Biological Macromolecule-Based Dressings for Combat Wounds: From Collagen to Growth Factors—A Review
Abstract
1. Introduction
2. Battlefield Wounds—Classification and Associated Challenges
3. Wound Healing Dressings Incorporating Bioactive Compounds—Characterization and Benefits
3.1. Hemostatic Materials in Wound Dressings—Characteristics, Benefits, and Limitations
3.1.1. Hemostatic Dressing Efficacy in Animal Models of Wound Healing—An Overview
3.1.2. Hemostatic Dressing Specifically Approved and Used in Battlefield Injuries and Austere Settings
QuikClot® Combat Gauze and Celox™
Axiostat Z-fold Hemostatic Gauze
Rev Medx’s xSTAT Hemostatic Agent
3.2. Next-Generation Multifunctional Wound Dressings That Offer Added Benefits
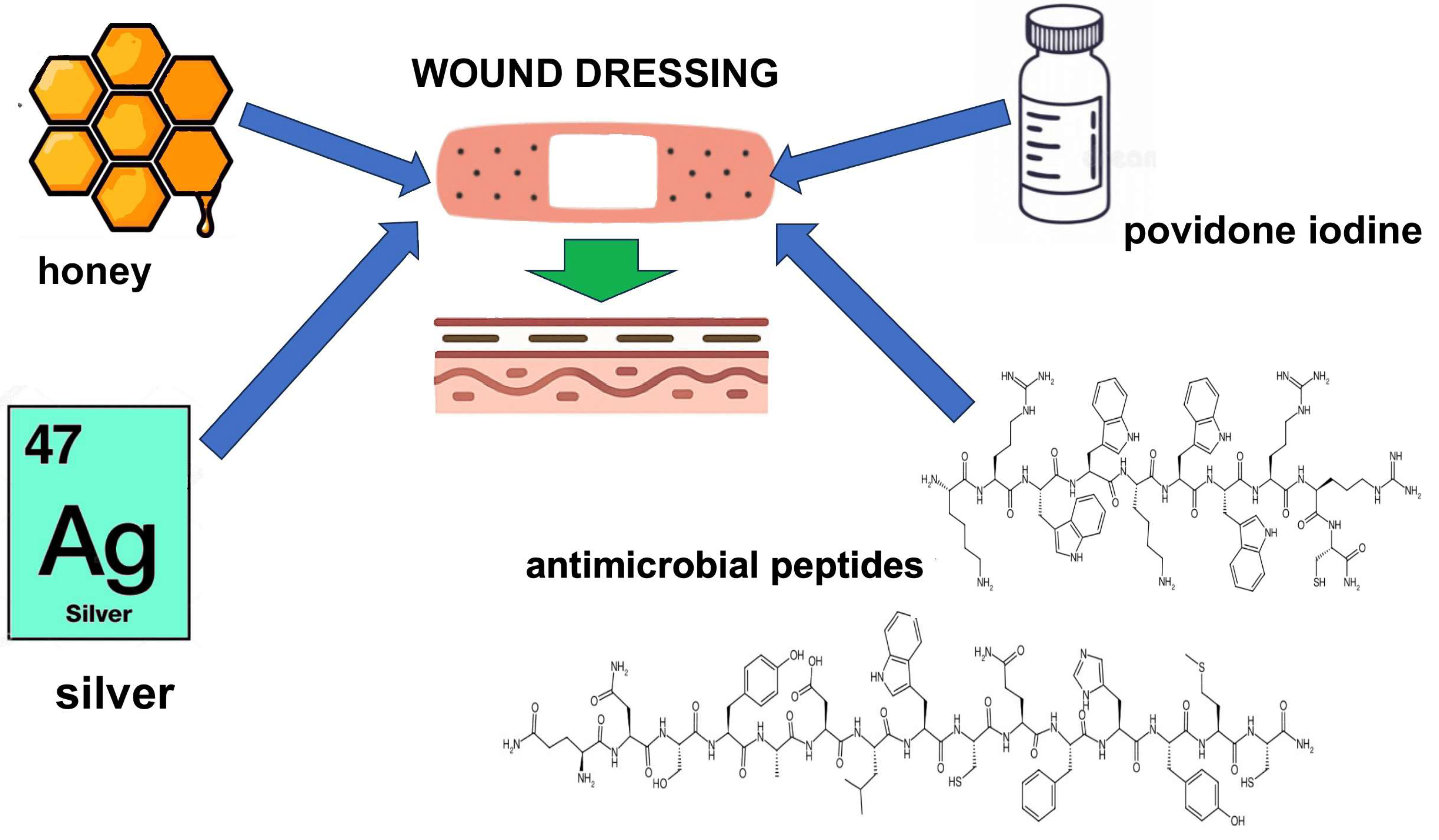
3.2.1. Wound Dressings with Antimicrobial Agents
3.2.2. Wound Dressings with Pain-Relieving Agents
3.2.3. Wound Dressings Containing Biological Factors
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pollock, P.J.; Schumacher, J. Principles of wound management. In Equine Medicine, Surgery and Reproduction, 2nd ed; Mair, T.S., Love, S., Schumacher, J., Smith, R.K.W., Frazer, G., Eds.; Saunders Ltd.: Uckfield, UK, 2012; pp. 469–487. [Google Scholar]
- Tabriz, A.G.; Douroumis, D. Recent advances in 3D printing for wound healing: A systematic review. J. Drug Deliv. Sci. Technol. 2022, 74, 103564. [Google Scholar] [CrossRef]
- Cooper, G.J.; Ryan, J.M. Interaction of penetrating missiles with tissues: Some common misapprehensions and implications for wound management. Br. J. Surg. 1990, 77, 606–610. [Google Scholar] [CrossRef]
- Boateng, J.S.; Matthews, K.H.; Stevens, H.N.; Eccleston, G.M. Wound healing dressings and drug delivery systems: A review. J. Pharm. Sci. 2008, 97, 2892–2923. [Google Scholar] [CrossRef] [PubMed]
- Chehade, M.; Granick, M. Surgical Wound Management; Informa: New York, NY, USA, 2007. [Google Scholar]
- Pinto, A.; Russo, A.; Reginelli, A.; Iacobellis, F.; Di Serafino, M.; Giovine, S.; Romano, L. Gunshot wounds: Ballistics and imaging Findings. Semin. Ultrasound CT MRI 2019, 40, 25–35. [Google Scholar] [CrossRef]
- Horrocks, C. Blast injuries: Biophysics, pathophysiology and management principles. J. R. Army Med. Corps 2000, 147, 28–40. [Google Scholar] [CrossRef]
- Zong, Z.; Zhang, L.Y.; Qin, H.; Chen, S.X.; Zhang, L.; Yang, L.; Li, X.X.; Bao, Q.W.; Liu, D.C.; He, S.H.; et al. Professional Committee and Youth Committee on Disaster Medicine. Expert consensus on the evaluation and diagnosis of combat injuries of the Chinese People’s Liberation Army. Mil. Med. Res. 2018, 5, 6. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://medcoeckapwstorprd01.blob.core.usgovcloudapi.net/pfw-images/dbimages/Ch%201.pdf (accessed on 14 May 2025).
- Kang, D.G.; Lehman, R.A., Jr.; Carragee, E.J. Wartime spine injuries: Understanding the improvised explosive device and biophysics of blast trauma. Spine J. 2012, 12, 849–857. [Google Scholar] [CrossRef]
- Available online: https://shop.icrc.org/classification-croix-rouge-des-plaies-perforantes-pdf-en.html (accessed on 13 May 2025).
- Bartoszewicz, M. Infection and treatment of chronic wounds. Lek. POZ 2017, 3, 37–41. [Google Scholar]
- Giannou, C.; Baldan, M. War Surgery: Working with Limited Resources in Armed Conflict and Other Situations of Violence Volume 1; International Committee of the Red Cross: Geneva, Switzerland, 2020; pp. 211–228. [Google Scholar]
- Jacob, E.; Settcrstrom, J.A. Infections in war wounds—Experience in recent military conflicts and future considerations. Mil. Med. 1989, 154, 311–315. [Google Scholar] [CrossRef] [PubMed]
- Dougherty, A.L.; Mohrie, C.R.; Galarneau, M.R.; Woodruff, S.I.; Dye, J.L.; Kimberly, H.Q. Battlefield extremity injuries in Operation Iraqi Freedom. Injury 2009, 40, 772–777. [Google Scholar] [CrossRef]
- Ursone, R.L. Unique complications of foot and ankle injuries secondary to warfare. Foot Ankle Clin. 2010, 15, 201–208. [Google Scholar] [CrossRef]
- Thomas, S. Hydrocolloid dressings in the management of acute wounds: A review of the literature. Int. Wound J. 2008, 5, 602–613. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.woundsource.com/sites/default/files/whitepapers/types_of_wound_dressings_-_features_indications_and_contraindications.pdf (accessed on 13 May 2025).
- Yoon, H.S.; Na, Y.C.; Choi, K.H.; Huh, W.H.; Kim, J.M. Wound healing effect of regenerated oxidized cellulose versus fibrin sealant patch: An in vivo study. Arch. Craniofac. Surg. 2019, 20, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Xu, C.; Li, G.; Liu, T.; Liang, J.F.; Wang, X. Graphene-kaolin composite sponge for rapid and riskless hemostasis. Colloids Surf. B Biointerfaces 2018, 169, 168–175. [Google Scholar] [CrossRef]
- Li, G.; Quan, K.; Xu, C.C.; Deng, B.; Wang, X. Synergy in thrombin-graphene sponge for improved hemostatic efficacy and facile utilization. Colloids Surf. B Biointerfaces 2018, 161, 27–34. [Google Scholar] [CrossRef]
- Yu, P.; Zhong, W. Hemostatic materials in wound care. Burns Trauma 2021, 9, tkab019. [Google Scholar] [CrossRef]
- Rothwell, S.W.; Settle, T.; Wallace, S.; Dorsey, J.; Simpson, D.; Bowman, J.R.; Janmey, P.; Saweyr, E. The long term immunological response of swine after two exposures to a salmon thrombin and fibrinogen hemostatic bandage. Biologicals 2010, 38, 619–628. [Google Scholar] [CrossRef]
- Tanaka, M.; Koyama, Y.; Nomura, Y. Effects of collagen peptide ingestion on UV-B-induced skin damage. Biosci. Biotechnol. Biochem. 2009, 73, 930–932. [Google Scholar] [CrossRef]
- Mathew-Steiner, S.S.; Roy, S.; Sen, C.K. Collagen in wound healing. Bioengineering 2021, 8, 63. [Google Scholar] [CrossRef]
- Diller, R.B.; Tabor, A.J. The role of the extracellular matrix (ECM) in wound healing: A review. Biomimetics 2022, 7, 87. [Google Scholar] [CrossRef] [PubMed]
- Gurtner, G.C.; Werner, S.; Barrandon, Y.; Longaker, M.T. Wound repair and regeneration. Nature 2008, 453, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Yang, P.; Zhou, C.; Li, S.; Hong, P. Marine collagen peptides from the skin of Nile tilapia (Oreochromis niloticus): Characterization and wound healing evaluation. Mar. Drugs 2017, 15, 102. [Google Scholar] [CrossRef] [PubMed]
- Xue, M.; Jackson, C.J. Extracellular matrix reorganization during wound healing and its impact on abnormal scarring. Adv. Wound Care 2015, 4, 119–136. [Google Scholar] [CrossRef] [PubMed]
- Al-Amer, O.M. The role of thrombin in haemostasis. Blood Coagul. Fibrinolysis 2022, 33, 145–148. [Google Scholar] [CrossRef]
- De Candia, E. Mechanisms of platelet activation by thrombin: A short history. Thromb. Res. 2012, 129, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Lisman, T.; Weeterings, C.; de Groot, P.G. Platelet aggregation: Involvement of thrombin and fibrin(ogen). Front. Biosci. 2005, 10, 2504–2517. [Google Scholar] [CrossRef]
- Larsen, J.B.; Hvas, A.M. Thrombin: A pivotal player in hemostasis and beyond. Semin. Thromb. Hemost. 2021, 47, 759–774. [Google Scholar] [CrossRef]
- Strukova, S.M. Thrombin as a regulator of inflammation and reparative processes in tissues. Biochemistry 2001, 66, 8–18. [Google Scholar] [CrossRef]
- Jesty, J. The kinetics of inhibition of alpha-thrombin in human plasma. J. Biol. Chem. 1986, 261, 10313–10318. [Google Scholar] [CrossRef] [PubMed]
- Awad, M.E.; López-Galindo, A.; Setti, M.; El-Rahmany, M.M.; Iborra, C.V. Kaolinite in pharmaceutics and biomedicine. Int. J. Pharm. 2017, 533, 34–48. [Google Scholar] [CrossRef]
- Margolis, J. The kaolin clotting time; a rapid one-stage method for diagnosis of coagulation defects. J. Clin. Pathol. 1958, 11, 406–409. [Google Scholar] [CrossRef]
- Liu, T.; Zhang, Z.; Liu, J.; Dong, P.; Tian, F.; Li, F.; Meng, X. Electrospun kaolin-loaded chitosan/PEO nanofibers for rapid hemostasis and accelerated wound healing. Int. J. Biol. Macromol. 2022, 217, 998–1011. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Liang, Y.; He, J.; Zhang, H.; Guo, B. Two-Pronged strategy of biomechanically active and biochemically multifunctional hydrogel wound dressing to accelerate wound closure and wound healing. Chem. Mater. 2020, 32, 9937–9953. [Google Scholar] [CrossRef]
- Syafruddin, I.R.; Putra, A.; Hidayat, M.S. Comparison between surfactant and chitosan organo-kaolin adsorbents to remove metal and organic compound in peat water. IOP Conf. Ser. Mater. Sci. Eng. 2019, 536, 012080. [Google Scholar] [CrossRef]
- Feng, P.; Luo, Y.; Ke, C.; Qiu, H.; Wei, W.; Zhu, Y.; Hou, R.; Xu, L.; Wu, S. Chitosan-based functional materials for skinn wound repair: Mechanisms and applications. Front. Bioeng. Biotechnol. 2021, 9, 650598. [Google Scholar] [CrossRef]
- Mohan, K.; Ganesan, A.R.; Muralisankar, T.; Jayakumar, R.; Sathishkumar, P.; Uthayakumar, V.; Chandirasekar, R.; Revathi, N. Recent insights into the extraction, characterization, and bioactivities of chitin and chitosan from insects. Trends Food Sci. Technol. 2020, 105, 17–42. [Google Scholar] [CrossRef]
- Arnaud, F.; Tomori, T.; Carr, W.; McKeague, A.; Teranishi, K.; Prusaczyk, K.; McCarron, R. Exothermic reaction in zeolite hemostatic dressings: QuikClot ACS and ACS+. Ann. Biomed. Eng. 2008, 36, 1708–1713. [Google Scholar] [CrossRef]
- Trabattoni, D.; Gatto, P.; Bartorelli, A.L. A new kaolin-based hemostatic bandage use after coronary diagnostic and interventional procedures. Int. J. Cardiol. 2012, 156, 53–54. [Google Scholar] [CrossRef] [PubMed]
- Kondapalli, S.S.; Czyz, C.N.; Stacey, A.W.; Cahill, K.V.; Foster, J.A. Use of kaolin-impregnated gauze for improvement of intraoperative hemostasis and postoperative wound healing in blepharoplasty. J. Clin. Aesthet. Dermatol. 2016, 9, 51–55. [Google Scholar] [PubMed] [PubMed Central]
- Sluka, K.A.; Bailey, K.; Bogush, J.; Olson, R.; Ricketts, A. Treatment with either high or low frequency TENS reduces the secondary hyperalgesia observed after injection of kaolin and carrageenan into the knee joint. Pain 1998, 77, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Fujiyoshi, T.; Hayashi, I.; Ohishi, S.; Kuwashima, M.; Iida, H.; Dozen, M.; Taniguchi, N.; Ikeda, K.; Ohnishi, H. Kaolin-induced writhing in mice, a new model of possible bradykinin-induced pain for assessment of analgesic agents. Agents Actions 1989, 27, 332–334. [Google Scholar] [CrossRef]
- Mabry, R.L.; Holcomb, J.B.; Baker, A.M.; Cloonan, C.C.; Uhorchak, J.M.; Perkins, D.E.; Canfield, A.J.; Hagmann, J.H. United States Army Rangers in Somalia: An analysis of combat casualties on an urban battlefield. J. Trauma 2000, 49, 515–529. [Google Scholar] [CrossRef]
- Alam, H.B.; Uy, G.B.; Miller, D.; Koustova, E.; Hancock, T.; Inocencio, R.; Anderson, D.; Llorente, O.; Rhee, P. Comparative analysis of hemostatic agents in a swine model of lethal groin injury. J. Trauma 2003, 54, 1077–1082. [Google Scholar] [CrossRef]
- Chan, M.W.; Schwaitzberg, S.D.; Demcheva, M.; Vournakis, J.; Finkielsztein, S.; Connolly, R.J. Comparison of poly-N-acetylglucosamine with absorbable collagen and fibrin sealant for achieving hemostasis in a swine model of splenic hemorrhage. J. Trauma 2000, 48, 454–458. [Google Scholar] [CrossRef]
- Pusateri, A.E.; Modrow, H.E.; Harris, R.A.; Holcomb, J.B.; Hess, J.R.; Mosebar, R.H.; Reid, T.J.; Nelson, J.H.; Goodwin, C.W., Jr.; Fitzpatrick, G.M.; et al. Advanced hemostatic dressing development program: Animal model selection criteria and results of a study of nine hemostatic dressings in a model of severe large venous hemorrhage and hepatic injury in swine. J. Trauma 2003, 55, 518–526. [Google Scholar] [CrossRef]
- Watters, J.M.; Van, P.Y.; Hamilton, G.J.; Sambasivan, C.; Differding, J.A.; Schreiber, M.A. Advanced hemostatic dressing are not superior to gauze for care under fire scenario. J. Trauma 2011, 70, 1413–1419. [Google Scholar] [CrossRef] [PubMed]
- Elliot, S.; Wikramanayake, T.C.; Jozic, I.; Tomic-Canic, M. A modeling conundrum: Murine models for cutaneous wound healing. J. Invesetig. Dermatol. 2018, 138, 736–740. [Google Scholar] [CrossRef]
- Lux, C.N. Wound healing in animals: A review of physiology and clinical evaluation. Vet. Dermatol. 2022, 33, 91-e27. [Google Scholar] [CrossRef] [PubMed]
- Ansell, D.M.; Kloepper, J.E.; Thomason, H.A.; Paus, R.; Hardman, M.J. Exploring the “hair growth–wound healing connection”: Anagen phase promotes wound re-epithelialization. J. Investig. Dermatol. 2011, 131, 518–528. [Google Scholar] [CrossRef]
- Raccuia, J.S.; Simonian, G.; Dardik, M.; Hallac, D.; Raccuia, S.V.; Stahl, R.; Dardik, H. Comparative efficacy of topical hemostatic agents in a rat kidney model. Am. J. Surg. 1992, 163, 234–238. [Google Scholar] [CrossRef] [PubMed]
- Laurens, N.; Koolwijk, P.; de Maat, M.P. Fibrin structure and wound healing. J. Thromb. Haemost. 2006, 4, 932–939. [Google Scholar] [CrossRef]
- Ulrich, D.; Smeets, R.; Unglaub, F.; Wöltje, M.; Pallua, N. Effect of oxidized regenerated cellulose/collagen matrix on proteases in wound exudate of patients with chronic venous ulceration. Int. Wound. J. 2008, 5, 195–203. [Google Scholar] [CrossRef]
- Liu, S.-A.; Cheng, C.-C.; Chen, J.-S.; Hung, Y.-W.; Chen, F.-J.; Chiu, Y.-T. Effect of oxidized regenerated cellulose on the healing of pharyngeal wound: An experimental animal study. J. Chin. Med. Assoc. 2012, 75, 176–182. [Google Scholar] [CrossRef]
- Ezer, M.; Doğantekin, E.; Çaydere, M.; Koç, A.; Öktem, C.; Hücümenoğlu, S. The impact of absorbable hemostatic agents on wound healing in an experimental penile fracture rat model. BMC Urol. 2025, 25, 13. [Google Scholar] [CrossRef] [PubMed]
- Ouanes, Y.; Saadi, M.H.; Alouene, H.H.; Bibi, M.; Sellami, A.; Rhouma, S.B.; Nouira, Y. Sexual function outcomes after surgical treatment of penile fracture. Sex Med. 2021, 9, 100353. [Google Scholar] [CrossRef]
- Cervini-Silva, J.; Ramírez-Apan, M.T.; Kaufhold, S.; Ufer, K.; Palacios, E.; Montoya, A. Role of bentonite clays on cell growth. Chemosphere 2016, 149, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Suh, H.N.; Choi, K.Y.; Song, C.W.; Hwang, J.H. Regenerative and anti-inflammatory effect of a novel bentonite complex on burn wounds. Vet. Med. Sci. 2022, 8, 2422–2433. [Google Scholar] [CrossRef]
- Khoshmohabat, H.; Dalfardi, B.; Dehghanian, A.; Rasouli, H.R.; Mortazavi, S.M.J.; Paydar, S. The effect of CoolClot hemostatic agent on skin wound healing in rats. J. Surg. Res. 2016, 200, 732–737. [Google Scholar] [CrossRef]
- Albahri, G.; Badran, A.; Hijazi, A.; Daou, A.; Baydoun, E.; Nasser, M.; Merah, O. The therapeutic wound healing bioactivities of various medicinal plants. Life 2023, 13, 317. [Google Scholar] [CrossRef]
- Garcia-Orue, I.; Gainza, G.; Gutierrez, F.B.; Aguirre, J.J.; Evora, C.; Pedraz, J.L.; Hernandez, R.M.; Delgado, A.; Igartua, M. Novel nanofibrous dressings containing rhEGF and Aloe vera for wound healing applications. Int. J. Pharm. 2017, 523, 556–566. [Google Scholar] [CrossRef]
- Ezzat, S.M.; Choucry, M.A.; Kandil, Z.A. Antibacterial, antioxidant, and topical anti-inflammatory activities of Bergia ammannioides: A wound-healing plant. Pharmaceutic. Biol. 2016, 54, 215–224. [Google Scholar] [CrossRef] [PubMed]
- Shedoeva, A.; Leavesley, D.; Upton, Z.; Fan, C. Wound healing and the use of medicinal plants. Evid. Based Complement. Alternat. Med. 2019, 2019, 2684108. [Google Scholar] [CrossRef]
- Wong, M.W.; Leung, P.C.; Wong, W.C. Limb salvage in extensive diabetic foot ulceration-a preliminary clinical study using simple debridement and herbal drinks. Hong Kong Med. J. 2001, 7, 403–407. [Google Scholar] [PubMed]
- Kim, H.; Kawazoe, T.; Han, D.W.; Matsumara, K.; Suzuki, S.; Tsutsumi, S.; Hyon, S.H. Enhanced wound healing by an epigallocatechin gallate-incorporated collagen sponge in diabetic mice. Wound Repair Regen. 2008, 16, 714–720. [Google Scholar] [CrossRef]
- Zouari Bouassida, K.; Bardaa, S.; Khimiri, M.; Rebaii, T.; Tounsi, S.; Jlaiel, L.; Trigui, M. Exploring the Urtica dioica leaves hemostatic and wound-healing potential. Biomed. Res. Int. 2017, 2017, 1047523. [Google Scholar] [CrossRef]
- Sutar, T.; Bangde, P.; Dandekar, P.; Adivarekar, R. Herbal hemostatic biopolymeric dressings of alginate/pectin coated with Croton oblongifolius extract. Carbohyd. Polym. Technol. Appl. 2021, 2, 100025. [Google Scholar] [CrossRef]
- Pandit, A.P.; Koyate, K.R.; Kedar, A.S.; Mute, V.M. Spongy wound dressing of pectin/carboxymethyl tamarind seed polysaccharide loaded with moxifloxacin beads for effective wound heal. Int. J. Biol. Macromol. 2019, 140, 1106–1115. [Google Scholar] [CrossRef]
- Rahmany, M.B.; Hantgan, R.R.; Van Dyke, M. A mechanistic investigation of the effect of keratin-based hemostatic agents on coagulation. Biomaterials 2013, 34, 2492–2500. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.; Amini-Nik, S. The role of phytochemicals in the inflammatory phase of wound healing. Int. J. Mol. Sci. 2017, 18, 1068. [Google Scholar] [CrossRef]
- Thida, M.; Nyein, C.M.; Chan, K.N.; Htet, Z.M.; Mya, K.M. Anti-oxidative and anti-inflammatory effects of Carissa spinarum L., Croton oblongifolius Roxb and Dioscorea bulbifera L., in LPS-induced RAW265.7 cell. J. Chem Pharm. Res. 2019, 11, 18–26. [Google Scholar]
- Urrutia-Hernández, T.A.; Santos-López, J.A.; Benedí, J.; Sánchez-Muniz, F.J.; Velázquez-González, C.; De la O-Arciniega, M.; Jaramillo-Morales, O.A.; Bautista, M. Antioxidant and hepatoprotective effects of croton hypoleucus extract in an induced-necrosis model in rats. Molecules 2019, 24, 2533. [Google Scholar] [CrossRef]
- Ozturk, O.; Ugur, M.; Guzel, Y.; Ozturk, M.A.; Gursoy, D.; Dogan, S.; Temiz, M. Hemostatic effecs of traditional Inula viscosa and Capsella bursa-pastoris plant mixture extract on rat liver parenchymal bleeding model. Ulus Taramva Acil. Cerrahi. Derg. 2022, 28, 1059–1065. [Google Scholar] [CrossRef]
- Şensoy, E.; Güneş, E.; Erdal, M.O. Determination of the effects of ankaferd wound dressing on the wound healing process in rats. Turk. J. Pharm. Sci. 2024, 21, 95–103. [Google Scholar] [CrossRef]
- Kurt, M.; Onal, I.; Akdogan, M.; Kekilli, M.; Arhan, M.; Sayilir, A.; Oztas, E.; Haznedaroglu, I. Ankaferd Blood Stopper for controlling gastrointestinal bleeding due to distinct benign lesions refractory to conventional antihemorrhagic measures. Can. J. Gastroenterol. 2010, 24, 380–384. [Google Scholar] [CrossRef] [PubMed]
- Goker, H.; Haznedaroglu, I.C.; Ercetin, S.; Kirazli, S.; Akman, U.; Oztruk; Firat, H.C. Haemostatic actions of the folkloric medicinal plant extract, Ankaferd Blood Stopper. J. Int. Med. Res. 2008, 36, 163–170. [Google Scholar] [CrossRef]
- Sezgin, S.Ö.; Saraç, G.; Şamdancı, E.; Şenol, M. The effects of Ankaferd, a hemostatic agent, on wound healing. Turkderm Turk Arch. Dermatol. Venereol. 2015, 49, 218–221. [Google Scholar] [CrossRef]
- Gülhan, P.Y.; Balbay, E.G.; Çelik, M.; Annakkaya, A.N.; Arbak, P. Fatigue frequency and related factors in patients with sarcoidosis. Turk. Thorac. J. 2019, 20 (Suppl. 1), 244. [Google Scholar] [CrossRef]
- Xie, Y.; Gao, P.; He, F.; Zhang, C. Application of alginate-based hydrogels in hemostasis. Gels 2022, 8, 109. [Google Scholar] [CrossRef]
- Atepileva, A.; Ogay, V.; Kudaibergen, G.; Kaukabaeva, G.; Nurkina; Mukhambetova, A.; Balgazarov, S.; Batpen, A.; Saginova; Ramazanov, Z.; et al. Exploring the antibacterial and regenerative properties of a two-stage alginate wound dressing in a rat model of purulent wounds. Biomedicines 2024, 12, 2122. [Google Scholar] [CrossRef] [PubMed]
- Ehterami, A.; Salehi, M.; Farzamfar, S.; Samadian, H.; Vaez, A.; Ghorbani, S.; Ai, J.; Sahrapeyma, H. Chitosan/alginate hydrogels containing alpha-tocopherol for wound healing in rat model. J. Drug Deliv. Sci. Technol. 2019, 51, 204–213. [Google Scholar] [CrossRef]
- Zhang, M.; Zhao, X. Alginate hydrogel dressings for advanced wound management. Int. J. Biol. Macromol. 2020, 162, 1414–1428. [Google Scholar] [CrossRef]
- Song, H.; Zhang, L.; Zhao, X. Hemostatic efficacy of biological self-assembling peptide nanofibers in a rat kidney model. Macromol. Biosci. 2010, 10, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Sun, X.S. Rational design of responsive self-assembling peptides from native protein sequences. Biomacromol. 2010, 11, 3390–3394. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.N.; Avery, R.K.; Vallmajo-Martin, Q.; Assmann, A.; Vegh, A.; Memic, A.; Olsen, B.D.; Annabi, N.; Khademhosseini, A. A highly elastic and rapidly crosslinkable elastin-like polypeptide-based hydrogel for biomedical applications. Adv. Funct. Mater. 2015, 25, 4814–4826. [Google Scholar] [CrossRef]
- Desai, M.S. Development of Diverse Hydrogels from the Protean Polimer, Elastin-Like Polypeptides. Available online: https://escholarship.org/content/qt3xn136g6/qt3xn136g6_noSplash_03f707a4846017c14217d3cd1273aff1.pdf (accessed on 3 June 2025).
- Desai, M.S.; Chen, M.; Hong, F.H.J.; Lee, J.H.; Wu, Y.; Lee, S.W. Catechol-functionalized elastin-like polypeptides as tissue adhesives. Biomacromolecules 2020, 21, 2938–2948. [Google Scholar] [CrossRef]
- Sharma; Sharma, P.; Roy, S. Elastin-inspired supramolecular hydrogels: A multifaceted extracellular matrix protein in biomedical engineering. Soft Matter 2021, 17, 3266–3290. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, L. Comparative evaluation of absorbable hemostats: Advantages of fibrin-based sheets. Biomaterials 2004, 25, 5557–5563. [Google Scholar] [CrossRef]
- Holcomb, J.B.; MacPhee, M.J.; Hetz, S.P.; Harris, R.; Pusateri, A.; Hess, J. Efficacy of a dry fibrin sealant dressing for hemorrhage control following ballistic injury. Arch. Surg. 1998, 113, 32–35. [Google Scholar] [CrossRef]
- Kim, J.O.; Park, J.K.; Kim, J.H.; Jin, S.G.; Yong, C.S.; Li, D.X.; Choi, J.Y.; Woo, J.S.; Yoo, B.K.; Lyoo, W.S.; et al. Development of polyvinyl alcohol-sodium alginate gel-matrix-based wound dressing system containing nitrofurazone. Int. J. Pharm. 2008, 359, 79–86. [Google Scholar] [CrossRef]
- Landers, G.D.; Townsend, C.; Gaspary, M.; Kachur, R.; Thorne, B.; Stuart, S.; Henao, J.; Zarow, G.J.; Natarajan, R.; Boboc, M. Efficacy of hemostatic gauzes in a swine model of prolonged field care with limb movement. Mil. Med. 2021, 186, 384–390. [Google Scholar] [CrossRef]
- Li, H.; Wang, L.; Alwaal, A.; Lee, Y.C.; Reed-Maldonado, A.; Spangler, T.A.; Banie, L.; O’Hara, R.B.; Lin, G. Comparison of topical hemostatic agents in a swine model of extremity arterial hemorrhage: BloodSTOP iV battle matrix vs. QuikClot combat gauze. Int. J. Mol. Sci. 2016, 17, 545. [Google Scholar] [CrossRef]
- Ekici, H.; Kumandaş, A.; Özbaykuş, A.C.; Dizdaroğlu, H.; Midi, A.; Balik, M.S.; Yeşilada, E. Investigation of the effectiveness of plant based algan hemostatic agent in a rat model of femoral arterial bleeding. Bezmialem Sci. 2022, 10, 88–95. [Google Scholar] [CrossRef]
- Obagi, Z.; Damiani, G.; Grada, A.; Falanga, V. Principles of wound dressings: A review. Surg. Technol. Int. 2019, 35, 50–57. [Google Scholar] [PubMed]
- Shingleton, S.; Folwell, J.; Jones, I.; Gleason, M.; Williams, A. Burn wound care strategies for the battlefield and austere settings. Eur. Burn J. 2024, 5, 49–65. [Google Scholar] [CrossRef]
- Cancio, L.C.; Barillo, D.J.; Kearns, R.D.; Holmes, J.H.T.; Conlon, K.M.; Matherly, A.F.; Cairns, B.A.; Hickerson, W.L.; Palmieri, T. Guidelines for burn care under austere conditions: Surgical and nonsurgical wound management. J. Burn Care Res. 2017, 38, 203–214. [Google Scholar] [CrossRef] [PubMed]
- Meng, F.C.; Lee, C.Y. Safety and efficiency of femoral artery access closure using QuikClot Combat Gauze in patients with severe arterial calcification of access sites. Quant. Imaging Med. Surg. 2013, 13, 282–292. [Google Scholar] [CrossRef]
- Johnson, D.; Bates, S.; Nukalo, S.; Staub, A.; Hines, A.; Leishman, T.; Michel, J.; Sikes, D.; Gegel, B.; Burgert, J. The effects of QuikClot Combat Gauze on hemorrhage control in the presence of hemodilution and hypothermia. Ann. Med. Surg. 2014, 3, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Khoshmohabat, H.; Paydar, S.; Kazemi, H.M.; Dalfardi, B. Overview of agents used for emergency hemostasis. Trauma Mon. 2016, 21, e26023. [Google Scholar] [CrossRef]
- Garcia-Blanco, J.; Gegel, B.; Burgert, J.; Johnson, S.; Johnson, D. The effects of movement on hemorrhage when QuikClot® Combat Gauze™ is used in a hypothermic hemodiluted porcine model. J. Spec. Oper. Med. 2015, 15, 57–60. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.K.; Kalns, J.; Wolf, E.A.; Traweek, F.; Schwarz, S.; Loeffler, C.K.; Snyder, W.; Yantis, L.D., Jr.; Eggers, J. Thermal injury resulting from application of a granular mineral hemostatic agent. J. Trauma 2004, 57, 224–230. [Google Scholar] [CrossRef]
- Rhee, P.; Brown, C.; Martin, M.; Salim, A.; Plurad, D.; Green, D.; Chambers, L.; Demetriades, D.; Velmahos, G.; Alam, H. QuikClot use in trauma for hemorrhage control: Case series of 103 documented uses. J. Trauma 2008, 64, 1093–1099. [Google Scholar] [CrossRef]
- Neuffer, M.C.; McDivitt, J.; Rose, D.; King, K.; Cloonan, C.C.; Vayer, J.S. Hemostatic dressings for the first responder: A review. Mil. Med. 2004, 169, 716–720. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kozen, B.G.; Kircher, S.J.; Henao, J.; Godinez, F.S.; Johnson, A.S. An alternative hemostatic dressing: Comparison of CELOX, HemCon, and QuikClot. Acad. Emerg. Med. 2008, 15, 74–81. [Google Scholar] [CrossRef]
- Hatamabadi, H.R.; Zarchi, A.F.; Kariman, H.; Dolatabadi, A.A.; Tabatabaey, A.; Amini, A. Celox-coated gauze for the treatment of civilian penetrating trauma: A randomized clinical trial. Trauma Mon. 2015, 20, e23862. [Google Scholar] [CrossRef]
- Available online: https://celoxmedical.com (accessed on 21 May 2025).
- Millner, R.W.; Lockhart, A.S.; Bird, H.; Alexiou, C. A new hemostatic agent: Initial life-saving experience with Celox (chitosan) in cardiothoracic surgery. Ann. Thorac. Surg. 2009, 87, e13-14. [Google Scholar] [CrossRef]
- Pozza, M.; Millner, R.W. Celox (chitosan) for haemostasis in massive traumatic bleeding: Experience in Afghanistan. Eur. J. Emerg. Med. 2011, 18, 31–33. [Google Scholar] [CrossRef]
- Littlejohn, L.F.; Devlin, J.J.; Kircher, S.S.; Lueken, R.; Melia, M.R.; Johnson, A.S. Comparison of Celox-A, ChitoFlex, WoundStat, and combat gauze hemostatic agents versus standard gauze dressing in control of hemorrhage in a swine model of penetrating trauma. Acad. Emerg. Med. 2011, 18, 340–350. [Google Scholar] [CrossRef]
- Perri, P.; Curcio, F.; De Luca, M.; Piro, P.; Trombino, S.; Cassano, R. Endovascular procedures in patients with leriche syndrome on anticoagulant therapy. Pharmaceuticals 2025, 18, 584. [Google Scholar] [CrossRef] [PubMed]
- Cao, S.; Xu, G.; Li, Q.; Zhang, S.; Yang, Y.; Chen, J. Double cross linking chitosan sponge with antibacterial and hemostatic properties for accelerating wound repair. Compos. Part B Eng. 2022, 234, 109746. [Google Scholar] [CrossRef]
- Ciarlantini, C.; Lacolla, E.; Francolini, I.; Fernández-García, M.; Muñoz-Núñez, C.; Muñoz-Bonilla, A.; Piozzi, A. Development of antioxidant and antimicrobial membranes based on functionalized and crosslinked chitosan for tissue regeneration. Int. J. Mol. Sci. 2024, 25, 1961. [Google Scholar] [CrossRef] [PubMed]
- Kabeer, M.; Venugopalan, P.P.; Subhash, V.C. Pre-hospital hemorrhagic control effectiveness of Axiostat® dressing versus conventional method in acute hemorrhage due to trauma. Cureus 2019, 11, e5527. [Google Scholar] [CrossRef]
- Available online: https://axiobio.com/axiostat/z-fold-haemostatic-gauze/ (accessed on 4 April 2025).
- Nakache, A.; Darmon, A.; Molho, A.; Steinecker, M.; Nejjari, M.; Digne, F. Evaluation of the safety and efficacy of the Axiostat® dressing device to achieve radial artery access hemostasis: The R3A study. Catheter. Cardiovasc. Interv. 2024, 104, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://woundclot.org/battlefield-tested-hemostatic-agents-their-applications-for-hemorrhage-control-in-hospital-settings/ (accessed on 4 April 2025).
- Allison, H.A. Hemorrhage control. Crit. Care Nurs. Q. 2019, 42, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.M.; Rall, J.M. Evaluation of XSTAT® and QuickClot® Combat Gauze® in a swine model of lethal junctional hemorrhage in coagulopathic swine. J. Spec. Oper. Med. 2017, 17, 64–67. [Google Scholar] [CrossRef]
- Pratt, G.A.; Kishman, A.J.; Glaser, J.J.; Castro, C.; Lorenzen, A.L.; Cardin, S.; Tiller, M.M.; McNeal, N.D.; Neidert, L.E.; Morgan, C.G. Evaluation of hemostatic devices in a randomized porcine model of junctional hemorrhage and 72-hour prolonged field care. J. Trauma Acute Care Surg. 2024, 96, 256–264. [Google Scholar] [CrossRef]
- Moradifar, F.; Sepahdoost, N.; Tavakoli, P.; Mirzapoor, A. Mutli-functional dressings for recovery and creenable treatment of wounds: A review. Heliyon 2025, 11, e41465. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Qu, H.; Wu, X.; Shi, J.; Wang, X. Rapid, sensitive, and user-friendly detection of Pseudomonas aeruginosa using the RPA/CRISPR/Cas12a system. BMC Infect. Dis. 2024, 24, 458. [Google Scholar] [CrossRef]
- Oogai, Y.; Matsuo, M.; Hashimoto, M.; Kato, F.; Sugai, M.; Komatsuzawa, H. Expression of virulence factors by Staphylococcus aureus grown in serum. Appl. Environ. Microbiol. 2011, 77, 8097–8105. [Google Scholar] [CrossRef]
- Qin, S.; Xiao, W.; Zhou, C.; Pu, Q.; Deng, X.; Lan, L.; Linag, H.; Sonbg; Wu, M. Pseudomonas aeruginosa: Pathogenesis, virulence factors, antibiotic resistance, interaction with host, technology advances and emerging therapeutics. Signal Transduct. Target Ther. 2022, 7, 199. [Google Scholar] [CrossRef]
- Liu, J.; Sonshine, D.A.; Shervani, S.; Hurt, R.H. Controlled release of biologically active silver from nanosilver surfaces. ACS Nano 2010, 4, 6903–6913. [Google Scholar] [CrossRef]
- Alexander, J.W. History of the medical use of silver. Surg. Infect. 2009, 10, 289–292. [Google Scholar] [CrossRef] [PubMed]
- Yildiz, T.; Durdu, S.; Ozcan, K.; Usta, K.M. Characterization and investigation of biological properties of silver nanoparticle-doped hydroxyapatite-based surfaces on zirconium. Sci. Rep. 2023, 13, 6773. [Google Scholar] [CrossRef]
- Mohamed, D.S.; El-Baky, R.M.A.; Sandle, T.; Mandour, S.A.; Ahmed, E.F. Antimicrobial activity of silver-treated bacteria against other multi-drug resistant pathogens in their environment. Antibiotics 2020, 9, 181. [Google Scholar] [CrossRef] [PubMed]
- Baghel, P.S.; Shukla, S.; Mathur, R.K.; Randa, R. A comparative study to evaluate the effect of honey dressing and silver sulfadiazene dressing on wound healing in burn patients. Indian J. Plast. Surg. 2009, 42, 176–181. [Google Scholar] [CrossRef]
- Mujalde, V.S.; Jalaj, A.; Pipariya, P.R. To assess the efficacy of honey in comparison with 1% silver sulfadiazine cream as a burn wound dressing in superficial and partial thickness of burns. Sch. J. Appl. Med. Sci. 2014, 2, 193–196. [Google Scholar] [CrossRef]
- Li, H.; Xu, H. Mechanisms of bacterial resistance to environmental silver and antimicrobial strategies for silver: A review. Environ. Res. 2024, 248, 118313. [Google Scholar] [CrossRef]
- Khansa, I.; Schoenbrunner, A.R.; Kraft, C.T.; Janis, J.E. Silver in wound care-friend or foe: A comprehensive review. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2390. [Google Scholar] [CrossRef]
- Poon, V.K.M.; Burd, A. In vitro cytotoxity of silver: Implication for clinical wound care. Burns 2004, 30, 140–147. [Google Scholar] [CrossRef]
- Aurora, A.; Beasy, A.; Rizzo, J.A.; Chung, K.K. The use of a silver-nylon dressing during evacuation of military burn casualties. J. Burn Care Res. 2018, 39, 593–597. [Google Scholar] [CrossRef] [PubMed]
- Pozza, M.; Matthew, P.; Lunardi, F. Experience in treating combat burns in Afghanistan by using silver-nylon dressing. J. Spec. Oper. Med. 2014, 14, 1–5. [Google Scholar] [CrossRef]
- Barillo, D.J.; Pozza, M.; Brandt, M.M. A literature review of the military uses of silver-nylon dressings with emphasis on wartime operations. Burns 2014, 40, S24–S29. [Google Scholar] [CrossRef]
- Cancio, L.C.; Horvath, E.E.; Barillo, D.J.; Kopchinski, B.J.; Charter, K.R.; Montalvo, A.E.; Buescher, T.M.; Brengman, M.L.; Brandt, M.M.; Holcomb, J.B. Burn support for Operation Iraqi Freedom and related operations, 2003–2004. J. Burn Care Rehab. 2005, 26, 151–161. [Google Scholar] [CrossRef]
- Available online: https://www.silverlon.com/silverlon-advantage/mrsa-kill-rate (accessed on 8 June 2025).
- Available online: https://l1enterprises.com/wp-content/uploads/2020/01/L1-Enterprises-Silverlon-Literature.pdf (accessed on 1 June 2025).
- Albrecht, M.C.; Renz, E.; Cancio, L.C.; White, C.E.; Blackbourne, L.H.; Chung, K.; Horvath, E.E.; Bielke, P.; Wolf, S.E.; Holcomb, J.B. Comparison of Silverlon Dressing to Xeroform Gauze in the Treatment of Skin Graft Donor Site Wounds. Available online: https://173839.fs1.hubspotusercontent-na1.net/hubfs/173839/Studies%20with%20Disclaimers/Comparison%20of%20Silverlon%20Dressing%20to%20Xeroform%20Gauze%20in%20the%20Treatment%20of%20Skin%20Graft%20Donor%20Site%20Wounds.pdf (accessed on 14 April 2025).
- Ressner, R.A.; Murray, C.K.; Griffith, M.E.; Rasnake, M.S.; Hospenthal, D.R.; Wolf, S.E. Outcomes of bacteremia in burn patients involved in combat operations overseas. J. Am. Coll. Surg. 2008, 206, 439–444. [Google Scholar] [CrossRef]
- Fries, C.A.; Ayalew, Y.; Penn-Barwell, J.G.; Porter, K.; Jeffery, S.L.A.; Midwinter, M.J. Prospective randomised controlled trial of nanocrystalline silver dressing versus plain gauze as the initial post-debridement management of military wounds on wound microbiology and healing. Injury 2014, 45, 1111–1116. [Google Scholar] [CrossRef] [PubMed]
- Drosou, A.; Falabella, A.; Kirsner, R.S. Antiseptics on wounds: An area of controversy. Wounds 2013, 15, 149–166. Available online: https://www.hmpgloballearningnetwork.com/site/wounds/article/1585 (accessed on 14 April 2025).
- Kapoor, N.; Yadav, R. Manuka honey: A promising wound dressing material for the chronic nonhealing discharging wounds: A retrospective study. Natl. J. Maxillofac. Surg. 2021, 12, 233–237. [Google Scholar] [CrossRef]
- Molan, P.C. Debridement of wounds with honey. J. Wound Technol. 2009, 5, 12–16. Available online: https://researchcommons.waikato.ac.nz/server/api/core/bitstreams/df7291ca-11aa-4011-9910-04c7f251df92/content (accessed on 1 June 2025).
- Haynes, J.S.; Callaghan, R. Properties of honey: Its mode of action and clinical outcomes. Wounds UK 2011, 7, 50–57. Available online: https://wounds-uk.com/wp-content/uploads/2023/02/content_9836.pdf (accessed on 14 April 2025).
- Guthrie, H.C.; Martin, K.R.; Taylor, C.; Spear, A.M.; Whiting, R.; Macildowie, S.; Clasper, J.C.; Watts, S.A. A pre-clinical evaluation of silver, iodine and Manuka honey based dressings in a model of traumatic extremity wounds contaminated with Staphylococcus aureus. Injury 2014, 45, 1171–1178. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, J.C. A povidone-iodine medicated dressing. J. Wound Care 1998, 7, 332–336. [Google Scholar] [CrossRef]
- Sibbald, R.G.; Elliott, J.A. The role of inadine in wound care: A consensus document. Int. Wound J. 2017, 14, 316–321. [Google Scholar] [CrossRef]
- Mandy, S.H. Evaluation of a new povidone-iodine-impregnated polyethylene oxide gel occlusive dressing. J. Am. Acad. Dermatol. 1985, 13, 655–659. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Chen, Z.; Su, F.; Zhang, T. Comparison of topical honey and povidone iodine-based dressings for wound healing: A systematic review and meta-analysis. J. Wound Care 2021, 30 (Suppl. 4), S28–S36. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Zhang, Q.; Wang, H.; Välimäki, M.; Zhou, Q.; Dai, W.; Guo, J. Effectiveness of silver and iodine dressings on wound healing: A systematic review and meta-analysis. BMJ Open 2024, 14, e077902. [Google Scholar] [CrossRef]
- Wilson, J.R.; Mills, J.G.; Prather, I.D.; Dimitrijevich, S.D. A toxicity index of skin and wound cleansers used on in vitro fibroblasts and keratinocytes. Adv. Skin Wound Care 2005, 18, 373–378. [Google Scholar] [CrossRef]
- Sood, A.; Granick, M.S.; Tomaselli, N.L. Wound dressings and comparative effectiveness data. Adv. Wound Care 2014, 3, 511–529. [Google Scholar] [CrossRef] [PubMed]
- Miao, F.; Li, Y.; Tai; Zhang, Y.; Gao, Y.; Hu, M.; Zhu, Q. Antimicrobial peptides: The promising therapeutics for cutaneous wound healing. Macromol. Biosci. 2021, 21, e2100103. [Google Scholar] [CrossRef]
- Chen, Y.; Qian, H.; Peng, D.; Jiang, Y.; Liu, Q.; Tan, Y.; Feng, L.; Cheng, B.; Li, G. Antimicrobial peptide-modified AIE visual composite wound dressing for promoting rapid healing of infected wounds. Front. Bioeng. Biotechnol. 2024, 11, 1338172. [Google Scholar] [CrossRef]
- Strömdahl, A.-C.; Ignatowicz, L.; Petruk, G.; Butrym, M.; Wasserstrom, S.; Schmidtchen, A.; Puthia, M. Peptide-coated polyurethane material reduces wound infection and inflammation. Acta Biomater. 2021, 128, 314–331. [Google Scholar] [CrossRef]
- Jia, Q.; Fu, Z.; Li, Y.; Kang, Z.; Wu, Y.; Ru, Z.; Peng, Y.; Huang, Y.; Lou, Y.; Li, W.; et al. Hydrogel loaded with peptide-containing nanocomplexes: Symphonic cooperation of photothermal antimicrobial nanoparticls and prohealing peptides for the treatment of infected wounds. ACS Appl. Mater. Interfaces 2024, 16, 13422–13438. [Google Scholar] [CrossRef]
- Wang, Y.; Feng, Z.; Yang, M.; Zeng, L.; Qi, B.; Yin, S.; Li, B.; Li, Y.; Fu, Z.; Shu, L.; et al. Discovery of a novel short peptide with efficacy in accelerating the healing of skin wounds. Pharmacol. Res. 2021, 163, 105296. [Google Scholar] [CrossRef]
- Price, P.E.; Fagervik-Morton, H.; Mudge, E.J.; Beele, H.; Ruiz, J.C.; Nystrøm, T.H.; Lindholm, C.; Maume, S.; Melby-Østergaard, B.; Peter, Y.; et al. Dressing-related pain in patients with chronic wounds: An international patient perspective. Int. Wound J. 2008, 5, 159–171. [Google Scholar] [CrossRef]
- Frescos, N. What causes wound pain. J. Foot Ankle Res. 2011, 4 (Suppl. 1), P22. [Google Scholar] [CrossRef]
- Niederauer, S.; Beeman, M.; Cleveland, A.; Wojtalewicz, S.; Erickson, S.; Reilly, C.A.; Rower, J.E.; Garrett, C.; Floyd, C.; Shea, J.; et al. A ropivacaine-eluting poly(lactide-co-caprolactone) wound dressing provided enhanced analgesia in partial-thickness porcine injuries. Plast. Reconstr. Surg. 2025, 155, 75e–85e. [Google Scholar] [CrossRef]
- Aycan, D.; Selmi, B.; Kelel, E.; Yildirim, T.; Alemdar, N. Conductive polymeric film loaded with ibuprofen as a wound dressing material. Eur. Polym. J. 2019, 121, 109308–109320. [Google Scholar] [CrossRef]
- Sibbald, R.G.; Coutts, P.; Fierheller, M.; Woo, K. A pilot (real-life) randomised clinical evaluation of a pain-relieving foam dressing: (ibuprofen-foam versus local best practice). Int. Wound J. 2007, 4 (Suppl. 1), 16–23. [Google Scholar] [CrossRef] [PubMed]
- Jørgensen, B.; Friis, G.J.; Gottrup, F. Pain and quality of life for patients with venous leg ulcers: Proof of concept of the efficacy of Biatain-Ibu, a new pain reducing wound dressing. Wound Repair Regen. 2006, 14, 233–239. [Google Scholar] [CrossRef]
- Gottrup, F.; Jørgensen, B.; Karlsmark, T.; Sibbald, R.G.; Rimdeika, R.; Harding, K.; Price, P.; Venning, V.; Vowden, P.; Jünger, M.; et al. Reducing wound pain in venous leg ulcers with Biatain Ibu: A randomized, controlled double-blind clinical investigation on the performance and safety. Wound Repair Regen. 2008, 16, 615–625. [Google Scholar] [CrossRef]
- Price, P.; Fogh, K.; Glynn, C.; Krasner, D.L.; Osterbrink, J.; Sibbald, R.G. Why combine a foam dressing with ibuprofen for wound pain and moist wound healing. Int. Wound J. 2007, 4 (Suppl. 1), 1. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.; Hamm, R.L. Factors that impair wound healing. J. Am. Coll. Clin. Wound Spec. 2014, 4, 84–91. [Google Scholar] [CrossRef]
- Costa, F.L.; Tiussi, L.D.; Nascimento, M.S.; Corrêa, A.C.; Yasojima, E.Y.; Pires, C.A. Diclofenac topical gel in excisional wounds maintains heal quality and reduces phlogistic signals. Acta Cir. Bras. 2014, 29, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Kowalski, G.; Zawadzki, M.; Leppert, W.; Szpot, P.; Siczek, M.; Słowiński, K.; Sobieszczańska, M.; Gawłowska, A.; Wieczorkowska-Tobis, K. Analgesic efficacy of sufentanil in dressings after surgical treatment of burn wounds. Burns 2021, 47, 880–887. [Google Scholar] [CrossRef] [PubMed]
- Binder, W.; Machelska, H.; Mousa, S.; Schmitt, T.; Riviere, P.J.; Junien, J.L.; Stein, S.; Schaefer, M. Analgesic and antiinflammatory effects of two novel kappa-opioid peptides. Anesthesiology 2021, 94, 1034–1044. [Google Scholar] [CrossRef]
- Shannon, H.E.; Lutz, E.A. Comparison of the peripheral and central effects of the opioid agonists loperamide and morphine in the formalin test in rats. Neuropharmacology 2002, 42, 253–261. [Google Scholar] [CrossRef]
- Tegeder; Meier, S.; Burian, M.; Schmidt, H.; Geisslinger, G.; Lotsch, J. Peripheral opioid analgesia in experimental human pain models. Brain 2003, 126, 1092–1102. [Google Scholar] [CrossRef]
- Stein, C. Targeting pain and inflammation by peripherally acting opioids. Front. Pharmacol. 2013, 4. [Google Scholar] [CrossRef] [PubMed]
- Kowalski, G.; Domagalska, M.; Słowiński, K.; Grochowicka, M.; Zawadzki, M.; Kropińska, S.; Leppert, W.; Wieczorkowska-Tobis, K. Morphine (10, 20 mg) in a postoperative dressing used with patients after surgical debridement of burn wounds: A prospective, double-blinded, randomized controlled trial. Adv. Wound Care 2023, 13, 115–122. [Google Scholar] [CrossRef]
- Lipkowski, A.W.; Konecka, A.M.; Sroczyńska, I. Double-enkephalins—Synthesis, activity on guinea-pig ileum, and analgesic effect. Peptides 1982, 3, 697–700. [Google Scholar] [CrossRef]
- Wang, Y.; Gupta, M.; Poonawala, T.; Farooqui, M.; Li, Y.; Peng, F.; Rao, S.; Ansonoff, M.; Pintar, J.E.; Gupta, K. Opioids and opioid receptors orchestrate wound repair. Transl. Res. 2017, 185, 13–23. [Google Scholar] [CrossRef]
- Ondrovics, M.; Hoelbl-Kovacic, A.; Fux, D.A. Opioids: Modulators of angiogenesis in wound healing and cancer. Oncotarget 2017, 8, 25783–25796. [Google Scholar] [CrossRef]
- Vang; Ericson, M.; Ansonoff, M.A.; Pintar, J.E.; Hebbel, R.P.; Gupta, K. Morphine stimulates wound healing via mu opioid receptor and promotes wound closure in sickle mice. Blood 2011, 118, 2118. [Google Scholar] [CrossRef]
- Konop, M.; Czuwara, J.; Kłodzińska, E.; Laskowska, A.K.; Zielenkiewicz, U.; Brzozowska, I.; Nabavi, S.M.; Rudnicka, L. Development of a novel keratin dressing which accelerates full-thickness skin wound healing in diabetic mice: In vitro and in vivo studies. J. Biomater. Appl. 2018, 33, 527–540. [Google Scholar] [CrossRef]
- Stallmeyer, B.; Kampfer, H.; Kolb, N.; Pfeilschifter, J.; Frank, S. The function of nitric oxide in wound repair: Inhibition of inducible nitric oxide-synthase severely impairs wound reepithelialization. J. Investig. Dermatol. 1999, 113, 1090–1098. [Google Scholar] [CrossRef]
- Zhao-Fleming, H.; Hand, A.; Zhang, K.; Polak, R.; Northcut, A.; Jacob, D.; Dissanaike, S.; Rumbaugh, K.P. Effect of non-steroidal anti-inflammatory drugs on post-surgical complications against the backdrop of the opioid crisis. Burns Trauma 2018, 13, 25. [Google Scholar] [CrossRef]
- ABryant, E.; Bayer, C.R.; Aldape, M.J.; Stevens, D.L. The roles of injury and nonsteroidal anti-inflammatory drugs in the development and outcomes of severe group A streptococcal soft tissue infections. Curr. Opin. Infect. Dis. 2015, 28, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.fda.gov/media/80384/download (accessed on 21 July 2025).
- Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/purpose-and-content-use-related-risk-analyses-drugs-biological-products-and-combination-products (accessed on 21 July 2025).
- Available online: https://www.exponent.com/article/fda-proposes-new-rule-reclassification-wound-dressings (accessed on 21 July 2025).
- Zarei, F.; Soleimaninejad, M. Role of growth factors and biomaterials in wound healing. Artif. Cells Nanomed. Biotechnol. 2018, 46 (Suppl. 1), 906–911. [Google Scholar] [CrossRef] [PubMed]
- Nissen, N.N.; Polverini, P.J.; Koch, A.E.; Volin, M.V.; Gamelli, R.L.; DiPietro, L.A. Vascular endothelial growth factor mediates angiogenic activity during the proliferative phase of wound healing. Am. J. Pathol. 1998, 152, 1445–1452. [Google Scholar] [PubMed] [PubMed Central]
- Bao, P.; Kodra, A.; Tomic-Canic, M.; Golinko, M.S.; Ehrlich, H.P.; Brem, H. The role of vascular endothelial growth factor in wound healing. J. Surg. Res. 2009, 153, 347–358. [Google Scholar] [CrossRef]
- Schultz, G.; Rotatori, D.S.; Clark, W. EGF and TGF-alpha in wound healing and repair. J. Cell Biochem. 1991, 45, 346–352. [Google Scholar] [CrossRef]
- Andrae, J.; Gallini, R.; Betsholtz, C. Role of platelet-derived growth factors in physiology and medicine. Genes Dev. 2008, 22, 1276–3112. [Google Scholar] [CrossRef]
- Mullin, J.A.; Rahmani, E.; Kiick, K.L.; Sullivan, M.O. Growth factors and growth factor gene therapies for treating chronic wounds. Bioeng. Transl. Med. 2023, 9, e10642. [Google Scholar] [CrossRef]
- Mitchell, A.C.; Briquez, P.S.; Hubbell, J.A.; Cochran, J.R. Engineering growth factors for regenerative medicine applications. Acta Biomater. 2016, 30, 1–12. [Google Scholar] [CrossRef]
- Embil, J.M.; Papp, K.; Sibbald, G.; Tousignant, J.; Smiell, J.M.; Wong, B.; Lau, C.Y. Recombinant human platelet-derived growth factor-BB (becaplermin) for healing chronic lower extremity diabetic ulcers: An open-label clinical evaluation of efficacy. Wound Repair Regen. 2000, 8, 162–168. [Google Scholar] [CrossRef]
- Steed, D.L. Clinical evaluation of recombinant human platelet-derived growth factor for the treatment of lower extremity diabetic ulcers. J. Vasc. Surg. 1995, 21, 71–81. [Google Scholar] [CrossRef]
- Chakrabarti, S.; Mazumder, B.; Rajkonwar, J.; Pathak, M.P.; Patowary, P.; Chattopadhyay, P. bFGF and collagen matrix hydrogel attenuates burn wound inflammation through activation of ERK and TRK pathway. Sci. Rep. 2021, 11, 3357. [Google Scholar] [CrossRef] [PubMed]
- Yun, Y.R.; Won, J.E.; Jeon, E.; Lee, S.; Kang, W.; Jo, H.; Jang, J.H.; Shin, U.S.; Kim, H.W. Fibroblast growth factors: Biology, function, and application for tissue regeneration. J. Tissue Eng. 2010, 2010, 218142. [Google Scholar] [CrossRef]
- Silva, A.K.A.; Richard, C.; Bessodes, M.; Scherman, D.; Merten, O.W. Growth factor delivery approaches in hydrogels. Biomacromolecules 2008, 10, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Barrientos, S.; Stojadinovic, O.; Golinko, M.S.; Brem, H.; Tomic-Canic, M. Growth factors and cytokines in wound healing. Wound Repair Regen. 2008, 16, 585–601. [Google Scholar] [CrossRef]
- Asiri, A.; Saidin, S.; Sani, M.H.; Al, R.H. Epidermal and fibroblast growth factors incorporated polyvinyl alcohol electrospun nanofibers as biological dressing scaffold. Sci. Rep. 2021, 11, 5634. [Google Scholar] [CrossRef]
- Yoshikawa, T.; Mitsuno, H.; Nonaka, I.; Sen, Y.; Kawanishi, K.; Inada, Y.; Takakura, Y.; Okuchi, K.; Nonomura, A. Wound therapy by marrow mesenchymal cell transplantation. Plast. Reconstr. Surg. 2008, 121, 860–877. [Google Scholar] [CrossRef] [PubMed]
- Buchtova, M.; Chaloupkova, R.; Zakrzewska, M.; Vesela, I.; Cela, P.; Barathova, J.; Gudernova, I.; Zajickova, R.; Trantirek, L.; Martin, J.; et al. Instability restricts signaling of multiple fibroblast growth factors. Cell. Mol. Life Sci. 2015, 72, 2445–2459. [Google Scholar] [CrossRef]
- Bradley, J.C.; Simoni, J.; Bradley, R.H.; McCartney, D.L.; Brown, S.M. Time- and temperature-dependent stability of growth factor peptides in human autologous serum eye drops. Cornea 2009, 28, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Gulbranson, D.R.; Yu, P.; Hou, Z.; Thomson, J.A. Thermal stability of fibroblast growth factor protein is a determinant factor in regulating self-renewal, differentiation, and reprogramming in human pluripotent stem cells. Stem Cells 2012, 30, 623–630. [Google Scholar] [CrossRef] [PubMed]
- Ejtehadifar, M.; Shamsasenjan, K.; Movassaghpour, A.; Akbarzadehlaleh, P.; Dehdilani, N.; Abbasi, P.; Molaeipour, Z.; Saleh, M. The effect of hypoxia on mesenchymal stem cell biology. Adv. Pharm. Bull. 2015, 5, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Nikolaev, N.I.; Liu, Y.; Hussein, H.; Williams, D.J. The sensitivity of human mesenchymal stem cells to vibration and cold storage conditions representative of cold transportation. J. R. Soc. Interface 2012, 9, 2503–2515. [Google Scholar] [CrossRef]
- Chen, W.; Lv, L.; Chen, N.; Cui, E. Immunogenicity of mesenchymal stromal/stem cells. Scand. J. Immunol. 2023, 97, e13267. [Google Scholar] [CrossRef]
- Mello, D.B.; Mesquita, F.C.P.; Santos, D.S.O.; Asensi, K.D.; Dias, M.L.; de Carvalho, A.C.C.; Goldenberg, R.C.D.S.; Kasai-Brunswick, T.H. Mesenchymal stromal cel-based products: Challenges and clinical therapeutic options. Int. J. Mol. Sci. 2024, 25, 6063. [Google Scholar] [CrossRef]
- Heathman, T.R.; Nienow, A.W.; McCall, M.J.; Coopman, K.; Kara, B.; Hewitt, C.J. The translation of cell-based therapies: Clinical landscape and manufacturing challenges. Regen. Med. 2015, 10, 49–64. [Google Scholar] [CrossRef]
- Available online: https://www.ema.europa.eu/en/human-regulatory-overview/marketing-authorisation/advanced-therapies-marketing-authorisation/scientific-recommendations-classification-advanced-therapy-medicinal-products (accessed on 21 July 2025).
- Available online: https://eur-lex.europa.eu/eli/reg/2007/1394/oj/eng (accessed on 21 July 2025).


| Wound Classification | Wound Size | Types of Wounds | ||||
|---|---|---|---|---|---|---|
| Entry/Exit Wound Diameters; E + X [cm] | Cavity Diameter; C [Finger] | Soft Tissue Injury (ST) | Fracture Type; F | Critical Organ Injury; V | Critical Organ Injury + Fracture; VF | |
| Grade I—low-energy transfer | <10 | Less than 2 | Small, simple | 1 | 1 | 1 |
| Grade II—high-energy transfer | <10 | >2 | 2 | 2 | 2 | 2 |
| Grade III—massive wounds | >10 | >2 | 3 | 3 | 3 | Large wounds that can be life-threatening or that can damage limb functions |
| Material | Absorptive Capacity | Biodegradability | Hemostatic Potential |
|---|---|---|---|
| Chitosan | Moderate | High | High |
| Kaolin | High | Non-biodegradable | High |
| Alginate | High | High | Moderate to high |
| Zeolite | High | Non-biodegradable | High (with exothermic risk) |
| Hemostatic Dressing Type (Including Type of the Active Ingredient) | Wound Type/Model | Animal | Outcomes | Ref. |
|---|---|---|---|---|
| Topical hemostatic dressings with one of the ingredients: microfibrillar collagen, oxidized cellulose, thrombin, fibrinogen, propyl gallate, aluminum sulfate, and fully acetylated poly-N-acetyl glucosamine | a model of severe venous hemorrhage and hepatic injury | Yorkshire swine | hemostatic dressing that contains fibrinogen or thrombin reduced posttreatment blood loss | [51] |
| Lyophilized, ready-to-use fibrin-based sheets | rabbit ear artery | rabbit | immediate stop of bleeding (in 3–5 s) | [94] |
| Fibrin bandage | ballistic (gunshot; 0.308 caliber high-velocity bullet) wound | Angora goats | significant reduction in the blood loss; the mean arterial pressure was also maintained higher | [95] |
| The mineral zeolite powder QuikClot | lethal groin injury model | Yorkshire swine | increased survival and decreased hemorrhage in comparison to the untreated control group | [49] |
| Polivynyl alcohol (PVA)/sodium alginate (SA) hydrogel loaded with nitrofurazone | excision of dorsum (two full thickness skin wounds of 1.5 cm × 1.5 cm area) | Male Sprague Dawley rats | wound size reduction with new epithelium noted at the edge of the defect. However, overall, the positive healing effect was similar to that with PVA only | [96] |
| Commonly used QuikClot Combat Gauze, ChitoGauze, NuStat Tactical, Kerlix with no clotting agent | a unilateral arterial hemorrhagic groin injury (a swine model of prolonged field care with limb movement) | Swine | combat Gauze proved to have the lowest incidence of rebleeding, while the NuStat Tactical (made of regenerated cellulose and silica-based fibers) had the highest incidence of rebleeding at wounds after limb movement | [97] |
| Woven fiber matrix made from regenerated cotton cellulose, BloodSTOP iX Battle Matrix | swine extremity arterial hemorrhage model | Yorkshire swine | longer survival and significantly shorter times to hemostasis as compared to animals treated with QuikClot Combat Gauze | [98] |
| Algan Hemostatic Agent (AHA) | the femoral artery damage model | Rats | a significantly shorter time of bleeding compared to that of the control | [99] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamysz, W.; Kleczkowska, P. Biological Macromolecule-Based Dressings for Combat Wounds: From Collagen to Growth Factors—A Review. Med. Sci. 2025, 13, 106. https://doi.org/10.3390/medsci13030106
Kamysz W, Kleczkowska P. Biological Macromolecule-Based Dressings for Combat Wounds: From Collagen to Growth Factors—A Review. Medical Sciences. 2025; 13(3):106. https://doi.org/10.3390/medsci13030106
Chicago/Turabian StyleKamysz, Wojciech, and Patrycja Kleczkowska. 2025. "Biological Macromolecule-Based Dressings for Combat Wounds: From Collagen to Growth Factors—A Review" Medical Sciences 13, no. 3: 106. https://doi.org/10.3390/medsci13030106
APA StyleKamysz, W., & Kleczkowska, P. (2025). Biological Macromolecule-Based Dressings for Combat Wounds: From Collagen to Growth Factors—A Review. Medical Sciences, 13(3), 106. https://doi.org/10.3390/medsci13030106







