Dietary Supplementation with Palmitoyl-Glucosamine Co-Micronized with Curcumin Relieves Osteoarthritis Pain and Benefits Joint Mobility
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Reagents
2.3. Carrageenan-Induced Inflammation and Treatment Administration
- CAR + curcumin (10 mg/kg)
- CAR + micronized PGA (20 mg/kg)
- CAR + co-micronized PGA-Cur (2:1) (30 mg/kg)
- CAR + carboxymethylcellulose (vehicle group)
2.3.1. Assessment of Paw Edema
2.3.2. Assessment of Inflammatory Pain
2.3.3. Histopathological Analysis of Paw Tissue
2.3.4. Evaluation of Myeloperoxidase Activity
2.4. Monoiodoacetate-Induced Osteoarthritis and Treatment Administration
2.4.1. Assessment of Mechanical Allodynia
2.4.2. Motor Function Analysis
2.4.3. Histological Analysis of Tibiofemoral Joint Cartilage Damage
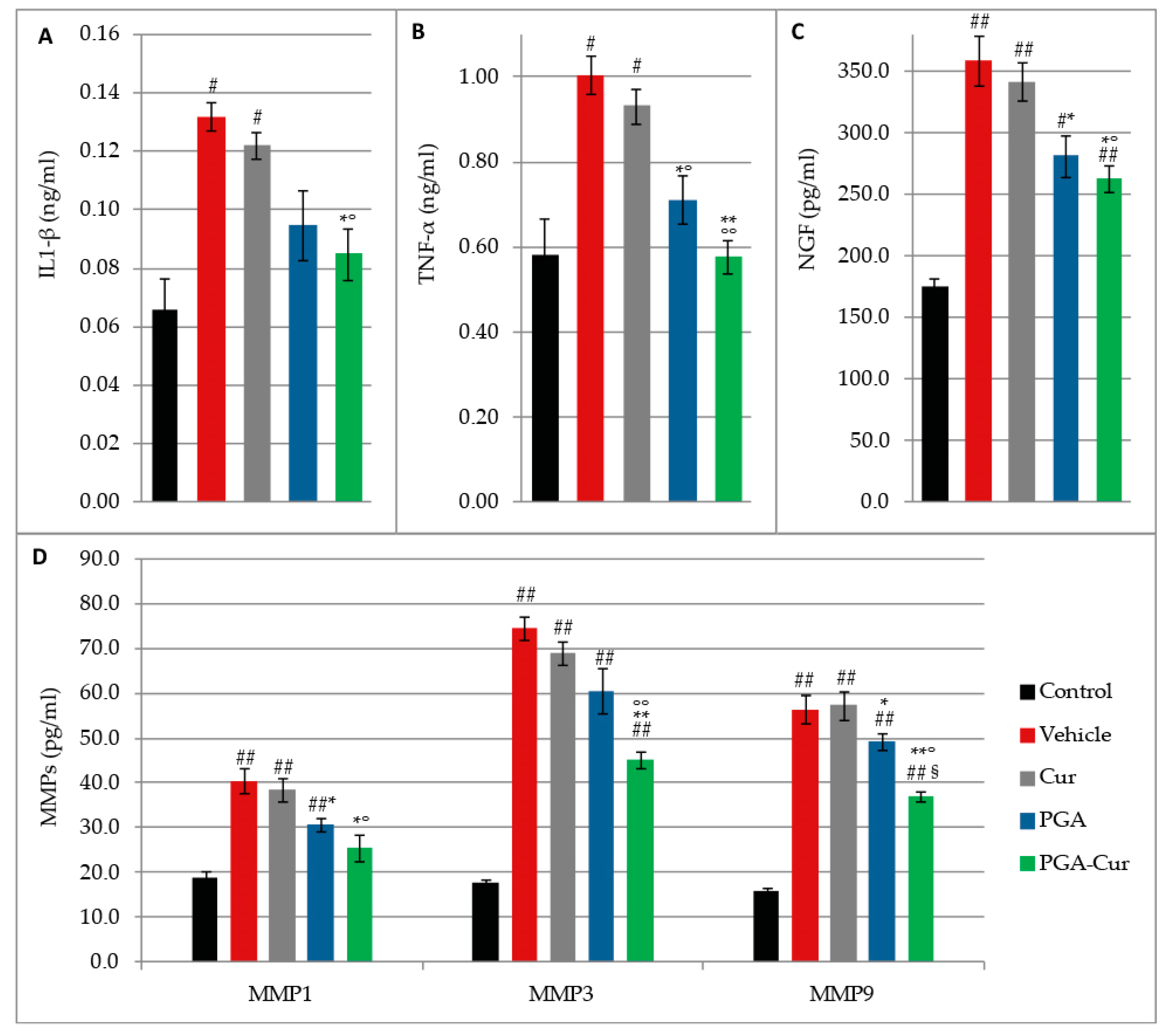
2.4.4. Measurement of Pro-Inflammatory, Sensitizing, and Matrix Degradation Serum Markers
2.5. Data Analysis
3. Results
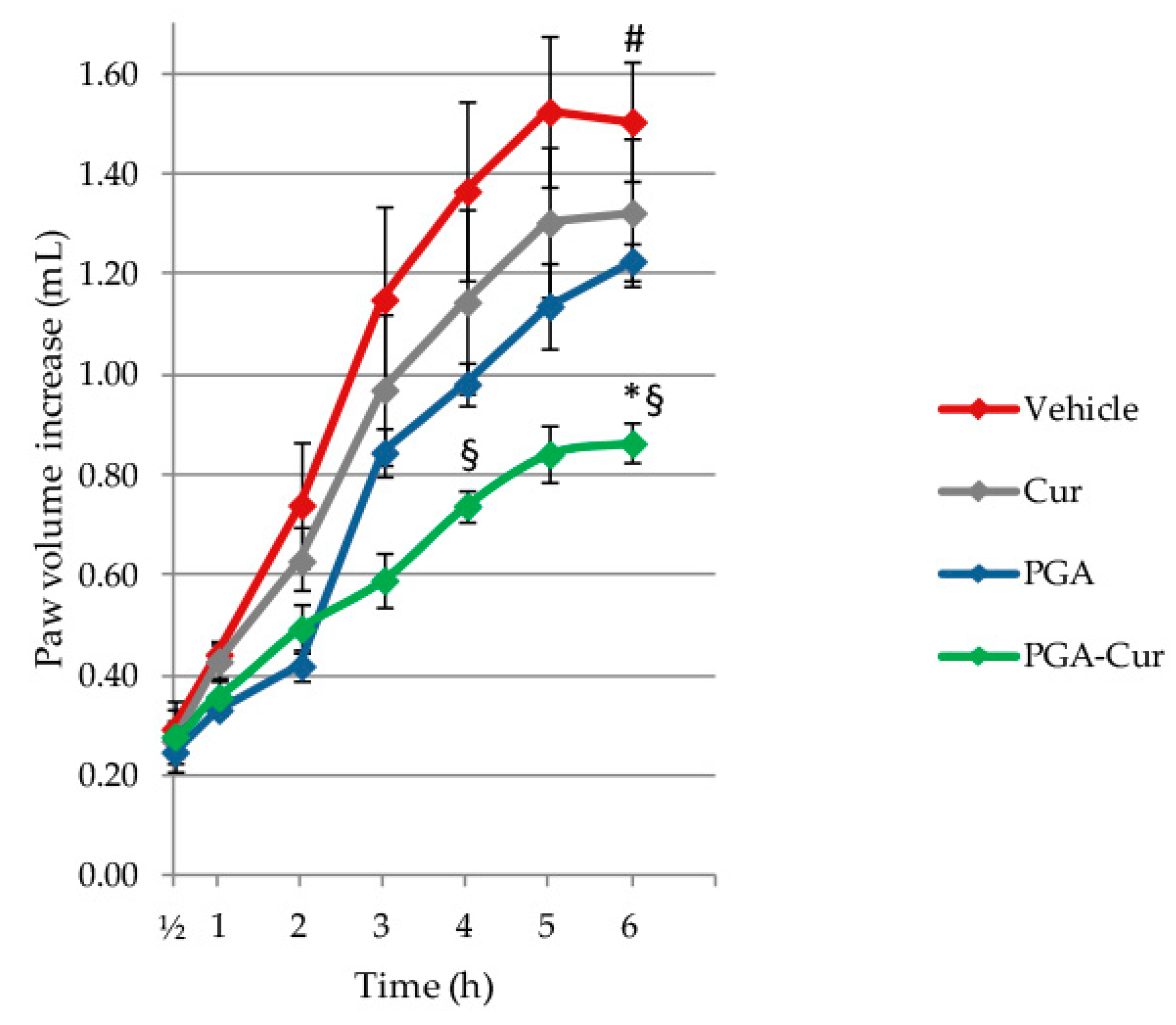
3.1. Effect on Carrageenan-Induced Paw Edema
3.2. Effect on Carrageenan-Induced Inflammatory Pain
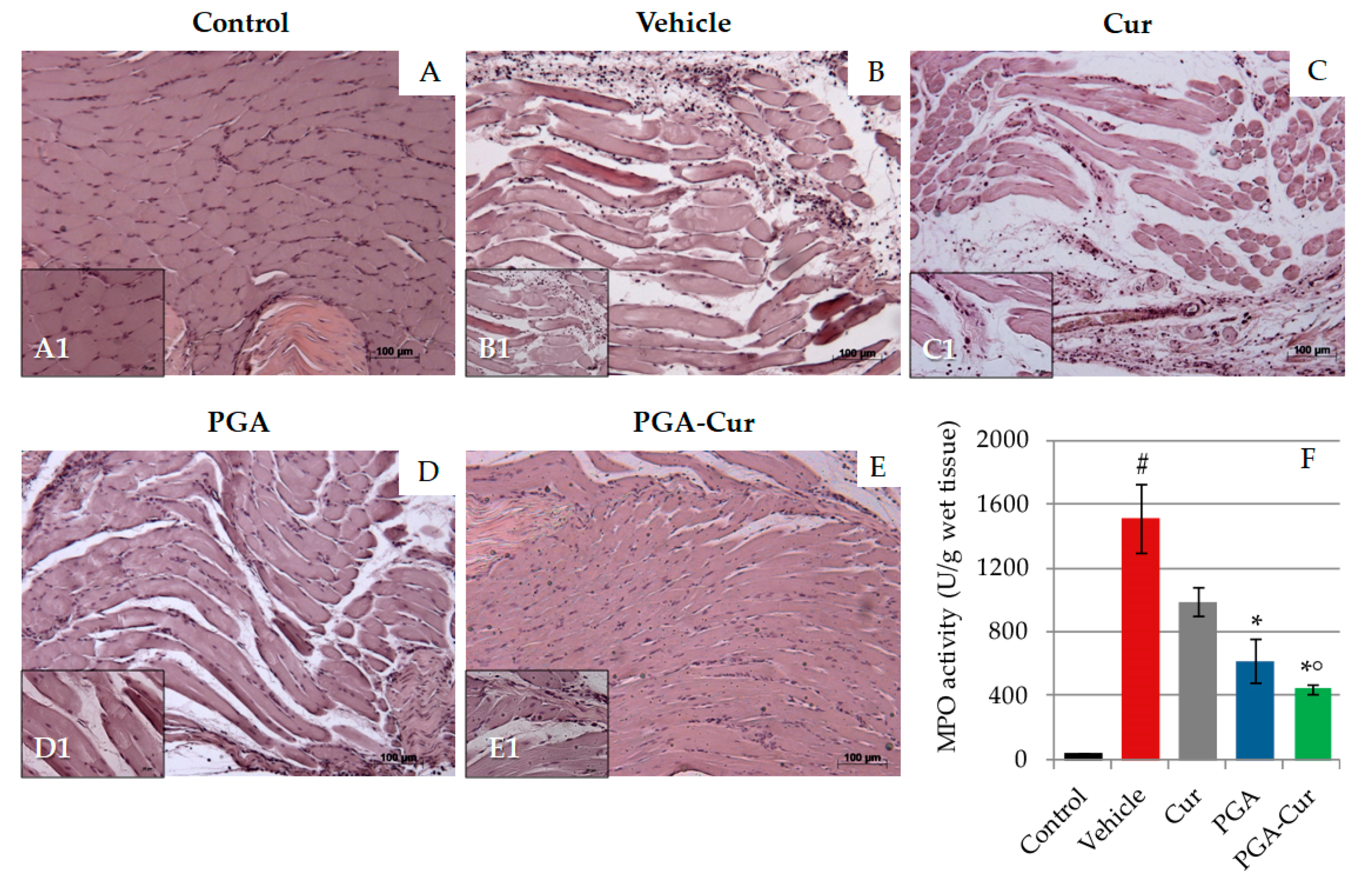
3.3. Effect on Carrageenan-Induced Histological Inflammation and Neutrophil Infiltration into the Paw
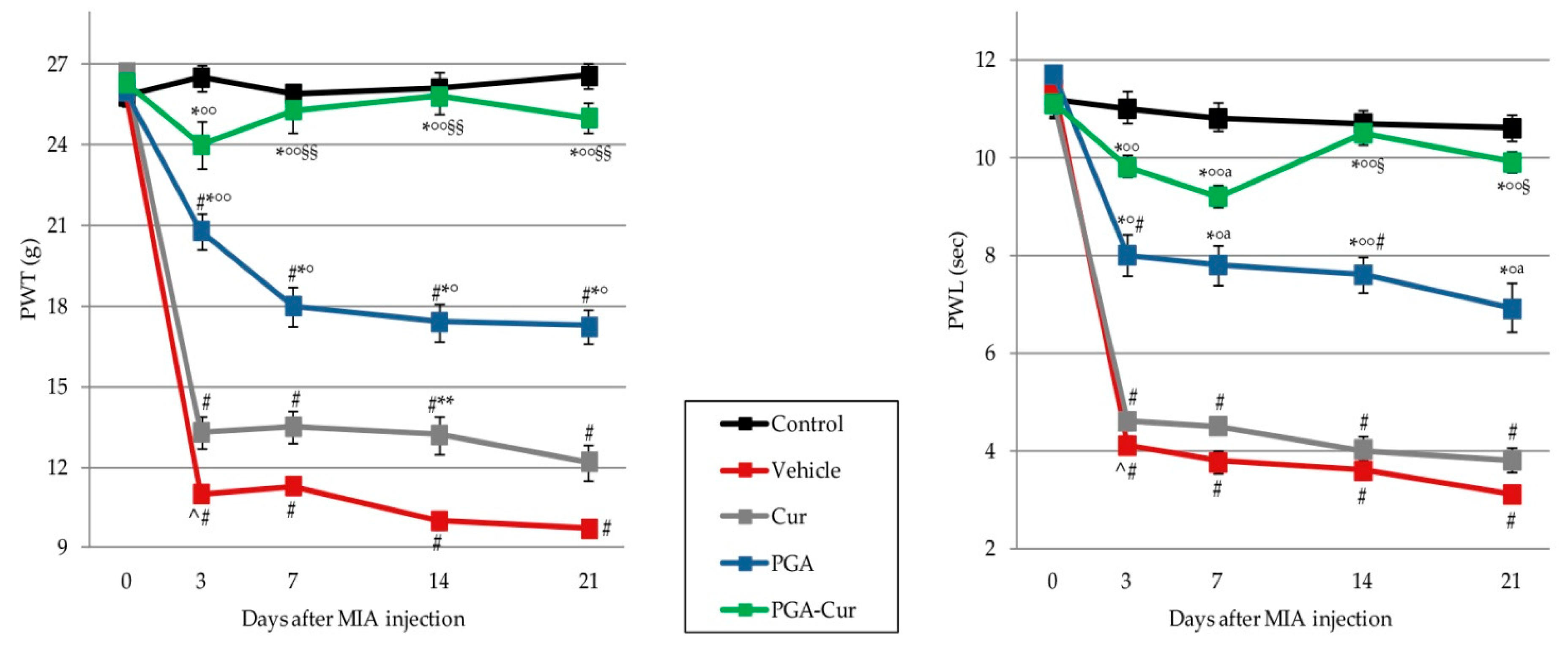
3.4. Effect on Monoiodoacetate-Induced Neuropathic Pain
3.5. Effect on Monoiodoacetate-Induced Locomotor Dysfunction
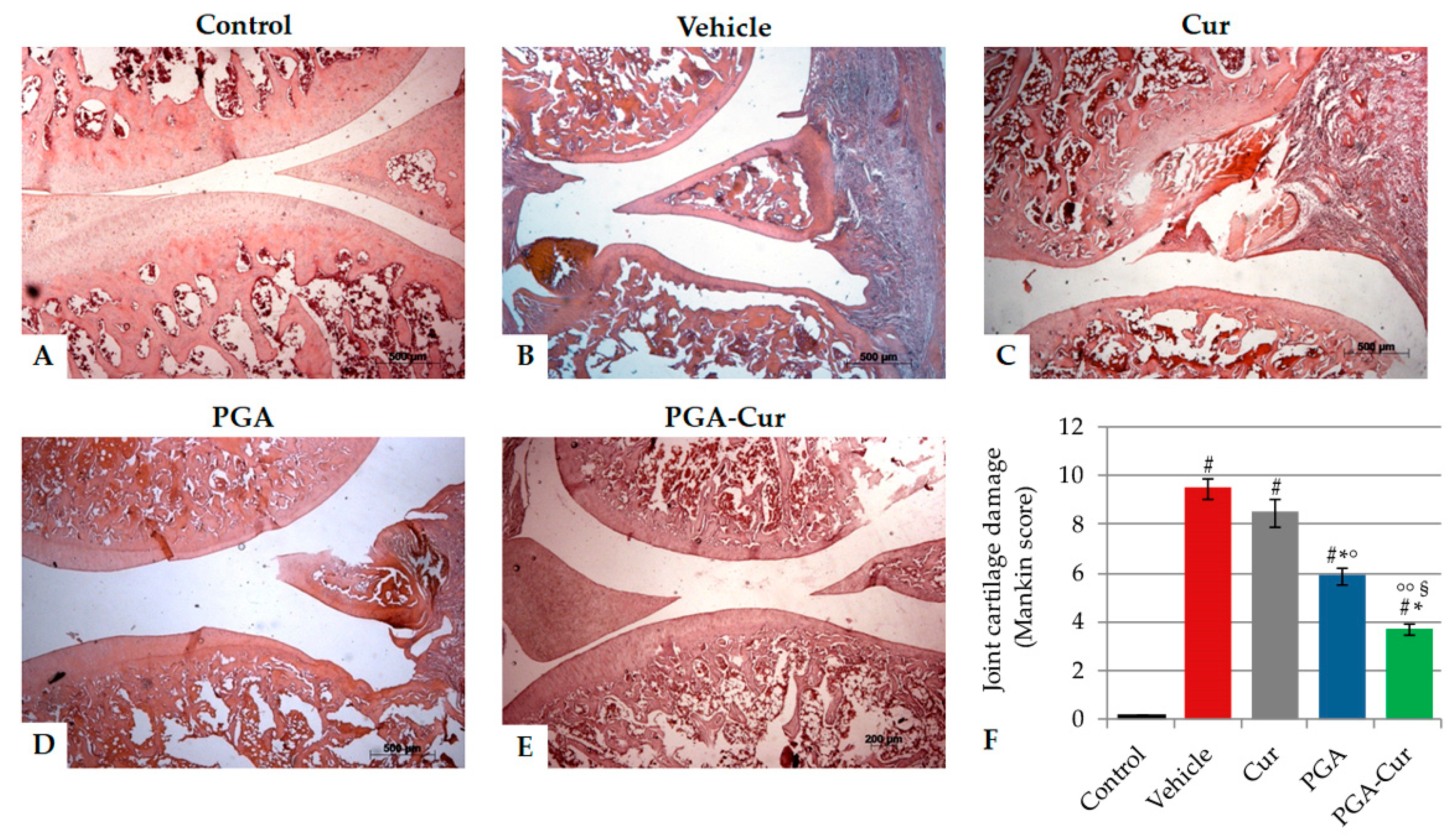
3.6. Effect on Monoiodoacetate-Induced Joint Cartilage Damage
3.7. Effect on Monoiodoacetate-Induced Increase of Proinflammatory, Sensitizing, and Matrix Degradation Mediators
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Johnston, S.A. Osteoarthritis. Joint anatomy, physiology, and pathobiology. Vet. Clin. N. Am. Small Anim. Pr. 1997, 27, 699–723. [Google Scholar] [CrossRef]
- Bennett, D.; Zainal Ariffin, S.M.; Johnston, P. Osteoarthritis in the cat: 1. how common is it and how easy to recognise? J. Feline Med. Surg. 2012, 14, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.L.; O’Neill, D.G.; Brodbelt, D.C.; Church, D.B.; Meeson, R.L.; Sargan, D.; Summers, J.F.; Zulch, H.; Collins, L.M. Prevalence, duration and risk factors for appendicular osteoarthritis in a UK dog population under primary veterinary care. Sci. Rep. 2018, 8, 5641. [Google Scholar] [CrossRef] [PubMed]
- Slingerland, L.I.; Hazewinkel, H.A.; Meij, B.P.; Picavet, P.; Voorhout, G. Cross-sectional study of the prevalence and clinical features of osteoarthritis in 100 cats. Vet. J. 2011, 187, 304–309. [Google Scholar] [CrossRef] [PubMed]
- Guillot, M.; Taylor, P.M.; Rialland, P.; Klinck, M.P.; Moreau, M.M.; Martel-Pelletier, J.; Pelletier, J.P.; Troncy, E. Evoked temporal summation in cats to highlight central sensitization related to osteoarthritis-associated chronic pain: A preliminary study. PLoS ONE 2014, 9, e97347. [Google Scholar] [CrossRef]
- Lascelles, B.D.; Robertson, S.A. DJD-associated pain in cats. What can we do to promote patient comfort? J. Feline Med. Surg. 2010, 12, 200–212. [Google Scholar] [CrossRef]
- Epstein, M.; Rodan, I.; Griffenhagen, G.; Kadrlik, J.; Petty, M.; Robertson, S.; Simpson, W. AAHA/AAFP pain management guidelines for dogs and cats. J. Am. Anim. Hosp. Assoc. 2015, 51, 67–84. [Google Scholar] [CrossRef]
- Fusco, M.; Skaper, S.D.; Coaccioli, S.; Paladini, A.; Varrassi, G. Degenerative joint diseases and neuroinflammation. Pain Pr. 2017, 17, 522–532. [Google Scholar] [CrossRef]
- Robinson, W.H.; Lepus, C.M.; Wang, Q.; Raghu, H.; Mao, R.; Lindstrom, T.M.; Sokolove, J. Low-grade inflammation as a key mediator of the pathogenesis of osteoarthritis. Nat. Rev. Rheumatol. 2016, 12, 580–592. [Google Scholar] [CrossRef]
- Costigan, M.; Scholz, J.; Woolf, C.J. Neuropathic pain: A maladaptive response of the nervous system to damage. Annu. Rev. Neurosci. 2009, 32, 1–32. [Google Scholar] [CrossRef] [Green Version]
- Syx, D.; Tran, P.B.; Miller, R.E.; Malfait, A.M. Peripheral mechanisms contributing to osteoarthritis pain. Curr. Rheumatol. Rep. 2018, 20, 9. [Google Scholar] [CrossRef] [PubMed]
- Bradesi, S. Role of spinal cord glia in the central processing of peripheral pain perception. Neurogastroenterol. Motil. 2010, 22, 499–511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miller, R.J.; Malfait, A.M.; Miller, R.E. The innate immune response as a mediator of osteoarthritis pain. Osteoarthr. Cartil. 2020, 28, 562–571. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.A. Managing neuropathic pain in dogs. Front. Vet. Sci. 2016, 3, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monteiro-Steagall, B.P.; Steagall, P.V.; Lascelles, B.D. Systematic review of nonsteroidal anti-inflammatory drug-induced adverse effects in dogs. J. Vet. Intern. Med. 2013, 27, 1011–1019. [Google Scholar] [CrossRef] [PubMed]
- Budsberg, S.C.; Torres, B.T.; Kleine, S.A.; Sandberg, G.S.; Berjeski, A.K. Lack of effectiveness of tramadol hydrochloride for the treatment of pain and joint dysfunction in dogs with chronic osteoarthritis. J. Am. Vet. Med. Assoc. 2018, 252, 427–432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gupta, R.C.; Doss, R.B.; Lall, R.; Srivastava, A.; Sinha, A. Nutraceuticals in arthritis. In Nutraceuticals in Veterinary Medicine, 1st ed.; Gupta, R.C., Srivastava, A., Lall, R., Eds.; Springer Nature: Basel, Switzerland, 2019; pp. 365–381. [Google Scholar]
- Johnson, K.A.; Lee, A.H.; Swanson, K.S. Nutrition and nutraceuticals in the changing management of osteoarthritis for dogs and cats. J. Am. Vet. Med. Assoc. 2020, 256, 1335–1341. [Google Scholar] [CrossRef]
- Alves, J.C.; Santos, A.M.; Jorge, P.I. Effect of an oral joint supplement when compared to carprofen in the management of hip osteoarthritis in working dogs. Top. Companion Anim. Med. 2017, 32, 126–129. [Google Scholar] [CrossRef]
- Scott, R.M.; Evans, R.; Conzemius, M.G. Efficacy of an oral nutraceutical for the treatment of canine osteoarthritis. A double-blind, randomized, placebo-controlled prospective clinical trial. Vet. Comp. Orthop. Traumatol. 2017, 30, 318–323. [Google Scholar]
- Valastro, C.; Campanile, D.; Marinaro, M.; Franchini, D.; Piscitelli, F.; Verde, R.; Di Marzo, V.; Di Bello, A. Characterization of endocannabinoids and related acylethanolamides in the synovial fluid of dogs with osteoarthritis: A pilot study. BMC Vet. Res. 2017, 13, 309. [Google Scholar] [CrossRef] [Green Version]
- Re, G.; Barbero, R.; Miolo, A.; Di Marzo, V. Palmitoylethanolamide, endocannabinoids and related cannabimimetic compounds in protection against tissue inflammation and pain: Potential use in companion animals. Vet. J. 2007, 173, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Gugliandolo, E.; Peritore, A.F.; Piras, C.; Cuzzocrea, S.; Crupi, R. Palmitoylethanolamide and related ALIAmides: Pro-homeostatic lipid compounds for animal health and wellbeing. Vet. Sci. 2020, 7, 78. [Google Scholar] [CrossRef] [PubMed]
- Calignano, A.; La Rana, G.; Giuffrida, A.; Piomelli, D. Control of pain initiation by endogenous cannabinoids. Nature 1998, 394, 277–281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piomelli, D.; Hohmann, A.G.; Seybold, V.; Hammock, B.D. A lipid gate for the peripheral control of pain. J. Neurosci. 2014, 34, 15184–15191. [Google Scholar] [CrossRef] [PubMed]
- Marini, I.; Cavallaro, M.; Bartolucci, M.L.; Alessandri-Bonetti, A.; Gatto, M.R.; Cordaro, M.; Checchi, L. Can celecoxib enhance palmitoylethanolamide’s effect in the treatment of temporo-mandibular arthralgia in osteoarthritis patients? J. Transl. Sci. 2018, 5, 1–4. [Google Scholar]
- Steels, E.; Venkatesh, R.; Steels, E.; Vitetta, G.; Vitetta, L. A double-blind randomized placebo controlled study assessing safety, tolerability and efficacy of palmitoylethanolamide for symptoms of knee osteoarthritis. Inflammopharmacology 2019, 27, 475–485. [Google Scholar] [CrossRef]
- Gugliandolo, E.; Barbagallo, A.; Peritore, A.F.; Cuzzocrea, S.; Crupi, R. Oral supplementation with ultramicronized palmitoylethanolamide for joint disease and lameness management in four jumping horses: A case report. Animals 2020, 10, 1469. [Google Scholar] [CrossRef]
- Alsalem, M.; Haddad, M.; Aldossary, S.A.; Kalbouneh, H.; Altarifi, A.; Jaffal, S.M.; Abbas, M.A.; Aldaoud, N.; El-Salem, K. Role of cannabinoid receptor 1 and the peroxisome proliferator-activated receptor a in mediating anti-nociceptive effects of synthetic cannabinoids and a cannabinoid-like compound. Inflammopharmacology 2019, 27, 1131–1142. [Google Scholar] [CrossRef]
- Cordaro, M.; Siracusa, R.; Impellizzeri, D.; D’Amico, R.; Peritore, A.F.; Crupi, R.; Gugliandolo, E.; Fusco, R.; Di Paola, R.; Schievano, C.; et al. Safety and efficacy of a new micronized formulation of the ALIAmide palmitoylglucosamine in preclinical models of inflammation and osteoarthritis pain. Arthritis Res. 2019, 21, 254. [Google Scholar] [CrossRef] [Green Version]
- Cerrato, S.; Brazis, P.; Miolo, A.; della Valle, M.F.; Puigdemont, A. Effects of palmitoylethanolamide on immunologically induced histamine, PGD2 and TNFα release from canine skin mast cells. Vet. Immunol. Immunopathol. 2010, 133, 9–15. [Google Scholar] [CrossRef]
- Miolo, A.; Badino, P.; Barbero, R.; Re, G. Glupamid: A novel nutraceutical approach to canine and feline osteoarthritis. J. Vet. Pharm. 2006, 29, 202–203. [Google Scholar] [CrossRef]
- Costa, B.; Comelli, F.; Miolo, A.; della Valle, M.F. Effect of Glupamid (N-palmitoyl-D-glucosamine) on knee osteoarthritis pain. In Proceedings of the 3rd WVOC (World Veterinary Orthopaedic) Congress 2010, Bologna, Italy, 15–18 September 2010; pp. 553–554. [Google Scholar]
- Prasad, S.; Gupta, S.C.; Tyagi, A.K.; Aggarwal, B.B. Curcumin, a component of golden spice: From bedside to bench and back. Biotechnol. Adv. 2014, 32, 1053–1064. [Google Scholar] [CrossRef] [PubMed]
- Chand, N. Standardized turmeric and curcumin. In Nutraceuticals in Veterinary Medicine, 1st ed.; Gupta, R.C., Srivastava, A., Lall, R., Eds.; Springer Nature: Basel, Switzerland, 2019; pp. 3–23. [Google Scholar]
- Kunwar, A.; Priyadarsini, K.I. Curcumin and its role in chronic diseases. Adv. Exp. Med. Biol. 2016, 928, 1–25. [Google Scholar] [PubMed]
- Henrotin, Y.; Priem, F.; Mobasheri, A. Curcumin: A new paradigm and therapeutic opportunity for the treatment of osteoarthritis: Curcumin for osteoarthritis management. Springerplus 2013, 2, 56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asperio, R. Dietary supplementation with PGA-Cur: A survey on 181 osteoarthritis dogs. Summa 2020, 8, 39–48. [Google Scholar]
- De Vito, V.; Salvadori, M.; Poapolathep, A.; Owen, H.; Rychshanova, R.; Giorgi, M. Pharmacokinetic/pharmacodynamic evaluation of grapiprant in a carrageenan-induced inflammatory pain model in the rabbit. J. Vet. Pharm. 2017, 40, 468–475. [Google Scholar] [CrossRef]
- Morris, C.J. Carrageenan-induced paw edema in the rat and mouse. Methods Mol. Biol. 2003, 225, 115–121. [Google Scholar]
- Britti, D.; Crupi, R.; Impellizzeri, D.; Gugliandolo, E.; Fusco, R.; Schievano, C.; Morittu, V.M.; Evangelista, M.; Di Paola, R.; Cuzzocrea, S. A novel composite formulation of palmitoylethanolamide and quercetin decreases inflammation and relieves pain in inflammatory and osteoarthritic pain models. BMC Vet. Res. 2017, 13, 229. [Google Scholar] [CrossRef]
- Hargreaves, K.; Dubner, R.; Brown, F.; Flores, C.; Joris, J. A new and sensitive method for measuring thermal nociception in cutaneous hyperalgesia. Pain 1988, 32, 77–88. [Google Scholar] [CrossRef]
- Bang, J.S.; Oh, D.H.; Choi, H.M.; Sur, B.J.; Lim, S.J.; Kim, J.Y.; Yang, H.I.; Yoo, M.C.; Hahm, D.H.; Kim, K.S. Anti-inflammatory and antiarthritic effects of piperine in human interleukin 1beta-stimulated fibroblast-like synoviocytes and in rat arthritis models. Arthritis Res. 2009, 11, R49. [Google Scholar] [CrossRef] [Green Version]
- D’Souza, W.N.; Ng, G.Y.; Youngblood, B.D.; Tsuji, W.; Lehto, S.G. A review of current animal models of osteoarthritis pain. Curr. Pharm. Biotechnol. 2011, 12, 1596–1612. [Google Scholar] [CrossRef] [PubMed]
- de Sousa Valente, J. The pharmacology of pain associated with the monoiodoacetate model of osteoarthritis. Front. Pharmacol. 2019, 10, 974. [Google Scholar] [CrossRef] [PubMed]
- Kuyinu, E.L.; Narayanan, G.; Nair, L.S.; Laurencin, C.T. Animal models of osteoarthritis: Classification, update, and measurement of outcomes. J. Orthop. Surg. Res. 2016, 11, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, P.; Okun, A.; Ren, J.; Guo, R.C.; Ossipov, M.H.; Xie, J.; King, T.; Porreca, F. Ongoing pain in the MIA model of osteoarthritis. Neurosci. Lett. 2011, 493, 72–75. [Google Scholar] [CrossRef] [Green Version]
- Zhang, R.X.; Ren, K.; Dubner, R. Osteoarthritis pain mechanisms: Basic studies in animal models. Osteoarthr. Cartil. 2013, 21, 1308–1315. [Google Scholar] [CrossRef] [Green Version]
- Xu, Y.; Liu, Q.; Liu, Z.L.; Lim, L.; Chen, W.H.; Lin, N. Treatment with SiMiaoFang, an anti-arthritis chinese herbal formula, inhibits cartilage matrix degradation in osteoarthritis rat model. Rejuvenation Res. 2013, 16, 364–376. [Google Scholar] [CrossRef] [Green Version]
- Jensen, T.S.; Finnerup, N.B. Allodynia and hyperalgesia in neuropathic pain: Clinical manifestations and mechanisms. Lancet Neurol. 2014, 13, 924–935. [Google Scholar] [CrossRef]
- Vonsy, J.L.; Ghandehari, J.; Dickenson, A.H. Differential analgesic effects of morphine and gabapentin on behavioural measures of pain and disability in a model of osteoarthritis pain in rats. Eur. J. Pain. 2009, 13, 786–793. [Google Scholar] [CrossRef]
- Malfait, A.M.; Little, C.B.; McDougall, J.J. A commentary on modelling osteoarthritis pain in small animals. Osteoarthr. Cartil. 2013, 21, 1316–1326. [Google Scholar] [CrossRef] [Green Version]
- Aborehab, N.M.; El Bishbishy, M.H.; Refaiy, A.; Waly, N.E. A putative Chondroprotective role for IL-1β and MPO in herbal treatment of experimental osteoarthritis. BMC Complement. Altern. Med. 2017, 17, 495. [Google Scholar] [CrossRef] [Green Version]
- Isola, M.; Ferrari, V.; Miolo, A.; Stabile, F.; Bernardini, D.; Carnier, P.; Busetto, R. Nerve Growth Factor concentrations in the synovial fluid from healthy dogs and dogs with secondary osteoarthritis. Vet. Comp. Orthop. Traumatol. 2011, 24, 279–284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malfait, A.M.; Schnitzer, T.J. Towards a mechanism-based approach to pain management in osteoarthritis. Nat. Rev. Rheumatol. 2013, 9, 654–664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pajak, A.; Kostrzewa, M.; Malek, N.; Korostynski, M.; Starowicz, K. Expression of matrix metalloproteinases and components of the endocannabinoid system in the knee joint are associated with biphasic pain progression in a rat model of osteoarthritis. J. Pain Res. 2017, 10, 1973–1989. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mehana, E.E.; Khafaga, A.F.; El-Blehi, S.S. The role of matrix metalloproteinases in osteoarthritis pathogenesis: An updated review. Life Sci. 2019, 234, 116786. [Google Scholar] [CrossRef]
- He, B.H.; Christin, M.; Mouchbahani-Constance, S.; Davidova, A.; Sharif-Naeini, R. Mechanosensitive ion channels in articular nociceptors drive mechanical allodynia in osteoarthritis. Osteoarthr. Cartil. 2017, 25, 2091–2099. [Google Scholar] [CrossRef] [Green Version]
- Bannuru, R.R.; Osani, M.C.; Al-Eid, F.; Wang, C. Efficacy of curcumin and Boswellia for knee osteoarthritis: Systematic review and meta-analysis. Semin. Arthritis Rheum. 2018, 48, 416–429. [Google Scholar] [CrossRef]
- Chin, K.Y. The spice for joint inflammation: Anti-inflammatory role of curcumin in treating osteoarthritis. Drug Des. Devel. 2016, 10, 3029–3042. [Google Scholar] [CrossRef] [Green Version]
- Comblain, F.; Barthélémy, N.; Lefèbvre, M.; Schwartz, C.; Lesponne, I.; Serisier, S.; Feugier, A.; Balligand, M.; Henrotin, Y. A randomized, double-blind, prospective, placebo-controlled study of the efficacy of a diet supplemented with curcuminoids extract, hydrolyzed collagen and green tea extract in owner’s dogs with osteoarthritis. BMC Vet. Res. 2017, 13, 395. [Google Scholar] [CrossRef] [Green Version]
- Petrosino, S.; Italian National Research Council, Institute of Biomolecular Chemistry, Pozzuoli, Italy. Personal communication, 2020.
- Malek, N.; Starowicz, K. Joint problems arising from lack of repair mechanisms: Can cannabinoids help? Br. J. Pharm. 2019, 176, 1412–1420. [Google Scholar] [CrossRef]
- La Porta, C.; Bura, S.A.; Negrete, R.; Maldonado, R. Involvement of the endocannabinoid system in osteoarthritis pain. Eur. J. Neurosci. 2014, 39, 485–500. [Google Scholar] [CrossRef] [Green Version]
- Richardson, D.; Pearson, R.G.; Kurian, N.; Latif, M.L.; Garle, M.J.; Barrett, D.A.; Kendall, D.A.; Scammell, B.E.; Reeve, A.J.; Chapman, V. Characterisation of the cannabinoid receptor system in synovial tissue and fluid in patients with osteoarthritis and rheumatoid arthritis. Arthritis Res. 2008, 10, R43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sagar, D.R.; Staniaszek, L.E.; Okine, B.N.; Woodhams, S.; Norris, L.M.; Pearson, R.G.; Garle, M.J.; Alexander, S.P.; Bennett, A.J.; Barrett, D.A.; et al. Tonic modulation of spinal hyperexcitability by the endocannabinoid receptor system in a model of osteoarthritic pain. Arthritis Rheum. 2010, 62, 3666–3676. [Google Scholar] [CrossRef] [PubMed]
- Schuelert, N.; Johnson, M.P.; Oskins, J.L.; Jassal, K.; Chambers, M.G.; McDougall, J.J. Local application of the endocannabinoid hydrolysis inhibitor URB597 reduces nociception in spontaneous and chemically induced models of osteoarthritis. Pain 2011, 152, 975–981. [Google Scholar] [CrossRef] [PubMed]
- Krustev, E.; Rioux, D.; McDougall, J.J. Mechanisms and mediators that drive arthritis pain. Curr. Osteoporos. Rep. 2015, 13, 216–224. [Google Scholar] [CrossRef] [PubMed]
- McDougall, J.J.; Muley, M.M.; Philpott, H.T.; Reid, A.; Krustev, E. Early blockade of joint inflammation with a fatty acid amide hydrolase inhibitor decreases end-stage osteoarthritis pain and peripheral neuropathy in mice. Arthritis Res. Ther. 2017, 19, 106. [Google Scholar] [CrossRef] [Green Version]
- Donvito, G.; Nass, S.R.; Wilkerson, J.L.; Curry, Z.A.; Schurman, L.D.; Kinsey, S.G.; Lichtman, A.H. The endogenous cannabinoid system: A budding source of targets for treating inflammatory and neuropathic pain. Neuropsychopharmacology 2018, 43, 52–79. [Google Scholar] [CrossRef] [Green Version]
- Gates, M.C.; Hinds, H.J.; Dale, A. Preliminary description of aging cats and dogs presented to a New Zealand first-opinion veterinary clinic at end-of-life. N. Z. Vet. J. 2017, 65, 313–317. [Google Scholar] [CrossRef]
- Chiu, K.W.; Hash, J.; Meyers, R.; Lascelles, B.D.X. The effect of spontaneous osteoarthritis on conditioned pain modulation in the canine model. Sci. Rep. 2020, 10, 1694. [Google Scholar] [CrossRef] [Green Version]
- Dadhaniya, P.; Patel, C.; Muchhara, J.; Bhadja, N.; Mathuria, N.; Vachhani, K.; Soni, M.G. Safety assessment of a solid lipid curcumin particle preparation: Acute and subchronic toxicity studies. Food Chem. Toxicol. 2011, 49, 1834–1842. [Google Scholar] [CrossRef]

| Time (h) | 0 | 1/2 | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|---|
| Vehicle | Mean | 14.5 | 14.2 | 10.5 ## | 7.9 # | 7.6 | 6.8 | 5.9 # | 5.6 |
| SEM | 0.07 | 0.13 | 0.06 | 0.11 | 0.12 | 0.21 | 0.24 | 0.22 | |
| Cur | Mean | 14.5 | 14.2 | 10.6 | 8.1 | 7.8 | 7.0 | 5.9 | 5.7 |
| SEM | 0.10 | 0.04 | 0.05 | 0.21 | 0.04 | 0.10 | 0.14 | 0.12 | |
| PGA | Mean | 14.2 | 14.1 | 10.0 | 7.7 | 7.4 | 7.4 | 8.0 * | 8.1 * |
| SEM | 0.07 | 0.06 | 0.06 | 0.09 | 0.11 | 0.10 | 0.20 | 0.18 | |
| PGA-Cur | Mean | 14.2 | 14.4 | 11.4 *°§ | 9.6 *°§ | 9.5 *°§ | 9.3 *°§ | 8.5 *° | 8.3 *° |
| SEM | 0.07 | 0.09 | 0.12 | 0.04 | 0.04 | 0.08 | 0.21 | 0.24 |
| Control | Vehicle | Cur | PGA | PGA-Cur | |
|---|---|---|---|---|---|
| N | 6 | 6 | 6 | 6 | 6 |
| Min | 0 | 4 | 3 | 2 | 2 |
| Median | 0 | 4 # | 3.5 | 3 | 2* |
| Max | 0 | 5 | 4 | 4 | 3 |
| Mean | 0 | 4.2 | 3.5 | 3.0 | 2.2 |
| SEM | 0 | 0.2 | 0.2 | 0.4 | 0.2 |
| Vehicle | Cur | PGA | PGA-Cur | |
|---|---|---|---|---|
| Day 7 | −35 ± 2.11 # | −34 ± 2.21 | −33 ± 2.26 | −26.5 ± 1.83 |
| Day 14 | −47 ± 2.38 # | −46.5 ± 2.48 | −40.5 ± 2.63 | −30.5 ± 1.89 *° |
| Day 21 | −56.5 ± 1.30 # | −52.5 ± 1.86 | −40 ± 2.11 *° | −31 ± 2.33 **°° |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gugliandolo, E.; Peritore, A.F.; Impellizzeri, D.; Cordaro, M.; Siracusa, R.; Fusco, R.; D’Amico, R.; Di Paola, R.; Schievano, C.; Cuzzocrea, S.; et al. Dietary Supplementation with Palmitoyl-Glucosamine Co-Micronized with Curcumin Relieves Osteoarthritis Pain and Benefits Joint Mobility. Animals 2020, 10, 1827. https://doi.org/10.3390/ani10101827
Gugliandolo E, Peritore AF, Impellizzeri D, Cordaro M, Siracusa R, Fusco R, D’Amico R, Di Paola R, Schievano C, Cuzzocrea S, et al. Dietary Supplementation with Palmitoyl-Glucosamine Co-Micronized with Curcumin Relieves Osteoarthritis Pain and Benefits Joint Mobility. Animals. 2020; 10(10):1827. https://doi.org/10.3390/ani10101827
Chicago/Turabian StyleGugliandolo, Enrico, Alessio Filippo Peritore, Daniela Impellizzeri, Marika Cordaro, Rosalba Siracusa, Roberta Fusco, Ramona D’Amico, Rosanna Di Paola, Carlo Schievano, Salvatore Cuzzocrea, and et al. 2020. "Dietary Supplementation with Palmitoyl-Glucosamine Co-Micronized with Curcumin Relieves Osteoarthritis Pain and Benefits Joint Mobility" Animals 10, no. 10: 1827. https://doi.org/10.3390/ani10101827
APA StyleGugliandolo, E., Peritore, A. F., Impellizzeri, D., Cordaro, M., Siracusa, R., Fusco, R., D’Amico, R., Di Paola, R., Schievano, C., Cuzzocrea, S., & Crupi, R. (2020). Dietary Supplementation with Palmitoyl-Glucosamine Co-Micronized with Curcumin Relieves Osteoarthritis Pain and Benefits Joint Mobility. Animals, 10(10), 1827. https://doi.org/10.3390/ani10101827











