Effectiveness of a Computer-Based Training Program of Attention and Memory in Patients with Acquired Brain Damage
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Methods
2.3. Rehabillitation Procedures
2.4. Procedure of the Intervention
3. Results
3.1. Analysis Within Groups
3.2. Analysis between Groups
- (a)
- The age did not show any effect on neuropsychological variables and the rest of the covariates.
- (b)
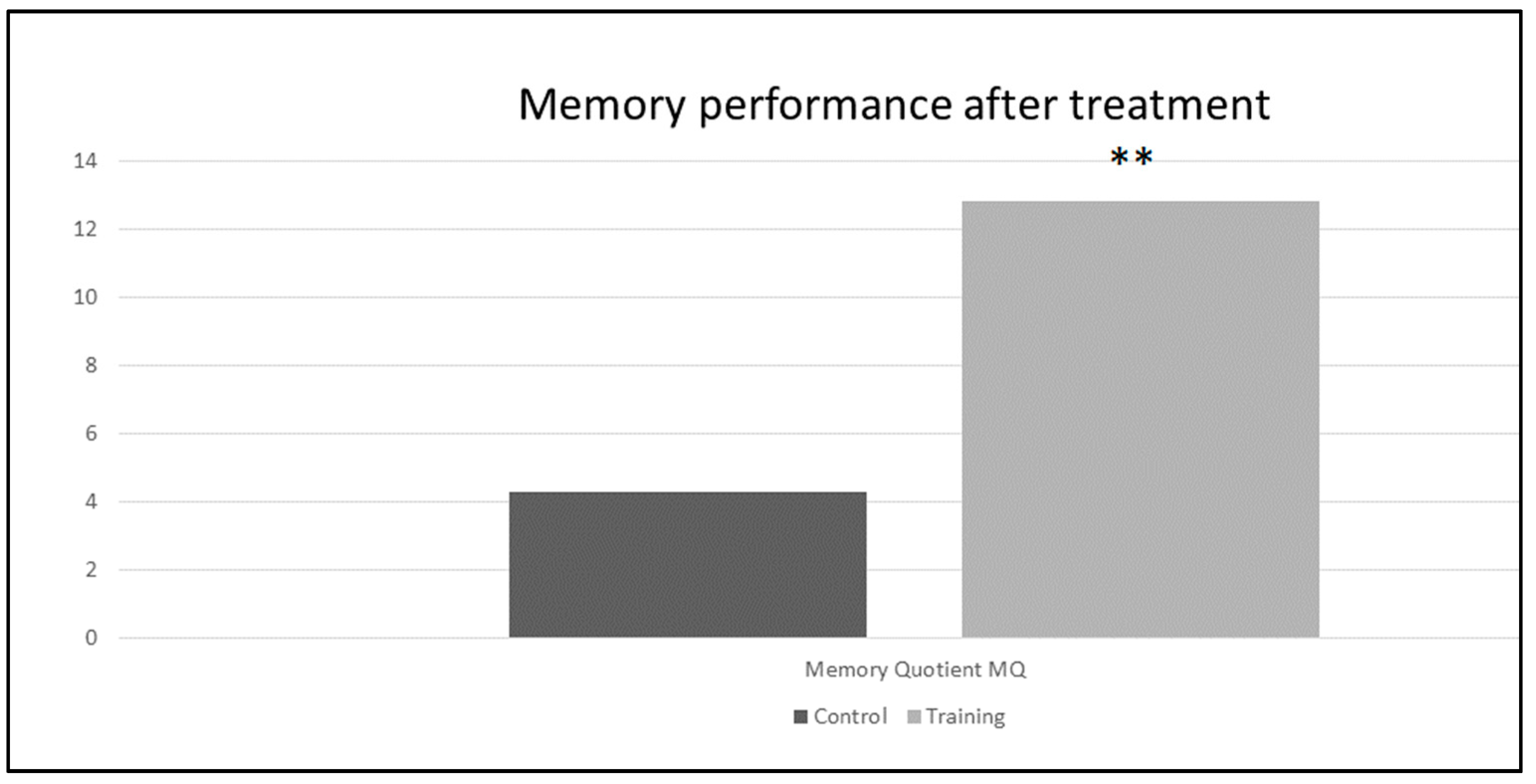
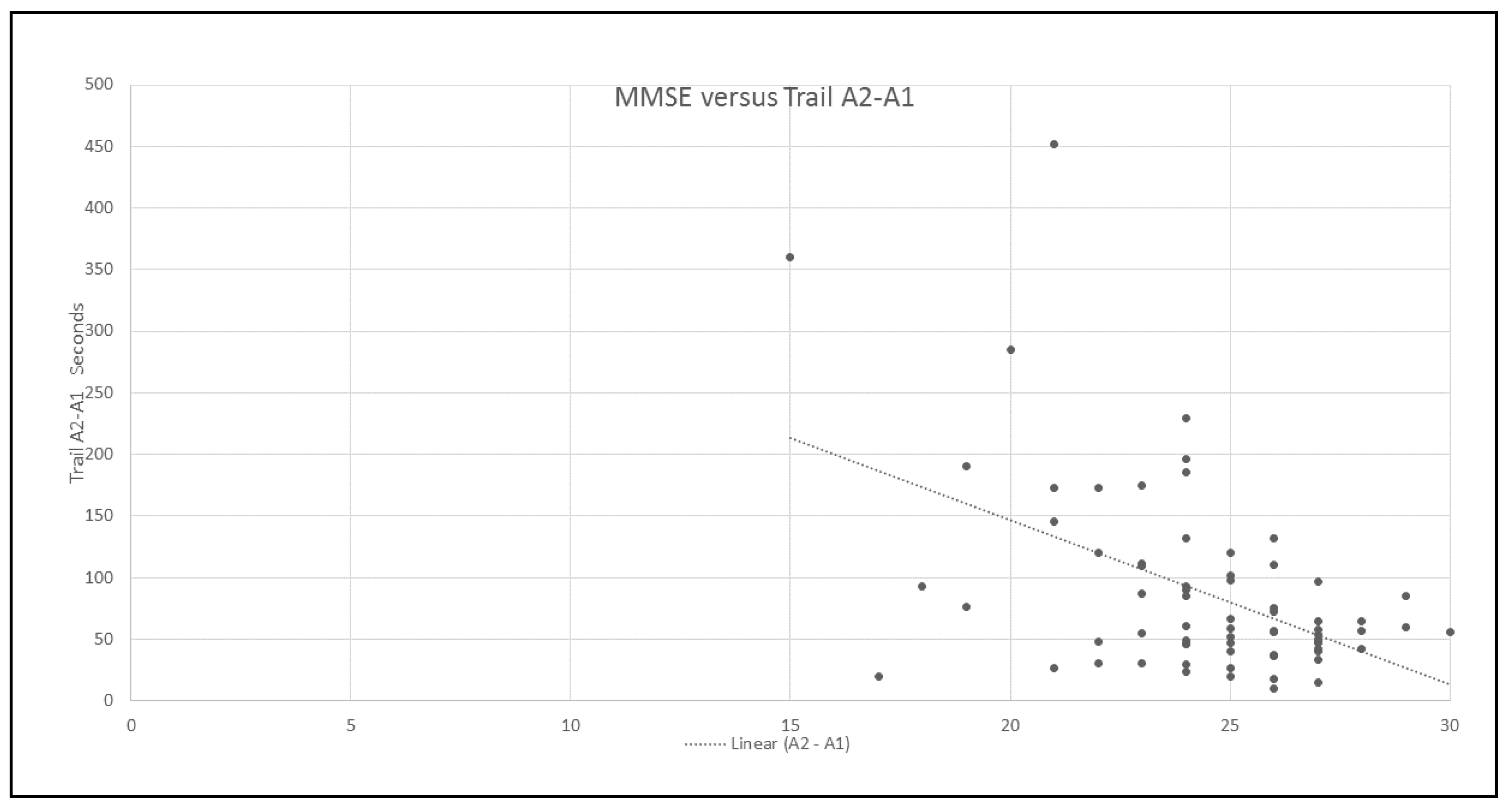
- The main effect of the group was related to four variables: the focused attention of the TMT (Trail A) (p = 7.698 × 10−606), two subtests of the WMS, digit span (p = 0.008) and logic memory (p = 0.01) and the Memory Quotient (p = 1.118 × 10−5).
- (c)
- The main effect of time of evolution was related to subtests orientation (p = 0.025) and associative learning (p = 0.010) of the WMS. Patients with more time of evolution of the ABD had the worst performance in these subtests.
- (d)
- The main effect of the educational level with WMS subtest orientation (p = 0.001).
- (e)
- The only interaction we found between group and the covariates was in the associative learning, where not main effect of group was found, but the interaction with educational level (p = 0.049) and time of evolution (p = 0.024*) was statistical significant.
4. Discussion
4.1. Mechanism Underlying the Cognitive Rehabilitation
4.2. Benefits of Computerized Rehabilitation Techniques
4.3. Global Cognitive Functioning
4.4. Cognitive Recovery and Other Clinical and Demographic Variables
4.5. Limitations of the Study
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Dotor, A.L.; Arango, J.C. Rehabilitacion Cognitiva de Personas con Lesion Cerebral; Dotor, A.L., Arango, J.C., Eds.; Editorial Trillas: Mexico City, Mexico, 2014. [Google Scholar]
- Ardila, A.; Ostrosky, F. Guía Para el Diagnóstico Neuropsicológico; Florida International University: Miami, FL, USA, 2012. [Google Scholar]
- Long, K.; Rager, B.; Adams, G. Deficit awareness and cognitive performance in individuals with acquired brain injury. NeuroRehabilitation 2014, 34, 45–53. [Google Scholar] [PubMed]
- Cuthbert, J.P.; Corrigan, J.D.; Harrison-Felix, C.; Coronado, V.; Dijkers, M.P.; Heinemann, A.W.; Whiteneck, G.G. Factors that predict acute hospitalization discharge disposition for adults with moderate to severe traumatic brain injury. Arch. Phys. Med. Rehabil. 2011, 92, 721–730. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, P.G.; Ometto, M.; Sendoya, G.; Lacet, C.; Monteiro, L.; Cunha, P. Neuropsychological Rehabilitation of Executive Functions: Challenges and Perspectives. J. Behav. Brain Sci. 2014, 4, 27–32. [Google Scholar] [CrossRef]
- Balmaseda, R.; Barroso, J.M.; Carrión, J.L. Déficits neuropsicológicos y conductuales de los trastornos cerebrovasculares. Rev. Esp. Neuropsicol. 2002, 4, 312–330. [Google Scholar]
- De Bettencourt, M.T.; Jonathan, D.; Cohen, R.F.; Kenneth, A.N.; Turk-Brownem, N.B. Closed-loop training of attention with real-time brain imaging. Nat. Neurosci. 2015, 18, 470–475. [Google Scholar] [CrossRef] [PubMed]
- Pijnenborg, G.H. The Neuropsychology of Mental Illness. Neuropsychol. Rehabil. 2011, 21, 138–140. [Google Scholar] [CrossRef]
- Ardila, A.; Rosselli, M. Neuropsicología Clínica; Editorial El Manual Moderno. S.A. de C.V.: Colombia, 2010. [Google Scholar]
- Winocur, G.; Palmer, H.; Stuss, D.; Alexander, M.; Craik, F.; Levine, B.; Moscovitch, M.; Robertson, I. Cognitive rehabilitation in clinical neuropsychology. Brain Cogn. 2002, 42, 120–123. [Google Scholar] [CrossRef] [PubMed]
- Cicerone, K.D.; Langenbahn, D.; Donna, M. Evidence-based cognitive rehabilitation: Updated review of the literature from 2003 through 2008. Arch. Phys. Med. Rehabil. 2011, 92, 519–530. [Google Scholar] [CrossRef] [PubMed]
- Malia, K. What works in cognitive rehabilitation: Opinion paper. NeuroRehabilitation 2014, 34, 3–13. [Google Scholar] [PubMed]
- Moreno, P.; Blanco, C. Hacia una teoría comprensiva de la rehabilitación de funciones cerebrales como base de los programas de rehabilitación en enfermos con daño cerebral. Rev. Neurol. 2000, 30, 779–783. [Google Scholar]
- Noreña, D.D.; Ríos, M.; Bombín, I.; Sánchez, I.; García, A.; Tirapu, J. Efectividad de la rehabilitación neuropsicológica en el daño cerebral adquirido (I): Atención, velocidad de procesamiento, memoria y lenguaje. Rev. Neurol. 2010, 51, 687–698. [Google Scholar] [PubMed]
- Miniussi, C.; Vallar, G. Brain stimulation and behavioural cognitive rehabilitation: A new tool for neurorehabilitation? Neuropsychol. Rehabil. 2011, 21, 553–559. [Google Scholar] [CrossRef] [PubMed]
- Lebowitz, M.S.; Dams-O’Connor, K.; Cantor, J.B. Feasibility of computerized brain plasticity-based cognitive training after traumatic brain injury. J. Rehabil. Res. Dev. 2012, 49, 1547–1556. [Google Scholar] [CrossRef] [PubMed]
- Ginarte, Y. Rehabilitación Cognitiva. Aspectos teóricos y metodológicos. Rev. Neurol. 2002, 35, 870–876. [Google Scholar]
- Van Schouwen-van Kranen, E.T. Clinical reasoning in cognitive rehabilitation therapy. NeuroRehabilitation 2014, 34, 15–21. [Google Scholar] [PubMed]
- Berlucchi, G. Brain plasticity and cognitive neurorehabilitation. Neuropsychol. Rehabil. 2011, 21, 560–578. [Google Scholar] [CrossRef] [PubMed]
- Parisi, L.; Rocca, M.A.; Valsasina, P.; Panicari, L.; Mattioli, F.; Filippi, M. Cognitive rehabilitation correlates with the functional connectivity of the anterior cingulate cortex in patients with multiple sclerosis. Brain Imaging Behav. 2014, 8, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Ríos-Lago, P.; Paúl-Lapedriza, N.; Muñoz-Céspedes, J.M.; Maestú, F.; Álvarez-Linera, J.; Ortiz, T. Aplicación de la neuroimagen funcional al estudio de la rehabilitación neuropsicológica. Rev. Neurol. 2004, 38, 366–373. [Google Scholar] [PubMed]
- Anguera, J.A.; Gazzaley, A. Video games, cognitive exercises, and the enhancement of cognitive abilities. Behav. Sci. 2015, 4, 160–165. [Google Scholar] [CrossRef]
- Mishra, J.; Anguera, J.; Gazzaley, A. Video Games for Neuro-Cognitive Optimization. Neuron 2016, 90, 214–218. [Google Scholar] [CrossRef] [PubMed]
- Sigmundsdottir, L.; Longley, W.; Tate, R. Computerized cognitive training in acquired brain injury: A systematic review of outcomes using the International Classification of Functioning (ICF). Neuropsychol. Rehabil. 2016, 26, 673–741. [Google Scholar] [CrossRef] [PubMed]
- Restrepo, D. La práctica neuropsicológica asistida por computadora: Un escenario para el diálogo interdisciplinario entre la tecnología y las neurociencias. Rev. CES Psicol. 2009, 2, 79–90. [Google Scholar]
- Zabala, A.; Muñoz, J.M.; Quemada, J.J. Efectividad de la rehabilitación neuropsicológica en pacientes con daño cerebral adquirido: Fundamentos y dificultades metodológicas en la investigación. Rehabilitación 2003, 37, 103–121. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. Mini-Mental State: A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 19, 189–198. [Google Scholar] [CrossRef]
- Tombaugh, T. Trail Making Test A and B: Normative data stratified by age and education. Arch. Clin. Neuropsychol. 2004, 19, 203–214. [Google Scholar] [CrossRef]
- Guinea, A.; Luna, P.; Tirapu, J. Evaluación de la memoria en el daño cerebral adquirido: Comparación entre la escala de memoria de Wechsler y el test conductual de memoria de Rivermead. Rev. Neurol. 2009, 49, 240–244. [Google Scholar]
- Schuhfried, G. RehaCom. Computer-aided cognitive rehabilitation. Available online: https://www.rehacom.com/what-is-rehacom.html (accessed on 30 December 2017).
- Mateer, C. Introduccion a la Rehabilitacion Cognitiva. Av. Psicol. Clín. Latinoam. 2003, 21, 11–20. [Google Scholar]
- Wilms, I.; Mala, H. Indirect versus direct feedback in computer-based Prism Adaptation Therapy. Neuropsychol. Rehabil. 2010, 20, 830–853. [Google Scholar] [CrossRef] [PubMed]
- Nordvik, J.E.; Walle, K.M.; Nyberg, C.K.; Fjell, A.M.; Walhovd, K.B.; Westlye, L.T.; Tornas, S. Bridging the gap between clinical neuroscience and cognitive rehabilitation: The role of cognitive training, models of neuroplasticity and advanced neuroimaging in future brain injury rehabilitation. NeuroRehabilitation 2014, 34, 81–85. [Google Scholar] [PubMed]
- Soto-Pérez, F.; Franco Martín, M.; Jiménez Gómez, F. Tecnologias y Neuropsicologia: Hacia una Ciber-Neuropsicologia. Cuad. Neuropsicol. 2010, 4, 112–130. [Google Scholar]
- Mattioli, F.; Stampatiori, C.; Zanotti, D.; Parrinello, G.; Capra, R. Efficacy and specificity of intensive cognitive rehabilitation of attention and executive functions in multiple sclerosis. J. Neurol. Sci. 2010, 288, 101–105. [Google Scholar] [PubMed]
- Velilla, L.M.; Soto, E.; Pineda, D. Efectos de un programa de estimulación cognitiva en la memoria operativa de pacientes con deterioro cognitivo leve amnésico. Rev. Chil. Neuropsicol. 2010, 5, 186–198. [Google Scholar]
- Wentink, M.M.; Berger, M.A.; de Kloet, A.J.; Meesters, J.; Band, G.P.; Wolterbeek, R.; Goossens, P.H.; Vliet Vlieland, T.P. The effects of an 8-week computerbased brain training programme on cognitive functioning, QoL and self-efficacy after stroke. Neuropsychol. Rehabil. 2016. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.D.; Lee, J.C.; Kim, K.Y. The effects of computarized cognitive rehabilitation with noise on memory and attention in elderly. Adv. Sci. Technol. Lett. 2013, 40, 33–39. [Google Scholar]
- Calleo, J.; Burrows, C.; Levin, H.; Marsh, L.; Lai, E.; York, M.K. Cognitive rehabilitation for executive dysfunction in Parkinson’s disease: Application and current directions. Parkinson’s Dis. 2011, 2012. [Google Scholar] [CrossRef]

| Training Group N = 50 | Control Group N = 30 | ||||
|---|---|---|---|---|---|
| Gender | No. | % | No. | % | |
| Male | 36 | 72 | 18 | 60 | |
| Female | 14 | 28 | 12 | 40 | |
| Total | 50 | 100 | 30 | 100 | |
| Etiology | TBI | 31 | 62 | 16 | 53 |
| stroke | 19 | 38 | 14 | 47 | |
| Total | 50 | 100 | 30 | 100 | |
| Media | SEM | Media | SEM | ||
| Evolution time | 5.6 | 0.96 | 5 | 0.87 | |
| Educational level | 13 | 0.47 | 13 | 0.60 | |
| Age | 33.7 | 1,77 | 34.2 | 2.27 | |
| Initial neuropsychological evaluation | Global (MMSE) | 23.4 | 0.46 | 25.1 | 0.30 |
| Focused attention (seconds) | 112 | 10.9 | 147.8 | 8.5 | |
| Executive attention (seconds) | 112 | 15.8 | 91 | 11.9 | |
| Memory MQ | 75.9 | 2.24 | 78,3 | 2.7 | |
| Variable | Control Group N = 30 | Training Group N = 50 | ||||||
|---|---|---|---|---|---|---|---|---|
| Initial | Final | Initial | Final | |||||
| Mean | SE | Mean | SE | Mean | SE | Mean | SE | |
| Focused attention Trail A | 147 | 8.5 | 138 * | 8.13 | 112.4 | 10.9 | 88.5 * | 9.35 |
| Executive attention Trail B | 91 | 11.9 | 80 * | 10.17 | 112.64 | 15.80 | 93.1 * | 13.82 |
| Orientation | 4.2 | 0.24 | 4.5 * | 0.17 | 3.98 | 0.21 | 4.60 * | 0.11 |
| Information | 4.1 | 0.25 | 4.8 * | 0.18 | 4.50 | 0.19 | 5.14 | 0.14 |
| Mental control | 5.9 | 0.51 | 6.4 * | 0.40 | 5.70 | 0.34 | 7.02 * | 0.29 |
| Digit span | 7.2 | 0.33 | 7.4 * | 0.30 | 7.12 | 0.27 | 8.36 * | 0.27 |
| Associative learning | 9.8 | 0.69 | 10.4 * | 0.68 | 9.54 | 0.57 | 11.2 * | 0.62 |
| Logical memory | 6.2 | 0.62 | 7.4 * | 0.59 | 5.66 | 0.50 | 8.40 * | 0.55 |
| Visual memory | 6.4 | 0.59 | 7.4 * | 0.58 | 6.28 | 0.40 | 8.00 * | 0.44 |
| Memory Quotient: MQ | 78.3 | 2.74 | 82.6 * | 2.87 | 75.9 | 2.24 | 88.7 * | 2.72 |
| Variables | Group | Time of Evolution | Educational Level | Interactions | |||
|---|---|---|---|---|---|---|---|
| F | p | F | p | p | |||
| Focused attention Trail A | 23.4 | 7.698–606 *** | |||||
| Orientation | 5.24 | 0.025 * | 10.5 | 0.001 ** | |||
| Information | |||||||
| Mental control | |||||||
| Digit span | 7.31 | 0.008 ** | |||||
| Associative learning | 6.87 | 0.010 * | Group*Educational level F = 4.0, p = 0.049 * Group*Time of evolution F = 5.24, p = 0.024 * | ||||
| Logical memory | 6.97 | 0.01 * | |||||
| Visual memory | |||||||
| Memory Quotient: MQ | 22.35 | 1.118 × 10−5 *** | |||||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernandez, E.; Bergado Rosado, J.A.; Rodriguez Perez, D.; Salazar Santana, S.; Torres Aguilar, M.; Bringas, M.L. Effectiveness of a Computer-Based Training Program of Attention and Memory in Patients with Acquired Brain Damage. Behav. Sci. 2018, 8, 4. https://doi.org/10.3390/bs8010004
Fernandez E, Bergado Rosado JA, Rodriguez Perez D, Salazar Santana S, Torres Aguilar M, Bringas ML. Effectiveness of a Computer-Based Training Program of Attention and Memory in Patients with Acquired Brain Damage. Behavioral Sciences. 2018; 8(1):4. https://doi.org/10.3390/bs8010004
Chicago/Turabian StyleFernandez, Elizabeth, Jorge A. Bergado Rosado, Daymi Rodriguez Perez, Sonia Salazar Santana, Maydane Torres Aguilar, and Maria Luisa Bringas. 2018. "Effectiveness of a Computer-Based Training Program of Attention and Memory in Patients with Acquired Brain Damage" Behavioral Sciences 8, no. 1: 4. https://doi.org/10.3390/bs8010004
APA StyleFernandez, E., Bergado Rosado, J. A., Rodriguez Perez, D., Salazar Santana, S., Torres Aguilar, M., & Bringas, M. L. (2018). Effectiveness of a Computer-Based Training Program of Attention and Memory in Patients with Acquired Brain Damage. Behavioral Sciences, 8(1), 4. https://doi.org/10.3390/bs8010004




