- Systematic Review
Systematic Review of Monoclonal Antibody Therapies in Relapsing Multiple Sclerosis: Comparator-Stratified Analysis of Relapse and Disability Outcomes
- Alin Ciubotaru,
- Cristina Grosu and
- Emilian Bogdan Ignat
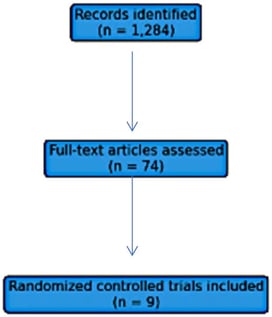
- + 13 authors
The Background: monoclonal antibody therapies represent high-efficacy treatment options for relapsing forms of multiple sclerosis (MS). However, the absence of direct head-to-head randomized trials and the use of heterogeneous comparators across pivotal studies complicate comparative effectiveness assessments. While network meta-analysis (NMA) offers a framework to integrate evidence, the fragmented structure of the available evidence base precludes a conventional NMA with global indirect comparisons and treatment ranking. Methods: A systematic review with qualitative assessment of treatment effects of randomized controlled trials evaluating monoclonal antibody therapies in relapsing forms of multiple sclerosis was conducted. Annualized relapse rate (ARR) was analyzed as the primary outcome, and six-month confirmed disability progression (CDP) as the key secondary outcome. Network geometry and connectivity were explicitly assessed for each outcome prior to quantitative synthesis. Analyses were restricted to comparator-defined connected components of the evidence base, and indirect comparisons across disconnected components were not performed. Sensitivity analyses, including descriptive analyses in progressive multiple sclerosis, were conducted where appropriate. Results: nine randomized controlled trials involving 6762 patients were included. For ARR, the evidence network was fragmented into three disconnected components defined by placebo-, interferon beta-1a-, and teriflunomide-controlled trials. Within connected sub-networks, monoclonal antibody therapies consistently demonstrated substantial reductions in ARR relative to their respective comparators, with overlapping confidence intervals suggesting broadly comparable relapse suppression among high-efficacy agents. For CDP, network connectivity was more limited, and treatment effects were more heterogeneous. Significant reductions in disability progression were observed for some agents within comparator-specific networks, while uncertainty remained for others. Due to network disconnection, no global treatment ranking was performed. Conclusions: this study provides a transparent synthesis of randomized evidence on monoclonal antibody therapies in relapsing MS. By explicitly accounting for network connectivity and comparator heterogeneity, the analysis avoids unsupported indirect comparisons and global treatment hierarchies. The findings support robust relapse suppression across monoclonal antibody therapies within comparable trial frameworks, while highlighting heterogeneity in disability outcomes. These results illustrate the importance of contextual interpretation in comparative effectiveness research in MS.
27 February 2026