Modeling Native EHEC Outer Membrane Vesicles by Creating Synthetic Surrogates
Abstract
1. Introduction
2. Materials and Methods
2.1. Preparation of Protein-Loaded Vesicles
2.2. Cell Culture and Cytotoxicity Assay
3. Results
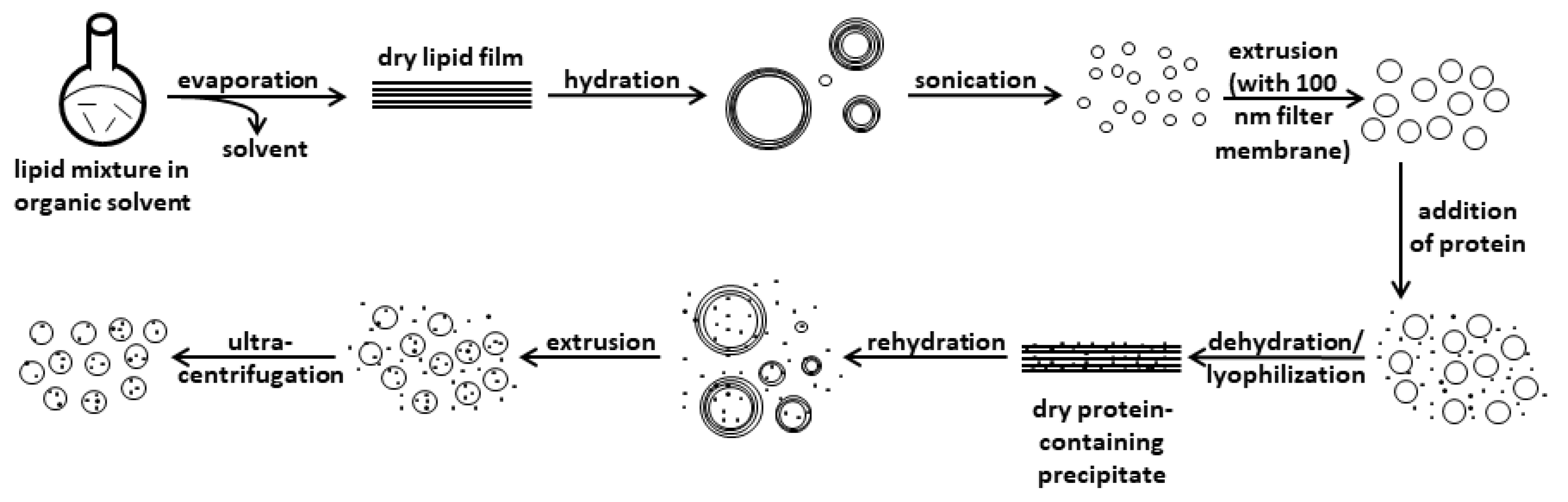
3.1. Developing a Protocol for the Preparation of sOMVs
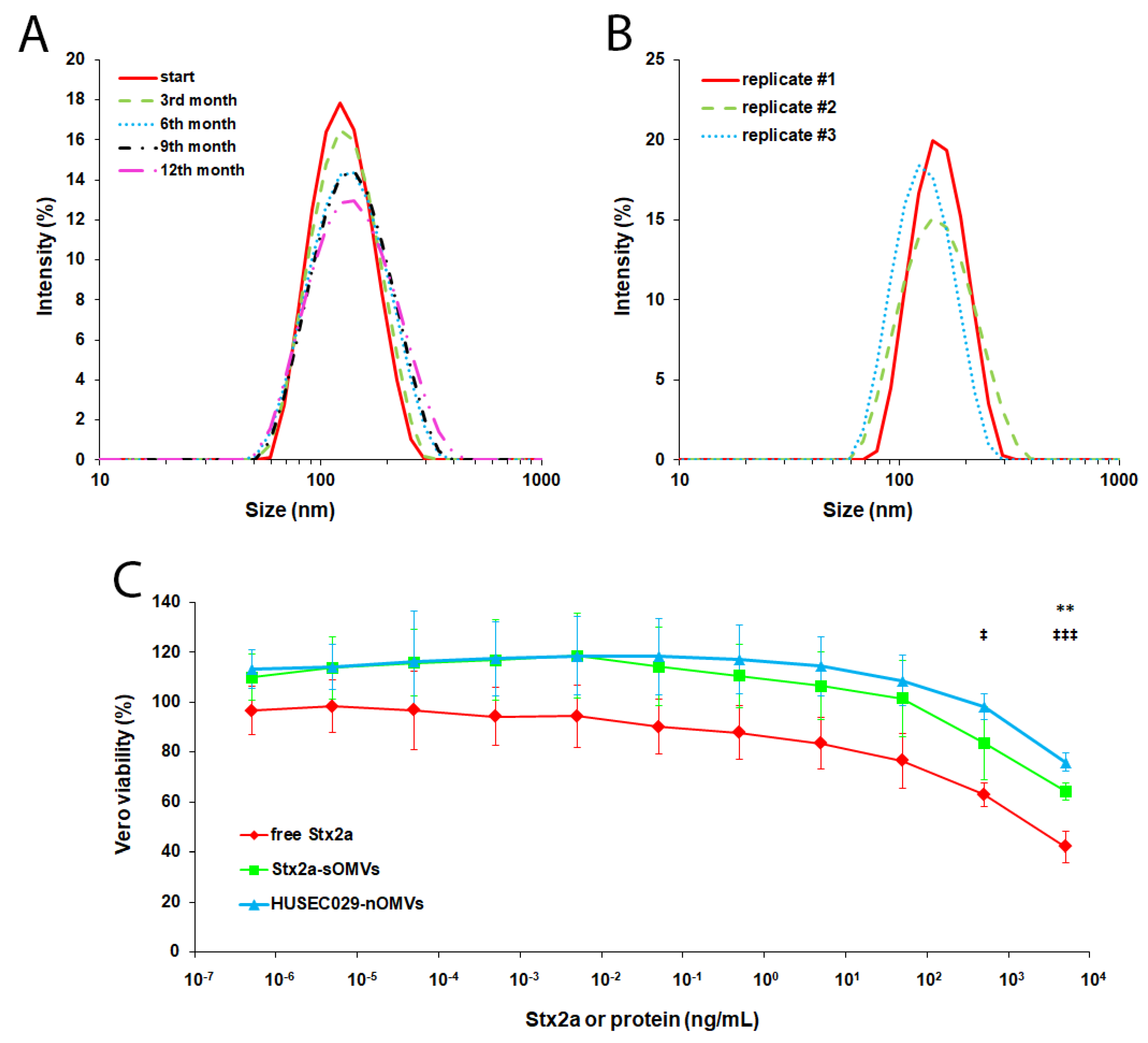
3.2. Defining Parameters for sOMV Preparation Using BSA as a Proxy
3.3. Preparing and Functionally Evaluating sOMVs Harboring Stx2a
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| CdtV | cytolethal distending toxin V |
| EHEC | enterohemorrhagic Escherichia coli |
| EHEC-Hly | EHEC hemolysin |
| nOMVs | native OMVs |
| OMVs | outer membrane vesicles |
| ShET1 | Shigella enterotoxin 1 |
| sOMVs | synthetic OMVs |
| STEC | Shiga-toxigenic Escherichia coli |
| Stx | Shiga toxin |
References
- Karch, H.; Tarr, P.I.; Bielaszewska, M. Enterohaemorrhagic Escherichia coli in human medicine. Int. J. Med. MicroBiol. 2005, 295, 405–418. [Google Scholar] [CrossRef] [PubMed]
- Tarr, P.I.; Gordon, C.A.; Chandler, W.L. Shiga-toxin-producing Escherichia coli and haemolytic uraemic syndrome. Lancet 2005, 365, 1073–1086. [Google Scholar] [CrossRef]
- Karpman, D.; Loos, S.; Tati, R.; Arvidsson, I. Haemolytic uraemic syndrome. J. Int. Med. 2017, 281, 123–148. [Google Scholar] [CrossRef] [PubMed]
- Bergan, J.; Dyve Lingelem, A.B.; Simm, R.; Skotland, T.; Sandvig, K. Shiga toxins. Toxicon 2012, 60, 1085–1107. [Google Scholar] [CrossRef] [PubMed]
- Johannes, L.; Römer, W. Shiga toxins--from cell biology to biomedical applications. Nat. Rev. MicroBiol. 2010, 8, 105–116. [Google Scholar] [CrossRef]
- Bauwens, A.; Betz, J.; Meisen, I.; Kemper, B.; Karch, H.; Müthing, J. Facing glycosphingolipid-Shiga toxin interaction: Dire straits for endothelial cells of the human vasculature. Cell Mol. Life Sci. 2013, 70, 425–457. [Google Scholar] [CrossRef]
- Trachtman, H.; Austin, C.; Lewinski, M.; Stahl, R.A. Renal and neurological involvement in typical Shiga toxin-associated HUS. Nat. Rev. Nephrol. 2012, 8, 658–669. [Google Scholar] [CrossRef]
- Kouzel, I.U.; Kehl, A.; Berger, P.; Liashkovich, I.; Steil, D.; Makalowski, W.; Suzuki, Y.; Pohlentz, G.; Karch, H.; Mellmann, A.; et al. RAB5A and TRAPPC6B are novel targets for Shiga toxin 2a inactivation in kidney epithelial cells. Sci. Rep. 2020, 10, 4945. [Google Scholar] [CrossRef]
- Kouzel, I.U.; Pohlentz, G.; Schmitz, J.S.; Steil, D.; Humpf, H.U.; Karch, H.; Müthing, J. Shiga toxin glycosphingolipid receptors in human Caco-2 and HCT-8 colon epithelial cell lines. Toxins 2017, 9, 338. [Google Scholar] [CrossRef]
- Betz, J.; Dorn, I.; Kouzel, I.U.; Bauwens, A.; Meisen, I.; Kemper, B.; Bielaszewska, M.; Mormann, M.; Weymann, L.; Sibrowski, W.; et al. Shiga toxin of enterohaemorrhagic Escherichia coli directly injures developing human erythrocytes. Cell MicroBiol. 2016, 18, 1339–1348. [Google Scholar] [CrossRef]
- Brigotti, M.; Alfieri, R.; Sestili, P.; Bonelli, M.; Petronini, P.G.; Guidarelli, A.; Barbieri, L.; Stirpe, F.; Sperti, S. Damage to nuclear DNA induced by Shiga toxin 1 and ricin in human endothelial cells. FASEB J. 2002, 16, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Ellis, T.N.; Kuehn, M.J. Virulence and immunomodulatory roles of bacterial outer membrane vesicles. MicroBiol. Mol. Biol. Rev. 2010, 74, 81–94. [Google Scholar] [CrossRef] [PubMed]
- Schwechheimer, C.; Kuehn, M.J. Outer-membrane vesicles from Gram-negative bacteria: Biogenesis and functions. Nat. Rev. MicroBiol. 2015, 13, 605–619. [Google Scholar] [CrossRef] [PubMed]
- Kolling, G.L.; Matthews, K.R. Export of virulence genes and Shiga toxin by membrane vesicles of Escherichia coli O157:H7. Appl. Env. MicroBiol. 1999, 65, 1843–1848. [Google Scholar] [CrossRef]
- Yokoyama, K.; Horii, T.; Yamashino, T.; Hashikawa, S.; Barua, S.; Hasegawa, T.; Watanabe, H.; Ohta, M. Production of Shiga toxin by Escherichia coli measured with reference to the membrane vesicle-associated toxins. Fems MicroBiol. Lett. 2000, 192, 139–144. [Google Scholar] [CrossRef]
- Mellmann, A.; Bielaszewska, M.; Kock, R.; Friedrich, A.W.; Fruth, A.; Middendorf, B.; Harmsen, D.; Schmidt, M.A.; Karch, H. Analysis of collection of hemolytic uremic syndrome-associated enterohemorrhagic Escherichia coli. Emerg. Infect. Dis. 2008, 14, 1287–1290. [Google Scholar] [CrossRef]
- Bielaszewska, M.; Rüter, C.; Kunsmann, L.; Greune, L.; Bauwens, A.; Zhang, W.; Kuczius, T.; Kim, K.S.; Mellmann, A.; Schmidt, M.A.; et al. Enterohemorrhagic Escherichia coli hemolysin employs outer membrane vesicles to target mitochondria and cause endothelial and epithelial apoptosis. PLoS Pathog. 2013, 9, e1003797. [Google Scholar] [CrossRef]
- Kunsmann, L.; Rüter, C.; Bauwens, A.; Greune, L.; Gluder, M.; Kemper, B.; Fruth, A.; Wai, S.N.; He, X.; Lloubes, R.; et al. Virulence from vesicles: Novel mechanisms of host cell injury by Escherichia coli O104:H4 outbreak strain. Sci. Rep. 2015, 5, 13252. [Google Scholar] [CrossRef]
- Bielaszewska, M.; Rüter, C.; Bauwens, A.; Greune, L.; Jarosch, K.A.; Steil, D.; Zhang, W.; He, X.; Lloubes, R.; Fruth, A.; et al. Host cell interactions of outer membrane vesicle-associated virulence factors of enterohemorrhagic Escherichia coli O157: Intracellular delivery, trafficking and mechanisms of cell injury. PLoS Pathog. 2017, 13, e1006159. [Google Scholar] [CrossRef]
- Guessous, F.; Marcinkiewicz, M.; Polanowska-Grabowska, R.; Kongkhum, S.; Heatherly, D.; Obrig, T.; Gear, A.R. Shiga toxin 2 and lipopolysaccharide induce human microvascular endothelial cells to release chemokines and factors that stimulate platelet function. Infect. Immun. 2005, 73, 8306–8316. [Google Scholar] [CrossRef]
- Jandhyala, D.M.; Rogers, T.J.; Kane, A.; Paton, A.W.; Paton, J.C.; Thorpe, C.M. Shiga toxin 2 and flagellin from Shiga-toxigenic Escherichia coli superinduce interleukin-8 through synergistic effects on host stress-activated protein kinase activation. Infect. Immun. 2010, 78, 2984–2994. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Cheng, Y.; Xiong, Y.; Ye, C.; Zheng, H.; Sun, H.; Zhao, H.; Ren, Z.; Xu, J. Enterohemorrhagic Escherichia coli specific enterohemolysin induced IL-1β in human macrophages and EHEC-induced IL-1β required activation of NLRP3 inflammasome. PLoS ONE 2012, 7, e50288. [Google Scholar] [CrossRef] [PubMed]
- Bielaszewska, M.; Marejkova, M.; Bauwens, A.; Kunsmann-Prokscha, L.; Mellmann, A.; Karch, H. Enterohemorrhagic Escherichia coli O157 outer membrane vesicles induce interleukin 8 production in human intestinal epithelial cells by signaling via Toll-like receptors TLR4 and TLR5 and activation of the nuclear factor NF-kappaB. Int. J. Med. MicroBiol. 2018, 308, 882–889. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, A.W.; Bielaszewska, M.; Zhang, W.L.; Pulz, M.; Kuczius, T.; Ammon, A.; Karch, H. Escherichia coli harboring Shiga toxin 2 gene variants: Frequency and association with clinical symptoms. J. Infect. Dis. 2002, 185, 74–84. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, R.C.; MacDonald, R.I.; Menco, B.P.; Takeshita, K.; Subbarao, N.K.; Hu, L.R. Small-volume extrusion apparatus for preparation of large, unilamellar vesicles. Biochim. Biophys. Acta 1991, 1061, 297–303. [Google Scholar] [CrossRef]
- Steil, D.; Pohlentz, G.; Legros, N.; Mormann, M.; Mellmann, A.; Karch, H.; Müthing, J. Combining mass spectrometry, surface acoustic wave interaction analysis, and cell viability assays for characterization of Shiga toxin subtypes of pathogenic Escherichia coli bacteria. Anal. Chem. 2018, 90, 8989–8997. [Google Scholar] [CrossRef]
- Detzner, J.; Steil, D.; Pohlentz, G.; Legros, N.; Humpf, H.U.; Mellmann, A.; Karch, H.; Müthing, J. Real-time interaction analysis of Shiga toxins and membrane microdomains of primary human brain microvascular endothelial cells. GlycoBiology 2020, 30, 174–185. [Google Scholar] [CrossRef]
- Smith, P.K.; Krohn, R.I.; Hermanson, G.T.; Mallia, A.K.; Gartner, F.H.; Provenzano, M.D.; Fujimoto, E.K.; Goeke, N.M.; Olson, B.J.; Klenk, D.C. Measurement of protein using bicinchoninic acid. Anal. BioChem. 1985, 150, 76–85. [Google Scholar] [CrossRef]
- Bauwens, A.; Bielaszewska, M.; Kemper, B.; Langehanenberg, P.; von Bally, G.; Reichelt, R.; Mulac, D.; Humpf, H.U.; Friedrich, A.W.; Kim, K.S.; et al. Differential cytotoxic actions of Shiga toxin 1 and Shiga toxin 2 on microvascular and macrovascular endothelial cells. Thromb. Haemost. 2011, 105, 515–528. [Google Scholar] [CrossRef]
- Walde, P.; Ichikawa, S. Enzymes inside lipid vesicles: Preparation, reactivity and applications. Biomol. Eng. 2001, 18, 143–177. [Google Scholar] [CrossRef]
- Antimisiaris, S.G. Preparation of DRV liposomes. Methods Mol. Biol. 2017, 1522, 23–47. [Google Scholar] [CrossRef] [PubMed]
- White, D.A.; Lennarz, W.J.; Schnaitman, C.A. Distribution of lipids in the wall and cytoplasmic membrane subfractions of the cell envelope of Escherichia coli. J. Bacteriol. 1972, 109, 686–690. [Google Scholar] [CrossRef] [PubMed]
- Lugtenberg, E.J.; Peters, R. Distribution of lipids in cytoplasmic and outer membranes of Escherichia coli K12. Biochim. Biophys. Acta 1976, 441, 38–47. [Google Scholar] [CrossRef]
- Zhang, H. Thin-film hydration followed by extrusion method for liposome preparation. Methods Mol. Biol. 2017, 1522, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Konowalchuk, J.; Speirs, J.I.; Stavric, S. Vero response to a cytotoxin of Escherichia coli. Infect. Immun. 1977, 18, 775–779. [Google Scholar] [CrossRef] [PubMed]
- Karmali, M.A.; Petric, M.; Lim, C.; Fleming, P.C.; Arbus, G.S.; Lior, H. The association between idiopathic hemolytic uremic syndrome and infection by verotoxin-producing Escherichia coli. J. Infect. Dis. 1985, 151, 775–782. [Google Scholar] [CrossRef]
- Naito, S.; Horino, A.; Komiya, T.; Fukuda, Y.; Takahashi, M.; Ami, Y.; Suzaki, Y.; Satoh, S.; Gondaira, F.; Sugiyama, J.; et al. Protection against verocytotoxin in mice induced by liposome-coupled verocytotoxin. Int. Arch. Allergy Immunol. 1997, 114, 293–297. [Google Scholar] [CrossRef]
- Fukuda, T.; Kimiya, T.; Takahashi, M.; Arakawa, Y.; Ami, Y.; Suzaki, Y.; Naito, S.; Horino, A.; Nagata, N.; Satoh, S.; et al. Induction of protection against oral infection with cytotoxin-producing Escherichia coli O157:H7 in mice by Shiga-like toxin-liposome conjugate. Int. Arch. Allergy Immunol. 1998, 116, 313–317. [Google Scholar] [CrossRef]
- Suzaki, Y.; Ami, Y.; Nagata, N.; Naito, S.; Kato, H.; Taneichi, M.; Takahashi, M.; Komiya, T.; Satoh, S.; Gondaira, F.; et al. Protection of monkeys against Shiga toxin induced by Shiga toxin-liposome conjugates. Int. Arch. Allergy Immunol. 2002, 127, 294–298. [Google Scholar] [CrossRef]
- Rodrigues-Jesus, M.J.; Fotoran, W.L.; Cardoso, R.M.; Araki, K.; Wunderlich, G.; Ferreira, L.C.S. Nano-multilamellar lipid vesicles (NMVs) enhance protective antibody responses against Shiga toxin (Stx2a) produced by enterohemorrhagic Escherichia coli strains (EHEC). Braz J. MicroBiol. 2019, 50, 67–77. [Google Scholar] [CrossRef]
- Lamblet, M.; Delord, B.; Johannes, L.; van Effenterre, D.; Bassereau, P. Key role of receptor density in colloid/cell specific interaction: A quantitative biomimetic study on giant vesicles. Eur. Phys. J. E Soft Matter 2008, 26, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Poirier, C.; van Effenterre, D.; Delord, B.; Johannes, L.; Roux, D. Specific adsorption of functionalized colloids at the surface of living cells: A quantitative kinetic analysis of the receptor-mediated binding. Biochim. Biophys. Acta 2008, 1778, 2450–2457. [Google Scholar] [CrossRef] [PubMed]
- Bouter, A.; Delord, B.; Dransart, E.; Poirier, C.; Johannes, L.; van Effenterre, D. Intracellular trafficking of Shiga-toxin-B-subunit-functionalized spherulites. Biol. Cell 2008, 100, 717–725. [Google Scholar] [CrossRef] [PubMed]
- Tana; Watarai, S.; Isogai, E.; Oguma, K. Induction of intestinal IgA and IgG antibodies preventing adhesion of verotoxin-producing Escherichia coli to Caco-2 cells by oral immunization with liposomes. Lett. Appl. MicroBiol. 2003, 36, 135–139. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kehl, A.; Kuhn, R.; Detzner, J.; Steil, D.; Müthing, J.; Karch, H.; Mellmann, A. Modeling Native EHEC Outer Membrane Vesicles by Creating Synthetic Surrogates. Microorganisms 2020, 8, 673. https://doi.org/10.3390/microorganisms8050673
Kehl A, Kuhn R, Detzner J, Steil D, Müthing J, Karch H, Mellmann A. Modeling Native EHEC Outer Membrane Vesicles by Creating Synthetic Surrogates. Microorganisms. 2020; 8(5):673. https://doi.org/10.3390/microorganisms8050673
Chicago/Turabian StyleKehl, Alexander, Ronja Kuhn, Johanna Detzner, Daniel Steil, Johannes Müthing, Helge Karch, and Alexander Mellmann. 2020. "Modeling Native EHEC Outer Membrane Vesicles by Creating Synthetic Surrogates" Microorganisms 8, no. 5: 673. https://doi.org/10.3390/microorganisms8050673
APA StyleKehl, A., Kuhn, R., Detzner, J., Steil, D., Müthing, J., Karch, H., & Mellmann, A. (2020). Modeling Native EHEC Outer Membrane Vesicles by Creating Synthetic Surrogates. Microorganisms, 8(5), 673. https://doi.org/10.3390/microorganisms8050673




