Invited Review: Increasing Milk Yield and Negative Energy Balance: A Gordian Knot for Dairy Cows?
Abstract
:Simple Summary
Abstract
1. Introduction
2. Dry Matter Intake during Transition
3. Milk Yield and Negative Energy Balance
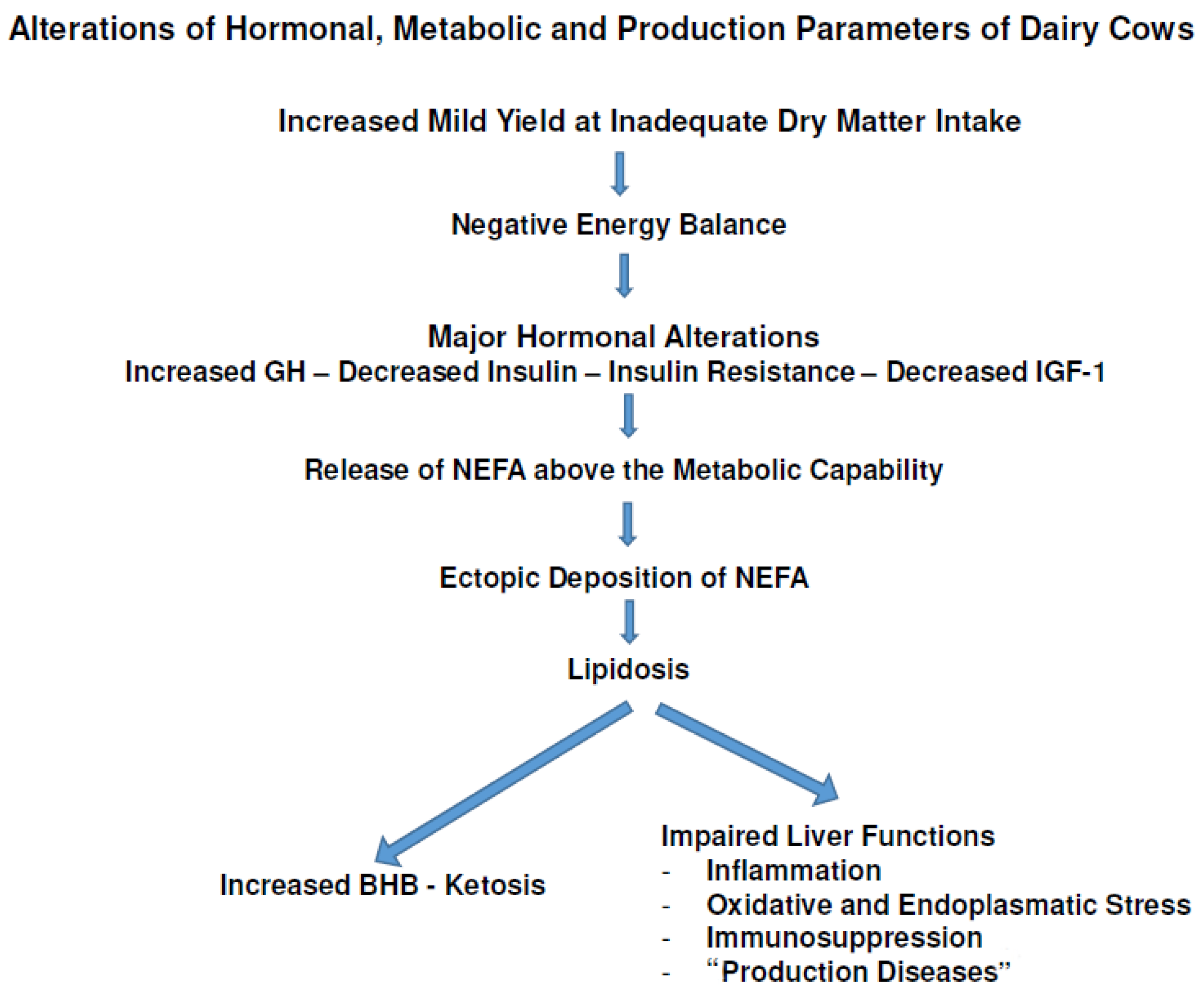
4. Mobilization of Reserves: Hormones and Metabolites
5. NEFAs, Lipidosis and Diseases
6. Limitations
7. Discussion
8. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baumgard, L.; Collier, R.; Bauman, D. A 100-Year Review: Regulation of nutrient partitioning to support lactation. J. Dairy Sci. 2017, 100, 10352–10366. [Google Scholar] [CrossRef] [PubMed]
- BRS (Bundesverband Rind and Schwein). Rinderproduktion in Deutschland 2022; Druck Center Meckenheim: Meckenheim, Germany, 2023; p. 17. ISSN 1439-8745. [Google Scholar]
- Collier, R.; Bauman, D. TRIENNIAL LACTATION SYMPOSIUM: Historical perspective of lactation biology in the 20th and early 21st centuries. J. Anim. Sci. 2017, 95, 5639–5652. [Google Scholar] [CrossRef] [PubMed]
- Tribout, T.; Minéry, S.; Vallée, R.; Saille, S.; Saunier, D.; Martin, P.; Ducrocq, V.; Faverdin, P.; Boichard, D. Genetic relationships between weight loss in early lactation and daily milk production throughout lactation in Holstein cows. J. Dairy Sci. 2023, 106, 4799–4812. [Google Scholar] [CrossRef] [PubMed]
- Mulligan, F.; Doherty, M. Production diseases of the transition cow. Vet. J. 2008, 176, 3–9. [Google Scholar] [CrossRef]
- Grummer, R.; Mashed, D.; Hayirly, A. Dry matter intake and energy balance in the transition period. Vet. Clin. Food Anim. 2004, 20, 447–470. [Google Scholar] [CrossRef]
- Shonka, B.; Tao, S.; Dahl, G.; Spurlock, D. Genetic regulation of prepartum dry matter intake in Holstein cows. J. Dairy Sci. 2015, 98, 8195–8200. [Google Scholar] [CrossRef]
- Kuhla, B.; Metges, C.; Hammon, H. Endogenous and dietary lipids influencing feed intake and energy metabolism of periparturient dairy cows. Domest. Anim. Endocrinol. 2016, 56, S2–S10. [Google Scholar] [CrossRef]
- Knight, C. Lactation and gestation in dairy cows: Flexibility avoids nutritional extremes. Proc. Nutr. Soc. 2001, 60, 527–537. [Google Scholar] [CrossRef]
- Vernon, R.; Pond, C. Adaptation of maternal adipose tissue to lactation. J. Mammary Gland Biol. Neoplasia 1997, 2, 231–241. [Google Scholar] [CrossRef]
- Gravert, H. Genetic factors controlling feed intake efficiency in dairy cows. Livest. Prod. Sci. 1985, 13, 87–95. [Google Scholar] [CrossRef]
- Balch, C. Feed intake regulation: A limiting factor in animal production. Livest. Prod. Sci. 1976, 3, 101–102. [Google Scholar] [CrossRef]
- Korver, S. Genetic aspects of feed intake and feed efficiency in dairy cattle: A review. Livest. Prod. Sci. 1988, 20, 1–13. [Google Scholar] [CrossRef]
- Arendonk, J.; Nieuwhof, G.; Vos, H.; Korver, S. Genetic aspects of feed intake and efficiency in lactating dairy heifers. Livest. Prod. Sci. 1991, 29, 263–275. [Google Scholar] [CrossRef]
- Von Leesen, R.; Tetens, J.; Stamer, E.; Junge, W.; Thaller, G.; Krattenmacher, N. Effect of genetic merit for energy balance on luteal activity and subsequent reproductive performance in primiparous Holstein-Friesian cows. J. Dairy Sci. 2014, 97, 1129–1138. [Google Scholar] [CrossRef] [PubMed]
- Rodehutscord, M.; Titze, N. Herausforderung Futteraufnahme—Überlegungen zur Milchkuh von morgen. Züchtungskunde 2018, 90, 7–12. [Google Scholar]
- McNamara, J. Research, improvement and application of mechanistic, biochemical, dynamic models of metabolism in lactating dairy cattle. Anim. Feed Sci. Technol. 2004, 112, 155–176. [Google Scholar] [CrossRef]
- Sheldon, M.; Cronin, J.; Pospiech, M.; Turner, M. Symposium Review: Mechanisms linking metabolic stress with innate immunity in the endometrium. J. Dairy Sci. 2018, 101, 3655–3664. [Google Scholar] [CrossRef] [PubMed]
- Bauman, D.; Currie, E. Partitioning of nutrients during pregnancy and lactation. J. Dairy Sci. 1980, 63, 1514–1529. [Google Scholar] [CrossRef] [PubMed]
- Vernon, R. Homeorhesis. In Yearbook; Hannah Research Institute: Ayr, UK, 1998; pp. 64–73. [Google Scholar]
- Martens, H. Transition period of the dairy cow revisited: I. Homeorhesis and its changes by selection and management. J. Agric. Sci. 2020, 12, 1. [Google Scholar] [CrossRef]
- Martens, H. Transition period of the dairy cow revisited: II. Homeorhetic stimulus and ketosis with implication for fertility. J. Agric. Sci. 2020, 12, 25–54. [Google Scholar] [CrossRef]
- Veerkamp, R.; Thompson, R. A covariance function for feed intake, live weight, and milk yield estimated using a random regression model. J. Dairy Sci. 1999, 82, 1565–1573. [Google Scholar] [CrossRef] [PubMed]
- Karacaören, B.; Jaffrézic, F.; Kadarmideen, H. Genetic parameters for functional traits in dairy cattle from random regression models. J. Dairy Sci. 2006, 89, 791–798. [Google Scholar] [CrossRef] [PubMed]
- Liinamo, A.; Mäntysaari, P.; Mäntysaari, E. Short communication: Genetic parameters for feed intake, production, and extent of negative energy balance in Nordic Red dairy cattle. J. Dairy Sci. 2012, 95, 6788–6794. [Google Scholar] [CrossRef] [PubMed]
- Krattenmacher, N.; Thaller, G.; Tetens, J. Analysis of the genetic architecture of energy balance and its major determinants dry matter intake and energy-corrected milk yield in primiparous Holstein cows. J. Dairy Sci. 2019, 102, 3241–3253. [Google Scholar] [CrossRef] [PubMed]
- Buttchereit, N.; Stamer, E.; Junge, W.; Thaller, G. Short communication: Genetic relationship among daily energy balance, feed intake, body condition score, and fat to protein ratio of milk in dairy cows. J. Dairy Sci. 2011, 94, 1586–1591. [Google Scholar] [CrossRef] [PubMed]
- Brandt, A.; Pabst, K.; Schulte-Coerne, H.; Gravert, H. Die Heritabilität der Futteraufnahme. Züchtungskunde 1985, 57, 299–308. [Google Scholar]
- Friggens, N.; Berg, P.; Theilgaard, P.; Korsgaard, I.; Ingvartsen, K.; Løvendahl, P.; Jensen, P. Breed and parity effects on energy balance profiles through lactation: Evidence of genetically driven body energy change. J. Dairy Sci. 2007, 90, 5291–5305. [Google Scholar] [CrossRef]
- Gruber, L.; Pries, M.; Schwarz, F.-J.; Spiekers, H.; Staudacher, W. Schätzung der Futteraufnahme bei der Milchkuh. DLG-Inf. 2006, 1, 2–29. Available online: https://www.dlg.org/fileadmin/downloads/landwirtschaft/themen/ausschuesse_facharbeit/tier/futtermittel/futteraufnahme_milchkuh06.pdf (accessed on 30 September 2023).
- Hart, I.; Bines, J.; Balch, C.; Cowie, A. Hormone and metabolite differences between lactating beef and dairy cattle. Life Sci. 1975, 16, 1285–1292. [Google Scholar] [CrossRef]
- Sutter, F.; Beever, D. Energy and nitrogen metabolism in Holstein-Friesian cows during early lactation. Animal Sci. 2000, 70, 503–514. [Google Scholar] [CrossRef]
- Coffey, M.; Simm, G.; Oldham, J.; Hill, W.; Brotherstone, S. Genotype and diet effect on energy balance in the first three lactations of dairy cows. J. Dairy Sci. 2004, 87, 4318–4326. [Google Scholar] [CrossRef] [PubMed]
- Schröder, U.; Staufenbiel, R. Invited review: Methods to determine body fat reserves in the dairy cow with special regard to ultrasonographic measurement of backfat thickness. J. Dairy Sci. 2006, 89, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Komaragiri, M.; Erdman, R. Factors affecting body tissue mobilization in early lactation dairy cows. 1. Effect of dietary protein on mobilization of body fat and protein. J. Dairy Sci. 1997, 80, 929–937. [Google Scholar] [CrossRef] [PubMed]
- Bauman, D. Regulation of nutrient portioning during lactation: Homeostasis and homeorhesis revisited. In Ruminant Physiology: Digestion, Metabolism, Growth and Reproduction; Cronje, J., Ed.; CAB International: London, UK, 2000; pp. 311–328. [Google Scholar]
- Horst, E.; Kvidera, S.; Baumgard, L. Invited review: The influence of immune activation on transition cow health and performance—A critical evaluation of traditional dogmas. J. Dairy Sci. 2021, 104, 8380–8410. [Google Scholar] [CrossRef] [PubMed]
- Martinez, B.; Ortiz, R. Thyroid hormone regulation and insulin resistance: Insights from animals naturally adapted to fasting. Physiology 2017, 32, 141–151. [Google Scholar] [CrossRef]
- Oftedal, O. The adaptation of milk secretion to the constrains of fasting in bears, seals, and Baleen whales. J. Dairy Sci. 1993, 76, 3234–3246. [Google Scholar] [CrossRef]
- Danfær, V. Nutrient metabolism and utilization in the liver. Livest. Prod. Sci. 1994, 39, 115–127. [Google Scholar] [CrossRef]
- Etherton, T.; Bauman, D. Biology of somatotropin in growth and lactation of domestic animals. Physiol. Rev. 1998, 78, 745–761. [Google Scholar] [CrossRef]
- Lucy, M. Mechanisms linking the somatotropic axis with insulin: Lessons from the postpartum dairy cow. N. Z. Soc. Anim. Prod. 2004, 64, 19–23. [Google Scholar]
- Butler, S.; Marr, A.; Pelton, S.; Radcliff, S.; Lucy, M.; Butler, R. Insulin restores GH responsiveness during lactation-induced negative energy balance in dairy cattle: Effects on expression of IGF-I and GH receptor 1A. J. Endocrinol. 2003, 176, 205–217. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Boyd, C.; Bracken, C.; Lamberson, W.; Keisler, D.; Lucy, M. Reduced growth hormone receptor (GHR) messenger ribonucleic acid in liver of periparturient cattle is caused by a specific down-regulation of GHR 1A that is associated with decreased insulin-like growth factor I. Endocrinology 1999, 140, 3947–3954. [Google Scholar] [CrossRef] [PubMed]
- Okamura, C.; Bader, J.; Keisler, D.; Lucy, M. Short communication: Growth hormone receptor expression in two dairy breeds during the periparturient period. J. Dairy Sci. 2009, 92, 2706–2710. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Lucy, M.; Crooker, B.; Beal, W. Expression of growth hormone Receptor 1A mRNA is decreased in dairy cows but not in beef cows at parturition. J. Dairy Sci. 2005, 88, 1370–1377. [Google Scholar] [CrossRef] [PubMed]
- Lucy, M.; Verkerk, G.; Whyte, B.; Macdonald, K.; Burton, L.; Cursons, R.; Holmes, C. Somatropic axis components and nutrient partitioning in genetically diverse dairy cows management under different feed allowances in a pasture system. J. Dairy Sci. 2009, 92, 526–539. [Google Scholar] [CrossRef] [PubMed]
- Gross, J.; Bruckmaier, R. Repeatability of metabolic responses to a nutrient deficiency in early and mid lactation and implications for robustness of dairy cows. J. Dairy Sci. 2015, 98, 8634–8643. [Google Scholar] [CrossRef] [PubMed]
- Arshad, U.; Santos, J. Hepatic triacylglycerol associations with production and health in dairy cows. J. Dairy Sci. 2022, 105, 5393–5409. [Google Scholar] [CrossRef] [PubMed]
- McNamara, J. Integrating genotype and nutrition on utilization of body reserves during lactation of dairy cattle. In Ruminant Physiology: Digestion, Metabolism, Growth and Reproduction; Cronje, J., Ed.; CAB International: London, UK, 2000; pp. 353–370. [Google Scholar]
- Roberts, C.; Reid, I.; Roelands, G.; Patterson, A. A fat mobilisation syndrome in dairy cows in early lactation. Vet. Rec. 1981, 108, 7–9. [Google Scholar] [CrossRef]
- Gross, J. Hepatic lipidosis in ruminants. Vet. Clin. Food Anim. 2023, 39, 371–383. [Google Scholar] [CrossRef]
- Martens, H. Die Leberverfettung der Milchkuh: Teil 1. Bedeutung von Insulin und der Wachstumshormon-IGF-1—Achse. Tierärztliche Prax. Ausg. G 2023, 51, 97–108. [Google Scholar] [CrossRef]
- Sundrum, A. Metabolic disorders in the transition period indicate that the dairy cows’ ability to adapt is overstressed. Animals 2015, 5, 978–1020. [Google Scholar] [CrossRef]
- Seifi, H.; Leblanc, S.; Leslie, K.; Duffield, T. Metabolic predictors of post-partum disease and culling risk in dairy cattle. Vet. J. 2011, 188, 216–220. [Google Scholar] [CrossRef] [PubMed]
- Martinez, N.; Risco, C.; Lima, F.; Bisinotto, R.; Greco, L.; Ribeiro, E.; Maunsell, F.; Galvão, K.; Santos, J. Evaluation of peripartal calcium status, energetic profile, and neutrophil function in dairy cows at low or high risk of developing uterine disease. J. Dairy Sci. 2012, 95, 7158–7172. [Google Scholar] [CrossRef] [PubMed]
- Chamberlin, W.; Middleton, J.; Spain, J.; Joknson, G.; Ellersieck, M.; Pithua, P. Subclinical hypomagnesemia, plasma biochemical parameters, liquid metabolis, postpartum disease, and fertility in postparturient dairy cows. J. Dairy Sci. 2013, 96, 7001–7013. [Google Scholar] [CrossRef]
- Blum, J.; Wilson, R.; Kronfeld, D. Plasma insulin concentrations in parturient cows. J. Dairy Sci. 1973, 56, 459–464. [Google Scholar] [CrossRef] [PubMed]
- Martinez, N.; Sinedino, L.; Bisinotto, R.; Ribeiro, E.; Gomes, G.; Lima, F.; Greco, L.; Risco, C.; Galvão, C.; Taylor-Rodriguez, D.; et al. Effect of induced subclinical hypocalcemia on physiological responses and neutrophil function in dairy cows. J. Dairy Sci. 2014, 97, 874–887. [Google Scholar] [CrossRef] [PubMed]
- Jorritsma, R.; Jorritsma, H.Y.; Schukken, H.; Wentink, G. Relationships between fatty liver and fertility and some periparturient diseases in commercial Dutch dairy herds. Theriogenology 2000, 54, 1065–1074. [Google Scholar] [CrossRef]
- Walsh, R.; Walton, J.; Kelton, D.; LeBlanc, S.; Leslie, K.; Duffield, T. The effect of subclinical ketosis in early lactation on reproductive performance of postpartum dairy cows. J. Dairy Sci. 2007, 90, 2788–2796. [Google Scholar] [CrossRef]
- Bell, A. Regulation of organic nutrients metabolism during transition from late pregnancy to early lactation. J. Anim. Sci. 1995, 73, 2804–2819. [Google Scholar] [CrossRef]
- Gross, J.; Bruckmaier, R. Review: Metabolic challenges in lactating dairy cows and their assessment via established and novel indicators in milk. Animal 2019, 13, s75–s81. [Google Scholar] [CrossRef]
- Merkuriaw, Y. Negative energy balance and its implication on productive and reproductive performance of early lactating cow. J. Appl. Animal. Res. 2023, 51, 220–229. [Google Scholar] [CrossRef]
- Trevisi, E.; Minuti, A. Assessment of the innate response in the periparturient cow. Res. Vet. Sci. 2018, 116, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Krogstad, K.; Bradford, B. Does feeding starch contribute to the risk of systemic inflammation in dairy cows? J. Dairy Sci. Commun. 2023, 4, 14–18. [Google Scholar]
- Sordillo, L.; Mavangira, V. The nexus between nutrient metabolism, oxidative stress and inflammation in transition cows. Anim. Prod. Sci. 2014, 54, 1204–1214. [Google Scholar] [CrossRef]
- Abuelo, A.; Mann, S.; Andres, G. Metabolic factors at the crossroads of periparturient immunity and inflammation. Vet. Clin. Food Animal. 2023, 39, 203–218. [Google Scholar] [CrossRef] [PubMed]
- Gessner, D.; Ringseis, R.; Eder, K. Potential of plant polyphenols to combat oxidative stress and inflammatory processes in farm animals. J. Anim. Physiol. Anim. Nutr. 2017, 101, 605–628. [Google Scholar] [CrossRef]
- Xie, W.; Chen, M.; Loor, J.; Song, X.; Ma, N.; Zhou, S.; Zhang, H.; Chang, G.; Shen, X. AMPK-endoplasmic reticulum stress axis contributes to lipopolysaccharide-caused mitochondrial dysfunction by regulating mitochondria-associated membrane function in bovine hepatocytes. J. Dairy Res. 2023, 106, 5146–5164. [Google Scholar] [CrossRef]
- Flachowsky, G.; Jeroch, H.; Kirchgeßner, M.; Pallauf, J.; Pfeffer, E.; Schulz, E.; Staudacher, W. (Eds.) GfE (Gesellschaft für Ernährungsphysiologie). In Empfehlungen zur Energie- und Nährstoffversorgung der Milchkühe und Aufzuchtrinder; DLG Verlag: Frankfurt, Germany, 2001. [Google Scholar]
- Oikonomou, G.; Valergakis, G.; Arsenos, G.; Roubies, N.; Banos, G. Genetic profile of body energy and blood metabolites traits across lactation in primiparous Holstein cows. J. Dairy Sci. 2008, 91, 2814–2822. [Google Scholar] [CrossRef]
- Buttchereit, N.; Stamer, E.; Junge, W.; Thaller, G. Genetic parameters for energy balance, fat/protein ratio, body condition score and disease traits in German Holstein cows. Anim. Breed. Genet. 2012, 129, 280–288. [Google Scholar] [CrossRef]
- Koeck, A.; Jamrozik, J.; Schenkel, F.; Moore, R.; Lefebvre, D.; Kelton, D.; Miglior, F. Genetic analysis of milk β-hydroxybutyrate and its association with fat-to-protein ratio, body condition score, clinical ketosis, and displaced abomasum in early first lactation of Canadian Holsteins. J. Dairy Sci. 2014, 97, 7286–7292. [Google Scholar] [CrossRef]
- Suthar, V.; Canelas-Raposo, J.; Deniz, A.; Heuwieser, W. Prevalence of subclinical ketosis and relationships with postpartum diseases in European dairy cows. J. Dairy Sci. 2013, 96, 2925–2938. [Google Scholar] [CrossRef]
- McArt, J.; Nydam, D.; Oetzel, G.; Overton, T.; Ospina, P. Elevated non-esterified fat acids and β-hydroxybutyrate and their association with transition dairy cows performance. Vet. J. 2013, 198, 560–570. [Google Scholar] [CrossRef] [PubMed]
- Berge, A.; Vertenten, G. A field study to determine the prevalence, dairy herd management systems, and fresh cow clinical conditions associated with ketosis in western European dairy herds. J. Dairy Sci. 2014, 97, 2145–2154. [Google Scholar] [CrossRef] [PubMed]
- Abuajamiehn, M.; Kvidera, S.; Fernandez, M.; Nayeri, A.; Upah, N.; Nolan, E.; Baumgard, L. Inflammatory biomarkers are associated with ketosis in periparturient Holstein cows. Res. Vet. Sci. 2016, 109, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Reid, I. Incidence and severity of fatty liver in dairy cows. Vet. Rec. 1980, 197, 281–284. [Google Scholar] [CrossRef] [PubMed]
- Bremmer, D.; Trower, S.; Bertics, S.; Besong, S.; Bernabucci, U.; Grummer, R. Etiology of fatty liver in Dairy cattle: Effects of nutrition and hormonal status on hepatic microsomal triglyceride transfer protein. J. Dairy Sci. 2000, 83, 2239–2251. [Google Scholar] [CrossRef]
- Bobe, G.; Young, J.; Beitz, D. Invited review: Pathology, aetiology, prevention, and treatment of fat liver in dairy cows. J. Dairy Sci. 2004, 87, 3105–3124. [Google Scholar] [CrossRef] [PubMed]
- Benedet, A.; Manuelian, C.; Zidi, A.; Penasa, M.; De Marchi, M. Invited review: β-hydroxybutyrate concentration in blood and milk and its associations with cow performance. Animal 2019, 13, 1676–1689. [Google Scholar] [CrossRef]
- Baird, G. Aspects of ruminant intermediary metabolism in relation to ketosis. Biochem. Soc. Trans. 1977, 5, 819–827. [Google Scholar] [CrossRef]
- Baird, G. Lactation, pregnancy and metabolic disorders in the ruminant. Proc. Nutr. Soc. 1981, 40, 115–120. [Google Scholar] [CrossRef]
- McArt, J.; Oetzel, G. Considerations in the diagnosis and treatment of early lactation calcium disturbances. Vet. Clin. Food Anim. 2023, 39, 241–259. [Google Scholar] [CrossRef]
- Scharrer, E. Control of food intake by fat acid oxidation and ketogenesis. Nutrition 1999, 15, 704–714. [Google Scholar] [CrossRef] [PubMed]
- Allen, M.; Piantoni, P. Metabolic control of feed intake. Implications for metabolic diseases of fresh cows. Vet. Clin. Food Anim. 2013, 29, 279–297. [Google Scholar] [CrossRef] [PubMed]
- Lean, I.; Farver, T.; Troutt, H.; Bruss, M.; Galland, J.; Baldwin, R.; Weaver, L. Time series cross-correlation analysis of postparturient relationships among serum metabolites and yield variables in Holstein cows. J. Dairy Sci. 1992, 75, 1891–1900. [Google Scholar] [CrossRef] [PubMed]
- Schlumbohm, C.; Harmeyer, J. Hyperketonemia impairs glucose metabolism in pregnant and nonpregnant ewes. J. Dairy Sci. 2004, 87, 350–358. [Google Scholar] [CrossRef] [PubMed]
- Zarrin, M.; De Matteis, L.; Vernay, M.; Wellnitz, O.; van Dorland, H.; Bruckmaier, R. Long-term elevation of β-hydroxybutyrate in dairy cows through infusion: Effects on feed intake, milk production, and metabolism. J. Dairy Sci. 2013, 96, 2960–2972. [Google Scholar] [CrossRef]
- Du, X.; Zhu, Y.; Peng, Z.; Cui, Y.; Zhang, Q.; Shi, Z.; Guan, Y.; Sha, X.; Shen, T.; Yang, Y.; et al. High concentrations of fat acids and β-hydroxybutyrate impair the growth hormone-mediated hepatic JAK2-STAT5 pathway in clinically ketotic cows. J. Dairy Sci. 2018, 101, 3476–3487. [Google Scholar] [CrossRef]
- Wathes, D.; Cheng, Z.; Bourne, N.; Taylor, V.; Coffey, M.; Brotherstone, S. Differences between primiparous and multiparous dairy cows in the inter-relationships between metabolic traits, milk yield and body condition score in the periparturient period. Domest. Anim. Endocrin. 2007, 33, 203–225. [Google Scholar] [CrossRef]
- Cheng, Z.; Oguejiofor, C.; Swangchan-Uthai, T.; Carr, S.; Wathes, D. Relationship between circulating urea concentrations and endometrial function in postpartum dairy cows. Animals 2015, 5, 748–773. [Google Scholar] [CrossRef]
- Piechotta, M.; Maysegades, W.; Ligges, U.; Lilientahl, J.; Hoeflich, A.; Miyamoto, A.; Bollwein, H. Antepartal insulin-like growth factor 1 and insulin-like growth factor binding protein 2 concentrations are indicative of ketosis in dairy cows. J. Dairy Sci. 2015, 98, 3100–3105. [Google Scholar] [CrossRef]
- Gohary, K.; Leslie, K.; Ford, J.; Capel, M.; LeBlanc, J.; Duffield, T. Effect of administration of recombinant bovine somatropin on health and performance of lactating cows diagnosed with hyperketonemia. J. Dairy Sci. 2015, 98, 4392–4400. [Google Scholar] [CrossRef]
- Lucy, M.; Jiang, H.; Kobayashi, Y. Changes in the somatotropic axis associated with the initiation of lactation. J. Dairy Sci. 2001, 84, E113–E119. [Google Scholar] [CrossRef]
- Barret, D.; Steele, M.; Overton, M. Managing energy balance in the transition cow. Vet. Rec. 2014, 174, 655–656. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Cordoba-Chacon, J.; Kineman, R.; Cronstein, B.; Muzumdar, R.; Gong, Z.; Yakar, S. Growth hormone control of hepatic lipid metabolism. Diabetes 2016, 65, 3598–3609. [Google Scholar] [CrossRef] [PubMed]
- Taylor, V.; Cheng, Z.; Pushpakumara, P.; Beever, D.; Wathes, D. Relationships between the plasma concentrations of insulin-like growth factor-I in dairy cows and their fertility and milk yield. Vet. Rec. 2004, 155, 583–588. [Google Scholar] [CrossRef]
- Heemskerk, V.; Daemen, M.; Buurman, W. Insulin-like growth factor (IGF-1) and growth hormone (GH) in immunity and inflammation. Cytokine Growth Factor Rev. 1999, 19, 5–14. [Google Scholar] [CrossRef]
- Smith, T. Insulin-like growth factor-I regulation of immune function: A potential therapeutic target in autoimmune diseases? Pharmacol. Rev. 2010, 63, 199–236. [Google Scholar] [CrossRef]
- Nesbitt, T.; Drezner, M. Insulin-like growth factor-I regulation of renal 25-hydroxycitamin D-1-hydroxlylase activity. Endocrinology 1993, 132, 133–138. [Google Scholar] [CrossRef]
- Beilharz, R.; Nitter, G. The missing E: The role of the environment in evolution and animal breeding. J. Anim. Breed. Genet. 1998, 115, 439–453. [Google Scholar] [CrossRef]
- Martens, H. Leistung und Gesundheit von Milchkühen: Bedeutung von Genetik (Ursache) und Management (Wirkung). Ein Beitrag zur Diskussion. Tierärztliche Prax. G 2016, 44, 253–258. [Google Scholar] [CrossRef]
- Emanuelson, U. Recording of production diseases in cattle and possibilities for genetic improvement. Livest. Prod. Sci. 1988, 20, 89–106. [Google Scholar] [CrossRef]
- Simianer, H.; Solbu, H.; Schaeffer, L. Estimated genetic correlations between disease and yield traits in dairy cattle. J. Dairy Sci. 1991, 74, 4358–4365. [Google Scholar] [CrossRef] [PubMed]
- Uribe, H.; Kennedy, B.; Martin, S.; Kelton, D. Genetic parameters for common health disorders of Holstein. J. Dairy Sci. 1995, 78, 421–430. [Google Scholar] [CrossRef]
- Royal, M.; Flint, A.; Woolliams, J. Genetic and phenotypic relationships among endocrine and traditional fertility traits and production traits in Holstein-Friesian dairy cows. J. Dairy Sci. 2002, 85, 958–967. [Google Scholar] [CrossRef] [PubMed]
- Pritchard, T.; Coffey, M.; Wall, E. Understanding the genetics of survival in dairy cows. J. Dairy Sci. 2013, 96, 3296–3309. [Google Scholar] [CrossRef] [PubMed]
- Ask-Gullstrand, P.; Strandberg, E.; Båge, R.; Christensen, J.; Berglund, B. Genetic parameters for reproductive losses estimated from in-line milk progesterone profiles in Swedish dairy cattle. J. Dairy Sci. 2021, 104, 3231–3239. [Google Scholar] [CrossRef] [PubMed]
- Koeck, A.; Loker, S.; Miglior, F.; Kelton, D.; Jamrozik, J.; Schenkel, F. Genetic relationship of clinical mastitis, cystic ovaries, and lameness with milk yield and somatic cell score in first-lactation Canadians Holsteins. J. Dairy Sci. 2014, 97, 5806–5813. [Google Scholar] [CrossRef]
- Ingvartsen, K. Feeding-and management-related diseases in transition cow. Physiological adaptations around calving and strategies to reduce feeding-related diseases. Anim. Feed Sci. Technol. 2006, 126, 175–213. [Google Scholar] [CrossRef]
- Dechow, C.; Goodling, R. Mortality, culling by sixty days in milk, and production profiles in highland low-survival Pennsylvania herds. J. Dairy Sci. 2008, 91, 4630–4639. [Google Scholar] [CrossRef]
- Berry, D.; Bermingham, M.; Good, M.; More, S. Genetic of animal health and disease in cattle. Ir. Vet. J. 2011, 64, 5. [Google Scholar] [CrossRef]
- Brito, L.; Bedere, N.; Douhard, F.; Oliveira, H.; Arnal, M.; Peñagaricano, F.; Schinckel, A.; Baes, C.; Miglior, F. Review: Genetic selection of high-yielding dairy cattle toward sustainable farming systems in a rapidly changing world. Animal 2021, 15, 100292. [Google Scholar] [CrossRef]
- Miglior, F.; Fleming, A.; Malchlodi, F.; Brito, L.; Martin, P. A 100.year review: Identification and genetic selection of economical important traits in cattle. J. Dairy Sci. 2017, 100, 10251–10271. [Google Scholar] [CrossRef] [PubMed]
- Brade, W. Personal communication, 2023.
- Britt, J.; Cushman, R.; Dechow, C.; Dobson, H.; Humblot, P.; Hutjens, M.; Jones, G.; Mitloehner, F.; Ruegg, P.; Sheldon, I.; et al. Review: Perspective on high-performing dairy cows and herds. Animal 2021, 2021, 100298. [Google Scholar] [CrossRef] [PubMed]
- Hoedemaker, M. Abschlussbericht: Tiergesundheit, Hygiene und Biosicherheit in Deutschen Milchkuhbetrieben—Eine Prävalenzstudie (PraeRi). 2020. Available online: https://www.vetmed.fu-berlin.de/news/_ressourcen/Abschlussbericht_PraeRi.pdf (accessed on 22 September 2023).
- Dallago, G.; Wade, K.; Cue, R.; McClure, J.; Lacroix, R.; Pellerin, D.; Vasseur, E. Keeping Dairy Cows for Longer: A critical literature review on dairy cow longevity in high milk-producing countries. Animals 2021, 11, 808. [Google Scholar] [CrossRef]
- Heringstad, B.; Egger-Danner, C.; Charfeddine, N.; Pryce, J.; Stock, K.; Kofler, F.J.; Sogstad, A.; Holzhauer, M.; Fiedler, A.; Müller, K.; et al. Invited review: Genetics and claw health: Opportunities to enhance claw health by genetic selection. J. Dairy Sci. 2018, 101, 4801–4821. [Google Scholar] [CrossRef] [PubMed]
- VIT (Vereinigte Informationssysteme Tierhaltung). Jahresbericht 2016. Available online: https://www.vit.de/fileadmin/Wir-sind-vit/Jahresberichte/vit-JB2016-gesamt.pdf (accessed on 30 September 2023).
- Agnew, R.; Yan, T. Impact of recent research on energy feeding system for dairy cattle. Livest. Prod. Sci. 2000, 66, 197–215. [Google Scholar] [CrossRef]
- Patton, J.; Kenny, D.; Mee O’Mara, F.; Wathes, D.; Cook, M.; Murphy, J. Effect of milking frequency and diet on milk production, energy balance and reproduction in dairy cows. J. Dairy Sci. 2006, 89, 1478–1487. [Google Scholar] [CrossRef]
- Allen, M. Review: Control of feed intake by hepatic oxidation in ruminants: Integration of homeostasis and homeorhesis. Animal 2020, 14, s55–s64. [Google Scholar] [CrossRef]
- Khorrami, B.; Khiaosa-ard, R.; Zebeli, Q. Models to predict the risk of subacute ruminal acidosis in dairy cows based on dietary and cow factors: A meta-analysis. J. Dairy Sci. 2021, 104, 7761–7780. [Google Scholar] [CrossRef]
- Humer, E.; Khol-Parisini, A.; Gruber, L.; Gasteiner, J.; Abdel-Raheem, sh.; Zebeli, Q. Long-term reticuloruminal pH dynamics and markers of liver health in early-lactating cows of various parities fed diets differing in grain processing. J. Dairy Sci. 2015, 98, 6433–6448. [Google Scholar] [CrossRef]
- Zhang, H.; Xue, Y.; Xie, W.; Wang, Y.; Ma, N.; Chang, G.; Shen, X. Subacute ruminal acidosis downregulates FOXA2, changes oxidative status, and induces autophagy in the livers of dairy cows fed a high-concentrate diet. J. Dairy Sci. 2023, 106, 2007–2018. [Google Scholar] [CrossRef]
- Wall, E.; McFadden, T. Triennial Lactation Symposium: A local affair: How the mammary gland adapts to changes in milking frequency. J. Anim. Sci. 2012, 90, 1695–1707. [Google Scholar] [CrossRef] [PubMed]
- Rukkwamsuk, T.; Wensing, T.; Geelen, M. Effect of fatty liver on hepatic gluconeogenesis in periparturient dairy cows. J. Dairy Sci. 2000, 82, 500–5005. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Armentano, L.; Bremmer, D.; Grummer, R.; Bertics, S. Plasma concentrations of urea, ammonia, glutamine around calving and the relation to hepatic triglyceride, to plasma ammonia removal and blood acid-base balance. J. Dairy Sci. 2000, 83, 734–740. [Google Scholar] [CrossRef]
- Strang, B.; Bertics, S.; Grummer, R.; Armentano, L. Effect of long-chain fatty acids on triglyceride accumulation, gluconeogenesis, and ureagenesis in bovine hepatocytes. J. Dairy Sci. 1998, 81, 728–739. [Google Scholar] [CrossRef] [PubMed]
- Mann, S.; McArt, J. Hyperketonemia. A marker of disease, a sign of a high-producing dairy cow, or both? Vet. Clin. Food Anim. 2023, 39, 307–324. [Google Scholar] [CrossRef]
- Hindman, M. Metabolic diseases in beef cattle. Vet. Clin. Food Anim. 2023, 39, 337–353. [Google Scholar] [CrossRef]
- Houlahan, K.; Schenkel, F.; Hailemariam, D.; Lassen, J.; Kargo, M.; Cole, J.; Baes, C. Effects of incorporating dry matter intake and residual feed intake into a selection index for dairy cattle using deterministic modeling. Animals 2021, 11, 1157. [Google Scholar] [CrossRef] [PubMed]
- Bedere, N.; Cutulic, E.; Delaby, L.; Garcia-Launay, F.; Disenhaus, B. Meta-analysis of the relationship between reproduction, milk yield and body condition score in dairy cows. Livest. Sci. 2018, 210, 73–84. [Google Scholar] [CrossRef]
- Rauw, M.; Kanis, E.; Nordhuizen, E.; Grommers, F. Undesirable side effects of selection for high production efficiency in farm animals: A review. Livest. Prod. Sci. 1998, 56, 15–33. [Google Scholar] [CrossRef]
- Knaus, W. Dairy cows trapped between performance demands and adaptability. J. Sci. Food Agric. 2009, 89, 1107–1114. [Google Scholar] [CrossRef]
- Oltenacu, P.; Broom, D. The impact of genetic selection for increased milk yield on the welfare of dairy cows. Anim. Welf. 2010, 19, 39–49. [Google Scholar] [CrossRef]
| Hormone Postpartum | Major Impact on Metabolism |
|---|---|
| High GH | Lipolysis in subcutaneous and abdominal fat tissue Stimulation of gluconeogenesis in the liver Synthesis of IGF-1 in the liver Growth of mammary gland and synthesis of milk Insulin resistance in muscle and fat tissue |
| Low insulin p.p. | General: reduction in anabolic metabolism Reduction in lipogenesis in fat tissue Reduced expression of growth hormone receptor 1A in the liver |
| GH-dependent insulin resistance p.p. | Insulin resistance in muscle and fat tissue Reduced uptake of glucose in muscle and fat tissue Partitioning of glucose to mammary gland No insulin resistance in the liver |
| Low IGF-1 | Lessening of a plethora of para-, auto- and hormonal effects of IGF-1 Reduction in negative feedback mechanism on GH release from the pituitary gland: increase in GH and uncoupling of GH-IGF-1 axis |
| Parameter p.p. | High NEFA versus Low NEFA |
|---|---|
| Growth hormone | Higher |
| Insulin | Lower (not significant) |
| Insulin resistance | Not significant |
| IGF-1 | Lower |
| NEFAs | Higher |
| BHB | Higher |
| Triglycerides | Higher |
| Glucose | Lower |
| Milk | Higher |
| DMI | Lower |
| NEB | Lower |
| Disease (%) | Lipidosis 2.5% TG | Lipidosis 5.0% TG | Lipidosis 7.5% TG |
|---|---|---|---|
| Subclinical ketosis (<1.2 mmol/L BHB) | 15.3 | 24.7 | 37.5 |
| Subclinical hypocalcemia (<2.0 mmol/L Ca) | 30.3 | 40.8 | 52.4 |
| Retained placenta | 9.3 | 11.9 | 15.1 |
| Metritis | 12.5 | 18.2 | 25.7 |
| Puerperal metritis | 6.9 | 10.2 | 14.7 |
| Mastitis | 14.2 | 16.9 | 19.9 |
| Displaced abomasum | 1.0 | 1.0 | 1.0 |
| Morbidity | 36.2 | 41.3 | 46.7 |
| Multiple diseases | 8.7 | 13.7 | 21.1 |
| Survival by day 300 | 91.1 | - | 86.3 |
| Production Data | Lipidosis 2.5% TG | Lipidosis 5.0% TG | Lipidosis 7.5% TG |
|---|---|---|---|
| Milk yield (kg/d) | 41.1 | 42.7 | 43.2 |
| Dry matter intake (kg/d) | 22.0 | 21.5 | 21.1 |
| Net energy balance (MJ/d) | −8.65 | −16.93 | −21.40 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martens, H. Invited Review: Increasing Milk Yield and Negative Energy Balance: A Gordian Knot for Dairy Cows? Animals 2023, 13, 3097. https://doi.org/10.3390/ani13193097
Martens H. Invited Review: Increasing Milk Yield and Negative Energy Balance: A Gordian Knot for Dairy Cows? Animals. 2023; 13(19):3097. https://doi.org/10.3390/ani13193097
Chicago/Turabian StyleMartens, Holger. 2023. "Invited Review: Increasing Milk Yield and Negative Energy Balance: A Gordian Knot for Dairy Cows?" Animals 13, no. 19: 3097. https://doi.org/10.3390/ani13193097
APA StyleMartens, H. (2023). Invited Review: Increasing Milk Yield and Negative Energy Balance: A Gordian Knot for Dairy Cows? Animals, 13(19), 3097. https://doi.org/10.3390/ani13193097








