Role of Circulating Immune Complexes in the Pathogenesis of Canine Leishmaniasis: New Players in Vaccine Development
Abstract
1. Introduction
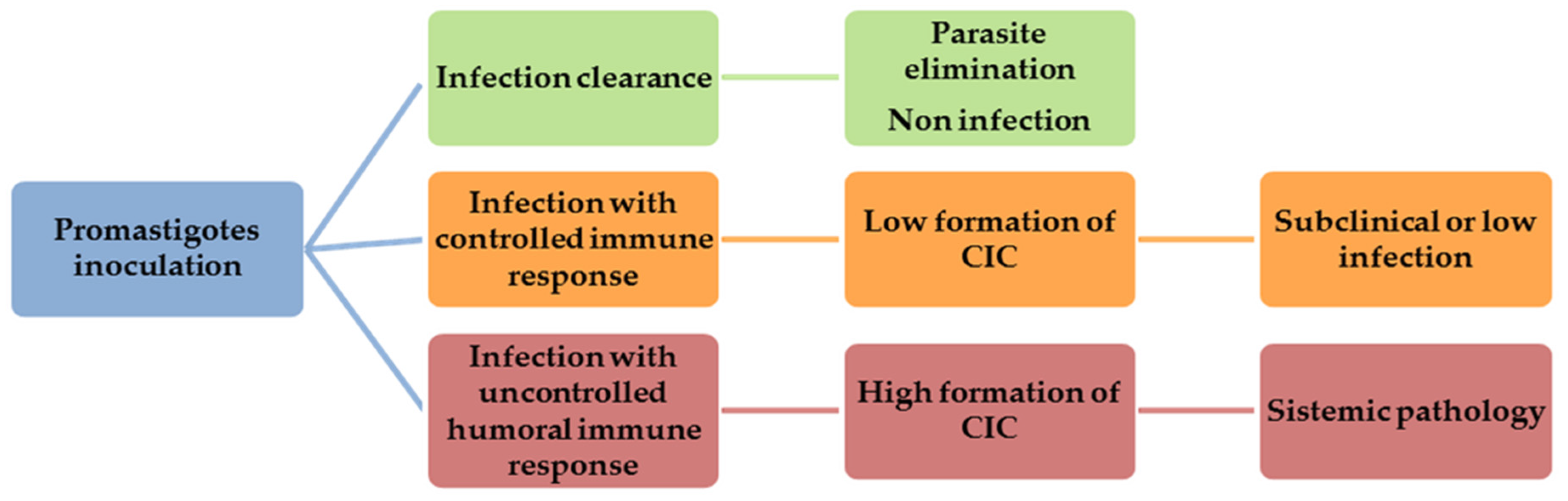
2. Role of CIC in CanL
3. Relationship between CIC Levels and Severity of CanL
4. CIC as Biomarkers for Measuring CanL Progression
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Adamama-Moraitou, K.K.; Rallis, T.S.; Koytinas, A.F.; Tontis, D.; Plevraki, K.; Kritsepi, M. Asymptomatic colitis in naturally infected dogs with Leishmania infantum: A prospective study. Am. J. Trop. Med. Hyg. 2007, 76, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Dantas-Torres, F.; Chomel, B.B.; Otranto, D. Ticks and tick-borne diseases: A One Health perspective. Trends Parasitol. 2012, 28, 437–446. [Google Scholar] [CrossRef]
- Dantas-Torres, F.; Solano-Gallego, L.; Baneth, G.; Ribeiro, V.M.; de Paiva-Cavalcanti, M.; Otranto, D. Canine leishmaniosis in the Old and New Worlds: Unveiled similarities and differences. Trends Parasitol. 2012, 28, 531–538. [Google Scholar] [CrossRef]
- Vilas, V.J.; Maia-Elkhoury, A.N.; Yadon, Z.E.; Cosivi, O.; Sanchez-Vazquez, M.J. Visceral leishmaniasis: A One Health approach. Vet. Rec. 2014, 175, 42–44. [Google Scholar] [CrossRef]
- Day, M.J. The immunopathology of canine vector-borne diseases. Parasit Vectors 2011, 4, 48. [Google Scholar] [CrossRef]
- Toepp, A.J.; Petersen, C.A. The balancing act: Immunology of leishmaniosis. Res. Vet. Sci. 2020, 130, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Abbehusen, M.M.C.; Almeida, V.D.A.; Solca, M.D.S.; Pereira, L.D.S.; Costa, D.J.; Gil-Santana, L.; Bozza, P.T.; Fraga, D.B.M.; Veras, P.S.T.; Dos-Santos, W.L.C.; et al. Clinical and immunopathological findings during long term follow-up in Leishmania infantum experimentally infected dogs. Sci. Rep. 2017, 7, 15914. [Google Scholar] [CrossRef] [PubMed]
- Alvar, J.; Canavate, C.; Molina, R.; Moreno, J.; Nieto, J. Canine leishmaniasis. Adv. Parasitol. 2004, 57, 1–88. [Google Scholar] [CrossRef]
- Guarga, J.L.; Moreno, J.; Lucientes, J.; Gracia, M.J.; Peribanez, M.A.; Alvar, J.; Castillo, J.A. Canine leishmaniasis transmission: Higher infectivity amongst naturally infected dogs to sand flies is associated with lower proportions of T helper cells. Res. Vet. Sci. 2000, 69, 249–253. [Google Scholar] [CrossRef]
- Pinelli, E.; Killick-Kendrick, R.; Wagenaar, J.; Bernadina, W.; del Real, G.; Ruitenberg, J. Cellular and humoral immune responses in dogs experimentally and naturally infected with Leishmania infantum. Infect. Immun. 1994, 62, 229–235. [Google Scholar] [CrossRef]
- Quinnell, R.J.; Courtenay, O.; Shaw, M.A.; Day, M.J.; Garcez, L.M.; Dye, C.; Kaye, P.M. Tissue cytokine responses in canine visceral leishmaniasis. J. Infect. Dis. 2001, 183, 1421–1424. [Google Scholar] [CrossRef][Green Version]
- Roura, X.; Cortadellas, O.; Day, M.J.; Benali, S.L.; Zatelli, A. Canine Leishmaniosis Working Group. Canine leishmaniosis and kidney disease: Q&A for an overall management in clinical practice. J. Small Anim. Pract. 2020. [Google Scholar] [CrossRef]
- Santos-Gomes, G.M.; Rosa, R.; Leandro, C.; Cortes, S.; Romao, P.; Silveira, H. Cytokine expression during the outcome of canine experimental infection by Leishmania infantum. Vet. Immunol. Immunopathol. 2002, 88, 21–30. [Google Scholar] [CrossRef]
- Gizzarelli, M.; Fiorentino, E.; Ben Fayala, N.E.H.; Montagnaro, S.; Torras, R.; Gradoni, L.; Oliva, G.; Foglia Manzillo, V. Assessment of circulating immune complexes during natural and experimental canine leishmaniasis. Front. Vet. Sci. 2020, 7, 273. [Google Scholar] [CrossRef]
- Parody, N.; Cacheiro-Llaguno, C.; Osuna, C.; Renshaw-Calderon, A.; Alonso, C.; Carnes, J. Circulating immune complexes levels correlate with the progression of canine leishmaniosis in naturally infected dogs. Vet. Parasitol. 2019, 274, 108921. [Google Scholar] [CrossRef]
- Miles, S.A.; Conrad, S.M.; Alves, R.G.; Jeronimo, S.M.; Mosser, D.M. A role for IgG immune complexes during infection with the intracellular pathogen Leishmania. J. Exp. Med. 2005, 201, 747–754. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.Y.; Wang, B.; Wen, Y.M. From therapeutic antibodies to immune complex vaccines. NPJ. Vaccines 2019, 4, 2. [Google Scholar] [CrossRef]
- Cacheiro-Llaguno, C.; Parody, N.; Renshaw-Calderon, A.; Osuna, C.; Alonso, C.; Carnes, J. Vaccination with LetiFend® reduces circulating immune complexes in dogs experimentally infected with L. infantum. Vaccine 2020, 38, 890–896. [Google Scholar] [CrossRef]
- Roura, X.; Fondati, A.; Lubas, G.; Gradoni, L.; Maroli, M.; Oliva, G.; Paltrinieri, S.; Zatelli, A.; Zini, E. Prognosis and monitoring of leishmaniasis in dogs: A working group report. Vet. J. 2013, 198, 43–47. [Google Scholar] [CrossRef]
- Solano-Gallego, L.; Miro, G.; Koutinas, A.; Cardoso, L.; Pennisi, M.G.; Ferrer, L.; Bourdeau, P.; Oliva, G.; Baneth, G. LeishVet guidelines for the practical management of canine leishmaniosis. Parasit Vectors 2011, 4, 86. [Google Scholar] [CrossRef]
- Solano-Gallego, L.; Koutinas, A.; Miró, G.; Cardoso, L.; Pennisi, M.G.; Ferrer, L.; Bourdeau, P.; Oliva, G.; Baneth, G. Directions for the diagnosis, clinical staging, treatment and prevention of canine leishmaniosis. Vet. Parasitol. 2009, 165, 1–18. [Google Scholar] [CrossRef]
- Maia, C.; Campino, L. Methods for diagnosis of canine leishmaniasis and immune response to infection. Vet. Parasitol. 2008, 158, 274–287. [Google Scholar] [CrossRef]
- Srivastava, P.; Dayama, A.; Mehrotra, S.; Sundar, S. Diagnosis of visceral leishmaniasis. Trans. R. Soc. Trop. Med. Hyg. 2011, 105, 1–6. [Google Scholar] [CrossRef]
- Nydegger, U.E. Immune complex pathophysiology. Ann. N. Y. Acad. Sci. 2007, 1109, 66–83. [Google Scholar] [CrossRef] [PubMed]
- Brachelente, C.; Muller, N.; Doherr, M.G.; Sattler, U.; Welle, M. Cutaneous leishmaniasis in naturally infected dogs is associated with a T helper-2-biased immune response. Vet. Pathol. 2005, 42, 166–175. [Google Scholar] [CrossRef]
- Chamizo, C.; Moreno, J.; Alvar, J. Semi-quantitative analysis of cytokine expression in asymptomatic canine leishmaniasis. Vet. Immunol. Immunopathol. 2005, 103, 67–75. [Google Scholar] [CrossRef]
- Costa, F.A.; Goto, H.; Saldanha, L.C.; Silva, S.M.; Sinhorini, I.L.; Silva, T.C.; Guerra, J.L. Histopathologic patterns of nephropathy in naturally acquired canine visceral leishmaniasis. Vet. Pathol. 2003, 40, 677–684. [Google Scholar] [CrossRef]
- Ordeix, L.; Solano-Gallego, L.; Fondevila, D.; Ferrer, L.; Fondati, A. Papular dermatitis due to Leishmania spp. infection in dogs with parasite-specific cellular immune responses. Vet. Dermatol. 2005, 16, 187–191. [Google Scholar] [CrossRef]
- Poli, A.; Abramo, F.; Mancianti, F.; Nigro, M.; Pieri, S.; Bionda, A. Renal involvement in canine leishmaniasis. A light-microscopic, immunohistochemical and electron-microscopic study. Nephron 1991, 57, 444–452. [Google Scholar] [CrossRef]
- Koutinas, A.F.; Koutinas, C.K. Pathologic mechanisms underlying the clinical findings in canine leishmaniasis due to Leishmania infantum/chagasi. Vet. Pathol. 2014, 51, 527–538. [Google Scholar] [CrossRef]
- Verroust, P. The search for circulating immune complex (IC) (author’s transl). Ann. Biol. Clin. (Paris) 1980, 38, 333–343. [Google Scholar]
- Rossi, M.; Fasel, N. How to master the host immune system? Leishmania parasites have the solutions! Int. Immunol. 2018, 30, 103–111. [Google Scholar] [CrossRef]
- Senbagavalli, P.; Hilda, J.N.; Ramanathan, V.D.; Kumaraswami, V.; Nutman, T.B.; Babu, S. Immune complexes isolated from patients with pulmonary tuberculosis modulate the activation and function of normal granulocytes. Clin. Vaccine Immunol. 2012, 19, 1965–1971. [Google Scholar] [CrossRef]
- AL-Fakhar, S.A. Circulating immune complexes in relation to polymorphonuclear leucocytes in patients infected with toxoplasmosis. Biomed. Pharmacol. J. 2017, 10. [Google Scholar] [CrossRef]
- Abrass, C.K.; Nies, K.M.; Louie, J.S.; Border, W.A.; Glassock, R.J. Correlation and predictive accuracy of circulating immune complexes with disease activity in patients with systemic lupus erythematosus. Arthritis Rheum. 1980, 23, 273–282. [Google Scholar] [CrossRef]
- Bernstein, K.A.; Kahl, L.E.; Balow, J.E.; Lefkowith, J.B. Serologic markers of lupus nephritis in patients: Use of a tissue-based ELISA and evidence for immunopathogenic heterogeneity. Clin. Exp. Immunol. 1994, 98, 60–65. [Google Scholar] [CrossRef]
- Nydegger, U.E.; Davis, J.S.t. Soluble immune complexes in human disease. CRC Crit. Rev. Clin. Lab. Sci. 1980, 12, 123–170. [Google Scholar] [CrossRef]
- Weissmann, G. Rheumatoid arthritis and systemic lupus erythematosus as immune complex diseases. Bull. NYU Hosp. Jt. Dis. 2009, 67, 251–253. [Google Scholar]
- Paganelli, R.; Levinsky, R.J.; Atherton, D.J. Detection of specific antigen within circulating immune complexes: Validation of the assay and its application to food antigen-antibody complexes formed in healthy and food-allergic subjects. Clin. Exp. Immunol. 1981, 46, 44–53. [Google Scholar]
- Park, H.S.; Nahm, D.H. Role of circulating immune complex in aspirin-sensitive asthma. Korean J. Intern. Med. 1998, 13, 51–55. [Google Scholar] [CrossRef]
- Parveen, S.; Taneja, N.; Bathi, R.J.; Deka, A.C. Evaluation of circulating immune complexes and serum immunoglobulins in oral cancer patients—A follow up study. Indian J. Dent. Res. 2010, 21, 10–15. [Google Scholar] [CrossRef]
- Urbaniak-Kujda, D. Circulating immune complexes as markers of Hodgkin’s disease activity. Pol. Tyg. Lek. 1996, 51, 303–304. [Google Scholar]
- Koraka, P.; Burghoorn-Maas, C.P.; Falconar, A.; Setiati, T.E.; Djamiatun, K.; Groen, J.; Osterhaus, A.D. Detection of immune-complex-dissociated nonstructural-1 antigen in patients with acute dengue virus infections. J. Clin. Microbiol. 2003, 41, 4154–4159. [Google Scholar] [CrossRef]
- Miles, S.A.; Balden, E.; Magpantay, L.; Wei, L.; Leiblein, A.; Hofheinz, D.; Toedter, G.; Stiehm, E.R.; Bryson, Y. Rapid serologic testing with immune-complex-dissociated HIV p24 antigen for early detection of HIV infection in neonates. Southern California Pediatric AIDS Consortium. N. Engl. J. Med. 1993, 328, 297–302. [Google Scholar] [CrossRef]
- Sengupta, K.; Ghosh, P.K.; Ganguly, S.; Das, P.; Maitra, T.K.; Jalan, K.N. Characterization of entamoeba histolytica antigens in circulating immune complexes in sera of patients with amoebiasis. J. Health Popul. Nutr. 2002, 20, 215–222. [Google Scholar] [PubMed]
- Soares, M.J.V.; Moraes, J.R.E.; Moraes, F.R. Renal involvement in canine leishmaniasis: A morphological and immunohistochemical study. Arq. Bras. Med. Vet. Zootec. 2009, 61, 785–790. [Google Scholar] [CrossRef]
- DE Brito, T.; Hoshino-Shimizu, S.; Neto, V.A.; Duarte, I.S.; Penna, D.O. Glomerular involvement in human kala-azar. A light, immunofluorescent, and electron microscopic study based on kidney biopsies. Am. J. Trop. Med. Hyg. 1975, 24, 9–18. [Google Scholar] [CrossRef]
- Harrus, S.; Day, M.J.; Waner, T.; Bark, H. Presence of immune-complexes, and absence of antinuclear antibodies, in sera of dogs naturally and experimentally infected with Ehrlichia canis. Vet. Microbiol. 2001, 83, 343–349. [Google Scholar] [CrossRef]
- Matsumura, K.; Kazuta, Y.; Endo, R.; Tanaka, K.; Inoue, T. Detection of circulating immune complexes in the sera of dogs infected with Dirofilaria immitis, by Clq-binding enzyme-linked immunosorbent assay. J. Helminthol. 1986, 60, 239–243. [Google Scholar] [CrossRef]
- Elshafie, A.I.; Ahlin, E.; Mathsson, L.; ElGhazali, G.; Ronnelid, J. Circulating immune complexes (IC) and IC-induced levels of GM-CSF are increased in sudanese patients with acute visceral Leishmania donovani infection undergoing sodium stibogluconate treatment: Implications for disease pathogenesis. J. Immunol. 2007, 178, 5383–5389. [Google Scholar] [CrossRef] [PubMed]
- Requena, J.M.; Soto, M.; Doria, M.D.; Alonso, C. Immune and clinical parameters associated with Leishmania infantum infection in the golden hamster model. Vet. Immunol. Immunopathol. 2000, 76, 269–281. [Google Scholar] [CrossRef]
- Al-Fakhar, S.A.; Ali, W.M.; Obaid, K.Y.; Mohammed, K.I.A.; Ali, S.H.M.; Mousa, J.M. Association of circulating immune complexes in the development of visceral leishmaniasis. Res. J. Pharm. Tech. 2020, 13, 3284–3288. [Google Scholar] [CrossRef]
- Clementi, A.; Battaglia, G.; Floris, M.; Castellino, P.; Ronco, C.; Cruz, D.N. Renal involvement in leishmaniasis: A review of the literature. NDT Plus 2011, 4, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Lopez, R.; Lucena, R.; Novales, M.; Ginel, P.J.; Martin, E.; Molleda, J.M. Circulating immune complexes and renal function in canine leishmaniasis. Zentralbl. Veterinarmed. B 1996, 43, 469–474. [Google Scholar] [CrossRef] [PubMed]
- Plevraki, K.; Koutinas, A.F.; Kaldrymidou, H.; Roumpies, N.; Papazoglou, L.G.; Saridomichelakis, M.N.; Savvas, I.; Leondides, L. Effects of allopurinol treatment on the progression of chronic nephritis in canine leishmaniosis (Leishmania infantum). J. Vet. Intern. Med. 2006, 20, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Datta, S.; Modak, D.; Sarkar, S.; Saha, B.; Mukhopadhyay, S. Identification and glycobiological characterization of circulating immune complexes in patients with visceral leishmaniasis and post kala azar dermal leishmaniasis. Indian J. Exp. Biol. 2015, 53, 321–328. [Google Scholar]
- Lux, A.; Yu, X.; Scanlan, C.N.; Nimmerjahn, F. Impact of immune complex size and glycosylation on IgG binding to human FcgammaRs. J. Immunol. 2013, 190, 4315–4323. [Google Scholar] [CrossRef] [PubMed]
- Grauer, G.F. Glomerulonephritis. Semin. Vet. Med. Surg. Small Anim. 1992, 7, 187–197. [Google Scholar] [PubMed]
- Brandonisio, O.; Carelli, G.; Altamura, M.; Varvara, B.; Ceci, L. Circulating immune complexes and autoantibodies in canine leishmaniasis. Parassitologia 1990, 32, 275–281. [Google Scholar]
- dos Santos, J.P.; Alves, L.C.; Ramos, R.A.; Pimentel Dde, S.; de Carvalho, G.A.; Monteiro, M.F.; Faustino, M.A. Histological changes and immunolabeling of Leishmania infantum in kidneys and urinary bladder of dogs. Rev. Bras. Parasitol. Vet. 2013, 22, 420–423. [Google Scholar] [CrossRef]
- Marcussen, N.; Vetner, M.; Kristensen, H.M. Interstitial nephritis and glomerulonephritis in visceral leishmaniasis in a dog. A case report. APMIS 1989, 97, 1137–1140. [Google Scholar] [CrossRef] [PubMed]
- Margarito, J.M.; Lucena, R.; Lopez, R.; Molleda, J.M.; Martin, E.; Ginel, P.J. Levels of IgM and IgA circulating immune complexes in dogs with leishmaniasis. Zentralbl. Veterinarmed. B 1998, 45, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Nieto, C.G.; Navarrete, I.; Habela, M.A.; Serrano, F.; Redondo, E. Pathological changes in kidneys of dogs with natural Leishmania infection. Vet. Parasitol. 1992, 45, 33–47. [Google Scholar] [CrossRef]
- Solano-Gallego, L.; Rodriguez, A.; Iniesta, L.; Arboix, M.; Portus, M.; Alberola, J. Detection of anti-Leishmania immunoglobulin G antibodies in urine specimens of dogs with leishmaniasis. Clin. Diagn. Lab. Immunol. 2003, 10, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Tafuri, W.L.; de Oliveira, M.R.; Melo, M.N. Canine visceral leishmaniosis: A remarkable histopathological picture of one case reported from Brazil. Vet. Parasitol. 2001, 96, 203–212. [Google Scholar] [CrossRef]
- Zatelli, A.; Borgarelli, M.; Santilli, R.; Bonfanti, U.; Nigrisoli, E.; Zanatta, R.; Tarducci, A.; Guarraci, A. Glomerular lesions in dogs infected with Leishmania organisms. Am. J. Vet. Res. 2003, 64, 558–561. [Google Scholar] [CrossRef] [PubMed]
- Aresu, L.; Valenza, F.; Ferroglio, E.; Pregel, P.; Uslenghi, F.; Tarducci, A.; Zanatta, R. Membranoproliferative glomerulonephritis type III in a simultaneous infection of Leishmania infantum and Dirofilaria immitis in a dog. J. Vet. Diagn. Investig. 2007, 19, 569–572. [Google Scholar] [CrossRef]
- Costa, F.A.; Guerra, J.L.; Silva, S.M.; Klein, R.P.; Mendonca, I.L.; Goto, H. CD4(+) T cells participate in the nephropathy of canine visceral leishmaniasis. Braz. J. Med. Biol. Res. 2000, 33, 1455–1458. [Google Scholar] [CrossRef][Green Version]
- Esch, K.J.; Schaut, R.G.; Lamb, I.M.; Clay, G.; Morais Lima, A.L.; do Nascimento, P.R.; Whitley, E.M.; Jeronimo, S.M.; Sutterwala, F.S.; Haynes, J.S.; et al. Activation of autophagy and nucleotide-binding domain leucine-rich repeat-containing-like receptor family, pyrin domain-containing 3 inflammasome during Leishmania infantum-associated glomerulonephritis. Am. J. Pathol. 2015, 185, 2105–2117. [Google Scholar] [CrossRef]
- Paltrinieri, S.; Solano-Gallego, L.; Fondati, A.; Lubas, G.; Gradoni, L.; Castagnaro, M.; Crotti, A.; Maroli, M.; Oliva, G.; Roura, X.; et al. Guidelines for diagnosis and clinical classification of leishmaniasis in dogs. J. Am. Vet. Med. Assoc. 2010, 236, 1184–1191. [Google Scholar] [CrossRef]
- Pierantozzi, M.; Roura, X.; Paltrinieri, S.; Poggi, M.; Zatelli, A. Variation of proteinuria in dogs with leishmaniasis treated with meglumine antimoniate and allopurinol: A retrospective study. J. Am. Anim. Hosp. Assoc. 2013, 49, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Proverbio, D.; Spada, E.; Bagnagatti de Giorgi, G.; Perego, R.; Valena, E. Relationship between Leishmania IFAT titer and clinicopathological manifestations (clinical score) in dogs. BioMed Res. Int. 2014, 2014, 412808. [Google Scholar] [CrossRef] [PubMed]
- Tafuri, W.L.; Michalick, M.S.; Dias, M.; Genaro, O.; Leite, V.H.; Barbosa, A.J.; Bambirra, E.A.; da Costa, C.A.; Melo, M.N.; Mayrink, W. Optical and electron microscopic study of the kidney of dogs naturally and experimentally infected with Leishmania (Leishmania) chagasi. Rev. Inst. Med. Trop. Sao Paulo 1989, 31, 139–145. [Google Scholar] [CrossRef]
- Filipe, V.; Hawe, A.; Jiskoot, W. Critical evaluation of Nanoparticle Tracking Analysis (NTA) by NanoSight for the measurement of nanoparticles and protein aggregates. Pharm. Res. 2010, 27, 796–810. [Google Scholar] [CrossRef]
- Korolevskaya, L.B.; Shmagel, K.V.; Shmagel, N.G.; Chereshnev, V.A. The size and composition of circulating immune complexes during HIV infection. Dokl. Biochem. Biophys. 2014, 457, 134–136. [Google Scholar] [CrossRef] [PubMed]
- Mannik, M. Physicochemical and functional relationships of immune complexes. J. Investig. Dermatol. 1980, 74, 333–338. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nangaku, M.; Couser, W.G. Mechanisms of immune-deposit formation and the mediation of immune renal injury. Clin. Exp. Nephrol. 2005, 9, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Pennisi, M.G. Leishmaniosis of companion animals in Europe: An update. Vet. Parasitol. 2015, 208, 35–47. [Google Scholar] [CrossRef]
- Hernández, L.; Montoya, A.; Checa, R.; Dado, D.; Gálvez, R.; Otranto, D.; Latrofa, M.S.; Baneth, G.; Miró, G. Course of experimental infection of canine leishmaniosis: Follow-up and utility of noninvasive diagnostic techniques. Vet. Parasitol. 2015, 207, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Giunchetti, R.C.; Silveira, P.; Resende, L.A.; Leite, J.C.; Melo-Junior, O.A.O.; Rodrigues-Alves, M.L.; Costa, L.M.; Lair, D.F.; Chaves, V.R.; Soares, I.D.S.; et al. Canine visceral leishmaniasis biomarkers and their employment in vaccines. Vet. Parasitol. 2019, 271, 87–97. [Google Scholar] [CrossRef]
- Muller, K.E.; Solberg, C.T.; Aoki, J.I.; Floeter-Winter, L.M.; Nerland, A.H. Developing a vaccine for leishmaniasis: How biology shapes policy. Tidsskr. Nor Laegeforen. 2018, 137. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Palatnik-de-Sousa, C.B.; Day, M.J. One Health: The global challenge of epidemic and endemic leishmaniasis. Parasit Vectors 2011, 4, 197. [Google Scholar] [CrossRef]
- Baharia, R.K.; Tandon, R.; Sahasrabuddhe, A.A.; Sundar, S.; Dube, A. Nucleosomal histone proteins of L. donovani: A combination of recombinant H2A, H2B, H3 and H4 proteins were highly immunogenic and offered optimum prophylactic efficacy against Leishmania challenge in hamsters. PLoS ONE 2014, 9, e97911. [Google Scholar] [CrossRef]
- Soto, M.; Requena, J.M.; Quijada, L.; Perez, M.J.; Nieto, C.G.; Guzman, F.; Patarroyo, M.E.; Alonso, C. Antigenicity of the Leishmania infantum histones H2B and H4 during canine viscerocutaneous leishmaniasis. Clin. Exp. Immunol. 1999, 115, 342–349. [Google Scholar] [CrossRef]
- Iborra, S.; Soto, M.; Carrion, J.; Alonso, C.; Requena, J.M. Vaccination with a plasmid DNA cocktail encoding the nucleosomal histones of Leishmania confers protection against murine cutaneous leishmaniosis. Vaccine 2004, 22, 3865–3876. [Google Scholar] [CrossRef] [PubMed]
- Soto, M.; Requena, J.M.; Quijada, L.; Garcia, M.; Guzman, F.; Patarroyo, M.E.; Alonso, C. Mapping of the linear antigenic determinants from the Leishmania infantum histone H2A recognized by sera from dogs with leishmaniasis. Immunol. Lett. 1995, 48, 209–214. [Google Scholar] [CrossRef]
- Iborra, S.; Soto, M.; Carrion, J.; Nieto, A.; Fernandez, E.; Alonso, C.; Requena, J.M. The Leishmania infantum acidic ribosomal protein P0 administered as a DNA vaccine confers protective immunity to Leishmania major infection in BALB/c mice. Infect. Immun. 2003, 71, 6562–6572. [Google Scholar] [CrossRef]
- Chang, K.P.; Reed, S.G.; McGwire, B.S.; Soong, L. Leishmania model for microbial virulence: The relevance of parasite multiplication and pathoantigenicity. Acta Trop. 2003, 85, 375–390. [Google Scholar] [CrossRef]
| Clinical Stages | Serology | CIC | Clinical Signs | Prognosis |
|---|---|---|---|---|
| Noninfected | Negative | Negative | Without clinical signs | Good |
| Infected asymptomatic | Negative | Negative | Without clinical signs | Good |
| Stage I (Mild disease) | Negative or low positive antibody levels | Low levels | Mild clinical signs such as peripheral lymphadenomegaly or papular dermatitis | Good-to-guarded |
| Stage II (Moderate disease) | Low to high positive antibody levels | Low to medium levels | Apart from the signs listed in stage I, may present: diffuse or symmetrical cutaneous lesions such as exfoliative dermatitis/onychogryphosis, ulcerations (planum nasale, footpads, bony prominences, mucocutaneous junctions), anorexia, weight loss, fever and epistaxis | Guarded-to-good |
| Stage III (Severe disease) | Medium to high positive antibody levels | Medium to high levels | Apart from the signs listed in stages I and II, may present signs related to CIC deposition: vasculitis, arthritis, uveitis and glomerulonephritis. | Guarded-to-poor |
| Stage IV (Very severe disease) | Medium to high positive antibody levels | Medium to high levels | Clinical signs listed in stage III and pulmonary thromboembolism or nephrotic syndrome and end-stage renal disease | Poor |
| Advantages of CIC Analysis in CanL |
|---|
| ✓ Noninvasive sampling |
| ✓ High CIC levels in the presence of compatible clinical signs and/or clinicopathological abnormalities are conclusive of clinical leishmaniasis |
| ✓ Biomarker associated to pathology |
| ✓ Prognostic value |
| ✓ Useful tool to monitor the treatment and vaccine efficacy |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cacheiro-Llaguno, C.; Parody, N.; Escutia, M.R.; Carnés, J. Role of Circulating Immune Complexes in the Pathogenesis of Canine Leishmaniasis: New Players in Vaccine Development. Microorganisms 2021, 9, 712. https://doi.org/10.3390/microorganisms9040712
Cacheiro-Llaguno C, Parody N, Escutia MR, Carnés J. Role of Circulating Immune Complexes in the Pathogenesis of Canine Leishmaniasis: New Players in Vaccine Development. Microorganisms. 2021; 9(4):712. https://doi.org/10.3390/microorganisms9040712
Chicago/Turabian StyleCacheiro-Llaguno, Cristina, Nuria Parody, Marta R. Escutia, and Jerónimo Carnés. 2021. "Role of Circulating Immune Complexes in the Pathogenesis of Canine Leishmaniasis: New Players in Vaccine Development" Microorganisms 9, no. 4: 712. https://doi.org/10.3390/microorganisms9040712
APA StyleCacheiro-Llaguno, C., Parody, N., Escutia, M. R., & Carnés, J. (2021). Role of Circulating Immune Complexes in the Pathogenesis of Canine Leishmaniasis: New Players in Vaccine Development. Microorganisms, 9(4), 712. https://doi.org/10.3390/microorganisms9040712









