Psychological Predictors of Sexual Intimate Partner Violence against Black and Hispanic Women
Abstract
1. Background
2. Methods
2.1. Design and Settings
2.2. Ethics
2.3. Participants and Sampling
2.4. Analytical Sample
2.5. Process
3. Measures
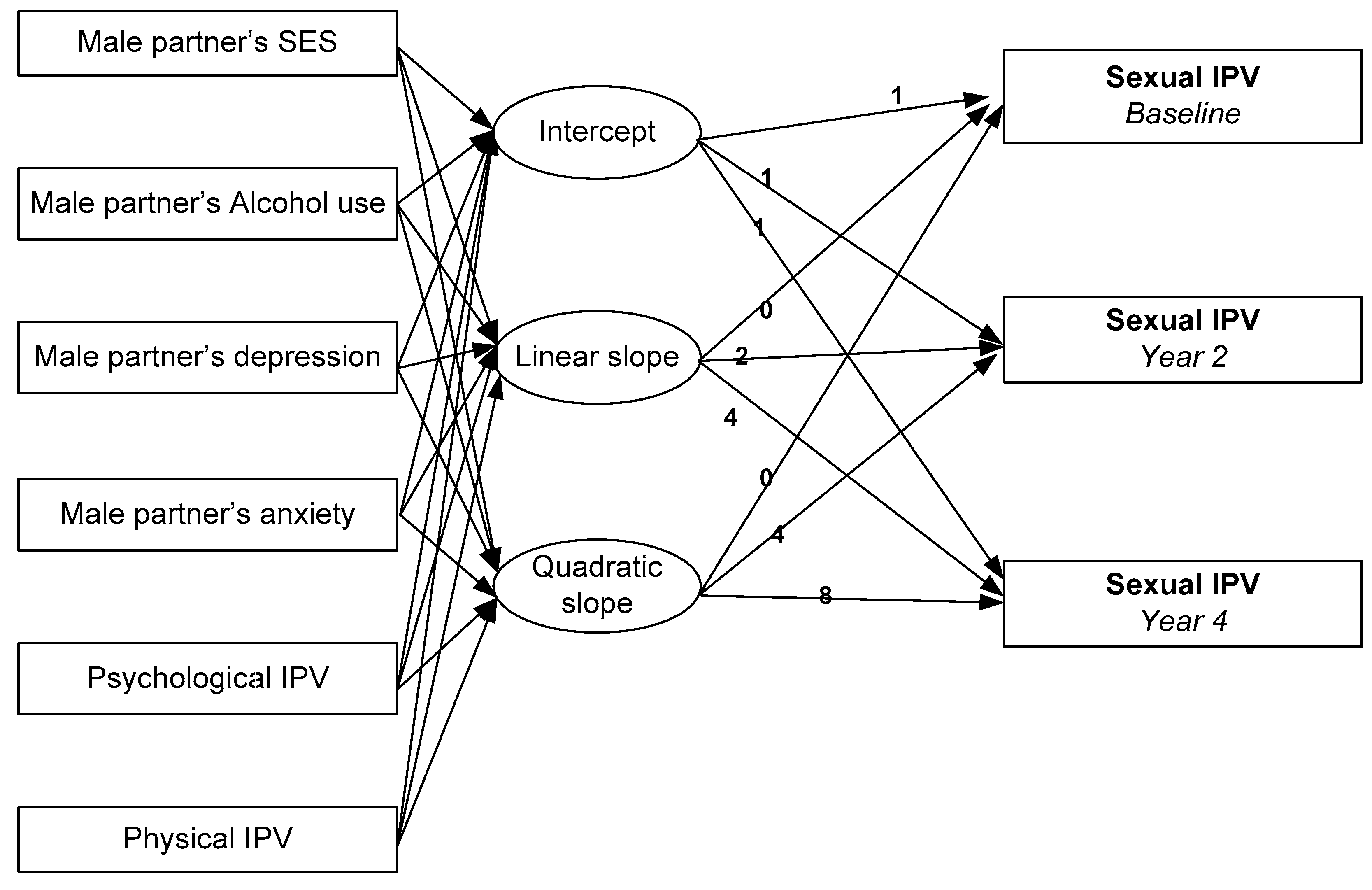
4. Analysis Plan
5. Results
5.1. Sexual IPV against Black Women
5.2. Sexual IPV against Hispanic Women
6. Discussion
6.1. Implications
6.2. Limitations
6.3. Future Research
6.4. Conclusions
Acknowledgment
Author Contributions
Conflicts of Interest
Funding
References
- Archer, J. Sex differences in aggression between heterosexual partners. A meta-analytic review. Psychol. Bull. 2000, 126, 651–680. [Google Scholar] [CrossRef] [PubMed]
- Krug, E.G.; Dalhberg, L.L.; Mercy, J.A.; Zwi, A.B.; Lozano, R. Sexual violence. In World Report on Violence and Health; World Health Organization: Geneva, Switzerland, 2002; pp. 149–181. [Google Scholar]
- Black, M.C. Intimate partner violence and adverse health consequences: Implications for clinicians. Am. J. Lifestyle Med. 2011, 5, 428–439. [Google Scholar] [CrossRef]
- Black, M.C.; Basile, K.C.; Breiding, M.J.; Smith, S.G.; Walters, M.L.; Merrick, M.T.; Chen, J.; Stevens, M.R. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report; National Center for Injury Prevention and Control, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2011.
- Coker, A.L.; Davis, K.E.; Arias, I.; Desai, S.; Sanderson, M.; Brandt, H.M.; Smith, P.H. Physical and mental health effects of intimate partner violence for men and women. Am. J. Lifestyle Med. 2002, 23, 260–268. [Google Scholar] [CrossRef]
- Warshaw, C.; Brashler, B.; Gil, J. Mental health consequences of intimate partner violence. In Intimate Partner Violence: A Health Based Perspective; Mitchell, C., Anglin, D., Eds.; Oxford University Press: New York, NY, USA, 2009; pp. 147–171. [Google Scholar]
- Honda, T.; Wynter, K.; Yokota, J.; Tran, T.; Ujiie, Y.; Niwa, M.; Nakayama, M.; Ito, F.; Kim, Y.; Fisher, J.; Kamo, T. Sexual Violence as a Key Contributor to Poor Mental Health Among Japanese Women Subjected to Intimate Partner Violence. J. Womens Health (Larchmt) 2017. [Google Scholar] [CrossRef] [PubMed]
- De Visser, R.O.; Smith, A.M.; Rissel, C.E.; Richters, J.; Grulich, A.E. Sex in Australia: Experiences of sexual coercion among a representative sample of adults. Aust. N. Z. J. Public Health 2003, 27, 198–203. [Google Scholar] [CrossRef] [PubMed]
- De Visser, R.O.; Rissel, C.E.; Richters, J.; Smith, A.M. The impact of sexual coercion on psychological, physical, and sexual well-being in a representative sample of Australian women. Arch. Sex. Behav. 2007, 36, 676–686. [Google Scholar] [CrossRef] [PubMed]
- Mohammadkhani, P.; Khooshabi, K.S.; Forouzan, A.S.; Azadmehr, H.; Assari, S.; Lankarani, M.M. Associations between coerced anal sex and psychopathology, marital distress and non-sexual violence. J. Sex. Med. 2009, 6, 1938–1946. [Google Scholar] [CrossRef] [PubMed]
- Campbell, R.; Greeson, M.R.; Bybee, D.; Raja, S. The co-occurrence of childhood sexual abuse, adult sexual assault, intimate partner violence, and sexual harassment: A mediational model of posttraumatic stress disorder and physical health outcomes. J. Consult. Clin. Psychol. 2008, 76, 194–207. [Google Scholar] [CrossRef] [PubMed]
- Tjaden, P.; Thoennes, N. Extent, Nature, and Consequences of Intimate Partner Violence: Findings from the National Violence against Women Survey; Publication No. NCJ 181867; Department of Justice (US): Washington, DC, USA, 2000. Available online: http://www.ojp.usdoj.gov/nij/pubssum/181867.htm (accessed on 8 November 2017).
- Jewkes, R.; Fulu, E.; Tabassam Naved, R.; Chirwa, E.; Dunkle, K.; Haardörfer, R.; Garcia-Moreno, C.; UN Multi-country Study on Men and Violence Study Team. Women’s and men’s reports of past-year prevalence of intimate partner violence and rape and women’s risk factors for intimate partner violence: A multicountry cross-sectional study in Asia and the Pacific. PLoS Med. 2017, 14, e1002381. [Google Scholar] [CrossRef] [PubMed]
- Lipsky, S.; Caetano, R.; Field, C.A.; Larkin, G.L. Psychosocial and substance-use risk factors for intimate partner violence. Drug Alcohol Depend. 2005, 78, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Miga, E.M.; Hare, A.; Allen, J.P.; Manning, N. The relation of insecure attachment states of mind and romantic attachment styles to adolescent aggression in romantic relationships. Attach. Hum. Dev. 2010, 12, 463–481. [Google Scholar] [CrossRef] [PubMed]
- Mohammadkhani, P.; Forouzan, A.S.; Khooshabi, K.S.; Assari, S.; Lankarani, M.M. Are the predictors of sexual violence the same as those of nonsexual violence? A gender analysis. J. Sex. Med. 2009, 6, 2215–2223. [Google Scholar] [CrossRef] [PubMed]
- Basile, K.C.; Hall, J.E. Intimate partner violence perpetration by court-ordered men: Distinctions and intersections among physical violence, sexual violence, psychological abuse, and stalking. J. Interpers. Violence 2011, 26, 230–253. [Google Scholar] [CrossRef] [PubMed]
- Agardh, A.; Tumwine, G.; Asamoah, B.O.; Cantor-Graae, E. The Invisible Suffering: Sexual Coercion, Interpersonal Violence, and Mental Health—A Cross-Sectional Study among University Students in South-Western Uganda. PLoS ONE 2012, 7, e51424. [Google Scholar] [CrossRef] [PubMed]
- Karamagi, C.A.S.; Tumwine, J.K.; Tylleskar, T.; Heggenhougen, K. Intimate partner violence against women in eastern Uganda: Implications for HIV prevention. BMC Public Health 2006, 6, 284. [Google Scholar] [CrossRef] [PubMed]
- Afifi, T.O.; Henriksen, C.A.; Asmundson, G.J.; Sareen, J. Victimization and perpetration of intimate partner violence and substance use disorders in a nationally representative sample. J. Nerv. Ment. Dis. 2012, 200, 684–691. [Google Scholar] [CrossRef] [PubMed]
- Lipsky, S.; Caetano, R.; Field, C.A.; Bazargan, S. The role of alcohol use and depression in intimate partner violence among black and Hispanic patients in an urban emergency department. Am. J. Drug Alcohol Abuse 2005, 31, 225–242. [Google Scholar] [CrossRef] [PubMed]
- Hankin, A.; Smith, L.S.; Daugherty, J.; Houry, D. Correlation between Intimate Partner Violence Victimization and Risk of Substance Abuse and Depression among African-American Women in an Urban Emergency Department. West. J. Emerg. Med. 2010, 11, 252–256. [Google Scholar] [PubMed]
- Loxton, D.; Dolja-Gore, X.; Anderson, A.E.; Townsend, N. Intimate partner violence adversely impacts health over 16 years and across generations: A longitudinal cohort study. PLoS ONE. 2017, 12, e0178138. [Google Scholar] [CrossRef] [PubMed]
- Peltzer, K.; Pengpid, S. Associations between intimate partner violence, depression, and suicidal behavior among women attending antenatal and general outpatients hospital services in Thailand. Niger. J. Clin. Pract. 2017, 20, 892–899. [Google Scholar] [CrossRef] [PubMed]
- Sparrow, K.; Kwan, J.; Howard, L.; Fear, N.; MacManus, D. Systematic review of mental health disorders and intimate partner violence victimisation among military populations. Soc. Psychiatry Psychiatr. Epidemiol. 2017. [Google Scholar] [CrossRef] [PubMed]
- Nduna, M.; Jewkes, R.K.; Dunkle, K.L.; Shai, N.P.; Colman, I. Associations between depressive symptoms, sexual behaviour and relationship characteristics: A prospective cohort study of young women and men in the Eastern Cape, South Africa. J. Int. AIDS Soc. 2010, 13, 44. [Google Scholar] [CrossRef] [PubMed]
- Vaeth, P.A.; Ramisetty-Mikler, S.; Caetano, R. Depression among couples in the United States in the context of intimate partner violence. J. Interpers. Violence 2010, 25, 771–790. [Google Scholar] [CrossRef] [PubMed]
- Graham, K.; Bernards, S.; Flynn, A.; Tremblay, P.F.; Wells, S. Does the relationship between depression and intimate partner aggression vary by gender, victim-perpetrator role, and aggression severity? Violence Vict. 2012, 27, 730–743. [Google Scholar] [CrossRef] [PubMed]
- Gabora, N.; Stewart, L.; Lilley, K.; Allegri, N. A Profile of Female Perpetrators of Intimate Partner Violence: Implications for Treatment. Correct. Serv. Can. 2007, 175, 1–10. [Google Scholar]
- Misca, G.; Forgey, M.A. The Role of PTSD in Bi-directional Intimate Partner Violence in Military and Veteran Populations: A Research Review. Front. Psychol. 2017, 8, 1394. [Google Scholar] [CrossRef] [PubMed]
- Moffitt, T.E.; Krueger, R.F.; Caspi, A.; Fagan, J. Partner abuse and general crime: How are they the same? How are they different? Criminology 2000, 38, 199–232. [Google Scholar] [CrossRef]
- Hines, D.A.; Douglas, E.M. Alcohol and drug abuse in men who sustain intimate partner violence. Aggress. Behav. 2012, 38, 31–46. [Google Scholar] [CrossRef] [PubMed]
- Foran, H.M.; O’Leary, K.D. Alcohol and intimate partner violence: A meta-analytic review. Clin. Psychol. Rev. 2008, 28, 1222–1234. [Google Scholar] [CrossRef] [PubMed]
- Yalch, M.M.; Levendosky, A.A. Main and Moderating Effects of Temperament Traits on the Association between Intimate Partner Violence and Hazardous Alcohol Use in a Sample of Young Adult Women. Psychol. Trauma 2017. [Google Scholar] [CrossRef] [PubMed]
- Coker, A.L.; Smith, P.H.; McKeown, R.E.; King, M.J. Frequency and correlates of intimate partner violence by type: Physical, sexual, and psychological battering. Am. J. Public Health 2000, 90, 553–559. [Google Scholar] [PubMed]
- Makara-Studzinska, M.; Gustaw, K. Intimate partner violence by men abusing and non-abusing alcohol in Poland. Int. J. Environ. Res. Public Health 2007, 4, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Zaleski, M.; Pinsky, I.; Laranjeira, R.; Ramisetty-Mikler, S.; Caetano, R. Intimate partner violence and alcohol consumption. Rev. Saude Publica 2010, 44, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Testa, M.; Kubiak, A.; Quigley, B.M.; Houston, R.J.; Derrick, J.L.; Levitt, A.; Homish, G.G.; Leonard, K.E. Husband and wife alcohol use as independent or interactive predictors of intimate partner violence. J. Stud. Alcohol Drugs 2012, 73, 268–276. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, R.; Rentsch, C.; Salazar, L.F.; Sullivan, P.S. Dyadic Characteristics and Intimate Partner Violence among Men Who Have Sex with Men. West. J. Emerg. Med. 2011, 12, 324–332. [Google Scholar] [PubMed]
- Reichman, N.; Teitler, J.; Garfinkel, I.; McLanahan, S. Fragile Families: Sample and Design. Child. Youth Serv. Rev. 2001, 23, 303–326. [Google Scholar] [CrossRef]
- Robert, W., Jr. How Representative Are the Fragile Families Study Families?: A Comparison of Early Childhood Longitudinal Study-Birth Cohort and Fragile Families Samples; CRCW Working Paper WP10-01-FF; The Trustees of Princeton University: Princeton, NJ, USA, 2010. [Google Scholar]
- Sara, M.; Irwin, G. External link The Fragile Families and Child Wellbeing Study: Questions, Design and a Few Preliminary Results; CRCW Working Paper 2000-07-FF; The Trustees of Princeton University: Princeton, NJ, USA, 2010. [Google Scholar]
- Fragile Families & Child Wellbeing Study. Fragile Families Publication Search. 2017. Available online: Https://ffpubs.princeton.edu/ (accessed on 12 December 2017).
- Fragile Families & Child Wellbeing Study. Data and Documentation. 2017. Available online: https://fragilefamilies.princeton.edu/documentation (accessed on 12 December 2017).
- Reichman, N.; Teitler, J.; Garfinkel, I.; McLanahan, S. Fragile families: Sample and design. Child. Youth Serv. Rev. 2001, 32, 303–326. [Google Scholar] [CrossRef]
- Lloyd, S. The Effects of Violence on Women’s Employment; Northwestern University/University of Chicago Joint Center for Poverty Research: Evanston, IL, USA, 1997. [Google Scholar]
- Weiss, R.L.; Margolin, G. Assessment of marital conflict and accord. In Handbook of Behavioral Assessment; John Wiley: New York, NY, USA, 1977; pp. 555–602. [Google Scholar]
- Nayak, M.B.; Patel, V.; Bond, J.C.; Greenfield, T.K. Partner alcohol use, violence and women’s mental health: Population-based survey in India. Br. J. Psychiatry 2010, 196, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Pillai, A.; Nayak, M.B.; Greenfield, T.K.; Bond, J.C.; Nadkarni, A.; Patel, V. Patterns of alcohol use, their correlates, and impact in male drinkers: A population-based survey from Goa, India. Soc. Psychiatry Psychiatr. Epidemiol. 2013, 48, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Sikweyiya, Y.; Jewkes, R. Force and temptation: Contrasting South African men’s accounts of coercion into sex by men and women. Cult. Health Sex. 2009, 11, 529–541. [Google Scholar] [CrossRef] [PubMed]
- Soeken, K.; Parker, B.; McFarlane, J.; Lominak, M.C. The Abuse-Assessment Screen: A clinical instrument to measure frequency, severity and perpetrator of abuse against women. In Beyond Diagnosis: Changing the Health Care Response to Battered Women and Their Children; Campbell, J.C., Ed.; Sage Publications: Newbury Park, CA, USA, 1998; pp. 195–203. [Google Scholar]
- Maman, S.; Mbwambo, J.K.; Hogan, N.M.; Kilonzo, G.P.; Campbell, J.C.; Weiss, E.; Sweat, M.D. HIV-positive women report more lifetime partner violence: Findings from a voluntary counseling and testing clinic in Dar es Salaam, Tanzania. Am. J. Public Health 2002, 92, 1331–1337. [Google Scholar] [CrossRef] [PubMed]
- Straus, M.A.; Hamby, S.L.; Boney-McCoy, S.; Sugarman, D.B. The Revised Conflict Tactics Scales (CTS2): Development and preliminary psychometric data. J. Fam. Issues 1996, 17, 283–316. [Google Scholar] [CrossRef]
- Duvvury, N.; Nayak, M.B.; Allendorf, K. Links between masculinity and violence: Aggregate analysis. In Domestic Violence in India: Exploring Strategies, Promoting Dialogue. Men, Masculinity and Domestic Violence in India. Summary Report of Four Studies; Young, M., ICRW Staff, Eds.; International Center for Research on Women: Washington, DC, USA, 2002; pp. 52–70. [Google Scholar]
- Patel, V.; Kirkwood, B.R.; Pednekar, S.; Pereira, B.; Barros, P.; Fernandes, J.; Datta, J.; Pai, R.; Weiss, H.; Mabey, D. Gender disadvantage and reproductive health risk factors for common mental disorders in women. Arch. Gen. Psychiatry 2006, 43, 404–413. [Google Scholar] [CrossRef] [PubMed]
- Straus, M.A. Measuring intrafamily conflict and violence: The Conflict Tactics (CS) Scale. J. Marriage Fam. 1979, 41, 75–88. [Google Scholar] [CrossRef]
- Kelly, J.; Johnson, M. Differentiation among types of intimate partner violence: Research update & implications for interventions. Fam. Court Rev. 2008, 46, 476–499. [Google Scholar]
- Kessler, R.C.; Andrews, G.; Mroczek, D.; Ustun, B.; Wittchen, H.U. The world health organization composite international diagnostic interview short-form (CIDI-SF). Int. J. Methods Psychiatr. Res. 1998, 7, 171–185. [Google Scholar] [CrossRef]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA). Recommended Alcohol Questions, 2017. Available online: https://www.niaaa.nih.gov/research/guidelines-and-resources/recommended-alcohol-questions (accessed on 9 November 2017).
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Assari, S. Association between obesity and depression among American Blacks: Role of ethnicity and gender. J. Racial Ethnic Health Disparities 2014, 1, 36–44. [Google Scholar] [CrossRef]
- Assari, S. Additive effects of anxiety and depression on body mass index among blacks: Role of ethnicity and gender. Int. Cardiovasc. Res. J. 2014, 8, 44–51. [Google Scholar] [PubMed]
- Assari, S.; Lankarani, M.M.; Lankarani, R.M. Ethnicity modifies the additive effects of anxiety and drug use disorders on suicidal ideation among Black adults in the United States. Int. J. Prev. Med. 2013, 4, 1251–1257. [Google Scholar] [PubMed]
- Assari, S.; Dejman, M.; Neighbors, H.W. Ethnic differences in separate and additive effects of anxiety and depression on self-rated mental health among Blacks. J. Racial Ethnic Health Disparities 2016, 3, 423–430. [Google Scholar] [CrossRef] [PubMed]
- US Department of Health and Human Services. Chapter 2: Culture Counts: The Influence of Culture and Society on Mental Health. Mental Health: Culture, Race, and Ethnicity—A Supplement to Mental health: A Report of the Surgeon General; US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services: Rockville, MD, USA, 2001.
- Leppink, E.W.; Lust, K.; Grant, J.E. Depression in university students: Associations with impulse control disorders. Int. J. Psychiatry Clin. Pract. 2016, 20, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, S.L.; Molina, B.S.; Belendiuk, K.A.; Donovan, J.E. Racial differences in the development of impulsivity and sensation seeking from childhood into adolescence and their relation to alcohol use. Alcohol Clin. Exp. Res. 2012, 36, 1794–1802. [Google Scholar] [CrossRef] [PubMed]
- Salami, T.K.; Brooks, B.A.; Lamis, D.A. Impulsivity and reasons for living among African American youth: A risk-protection framework of suicidal ideation. Int. J. Environ. Res. Public Health 2015, 12, 5196–5214. [Google Scholar] [CrossRef] [PubMed]
- Meier, M.H.; Slutske, W.S.; Arndt, S.; Cadoret, R.J. Impulsive and callous traits are more strongly associated with delinquent behavior in higher risk neighborhoods among boys and girls. J. Abnorm Psychol. 2008, 117, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Auger, N.; Lo, E.; Cantinotti, M.; O’Loughlin, J. Impulsivity and socio-economic status interact to increase the risk of gambling onset among youth. Addiction 2010, 105, 2176–2183. [Google Scholar] [CrossRef] [PubMed]
- Winkler, D.; Pjrek, E.; Kasper, S. Anger attacks in depression—Evidence for a male depressive syndrome. Psychother. Psychosom. 2005, 74, 303–307. [Google Scholar] [CrossRef] [PubMed]
- Abram, K.M.; Teplin, L.A.; McClelland, G.M.; Dulcan, M.K. Comorbid psychiatric disorders in youth in juvenile detention. Arch. Gen. Psychiatry 2003, 60, 1097–1108. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Gonzalez, H.M.; Neighbors, H.; Nesse, R.; Abelson, J.M.; Sweetman, J.; Jackson, J.S. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: Results from the National Survey of American Life. Arch. Gen. Psychiatry 2007, 64, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Fava, M. Depression with anger attacks. J. Clin. Psychiatry 1998, 59 (Suppl. S18), 18–22. [Google Scholar] [CrossRef]
- Akiskal, H.S.; Benazzi, F.; Perugi, G.; Rihmer, Z. Agitated “unipolar” depression re-conceptualized as a depressive mixed state: Implications for the antidepressant-suicide controversy. J. Affect. Disord. 2005, 85, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Benazzi, F.; Akiskal, H. Irritable-hostile depression: Further validation as a bipolar depressive mixed state. J. Affect. Disord. 2005, 84, 197–207. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Geneva (WHO). World Report on Violence and Health: Summary; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- De Jong, J.T.; Komproe, I.H.; Van Ommeren, M. Lifetime Events and Posttraumatic Stress Disorder in 4 Postconflict Settings. JAMA J. Am. Med. Assoc. 2001, 286, 555–563. [Google Scholar] [CrossRef]
- Prospero, M.; Fawson, P. Sexual coercion and mental health symptoms among heterosexual men: The pressure to say “yes”. Am. J. Men’s Health 2010, 4, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Zhan, W.; Shaboltas, A.V.; Skochilov, R.V.; Kozlov, A.P.; Krasnoselskikh, T.V.; Abdala, N. Alcohol misuse, drinking contexts and intimate partner violence in St. Petersburg, Russia: Results from a cross-sectional study. BMC Public Health 2011, 11, 629. [Google Scholar] [CrossRef] [PubMed]
- Schafer, J.; Caetano, R.; Cunradi, C.B. A path model of risk factors for intimate partner violence among couples in the United States. J. Interpers. Violence 2004, 19, 127–142. [Google Scholar] [CrossRef] [PubMed]
- Caetano, R.; Schafer, J.; Cunradi, C.B. Alcohol-related intimate partner violence among white, black, and Hispanic couples in the United States. Alcohol. Res. Health 2001, 25, 58–65. [Google Scholar] [PubMed]
- Smith, P.H.; Homish, G.G.; Leonard, K.E.; Cornelius, J.R. Intimate partner violence and specific substance use disorders: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol. Addict. Behav. 2012, 26, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Tumwesigye, N.M.; Kyomuhendo, G.B.; Greenfield, T.K.; Wanyenze, R.K. Problem drinking and physical intimate partner violence against women: Evidence from a national survey in Uganda. BMC Public Health 2012, 12, 399. [Google Scholar] [CrossRef] [PubMed]
- Caetano, R.; McGrath, C.; Ramisetty-Mikler, S.; Field, C.A. Drinking, alcohol problems and the five-year recurrence and incidence of male to female and female to male partner violence. Alcohol. Clin. Exp. Res. 2005, 29, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Houry, D.; Kemball, R.S.; Click, L.A.; Kaslow, N. Development of a Brief Mental Health Screen for Intimate Partner Violence Victims in the Emergency Department. Acad. Emerg. Med. 2007, 14, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Taft, A.; O’Doherty, L.; Hegarty, K.; Ramsay, J.; Davidson, L.; Feder, G. Screening women for intimate partner violence in healthcare settings. Cochrane Database Syst Rev. 2013, 30, CD007007. [Google Scholar] [CrossRef]
- Hayer, M.K. Perceptions of sexual coercion among young women in Uganda. J. Health Organ. Manag. 2010, 24, 498–504. [Google Scholar] [CrossRef] [PubMed]
- Moore, A.M.; Awusabo-Asare, K.; Madise, N.; John-Langba, J.; Kumi-Kyereme, A. Coerced first sex among adolescent girls in sub-Saharan Africa: Prevalence and context. Afr. J. Reprod. Health 2007, 11, 62–82. [Google Scholar] [CrossRef] [PubMed]
- Wagman, J.; Baumgartner, J.N.; Waszak Geary, C.; Nakyanjo, N.; Ddaaki, W.G.; Serwadda, D.; Gray, R.; Nalugoda, F.K.; Wawer, M.J. Experiences of sexual coercion among adolescent women: Qualitative findings from Rakai district, Uganda. J. Interpers. Violence 2009, 24, 2073–2095. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.T.; Chou, S.; Browne, K. A critique of the revised conflict tactics scales-2 (CTS-2). Aggress. Violent Behav. 2017, 37, 83–90. [Google Scholar] [CrossRef]
- Dobash, R.P. Dobash, R.E. Women’s violence to men in intimate relationships working on a puzzle. Br. J. Criminol. 2004, 44, 324–349. [Google Scholar] [CrossRef]
- Hamby, S. A scientific answer to a scientific question: The gender debate on intimate partner violence. Trauma Violence Abuse 2015. [Google Scholar] [CrossRef] [PubMed]
- Giles-Sim, J. Wife Battering: A Systems Theory Approach; Guildford Press: New York, NY, USA, 1983. [Google Scholar]
| Characteristics- | Blacks (n = 561) | Hispanics (n = 475) | ||
|---|---|---|---|---|
| n | % | n | % | |
| Race and Ethnicity | ||||
| Hispanic | 27 | 4.81 | 415 | 87.37 |
| Black | 504 | 89.84 | 14 | 2.95 |
| Education | ||||
| Less than high school | 127 | 22.64 | 246 | 51.79 |
| Completed high school or equivalent | 224 | 39.93 | 115 | 24.21 |
| Some college | 160 | 28.52 | 85 | 17.89 |
| College or graduate level | 48 | 8.56 | 24 | 5.05 |
| Relationship Status at Baseline | ||||
| Married | 223 | 39.75 | 228 | 48.00 |
| Romantic Cohabiting | 249 | 44.39 | 223 | 46.95 |
| Romantic Some Visit | 41 | 7.31 | 13 | 2.74 |
| Romantic No Visit | 47 | 8.38 | 11 | 2.32 |
| Relationship Status at Year 2 | ||||
| Married | 263 | 46.88 | 278 | 58.53 |
| Romantic Cohabiting | 228 | 40.64 | 185 | 38.95 |
| Romantic Some Visit | 33 | 5.88 | 6 | 1.26 |
| Romantic No Visit | 37 | 6.60 | 6 | 1.26 |
| Relationship Status at Year 4 | ||||
| Married | 310 | 55.26 | 309 | 65.05 |
| Romantic Cohabiting | 193 | 34.4 | 151 | 31.79 |
| Romantic Some Visit | 23 | 4.10 | 5 | 1.05 |
| Romantic No Visit | 35 | 6.24 | 10 | 2.11 |
| Anxiety | ||||
| No | 499 | 88.95 | 442 | 93.05 |
| Yes | 3 | 0.53 | 3 | 0.63 |
| Depression | ||||
| No | 481 | 85.74 | 426 | 89.68 |
| Yes | 21 | 3.74 | 19 | 4.00 |
| Problem Alcohol Use * | ||||
| 0 day | 185 | 67.27 | 117 | 45.00 |
| 1 day | 27 | 9.82 | 54 | 20.76 |
| 2 day | 23 | 8.36 | 39 | 15.00 |
| 4 day | 18 | 6.55 | 29 | 11.15 |
| 8 day | 14 | 5.09 | 13 | 5.00 |
| 10 or more days | 8 | 2.91 | 7 | 2.69 |
| Blacks (n = 561) | Hispanics (n = 475) | |||
|---|---|---|---|---|
| n | % | n | % | |
| Physical IPV Score at Baseline | ||||
| 0 | 553 | 98.57 | 455 | 95.79 |
| 1 | 4 | 0.71 | 12 | 2.53 |
| 2 | 3 | 0.53 | 6 | 1.26 |
| 3 | 1 | 0.18 | 0 | 0.00 |
| Sexual IPV | ||||
| Baseline | ||||
| Often | 2 | 0.36 | 0 | .000 |
| Sometimes | 13 | 2.32 | 7 | 1.47 |
| Never | 546 | 97.33 | 468 | 98.53 |
| 2 Years Later | ||||
| Often | 5 | 0.89 | 1 | 0.21 |
| Sometimes | 8 | 1.43 | 4 | 0.84 |
| Never | 548 | 97.68 | 470 | 98.95 |
| 4 Years Later | ||||
| Often | 1 | 0.18 | 3 | 0.63 |
| Sometimes | 12 | 2.14 | 11 | 2.32 |
| Never | 548 | 97.68 | 461 | 97.05 |
| Blacks (n = 561) | Hispanics (n = 475) | |||||
|---|---|---|---|---|---|---|
| Range | Min-Max | Mean (SD) | Range | Min-Max | Mean (SD) | |
| Female parent age | 27 | 15–42 | 25.98 (5.90) | 28 | 15–43 | 25.38 (5.56) |
| Male parent age | 37 | 16–53 | 28.75 (7.47) | 37 | 16–53 | 27.63 (6.39) |
| Household income | 133,750 | 0–13,3750 | 32,673.38 (28,541.69) | 131,508 | 0–131,508 | 30,015.92 (26,757.84) |
| Problem alcohol use | 31 | 0–31 | 1.38 (3.84) | 30 | 0–30 | 1.73 (3.43) |
| Physical IPV at baseline | 3 | 0–3 | 0.02 (0.21) | 2.00 | 0–2 | 0.05 (0.27) |
| Psychological IPV at baseline | 8 | 0–8 | 0.70 (1.17) | 7.00 | 0–7 | 0.82 (1.21) |
| Sexual IPV baseline | 2 | 1–3 | 2.97 (0.19) | 1 | 2–3 | 2.99 (0.12) |
| Sexual IPV at 2 years | 2 | 1–3 | 2.97 (0.22) | 2 | 1–3 | 2.99 (0.12) |
| Sexual IPV at 4 years | 2 | 1–3 | 2.98 (0.16) | 2 | 1–3 | 2.96 (0.21) |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Female partner age | 1 | 0.727 ** | 0.326 ** | 0.369 ** | 0.329 ** | −0.299 ** | −0.023 | 0.050 | −0.044 | −0.086 | −0.003 | 0.011 | 0.020 | −0.050 | −0.046 | −0.075 |
| Male partner age | 0.727 ** | 1 | 0.218 ** | 0.214 ** | 0.251 ** | −0.274 ** | −0.030 | −0.008 | −0.051 | −0.067 | −0.052 | −0.029 | 0.051 | −0.024 | −0.034 | −0.039 |
| Household income | 0.102 * | 0.131 ** | 1 | 0.515 ** | 0.402 ** | −0.326 ** | −0.037 | 0.066 | −0.018 | −0.030 | −0.125 * | −0.045 | −0.142 ** | −0.023 | 0.059 | 0.029 |
| Female partner education | 0.192 ** | 0.116 * | 0.286 ** | 1 | 0.529 ** | −0.290 ** | 0.038 | −0.010 | −0.028 | −0.128 ** | −0.011 | −0.011 | −0.125 ** | 0.025 | 0.093 * | 0.063 |
| Male partner education | 0.127 ** | 0.211 ** | 0.311 ** | 0.494 ** | 1 | −0.315 ** | 0.026 | −0.039 | −0.050 | −0.100 * | −0.069 | −0.038 | −0.078 | −0.001 | −0.008 | 0.015 |
| Relationship | −0.122 ** | −0.146 ** | −0.107 * | −0.077 | −0.134 ** | 1 | −0.054 | 0.074 | −0.043 | −0.001 | 0.031 | 0.125 ** | 0.065 | −0.007 | 0.011 | −0.051 |
| Hispanic men | −0.029 | −0.034 | −0.159 ** | −0.220 ** | −0.203 ** | 0.016 | 1 | −0.669 ** | 0.104 * | 0.046 | 0.099 | 0.015 | 0.042 | 0.036 | 0.033 | −0.016 |
| Black men | −0.039 | −0.069 | 0.070 | 0.054 | 0.019 | 0.032 | −0.458 ** | 1 | −0.062 | 0.002 | −0.057 | 0.009 | −0.039 | 0.008 | −0.049 | 0.020 |
| Anxiety | −0.020 | 0.038 | −0.020 | −0.012 | 0.051 | 0.055 | −0.051 | −0.015 | 1 | 0.242 ** | −0.022 | −0.009 | 0.111 * | 0.013 | 0.012 | 0.012 |
| Depression | −0.062 | −0.020 | −0.007 | −0.001 | −0.007 | 0.087 | −0.085 | 0.089 | 0.390 ** | 1 | 0.018 | 0.114 * | 0.057 | −0.017 | −0.011 | −0.136 ** |
| Alcohol | −0.009 | −0.037 | −0.109 | −0.070 | −0.062 | 0.116 | 0.012 | −0.032 | −0.045 | −0.025 | 1 | 0.068 | 0.192 ** | 0.023 | −0.002 | 0.045 |
| Physical IPV | −0.035 | 0.010 | −0.088 | −0.044 | −0.070 | −0.015 | −0.046 | 0.059 | −0.016 | −0.041 | 0.039 | 1 | 0.288 ** | −0.160 ** | −0.061 | −0.085 * |
| Psychological IPV | 0.029 | 0.064 | −0.108 * | −0.062 | −0.100 * | 0.059 | −0.032 | −0.019 | 0.101 * | 0.064 | 0.172 ** | 0.323 ** | 1 | −0.159 ** | −0.119 ** | −0.055 |
| Sexual IPV baseline | 0.052 | 0.033 | −0.033 | −0.047 | −0.009 | −0.022 | 0.059 | −0.082 | 0.010 | 0.027 | −0.068 | −0.235 ** | −0.321 ** | 1 | 0.230 ** | 0.423 ** |
| Sexual IPV 2 years | −0.093 * | −0.111 * | −0.028 | 0.014 | 0.034 | −0.011 | −0.037 | 0.017 | 0.008 | 0.021 | −0.409 ** | −0.042 | −0.324 ** | 0.394 ** | 1 | 0.316 ** |
| Sexual IPV 4 years | −0.010 | −0.006 | −0.018 | 0.091 * | 0.056 | 0.045 | 0.054 | −0.086 | 0.014 | 0.036 | −0.109 | −0.220 ** | −0.200 ** | 0.302 ** | 0.359 ** | 1 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Preiser, B.; Assari, S. Psychological Predictors of Sexual Intimate Partner Violence against Black and Hispanic Women. Behav. Sci. 2018, 8, 3. https://doi.org/10.3390/bs8010003
Preiser B, Assari S. Psychological Predictors of Sexual Intimate Partner Violence against Black and Hispanic Women. Behavioral Sciences. 2018; 8(1):3. https://doi.org/10.3390/bs8010003
Chicago/Turabian StylePreiser, Brianna, and Shervin Assari. 2018. "Psychological Predictors of Sexual Intimate Partner Violence against Black and Hispanic Women" Behavioral Sciences 8, no. 1: 3. https://doi.org/10.3390/bs8010003
APA StylePreiser, B., & Assari, S. (2018). Psychological Predictors of Sexual Intimate Partner Violence against Black and Hispanic Women. Behavioral Sciences, 8(1), 3. https://doi.org/10.3390/bs8010003






