Spatio-Temporal Distribution of Acinetobacter baumannii in Germany—A Comprehensive Systematic Review of Studies on Resistance Development in Humans (2000–2018)
Abstract
1. Introduction
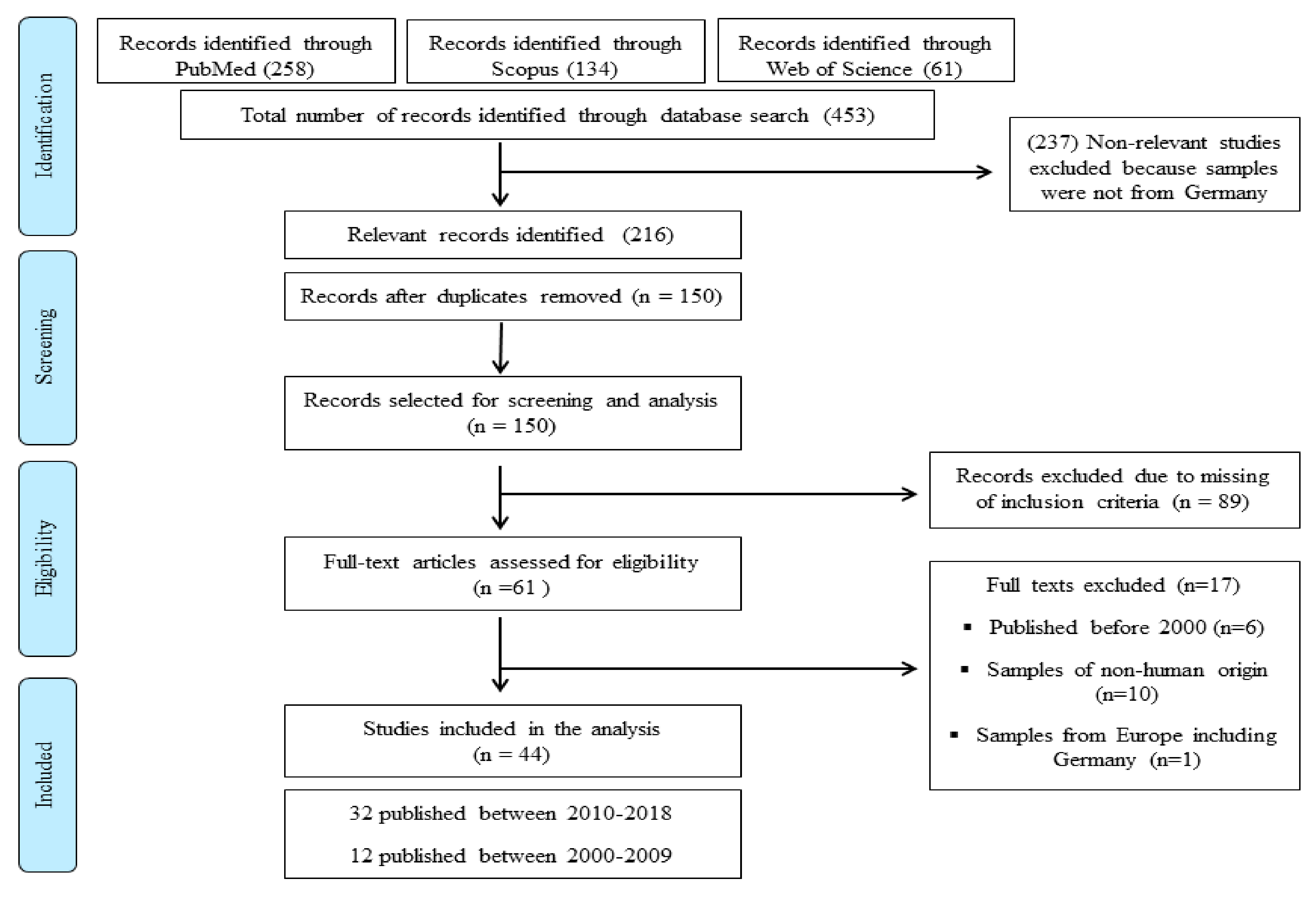
2. Materials and Methods
2.1. Data Sources and Search Strategy
2.2. Selection Criteria and Data Extraction
2.3. Data Acquisition and Analysis
2.4. Relative Research Interest
3. Results
3.1. Data Analysis
3.2. Temporal Distribution of the Analyzed Studies
3.3. Spatial Distribution of the Analyzed Studies Based on Geographical Location of Sampling
3.4. Official Data Concerning the Infection and Epidemiology of Acinetobacter in Germany
3.5. Identification of A. baumannii and Antibiotic Susceptibility Testing (AST)
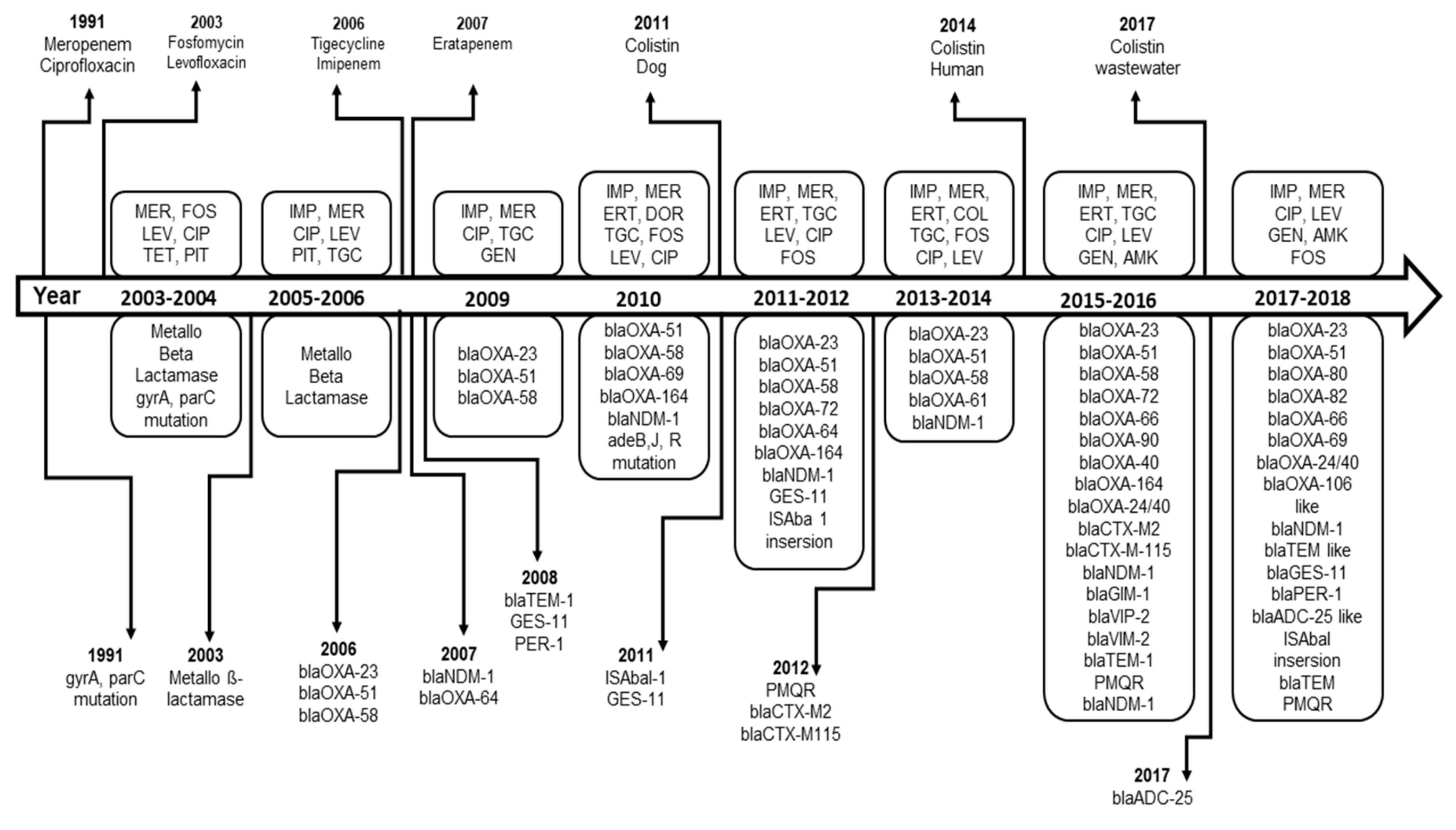
3.6. Resistance Development of A. baumannii
3.7. Resistance Genes in A. baumannii
3.8. Clonality and Sequence Typing
3.9. The Risk Factors Associated with A. baumannii Infections
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lin, M.F.; Lan, C.Y. Antimicrobial resistance in Acinetobacter baumannii: From bench to bedside. World J. Clin. Cases 2014, 2, 787–814. [Google Scholar] [CrossRef] [PubMed]
- Howard, A.; O'Donoghue, M.; Feeney, A.; Sleator, R.D. Acinetobacter baumannii: An emerging opportunistic pathogen. Virulence 2012, 3, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Antunes, L.C.; Visca, P.; Towner, K.J. Acinetobacter baumannii: Evolution of a global pathogen. Pathog. Dis. 2014, 71, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Yakkala, H.; Samantarrai, D.; Gribskov, M.; Siddavattam, D. Comparative genome analysis reveals niche-specific genome expansion in Acinetobacter baumannii strains. PLoS ONE 2019, 14, e0218204. [Google Scholar] [CrossRef] [PubMed]
- Doi, Y.; Murray, G.L.; Peleg, A.Y. Acinetobacter baumannii: Evolution of antimicrobial resistance-treatment options. Semin. Respir. Crit. Care Med. 2015, 36, 85–98. [Google Scholar] [CrossRef] [PubMed]
- Lupo, A.; Haenni, M.; Madec, J.Y. Antimicrobial resistance in Acinetobacter spp. and Pseudomonas spp. Microbiol. Spectr. 2018, 6, 377–393. [Google Scholar] [CrossRef]
- Pagano, M.; Martins, A.F.; Barth, A.L. Mobile genetic elements related to carbapenem resistance in Acinetobacter baumannii. Braz. J. Microbiol. 2016, 47, 785–792. [Google Scholar] [CrossRef]
- Rodloff, A.C.; Dowzicky, M.J. Antimicrobial susceptibility among European Gram-negative and Gram-positive isolates collected as part of the Tigecycline Evaluation and Surveillance Trial (2004–2014). Chemotherapy 2017, 62, 1–11. [Google Scholar] [CrossRef]
- Graser, Y.; Klare, I.; Halle, E.; Gantenberg, R.; Buchholz, P.; Jacobi, H.D.; Presber, W.; Schonian, G. Epidemiological study of an Acinetobacter baumannii outbreak by using polymerase chain reaction fingerprinting. J. Clin. Microbiol. 1993, 31, 2417–2420. [Google Scholar] [CrossRef]
- Seifert, H.; Baginski, R.; Schulze, A.; Pulverer, G. The distribution of Acinetobacter species in clinical culture materials. Zent. Bakteriol. Int. J. Med Microbiol. 1993, 279, 544–552. [Google Scholar] [CrossRef]
- Thurm, V.; Ritter, E. Genetic diversity and clonal relationships of Acinetobacter baumannii strains isolated in a neonatal ward: Epidemiological investigations by allozyme, whole-cell protein and antibiotic resistance analysis. Epidemiol. Infect. 1993, 111, 491–498. [Google Scholar] [CrossRef]
- Seifert, H.; Baginski, R. The clinical significance of Acinetobacter baumannii in blood cultures. Zent. Bakteriol. Int. J. Med Microbiol. 1992, 277, 210–218. [Google Scholar] [CrossRef]
- Wieland, K.; Chhatwal, P.; Vonberg, R.P. Nosocomial outbreaks caused by Acinetobacter baumannii and Pseudomonas aeruginosa: Results of a systematic review. Am. J. Infect. Control 2018, 46, 643–648. [Google Scholar] [CrossRef]
- Borgmann, S.; Wolz, C.; Grobner, S.; Autenrieth, I.B.; Heeg, P.; Goerke, C.; Muller, K.; Kyme, P.; Marschal, M. Metallo-beta-lactamase expressing multi-resistant Acinetobacter baumannii transmitted in the operation area. J. Hosp. Infect. 2004, 57, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Frickmann, H.; Crusius, S.; Walter, U.; Podbielski, A. Management eines Ausbruchs nosokomialer Pneumonien durch einen neuen multiresistenten Acinetobacter baumannii-Klon. Pneumologie 2010, 64, 686–693. [Google Scholar] [CrossRef] [PubMed]
- Kohlenberg, A.; Brummer, S.; Higgins, P.G.; Sohr, D.; Piening, B.C.; de Grahl, C.; Halle, E.; Ruden, H.; Seifert, H. Outbreak of carbapenem-resistant Acinetobacter baumannii carrying the carbapenemase OXA-23 in a German university medical centre. J. Med Microbiol. 2009, 58, 1499–1507. [Google Scholar] [CrossRef] [PubMed]
- Siemers, F.; Fanghanel, S.; Bergmann, P.A.; Tamouridis, G.; Stuttmann, R.; Stolze, B.; Hofmann, G.O. Management eines Ausbruches mit 4 MRGN Acinetobacter baumannii in einem Brandverletzten-zentrum. Handchir. Mikrochir. Plast. Chir. 2014, 46, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Wendel, A.F.; Malecki, M.; Otchwemah, R.; Tellez-Castillo, C.J.; Sakka, S.G.; Mattner, F. One-year molecular surveillance of carbapenem-susceptible A. baumannii on a German intensive care unit: Diversity or clonality. Antimicrob. Resist. Infect. Control 2018, 7, 145. [Google Scholar] [CrossRef]
- Gottig, S.; Gruber, T.M.; Higgins, P.G.; Wachsmuth, M.; Seifert, H.; Kempf, V.A. Detection of pan drug-resistant Acinetobacter baumannii in Germany. J. Antimicrob. Chemother. 2014, 69, 2578–2579. [Google Scholar] [CrossRef]
- Brandt, C.; Makarewicz, O.; Fischer, T.; Stein, C.; Pfeifer, Y.; Werner, G.; Pletz, M.W. The bigger picture: The history of antibiotics and antimicrobial resistance displayed by scientometric data. Int. J. Antimicrob. Agents 2014, 44, 424–430. [Google Scholar] [CrossRef]
- Katchanov, J.; Asar, L.; Klupp, E.M.; Both, A.; Rothe, C.; Konig, C.; Rohde, H.; Kluge, S.; Maurer, F.P. Carbapenem-resistant Gram-negative pathogens in a German university medical center: Prevalence, clinical implications and the role of novel beta-lactam/beta-lactamase inhibitor combinations. PLoS ONE 2018, 13, e0195757. [Google Scholar] [CrossRef]
- Kerz, T.; von Loewenich, F.D.; Roberts, J.; Neulen, A.; Ringel, F. Cerebrospinal fluid penetration of very high-dose meropenem: A case report. Ann. Clin. Microbiol. Antimicrob. 2018, 17, 47. [Google Scholar] [CrossRef]
- Papan, C.; Meyer-Buehn, M.; Laniado, G.; Huebner, J. Evaluation of the multiplex PCR based assay Unyvero implant and tissue infection application for pathogen and antibiotic resistance gene detection in children and neonates. Infection 2018, 47, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Lohr, B.; Pfeifer, Y.; Heudorf, U.; Rangger, C.; Norris, D.E.; Hunfeld, K.P. High prevalence of multidrug-resistant bacteria in Libyan War Casualties admitted to a tertiary care hospital, Germany. Microb. Drug Resist. 2018, 24, 578–584. [Google Scholar] [CrossRef] [PubMed]
- Tafelski, S.; Wagner, L.; Angermair, S.; Deja, M. Therapeutic drug monitoring for colistin therapy in severe multi-resistant Acinetobacter intracerebral abscess: A single case study with high-dose colistin and review of literature. SAGE Open Med Case Rep. 2017, 5, 2050313x17711630. [Google Scholar] [CrossRef] [PubMed]
- Rieber, H.; Frontzek, A.; Pfeifer, Y. Molecular investigation of carbapenem-resistant Acinetobacter spp. from hospitals in North Rhine-Westphalia, Germany. Microb. Drug Resist. 2017, 23, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Reinheimer, C.; Kempf, V.A.; Gottig, S.; Hogardt, M.; Wichelhaus, T.A.; O’Rourke, F.; Brandt, C. Multidrug-resistant organisms detected in refugee patients admitted to a University Hospital, Germany June to December 2015. Eurosurveillance 2016, 21, 30110. [Google Scholar] [CrossRef]
- Pfeifer, Y.; Hunfeld, K.P.; Borgmann, S.; Maneg, D.; Blobner, W.; Werner, G.; Higgins, P.G. Carbapenem-resistant Acinetobacter baumannii ST78 with OXA-72 carbapenemase and ESBL gene blaCTX-M-115. J. Antimicrob. Chemother. 2016, 71, 1426–1428. [Google Scholar] [CrossRef]
- Huenges, K.; Reinecke, A.; Bewig, B.; Haneya, A.; Cremer, J. Lung transplantation in a multidrug-resistant Gram-negative Acinetobacter baumannii-colonized aatient: A case report. Thorac. Cardiovasc. Surg. Rep. 2016, 5, 16–17. [Google Scholar] [CrossRef]
- Molter, G.; Seifert, H.; Mandraka, F.; Kasper, G.; Weidmann, B.; Hornei, B.; Ohler, M.; Schwimmbeck, P.; Kroschel, P.; Higgins, P.G.; et al. Outbreak of carbapenem-resistant Acinetobacter baumannii in the intensive care unit: A multi-level strategic management approach. J. Hosp. Infect. 2016, 92, 194–198. [Google Scholar] [CrossRef]
- Willems, S.; Kampmeier, S.; Bletz, S.; Kossow, A.; Kock, R.; Kipp, F.; Mellmann, A. Whole genome sequencing elucidates epidemiology of nosocomial clusters of Acinetobacter baumannii. J. Clin. Microbiol. 2016, 54, 2391–2394. [Google Scholar] [CrossRef] [PubMed]
- Ghebremedhin, B.; Halstenbach, A.; Smiljanic, M.; Kaase, M.; Ahmad-Nejad, P. MALDI-TOF MS based carbapenemase detection from culture isolates and from positive blood culture vials. Ann. Clin. Microbiol. Antimicrob. 2016, 15, 5. [Google Scholar] [CrossRef] [PubMed]
- Hischebeth, G.T.; Wimmer, M.D.; Molitor, E.; Seifert, H.; Gravius, S.; Bekeredjian-Ding, I. Multidrug resistant Acinetobacter baumannii reaches a new frontier: Prosthetic hip joint infection. Infection 2015, 43, 95–97. [Google Scholar] [CrossRef] [PubMed]
- Dersch, R.; Robinson, E.; Beume, L.; Rauer, S.; Niesen, W.D. Full remission in a patient with catheter-associated ventriculitis due to Acinetobacter baumannii treated with intrathecal and intravenous colistin besides coinfections with other multidrug-resistant bacteria. Neurol. Sci. 2015, 36, 633–634. [Google Scholar] [CrossRef]
- Leistner, R.; Denkel, L.A.; Gastmeier, P.; Werner, G.; Layer, F.; Pfeifer, Y. Prevalence of MRSA and Gram-negative bacteria with ESBLs and carbapenemases in patients from Northern Africa at a German hospital. J. Antimicrob. Chemother. 2015, 70, 3161–3164. [Google Scholar] [CrossRef]
- Hauri, A.M.; Kaase, M.; Hunfeld, K.P.; Heinmüller, P.; Imirzalioglu, C.; Wichelhaus, T.A.; Heudorf, U.; Bremer, J.; Wirtz, A. Meldepflicht für Carbapenem-resistente gramnegative Erreger: Eine Public Health-Priorität? Hyg. Med. 2015, 40, 26–35. [Google Scholar]
- Lahmer, T.; Messer, M.; Schnappauf, C.; Schmidt, A.; Schmid, R.M.; Huber, W. Acinetobacter baumannii sepsis is fatal in medical intensive care unit patients: Six cases and review of literature. Anaesth. Intensive Care 2014, 42, 666–668. [Google Scholar]
- Kleinkauf, N.; Hausemann, A.; Kempf, V.A.J.; Gottschalk, R.; Heudorf, U. Burden of carbapenem-resistant organisms in the Frankfurt/Main Metropolitan Area in Germany 2012/2013—First results and experiences after the introduction of legally mandated reporting. BMC Infect. Dis. 2014, 14, 446. [Google Scholar] [CrossRef]
- Schleicher, X.; Higgins, P.G.; Wisplinghoff, H.; Korber-Irrgang, B.; Kresken, M.; Seifert, H. Molecular epidemiology of Acinetobacter baumannii and Acinetobacter nosocomialis in Germany over a 5-year period (2005-2009). Clin. Microbiol. Infect. 2013, 19, 737–742. [Google Scholar] [CrossRef]
- Kaase, M. Carbapenemasen bei Acinetobacter baumannii: Molekulare epidemiologie in Deutschland und Hinweise zur Diagnostik. Hyg. Med. 2012, 37, 16–19. [Google Scholar]
- Kaase, M. Carbapenemasen bei gramnegativen Erregern in Deutschland. Daten des Nationalen Referenzzentrums fur gramnegative Krankenhauserreger. Bundesgesundheitsblatt Gesundh. Gesundh. 2012, 55, 1401–1404. [Google Scholar] [CrossRef] [PubMed]
- Pfeifer, Y.; Wilharm, G.; Zander, E.; Wichelhaus, T.A.; Gottig, S.; Hunfeld, K.P.; Seifert, H.; Witte, W.; Higgins, P.G. Molecular characterization of blaNDM-1 in an Acinetobacter baumannii strain isolated in Germany in 2007. J. Antimicrob. Chemother. 2011, 66, 1998–2001. [Google Scholar] [CrossRef] [PubMed]
- Wagner, J.A.; Nenoff, P.; Handrick, W.; Renner, R.; Simon, J.; Treudler, R. Nekrotisierende Fasziitis durch Acinetobacter baumannii: Ein Fallbericht. Hautarzt 2011, 62, 128–130. [Google Scholar] [CrossRef] [PubMed]
- Higgins, P.G.; Schneiders, T.; Hamprecht, A.; Seifert, H. In vivo selection of a missense mutation in adeR and conversion of the novel blaOXA-164 gene into blaOXA-58 in carbapenem-resistant Acinetobacter baumannii isolates from a hospitalized patient. Antimicrob. Agents Chemother. 2010, 54, 5021–5027. [Google Scholar] [CrossRef] [PubMed]
- Aivazova, V.; Kainer, F.; Friese, K.; Mylonas, I. Acinetobacter baumannii infection during pregnancy and puerperium. Arch. Gynecol. Obstet. 2010, 281, 171–174. [Google Scholar] [CrossRef] [PubMed]
- Wadl, M.; Heckenbach, K.; Noll, I.; Ziesing, S.; Pfister, W.; Beer, J.; Schubert, S.; Eckmanns, T. Increasing occurrence of multidrug-resistance in Acinetobacter baumannii isolates from four German University Hospitals, 2002–2006. Infection 2010, 38, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Gottig, S.; Pfeifer, Y.; Wichelhaus, T.A.; Zacharowski, K.; Bingold, T.; Averhoff, B.; Brandt, C.; Kempf, V.A. Global spread of New Delhi metallo-beta-lactamase 1. Lancet. Infect. Dis. 2010, 10, 828–829. [Google Scholar] [CrossRef]
- Pfeifer, Y. Zum Auftreten multiresistenter NDM-1-carbapenemase bildender Escherichia coli und Acinetobacter baumannii in Deutschland. Hyg. Med. 2010, 35, 326–327. [Google Scholar]
- Seifert, H.; Dowzicky, M.J. A longitudinal analysis of antimicrobial susceptibility in clinical institutions in Germany as part of the Tigecycline Evaluation and Surveillance Trial (2004–2007). Chemotherapy 2009, 55, 241–252. [Google Scholar] [CrossRef]
- Kresken, M.; Leitner, E.; Seifert, H.; Peters, G.; von Eiff, C. Susceptibility of clinical isolates of frequently encountered bacterial species to tigecycline one year after the introduction of this new class of antibiotics: Results of the second multicentre surveillance trial in Germany (G-TEST II, 2007). Eur. J. Clin. Microbiol. Infect. Dis. 2009, 28, 1007–1011. [Google Scholar] [CrossRef]
- Rodloff, A.C.; Leclercq, R.; Debbia, E.A.; Canton, R.; Oppenheim, B.A.; Dowzicky, M.J. Comparative analysis of antimicrobial susceptibility among organisms from France, Germany, Italy, Spain and the UK as part of the Tigecycline Evaluation and Surveillance Trial. Clin. Microbiol. Infect. 2008, 14, 307–314. [Google Scholar] [CrossRef]
- Weyrich, P.; Borgmann, S.; Mayer, F.; Heeg, P.; Riessen, R.; Kotter, I. Fatal multidrug-resistant Acinetobacter baumannii sepsis in a patient with travel history and recent onset of systemic lupus erythematosus: A case report. Int. J. Hyg. Environ. Health 2006, 209, 581–583. [Google Scholar] [CrossRef]
- Schulte, B.; Goerke, C.; Weyrich, P.; Grobner, S.; Bahrs, C.; Wolz, C.; Autenrieth, I.B.; Borgmann, S. Clonal spread of meropenem-resistant Acinetobacter baumannii strains in hospitals in the Mediterranean region and transmission to South-West Germany. J. Hosp. Infect. 2005, 61, 356–357. [Google Scholar] [CrossRef]
- Brauers, J.; Frank, U.; Kresken, M.; Rodloff, A.C.; Seifert, H. Activities of various beta-lactams and beta-lactam/beta-lactamase inhibitor combinations against Acinetobacter baumannii and Acinetobacter DNA group 3 strains. Clin. Microbiol. Infect. 2005, 11, 24–30. [Google Scholar] [CrossRef][Green Version]
- Higgins, P.G.; Wisplinghoff, H.; Stefanik, D.; Seifert, H. Selection of topoisomerase mutations and overexpression of adeB mRNA transcripts during an outbreak of Acinetobacter baumannii. J. Antimicrob. Chemother. 2004, 54, 821–823. [Google Scholar] [CrossRef]
- Frank, U.; Mutter, J.; Schmidt-Eisenlohr, E.; Daschner, F.D. Comparative in vitro activity of piperacillin, piperacillin-sulbactam and piperacillin-tazobactam against nosocomial pathogens isolated from intensive care patients. Clin. Microbiol. Infect. 2003, 9, 1128–1132. [Google Scholar] [CrossRef][Green Version]
- Andermahr, J.; Greb, A.; Hensler, T.; Helling, H.J.; Bouillon, B.; Sauerland, S.; Rehm, K.E.; Neugebauer, E. Pneumonia in multiple injured patients: A prospective controlled trial on early prediction using clinical and immunological parameters. Inflamm. Res. 2002, 51, 265–272. [Google Scholar] [CrossRef]
- Heinemann, B.; Wisplinghoff, H.; Edmond, M.; Seifert, H. Comparative activities of ciprofloxacin, clinafloxacin, gatifloxacin, gemifloxacin, levofloxacin, moxifloxacin and trovafloxacin against epidemiologically defined Acinetobacter baumannii strains. Antimicrob. Agents Chemother. 2000, 44, 2211–2213. [Google Scholar] [CrossRef]
- Robert Koch Institiute (RKI). Infection epidemiological yearbook (2006–2018). Available online: https://www.rki.de/DE/Content/Infekt/Jahrbuch/jahrbuch_node.html (accessed on 5 March 2020).
- Robert Koch Institiute (RKI). Infektionsepidemiologisches Jahrbuch meldepflichtiger Krankheiten für 2018. Reported cases of Acinetobacter infection or colonization with carbapenem insensitivity by category the case definition, Germany, 2017 and 2018. Available online: https://www.rki.de/DE/Content/Infekt/Jahrbuch/Jahrbuch_2018.pdf?__blob=publicationFile (accessed on 5 March 2020).
- Meyer, E.; Schwab, F.; Schroeren-Boersch, B.; Gastmeier, P. Dramatic increase of third-generation cephalosporin-resistant E. coli in German intensive care units: Secular trends in antibiotic drug use and bacterial resistance, 2001 to 2008. Crit. Care Lond. Engl. 2010, 14, R113. [Google Scholar] [CrossRef]
- Pfeifer, Y.; Cho, S.; Higgins, P.; Fahr, A.; Wichelhaus, T.; Hunfeld, K.; Martin, M.; Witte, W. Molecular characterisation and outbreak analysis of multidrug-resistant Acinetobacter baumannii from German hospitals. Clin. Microbiol. Infect. 2010, 6 (Suppl. S2), P797. [Google Scholar] [CrossRef]
- Zordan, S.; Prenger-Berninghoff, E.; Weiss, R.; van der Reijden, T.; van den Broek, P.; Baljer, G.; Dijkshoorn, L. Multidrug-resistant Acinetobacter baumannii in veterinary clinics, Germany. Emerg. Infect. Dis. 2011, 17, 1751–1754. [Google Scholar] [CrossRef]
- Hembach, N.; Schmid, F.; Alexander, J.; Hiller, C.; Rogall, E.T.; Schwartz, T. Occurrence of the mcr-1 colistin resistance gene and other clinically relevant antibiotic resistance genes in microbial populations at different municipal wastewater treatment plants in Germany. Front. Microbiol. 2017, 8, 1282. [Google Scholar] [CrossRef]
- Matuschek, E.; Ahman, J.; Webster, C.; Kahlmeter, G. Antimicrobial susceptibility testing of colistin—Evaluation of seven commercial MIC products against standard broth microdilution for Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa and Acinetobacter spp. Clin. Microbiol. Infect. 2018, 24, 865–870. [Google Scholar] [CrossRef]
- Fritzenwanker, M.; Imirzalioglu, C.; Herold, S.; Wagenlehner, F.M.; Zimmer, K.P.; Chakraborty, T. Treatment options for carbapenem-resistant Gram-negative infections. Dtsch. Arztebl. Int. 2018, 115, 345–352. [Google Scholar] [CrossRef]
- Valencia, R.; Arroyo, L.A.; Conde, M.; Aldana, J.M.; Torres, M.J.; Fernandez-Cuenca, F.; Garnacho-Montero, J.; Cisneros, J.M.; Ortiz, C.; Pachon, J.; et al. Nosocomial outbreak of infection with pan-drug-resistant Acinetobacter baumannii in a tertiary care university hospital. Infect. Control Hosp. Epidemiol. 2009, 30, 257–263. [Google Scholar] [CrossRef]
- Ballouz, T.; Aridi, J.; Afif, C.; Irani, J.; Lakis, C.; Nasreddine, R.; Azar, E. Risk Factors, Clinical presentation and outcome of Acinetobacter baumannii bacteremia. Front. Cell. Infect. Microbiol. 2017, 7, 156. [Google Scholar] [CrossRef]
- Wareth, G.; Neubauer, H.; Sprague, L.D. Acinetobacter baumannii—A neglected pathogen in veterinary and environmental health in Germany. Vet. Res. Commun. 2019, 43, 1–6. [Google Scholar] [CrossRef]
- Cho, G.S.; Li, B.; Rostalsky, A.; Fiedler, G.; Rosch, N.; Igbinosa, E.; Kabisch, J.; Bockelmann, W.; Hammer, P.; Huys, G.; et al. Diversity and antibiotic susceptibility of Acinetobacter strains from milk powder produced in Germany. Front. Microbiol. 2018, 9, 536. [Google Scholar] [CrossRef]
- Wilharm, G.; Skiebe, E.; Higgins, P.G.; Poppel, M.T.; Blaschke, U.; Leser, S.; Heider, C.; Heindorf, M.; Brauner, P.; Jackel, U.; et al. Relatedness of wildlife and livestock avian isolates of the nosocomial pathogen Acinetobacter baumannii to lineages spread in hospitals worldwide. Environ. Microbiol. 2017, 19, 4349–4364. [Google Scholar] [CrossRef]
- Klotz, P.; Higgins, P.G.; Schaubmar, A.R.; Failing, K.; Leidner, U.; Seifert, H.; Scheufen, S.; Semmler, T.; Ewers, C. Seasonal occurrence and carbapenem susceptibility of bovine Acinetobacter baumannii in Germany. Front. Microbiol. 2019, 10, 272. [Google Scholar] [CrossRef]
- Szabados, F.; Tix, H.; Anders, A.; Kaase, M.; Gatermann, S.G.; Geis, G. Evaluation of species-specific score cutoff values of routinely isolated clinically relevant bacteria using a direct smear preparation for matrix-assisted laser desorption/ionization time-of-flight mass spectrometry-based bacterial identification. Eur. J. Clin. Microbiol. Infect. Dis. 2012, 31, 1109–1119. [Google Scholar] [CrossRef]
- Osei Sekyere, J.; Govinden, U.; Bester, L.A.; Essack, S.Y. Colistin and tigecycline resistance in carbapenemase-producing Gram-negative bacteria: Emerging resistance mechanisms and detection methods. J. Appl. Microbiol. 2016, 121, 601–617. [Google Scholar] [CrossRef]
- Gil-Marques, M.L.; Moreno-Martinez, P.; Costas, C.; Pachon, J.; Blazquez, J.; McConnell, M.J. Peptidoglycan recycling contributes to intrinsic resistance to fosfomycin in Acinetobacter baumannii. J. Antimicrob. Chemother. 2018, 73, 2960–2968. [Google Scholar] [CrossRef]
- Remschmidt, C.; Schneider, S.; Meyer, E.; Schroeren-Boersch, B.; Gastmeier, P.; Schwab, F. Surveillance of antibiotic use and resistance in intensive care units (SARI). Dtsch. Arztebl. Int. 2017, 114, 858–865. [Google Scholar] [CrossRef]
- Scaife, W.; Young, H.K.; Paton, R.H.; Amyes, S.G. Transferable imipenem-resistance in Acinetobacter species from a clinical source. J. Antimicrob. Chemother. 1995, 36, 585–586. [Google Scholar] [CrossRef]
- Guerra, B.; Fischer, J.; Helmuth, R. An emerging public health problem: Acquired carbapenemase-producing microorganisms are present in food-producing animals, their environment, companion animals and wild birds. Vet. Microbiol. 2014, 171, 290–297. [Google Scholar] [CrossRef]
- Eigenbrod, T.; Reuter, S.; Gross, A.; Kocer, K.; Gunther, F.; Zimmermann, S.; Heeg, K.; Mutters, N.T.; Nurjadi, D. Molecular characterization of carbapenem-resistant Acinetobacter baumannii using WGS revealed missed transmission events in Germany from 2012-15. J. Antimicrob. Chemother. 2019, 74, 3473–3480. [Google Scholar] [CrossRef]
- Jones, C.L.; Clancy, M.; Honnold, C.; Singh, S.; Snesrud, E.; Onmus-Leone, F.; McGann, P.; Ong, A.C.; Kwak, Y.; Waterman, P.; et al. Fatal outbreak of an emerging clone of extensively drug-resistant Acinetobacter baumannii with enhanced virulence. Clin. Infect. Dis. 2015, 61, 145–154. [Google Scholar] [CrossRef]
- Higgins, P.G.; Dammhayn, C.; Hackel, M.; Seifert, H. Global spread of carbapenem-resistant Acinetobacter baumannii. J. Antimicrob. Chemother. 2010, 65, 233–238. [Google Scholar] [CrossRef]
- Wisplinghoff, H.; Hippler, C.; Bartual, S.G.; Haefs, C.; Stefanik, D.; Higgins, P.G.; Seifert, H. Molecular epidemiology of clinical Acinetobacter baumannii and Acinetobacter genomic species 13TU isolates using a multilocus sequencing typing scheme. Clin. Microbiol. Infect. 2008, 14, 708–715. [Google Scholar] [CrossRef]

| Ref | First Author | Yr. of Report | Sampling Date | Location of Sampling | Study Population | Sample Type | No. Of Strains/Cases | Type of Study |
|---|---|---|---|---|---|---|---|---|
| [21] | (Katchanov et al., 2018) | 2018 | Sep. 2015 till Aug. 2016 | Hamburg-Eppendorf, Hamburg | 119 Individual patients | Pneumonia and bloodstream infection | 18 patients | Retrospective analysis |
| [18] | (Wendel et al., 2018) | 2018 | Apr. 2017 till Mar. 2018 | Cologne, North Rhine-Westphalia | 44 Individual patients | Rectal and nose/throat swabs, tracheal secretion and patients environment | 43/48 isolates | Retrospective analysis |
| [22] | (Kerz et al., 2018) | 2018 | ND | Mainz, Rhineland-Palatinate | One patient | Blood culture and CSF | 1 case | Case report |
| [23] | (Papan et al., 2018) | 2018 | Feb. till Dec. 2015 | Munich, Bavaria | 29 Individual patients | Wound, skin abscess, burn, synovial and thoracic drainage | 1 isolate | Routine bacterial diagnosis |
| [24] | (Lohr et al., 2018) | 2018 | Aug. 2016 till Jan. 2017 | NMC, Frankfurt/Main, Hesse | 67 Libyan war victims | Rectal, nasopharyngeal and inguinal swabs and wounds | 15 isolates | Prevalence and investigation |
| [25] | (Tafelski et al., 2017) | 2017 | ND | Berlin, Berlin | 1 patient | Cranial wound | 1 isolate | Case report |
| [26] | (Rieber et al., 2017) | 2017 | Feb. 2008 till Jan. 2012 | North Rhine-Westphalia | 22/44 hospitals | Respiratory tract, wound, urine, vascular, joint, catheter, blood, intraoperative tissue, pharyngeal swabs | 79/1167 isolates | Investigation study |
| [27] | (Reinheimer et al., 2016) | 2016 | Jun. till Dec. 2015 | UHF, Frankfurt/Main, Hesse | 143 refugee, 1489 residents | Rectal swabs | 4 isolates | Investigation study |
| [28] | (Pfeifer et al., 2016) | 2016 | Jul. 2012 till Sep. 2013 | Hospitals in Hesse and Bavaria | 2 Russian patients | Intraoperative wound swab | 3 isolates | Case report |
| [29] | (Huenges et al., 2016) | 2016 | ND | Kiel, Schleswig-Holstein | 1 patient | Skin swab and urine | 1 case | Case report |
| [30] | (Molter et al., 2016) | 2016 | 7 Dec. 2011 till 24 Jan. 2012 | Leverkusen | Outbreak, 10 patients | Throat, groin, trachea | 10 cases | Outbreak investigation |
| [31] | (Willems et al., 2016) | 2016 | Oct. 2013 till Mar. 2014 | Muenster, North Rhine-Westphalia | 2 ICUs at UH | Skin, central intravenous catheter, respiratory samples | 32 isolates | Routine surveillance study |
| [32] | (Ghebremedhin et al., 2016) | 2016 | ND | UH Bochum and Wuppertal, North Rhine-Westphalia | Strain collection | Culture isolates from laboratories | 38 isolates | Diagnostic study |
| [33] | (Hischebeth et al., 2015) | 2015 | ND | UH Bonn, North Rhine-Westphalia | 1 patient | Hip joint infection | 1 isolate | Case report |
| [34] | (Dersch et al., 2015) | 2015 | ND | Freiburg, Baden-Württemberg | 1 patient | Catheter associated ventriculitis/CSF | 1 isolate | Case report |
| [35] | (Leistner et al., 2015) | 2015 | Jan. 2012 till Dec. 2013 | Berlin, Berlin | 213 Libyan patients | Rectal and nasal swabs | 4 cases | Prevalence and investigation |
| [36] | (Hauri et al., 2015) | 2015 | Jan. 2012 till Sep. 2014 | Hesse | Laboratories information | Notification cases | 185 complex | Data survey |
| [17] | (Siemers et al., 2014) | 2014 | 24 Dec. 2012 till 16 Jan. 2013 | Burn center in Halle (Saale), Saxony-Anhalt | Outbreak, 7 patients | Nasal and throat swabs, blood, skin and wounds | 7 cases | Outbreak investigation |
| [19] | (Gottig et al., 2014) | 2014 | Dec. 2013 | Frankfurt, Hesse | 1 patient | Skin and rectal swab | 1 PDR strain | Case report |
| [37] | (Lahmer et al., 2014) | 2014 | ND | Munich, Bavaria | Outbreak, 6 patients | Blood culture, bronchoalveolar lavage and ascites | 6 cases | Outbreak investigation |
| [38] | (Kleinkauf et al., 2014) | 2014 | Apr. 2012 till Mar. 2013 | Frankfurt/Main, Hesse | Health care facilities | Notification cases, mainly wound swabs | 28 cases | Descriptive analysis of data |
| [39] | (Schleicher et al., 2013) | 2013 | 2005, 2007 and 2009 | ND | 15 Diagnostic laboratories | Respiratory tract, wound, intra-abdominal, blood culture | 140 isolates | Surveillance study |
| [40] | (Kaase, 2012a) | 2012 | 2011 | multi-centric study, NRL for MDRGNB, Bochum | Strain collection | Respiratory, wound, urine and blood culture | 292 isolates | Surveillance study |
| [41] | (Kaase, 2012b) | 2012 | 2011 | Nationwide (16 States), NRL for MDRGNB, Bochum | Strain collection | ND | 287 isolates | Surveillance study |
| [42] | (Pfeifer et al., 2011) | 2011 | 2007 | ND | 1 patient | ND | 1 isolate 161/07 | Investigation study |
| [43] | (Wagner et al., 2011) | 2011 | ND | Leipzig, Saxony | 1 patient | Deep wound | 1 isolate | Case report |
| [44] | (Higgins et al., 2010) | 2010 | ND | Cologne UH, North Rhine-Westphalia | 1 patient | Respiratory, blood and bedsore | 33 isolates | Case report |
| [45] | (Aivazova et al., 2010) | 2010 | ND | LMU, Munich, Bavaria | 1 patient | Vaginal smear | 1 isolate | Case report |
| [46] | (Wadl et al., 2010) | 2010 | 2002 till 2006 | Thuringia, Baden-Wuerttemberg, Hesse, Lower Saxony, Saxony, Schleswig– Holstein | 4 from 6 University hospitals | Respiratory, blood, urine, non-specific | 1190 isolates | Retrospective and descriptive analysis of data |
| [47] | (Gottig et al., 2010) | 2010 | 2007 | UHF, Frankfurt, Hesse | 1 patient | Skin, tracheal secretion, vessels prosthesis and wound | ND | Case report |
| [15] | (Frickmann et al., 2010) | 2010 | ND | UH Rostock, Mecklenburg-Vorpommern | Outbreak, 7 patients | Medical devices, patient associated objectives, room equipment, urine, blood, testicular smear, lower respiratory, buccal swab, skin lesions | 13 isolates | Outbreak investigation |
| [48] | (Pfeifer, 2010) | 2010 | 2007 | South-Western Germany | Hospital | ND | Ten isolates | Case report |
| [49] | (Seifert and Dowzicky, 2009) | 2009 | 2004–2007 | Throug out Germany | 13 Centers | ND | 187 isolates | Evaluation of antibiotic activities |
| [50] | (Kresken et al., 2009) | 2009 | 2007 | Throug out Germany | 15 Centers | Peritoneal cavity, respiratory, blood, urine and wound | 117 isolates | Evaluation of antibiotic activities |
| [16] | (Kohlenberg et al., 2009) | 2009 | 18 Jun till 31 Aug. 2006 | ND | Outbreak, 39 patients | Wound, lower respiratory (one from each infusion pump, oxygen mask, hand of health care worker) | 39 isolates | Outbreak investigation |
| [51] | (Rodloff et al., 2008) | 2008 | Jan. 2004 till Aug. 2006 | Throug out Germany | 7 Medical centers | Blood, wound, skin, urine, respiratory | 86 isolates | Evaluation of antibiotic activities |
| [52] | (Weyrich et al., 2006) | 2006 | ND | UH, Tuebingen, Baden-Württemberg | 1 patient | Blood culture | 1 case | Case report |
| [53] | (Schulte et al., 2005) | 2005 | ND | South-Western Germany | 2 patients | Blood culture, excised tissue from fracture patella | 2 isolates | Case report |
| [54] | (Brauers et al., 2005) | 2005 | ND | Throug out Germany + HU in Cologne, Freiburg, Leipzig | 13 Laboratories | Blood culture, respiratory and urine | 395 isolates | Evaluation of antibiotic activities |
| [14] | (Borgmann et al., 2004) | 2004 | Feb. until Mar. 2003 | UH, Tuebingen, Baden-Württemberg | Outbreak, 14 patients | Wound, skin, respiratory | 250 isolates | Outbreak investigation |
| [55] | (Higgins et al., 2004b) | 2004 | 1991–1992 | Cologne, North Rhine-Westphalia | 2 Hospital outbreaks | Urine, blood culture | 34 cases | Outbreak investigation |
| [56] | (Frank et al., 2003) | 2003 | ND | Throug out Germany | 19 Laboratories | Urinary, respiratory tract, wound, blood | 51 isolates | Evaluation of antibiotic activities |
| [57] | (Andermahr et al., 2002) | 2002 | Jun. 1996 till Jun 2001 | Cologne, North Rhine-Westphalia | 266 patients | Tracheal aspirate | 41 cases | Routine bacterial diagnosis |
| [58] | (Heinemann et al., 2000) | 2000 | Jul. 1990 till Dec. 1998 | Cologne, North Rhine-Westphalia | Outbreaks and sporadic cases | Blood, urine, wound, tracheal secretion | 47 isolates | Evaluation of antibiotic activities |
| Year of Report | No. of Outbreaks | No. of Cases | No. of Deaths | No. of Infection | Incidence |
|---|---|---|---|---|---|
| 2018 | 5 | 18 | 5 | 784 | 0.9 |
| 2017 | 7 | 41 | 11 | 794 | 1.0 |
| 2016 | 10 | 38 | 8 | - | - |
| 2015 | 8 | 56 | 27 | - | - |
| 2014 | 6 | 29 | 1 | - | - |
| 2013 | 14 | 67 | 4 | - | - |
| 2012 | 13 | 86 | 9 | - | - |
| 2011 | - | - | - | - | - |
| 2010 | - | - | - | - | - |
| No. | References | Sampling Date | Resistant Antibiotics | Susceptible Antibiotics | Resistance Genes | ST/IC |
|---|---|---|---|---|---|---|
| [21] | (Katchanov et al., 2018) | Sep. 2015 till Aug. 2016 | MDR, carbapenem-resistant | Colistin in all tested ten isolates | Ten isolates carry blaOXA-23 | ND |
| [18] | (Wendel et al., 2018) | Apr. 2017 till Mar. 2018 | Two strains were carbapenem-resistant | Carbapenem-2.1. Historical glance on the situation in human | Cephalosporinase-encoding blaADC-25-like, blaOXA-106-like, blaOXA-51 | ND |
| [22] | (Kerz et al., 2018) | ND | Carbapenemase-producing (Meropenem > 32 mg/L) | Colistin < 1 mg/L | blaOXA-23 and blaNDM-1 | ND |
| [23] | (Papan et al., 2018) | Feb. till Dec. 2015 | One strain was carbapenem-resistant | ND | blaOXA-24/40 | ND |
| [24] | (Lohr et al., 2018) | Aug. 2016 till Jan. 2017 | Carbapenemase-producing | ND | blaOXA-23 (n = 9), blaNDM (n = 2), blaNDM+OXA-51-ISAbaI (n = 4), TEM and PMQR gene aac(6`)-Ib-cr | ND |
| [25] | (Tafelski et al., 2017) | ND | MDR, imipenem, meropenem ceftriaxone, amikacin, cotrimoxazole, fosfomycin, ciprofloxacin, levofloxacin. | Colistin < 0.5 mg/L and tobramycin | ND | ND |
| [26] | (Rieber et al., 2017) | Feb. 2008 till Jan. 2012 | ESBL, Carbapenem-resistant, ciprofloxacin and gentamicin | Polymyxin B | blaOXA-23 (n = 66), blaOXA-80 (n = 1), blaOXA-82 (n = 3), TEM-like (n = 62), GES-11 (n = 1), PER-1 (n = 1); blaOXA-51-like (OXA-51, OXA-66, OXA-69) | ND |
| [27] | (Reinheimer et al., 2016) | Jun. till Dec. 2015 | Three strains were carbapenem-resistant from refugee and one from residents | ND | blaOXA-23 and blaOXA-24 in refugee and blaOXA-51 in resident | IC-2 |
| [28] | (Pfeifer et al., 2016) | Jul. 2012 till Sep. 2013 | Penicillin/inhibitor combinations, cefepime, imipenem, meropenem, aminoglycosides (gentamicin, tobramycin and amikacin), fluoroquinolones (ciprofloxacin) and sulfamethoxazole/trimethoprim. | Colistin | blaOXA-40/24 related blaOXA-72, blaOXA-66, blaOXA-90, ESBL-blaCTX-M-2-like genes and blaCTX-M-115 | IC-2, IC-6, ST944/ST78 ST348/ST2 |
| [29] | (Huenges et al., 2016) | ND | 4MRGN-ab, intermediate to carbapenems | Colistin | ND | ND |
| [30] | (Molter et al., 2016) | 7 Dec. 2011 till 24 Jan. 2012 | Carbapenems, ciprofloxacin and tobramycin; variable to tigecycline (≤0.5 to 4 mg/L) and amikacin (4 to ≥ 64 mg/L). | Colistin (MIC 0.5–1 mg/L) | blaOXA-51-like and blaOXA-23-like | IC-2, ST195 and ST218 |
| [31] | (Willems et al., 2016) | Oct. 2013 till Mar. 2014 | MDR, piperacillin, 3rd/4th generation cephalosporins and fluoroquinolones | Carbapenems, imipenem and meropenem | ND | ND |
| [32] | (Ghebremedhin et al., 2016) | ND | Carbapenemase-producing | ND | blaOXA-23, blaOXA-40, blaOXA-58, blaOXA-72, blaOXA-164, blaNDM-1, GIM-1, VIP-2 and VIM-2 | ND |
| [33] | (Hischebeth et al., 2015) | ND | Carbapenemase-producing, meropenem (MIC ≥ 32 mg/L) and imipenem (MIC ≥ 32 mg/L), tobramycin (MIC ≥ 16 mg/L) gentamicin (MIC ≥ 16 mg/L) | Colistin only (MIC ≤ 0.5 mg/L) | blaOXA-23-like and blaOXA-51-like. | IC-2 |
| [34] | (Dersch et al., 2015) | ND | MDR | Colistin | ND | ND |
| [35] | (Leistner et al., 2015) | Jan. 2012 till Dec. 2013 | ESBL, Carbapenem-resistant, Imipenem and Meropenem (MIC ≥ 16 mg/L), Ertapenem (MIC ≥ 32 mg/L). | ND | blaOXA-23, TEM-1, GES-11; PMQR genes (aac(6´)1b-cr) | ND |
| [36] | (Hauri et al., 2015) | Jan. 2012 till Sep. 2014 | 4MRGN, acylureidopenicillins, 3rd/4th generation cephalosporins, carbapenems, fluoroquinolone. | ND | blaOXA-23 and blaNDM | ND |
| [17] | (Siemers et al., 2014) | 24 Dec. till 2012 to 16 Jan. 2013 | 4MRGN, acylureidopenicillins, 3rd/4th generation cephalosporins, carbapenems, fluoroquinolone. | Colistin | blaOXA-58 | ND |
| [19] | (Gottig et al., 2014) | Dec. 2013 | PDR, penicillins/β-lactamase inhibitors, extended-spectrum cephalosporins, carbapenems, tetracyclines, fluoroquinolones, aminoglycosides, folate pathway inhibitors and polymyxins, including colistin (MIC > 128 mg/L) and tigecycline (MIC > 8 mg/L), chloramphenicol and fosfomycin | Intermediately susceptible to minocycline (MIC 8 mg/L) | BlaOXA-23, blaOXA-51-like (blaOXA-61) | IC-2 |
| [37] | (Lahmer et al., 2014) | ND | MDR, Carbapenem-resistant | Tigecycline and colistin | ND | ND |
| [38] | (Kleinkauf et al., 2014) | Apr. 2012 till Mar. 2013 | Carbapenem-resistant | blaOXA-23-like and blaNDM-1 | ND | |
| [39] | (Schleicher et al., 2013) | 2005, 2007 and 2009 | Non-susceptible to carbapenem and imipenem | ND | blaOXA-58-like and blaOXA-23-like. | IC-2, IC-1, IC-4, IC-7 |
| [40] | (Kaase, 2012a) | 2011 | Carbapenem-resistant, imipenem and meropenem, | ND | blaOXA-23, blaOXA-72, blaOXA-58, blaOXA-164, NDM-1, ISAba1 insertion blaOXA-51 and GES-11 | ND |
| [41] | (Kaase, 2012b) | 2011 | Carbapenem-resistant, imipenem and meropenem, | ND | blaOXA-23, blaOXA-72, blaOXA-58, blaOXA-164, NDM-1, ISAba1 insertion blaOXA-51 and GES-11 | ND |
| [42] | (Pfeifer et al., 2011) | 2007 | MDR, imipenem and meropenem, ertapenem (MIC >32 mg/L), tigecycline (MIC1 mg/L) | Colistin (MIC 0.38 mg/L) | blaNDM-1 and blaOXA-64 | IC-7 |
| [43] | (Wagner et al., 2011) | ND | MDR, ampicillin + sulbactam, piperacillin + tazobactam, cefuroxime, cefotaxime, ceftriaxone, ceftazidime, aztreonam, ertapenem, amikacin, fosfomycin, levofloxacin, ciprofloxacin and moxifloxacin. | Imipenem and tobramycin | ND | ND |
| [44] | (Higgins et al., 2010) | ND | Cefepime, cefotaxime, cefoxitin, ceftazidime, ciprofloxacin, moxifloxacin, fosfomycin, gentamicin, piperacillin, piperacillin-tazobactam and ampicillin-sulbactam, imipenem, meropenem. Amikacin variable (MIC ≤ 2 and ≥ 32 mg/L), tigecycline variable (MIC 2 and ≥ 8 µg/mL). | Colistin (MIC ≤1 µg/mL) and tobramycin (MIC ≤ 1 µg/mL) | blaOXA-51-like (blaOXA-69), blaOXA-58-like variant (novel blaOXA-164 and blaOXA-58). adeB, adeJ, novel adeR mutation | IC-1 |
| [45] | (Aivazova et al., 2010) | ND | ND | Meropenem | ND | ND |
| [46] | (Wadl et al., 2010) | 2002 till 2006 | 66 are MDR, beta-lactams (piperacillin/ tazobactam), fluoroquinolones (ciprofloxacin, levofloxacin), cephalosporins (ceftazidime, cefepime), Aminoglycosides (tobramycin, gentamicin) and trimethoprim/ sulphamethoxazole combination cotrimoxazole. | Lowest resistance in carbapenems (meropenem, imipenem) and beta-lactams (ampicillin/sulbactam). | ND | ND |
| [47] | (Gottig et al., 2010) | 2007 | Carbapenems, fluoroquinolones, aminoglycosides, tigecycline, aztreonam, | Colistin (MIC ≤ 1 µg/mL) | blaNDM-1 | ND |
| [15] | (Frickmann et al., 2010) | ND | MDR (ampicillin-sulbactam, piperacillin-tazobactam, cefuroxime, cefotaxime, cefpodoxime, ceftazidime, imipenem, meropenem, ciprofloxacin, levofloxacin, gentamycin, tobramycin, tetracycline, trimethoprim-sulfamethoxazole, tigecycline, doripenem, cefepime, ertapenem, moxifloxacin, fosfomycin, aztreonam). | Colistin | ND | ST22, ST53 |
| [48] | (Pfeifer, 2010) | 2007 | MDR, carbapenems | Colistin (MIC 0.25 µg/mL) | blaNDM-1 | ND |
| [49] | (Seifert and Dowzicky, 2009) | 2004–2007 | Ampicillin and amoxicillin/clavulanic acid (MIC ≥ 64 µg/mL), ceftriaxone (MIC ≥ 128 µg/mL) and cefepime (MIC 32 µg/mL) | Tigecycline, amikacin and minocycline (MIC ≤1 µg/mL), imipenem, meropenem, levofloxacin, | ND | ND |
| [50] | (Kresken et al., 2009) | 2007 | Imipenem (11.1%), ciprofloxacin (27.4%), gentamycin (22.2%) | Tigecycline (MIC ≤ 0.25/1 µg/mL) | ND | ND |
| [16] | (Kohlenberg et al., 2009) | 18 Jun till 31 Aug. 2006 | Carbapenem-resistant, penicillins, cephalosporins, ciprofloxacin, gentamicin, tobramycin, tigecycline (4 mg/L), imipenem and meropenem (MIC ≥ 32 mg/L) | Colistin (MIC ≤ 0.5 mg/L) and amikacin (MIC 4–8 mg/L). Two isolates susceptible to imipenem | blaOXA-23-like, blaOXA-58-like intrinsic blaOXA-51 | IC-2 |
| [51] | (Rodloff et al., 2008) | Jan. 2004 till Aug. 2006 | ND | Tigecycline (MIC ≤ 1 mg/L), >80% for amikacin, cefepime, ceftazidime, imipenem (MIC 1 mg/L), levofloxacin, minocycline, piperacillin-tazobactam. | ND | ND |
| [52] | (Weyrich et al., 2006) | ND | MDR, penicillins, cephalosporins, aminoglycosides, fluoroquinolones, rifampicin, tetracyclines, oxazolidinones, macrolides and carbapenems (imipenem and imipenem/EDTA | Colistin | Metallo-ß-lactamase | ND |
| [53] | (Schulte et al., 2005) | ND | Carbapenems, meropenem, penicillins, cephalosporins, aminoglycosides, quinolones | ND | Metallo-ß-lactamase | ND |
| [54] | (Brauers et al., 2005) | ND | MIC ≥ 64 mg/L in amoxicillin-clavulanate combinations, piperacillin-tazobactam and cefotaxime | Ampicillin-sulbactam and piperacillin-sulbactam (MIC ≤ 0.06 mg/L), meropenem (MIC ≤ 1 mg/L) | ND | ND |
| [14] | (Borgmann et al., 2004) | Feb. until Mar. 2003 | MDR, gentamicin, aztreonam, piperacillin, piperacillin/ tazobactam, cefuroxime, cefotaxime, ceftazidime, cefepime, meropenem, tetracycline, levofloxacin, ciprofloxacin and fosfomycin | Tobramycin, amikacin and colistin | Metallo-ß-lactamase | ND |
| [55] | (Higgins et al., 2004b) | 1991–1992 | Ciprofloxacin, ofloxacin, meropenem, netilmicin, tetracycline, tobramycin, clarithromycin | ND | gyrA and parC mutation, up-regulation of adeB gene | ND |
| [56] | (Frank et al., 2003) | ND | ND | Piperacillin-sulbactam | ND | ND |
| [57] | (Andermahr et al., 2002) | Jun. 1996 till Jun 2001 | ND | ND | ND | ND |
| [58] | (Heinemann et al., 2000) | Jul. 1990 till Dec. 1998 | Novel quinolones superior to ciprofloxacin | Clinafloxacin most active | ND | ND |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wareth, G.; Brandt, C.; Sprague, L.D.; Neubauer, H.; Pletz, M.W. Spatio-Temporal Distribution of Acinetobacter baumannii in Germany—A Comprehensive Systematic Review of Studies on Resistance Development in Humans (2000–2018). Microorganisms 2020, 8, 375. https://doi.org/10.3390/microorganisms8030375
Wareth G, Brandt C, Sprague LD, Neubauer H, Pletz MW. Spatio-Temporal Distribution of Acinetobacter baumannii in Germany—A Comprehensive Systematic Review of Studies on Resistance Development in Humans (2000–2018). Microorganisms. 2020; 8(3):375. https://doi.org/10.3390/microorganisms8030375
Chicago/Turabian StyleWareth, Gamal, Christian Brandt, Lisa D. Sprague, Heinrich Neubauer, and Mathias W. Pletz. 2020. "Spatio-Temporal Distribution of Acinetobacter baumannii in Germany—A Comprehensive Systematic Review of Studies on Resistance Development in Humans (2000–2018)" Microorganisms 8, no. 3: 375. https://doi.org/10.3390/microorganisms8030375
APA StyleWareth, G., Brandt, C., Sprague, L. D., Neubauer, H., & Pletz, M. W. (2020). Spatio-Temporal Distribution of Acinetobacter baumannii in Germany—A Comprehensive Systematic Review of Studies on Resistance Development in Humans (2000–2018). Microorganisms, 8(3), 375. https://doi.org/10.3390/microorganisms8030375







