Exploring Factors Associated with Physical Activity in the Elderly: A Cross-Sectional Study during the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
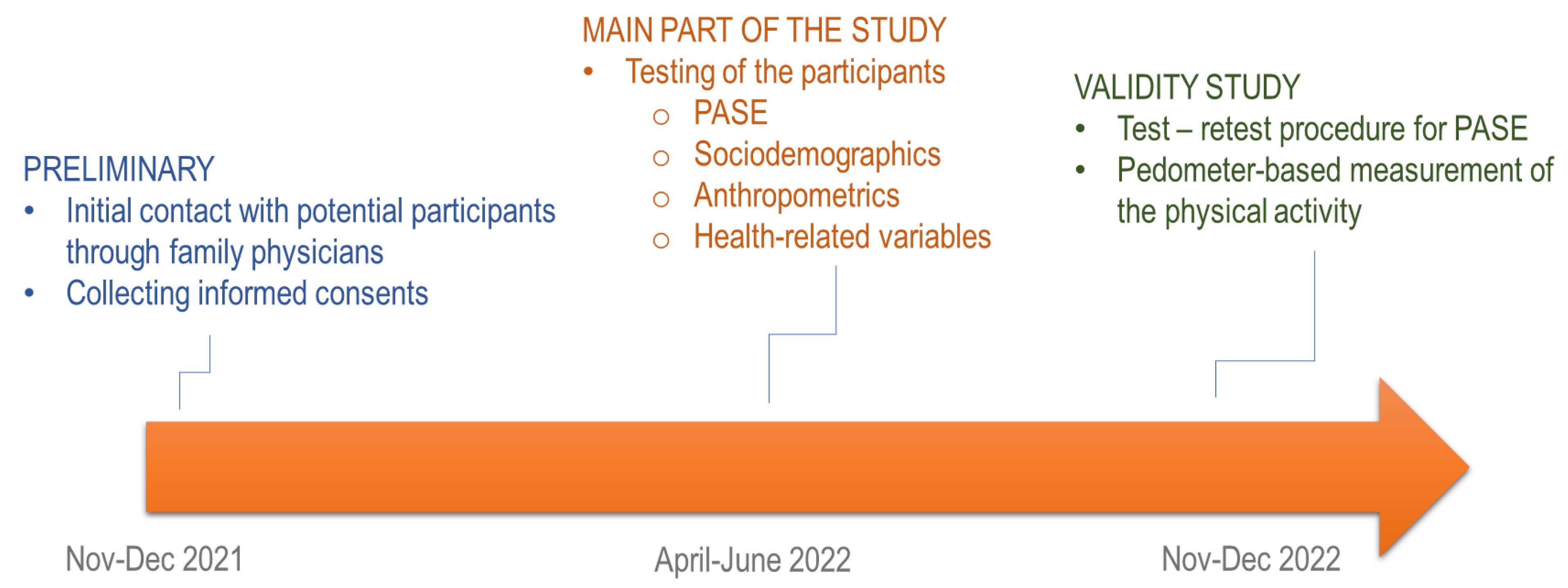
2.1. Participants and Study Design
2.2. Variables and Measurement
2.3. Statistics
3. Results
3.1. Descriptive Statistics
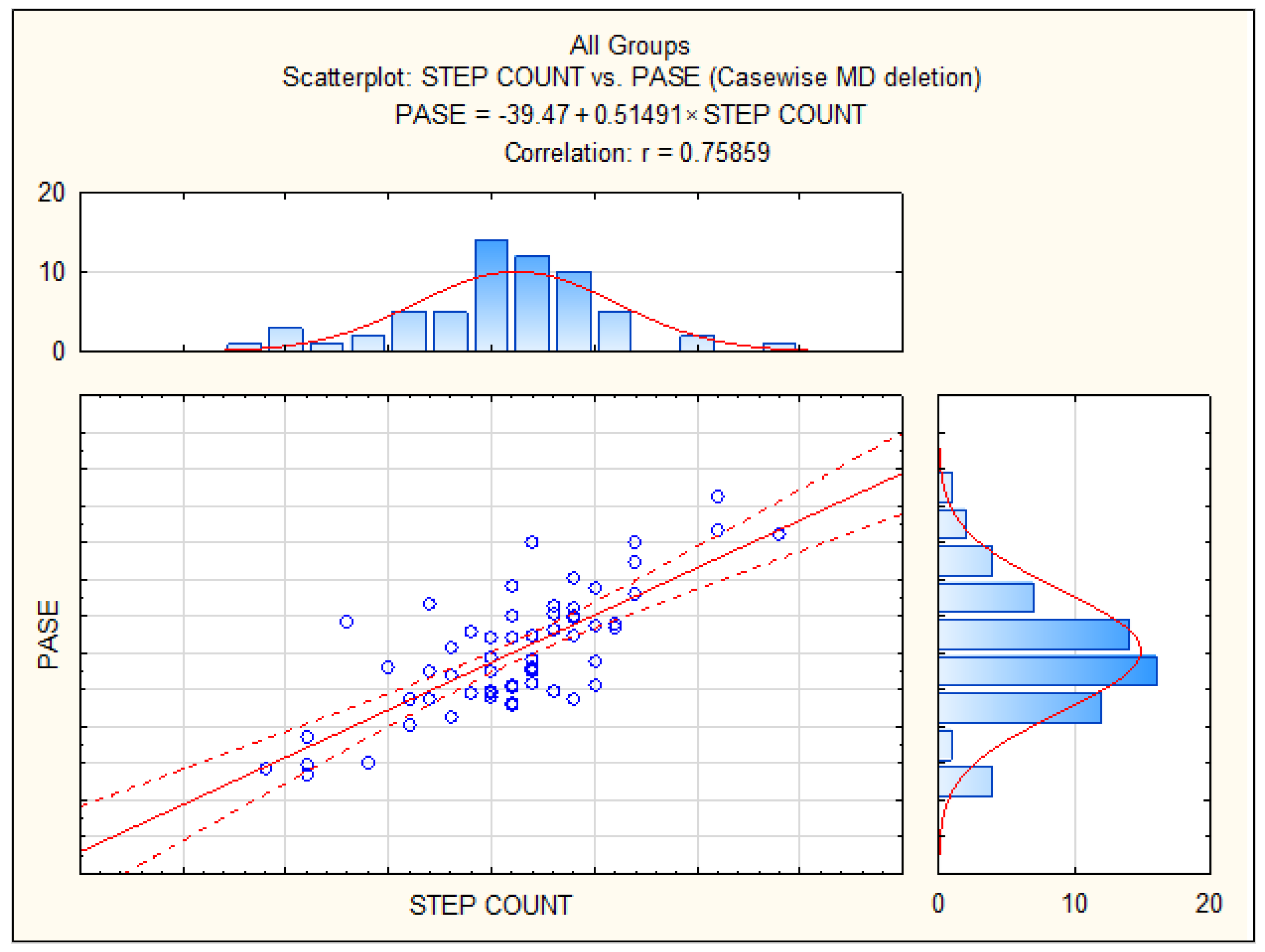
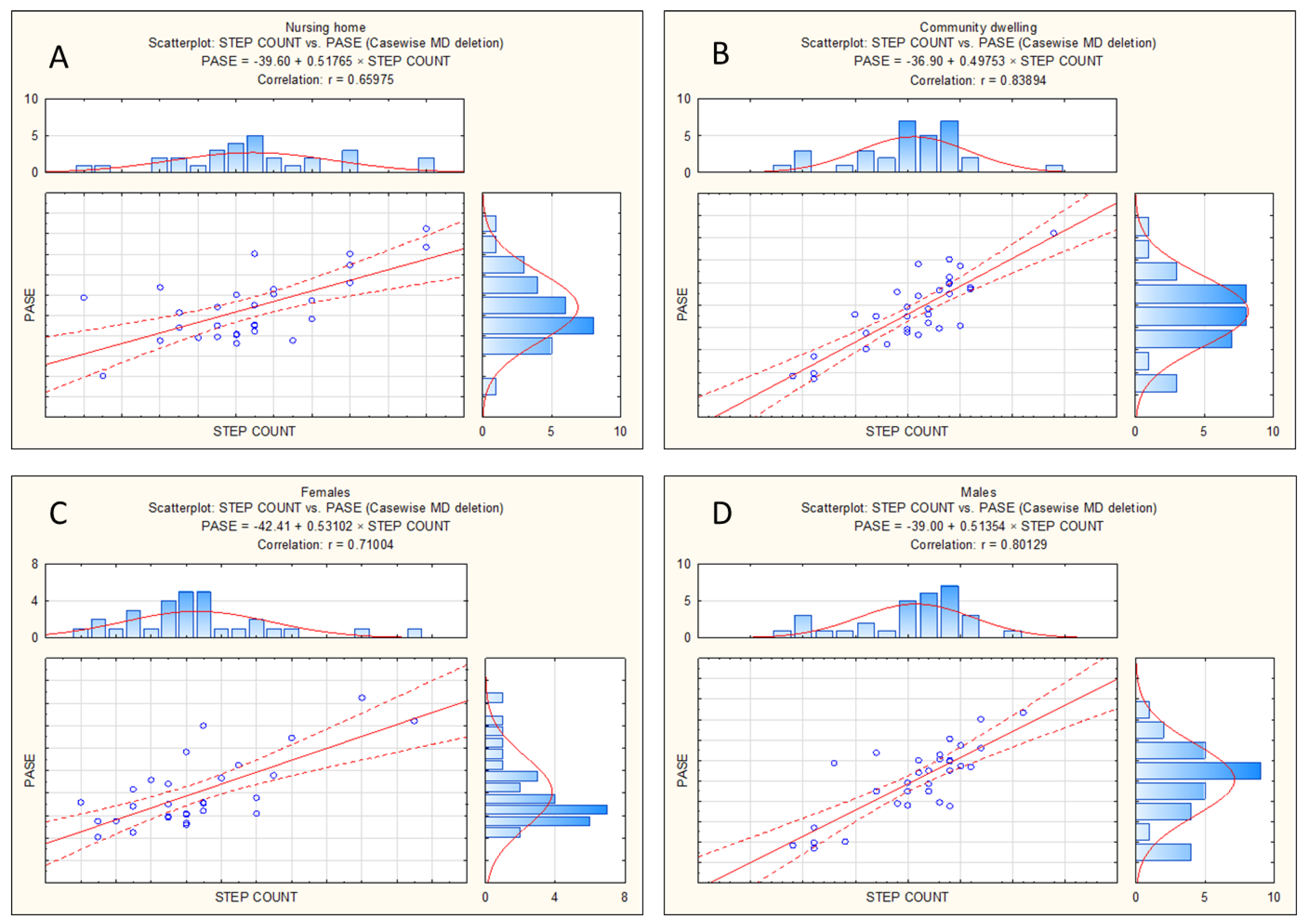
3.2. Reliability and Validity
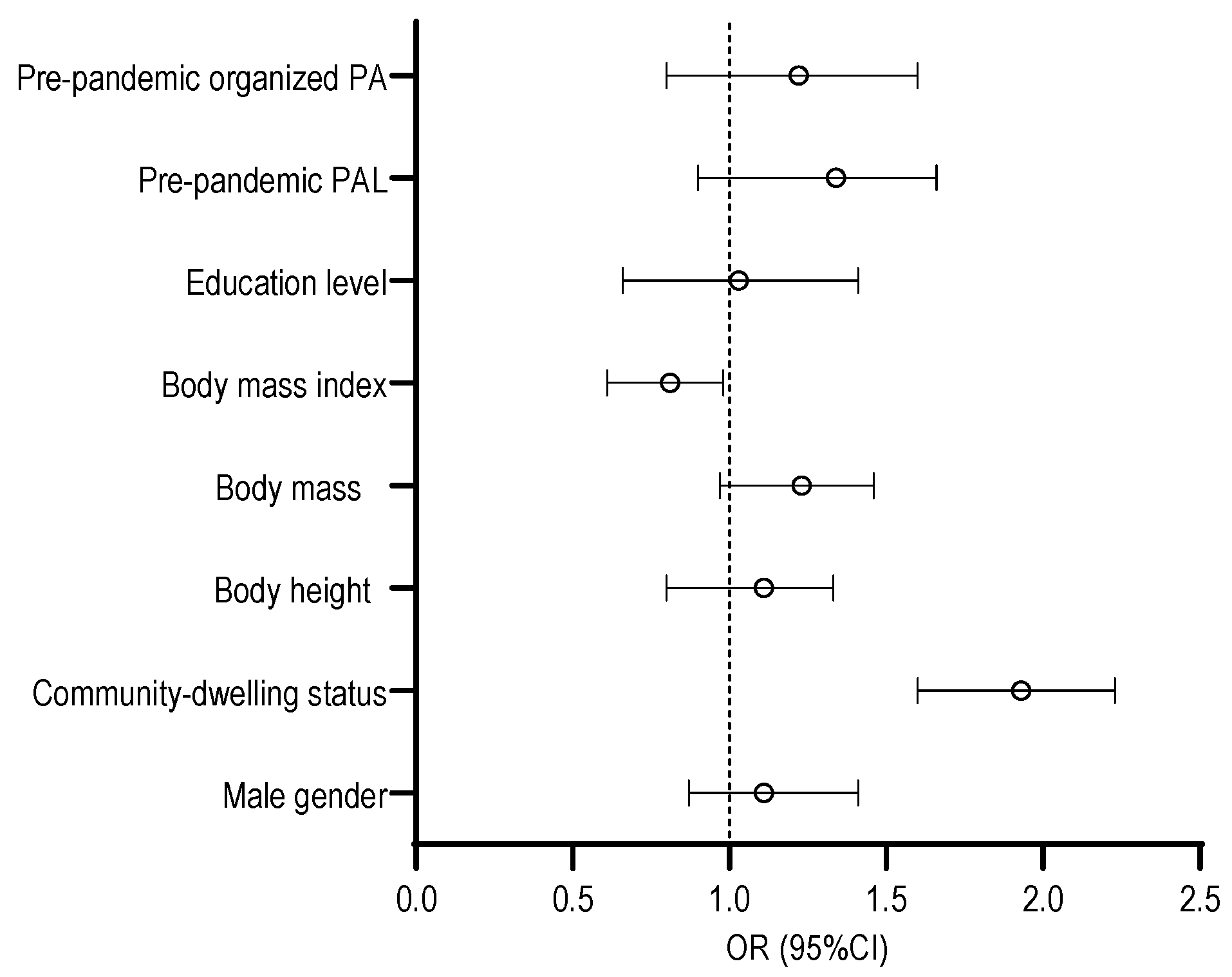
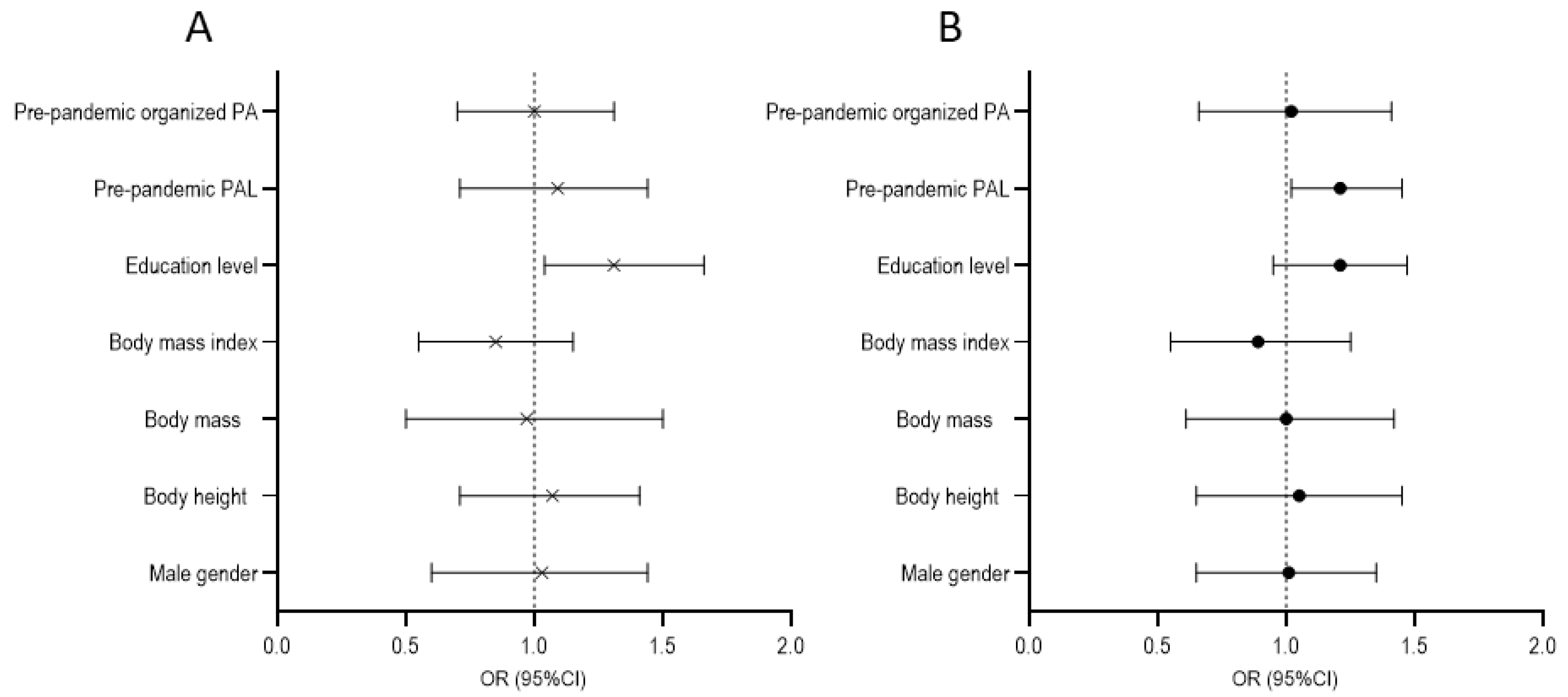
3.3. Correlates of Physical Activity Levels
4. Discussion
4.1. Psychometric Properties of the Physical Activity Questionnaire for Elderly
4.2. Predictors of Physical Activity Levels during the COVID-19 Pandemic
4.3. Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rippe, J.M. Physical activity and lifestyle medicine. J. Fam. Pract. 2021, 15, 212–213. [Google Scholar] [CrossRef] [PubMed]
- Booth, F.W.; Roberts, C.K.; Laye, M.J. Lack of exercise is a major cause of chronic diseases. Compr. Physiol. 2012, 2, 1143–1211. [Google Scholar] [CrossRef] [PubMed]
- Kokkinos, P.; Sheriff, H.; Kheirbek, R. Physical inactivity and mortality risk. Cardiol. Res. Pract. 2011, 2011, 924945. [Google Scholar] [CrossRef] [PubMed]
- Harridge, S.D.; Lazarus, N.R. Physical Activity, Aging, and Physiological Function. Physiology 2017, 32, 152–161. [Google Scholar] [CrossRef]
- Parra-Rizo, M.A.; Vasquez-Gomez, J.; Alvarez, C.; Diaz-Martinez, X.; Troncoso, C.; Leiva-Ordonez, A.M.; Zapata-Lamana, R.; Cigarroa, I. Predictors of the Level of Physical Activity in Physically Active Older People. Behav. Sci. 2022, 12, 331. [Google Scholar] [CrossRef] [PubMed]
- Krems, C.; Luhrmann, P.; Neuhauser-Berthold, M. Physical activity in young and elderly subjects. J. Sports Med. Phys. Fit. 2004, 44, 71. [Google Scholar]
- Bull, F.; Fox, K. Start Active, Stay Active. Sport. Exerc. Sci. 2011, 29. [Google Scholar]
- Oswald, F.; Wahl, H.-W. Housing and health in later life. Rev. Environ. Health 2004, 19, 223–252. [Google Scholar] [CrossRef]
- Kazoglu, M.; Yuruk, Z.O. Comparison of the physical fitness levels in nursing home residents and community-dwelling older adults. Arch. Gerontol. Geriatr. 2020, 89, 104106. [Google Scholar] [CrossRef]
- Ramocha, L.M.; Louw, Q.A.; Tshabalala, M.D. Quality of life and physical activity among older adults living in institutions compared to the community. S. Afr. J. Physiother. 2017, 73, 1–6. [Google Scholar] [CrossRef]
- Ikezoe, T.; Asakawa, Y.; Shima, H.; Kishibuchi, K.; Ichihashi, N. Daytime physical activity patterns and physical fitness in institutionalized elderly women: An exploratory study. Arch. Gerontol. Geriatr. 2013, 57, 221–225. [Google Scholar] [CrossRef]
- Chen, Y.M. Perceived barriers to physical activity among older adults residing in long—Term care institutions. J. Clin. Nurs. 2010, 19, 432–439. [Google Scholar] [CrossRef]
- Dallosso, H.; Morgan, K.; Bassey, E.; Ebrahim, S.; Fentem, P.; Arie, T. Levels of customary physical activity among the old and the very old living at home. J. Epidemiol. Community Health 1988, 42, 121. [Google Scholar] [CrossRef]
- Yon, A.L.; Reel, J.J.; Chen-Edinboro, L.P.; Pate, M.R.; Reich, J.C.; Hillhouse, L.A.; Kantor, R. Influences of the COVID-19 Pandemic on Intuitive Exercise and Physical Activity among College Students. Behav. Sci. 2022, 12, 72. [Google Scholar] [CrossRef]
- Orr, K.; Ta, Z.; Shoaf, K.; Halliday, T.M.; Tobin, S.; Baron, K.G. Sleep, Diet, Physical Activity, and Stress during the COVID-19 Pandemic: A Qualitative Analysis. Behav. Sci. 2022, 12, 66. [Google Scholar] [CrossRef]
- Martinez, E.Z.; Silva, F.M.; Morigi, T.Z.; Zucoloto, M.L.; Silva, T.L.; Joaquim, A.G.; Dall’Agnol, G.; Galdino, G.; Martinez, M.O.Z.; Silva, W.R.D. Physical activity in periods of social distancing due to COVID-19: A cross-sectional survey. Cien Saude Colet. 2020, 25, 4157–4168. [Google Scholar] [CrossRef]
- Stockwell, S.; Trott, M.; Tully, M.; Shin, J.; Barnett, Y.; Butler, L.; McDermott, D.; Schuch, F.; Smith, L. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport. Exerc. Med. 2021, 7, e000960. [Google Scholar] [CrossRef]
- Caputo, E.L.; Reichert, F.F. Studies of physical activity and COVID-19 during the pandemic: A scoping review. J. Phys. Act. Health 2020, 17, 1275–1284. [Google Scholar] [CrossRef]
- Wunsch, K.; Kienberger, K.; Niessner, C. Changes in physical activity patterns due to the COVID-19 pandemic: A systematic review and meta-analysis. Int. J. Environ. Res. Public. Health 2022, 19, 2250. [Google Scholar] [CrossRef]
- Oliveira, M.R.; Sudati, I.P.; Konzen, V.M.; de Campos, A.C.; Wibelinger, L.M.; Correa, C.; Miguel, F.M.; Silva, R.N.; Borghi-Silva, A. Covid-19 and the impact on the physical activity level of elderly people: A systematic review. Exp. Gerontol. 2022, 159, 111675. [Google Scholar] [CrossRef]
- Pelicioni, P.H.S.; Lord, S.R. COVID-19 will severely impact older people’s lives, and in many more ways than you think! Braz. J. Phys. Ther. 2020, 24, 293–294. [Google Scholar] [CrossRef]
- Aubertin-Leheudre, M.; Rolland, Y. The Importance of Physical Activity to Care for Frail Older Adults During the COVID-19 Pandemic. J. Am. Med. Dir. Assoc. 2020, 21, 973–976. [Google Scholar] [CrossRef]
- Pérez, L.M.; Castellano-Tejedor, C.; Cesari, M.; Soto-Bagaria, L.; Ars, J.; Zambom-Ferraresi, F.; Baró, S.; Díaz-Gallego, F.; Vilaró, J.; Enfedaque, M.B.; et al. Depressive Symptoms, Fatigue and Social Relationships Influenced Physical Activity in Frail Older Community-Dwellers during the Spanish Lockdown due to the COVID-19 Pandemic. Int. J. Env. Environ. Res. Public. Health 2021, 18, 808. [Google Scholar] [CrossRef]
- Maugeri, G.; Castrogiovanni, P.; Battaglia, G.; Pippi, R.; D’Agata, V.; Palma, A.; Di Rosa, M.; Musumeci, G. The impact of physical activity on psychological health during COVID-19 pandemic in Italy. Heliyon 2020, 6, e04315. [Google Scholar] [CrossRef]
- Qin, F.; Song, Y.; Nassis, G.P.; Zhao, L.; Dong, Y.; Zhao, C.; Feng, Y.; Zhao, J. Physical Activity, Screen Time, and Emotional Well-Being during the 2019 Novel Coronavirus Outbreak in China. Int. J. Environ. Res. Public Health 2020, 17, 5170. [Google Scholar] [CrossRef] [PubMed]
- Chambonniere, C.; Lambert, C.; Tardieu, M.; Fillon, A.; Genin, P.; Larras, B.; Melsens, P.; Baker, J.S.; Pereira, B.; Tremblay, A.; et al. Physical Activity and Sedentary Behavior of Elderly Populations during Confinement: Results from the FRENCH COVID-19 ONAPS Survey. Exp. Aging Res. 2021, 47, 401–413. [Google Scholar] [CrossRef]
- Shinohara, T.; Saida, K.; Tanaka, S.; Murayama, A. Association between frailty and changes in lifestyle and physical or psychological conditions among older adults affected by the coronavirus disease 2019 countermeasures in Japan. Geriatr. Gerontol. Int. 2021, 21, 39–42. [Google Scholar] [CrossRef]
- Sekulic, D.; Blazevic, M.; Gilic, B.; Kvesic, I.; Zenic, N. Prospective Analysis of Levels and Correlates of Physical Activity during COVID-19 Pandemic and Imposed Rules of Social Distancing; Gender Specific Study among Adolescents from Southern Croatia. Sustainability 2020, 12, 4072. [Google Scholar] [CrossRef]
- Franc, S.; Časni, A.Č.; Barišić, A. Determinants of migration following the EU enlargement: A panel data analysis. South. East. Eur. J. Econ. Bus. 2019, 14, 13–22. [Google Scholar] [CrossRef]
- Washburn, R.A.; Smith, K.W.; Jette, A.M.; Janney, C.A. The Physical Activity Scale for the Elderly (PASE): Development and evaluation. J. Clin. Epidemiol. 1993, 46, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Washburn, R.A.; McAuley, E.; Katula, J.; Mihalko, S.L.; Boileau, R.A. The physical activity scale for the elderly (PASE): Evidence for validity. J. Clin. Epidemiol. 1999, 52, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Jenkinson, C.; Layte, R.; Jenkinson, D.; Lawrence, K.; Petersen, S.; Paice, C.; Stradling, J. A shorter form health survey: Can the SF-12 replicate results from the SF-36 in longitudinal studies? J. Public. Health Med. 1997, 19, 179–186. [Google Scholar] [CrossRef]
- Ozic, S.; Vasiljev, V.; Ivkovic, V.; Bilajac, L.; Rukavina, T. Interventions aimed at loneliness and fall prevention reduce frailty in elderly urban population. Medicine 2020, 99, e19145. [Google Scholar] [CrossRef]
- Shou, J.; Ren, L.; Wang, H.; Yan, F.; Cao, X.; Wang, H.; Wang, Z.; Zhu, S.; Liu, Y. Reliability and validity of 12-item Short-Form health survey (SF-12) for the health status of Chinese community elderly population in Xujiahui district of Shanghai. Aging Clin. Exp. Res. 2016, 28, 339–346. [Google Scholar] [CrossRef]
- Ruuskanen, J.; Parkatti, T. Physical activity and related factors among nursing home residents. J. Am. Geriatr. Soc. 1994, 42, 987–991. [Google Scholar] [CrossRef]
- Loland, N. Reliability of the physical activity scale for the elderly (PASE). Eur. J. Sport. Sci. 2002, 2, 1–12. [Google Scholar] [CrossRef]
- Herrmann, S.D.; Heumann, K.J.; Der Ananian, C.A.; Ainsworth, B.E. Validity and reliability of the global physical activity questionnaire (GPAQ). Meas. Phys. Educ. Exerc. 2013, 17, 221–235. [Google Scholar] [CrossRef]
- Heise, D.R.; Blalock, H., Jr. Separating reliability and stability in test-retest correlation. Causal Models Exp. Des. 2007, 117, 93–101. [Google Scholar]
- Hagiwara, A.; Ito, N.; Sawai, K.; Kazuma, K. Validity and reliability of the Physical Activity Scale for the Elderly (PASE) in Japanese elderly people. Geriatr. Gerontol. Int. 2008, 8, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Ayvat, E.; Kilinc, M.; Kirdi, N. The Turkish version of the Physical Activity Scale for theElderly (PASE): Its cultural adaptation, validation, and reliability. Turk. J. Med. Sci. 2017, 47, 908–915. [Google Scholar] [CrossRef]
- Ngai, S.P.; Cheung, R.T.; Lam, P.L.; Chiu, J.K.; Fung, E.Y. Validation and reliability of the Physical Activity Scale for the Elderly in Chinese population. J. Rehabil. Med. 2012, 44, 462–465. [Google Scholar] [CrossRef] [PubMed]
- Alinia, P.; Cain, C.; Fallahzadeh, R.; Shahrokni, A.; Cook, D.; Ghasemzadeh, H. How accurate is your activity tracker? A comparative study of step counts in low-intensity physical activities. JMIR Mhealth Uhealth 2017, 5, e6321. [Google Scholar] [CrossRef]
- Ainsworth, B.E. Issues in the assessment of physical activity in women. Res. Q. Exerc. Sport. 2000, 71, 37–42. [Google Scholar] [CrossRef]
- Santos, D.A.; Silva, A.M.; Baptista, F.; Santos, R.; Vale, S.; Mota, J.; Sardinha, L.B. Sedentary behavior and physical activity are independently related to functional fitness in older adults. Exp. Gerontol. 2012, 47, 908–912. [Google Scholar] [CrossRef]
- Sarkisian, C.A.; Prohaska, T.R.; Wong, M.D.; Hirsch, S.; Mangione, C.M. The relationship between expectations for aging and physical activity among older adults. J. Gen. Intern. Med. 2005, 20, 911–915. [Google Scholar] [CrossRef]
- Benedetti, T.R.B.; Borges, L.J.; Petroski, E.L.; Gonçalves, L.H.T. Physical activity and mental health status among elderly people. Rev. De. Saúde Pública 2008, 42, 302–307. [Google Scholar] [CrossRef]
- McAuley, E.; Konopack, J.F.; Motl, R.W.; Morris, K.S.; Doerksen, S.E.; Rosengren, K.R. Physical activity and quality of life in older adults: Influence of health status and self-efficacy. Ann. Behav. Med. 2006, 31, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Pernambuco, C.S.; Rodrigues, B.M.; Bezerra, J.C.P.; Carrielo, A.; Fernandes, A.; Vale, R.; Dantas, E. Quality of life, elderly and physical activity. Health 2012, 4, 88–93. [Google Scholar] [CrossRef][Green Version]
- Whitehead, M. The concept of physical literacy. Eur. J. Phys. Educ. 2001, 6, 127–138. [Google Scholar] [CrossRef]
- Whitehead, M. Definition of physical literacy and clarification of related issues. Icsspe Bull. 2013, 65, 15–23. [Google Scholar]
- Whitehead, M. Physical Literacy: Throughout the Lifecourse; Routledge: New York, NY, USA, 2010. [Google Scholar]
- Huang, Y.; Sum, K.R.; Yang, Y.J.; Chun-Yiu Yeung, N. Measurements of Older Adults’ Physical Competence under the Concept of Physical Literacy: A Scoping Review. Int. J. Environ. Res. Public Health 2020, 17, 6570. [Google Scholar] [CrossRef]
- Roetert, E.P.; Ortega, C. Physical literacy for the older adult. Strength. Cond. J. 2019, 41, 89–99. [Google Scholar] [CrossRef]
- Pavey, T.G.; Peeters, G.G.; Gomersall, S.R.; Brown, W.J. Long-term effects of physical activity level on changes in healthy body mass index over 12 years in young adult women. Mayo Clin. Proc. 2016, 91, 735–744. [Google Scholar] [CrossRef]
- Van Dyck, D.; Cerin, E.; De Bourdeaudhuij, I.; Hinckson, E.; Reis, R.S.; Davey, R.; Sarmiento, O.L.; Mitas, J.; Troelsen, J.; MacFarlane, D.; et al. International study of objectively measured physical activity and sedentary time with body mass index and obesity: IPEN adult study. Int. J. Obes. 2015, 39, 199–207. [Google Scholar] [CrossRef]
- Cárdenas Fuentes, G.; Bawaked, R.A.; Martínez González, M.Á.; Corella, D.; Subirana Cachinero, I.; Salas-Salvadó, J.; Estruch, R.; Serra-Majem, L.; Ros, E.; Lapetra Peralta, J.; et al. Association of physical activity with body mass index, waist circumference and incidence of obesity in older adults. Eur. J. Public. Health 2018, 28, 944–950. [Google Scholar] [CrossRef]
- Silva, B.; Camões, M.; Simões, M.; Bezerra, P. Obesity, Physical Fitness and Inflammation in the Elderly. Geriatrics 2017, 2, 30. [Google Scholar] [CrossRef]
- Brach, J.S.; Almeida, G.J.; Perera, S.; Hergenroeder, A.; Kotlarczyk, M.; Gibbs, B.B. The Role of the Environment on Sedentary Behavior in Community-Dwelling Older Adults. J. Hous. Elder. 2019, 33, 31–40. [Google Scholar] [CrossRef]
- Siltanen, S.; Keskinen, K.E.; Lahti, A.M.; Rantanen, T.; von Bonsdorff, M. Active Aging in Senior Housing Residents and Community-Dwelling Older Adults: A Comparative Study in Finland. J. Aging Health 2023, 8982643231186627. [Google Scholar] [CrossRef]
- MacRae, P.G.; Asplund, L.A.; Schnelle, J.F.; Ouslander, J.G.; Abrahamse, A.; Morris, C. A walking program for nursing home residents: Effects on walk endurance, physical activity, mobility, and quality of life. J. Am. Geriatr. Soc. 1996, 44, 175–180. [Google Scholar] [CrossRef]
- Kalinowski, S.; Wulff, I.; Kölzsch, M.; Kopke, K.; Kreutz, R.; Dräger, D. Physical activity in nursing homes—Barriers and facilitators: A cross-sectional study. J. Aging Phys. Act. 2012, 20, 421–441. [Google Scholar] [CrossRef][Green Version]
- Li, Y.; Cheng, Z.; Cai, X.; Mao, Y.; Temkin-Greener, H. State social distancing restrictions and nursing home outcomes. Sci. Rep. 2022, 12, 1058. [Google Scholar] [CrossRef] [PubMed]
- Aggio, D.; Papacosta, O.; Lennon, L.; Whincup, P.; Wannamethee, G.; Jefferis, B.J. Association between physical activity levels in mid-life with physical activity in old age: A 20-year tracking study in a prospective cohort. BMJ Open 2017, 7, e017378. [Google Scholar] [CrossRef] [PubMed]
- Telama, R. Tracking of Physical Activity from Childhood to Adulthood: A Review. Obes. Facts 2009, 2, 187–195. [Google Scholar] [CrossRef]
- Vogel, T.; Brechat, P.H.; Leprêtre, P.M.; Kaltenbach, G.; Berthel, M.; Lonsdorfer, J. Health benefits of physical activity in older patients: A review. Int. J. Clin. Pract. 2009, 63, 303–320. [Google Scholar] [CrossRef] [PubMed]
- Tammelin, T.; Näyhä, S.; Laitinen, J.; Rintamäki, H.; Järvelin, M.-R. Physical activity and social status in adolescence as predictors of physical inactivity in adulthood. Prev. Med. 2003, 37, 375–381. [Google Scholar] [CrossRef]
- Droomers, M.; Schrijvers, C.T.; Mackenbach, J.P. Educational level and decreases in leisure time physical activity: Predictors from the longitudinal GLOBE study. J. Epidemiol. Community Health 2001, 55, 562–568. [Google Scholar] [CrossRef]
- Schüz, B.; Li, A.S.-W.; Hardinge, A.; McEachan, R.R.; Conner, M. Socioeconomic status as a moderator between social cognitions and physical activity: Systematic review and meta-analysis based on the Theory of Planned Behavior. Psychol. Sport. Exerc. 2017, 30, 186–195. [Google Scholar] [CrossRef]

| Total Sample (n = 211) | Males (n = 110) | Females (n = 101) | |
|---|---|---|---|
| Age (years) | 71.44 ± 3.54 | 71.12 ± 4.11 | 72.01 ± 4.54 |
| Body height (cm) | 163.11 ± 4.58 | 166.11 ± 4.01 | 161.21 ± 3.11 * |
| Body mass (kg) | 73.13 ± 6.01 | 74.13 ± 3.22 | 72.41 ± 5.11 * |
| Body mass index (kg/m2) | 27.21 ± 5.01 | 26.65 ± 3.33 | 28.2 ± 4.00 * |
| SF-12_MCS (score) | 55.02 ± 10.11 | 54.12 ± 8.33 | 56.81 ± 11.12 |
| SF-12_PCS (score) | 49.44 ± 8.31 | 50.56 ± 10.13 | 48.91 ± 7.84 |
| PASE (score) | 156.32 ± 40.12 | 161.32 ± 39.18 | 152.31 ± 40.72 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miljanovic Damjanovic, V.; Obradovic Salcin, L.; Ostojic, D.; Ostojic, L.; Gilic, B.; Geets Kesic, M.; Uzicanin, E.; Sekulic, D. Exploring Factors Associated with Physical Activity in the Elderly: A Cross-Sectional Study during the COVID-19 Pandemic. Behav. Sci. 2024, 14, 62. https://doi.org/10.3390/bs14010062
Miljanovic Damjanovic V, Obradovic Salcin L, Ostojic D, Ostojic L, Gilic B, Geets Kesic M, Uzicanin E, Sekulic D. Exploring Factors Associated with Physical Activity in the Elderly: A Cross-Sectional Study during the COVID-19 Pandemic. Behavioral Sciences. 2024; 14(1):62. https://doi.org/10.3390/bs14010062
Chicago/Turabian StyleMiljanovic Damjanovic, Vesna, Lejla Obradovic Salcin, Daria Ostojic, Ljerka Ostojic, Barbara Gilic, Marijana Geets Kesic, Edin Uzicanin, and Damir Sekulic. 2024. "Exploring Factors Associated with Physical Activity in the Elderly: A Cross-Sectional Study during the COVID-19 Pandemic" Behavioral Sciences 14, no. 1: 62. https://doi.org/10.3390/bs14010062
APA StyleMiljanovic Damjanovic, V., Obradovic Salcin, L., Ostojic, D., Ostojic, L., Gilic, B., Geets Kesic, M., Uzicanin, E., & Sekulic, D. (2024). Exploring Factors Associated with Physical Activity in the Elderly: A Cross-Sectional Study during the COVID-19 Pandemic. Behavioral Sciences, 14(1), 62. https://doi.org/10.3390/bs14010062










