Er:YAG Laser Irradiation Reduces Microbial Viability When Used in Combination with Irrigation with Sodium Hypochlorite, Chlorhexidine, and Hydrogen Peroxide
Abstract
1. Introduction
2. Material and Methods
2.1. Culture Conditions
2.2. Laser Irradiation PARAMETERS
2.3. Study Groups
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Hajishengallis, G.; Liang, S.; Payne, M.A.; Hashimm, A.; Jotwani, R.; Eskan, M.A.; McIntosh, M.L.; Alsam, A.; Kirkwood, K.L.; Lambris, J.D.; et al. Low-abundance biofilm species orchestrates inflammatory periodontal disease through the commensal microbiota and complement. Cell Host Microbe 2011, 10, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Caton, G.J.; Armitage, G.; Berglundh, T.; Chapple, I.L.C.; Jepsen, S.; Kornman, S.K.; Mealey, L.B.; Papapanou, P.N.; Sanz, M.; Tonetti, S.M. A new classification scheme for periodontal and peri-implant diseases and conditions—Introduction and key changes from the 1999 classification. J. Clin. Periodontol. 2018, 45, S1–S8. [Google Scholar] [CrossRef] [PubMed]
- Socransky, S.; Haffajee, A.; Cugini, M.; Smith, C.; Kent, R.L. Microbial complexes in subgingival plaque. J. Clin. Periodontol. 1998, 25, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Signat, B.; Roques, C.; Poulet, P. Fusobacterium nucleatum in periodontal health and disease. Curr. Issues Mol. Biol. 2011, 13, 25–36. [Google Scholar]
- Ahn, S.H.; Song, J.E.; Kim, S.; Cho, S.H.; Lim, Y.K.; Kook, J.K.; Kook, M.S.; Lee, T.H. NOX1/2 activation in human gingival fibroblasts by Fusobacterium nucleatum facilitates attachment of Porphyromonas gingivalis. Arch. Microbiol. 2016, 198, 573–583. [Google Scholar] [CrossRef]
- Maeda, K.; Nagata, H.; Yamamoto, Y.; Tanaka, M.; Tanaka, J.; Minamino, N.; Shizukuishi, S. Glyceraldehyde-3-phosphate dehydrogenase of Streptococcus oralis functions as a coadhesin for Porphyromonas gingivalis major fimbriae. Infect. Immun. 2004, 72, 1341–1348. [Google Scholar] [CrossRef]
- Park, Y.; Simionato, M.; Sekiya, K.; Murakami, Y.; James, D.; Chen, W.; Hackett, M.; Yoshimura, F.; Demuth, D.; Lamont, R. Short fimbriae of Porphyromonas gingivalis and their role in coadhesion with Streptococcus gordonii. Infect. Immun. 2005, 3983–3989. [Google Scholar] [CrossRef]
- Hajishengallis, G.; Darveau, R.; Curtis, M. The keystone-pathogen hypothesis. Nat. Rev. Microbiol. 2012, 10, 717–725. [Google Scholar] [CrossRef]
- Adriaens, P.; Edwards, C.; De Boever, J.; Loesche, W. Ultrastructural observations on bacterial invasion in cementum and radicular dentin of periodontally diseased human teeth. J. Periodontol. 1988, 59, 493–503. [Google Scholar] [CrossRef]
- Smiley, C.J.; Tracy, S.L.; Abt, E.; Michalowicz, B.S.; John, M.T.; Gunsolley, J.; Cobb, C.M.; Rossmann, J.; Harrel, S.K.; Forrest, J.L.; et al. Evidence-based clinical practice guideline on the nonsurgical treatment of chronic periodontitis by means of scaling and root planing with or without adjuncts. J. Am. Dent. Assoc. 2015, 146, 525–535. [Google Scholar] [CrossRef]
- Rams, T.; Degener, J.; van Winkelhoff, A. Antibiotic resistance in human chronic periodontitis microbiota. J. Periodonto. 2014, 85, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Olsen, I. Biofilm-specific antibiotic tolerance and resistance. Eur. J. Clin. Microbiol. Infect. Dis. 2015, 34, 877–886. [Google Scholar] [CrossRef] [PubMed]
- Aoki, A.; Sasaki, K.; Watanabe, H.; Ishikawa, I. Lasers in non-surgical periodontal therapy. Periodontol 2000 2004, 36, 59–97. [Google Scholar] [CrossRef] [PubMed]
- Aoki, A.; Mizutani, K.; Takasaki, A.; Sasaki, K.; Nagai, S.; Schwarz, F.; Yoshida, I.; Eguro, T.; Zeredo, J.; Izumi, Y. Current status of clinical laser applications in periodontal therapy. Gen. Dent. 2008, 56, 674–687. [Google Scholar] [PubMed]
- Schwarz, F.; Aoki, A.; Becker, J.; Sculean, A. Laser application in non-surgical periodontal therapy: A systematic review. J. Clin. Periodontol. 2008, 35, 29–44. [Google Scholar] [CrossRef] [PubMed]
- Grzech-Lesniak, K. Making Use of Lasers in Periodontal Treatment: A New Gold Standard? Photomed. Laser Surg. 2017, 35, 513–514. [Google Scholar] [CrossRef]
- De Paula Eduardo, C.; De Freitas, P.M.; Esteves-Oliveira, M.; Aranha, A.C.; Ramalho, K.M.; Simões, A.; Bello-Silva, M.S.; Tunér, J. Laser phototherapy in the treatment of periodontal disease. A review. Lasers Med. Sci. 2010, 25, 781–792. [Google Scholar] [CrossRef]
- Raffetto, N. Lasers for initial periodontal therapy. Dent. Clin. North. Am. 2004, 48, 923–936. [Google Scholar] [CrossRef]
- Schwarz, F.; Aoki, A.; Sculean, A.; Becker, J. The impact of laser application on periodontal and peri-implant wound healing. Periodontol. 2000 2009, 51, 79–108. [Google Scholar] [CrossRef]
- Swider, K.; Dominiak, M.; Grzech-Leśniak, K.; Matys, J. Effect of Different Laser Wavelengths on Periodontopathogens in Peri-Implantitis: A Review of In Vivo Studies. Microorganisms 2019, 29, 7. [Google Scholar] [CrossRef]
- Matys, J.; Grzech-Leśniak, K.; Flieger, R.; Dominiak, M. Assessment of an impact of a diode laser mode with wavelength of 980 nm on a temperature rise measured by means of k-02 thermocouple: Preliminary results. Dent. Med. Probl. 2016, 53. [Google Scholar] [CrossRef]
- Matys, J.; Flieger, R.; Tenore, G.; Grzech-Leśniak, K.; Romeo, U.; Dominiak, M. Er:YAG laser, piezosurgery, and surgical drill for bone decortication during orthodontic mini-implant insertion: Primary stability analysis—an animal study. Lasers Med. Sci. 2018, 33, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Grzech-Lesniak, K.; Matys, J.; Jurczyszyn, K.; Ziółkowski, P.; Dominiak, M.; Brugnera Junior, A.; Romeo, U. Histological and thermometric examination of soft tissue de-epithelialization using digitally controlled Er:YAG laser handpiece: An ex vivo study, Photomed. Laser Surg. 2018, 36. [Google Scholar] [CrossRef] [PubMed]
- Grzech-Leśniak, K.; Gaspirc, B.; Sculean, A. Photodiagnosis and Photodynamic Therapy Clinical and microbiological effects of multiple applications of antibacterial photodynamic therapy in periodontal maintenance patients. A randomized controlled clinical study. Photodiagnosis Photodyn. Ther. 2019, 27, 44–50. [Google Scholar] [CrossRef]
- Grzech-Leśniak, K.; Sculean, A.; Gašpirc, B. Laser reduction of specific microorganisms in the periodontal pocket using Er:YAG and Nd:YAG lasers: A randomized controlled clinical study. Lasers Med. Sci. 2018, 33, 1461–1470. [Google Scholar] [CrossRef]
- Harris, D.M.; Nicholson, D.M.; McCarthy, D.; Yukna, R.A.; Reynolds, M.A.; Greenwell, H.; Finley, J.; McCawley, T.K.; Xenoudi, P.; Gregg, R.H. Change in clinical indices following laser or scalpel treatment for periodontitis: A split-mouth, randomized, multi-center trial. Lasers Dent. 2014, 8929, 89290G. [Google Scholar] [CrossRef]
- Grzech-Leśniak, K.; Matys, J.; Dominiak, M. Comparison of the clinical and microbiological effects of antibiotic therapy in periodontal pockets following laser treatment: An in vivo study. Adv. Clin. Exp. Med. 2018, 27, 1263–1270. [Google Scholar] [CrossRef]
- Almehdi, A.; Aoki, A.; Ichinose, S. Histological and SEM analysis of root cementum following irradiation with Er: YAG and CO2 lasers. Lasers Med. Sci. 2013, 28, 203–213. [Google Scholar] [CrossRef]
- Schwarz, F.; Sculean, A.; Berakdar, M.; Szathmari, L.; Georg, T. In Vivo and In Vitro Effects of an Er : YAG Laser, a GaAlAs Diode Laser, and Scaling and Root Planing on Periodontally Diseased Root Surfaces : A Comparative Histologic Study. Lasers Surg. Med. 2003, 366, 359–366. [Google Scholar] [CrossRef]
- Ting, C.C.; Fukuda, M.; Watanabe, T.; Sanaoka, A.; Mitani, A.; Noguchi, T. Morphological Alterations of Periodontal Pocket Epithelium Following Nd:YAG Laser Irradiation. Photomed. Laser Surg. 2014, 32, 649–657. [Google Scholar] [CrossRef]
- Niwano, Y.; Konno, K.; Matayoshi, T.; Nakamura, K. Oral mucosal irritation study in hamster to evaluate a therapeutic apparatus using hydrogen peroxide photolysis for periodontitis treatment. Regul. Toxicol. Pharmacol. 2017, 90, 206–213. [Google Scholar] [CrossRef] [PubMed]
- Kanno, T.; Nakamura, K.; Ishiyama, K.; Yamada, Y.; Shirato, M. Adjunctive antimicrobial chemotherapy based on hydrogen peroxide photolysis for non-surgical treatment of moderate to severe periodontitis : A randomized controlled trial. Sci. Rep. 2017, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Yi, T.; Shah, M.; Raulji, D.; Dave, D. Comparative Evaluation of Antimicrobial Efficacy of Coffee Extract and 0.2% Chlorhexidine Mouthwash on the Periodontal Pathogens Porphyromonas Gingivalis, Prevotella Intermedia, Fusobacterium Nucleatum and Aggregatibacter Actinomycetemcomitans: An In Vitr. Adv. Hum. Biol. 2016, 6, 99. [Google Scholar] [CrossRef]
- Wolff, L.; Bandt, C.; Pihlstrom, B.; Brayer, L. Phase contrast microscopic evaluation of subgingival plaque in combination with either conventional or antimicrobial home treatment of patients with periodontal inflammation. J. Periodontal. Res. 1982, 17, 537–540. [Google Scholar] [CrossRef]
- Kalkwarf, K.; Tussing, G.; Davis, M. Histologic evaluation of gingival curettage facilitated by sodium hypochlorite solution. J. Periodontol. 1982, 53, 63–70. [Google Scholar] [CrossRef]
- Perova, M.; Lopunova, Z.; Banchenko, G.; Petrosian, E. A clinico-morphological assessment of the efficacy of sodium hypochlorite in the combined therapy of periodontitis. Stomatol 1990, 69, 23–26. [Google Scholar]
- Gregg, R.; McCarthy, D. Laser ENAP for periodontal bone regeneration. Dent. Today. 1998, 17, 88–91. [Google Scholar]
- Mizutani, K.; Aoki, A.; Coluzzi, D.; Yukna, R.; Wang, C.Y.; Pavlic, V.; Izumi, Y. Lasers in minimally invasive periodontal and peri-implant therapy. Periodontol. 2000 2016, 71, 185–212. [Google Scholar] [CrossRef]
- Gaspirc, B.; Skaleric, U. Clinical Evaluation of Periodontal Surgical Treatment With an Er:YAG Laser: 5-Year Results. J. Periodontol. 2007, 78, 1864–1871. [Google Scholar] [CrossRef]
- Yaneva, B.; Firkova, E.; Karaslavova, E.; Romanos, G.E. Bactericidal effects of using a fiber-less Er : YAG laser system for treatment of moderate chronic periodontitis : Preliminary results. Quintessence Int. 2014, 45, 489–497. [Google Scholar] [CrossRef]
- Jorgensen, M.G.; Aalam, A.; Slots, J.; Angeles, L. Periodontal antimicrobials–finding the right solutions. Int Dent J. 2005, 55, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Pryor, W. Oxy-radicals and related species: their formation, lifetimes, and reaction. Annu. Rev. Physiol. 1986, 48, 657–667. [Google Scholar] [CrossRef]
- Akiyama, F.; Aoki, A.; Miura-Uchiyama, M.; Sasaki, K.M.; Ichinose, S.; Umeda, M.; Ishikawa, I. In vitro studies of the ablation mechanism of periodontopathic bacteria and decontamination effect on periodontally diseased root surfaces by erbium:yttrium-aluminum-garnet laser. Lasers Med Sci. 2011, 26, 193–204. [Google Scholar] [CrossRef] [PubMed]
- Ando, Y.; Aoki, A.; Watanabe, H. Bactericidal effect of erbium YAG laser on periodontopathic bacteria. Lasers Surg. Med. 1996, 19, 190–200. [Google Scholar] [CrossRef]
- Coffelt, D.W.; Cobb, C.M.; MacNeill, S.; Rapley, J.; Killoy, W. Determination of energy density threshold for laser ablation of bacteria. An in vitro study. J. Clin. Periodontol. 1997, 24, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kojima, T.; Shimada, K.; Iwasaki, H. Inhibitory effects of a super pulsed carbon dioxide laser at low energy density on periodontopathic bacteria and lipopolysaccharide in vitro. J. Periodontal. Res. 2005, 40, 469–473. [Google Scholar] [CrossRef]
- Rooney, J.; Midda, M. A laboratory investigation of the bactericidal effect of a NdYAG laser. Br. Dent. J. 1994, 176, 61–64. [Google Scholar] [CrossRef]
- Schoop, U.; Kluger, W.; Moritz, A.; Nedjelik, N.; Georgopoulos, A. Bactericidal effect of different laser systems in the deep layers of dentin. Lasers Surg. Med. 2004, 35, 111–116. [Google Scholar] [CrossRef]
- Mullarky, M.; Norris, C.; Goldberg, I. The efficacy of the CO2 laser in the sterilization of skin seeded with bacteria: survival at the skin surface and in the plume emissions. Laryngoscope 1985, 95, 186–187. [Google Scholar] [CrossRef]
- Moreira, A.L.; Novaes, A.B.; Grisi, M.F.; Taba, M.; Souza, S.L.; Palioto, D.B.; de Oliveira, P.G.; Casati, M.Z.; Casarin, R.C.; Messora, M.R. Antimicrobial Photodynamic Therapy as an Adjunct to Non-Surgical Treatment of Aggressive Periodontitis: A Split-Mouth Randomized Controlled Trial. J. Periodontol. 2014, 86, 376–386. [Google Scholar] [CrossRef]
- Krohn-Dale, I.; Boe, O.E.; Enersen, M.; Leknes, K.N. Er : YAG laser in the treatment of periodontal sites with recurring chronic inflammation : A 12-month randomized, controlled clinical trial. J. Clin. Periodontol. 2012, 39, 745–752. [Google Scholar] [CrossRef] [PubMed]
- Ramfjord, S.P.; Caffesse, R.G.; Morrison, E.C.; Hill, R.W.; Kerry, G.J.; Appleberry, E.A.; Nissle, R.R.; Stults, D.L. Four modalities of periodontal treatment compared over five years. J. Periodontal. Res. 2006, 22, 222–223. [Google Scholar] [CrossRef] [PubMed]
- Yan, M.; Liu, M.; Wang, M.; Yin, F.; Xia, H. The effects of Er:YAG on the treatment of peri-implantitis: A meta-analysis of randomized controlled trials. Lasers Med. Sci. 2015, 30, 1843–1853. [Google Scholar] [CrossRef] [PubMed]


| Untreated | Er:YAG | CHX 0.03% | Er:YAG + CHX | H2O2 0.5% | Er:YAG + H2O2 | NaOCl 0.5% | Er:YAG + NaOCl | |
|---|---|---|---|---|---|---|---|---|
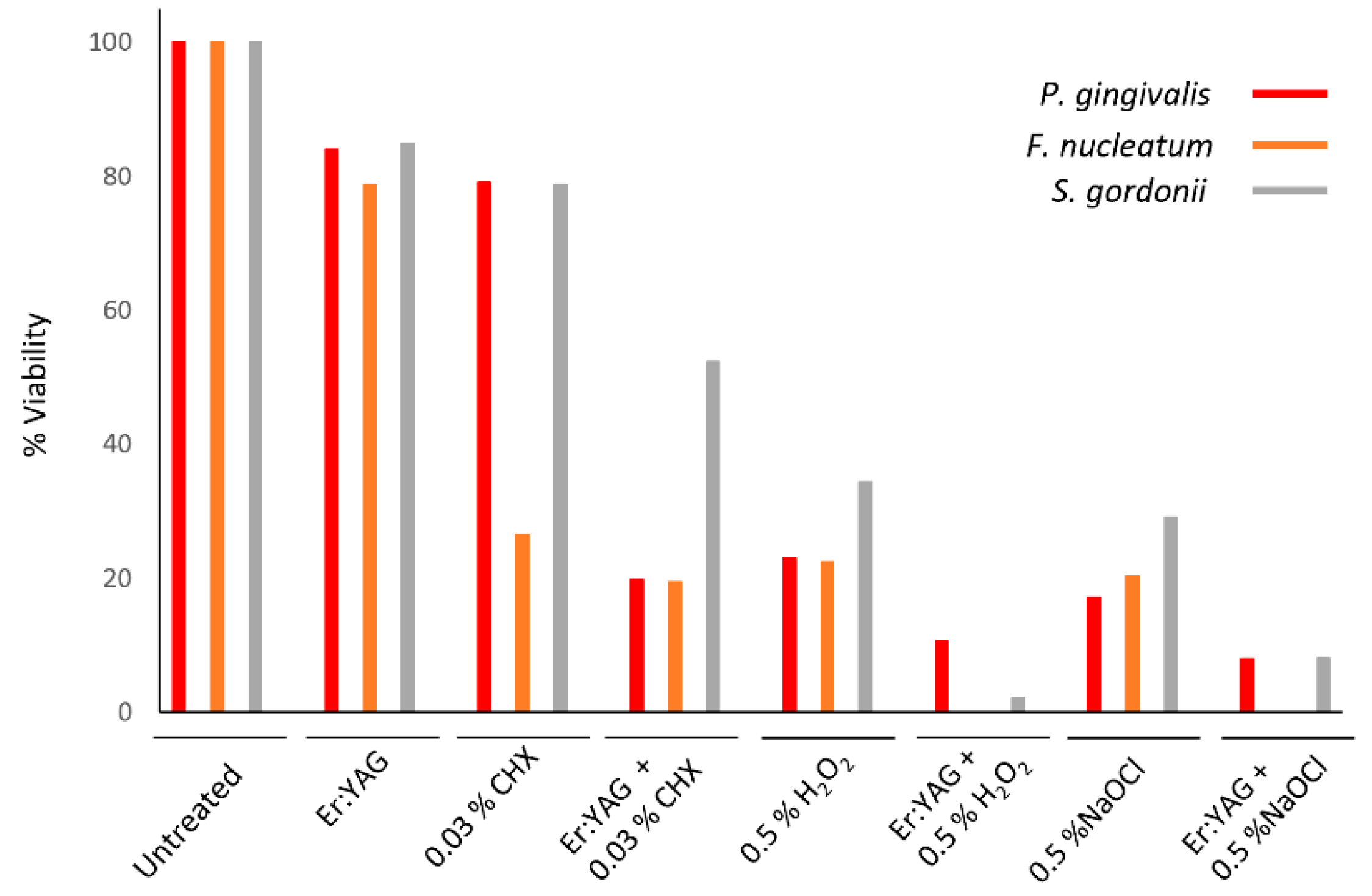
| P. gingivalis | 9.5 ± 0.06 | 7.98 ± 1.75; p = 0.22 | 7.51 ± 0.29; p = 0.009 | 1.88 ± 1.8; p = 0.005 | 2.18 ± 0.48; p = 0002 | 1.0 ± 1.0; p = 0006 | 1.62 ± .53; p = 0001 | 0.75 ±0.83; p = 0003 |
| p = 0.009 | p = 0.15 | p = 0.15 | ||||||
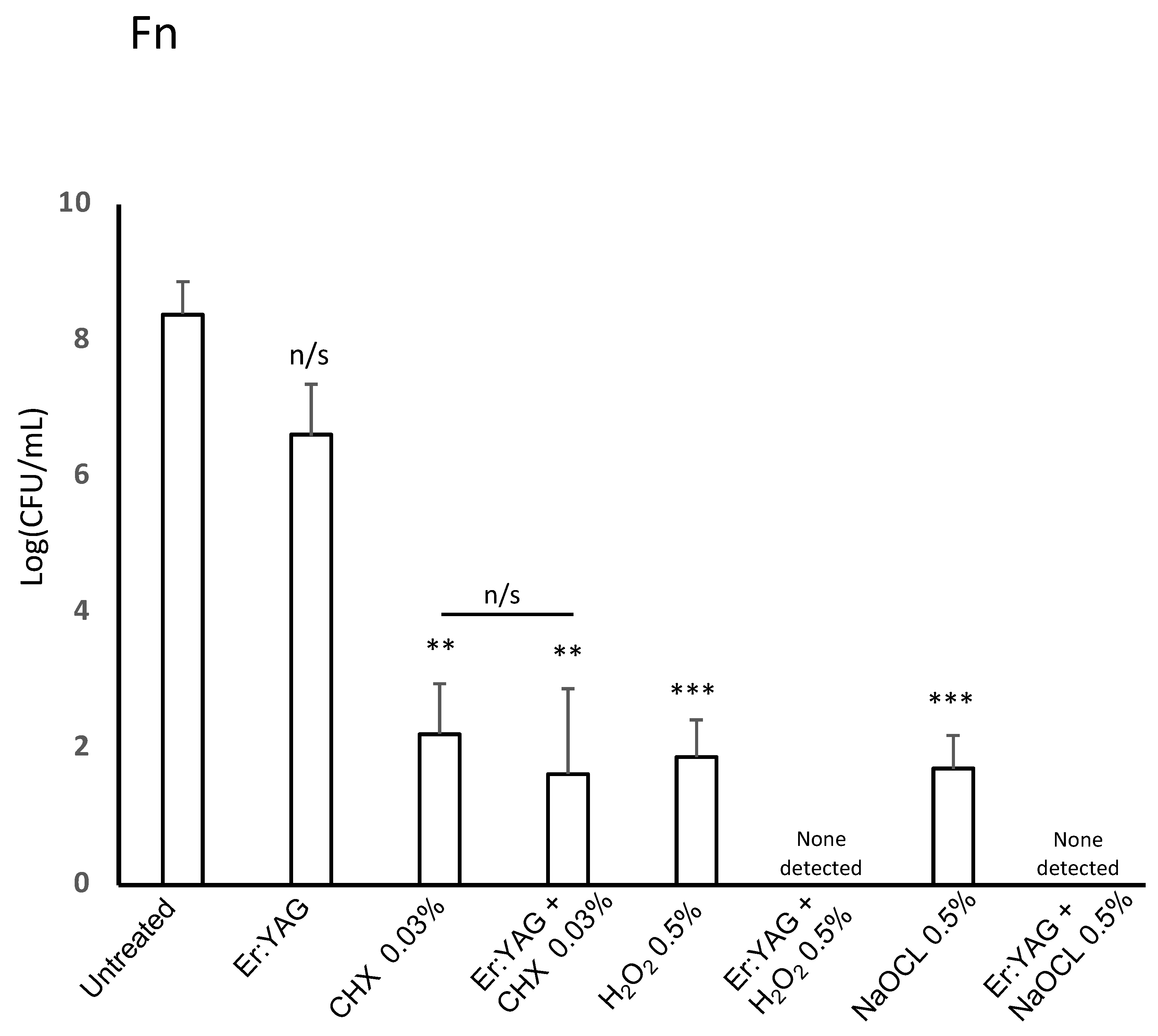
| F. nucleatum | 8.39 ± 0.48 | 6.6 ± 0.76; p = 0.062 | 2.22 ± 0.74; p = 0.003 | 1.63 ± 1.25; p = 0.003 | 1.88 ± 0.55; p = 0.0007 | N.D.* | 1.7 ± 0.49; p = 0.0009 | N.D.* |
| p = 0.47 | ||||||||
| S. gordonii | 9.37 ± 0.08 | 7.94 ± 0.92; p = 0.065 | 7.37 ± 0.26; p = 0.0002 | 4.89 ± 0.67; p = 0.0009 | 3.22 ± 0.37; p = 0.0001 | 0.2 ± 0.28; p = 0.0004 | 2.72 ± 0.27; p < 0.00001 | 0.75 ± 0.8; p = 0.0004 |
| p = 0.031 | p = 0.024 | p = 0.04 | ||||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Golob Deeb, J.; Smith, J.; Belvin, B.R.; Lewis, J.; Grzech-Leśniak, K. Er:YAG Laser Irradiation Reduces Microbial Viability When Used in Combination with Irrigation with Sodium Hypochlorite, Chlorhexidine, and Hydrogen Peroxide. Microorganisms 2019, 7, 612. https://doi.org/10.3390/microorganisms7120612
Golob Deeb J, Smith J, Belvin BR, Lewis J, Grzech-Leśniak K. Er:YAG Laser Irradiation Reduces Microbial Viability When Used in Combination with Irrigation with Sodium Hypochlorite, Chlorhexidine, and Hydrogen Peroxide. Microorganisms. 2019; 7(12):612. https://doi.org/10.3390/microorganisms7120612
Chicago/Turabian StyleGolob Deeb, Janina, John Smith, B. Ross Belvin, Janina Lewis, and Kinga Grzech-Leśniak. 2019. "Er:YAG Laser Irradiation Reduces Microbial Viability When Used in Combination with Irrigation with Sodium Hypochlorite, Chlorhexidine, and Hydrogen Peroxide" Microorganisms 7, no. 12: 612. https://doi.org/10.3390/microorganisms7120612
APA StyleGolob Deeb, J., Smith, J., Belvin, B. R., Lewis, J., & Grzech-Leśniak, K. (2019). Er:YAG Laser Irradiation Reduces Microbial Viability When Used in Combination with Irrigation with Sodium Hypochlorite, Chlorhexidine, and Hydrogen Peroxide. Microorganisms, 7(12), 612. https://doi.org/10.3390/microorganisms7120612






