Effect of Dancing Interventions on Depression and Anxiety Symptoms in Older Adults: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
- P (Population): Older adults (as defined by each study or, in cases where the population was not specifically restricted, study sample with a mean age of 60 or older [29]).
- I (Intervention): Dance.
- C (Comparator): Other types of intervention or no intervention, as well as participants’ comorbidities.
- O (Outcome): Symptoms of depression and/or anxiety.
- S (Study design): Randomized controlled clinical trials.
2.1. Search Strategy and Study Selection
2.2. Eligibility Criteria
2.3. Data Extraction
2.4. Risk of Bias
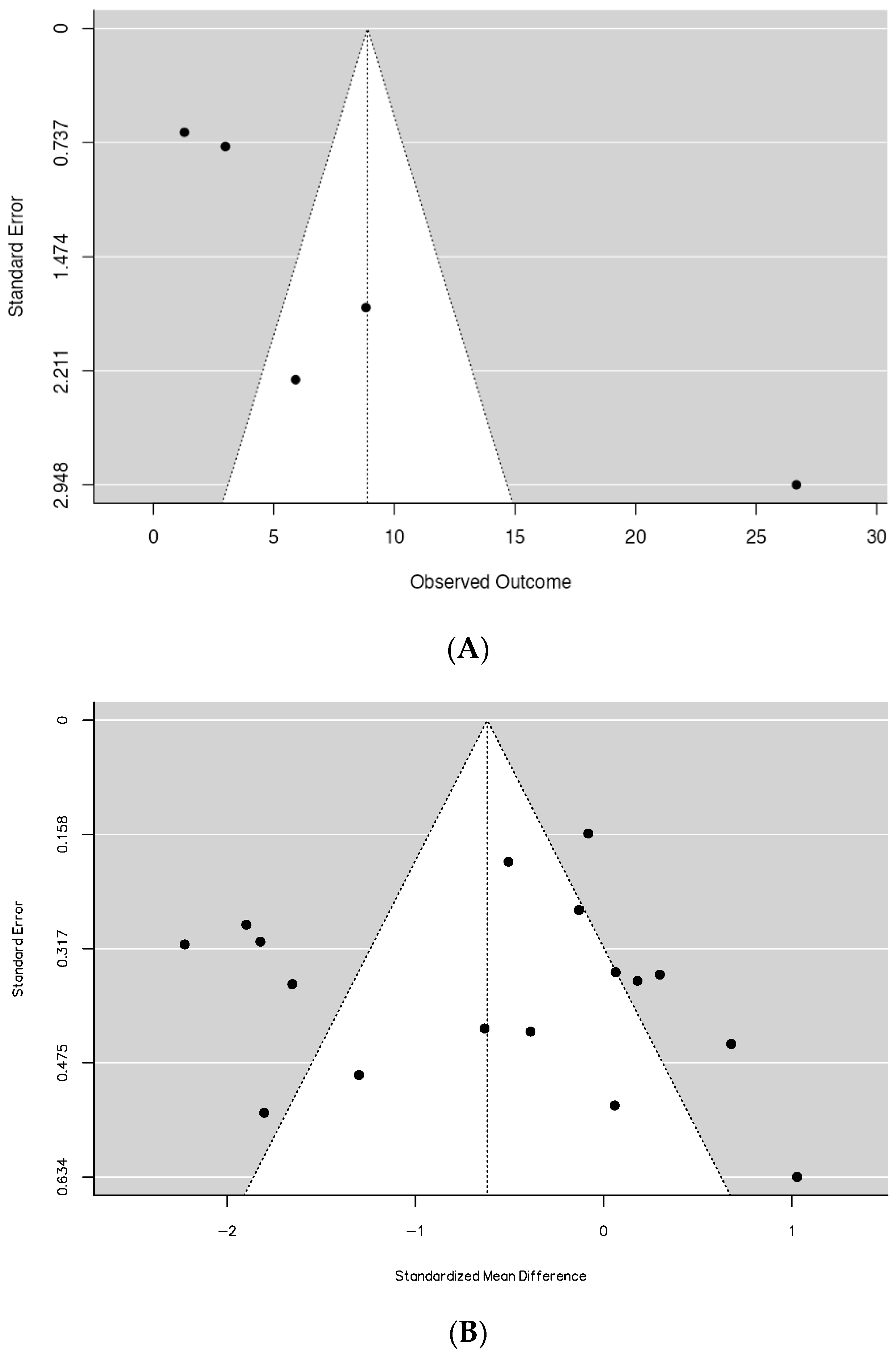
2.5. Publication Bias
2.6. Certainty of Evidence
2.7. Statistical Analysis
3. Results
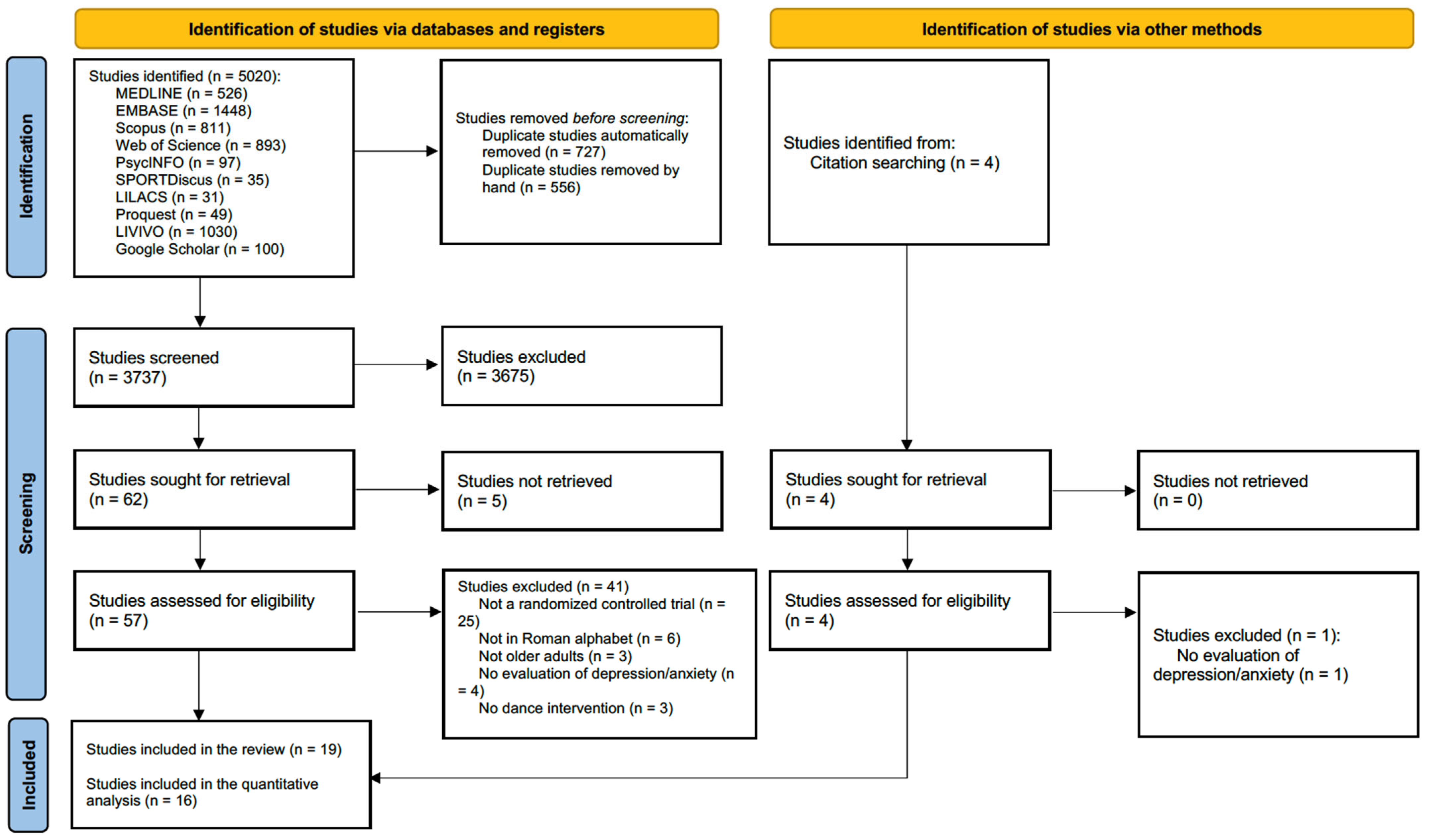
3.1. Selection Process
3.2. Study Characteristics
3.2.1. Anxiety
3.2.2. Depression
| Author, Year | Country | Control Group (n) | Dance Group (n) | Comorbidities | Dance Type | Dance Schedule | Dance Program Duration | Control | Setting | Measurement of Depression * | Measurement of Anxiety * | Result (Intergroup) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anxiety | ||||||||||||
| Mavrovouniotis, et al., 2010 [16] | Greece | 35 | 76 | None | Greek traditional dance | 60 min/session | 2.5 months | Socialization | Health center | NA | SAI | ↓ |
| Alves, et al., 2013 [42] | Brazil | 25 | 25 | None | Ballroom dance | 120 min 2 times/week | 4 months | None | NR | NA | BAI | ↓ |
| Depression | ||||||||||||
| Haboush, et al., 2006 [49] | USA | 12 | 10 | None | Ballroom dance | 45 min 1 day/week | 2 months | None | NR | GDS and HRSD | NA | — |
| Castro, et al., 2009 [46] | Brazil | 20 | 20 | None | Various | 50 min 3 times/week | 6 months | None | NR | BDI | NA | ↓ |
| Eyigor, et al., 2009 [48] | Turkey | 18 | 19 | None | Folkloric dance | 60 min 3 times/week | 2 months | None | Rehabilitation unit | GDS | NA | — |
| Vankova, et al., 2014 [17] | Czech Republic | 83 | 79 | None | Various | 60 min 1 day/week | 3 months | None | Nursing homes | GDS | NA | ↓ |
| Broadbent, et al., 2015 [45] | Brazil | 7 | 7 | None | Belly dance | 45 min 2 times/week | 5 weeks | None | Community center | GDS | NA | ↓ |
| Lee, et al., 2015 [50] | South Korea | 10 | 10 | PD | Video game dancing | 30 min 5 days/week | 1.5 month | NDT and FES | NR | BDI | NA | ↓ |
| Rios, et al., 2015 [52] | Canada | 15 | 18 | PD | Tango | 60 min 2 days/week | 3 months | None | NR | BDI | NA | — |
| Aguinaga, et al., 2016 [56] | USA | 11 | 10 | MCI | Latin dance | 60 min 2 times/week | 4 months | None | Day care center | GDS | NA | ↑ |
| Michels, et al., 2018 [51] | USA | 4 | 9 | PD | Dance therapy | 60 min 1 day/week | 2.5 months | Talk therapy | Movement studio | BDI | NA | NR |
| Zhu, et al., 2018 [55] | China | 31 | 27 | MCI | Aerobic dance | 35 min 3 days/week | 3 months | Physician counseling | Hospital | GDS | NA | — |
| Solla, et al., 2019 [53] | Italy | 9 | 10 | PD | Sardinian Folk dance | 90 min 2 days/week | 3 months | None | NR | BDI | NA | ↓ |
| Chang, et al., 2021 [47] | China | 47 | 62 | MCI | Square dance | 30 min 3 times/week | 4.5 months | None | Nursing homes | GDS | NA | ↓ |
| Ayari, et al., 2023 [44] | France | 12 | 11 | MCI | Improvised dance | 60 min 1 day/week | 4 months | Aerobic exercise | Day care center | GDS | NA | — |
| Zhang, et al., 2023 [54] | China | 36 | 36 | None | Square dance | 60 min 4 days/week | 4 months | None | Outdoors | GDS | NA | ↓ |
| Anxiety and depression | ||||||||||||
| Zhang, et al., 2014 [43] | China | 30 | 30 | None | Square dance | 30–60 min ≥4 days/week | 18 months | Various | NR | HAMD | HAMA | ↓ both |
| Serrano-Guzman, et al., 2016 [40] | Spain | 35 | 32 | HTN | Dance therapy | 50 min 3 days/week | 2 months | None | NR | EuroQoL-5D | EuroQoL-5D | ↓ both |
| Bisbe, et al., 2020 [41] | Spain | 14 | 17 | MCI | Aerobic dance | 60 min 2 days/week | 3 months | Physical therapy | Hospital | HADS | HADS | — both |
3.3. Statistical Analysis
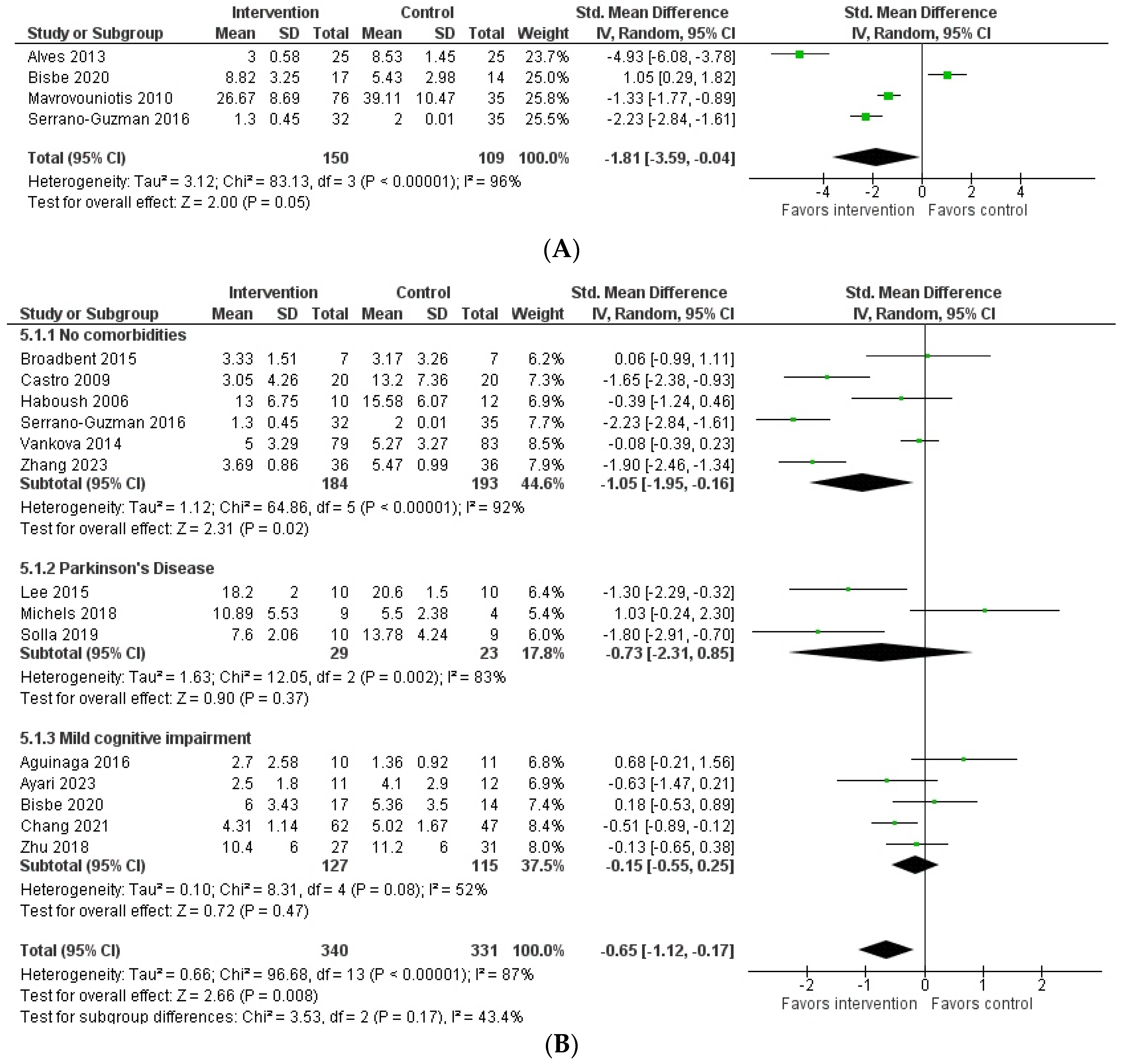
3.3.1. Anxiety
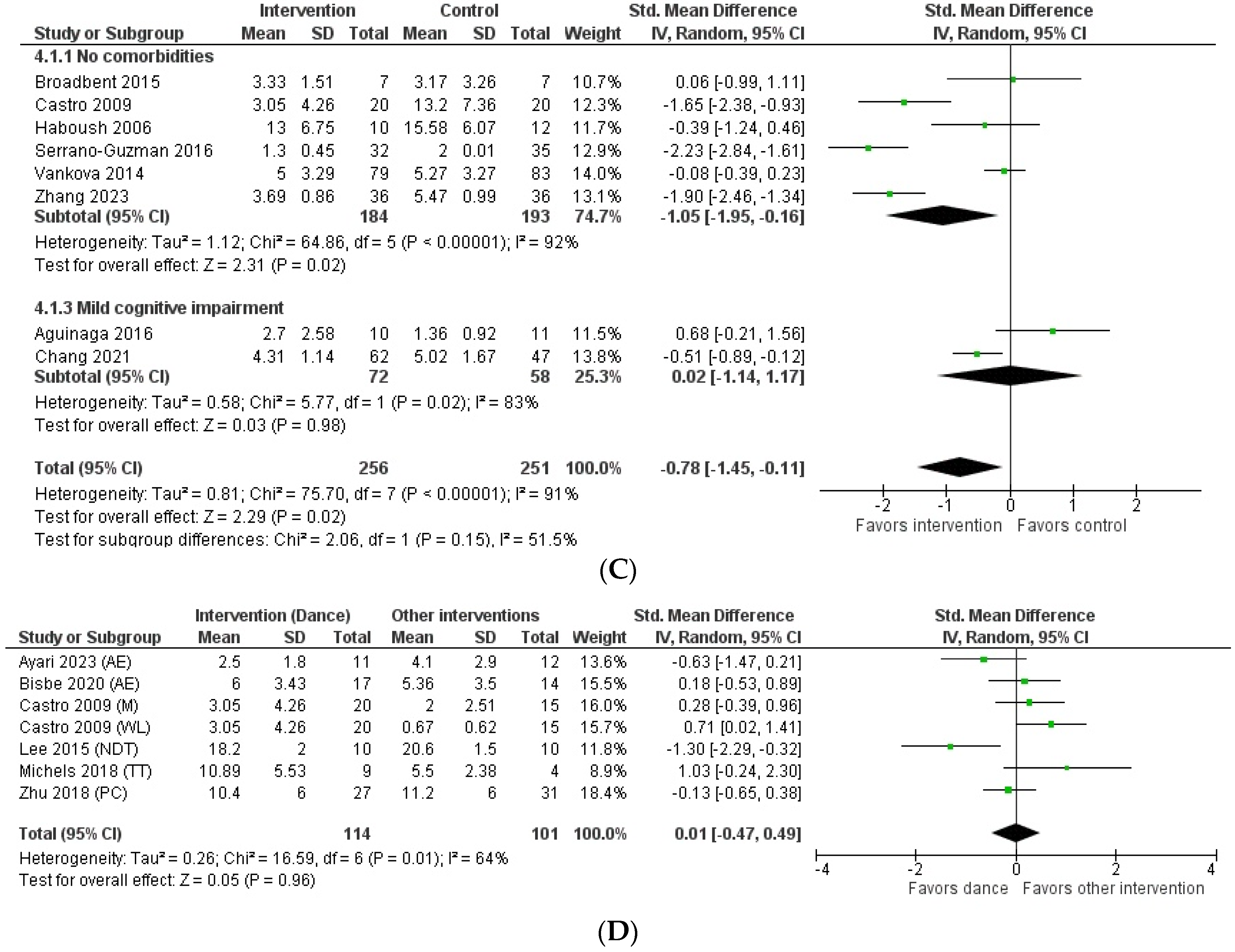
3.3.2. Depression
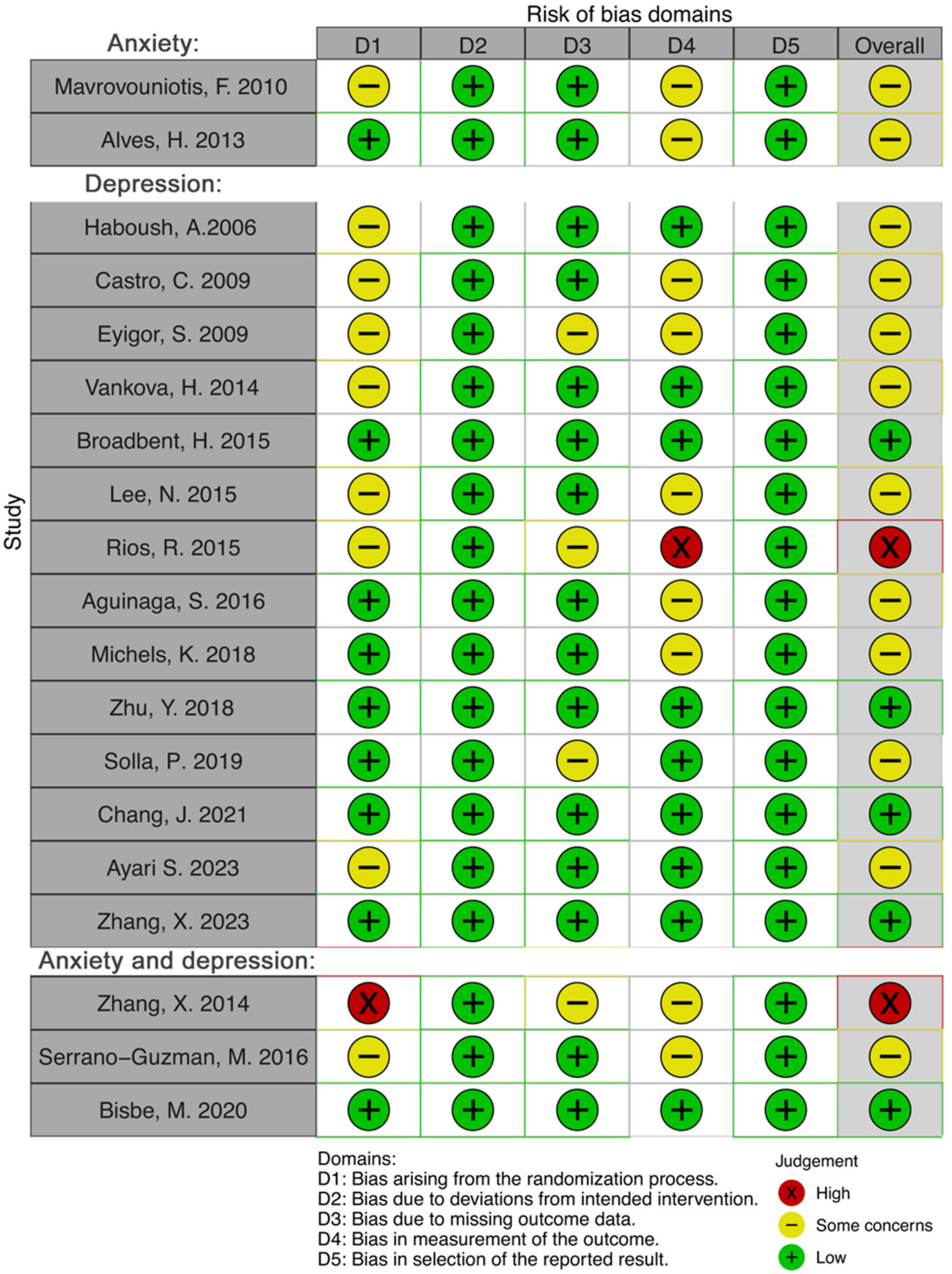
3.4. Risk of Bias
3.5. Publication Bias
3.6. Certainty of Evidence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rudnicka, E.; Napierała, P.; Podfigurna, A.; Męczekalski, B.; Smolarczyk, R.; Grymowicz, M. The World Health Organization (WHO) Approach to Healthy Ageing. Maturitas 2020, 139, 6–11. [Google Scholar] [CrossRef]
- Zenebe, Y.; Akele, B.; W/Selassie, M.; Necho, M. Prevalence and Determinants of Depression among Old Age: A Systematic Review and Meta-Analysis. Ann. Gen. Psychiatry 2021, 20, 55. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention and National Association of Chronic Disease Directors. The State of Mental Health and Aging in America Issue Brief 1: What Do the Data Tell Us? National Association of Chronic Disease Directors: Atlanta, GA, USA, 2008. [Google Scholar]
- Holvast, F.; Massoudi, B.; Oude Voshaar, R.C.; Verhaak, P.F.M. Non-Pharmacological Treatment for Depressed Older Patients in Primary Care: A Systematic Review and Meta-Analysis. PLoS ONE 2017, 12, e0184666. [Google Scholar] [CrossRef] [PubMed]
- Heissel, A.; Heinen, D.; Brokmeier, L.L.; Skarabis, N.; Kangas, M.; Vancampfort, D.; Stubbs, B.; Firth, J.; Ward, P.B.; Rosenbaum, S.; et al. Exercise as Medicine for Depressive Symptoms? A Systematic Review and Meta-Analysis with Meta-Regression. Br. J. Sports Med. 2023, 57, 1049–1057. [Google Scholar] [CrossRef]
- Mackrell, J.R. Dance. Encyclopedia Britannica, 4 December 2023. Available online: https://www.britannica.com/art/dance (accessed on 23 December 2023).
- Wang, L.; Guo, F.; Zhao, C.; Zhao, M.; Zhao, C.; Guo, J.; Zhang, L.; Zhang, L.; Li, Z.; Zhu, W. The Effect of Aerobic Dancing on Physical Fitness and Cognitive Function in Older Adults during the COVID-19 Pandemic-a Natural Experiment. Sports Med. Health Sci. 2023, 5, 196–204. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.X.; Yap, X.Y.; Tam, W.S.W.; Goh, J.; Mok, W.Y.J.; Ramazanu, S. Qualitative Inquiry of a Community Dance Program for Older Adults in Singapore. Nurs. Health Sci. 2023, 25, 341–353. [Google Scholar] [CrossRef]
- Sodums, D.J.; Kim, S.; Gallucci, C.E.; Natadiria, M.; Bar, R.; Gardner, S.; Tafler, M. Impact of Sharing Dance Older Adults on Physical and Psychosocial Outcomes. Can. J. Aging 2023, 5, 1–14. [Google Scholar] [CrossRef]
- Akandere, M.; Demir, B. The Effect of Dance over Depression. Coll Antropol 2011, 35, 651–656. [Google Scholar]
- Salihu, D.; Kwan, R.Y.C.; Wong, E.M.L. The Effect of Dancing Interventions on Depression Symptoms, Anxiety, and Stress in Adults without Musculoskeletal Disorders: An Integrative Review and Meta-Analysis. Complement. Ther. Clin. Pract. 2021, 45, 101467. [Google Scholar] [CrossRef]
- Zhao, Y.; Yin, M.; Yao, X.; Li, Z. Effects of Nurse-Led Square Dancing on Older Patients with Mild Cognitive Impairment Combined with Depressive Symptoms: A Pilot Study. Geriatr. Nurs. 2021, 42, 1164–1171. [Google Scholar] [CrossRef]
- Wang, S.; Yin, H.; Meng, X.; Shang, B.; Meng, Q.; Zheng, L.; Wang, L.; Chen, L. Effects of Chinese Square Dancing on Older Adults with Mild Cognitive Impairment. Geriatr. Nurs. 2020, 41, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Adam, D.; Ramli, A.; Shahar, S. Effectiveness of a Combined Dance and Relaxation Intervention on Reducing Anxiety and Depression and Improving Quality of Life among the Cognitively Impaired Elderly. Sultan Qaboos Univ. Med. J. 2016, 16, e47–e53. [Google Scholar] [CrossRef] [PubMed]
- Alpert, P.T.; Miller, S.K.; Wallmann, H.; Havey, R.; Cross, C.; Chevalia, T.; Gillis, C.B.; Kodandapari, K. The Effect of Modified Jazz Dance on Balance, Cognition, and Mood in Older Adults. J. Am. Acad. Nurse Pract. 2009, 21, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Mavrovouniotis, F.H.; Argiriadou, E.A.; Papaioannou, C.S. Greek Traditional Dances and Quality of Old People’s Life. J. Bodyw. Mov. Ther. 2010, 14, 209–218. [Google Scholar] [CrossRef]
- Vankova, H.; Holmerova, I.; Machacova, K.; Volicer, L.; Veleta, P.; Celko, A.M. The Effect of Dance on Depressive Symptoms in Nursing Home Residents. J. Am. Med. Dir. Assoc. 2014, 15, 582–587. [Google Scholar] [CrossRef] [PubMed]
- Cross, K.; Flores, R.; Butterfield, J.; Blackman, M.; Lee, S. The Effect of Passive Listening versus Active Observation of Music and Dance Performances on Memory Recognition and Mild to Moderate Depression in Cognitively Impaired Older Adults. Psychol. Rep. 2012, 111, 413–423. [Google Scholar] [CrossRef]
- Ismail, Z.; Elbayoumi, H.; Fischer, C.E.; Hogan, D.B.; Millikin, C.P.; Schweizer, T.; Mortby, M.E.; Smith, E.E.; Patten, S.B.; Fiest, K.M. Prevalence of Depression in Patients with Mild Cognitive Impairment. JAMA Psychiatry 2017, 74, 58. [Google Scholar] [CrossRef]
- Chendo, I.; Silva, C.; Duarte, G.S.; Prada, L.; Vian, J.; Quintão, A.; Voon, V.; Ferreira, J.J. Frequency of Depressive Disorders in Parkinson’s Disease: A Systematic Review and Meta-Analysis. J. Park. Dis. 2022, 12, 1409–1418. [Google Scholar] [CrossRef]
- Wu, V.X.; Chi, Y.; Lee, J.K.; Goh, H.S.; Chen, D.Y.M.; Haugan, G.; Chao, F.F.T.; Klainin-Yobas, P. The Effect of Dance Interventions on Cognition, Neuroplasticity, Physical Function, Depression, and Quality of Life for Older Adults with Mild Cognitive Impairment: A Systematic Review and Meta-Analysis. Int. J. Nurs. Stud. 2021, 122, 104025. [Google Scholar] [CrossRef]
- McNeely, M.E.; Duncan, R.P.; Earhart, G.M. Impacts of Dance on Non-Motor Symptoms, Participation, and Quality of Life in Parkinson Disease and Healthy Older Adults. Maturitas 2015, 82, 336–341. [Google Scholar] [CrossRef]
- Podolski, O.S.; Whitfield, T.; Schaaf, L.; Cornaro, C.; Köbe, T.; Koch, S.; Wirth, M. The Impact of Dance Movement Interventions on Psychological Health in Older Adults without Dementia: A Systematic Review and Meta-Analysis. Brain Sci. 2023, 13, 981. [Google Scholar] [CrossRef] [PubMed]
- Rittiwong, T.; Reangsing, C.; Schneider, J.K. The Effects of Dance Interventions on Depression in Older Adults: A Meta-Analysis. J. Appl. Gerontol. 2023, 42, 2009–2024. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Liu, M.; Tan, Y.; Dong, Z.; Wu, J.; Cui, H.; Shen, D.; Chi, I. Effectiveness of Dance-Based Interventions on Depression for Persons with MCI and Dementia: A Systematic Review and Meta-Analysis. Front. Psychol. 2022, 12, 709208. [Google Scholar] [CrossRef]
- Dwarika, M.S.; Haraldsen, H.M. Mental Health in Dance: A Scoping Review. Front. Psychol. 2023, 14, 1090645. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Building Leadership and Capacity for the UN Decade of Healthy Ageing (2021–2030). Available online: https://www.who.int/activities/building-leadership-and-capacity-for-the-un-decade-of-healthy-ageing-(2021-2030) (accessed on 23 November 2023).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. J. Clin. Epidemiol. 2021, 134, 178–189. [Google Scholar] [CrossRef] [PubMed]
- Organization of American States. Inter-American Convention on Protecting the Human Rights of Older Persons; OAS: Washington, DC, USA, 2015; Available online: https://www.oas.org/en/sla/dil/docs/inter_american_treaties_A-70_human_rights_older_persons.pdf (accessed on 5 December 2023).
- Rethlefsen, M.L.; Kirtley, S.; Waffenschmidt, S.; Ayala, A.P.; Moher, D.; Page, M.J.; Koffel, J.B.; Blunt, H.; Brigham, T.; Chang, S.; et al. PRISMA-S: An Extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews. Syst. Rev. 2021, 10, 39. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Begg, C.B.; Mazumdar, M. Operating Characteristics of a Rank Correlation Test for Publication Bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef]
- Rosenthal, R. The File Drawer Problem and Tolerance for Null Results. Psychol. Bull. 1979, 86, 638–641. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in Meta-Analysis Detected by a Simple, Graphical Test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Schünemann, H.J.; Higgins, J.P.; Vist, G.E.; Glasziou, P.; Akl, E.A.; Skoetz, N.; Guyatt, G.H. Completing ‘Summary of Findings’ Tables and Grading the Certainty of the Evidence. In Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Hoboken, NJ, USA, 2019; pp. 375–402. [Google Scholar]
- Review Manager (RevMan), Version 5.4; The Cochrane Collaboration, 2020. Available online: https://revman.cochrane.org (accessed on 15 November 2023).
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Hoboken, NJ, USA, 2019; ISBN 9781119536628. [Google Scholar]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. A Basic Introduction to Fixed-Effect and Random-Effects Models for Meta-Analysis. Res. Synth. Methods 2010, 1, 97–111. [Google Scholar] [CrossRef]
- The Jamovi Project. Jamovi, Version 2.3. 2023. Available online: https://www.jamovi.org (accessed on 15 November 2023).
- Serrano-Guzmán, M.; Valenza-Peña, C.M.; Serrano-Guzmán, C.; Aguilar-Ferrándiz, E.; Valenza-Demet, G.; Villaverde-Gutiérrez, C. Efectos de Un Programa de Terapia de Baile En La Calidad de Vida, El Sueño y La Presión Arterial En Mujeres de Mediana Edad: Un Ensayo Controlado Aleatorizado. Med. Clin. 2016, 147, 334–339. [Google Scholar] [CrossRef]
- Bisbe, M.; Fuente-Vidal, A.; López, E.; Moreno, M.; Naya, M.; de Benetti, C.; Milà, R.; Bruna, O.; Boada, M.; Alegret, M. Comparative Cognitive Effects of Choreographed Exercise and Multimodal Physical Therapy in Older Adults with Amnestic Mild Cognitive Impairment: Randomized Clinical Trial. J. Alzheimer’s Dis. 2020, 73, 769–783. [Google Scholar] [CrossRef] [PubMed]
- Alves, H.V.D. Dancing and the Aging Brain: The Effects of a 4-Month Ballroom Dance Intervention on the Cognition of Healthy Older Adults; University of Illinois Urbana-Champaign: Champaign, IL, USA, 2013. [Google Scholar]
- Zhang, X.; Ni, X.; Chen, P. Study About the Effects of Different Fitness Sports on Cognitive Function and Emotion of the Aged. Cell Biochem. Biophys. 2014, 70, 1591–1596. [Google Scholar] [CrossRef] [PubMed]
- Ayari, S.; Abellard, A.; Sakrani, S.; Krinitskaia, A.; Grzelak, M.; Nader, R.B.; Gavarry, O. Comparison of Dance and Aerobic Exercise on Cognition and Neuropsychiatric Symptoms in Sedentary Older Adults with Cognitive Impairment. Eur. Geriatr. Med. 2023, 14, 1289–1299. [Google Scholar] [CrossRef] [PubMed]
- Hoyer, B.P.B.; Teodoro, V.J.R.; de Borges, S.M. A Influência da Dança do Ventre nos Sintomas Depressivos em Idosas da Comunidade. Rev. Kairós 2015, 18, 277–288. [Google Scholar]
- Castro, J.C.; Giani, T.S.; Ferreira, M.A.; Bastos, F.A.C.; Cruz, T.H.P.; Boechat, R.; Dantas, E.H.M. Depression in Inactive and Active Elderly Women Practitioners of Dance, Weight-Lifting or Meditation. Acta Med. Litu. 2009, 16, 52–57. [Google Scholar] [CrossRef]
- Chang, J.; Zhu, W.; Zhang, J.; Yong, L.; Yang, M.; Wang, J.; Yan, J. The Effect of Chinese Square Dance Exercise on Cognitive Function in Older Women with Mild Cognitive Impairment: The Mediating Effect of Mood Status and Quality of Life. Front. Psychiatry 2021, 12, 711079. [Google Scholar] [CrossRef]
- Eyigor, S.; Karapolat, H.; Durmaz, B.; Ibisoglu, U.; Cakir, S. A Randomized Controlled Trial of Turkish Folklore Dance on the Physical Performance, Balance, Depression and Quality of Life in Older Women. Arch. Gerontol. Geriatr. 2009, 48, 84–88. [Google Scholar] [CrossRef]
- Haboush, A.; Floyd, M.; Caron, J.; LaSota, M.; Alvarez, K. Ballroom Dance Lessons for Geriatric Depression: An Exploratory Study. Arts Psychother. 2006, 33, 89–97. [Google Scholar] [CrossRef]
- Lee, N.-Y.; Lee, D.-K.; Song, H.-S. Effect of Virtual Reality Dance Exercise on the Balance, Activities of Daily Living, and Depressive Disorder Status of Parkinson’s Disease Patients. J. Phys. Ther. Sci. 2015, 27, 145–147. [Google Scholar] [CrossRef]
- Michels, K.; Dubaz, O.; Hornthal, E.; Bega, D. “Dance Therapy” as a Psychotherapeutic Movement Intervention in Parkinson’s Disease. Complement. Ther. Med. 2018, 40, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Rios Romenets, S.; Anang, J.; Fereshtehnejad, S.-M.; Pelletier, A.; Postuma, R. Tango for Treatment of Motor and Non-Motor Manifestations in Parkinson’s Disease: A Randomized Control Study. Complement. Ther. Med. 2015, 23, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Solla, P.; Cugusi, L.; Bertoli, M.; Cereatti, A.; Della Croce, U.; Pani, D.; Fadda, L.; Cannas, A.; Marrosu, F.; Defazio, G.; et al. Sardinian Folk Dance for Individuals with Parkinson’s Disease: A Randomized Controlled Pilot Trial. J. Altern. Complement. Med. 2019, 25, 305–316. [Google Scholar] [CrossRef]
- Zhang, X.; van der Schans, C.P.; Liu, Y.; Krijnen, W.P.; Hobbelen, J.S.M. Efficacy of Dance Intervention for Improving Frailty Among Chinese Older Adults Living in the Community: A Randomized Controlled Trial. J. Aging Phys. Act. 2023, 31, 806–814. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Wu, H.; Qi, M.; Wang, S.; Zhang, Q.; Zhou, L.; Wang, S.; Wang, W.; Wu, T.; Xiao, M.; et al. Effects of a Specially Designed Aerobic Dance Routine on Mild Cognitive Impairment. Clin. Interv. Aging 2018, 13, 1691–1700. [Google Scholar] [CrossRef]
- Aguiñaga, S. Latinos Unique Scenario, Addressing Cognitive Impairment via Dance; University of Illinois: Chicago, IL, USA, 2016. [Google Scholar]
- Liu, X.; Shen, P.-L.; Tsai, Y.-S. Dance Intervention Effects on Physical Function in Healthy Older Adults: A Systematic Review and Meta-Analysis. Aging Clin. Exp. Res. 2021, 33, 253–263. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Soh, K.G.; Omar Dev, R.D. Effect of Latin Dance on Physical and Mental Health: A Systematic Review. BMC Public Health 2023, 23, 1332. [Google Scholar] [CrossRef]
- Tao, D.; Gao, Y.; Cole, A.; Baker, J.S.; Gu, Y.; Supriya, R.; Tong, T.K.; Hu, Q.; Awan-Scully, R. The Physiological and Psychological Benefits of Dance and Its Effects on Children and Adolescents: A Systematic Review. Front. Physiol. 2022, 13, 925958. [Google Scholar] [CrossRef]
- Fiske, A.; Wetherell, J.L.; Gatz, M. Depression in Older Adults. Annu. Rev. Clin. Psychol. 2009, 5, 363–389. [Google Scholar] [CrossRef]
- Soysal, P.; Veronese, N.; Thompson, T.; Kahl, K.G.; Fernandes, B.S.; Prina, A.M.; Solmi, M.; Schofield, P.; Koyanagi, A.; Tseng, P.-T.; et al. Relationship between Depression and Frailty in Older Adults: A Systematic Review and Meta-Analysis. Ageing Res. Rev. 2017, 36, 78–87. [Google Scholar] [CrossRef]
- de Oliveira, J.M.B.; Vera, I.; Lucchese, R.; Silva, G.C.; Tomé, E.M.; Elias, R.A. Aging, Mental Health, and Suicide. An Integrative Review. Rev. Bras. Geriatr. Gerontol. 2018, 21, 488–498. [Google Scholar] [CrossRef]
- Maier, A.; Riedel-Heller, S.G.; Pabst, A.; Luppa, M. Risk Factors and Protective Factors of Depression in Older People 65+. A Systematic Review. PLoS ONE 2021, 16, e0251326. [Google Scholar] [CrossRef] [PubMed]
- Fernández-López, R.; Riquelme-Gallego, B.; Bueno-Cavanillas, A.; Khan, K.S. Influence of Placebo Effect in Mental Disorders Research: A Systematic Review and Meta-analysis. Eur. J. Clin. Investig. 2022, 52, e13762. [Google Scholar] [CrossRef] [PubMed]
- Prange, S.; Klinger, H.; Laurencin, C.; Danaila, T.; Thobois, S. Depression in Patients with Parkinson’s Disease: Current Understanding of Its Neurobiology and Implications for Treatment. Drugs Aging 2022, 39, 417–439. [Google Scholar] [CrossRef] [PubMed]
- Bennett, C.G.; Fox, H.; McLain, M.; Medina-Pacheco, C. Impacts of Dance on Agitation and Anxiety among Persons Living with Dementia: An Integrative Review. Geriatr. Nurs. 2021, 42, 181–187. [Google Scholar] [CrossRef]
- Wu, F.; Zhang, J.; Yang, H.; Jiang, J. The Effect of Physical Exercise on the Elderly’s Anxiety: Based on Systematic Reviews and Meta-Analysis. Comput. Math. Methods Med. 2022, 2022, 4848290. [Google Scholar] [CrossRef]
- Lim, G.Y.; Tam, W.W.; Lu, Y.; Ho, C.S.; Zhang, M.W.; Ho, R.C. Prevalence of Depression in the Community from 30 Countries between 1994 and 2014. Sci. Rep. 2018, 8, 2861. [Google Scholar] [CrossRef]
- Soete, L.; Schneegans, S.; Eröcal, D.; Angathevar, B.; Rasiah, R. A World in Search of an Effective Growth Strategy. In UNESCO Science Report Towards 2030; UNESCO Publishing: Paris, France, 2015; pp. 20–55. [Google Scholar]
- Geidl, W.; Schlesinger, S.; Mino, E.; Miranda, L.; Pfeifer, K. Dose–Response Relationship between Physical Activity and Mortality in Adults with Noncommunicable Diseases: A Systematic Review and Meta-Analysis of Prospective Observational Studies. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 109. [Google Scholar] [CrossRef]
- Singh, B.; Olds, T.; Curtis, R.; Dumuid, D.; Virgara, R.; Watson, A.; Szeto, K.; O’Connor, E.; Ferguson, T.; Eglitis, E.; et al. Effectiveness of Physical Activity Interventions for Improving Depression, Anxiety and Distress: An Overview of Systematic Reviews. Br. J. Sports Med. 2023, 57, 1203–1209. [Google Scholar] [CrossRef]
- Rowley, N.; Mann, S.; Steele, J.; Horton, E.; Jimenez, A. The Effects of Exercise Referral Schemes in the United Kingdom in Those with Cardiovascular, Mental Health, and Musculoskeletal Disorders: A Preliminary Systematic Review. BMC Public Health 2018, 18, 949. [Google Scholar] [CrossRef]
- Pearce, M.; Garcia, L.; Abbas, A.; Strain, T.; Schuch, F.B.; Golubic, R.; Kelly, P.; Khan, S.; Utukuri, M.; Laird, Y.; et al. Association Between Physical Activity and Risk of Depression. JAMA Psychiatry 2022, 79, 550. [Google Scholar] [CrossRef] [PubMed]
- Vlašić, J.; Oreb, G.; Katović, D. Dance Attitude Differences between Female and Male Students. Sci. Mov. Health 2012, 12. [Google Scholar]
- Addis, M.E.; Mahalik, J.R. Men, Masculinity, and the Contexts of Help Seeking. Am. Psychol. 2003, 58, 5–14. [Google Scholar] [CrossRef]
- Sánchez-Alcalá, M.; Aibar-Almazán, A.; Afanador-Restrepo, D.F.; del Carcelén-Fraile, M.C.; Achalandabaso-Ochoa, A.; Castellote-Caballero, Y.; Hita-Contreras, F. The Impact of Rhythmic Physical Activity on Mental Health and Quality of Life in Older Adults with and without Cognitive Impairment: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 7084. [Google Scholar] [CrossRef]
- Huang, C.; Yan, Y.; Luo, Y.; Lin, R.; Li, H. Effects of Dance Therapy on Cognitive and Mental Health in Adults Aged 55 Years and Older with Mild Cognitive Impairment: A Systematic Review and Meta-Analysis. BMC Geriatr. 2023, 23, 695. [Google Scholar] [CrossRef]
- Liu, C.; Su, M.; Jiao, Y.; Ji, Y.; Zhu, S. Effects of Dance Interventions on Cognition, Psycho-Behavioral Symptoms, Motor Functions, and Quality of Life in Older Adult Patients with Mild Cognitive Impairment: A Meta-Analysis and Systematic Review. Front. Aging Neurosci. 2021, 13. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prudente, T.P.; Mezaiko, E.; Silveira, E.A.; Nogueira, T.E. Effect of Dancing Interventions on Depression and Anxiety Symptoms in Older Adults: A Systematic Review and Meta-Analysis. Behav. Sci. 2024, 14, 43. https://doi.org/10.3390/bs14010043
Prudente TP, Mezaiko E, Silveira EA, Nogueira TE. Effect of Dancing Interventions on Depression and Anxiety Symptoms in Older Adults: A Systematic Review and Meta-Analysis. Behavioral Sciences. 2024; 14(1):43. https://doi.org/10.3390/bs14010043
Chicago/Turabian StylePrudente, Tiago Paiva, Eleazar Mezaiko, Erika Aparecida Silveira, and Túlio Eduardo Nogueira. 2024. "Effect of Dancing Interventions on Depression and Anxiety Symptoms in Older Adults: A Systematic Review and Meta-Analysis" Behavioral Sciences 14, no. 1: 43. https://doi.org/10.3390/bs14010043
APA StylePrudente, T. P., Mezaiko, E., Silveira, E. A., & Nogueira, T. E. (2024). Effect of Dancing Interventions on Depression and Anxiety Symptoms in Older Adults: A Systematic Review and Meta-Analysis. Behavioral Sciences, 14(1), 43. https://doi.org/10.3390/bs14010043






