic (Omran et al. 2007). It is necessary to also look at social researches, which are based on cluster analysis conducted by Trzebiński et al. 2020. Very interesting results have come from researches connected to feelings of fear and negative emotions connected to isolation during pandemic times. The results show that most people “are capable of effectively managing the negative effects of isolation despite the fact they were also most consistent in complying with the government health directives” (Trzebiński et al. 2020). The other kind of research based on cluster analysis is trying to “cluster” people types of reacts and behaviour during the first few weeks from a pandemic outbreak. In this research, 3 types of people’s behaviour were described and assigned to one of the several clusters: “adapted”, “antagonistic”, “passed”. These clusters described the reaction to pandemic (Branovački et al. 2021; Orzeł and Horodecka 2021; Tang et al. 2020). It may be a good idea to conduct cluster analysis research about physical reactions of medical staff and their emotions, such as: fear, stress, sense of safety connected to good personal protective equipment quality, etc., in Polish medical facilities. The other idea to conduct cluster-analysis research is the personality type of healthcare professionals influence their approach to pandemic-fight challenge and risks connected with it. Such research could be based on the Big Five Model of personality. The survey conducted during research shows that a very serious deficiency in ensuring the quality of employee health protection measures in the surveyed facilities is the flow of information. Problems related to adequate information of employees on issues related to self-protection, as well as rules of conduct in COVID-19 pandemic times, are implemented at a much lower level than issues related to access to disinfectants. Problems also occur concerning the proper separation of COVID-19 risk areas. Medical facilities have considerable problems with this and are not always able to properly separate and label the relevant areas. The survey showed that the “hard” aspects of quality assurance of protection measures for healthcare workers are implemented at a much higher level than the soft aspects. It appears that the surveyed medical facilities provide adequate disinfectants at a good level, also the issues of compliance with COVID-19 procedures are implemented at a decent level. On the other hand, the biggest problems lie in the “soft” aspects of the surveyed issue. This is interesting as it might seem that the implementation of soft aspects, such as ensuring the proper flow of information concerning COVID-19 and related procedures, is not difficult and does not require large resources. However, in this area, the biggest problems occur. It seems that the reason for this may lie in the lack of knowledge of hospital managers regarding the need to provide much more information to staff. In the case of COVID-19, there is a lot of contradictory information in the media resulting in increased levels of uncertainty for medical staff and sometimes a misunderstanding of decisions taken by hospital management or national authorities (Branovački et al. 2021; Orzeł and Horodecka 2021; Springer, 2021; Orzeł, 2021; Tang et al. 2020). The provision of detailed information on this subject can help to improve their satisfaction and ultimately better delivery of medical services. Additionally, according to a study on information and personal protective equipment usage: “To a vast extent, face-to-face training may reduce non-compliance with doffing guidance” (CDC 2020). Additionally, according to a study on information and personal protective equipment usage: “To a vast extent, face-to-face training may reduce non-compliance with doffing guidance” (CDC 2020). This study shows that, despite emergencies and unusual situations, an appropriate approach to the use of protective equipment and training are essential. Based on the research, the following recommendations can be made for managers of medical facilities in COVID-19 conditions:
- ▪
- Provide workers with adequate and reliable information on the current status of the COVID-19 outbreak and the methods and ways to combat it;
- ▪
- Staff should be trained on the need to take precautions during an outbreak;
- ▪
- Special attention should be paid to the proper delineation of COVID-19 risk areas. This will facilitate the securing of such areas and reduce the likelihood of virus transmission.
There are some limitations of the study. The first one is the operationalization of variables. The conception of variables operationalization used in the presented paper is one of many possibilities. Another operationalization can be done by other researchers. The second limitation was connected with a small sample of the medical staff which was the base of the paper. This study presents only results of research conducted in Silesian voivodeship in Poland and it is not possible to generalize it on all populations.
Author Contributions
The main activities of the team of authors can be described as follows: Conceptualization, B.O., R.W.; methodology, B.O., R.W., software, B.O., R.W.; validation, B.O., R.W.; formal analysis B.O., R.W.; investigation, B.O.; resources, A B.O., R.W.; data curation, B.O., R.W.; writing—original draft preparation, B.O., R.W.; writing—review and editing, B.O., R.W.; visualization, B.O., R.W., supervision, R.W.; funding acquisition, R.W. All authors have read and agreed to the published version of the manuscript.
Funding
The analysis in this publication has been made in the course of the internal research project of Silesian University of Technology project 13/010/BK_21/0057.
Data Availability Statement
Data is contained within the article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Adams, James G., and Ron M. Walls. 2020. Supporting the health care workforce during the COVID-19 global epidemic. JAMA 323: 1439–40. [Google Scholar] [CrossRef]
- Aleinikov, A. V., D. A. Maltseva, and A. N. Sunami. 2020. Information Management of the Risks and Threats of the Covid-19 Pandemic. Scientific and Technical Information Processing 47: 200–6. [Google Scholar] [CrossRef]
- Atlani-Duault, Laëtitia, Jeremy K. Ward, Melissa Roy, Céline Morin, and Andrew Wilson. 2020. Tracking online heroisation and blame in epidemics. Lancet Public Health 5: 137–38. [Google Scholar] [CrossRef]
- Austin, J. Matthew, and Allen Kachalia. 2020. The State of Health Care Quality Measurement in the Era of COVID-19 The Importance of Doing Better. JAMA 324: 333–34. [Google Scholar] [CrossRef] [PubMed]
- Beam, Elizabeth L., Shawn G. Gibbs, Kathleen C. Boulter, Marcia E. Beckerdite, and Philip W. Smith. 2011. A method for evaluating health care workers’ personal protective equipment technique. American Journal of Infection Control 39: 415–20. [Google Scholar] [CrossRef]
- Belasen, Alan T., Ariel R. Belasen, Jane Oppenlander, and Attila Hertelendy. 2020. Factors Affecting Patients’ Perceptions of Quality, Hospital Ratings, and Some Thoughts about Post-COVID-19 Challenges. Available online: https://ssrn.com/abstract=3629972 (accessed on 29 March 2021).
- Boškoski, Ivo, Camilla Gallo, Michael B. Wallace, and Guido Costamagna. 2020. COVID-19 pandemic and personal protective equipment shortage: Protective efficacy comparing masks and scientific methods for respirator reuse. Gastrointestinal Endoscopy. [Google Scholar] [CrossRef]
- Branovački, Bojan, Selka Sadiković, Snežana Smederevac, Dušanka Mitrović, and Dejan Pajić. 2021. A person-centered approach in studying coronavirus pandemic response: The role of HEXACO-PI-R and PANAS dimensions. Personality and Individual Differences. [Google Scholar] [CrossRef]
- Brlek, A., S. Vidovič, S. Vuzem, K. Turk, and Zoran Simonović. 2020. Possible indirect transmission of COVID-19 at a squash court, Slovenia, March 2020: Case report. Epidemiol Infection 148: e120. [Google Scholar] [CrossRef] [PubMed]
- CDC. 2020. Science Brief: SARS-CoV-2 and Potential Airborne Transmission, CDC. Available online: https://www.cdc.gov/coronavirus/2019-ncov/more/scientific-brief-sars-cov-2.html (accessed on 23 March 2021).
- Deloitte. 2021. Implications of the COVID-19 Crisis for the Health Care Ecosystem. Available online: https://www2.deloitte.com/content/dam/Deloitte/us/Documents/life-sciences-health-care/implications-of-the-covid19-crisis.pdf (accessed on 19 March 2021).
- Diptanu, Paul, Ayush Gupta, and Anand Kumar Maurya. 2020. Exploring options for reprocessing of N95 Filtering Facepiece Respirators (N95-FFRs) amidst COVID-19 pandemic: A systematic review. PLoS ONE 15: e0242474. [Google Scholar] [CrossRef]
- Dixon, Jennifer. 2021. Improving the quality of care in health systems: Towards better strategies. Israel Journal of Health Policy Research 10: 15. [Google Scholar] [CrossRef] [PubMed]
- European Union. 2020a. The Impact of COVID-19 on Community Health Services, NHS Confederation, London. Available online: https://nhsproviders.org/media/689993/impact-of-covid-19-on-chs_5.pdf (accessed on 19 March 2021).
- European Union. 2020b. The Organization of Resilient Health and Social Care following the CIVID-19 Pandemic, European Comission. Available online: https://ec.europa.eu/health/sites/health/files/expert_panel/docs/026_health_socialcare_covid19_en.pdf (accessed on 19 March 2021).
- Ferreira, Gill, and Susana Borges. 2020. Media and Misinformation in Times of COVID-19: How People Informed Themselves in the Days Following the Portuguese Declaration of the State of Emergency. Journalism and Media 1: 8. [Google Scholar] [CrossRef]
- Fitzsimons, John. 2021. Quality and safety in the time of Coronavirus: Design better, learn faster. International Journal for Quality in Health Care 33: mzaa051. [Google Scholar] [CrossRef]
- Gajdzik, Bożena, and Radosław Wolniak. 2021. Influence of the COVID-19 crisis on steel production in Poland compared to the financial crisis of 2009 and to boom periods in the market. Resources 10: 4. [Google Scholar] [CrossRef]
- Gallagher, Jennifer E., Ilona Johnson, Jos H. Verbeek, Janet E. Clarkson, and Nicola Innes. 2020. Relevance and paucity of evidence: A dental perspective on personal protective equipment during COVID-19 pandemic. British Dental Journal 229: 121–24. [Google Scholar] [CrossRef] [PubMed]
- Hegde, Shalika. 2020. Which type of personal protective equipment (PPE) and which method of donning or doffing PPE carries the least risk of infection for healthcare workers? Evidence-Based Dentistry 21: 74–76. [Google Scholar] [CrossRef]
- Hon, Chun-Yip Hon, B. Bruce Gamage, Elizabeth Ann Bryce, Justin LoChang, Annalee Yassi, Deirdre Maultsaid, and Shicheng Yu. 2008. Personal protective equipment in health care: Can online infection control courses transfer knowledge and improve proper selection and use? American Journal of Infection Control 36: 33–37. [Google Scholar] [CrossRef] [PubMed]
- Howells, Kelly, Martin Burrows, Mat Amp, Rachel Brennan, Wan-Ley Yeun, Shaun Jackson, Joanne Dickinson, Julie Draper, Stephen Campbell, Darren Ashcroft, and et al. 2021. Exploring the experiences of changes to support access to primary health care services and the impact on the quality and safety of care for homeless people during the COVID-19 pandemic: A study protocol for a qualitative mixed methods approach. International Journal for Equity in Health 20: 29. [Google Scholar] [CrossRef] [PubMed]
- Kang, JaHyun, John M. O’Donnell, Bonnie Colaianne, Nicholas Bircher, Dianxu Ren, and Kenneth J. Smith. 2017. Use of personal protective equipment among health care personnel: Results of clinical observations and simulations. American Journal of Infection Control 45: 17–23. [Google Scholar] [CrossRef] [PubMed]
- Kim, Ji SooJ.-S., and Jeong-SilJ.-S. Choi. 2016. Factors Influencing Emergency Nurses’ Burnout during an Outbreak of Middle East Respiratory Syndrome Coronavirus in Korea. Asian Nursing Research, 295–99. [Google Scholar] [CrossRef] [PubMed]
- Meng, L., F. Hua, and Z. Bian. 2020. Coronavirus disease 2019 (COVID-19): Emerging and future challenges for dental and oral medicine. Journal of Dental Research 99: 481–87. [Google Scholar] [CrossRef] [PubMed]
- Mick, Paul, and Russell Murphy. 2020. Aerosol-generating otolaryngology procedures and the need for enhanced PPE during the COVID-19 pandemic: A literature review. Journal of Otolaryngology-Head & Neck Surgery. [Google Scholar] [CrossRef]
- Morawska, Lidia, and Donald K. Milton. 2020. It Is Time to Address Airborne Transmission of Coronavirus Disease 2019 (COVID-19). Clinical Infectious Diseases 71: 2311–13. [Google Scholar] [CrossRef] [PubMed]
- Mulenga, Eddie M., and José M. Marbán. 2020. Prospective Teachers’ Online Learning Mathematics Activities in The Age of COVID-19: A Cluster Analysis Approach, Eurasia journal of Mathematics. Science and Technology Education 16. [Google Scholar] [CrossRef]
- Murtagh, Fionn, and Pierre Legendre. 2011. Ward’s Hierarchical Clustering Method: Clustering Criterion and Agglomerative Algorithm. arXiv arXiv:1111.6285v2. [Google Scholar]
- Narayane, Madhavi Madhukar, Vaishali D. Tendolkar, Ranjit Ambad, and Roshan Kumar Jha. 2020. Covid-19 and PPE. International Journal of Research in Pharmaceutical Sciences 11: 1668–72. [Google Scholar] [CrossRef]
- Omran, Mahamed G. H., Andries P. Engelbrecht, and Ayed Salman. 2007. An Overview of Clustering Methods. Intelligent Data Analysis 11: 583–605. [Google Scholar] [CrossRef]
- Orzeł, Bartosz, A. M. Horodecka, and Anna Maria. 2021. The Adoption of Servqual Method to Analyze the Quality Assurance Factors of Personal Protective Equipment for Health Care Workers, (2021). Silesian University of Technology Scientific Papers: Organization and Management Series; Gliwice: Silesian University of Technology Publishing House, p. 151. [Google Scholar] [CrossRef]
- Pacana, Andrzej, Gazda Andrzej, and Lucia Gazda Bednárová. 2014. The impact of quality information on innovatory environment of the public administration. International Journal of Interdisciplinarity in Theory and Practice, ITPB 4: 25–26. [Google Scholar]
- Pacana, Andrzej, and Robert Ulewicz. 2020. Analysis of causes and effects of implementation of the quality management system complaint with ISO 9001. Polish Journal of Management Studies 21: 283–96. [Google Scholar] [CrossRef]
- Phan, Lan T., Thuong V. Nguyen, Quang C. Luong, Thinh V. Nguyen, Hieu T. Nguyen, Hung Q. Le, Thuc T. Nguyen, Thang M. Cao, and Quang D. Pham. 2020. Importation and Human-to-Human Transmission of a Novel Coronavirus in Vietnam. New England Journal of Medicine 382: 872–74. [Google Scholar] [CrossRef]
- Qiu, Yun, Xi Chen, and Wei Shi. 2020. Impacts of social and economic factors on the transmission of coronavirus disease 2019 (COVID-19) in China. Journal of Population Economics 33: 1127–72. [Google Scholar] [CrossRef]
- Roder-DeWan, Roder S. 2020. Health system quality in the time of COVID-19. The Lancet Global Health. [Google Scholar] [CrossRef]
- Rowan, Neil J., and John G. Laffey. 2020. Challenges and solutions for addressing critical shortage of supply chain for personal and protective equipment (PPE) arising from Coronavirus disease (COVID19) pandemic—Case study from the Republic of Ireland. Science of The Total Environment 138: 532. [Google Scholar] [CrossRef]
- Rowan, Neil J., and John G. Rowan Laffey. 2021. Unlocking the surge in demand for personal and protective equipment (PPE) and improvised face coverings arising from coronavirus disease (COVID-19) pandemic—Implications for efficacy, re-use and sustainable waste management. Science of the Total Environment 752: 142259. [Google Scholar] [CrossRef]
- Shen, Ye, Changwei Li, Hongjun Dong, Zheng Wang, Leonardo Martinez, Zhou Sun, Andreas Hande, Zhiping Chen, Enfu Chen, Mark H. Ebell, and et al. 2020. Community Outbreak Investigation of SARS-CoV-2 Transmission Among Bus Riders in Eastern China. JAMA Internal Medicine. [Google Scholar] [CrossRef] [PubMed]
- Shirazi, Hossein, Reza Kia Reza, and Peiman Ghasemi. 2020. Ranking of hospitals in the case of COVID-19 outbreak: A new integrated approach using patient satisfaction criteria. International Journal of Healthcare Management 13: 312–24. [Google Scholar] [CrossRef]
- Shreffler, Jacob, Jacob Jessica Petrey, and Martin Huecker. 2020. The Impact of COVID-19 on Healthcare Worker Wellness: A Scoping Review. Western Journal of Emergency Medicine 21: 1059–66. [Google Scholar] [CrossRef] [PubMed]
- Tang, Song, Yixin Zhao, Rachael M. Jones, Qiyue Tan, John S. Ji, Na Li, Jin Shen, Yuebin Lv, Lijun Pan, Pei Ding, and et al. 2020. Aerosol transmission of SARS-CoV-2? Evidence, prevention and control. Environment International 144: 106039. [Google Scholar] [CrossRef] [PubMed]
- Teng, Ziwei, Jing Huang, Yan Qiu, Yuxi Tan, Qiuping Zhong, Hui Tang, Haishan Wu, Ying Wu, and Jindong Chen. 2020. Mental health of front-line staff in prevention of coronavirus disease 2019. Journal of Central South University (Medical Sciences) 2020: 613–19. [Google Scholar]
- Thrun, Michael Christoph. 2018. Approaches to Cluster Analysis. Available online: https://link.springer.com/chapter/10.1007%2F978-3-658-20540-9_3 (accessed on 23 January 2021).
- Trzebiński, Jerzy, Maciej Cabański, and Jolanta Zuzanna Czarnecka. 2020. Reaction to the COVID-19 Pandemic: The Influence of Meaning in Life, Life Satisfaction, and Assumptions on World Orderliness and Positivity. Journal of Loss and Trauma 25: 544–57. [Google Scholar] [CrossRef]
- Verbeek, Jos H., Blair Rajamaki, Sharea Ijaz, Riitta Sauni, Elaine Toomey, Bronagh Blackwood, Christina Tikka, Jani H. Ruotsalainen, and F. Selcen Kilinc Balci. 2020. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database of Systematic Reviews. [Google Scholar] [CrossRef]
- Ward, Joe H., Jr. 1963. Hierarchical grouping to optimize an objective function. Journal of the American Statistical Association 58: 236–44. [Google Scholar] [CrossRef]
- Wolniak, Radosław, and Bozena Skotnicka-Zasadzień. 2012. The concept study of Servqual method’s gap. Quality & Quantity 46: 1239–47. [Google Scholar]
- Wolniak, Radosław, and Bożena Skotnicka-Zasadzień. 2018. Developing a model of factors influencing the quality of service for disabled customers in the condition s of sustainable development, illustrated by an example of the Silesian Voivodeship public administration. Sustainability 10: 2171. Available online: https://www.mdpi.com/2071-1050/10/7/2171/htm (accessed on 29 March 2020). [CrossRef]
- Wolniak, Radosław, Bożena Skotnicka-Zasadzaień, and Michał Zasadzień. 2019. Problems of the functioning of e-administration in the Silesian region of Poland from the perspective of a person with disabilities. Transylvanian Review of Administrative Sciences 57E: 137–55. [Google Scholar]
- World Health Organisation. 2014. Infection Prevention and Control of Epidemic and Pandemic-Prone Acute Respiratory Infections in HealthCare; Who Guideline. Geneva: World Health Organization. [Google Scholar]
- World Health Organisation. 2020. Rational Use of Personal Protective Equipment (Ppe) For Coronavirus Disease (Covid-19): Interim Guidance. Geneva: WHO Headquarters (HQ). [Google Scholar]
- Xia, Wei, Liu Fu, Haihan Liao, Chan Yang, Haipeng Guo, and Zhouyan Bian. 2020. The Physical and Psychological Effects of Personal Protective Equipment on Health Care Workers in Wuhan, China: A Cross-Sectional Survey Study. Journal of Emergency Nursing 46: 791–801.e7. [Google Scholar] [CrossRef]
- Zarikas, Zarikas, Stavros G. Poulopoulos, Zoe Gareiou, and Efthimios Zervas. 2020. Clustering analysis of countries using Covid-19 cases dataset. Data in Brief 31: 105787. [Google Scholar] [CrossRef]
- Zhao, Yanjie, Chunlin Xiang, Shaofang Wang, Chengdong Peng, Qian Zou, Jun Wu, and Hu Zhao. 2020. Radiology department strategies to protect radiologic technologists against COVID19: Experience from Wuhan. European Journal of Radiology 127: 108996. [Google Scholar] [CrossRef]
- Zhu, Na, Dingyu Zhang, Wenling Wang, Xingwang Li, Bo Yang, Jingdong Song, Xiang Zhao, Baoying Huang, Weifeng Shi, Roujian Lu, and et al. 2020. A novel coronavirus from patients with pneumonia in China, 2019. New England Journal of Medicine 382: 727–33. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).