Abstract
The COVID-19 pandemic represents a major global health crisis, with clinical manifestations ranging from asymptomatic infection to fatal outcomes. While all individuals are susceptible, specific populations, particularly those with pre-existing medical conditions, face a heightened risk of severe disease. This study aimed to assess the prevalence of severe COVID-19 among hospitalized patients with comorbidities in the Central Region of Romania, and to analyze the association between these conditions and mortality. We conducted a retrospective cohort study using data from the Corona Forms platform (2020–2022), encompassing hospitalized cases across three Romanian counties. A total of 1458 patients with confirmed SARS-CoV-2 infection and documented comorbidities were included. Demographic characteristics, comorbid conditions, and hospitalization outcomes were analyzed. The overall mortality rate among comorbid patients was 89.3%. Renal, neurologic, hepatic disease, cardiovascular conditions, obesity, type 2 diabetes mellitus, and cerebrovascular accidents are significant risk factors for death outcomes in the SARS-CoV-2-infected study population. The strength of their association varies, with odds ratios ranging from 25.32 to 1. The findings underscore the critical impact of comorbidities on COVID-19 severity and mortality among the Central Romanian population, emphasizing the necessity of targeted clinical interventions and public health strategies to protect high-risk populations.
1. Introduction
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) was a major global health threat responsible for a prolonged and highly fatal pandemic, primarily causing respiratory disease with recurrent infection waves [1]. The clinical manifestations of COVID-19 range from asymptomatic infection to critical illness and mortality. Although SARS-CoV-2 infection poses a risk to all individuals, specific populations are disproportionately susceptible to severe disease. This susceptibility is influenced by factors such as age, gender, socioeconomic status, smoking history, and, most critically, underlying medical comorbidities [2,3,4,5,6,7,8]. Several pre-existing conditions have been identified as risk factors for severe COVID-19.
Chronic obstructive pulmonary disease (COPD) has been identified as a significant risk factor for both hospitalization and mortality in COVID-19, independent of age, sex, and other comorbidities. The increased mortality risk is attributed to pre-existing respiratory impairment, ventilation/perfusion mismatch, and secondary bacterial infections [9,10,11]. Respiratory support methods and barotrauma were also studied. Chest CT score and SpO2/FiO2 ratio contribute to worse clinical outcomes regardless of ventilatory strategies [12,13].
Metabolic syndrome. Several systematic reviews and meta-analyses have consistently demonstrated that metabolic comorbidities—including diabetes, obesity, dyslipidemia, and hypertension—synergistically exacerbate disease severity and mortality [14].
Diabetes mellitus (DM). Liu K. et al.’s meta-analysis highlights that DM significantly increases the risk of severe COVID-19 infection and mortality. Diabetic patients, particularly those with hypertension and other comorbidities, exhibit worse outcomes, including higher intensive care unit (ICU) admission and lower hospital discharge rates, due to exacerbated inflammatory responses, immune dysfunction, and increased susceptibility to complications such as cardiovascular and kidney diseases [15].
Obesity is a critical modifiable risk factor linked to increased inflammation, prothrombotic state, and impaired immune responses. Several pathophysiological mechanisms contribute to the heightened severity and mortality risk in obese individuals with COVID-19. Ectopic fat accumulation exacerbates COVID-19-induced inflammation. Additionally, obesity is associated with decreased levels of the anti-inflammatory adipokine adiponectin and overexpression of angiotensin-converting enzyme 2 (ACE2) receptors, potentially enhancing viral entry. Moreover, obesity contributes to endothelial dysfunction via multiple pathological pathways, including activation of the renin-angiotensin system, promotion of a procoagulant state, insulin resistance, oxidative stress, platelet dysfunction, and immune dysregulation [16,17,18,19].
Hypertension (HT). A Swedish study demonstrated that hypertension serves as an independent risk factor for severe COVID-19, regardless of age and other comorbidities. HT is associated with endothelial dysfunction, chronic inflammation, and immune dysregulation, potentially exacerbated by SARS-CoV-2-induced depletion of ACE2 [20,21,22,23,24].
Congestive heart failure. A South Korean population-based study demonstrated that a history of heart failure (HF) is significantly correlated with an increased risk of severe complications and mortality in COVID-19 patients [25]. The heightened mortality risk is due to pro-inflammatory cytokine release, myocardial injury, and thromboembolism [26,27,28].
Chronic kidney disease (CKD). A Swedish national study identified a strong and independent association between CKD and severe COVID-19 outcomes, including ICU admission and mortality, regardless of the underlying etiology of CKD. CKD is an independent predictor of severe COVID-19 and is characterized by immune dysfunction, cardiovascular risk, and predisposition to acute kidney injury [29,30,31].
Cancer. Both malignancy itself and anticancer therapies contribute to immune suppression, increasing the risk of infection and exacerbating the severity of SARS-CoV-2, particularly among patients with lung and hematologic cancer [32,33].
Thanks to public health surveillance and numerous clinical-epidemiological studies, several meta-analyses have been published post-pandemic, statistically supporting the role of multiple long-term conditions (MLTCs). The presence of two or more chronic diseases in an individual is associated with severe COVID-19 outcomes [34,35]. Some Romanian studies with smaller sample sizes have been conducted, accentuating the need for future policies in Romania to protect high-risk groups, provide personalized care, and offer guidance for healthcare policymakers to enhance clinical management [36,37,38,39]. This study aims to evaluate the association between various comorbidities and COVID-19 mortality in hospitalized patients, focusing on identifying the impact of specific comorbidities on the increased risk of death across different age groups in the Central Region of Romania.
2. Materials and Methods
2.1. Study Design
This retrospective cohort study was conducted in Romania’s Central Macroregion, as defined by the Eurostat Nomenclature of Territorial Units for Statistics (2024).
2.2. Data Collection
The study cohort included patients diagnosed with SARS-CoV-2 infection and recorded in the Corona Forms, a national database for tracking SARS-CoV-2 infections.
The dataset was obtained from the Corona Forms platform with authorization from the Public Health Directorate of each county. The Special Telecommunications Service developed Corona Forms at the request of the Ministry of Health to collect and integrate data from public authorities monitoring SARS-CoV-2 infections. The Ministry of Health, the National Institute of Public Health, county and municipal public health directorates, accredited RT-PCR testing laboratories, and healthcare facilities responsible for managing COVID-19 cases utilize it.
2.3. Sampling Method
The Central Macroregion comprises six counties: Alba, Brașov, Covasna, Harghita, Mureș, and Sibiu. A non-probability convenience sampling was applied. Only cases from three counties (Harghita, Covasna, and Mureș) were included.
Harghita, Covasna, and Mureș counties, according to the 2021 census, have a combined population of 2,271,067 inhabitants, representing 11.91% of Romania’s total population.
The inclusion criterion was isolation in public hospitals within the three selected counties between 26 February 2020, and 26 February 2022, covering the first two years of the COVID-19 pandemic in Romania.
In the studied counties, 15 public hospitals were involved in the isolation and management of COVID-19 patients, with a mandatory reporting obligation to the Corona Forms platform (see Appendix A).
2.4. Study Population
A total of 24,633 cases were identified and extracted from the Corona Forms database, excluding personal identifiers.
Following data collection, preprocessing was performed using Microsoft Excel. The study included only patients explicitly documented as having at least one comorbidity. Comorbidities were classified into the following 12 categories:
- Respiratory diseases (COPD, asthma, emphysema)
- Obesity (all grades)
- Type 2 diabetes mellitus (T2DM)
- Hypertension
- Chronic ischemic heart disease (IHD)
- Congestive heart failure (CHF)
- Atrial fibrillation (AF)
- Renal diseases
- Hepatic diseases (cirrhosis, steatosis, liver failure)
- Neurological disorders (excluding cerebrovascular accidents [CVA])
- Cerebrovascular accidents (CVA)
- Neoplastic diseases
A total of 1458 patients with documented comorbidities were identified.
Age was categorized into decades: <10, 11–20, 21–30, 31–40, 41–50, 51–60, 61–70, 71–80, and 91–99 years. The hospitalization period was determined based on the admission date, discharge date, or date of death.
2.5. Data Analysis
Quantitative data (e.g., age) were presented as means with standard deviation for normally distributed variables, while frequency tables were also used for categorical data. Qualitative data were summarized as counts and percentages. Statistical analysis was conducted using the Statistical Package for the Social Sciences (SPSS, version 23, Chicago, IL, USA). For categorical variables, the Chi-squared test was used to assess the association between comorbidities and mortality. The odds ratio (OR) was calculated to evaluate the strength of the association between comorbidities and the risk of mortality. A p-value of <0.05 was considered statistically significant for all tests.
3. Results
The number of cases recorded on the Corona Forms platform is summarized in Table 1. From these, only cases isolated in public hospitals in Mureș, Harghita, and Covasna counties were filtered and processed in our study (see Table 1).

Table 1.
Registered COVID-19 cases during the first two pandemic years in three central region counties of Romania.
Out of 96,785 registered cases, only 24,633 (25.45%) required hospital isolation. Among hospitalized COVID-19 cases in Mureș, Harghita, and Covasna counties, during the first two years of the pandemic, 5.91% (1458) of cases had mentioned comorbidities. Males accounted for 52.7% of the analyzed cases. The mean age of the study population was 71.6 years (±12.7 SD), with the majority being elderly individuals over 60 years old (see Figure 1).
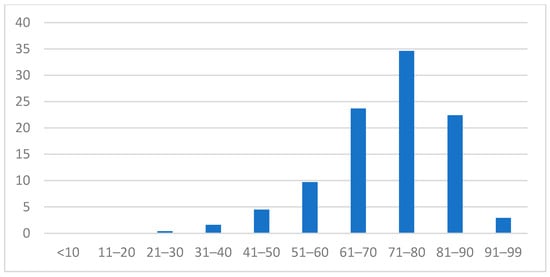
Figure 1.
Characteristics of the study population—age distribution.
The median duration of hospitalization was 7 days (range: 0–393 days). The relationship between age and length of hospitalization (number of days) is presented in Table 2. (see Table 2).

Table 2.
Age analysis by decades and length of hospitalization in days.
The distribution of comorbidities per patient is presented graphically in Figure 2. (see Figure 2). A total of 16.2% of patients had a single comorbidity, whereas those with more than seven comorbidities accounted for only 1.4% of the study sample.
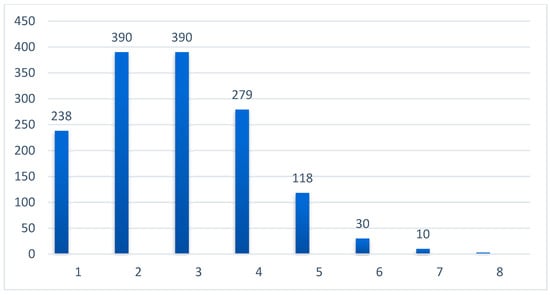
Figure 2.
Incidence of number of associated comorbidities (numerical).
The distribution of MLTCs by age group is shown in Table 3, illustrating that the number of comorbidities experienced by the studied population increases with age, especially in the 61–80 age range (see Table 3).

Table 3.
Number of associated comorbidities divided into age groups.
A total of 298 patients in the study cohort had renal comorbidities at the time of hospitalization for COVID-19. In contrast, 129 patients had a history of neoplastic disease, representing a relatively small proportion of the sample.
Among all comorbidities, ischemic heart disease (ICD) was the most frequent, affecting 988 patients. Regarding metabolic disorders, T2DM was more common than obesity, with 454 patients (31.13%) diagnosed with T2DM. Additionally, 102 patients (6.99%) had a history of stroke, representing the neurological sequelae within the cohort Table 4 (see Table 4).

Table 4.
Distribution of comorbidities by category.
The association between the number of comorbidities and mortality outcomes is presented in Table 5 (see Table 5).

Table 5.
Negative health outcomes and accumulation of associated comorbidities.
To assess the correlation between the variable sets, a Chi-squared test was conducted, and the odds ratio (OR) was calculated. The results are presented in Table 6 (see Table 6).

Table 6.
Multivariate analysis between age, sex, comorbidities, and death, OR value.
In the present study, the contingency table data (see Table 6) revealed no statistically significant association between the presence of neoplastic comorbidities and mortality. Both the Chi-squared test and the calculated POR of 0.715 indicated no increased risk of death in patients with neoplastic comorbidities. The highest POR was observed between neurological comorbidities and mortality.
The analysis between the number of comorbidities and hospitalization duration in this dataset suggests no significant correlation. The correlation coefficient (ρ) was −0.019, indicating a very weak negative correlation between the two variables. This shows that an increase in the number of comorbidities is associated with a slight decrease in hospitalization duration; however, this relationship is negligible. The correlation was not statistically significant (p = 0.465, p > 0.05), indicating that the observed association could be due to chance rather than a true effect (see Table 7). This finding implies that the number of comorbidities alone may not be a determining factor in the length of hospital stay for patients.

Table 7.
Results of a Spearman’s rank correlation analysis between the number of hospitalization days and the number of comorbidities.
4. Discussion
This study aimed to evaluate the association between multimorbidity and COVID-19 mortality in hospitalized patients, with a particular focus on the impact of specific comorbidities.
Multimorbidity, or MLTCs, refers to the coexistence of two or more chronic conditions and poses a considerable global public health challenge. The high prevalence of multimorbidity contributes to increased mortality, healthcare utilization, and associated costs. A systematic review and meta-analysis conducted by Chowdhury et al. assessed the prevalence and patterns of multimorbidity across various regions and over time. Between 2020 and 2021, the authors analyzed data from 126 peer-reviewed studies encompassing nearly 15.4 million individuals from 54 countries. The global prevalence of multimorbidity was found to be 37.2%, with more than half of the adult population over 60 years of age being affected by multimorbidity conditions [40].
The COVID-19 pandemic has further exacerbated health disparities, particularly for individuals with pre-existing conditions. While key risk factors for severe disease and mortality—such as older age, male sex, socioeconomic deprivation, and ethnic minority status—are well established, the impact of MLTCs on COVID-19 outcomes remains underexplored. Salisu-Olatunji et al. (2024) conducted a systematic review and meta-analysis to examine the influence of MLTCs on COVID-19-related morbidity and mortality. Their analysis, which included data from over 4 million individuals, revealed that MLTCs significantly increase the risk of severe COVID-19 outcomes and death. Patients with MLTCs were found to have more than twice the risk of mortality compared to those without MLTCs [35].
Additionally, Gebremedhn Gebremeskel et al. (2024) reported that the mortality rate among critically ill COVID-19 patients across 24 studies involving 142,291 participants ranged from 4.5% to 69.5%. Notably, 68.7% of these critically ill patients had chronic disease comorbidities [34]. In our study population of hospitalized COVID-19 patients, the mortality rate was 16.83%, and 89% in comorbid patients. The following section discusses the various comorbidities observed in our cohort, with a comparative analysis of the results reported in the existing literature.
Respiratory comorbidities. Meta-analyses involving 59 studies have consistently shown that COPD is associated with an increased risk of hospitalization, ICU admission, and mortality in COVID-19 patients [41]. A retrospective cohort study from the Republic of Korea also found COPD to be an independent risk factor for all-cause mortality, even after adjusting for age, sex, and the Charlson comorbidity index [42]. Similarly, a US study with over 11,000 COVID-19 patients identified COPD as the comorbidity most strongly associated with mortality, although obesity, diabetes, and hypertension were also independent predictors [43]. Moreover, a large cohort study from China involving over 39,000 patients revealed that patients with COPD and asthma had a higher likelihood of requiring invasive ventilation, ICU admission, or dying within 30 days of hospitalization after adjusting for age, sex, and other comorbidities [44]. In contrast, our study did not find a significant association between pulmonologic comorbidities and COVID-19 mortality. This could be due to several factors: the relatively small number of patients with pulmonologic conditions (n = 182), the inclusion of a wide range of pulmonary diseases (COPD, asthma, emphysema, etc.), varying severity levels, and inconsistencies in data collection across different centers.
Obesity. A large Swedish national study identified a strong, independent, and statistically significant correlation between obesity and severe COVID-19 outcomes, including mechanical ventilation, continuous renal replacement therapy, and death after ICU admission [29]. In 2022, a meta-analysis that included 3,140,413 COVID-19 patients from 167 studies found that obesity was associated with an increased risk of severe and high mortality [16]. Another meta-analysis from China, encompassing 46 studies, demonstrated that obese patients had significantly higher risks of hospitalization, severe illness, mechanical ventilation, ICU admission, and mortality [45]. Additionally, a Serbian study suggested that bioelectrical impedance analysis measurements could serve as more reliable predictors of severe obesity-related COVID-19 than body mass index alone [46]. Consistent with these findings, our study suggests that obesity may be associated with an increased risk of mortality from COVID-19 (OR = 1.002).
Type 2 diabetes mellitus. Sörling et al. identified a strong, independent, and statistically significant correlation between T2DM and severe COVID-19 outcomes, such as mechanical ventilation, continuous renal replacement therapy, and death after ICU admission [29]. Data from a meta-analysis underscore that, after adjusting for confounders, diabetes is a significant predictor of poor COVID-19 prognosis [4,5]. Our study suggests that T2DM may be associated with an increased risk of mortality from COVID-19 (OR = 1.458), although this association was not statistically confirmed.
High blood pressure. Research from 2022 indicated that hypertension alone was not an independent predictor of clinical outcomes, but was associated with poorer outcomes only when combined with diabetes or another risk factor [47]. It should be noted that some studies have shown no significant impact of hypertension or diabetes on the course of COVID-19, while others have reported that both hypertension and diabetes, with or without obesity, were independently linked to an unfavorable outcome [48]. Bauer et al. suggested that hypertension was an independent predictor of severe COVID-19 only in patients younger than 65 years, but not in the entire study population [49]. In contrast, Barrera et al., based on a study of 15,794 patients, reported that hypertension and diabetes, when considered separately, were significantly associated with ICU admission and death [50]. Thus, the impact of hypertension on the severity of COVID-19 remains controversial. In our study, we were able to demonstrate an association between hypertension and COVID-19 mortality, with a modest OR of 2.058, despite the ongoing debate on this topic.
Chronic ischemic heart disease. Our study shows a strong association between IHD and COVID-19 mortality (OR = 13.465), further emphasizing the severity of IHD as a comorbidity in COVID-19 patients. A meta-analysis encompassing 157,439 COVID-19 patients across 81 studies revealed that patients with pre-existing ischemic heart disease (IHD) faced an increased risk of mortality, severe/critical COVID-19, ICU admission, and a lower likelihood of discharge/recovery compared to COVID-19 patients without pre-existing IHD. In conclusion, pre-existing IHD significantly increases the risk of unfavorable outcomes in COVID-19 patients, particularly in male and hypertensive patients [51].
Congestive heart failure. A study conducted in Poland determined that patients hospitalized for COVID-19 with a history of congestive heart failure (CHF) had significantly higher in-hospital mortality (35% vs. 12%), and at three months (53% vs. 22%) and six months (72% vs. 47%) follow-up, compared to patients without a history of CHF. This study concluded that a history of CHF identifies patients with COVID-19 at high risk of in-hospital complications and mortality up to six months of follow-up [52]. Similarly, a national study from Korea found that the presence of CHF was independently associated with increased mortality [27]. Our study also suggests that CHF may be associated with an increased risk of mortality due to COVID-19 (OR = 2.524), although this association was not statistically significant (p > 0.05), likely due to the modest sample size.
Atrial fibrillation. A meta-analysis of 36 studies found pre-existing AF linked to higher in-hospital and post-discharge mortality, as well as increased ventilator use in COVID-19 patients [53]. However, a study of 31,000 U.S. patients showed that new-onset AF was not significantly associated with mortality, suggesting it may indicate disease severity rather than being an independent risk factor [54]. Our study found no link between AF and COVID-19 mortality, possibly due to the inability to distinguish between pre-existing and newly developed AF during hospitalization.
Renal comorbidities. Several studies have established that CKD increases the risk of severe COVID-19 outcomes, including hospitalization, mechanical ventilation, and mortality. A meta-analysis by Jdiaa et al. [31] highlighted a consistent association between CKD and COVID-19 severity, although the extent of its impact remains uncertain due to variations across studies. Similarly, other large studies report a significant correlation between CKD and poor COVID-19 prognosis, including a higher risk of requiring renal replacement therapy and increased mortality [29,30]. In line with these findings, our study confirms that renal comorbidities are strongly associated with COVID-19 mortality (OR = 3.677, p = 0.000), supporting the established role of CKD as a major risk factor for adverse COVID-19 outcomes. Investigations are needed to determine whether different stages of CKD influence COVID-19 mortality, and that will provide answers. A nationwide cohort study in Sweden also investigated the risk of severe COVID-19 associated with different CKD stages. The study found that worsening CKD stage and dialysis were independent risk factors for COVID-19-related hospitalization and mortality [55].
Hepatic comorbidities. A U.S. multicenter study identified alcoholic liver disease, cirrhosis, and hepatocellular carcinoma as risk factors for COVID-19 mortality [56]. Another study found cirrhosis linked to poorer 30-day survival [57], while a Korean analysis of non-alcoholic fatty liver disease (NAFLD) patients showed higher fatty liver index (FLI) scores correlated with severe COVID-19 outcomes [58]. However, our study found no link between liver comorbidities and COVID-19 mortality. This aligns with other studies suggesting that only severe liver conditions, such as cirrhosis and high FLI scores, affect COVID-19 outcomes. Future research should categorize liver comorbidities by severity for better clarity.
Neoplastic Comorbidities. Meta-analyses across diverse patient populations have shown that cancer patients with COVID-19 experience a mortality rate of approximately 22%, which is about four times higher than that observed in non-cancer patients. Subgroup analyses reveal even higher mortality in those with lung and hematologic cancers, with rates ranging from 33% to 34%, approximately double the rates seen in other cancer types. Additionally, severe outcomes, including ICU admission and mechanical ventilation, are consistently high, affecting 55% to 60% of cancer patients, regardless of cancer type [32,33]. In contrast, our study found no significant association between neoplastic comorbidities and COVID-19 mortality. This discrepancy may be attributed to the relatively small number of cancer patients in our cohort (n = 129), which could have limited our ability to detect a meaningful association. The impact of active (with the effect of cancer treatment) vs. remission cancer status on COVID-19 outcomes needs to be confirmed with further research.
Our findings raise the question of why certain comorbidities, such as chronic ischemic heart disease, have a stronger association with mortality than others, such as obesity. One possible explanation could be the underlying inflammatory processes or cardiovascular complications in these patients, which could exacerbate the effects of COVID-19. Future studies should explore these pathways in greater detail.
In addition to comorbidities, we also analyzed demographic parameters of the study population concerning COVID-19 mortality. Among the deceased, 63.44% were over 70 years of age, and 53.2% were male. However, while sex was not significantly associated with an increased risk of COVID-19 mortality, age demonstrated a clear correlation with mortality outcomes. A meta-analysis of 70 studies by Starke et al. found that the risk of in-hospital and case mortality increased by 5.7% and 7.4%, respectively, for each year of age, and the risk of hospitalization increased by 3.4% per year. The study did not identify a specific age threshold where the risk significantly accelerated, offering a quantifiable measure of how age influences COVID-19 severity [59]. Fabião et al. reported that men had a relative risk of 1.36 for mortality and 1.29 for COVID-19 severity compared to women. Importantly, age did not significantly influence the meta-regression results for either mortality or severity [60]. Our study, however, found no association between sex and an increased risk of COVID-19 mortality.
Study Limitations. The primary limitation of this study lies in the relatively small sample size (1458 patients), which increases the likelihood of a Type II error (β), whereby a statistically significant relationship that may exist is not detected due to insufficient statistical power.
Another limitation is the study design itself: this is a retrospective cohort study. This reliance on past data also introduces the potential for selection bias, which may reduce the generalizability and external validity of the findings. The retrospective nature of the study relies on previously collected data, which may be incomplete or inaccurate.
For instance, patients with chronic kidney disease (CKD) were grouped into a single heterogeneous category of renal comorbidities without differentiation by disease stage. Similarly, regarding obesity, there was a lack of information on obesity classes, which could have led to inconsistencies in the data analysis.
The observational nature of this study cannot establish a causal relationship; we can show associations and cannot definitively prove that one factor caused another.
5. Conclusions
This study highlights the strong impact of multimorbidity on COVID-19 mortality, with chronic ischemic heart disease, renal disease, and hypertension emerging as key risk factors. A novel finding is the exceptionally high mortality rate (89%) among comorbid patients, emphasizing the need for targeted interventions. Unlike prior studies, we found no significant link between neoplastic, respiratory, and liver comorbidities and mortality, likely due to sample size limitations. Our findings also raise questions about why some comorbidities, like chronic ischemic heart disease, pose greater risks than others, such as obesity, warranting further research. Despite limitations, this study underscores the need for personalized risk assessment in hospitalized COVID-19 patients.
Author Contributions
Conceptualization, R.B. and L.I.F.; methodology, R.B.; software, T.S.V.; validation, all authors.; formal analysis, T.S.V.; investigation, R.B.; data curation, R.B. and L.I.F.; writing—original draft preparation, R.B.; writing—review and editing, T.S.V. and Z.Á.; visualization, R.B. and L.I.F.; supervision, T.S.V. and Z.Á. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of G.E. Palade UMPhST of Targu Mures (3651/25 February 2025).
Informed Consent Statement
Patient consent was waived due to not receiving personal data of study participants from Health Directories.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ACE2 | Angiotensin-converting enzyme 2 |
| AF | Atrial fibrillation |
| BMI | Body Mass Index |
| CHF | Congestive Heart Failure |
| CKD | Chronic kidney disease |
| COPD | Chronic Obstructive Pulmonary Disease |
| CVA | Cerebrovascular Accident |
| DM | Diabetes Mellitus |
| FLI | Fatty liver index |
| HF | Heart Failure |
| HT | Hypertension |
| ICU | Intensive Care Unit |
| IHD | Chronic ischemic heart disease |
| MLTCs | Multiple long-term conditions |
| NAFLD | Nonalcoholic fatty liver disease |
| OR | Odds Ratio |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus-2 |
| T2DM | Type 2 diabetes mellitus |
Appendix A
| County | Hospital Name |
| Mureș County | Târgu Mureș County Emergency Hospital |
| (7 hospitals) | Emergency Institute for Cardiovascular Diseases and Transplantation, Târgu Mureș |
| Mureș County Hospital | |
| Sighișoara Municipal Hospital | |
| Reghin Municipal Hospital “Dr. Eugen Nicoară” | |
| Târnăveni Municipal Hospital “Dr. Gheorghe Marinescu” | |
| Luduș City Hospital “Dr. Valer Russu” | |
| Harghita County | Miercurea Ciuc County Emergency Hospital |
| (4 hospitals) | Odorheiu Secuiesc Municipal Hospital |
| Gheorgheni Municipal Hospital | |
| Toplița Municipal Hospital | |
| Covasna County (4 hospitals) | County Emergency Hospital “Dr. Fogolyán Kristóf”, Sfântu Gheorghe |
| Târgu Secuiesc Municipal Hospital | |
| Baraolt City Hospital | |
| Cardiovascular Rehabilitation Hospital “Dr. Benedek Géza”, Covasna |
References
- Gupta, P.; Gupta, V.; Singh, C.M.; Singhal, L. Emergence of COVID-19 Variants: An Update. Cureus 2023, 15, e41295. [Google Scholar] [CrossRef] [PubMed]
- Qiu, S.; Cai, X.; Jia, L.; Sun, Z.; Wu, T.; Wendt, J.; Steinacker, J.M.; Schumann, U. Does Objectively Measured Light-Intensity Physical Activity Reduce the Risk of Cardiovascular Mortality? A Meta-Analysis. Eur. Heart J. Qual. Care Clin. Outcomes 2021, 7, 496–504. [Google Scholar] [CrossRef]
- Froldi, G.; Dorigo, P. Endothelial Dysfunction in Coronavirus Disease 2019 (COVID-19): Gender and Age Influences. Med. Hypotheses 2020, 144, 110015. [Google Scholar] [CrossRef] [PubMed]
- Sanyaolu, A.; Okorie, C.; Marinkovic, A.; Patidar, R.; Younis, K.; Desai, P.; Hosein, Z.; Padda, I.; Mangat, J.; Altaf, M. Comorbidity and its Impact on Patients with COVID-19. SN Compr. Clin. Med. 2020, 2, 1069–1076. [Google Scholar] [CrossRef] [PubMed]
- Corona, G.; Pizzocaro, A.; Vena, W.; Rastrelli, G.; Semeraro, F.; Isidori, A.M.; Pivonello, R.; Salonia, A.; Sforza, A.; Maggi, M. Diabetes is most important cause for mortality in COVID-19 hospitalized patients: Systematic review and meta-analysis. Rev. Endocr. Metab. Disord. 2021, 22, 275–296. [Google Scholar] [CrossRef]
- Floyd, J.S.; Walker, R.L.; Kuntz, J.L.; Shortreed, S.M.; Fortmann, S.P.; Bayliss, E.A.; Harrington, L.B.; Fuller, S.; Albertson-Junkans, L.H.; Powers, J.D.; et al. Association Between Diabetes Severity and Risks of COVID-19 Infection and Outcomes. J. Gen. Intern. Med. 2023, 38, 1484–1492. [Google Scholar] [CrossRef]
- McGurnaghan, S.J.; Weir, A.; Bishop, J.; Kennedy, S.; Blackbourn, L.A.K.; McAllister, D.A.; Hutchinson, S.; Caparrotta, T.M.; Mellor, J.; Jeyam, A.; et al. Risks of and Risk Factors for COVID-19 Disease in People with Diabetes: A Cohort Study of the Total Population of Scotland. Lancet Diabetes Endocrinol. 2021, 9, 82–93. [Google Scholar] [CrossRef]
- Patel, R.; Kooner, J.S.; Zhang, W. Comorbidities Associated with the Severity of COVID-19, and Differences across Ethnic Groups: A UK Biobank Cohort Study. BMC Public Health 2023, 23, 1566. [Google Scholar] [CrossRef]
- Aveyard, P.; Gao, M.; Lindson, N.; Hartmann-Boyce, J.; Watkinson, P.; Young, D.; Coupland, C.A.C.; Tan, P.S.; Clift, A.K.; Harrison, D.; et al. Association between Pre-Existing Respiratory Disease and Its Treatment, and Severe COVID-19: A Population Cohort Study. Lancet Respir. Med. 2021, 9, 909–923. [Google Scholar] [CrossRef]
- Lang, M.; Som, A.; Mendoza, D.P.; Flores, E.J.; Reid, N.; Carey, D.; Li, M.D.; Witkin, A.; Rodriguez-Lopez, J.M.; Shepard, J.O.; et al. Hypoxaemia Related to COVID-19: Vascular and Perfusion Abnormalities on Dual-Energy CT. Lancet Infect. Dis. 2020, 20, 1365–1366. [Google Scholar] [CrossRef]
- Singh, D.; Mathioudakis, A.G.; Higham, A. Chronic Obstructive Pulmonary Disease and COVID-19: Interrelationships. Curr. Opin. Pulm. Med. 2022, 28, 76–83. [Google Scholar] [CrossRef] [PubMed]
- da Cruz, A.P.; Martins, G.; Martins, C.M.; Marques, V.; Christovam, S.; Battaglini, D.; Robba, C.; Pelosi, P.; Rocco, P.R.M.; Cruz, F.F.; et al. Comparison between high-flow nasal oxygen (HFNO) alternated with non-invasive ventilation (NIV) and HFNO and NIV alone in patients with COVID-19: A retrospective cohort study. Eur. J. Med. Res. 2024, 29, 248. [Google Scholar] [CrossRef]
- Vetrugno, L.; Castaldo, N.; Fantin, A.; Deana, C.; Cortegiani, A.; Longhini, F.; Forfori, F.; Cammarota, G.; Grieco, D.L.; Isola, M.; et al. Ventilatory associated barotrauma in COVID-19 patients: A multicenter observational case control study (COVI-MIX-study). Pulmonology 2023, 29, 457–468. [Google Scholar] [CrossRef] [PubMed]
- Rico-Martín, S.; Calderón-García, J.F.; Basilio-Fernández, B.; Clavijo-Chamorro, M.Z.; Sánchez Muñoz-Torrero, J.F. Metabolic Syndrome and Its Components in Patients with COVID-19: Severe Acute Respiratory Syndrome (SARS) and Mortality. A Systematic Review and Meta-Analysis. J. Cardiovasc. Dev. Dis. 2021, 8, 162. [Google Scholar] [CrossRef]
- Liu, K.; Liu, S.; Xu, T.T.; Qiao, H. The clinical features and outcomes of diabetes patients infected with COVID-19: A systematic review and meta-analysis comprising 192,693 patients. Front. Med. 2025, 12, 1523139. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Rathore, S.S.; Khan, H.; Karale, S.; Chawla, Y.; Iqbal, K.; Bhurwal, A.; Tekin, A.; Jain, N.; Mehra, I.; et al. Association of Obesity With COVID-19 Severity and Mortality: An Updated Systemic Review, Meta-Analysis, and Meta-Regression. Front. Endocrinol. 2022, 13, 780872. [Google Scholar] [CrossRef]
- Kruglikov, I.L.; Scherer, P.E. The Role of Adipocytes and Adipocyte-Like Cells in the Severity of COVID-19 Infections. Obesity 2020, 28, 1187–1190. [Google Scholar] [CrossRef]
- Kwaifa, I.K.; Bahari, H.; Yong, Y.K.; Noor, S.M. Endothelial Dysfunction in Obesity-Induced Inflammation: Molecular Mechanisms and Clinical Implications. Biomolecules 2020, 10, 291. [Google Scholar] [CrossRef]
- Daryabor, G.; Kabelitz, D.; Kalantar, K. An Update on Immune Dysregulation in Obesity-related Insulin Resistance. Scand. J. Immunol. 2019, 90, 12747. [Google Scholar] [CrossRef]
- Drummond, G.R.; Vinh, A.; Guzik, T.J.; Sobey, C.G. Immune Mechanisms of Hypertension. Nat. Rev. Immunol. 2019, 19, 517–532. [Google Scholar] [CrossRef]
- Siedlinski, M.; Jozefczuk, E.; Xu, X.; Teumer, A.; Evangelou, E.; Schnabel, R.B.; Welsh, P.; Maffia, P.; Erdmann, J.; Tomaszewski, M.; et al. White Blood Cells and Blood Pressure. Circulation 2020, 141, 1307–1317. [Google Scholar] [CrossRef]
- Pons, S.; Fodil, S.; Azoulay, E.; Zafrani, L. The Vascular Endothelium: The Cornerstone of Organ Dysfunction in Severe SARS-CoV-2 Infection. Crit. Care 2020, 24, 353. [Google Scholar] [CrossRef]
- Svensson, P.; Hofmann, R.; Häbel, H.; Jernberg, T.; Nordberg, P. Association between Cardiometabolic Disease and Severe COVID-19: A Nationwide Case–Control Study of Patients Requiring Invasive Mechanical Ventilation. BMJ Open 2021, 11, e044486. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; Zhou, N.; Zha, W.; Lv, Y. Hypertension Is a Clinically Important Risk Factor for Critical Illness and Mortality in COVID-19: A Meta-Analysis. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 745–755. [Google Scholar] [CrossRef]
- Kim, W.; Kim, E.J. Heart Failure as a Risk Factor for Stroke. J. Stroke 2018, 20, 33–45. [Google Scholar] [CrossRef]
- Shafi, A.M.A.; Shaikh, S.A.; Shirke, M.M.; Iddawela, S.; Harky, A. Cardiac Manifestations in COVID-19 Patients—A Systematic Review. J. Cardiac Surg. 2020, 35, 1988–2008. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Park, M.S.; Shin, J.I.; Park, J.; Kim, D.H.; Jeon, J.; Kim, J.; Song, T. Associations of Heart Failure with Susceptibility and Severe Complications of COVID-19: A Nationwide Cohort Study. J. Med. Virol. 2022, 94, 1138–1145. [Google Scholar] [CrossRef]
- Yonas, E.; Alwi, I.; Pranata, R.; Huang, I.; Lim, M.A.; Gutierrez, E.J.; Yamin, M.; Siswanto, B.B.; Virani, S.S. Effect of Heart Failure on the Outcome of COVID-19—A Meta Analysis and Systematic Review. Am. J. Emerg. Med. 2021, 46, 204. [Google Scholar] [CrossRef] [PubMed]
- Sörling, A.; Nordberg, P.; Hofmann, R.; Häbel, H.; Svensson, P. Association Between CKD, Obesity, Cardiometabolic Risk Factors, and Severe COVID-19 Outcomes. Kidney Int. Rep. 2023, 8, 775–784. [Google Scholar] [CrossRef]
- Lin, Y.-C.; Lai, T.S.; Lin, S.L.; Chen, Y.M.; Chu, T.S.; Tu, Y.K. Outcomes of Coronavirus 2019 Infection in Patients with Chronic Kidney Disease: A Systematic Review and Meta-Analysis. Ther. Adv. Chronic Dis. 2021, 12, 2040622321998860. [Google Scholar] [CrossRef]
- Jdiaa, S.S.; Mansour, R.; El Alayli, A.; Gautam, A.; Thomas, P.; Mustafa, R.A. COVID–19 and Chronic Kidney Disease: An Updated Overview of Reviews. J. Nephrol. 2022, 35, 69–85. [Google Scholar] [CrossRef]
- Silaghi-Dumitrescu, R.; Patrascu, I.; Lehene, M.; Bercea, I. Comorbidities of COVID-19 Patients. Medicina 2023, 59, 1393. [Google Scholar] [CrossRef]
- Bajgain, K.T.; Badal, S.; Bajgain, B.B.; Santana, M.J. Prevalence of Comorbidities among Individuals with COVID-19: A Rapid Review of Current Literature. Am. J. Infect. Control 2021, 49, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Gebremeskel, G.G.; Tadesse, D.B.; Haile, T.G. Mortality and morbidity in critically ill COVID-19 patients: A systematic review and meta-analysis. J. Infect. Public Health 2024, 17, 102533. [Google Scholar] [CrossRef]
- Salisu-Olatunji, S.O.; Chudasama, Y.V.; Kaur, N.; Kayani, Z.; Odugbemi, B.A.; Bolodeoku, O.E.; Konnor, S.A.; Vounzoulaki, E.; Bhattacharjee, A.; Fahami, R.; et al. COVID-19-related morbidity and mortality in people with multiple long-term conditions: A systematic review and meta-analysis of over 4 million people. J. R. Soc. Med. 2024, 117, 336–351. [Google Scholar] [CrossRef] [PubMed]
- Barbu, M.G.; Thompson, R.J.; Thompson, D.C.; Cretoiu, D.; Suciu, N. The Impact of SARS-CoV-2 on the Most Common Comorbidities—A Retrospective Study on 814 COVID-19 Deaths in Romania. Front. Med. 2020, 7, 567199. [Google Scholar] [CrossRef]
- Marc, M.S.; Rosca, D.; Bratosin, F.; Fira-Mladinescu, O.; Oancea, C.; Pescaru, C.C.; Velescu, D.; Wellmann, N.; Moto-felea, A.C.; Ciuca, I.M.; et al. The Effect of Comorbidities and Complications on COVID-19 Mortality: A Detailed Retrospective Study in Western Romania. J. Pers. Med. 2023, 13, 1552. [Google Scholar] [CrossRef]
- Marincu, I.; Bratosin, F.; Vidican, I.; Bostanaru, A.-C.; Frent, S.; Cerbu, B.; Turaiche, M.; Tirnea, L.; Timircan, M. Predictive Value of Comorbid Conditions for COVID-19 Mortality. J. Clin. Med. 2021, 10, 2652. [Google Scholar] [CrossRef]
- Pantea Stoian, A.; Pricop-Jeckstadt, M.; Pana, A.; Ileanu, B.V.; Schitea, R.; Geanta, M.; Catrinoiu, D.; Suceveanu, A.I.; Serafinceanu, C.; Pituru, S.; et al. Death by SARS-CoV 2: A Romanian COVID-19 Multi-Centre Comorbidity Study. Sci. Rep. 2020, 10, 21613. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, S.R.; Das, D.C.; Sunna, T.C.; Beyene, J.; Hossain, A. Global and Regional Prevalence of Multimorbidity in the Adult Population in Community Settings: A Systematic Review and Meta-Analysis. eClinicalMedicine 2023, 57, 101860. [Google Scholar] [CrossRef]
- Gerayeli, F.V.; Milne, S.; Cheung, C.; Li, X.; Yang, C.W.T.; Tam, A.; Choi, L.H.; Bae, A.; Sin, D.D. COPD and the Risk of Poor Outcomes in COVID-19: A Systematic Review and Meta-Analysis. EClinicalMedicine 2021, 33, 100789. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.C.; Son, K.J.; Han, C.H.; Park, S.C.; Jung, J.Y. Impact of COPD on COVID-19 Prognosis: A Nationwide Population-Based Study in South Korea. Sci. Rep. 2021, 11, 83226. [Google Scholar] [CrossRef]
- Girardin, J.-L.; Seixas, A.; Ramos Cejudo, J.; Osorio, R.S.; Avirappattu, G.; Reid, M.; Parthasarathy, S. Contribution of Pulmonary Diseases to COVID-19 Mortality in a Diverse Urban Community of New York. Chronic Respir. Dis. 2021, 18, 1479973120986806. [Google Scholar] [CrossRef]
- Guan, W.-J.; Liang, W.H.; Shi, Y.; Gan, L.X.; Wang, H.B.; He, J.X.; Zhong, N.S. Chronic Respiratory Diseases and the Outcomes of COVID-19: A Nationwide Retrospective Cohort Study of 39,420 Cases. J. Allergy Clin. Immunol. Pract. 2021, 9, 2645–2655.e14. [Google Scholar] [CrossRef] [PubMed]
- Cai, Z.; Yang, Y.; Zhang, J. Obesity Is Associated with Severe Disease and Mortality in Patients with Coronavirus Disease 2019 (COVID-19): A Meta-Analysis. BMC Public Health 2021, 21, 1505. [Google Scholar] [CrossRef]
- Stevanovic, D.; Zdravkovic, V.; Poskurica, M.; Petrovic, M.; Cekerevac, I.; Zdravkovic, N.; Mijailovic, S.; Todorovic, D.; Divjak, A.; Bozic, D.; et al. The Role of Bioelectrical Impedance Analysis in Predicting COVID-19 Outcome. Front. Nutr. 2022, 9, 906659. [Google Scholar] [CrossRef]
- Sun, Y.; Guan, X.; Jia, L.; Xing, N.; Cheng, L.; Liu, B.; Zhang, S.; He, K. Independent and Combined Effects of Hypertension and Diabetes on Clinical Outcomes in Patients with COVID-19: A Retrospective Cohort Study of Huoshen Mountain Hospital and Guanggu Fangcang Shelter Hospital. J. Clin. Hypertens. 2020, 23, 218–231. [Google Scholar] [CrossRef]
- Tadic, M.; Saeed, S.; Grassi, G.; Taddei, S.; Mancia, G.; Cuspidi, C. Hypertension and COVID-19: Ongoing Controversies. Front. Cardiovasc. Med. 2021, 8, 639222. [Google Scholar] [CrossRef]
- Bauer, A.Z.; Gore, R.; Sama, S.R.; Rosiello, R.; Garber, L.; Sundaresan, D.; McDonald, A.; Arruda, P.; Kriebel, D. Hypertension, Medications, and Risk of Severe COVID-19: A Massachusetts Community-based Observational Study. J. Clin. Hypertens. 2020, 23, 21–27. [Google Scholar] [CrossRef]
- Barrera, F.J.; Shekhar, S.; Wurth, R.; Moreno-Pena, P.J.; Ponce, O.J.; Hajdenberg, M.; Alvarez-Villalobos, N.A.; Hall, J.E.; Schiffrin, E.; Eisenhofer, G.; et al. Prevalence of Diabetes and Hypertension and Their Associated Risks for Poor Outcomes in COVID-19 Patients. J. Endocr. Soc. 2020, 4, bvaa102. [Google Scholar] [CrossRef]
- Wang, S.; Zhu, R.; Zhang, C.; Guo, Y.; Lv, M.; Zhang, C.; Bian, C.; Jiang, R.; Zhou, W.; Guo, L. Effects of the Pre-Existing Coronary Heart Disease on the Prognosis of COVID-19 Patients: A Systematic Review and Meta-Analysis. PLoS ONE 2023, 18, e0292021. [Google Scholar] [CrossRef] [PubMed]
- Sokolski, M.; Reszka, K.; Suchocki, T.; Adamik, B.; Doroszko, A.; Drobnik, J.; Gorka-Dynysiewicz, J.; Jedrzejczyk, M.; Kaliszewski, K.; Kilis-Pstrusinska, K.; et al. History of Heart Failure in Patients Hospitalized Due to COVID-19: Relevant Factor of In-Hospital Complications and All-Cause Mortality up to Six Months. J. Clin. Med. 2022, 11, 241. [Google Scholar] [CrossRef]
- Chen, M.-Y.; Xiao, F.P.; Kuai, L.; Zhou, H.B.; Jia, Z.Q.; Liu, M.; He, H.; Hong, M. Outcomes of Atrial Fibrillation in Patients with COVID-19 Pneumonia: A Systematic Review and Meta-Analysis. Am. J. Emerg. Med. 2021, 50, 661–669. [Google Scholar] [CrossRef] [PubMed]
- Rosenblatt, A.G.; Ayers, C.R.; Rao, A.; Howell, S.J.; Hendren, N.S.; Zadikany, R.H.; Ebinger, J.E.; Daniels, J.D.; Link, M.S.; de Lemos, J.A.; et al. New-Onset Atrial Fibrillation in Patients Hospitalized With COVID-19: Results from the American Heart Association COVID-19 Cardiovascular Registry. Circ. Arrhythmia Electrophysiol. 2022, 15, e010666. [Google Scholar] [CrossRef]
- Artborg, A.; Caldinelli, A.; Wijkström, J.; Nowak, A.; Fored, M.; Stendhal, M.; Evans, M.; Rydell, H. Risk Factors for COVID-19 Hospitalization and Mortality in Patients with Chronic Kidney Disease: A Nationwide Cohort Study. Clin. Kidney J. 2024, 17, sfad283. [Google Scholar] [CrossRef]
- Kim, D.; Adeniji, N.; Latt, N.; Kumar, S.; Bloom, P.P.; Aby, E.S.; Perumalswami, P.; Roytman, M.; Li, M.; Vogel, A.S.; et al. Predictors of Outcomes of COVID-19 in Patients with Chronic Liver Disease: US Multi-Center Study. Clin. Gastroenterol. Hepatol. 2021, 19, 1469–1479.e19. [Google Scholar] [CrossRef] [PubMed]
- Grgurevic, I.; Lucijanić, M.; Pastrovic, F.; Barisic Jaman, M.; Tjesic Drinkovic, I.; Zelenika, M.; Milosevic, M.; Medic, B.; Kardum, D.; Bokun, T.; et al. The Short-term Outcomes of Patients with Chronic Liver Disease Hospitalized with COVID-19. Intern. Med. J. 2022, 52, 1433–1438. [Google Scholar] [CrossRef]
- Chang, Y.; Jeon, J.; Song, T.J.; Kim, J. Association between the Fatty Liver Index and the Risk of Severe Complications in COVID-19 Patients: A Nationwide Retrospective Cohort Study. BMC Infect. Dis. 2022, 22, 384. [Google Scholar] [CrossRef]
- Romero Starke, K.; Reissig, D.; Petereit-Haack, G.; Schmauder, S.; Nienhaus, A.; Seidler, A. The Isolated Effect of Age on the Risk of COVID-19 Severe Outcomes: A Systematic Review with Meta-Analysis. BMJ Glob. Health 2021, 6, e006434. [Google Scholar] [CrossRef]
- Fabião, J.; Sassi, B.; Pedrollo, E.F.; Gerchman, F.; Kramer, C.K.; Leitão, C.B.; Pinto, L.C. Why Do Men Have Worse COVID-19-Related Outcomes? A Systematic Review and Meta-Analysis with Sex Adjusted for Age. Braz. J. Med. Biol. Res. 2022, 55, e11711. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
