The Impact of Age and Sex on Mouse Models of Melioidosis
Abstract
1. Introduction
2. Results
2.1. The Impact of Sex on the Disease Outcome in the Mouse Model of B. pseudomallei Infection
2.2. The Impact of Age on the Disease Outcome in the Mouse Model of B. pseudomallei Infection
2.3. The Impact of Animal Supplier on the Disease Outcome in the Mouse Model of B. pseudomallei Infection
2.4. Sex-Specific Pathology Associated with B. pseudomallei Infection in Mice
2.4.1. Intraperitoneal Route of Infection
2.4.2. Inhalational Route of Infection
3. Discussion
4. Materials and Methods
4.1. Animal Challenges
4.2. Histological Pathology
4.3. Ethics Statement
4.4. Statistical Analyses
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Dance, D.A. Melioidosis: The tip of the iceberg? Clin. Microbiol. Rev. 1991, 4, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Dance, D.A. Melioidosis as an emerging global problem. Acta Trop. 2000, 74, 115–119. [Google Scholar] [CrossRef]
- Limmathurotsakul, D.; Golding, N.; Dance, D.A.; Messina, J.P.; Pigott, D.M.; Moyes, C.L.; Rolim, D.B.; Bertherat, E.; Day, N.P.; Peacock, S.J.; et al. Predicted global distribution of and burden of melioidosis. Nat. Microbiol. 2016, 1, 15008. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.R.; Pani, S.P.; Peng, N.P.; Voralu, K.; Vijayalakshmi, N.; Mehanderkar, R.; Aziz, N.A.; Michael, E. Incidence, risk factors and clinical epidemiology of melioidosis: A complex socio-ecological emerging infectious disease in the Alor Setar region of Kedah, Malaysia. BMC Infect. Dis. 2010, 10, 302. [Google Scholar] [CrossRef]
- Thomas, R.J.; Davies, C.; Nunez, A.; Hibbs, S.; Eastaugh, L.; Harding, S.; Jordan, J.; Barnes, K.; Oyston, P.; Eley, S. Particle-size dependent effects in the BALB/c murine model of inhalational melioidosis. Front. Cell. Infect. Microbiol. 2012, 2, 101. [Google Scholar] [CrossRef]
- West, T.E.; Myers, N.D.; Liggitt, H.D.; Skerrett, S.J. Murine pulmonary infection and inflammation induced by inhalation of Burkholderia pseudomallei. Int. J. Exp. Pathol. 2012, 93, 421–428. [Google Scholar] [CrossRef]
- Limmathurotsakul, D.; Wongsuvan, G.; Aanensen, D.; Ngamwilai, S.; Saiprom, N.; Rongkard, P.; Thaipadungpanit, J.; Kanoksil, M.; Chantratita, N.; Day, N.P.J.; et al. Melioidosis caused by Burkholderia pseudomallei in drinking water, Thailand, 2012. Emerg. Infect. Dis. 2014, 20, 265–268. [Google Scholar] [CrossRef]
- Suputtamongkol, Y.; Chaowagul, W.; Chetchotisakd, P.; Lertpatanasuwun, N.; Intaranongpai, S.; Ruchutrakool, T.; Budhsarawong, D.; Mootsikapun, P.; Wuthiekanun, V.; Teerawatasook, N.; et al. Risk factors for melioidosis and bacteremic melioidosis. Clin. Infect. Dis. 1999, 29, 408–413. [Google Scholar] [CrossRef]
- Amemiya, K.; Bozue, J.A.; Cote, C.K.; DeShazer, D.; Soffler, C.; Welkos, S.L.; Worsham, P.L. Animal models for melioidosis. Curr. Trop. Med. Rep. 2017, 4, 208–222. [Google Scholar] [CrossRef]
- Currie, B.J.; Jacups, S.P. Intensity of rainfall and severity of melioidosis, Australia. Emerg. Infect. Dis. 2003, 9, 1538–1542. [Google Scholar] [CrossRef]
- Liu, X.; Pang, L.; Sim, S.H.; Goh, K.T.; Ravikumar, S.; Win, M.S.; Tan, G.; Cook, A.R.; Fisher, D.; Chai, L.Y. Association of melioidosis incidence with rainfall and humidity, Singapore, 2003-2012. Emerg. Infect. Dis. 2015, 21, 159–162. [Google Scholar] [CrossRef] [PubMed]
- Meumann, E.M.; Cheng, A.C.; Ward, L.; Currie, B.J. Clinical features and epidemiology of melioidosis pneumonia: Results from a 21-year study and review of the literature. Clin. Infect. Dis. 2012, 54, 362–369. [Google Scholar] [CrossRef] [PubMed]
- Currie, B.J. Melioidosis: An important cause of pneumonia in residents of and travellers returned from endemic regions. Eur. Respir. J. 2003, 22, 542–550. [Google Scholar] [CrossRef] [PubMed]
- Dance, D. Treatment and prophylaxis of melioidosis. Int. J. Antimicrob. Agents 2014, 43, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Limmathurotsakul, D.; Funnell, S.G.; Torres, A.G.; Morici, L.A.; Brett, P.J.; Dunachie, S.; Atkins, T.; Altmann, T.M.; Bancroft, G.; Peacock, S.J.; et al. Consensus on the development of vaccines against naturally acquired melioidosis. Emerg. Infect. Dis. 2015, 21, e141480. [Google Scholar] [CrossRef] [PubMed]
- Peacock, S.J.; Limmathurotsakul, D.; Lubell, Y.; Koh, G.C.; White, L.J.; Day, N.P.; Titball, R.W. Melioidosis vaccines: A systematic review and appraisal of the potential to exploit biodefense vaccines for public health purposes. PLoS Negl. Trop. Dis. 2012, 6, e1488. [Google Scholar] [CrossRef] [PubMed]
- Barnes, J.L.; Ketheesan, N. Route of infection in melioidosis. Emerg. Infect. Dis. 2005, 11, 638–639. [Google Scholar] [CrossRef]
- Barnes, J.L.; Ulett, G.C.; Ketheesan, N.; Clair, T.; Summers, P.M.; Hirst, R.G. Induction of multiple chemokine and colony-stimulating factor genes in experimental Burkholderia pseudomallei infection. Immunol. Cell Biol. 2001, 79, 490–501. [Google Scholar] [CrossRef]
- Barnes, J.L.; Warner, J.; Melrose, W.; Durrheim, D.; Speare, R.; Reeder, J.C.; Ketheesan, N. Adaptive immunity in melioidosis: A possible role for T cells in determining outcome of infection with Burkholderia pseudomallei. Clin. Immunol. 2004, 113, 22–28. [Google Scholar] [CrossRef]
- Barnes, J.L.; Williams, N.L.; Ketheesan, N. Susceptibility to Burkholderia pseudomallei is associated with host immune responses involving tumor necrosis factor receptor-1 (TNFR1) and TNF receptor-2 (TNFR2). FEMS Immunol. Med. Microbiol. 2008, 52, 379–388. [Google Scholar] [CrossRef]
- Leakey, A.K.; Ulett, G.C.; Hirst, R.G. BALB/c and C57Bl/6 mice infected with virulent Burkholderia pseudomallei provide contrasting animal models for the acute and chronic forms of human melioidosis. Microb. Pathog. 1998, 24, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Bearss, J.J.; Hunter, M.; Dankmeyer, J.L.; Fritts, K.A.; Klimko, C.P.; Weaver, C.H.; Shoe, J.L.; Quirk, A.V.; Toothman, R.G.; Webster, W.M.; et al. Characterization of pathogenesis of and immune response to Burkholderia pseudomallei K96243 using both inhalational and intraperitoneal infection models in BALB/c and C57BL/6 mice. PLoS ONE 2017, 12, e0172627. [Google Scholar] [CrossRef] [PubMed]
- Tan, G.Y.; Liu, Y.; Sivalingam, S.P.; Sim, S.H.; Wang, D.; Paucod, J.C.; Gathier, Y.; Ooi, E.E. Burkholderia pseudomallei aerosol infection results in differential inflammatory responses in BALB/c and C57Bl/6 mice. J. Med. Microbiol. 2008, 57, 508–515. [Google Scholar] [CrossRef] [PubMed]
- Trevino, S.R.; Klimko, C.P.; Reed, M.C.; Aponte-Cuadrado, M.J.; Hunter, M.; Shoe, J.L.; Meyer, J.R.; Dankmeyer, J.L.; Biryukov, S.S.; Quirk, A.V.; et al. Disease progression in mice exposed to low-doses of aerosolized clinical isolates of Burkholderia pseudomallei. PLoS ONE 2018, 13, e0208277. [Google Scholar] [CrossRef] [PubMed]
- Welkos, S.L.; Klimko, C.P.; Kern, S.J.; Bearss, J.J.; Bozue, J.; Bernhards, R.C.; Trevin, S.; Waag, D.M.; Amemiya, K.; Worsham, P.; et al. Characterization of Burkholderia pseudomallei strains using a murine intraperitoneal infection model and in vitro macrophage assays. PLoS ONE 2015, 10, e0124667. [Google Scholar] [CrossRef] [PubMed]
- Amemiya, K.; Dankmeyer, J.L.; Fetterer, D.P.; Worsham, P.L.; Welkos, S.L.; Cote, C.K. Comparison of the early host immune response to two widely diverse virulent strains of Burkholderia pseudomallei that cause acute and chronic infections in BALB/c mice. Microb. Pathog. 2015, 86, 53–63. [Google Scholar] [CrossRef]
- Van Zandt, K.E.; Tuanyok, A.; Keim, P.S.; Warren, R.L.; Gelhaus, H.C. An objective approach for Burkholderia pseudomallei strain selection as challenge material for medical countermeasures efficacy testing. Front. Cell. Infect. Microbiol. 2012, 2, 120. [Google Scholar] [CrossRef]
- Dannenberg, A.M.; Scott, E.M., Jr. Melioidosis: Pathogenesis and immunity in mice and hamsters. I. Studies with virulent strains of Malleomyces pseudomallei. J. Exp. Med. 1958, 107, 153–166. [Google Scholar] [CrossRef]
- Raja, N.S.; Scarsbrook, C. Burkholderia Pseudomallei Causing Bone and Joint Infections: A Clinical Update. Infect. Dis. Ther. 2016, 5, 17–29. [Google Scholar] [CrossRef]
- Teparrakkul, P.; Tsai, J.J.; Chierakul, W.; Gerstenmaier, J.F.; Wacharaprechasgu, T.; Piyaphanee, W.; Limmathurotsakul, D.; Chaowagul, W.; Day, N.P.; Peacock, S.J. Rheumatological manifestations in patients with melioidosis. Southeast Asian J. Trop. Med. Public Health 2008, 39, 649–655. [Google Scholar]
- Chen, P.S.; Chen, Y.S.; Lin, H.H.; Liu, P.J.; Ni, W.F.; Hsueh, P.T.; Liang, S.H.; Chen, C.; Chen, Y.L. Airborne transmission of melioidosis to humans from environmental aerosols contaminated with B. pseudomallei. PLoS Negl. Trop. Dis. 2015, 9, e0003834. [Google Scholar] [CrossRef] [PubMed]
- Lever, M.S.; Nelson, M.; Stagg, A.J.; Beedham, R.J.; Simpson, A.J. Experimental acute respiratory Burkholderia pseudomallei infection in BALB/c mice. Int. J. Exp. Pathol. 2009, 90, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Massey, S.; Yeager, L.A.; Blumentritt, C.A.; Vijayakumar, S.; Sbrana, E.; Peterson, J.W.; Brasel, T.; LeDuc, J.W.; Endsley, J.J.; Torres, A.G. Comparative Burkholderia pseudomallei natural history virulence studies using an aerosol murine model of infection. Sci. Rep. 2014, 4, 4305. [Google Scholar] [CrossRef] [PubMed]
- Challacombe, J.F.; Stubben, C.J.; Klimko, C.P.; Welkos, S.L.; Kern, S.J.; Bozue, J.A.; Worsham, P.L.; Cote, C.K.; Wolfe, D.L. Interrogation of the Burkholderia pseudomallei Genome to Address Differential Virulence among Isolates. PLoS ONE 2014, 9, e115951. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, I.; Brenneke, B.; Rohde, M.; Kreft, A.; Häußler, S.; Reganzerowski, A.; Steinmetz, I. Characterization of a murine model of melioidosis: Comparison of different strains of mice. Infect. Immun. 1999, 67, 2891–2900. [Google Scholar] [CrossRef] [PubMed]
- Webster Marketon, J.I.; Glaser, R. Stress hormones and immune function. Cell. Immunol. 2008, 252, 16–26. [Google Scholar] [CrossRef]
- Corea, E.M.; Merritt, A.J.; Ler, Y.H.; Thevanesam, V.; Inglis, T.J. Sri Lankan National Melioidosis surveillance program uncovers a nationwide distribution of invasive melioidosis. Am. J. Trop. Med. Hyg. 2016, 94, 292–298. [Google Scholar] [CrossRef][Green Version]
- Currie, B.J.; Jacups, S.P.; Cheng, A.C.; Fisher, D.A.; Anstey, N.M.; Huffam, S.E.; Krause, V.L. Melioidosis epidemiology and risk factors from a prospective whole-population study in northern Australia. Trop. Med. Int. Health 2004, 9, 1167–1174. [Google Scholar] [CrossRef]
- Suntornsut, P.; Kasemsupat, K.; Silairatana, S.; Wongsuvan, G.; Jutrakul, Y.; Wuthiekanun, V.; Day, N.P.; Peacock, S.J.; Limmathurotsakul, D. Prevalence of melioidosis in patients with suspected pulmonary tuberculosis and sputum smear negative for acid-fast bacilli in northeast Thailand. Am. J. Trop. Med. Hyg. 2013, 89, 983–985. [Google Scholar] [CrossRef]
- Klein, S.L.; Flanagan, K.L. Sex differences in immune responses. Nat. Rev. Immunol. 2016, 16, 626–638. [Google Scholar] [CrossRef]
- Chirakul, S.; Bartpho, T.; Wongsurawat, T.; Taweechaisupapong, S.; Karoonutaisiri, N.; Talaat, A.M.; Wongratanacheewin, S.; Ernst, R.K.; Sermswan, R.W. Characterization of BPSS1521 (bprD), a regulator of Burkholderia pseudomallei virulence gene expression in the mouse model. PLoS ONE 2014, 9, e104313. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gelhaus, H.C.; Anderson, M.S.; Fisher, D.A.; Flavin, M.T.; Xu, Z.Q.; Sanford, D.C. Efficacy of post exposure administration of doxycycline in a murine model of inhalational melioidosis. Sci. Rep. 2013, 3, 1146. [Google Scholar] [CrossRef]
- Ulett, G.C.; Ketheesan, N.; Hirst, R.G. Cytokine gene expression in innately susceptible BALB/c mice and relatively resistant C57BL/6 mice during infection with virulent Burkholderia pseudomallei. Infect. Immun. 2000, 68, 2034–2042. [Google Scholar] [CrossRef] [PubMed]
- Wiersinga, W.J.; Calandra, T.; Kager, L.M.; van der Windt, G.J.; Roger, T.; le Roy, D.; Florquin, S.; Peacock, S.J.; Sweep, F.C.; van der Poll, T. Expression and function of macrophage migration inhibitory factor (MIF) in melioidosis. PLoS Negl. Trop. Dis. 2010, 4, e605. [Google Scholar] [CrossRef] [PubMed]
- Hodgson, K.A.; Govan, B.L.; Walduck, A.K.; Ketheesan, N.; Morris, J.L. Impaired early cytokine responses at the site of infection in a murine model of type 2 diabetes and melioidosis comorbidity. Infect. Immun. 2013, 81, 470–477. [Google Scholar] [CrossRef]
- Puangpetch, A.; Anderson, R.; Huang, Y.Y.; Sermswan, R.W.; Chaicumpa, W.; Sirisinha, S.; Wongratanacheewin, S. Cationic liposomes extend the immunostimulatory effect of CpG oligodeoxynucleotide against Burkholderia pseudomallei infection in BALB/c mice. Clin. Vaccine Immunol. 2012, 19, 675–683. [Google Scholar] [CrossRef]
- Tay, T.F.; Maheran, M.; Too, S.L.; Hasidah, M.S.; Ismail, G.; Embi, N. Glycogen synthase kinase-3beta inhibition improved survivability of mice infected with Burkholderia pseudomallei. Trop Biomed. 2012, 29, 551–567. [Google Scholar]
- Kager, L.M.; Weehuizen, T.A.; Wiersinga, W.J.; Roelofs, J.J.; Meijers, J.C.; Dondorp, A.M.; van‘t Veer, C.; van der Poll, T. Endogenous alpha2-antiplasmin is protective during severe gram-negative sepsis (melioidosis). Am. J. Respir. Crit. Care Med. 2013, 188, 967–975. [Google Scholar] [CrossRef]
- Kager, L.M.; Wiersinga, W.J.; Roelofs, J.J.; Stroo, I.; Achouiti, A.; van’t Veer, C.; Conway, E.M.; van der Poll, T. Mice lacking the lectin-like domain of thrombomodulin are protected against melioidosis. Crit. Care Med. 2014, 42, e221–e230. [Google Scholar] [CrossRef]
- Weehuizen, T.A.; Wieland, C.W.; van der Windt, G.J.; Duitman, J.W.; Boon, L.; Day, N.P.; Peacock, S.J.; van der Poll, T.; Wiersinga, W.J. Expression and function of transforming growth factor beta in melioidosis. Infect. Immun. 2012, 80, 1853–1857. [Google Scholar] [CrossRef]
- Mariappan, V.; Vellasamy, K.M.; Vadivelu, J. Host-adaptation of Burkholderia pseudomallei alters metabolism and virulence: A global proteome analysis. Sci. Rep. 2017, 7, 9015. [Google Scholar] [CrossRef] [PubMed]
- Weehuizen, T.A.; Prior, J.L.; van der Vaart, T.W.; Ngugi, S.A.; Nepogodiev, S.A.; Field, R.A.; Kager, L.M.; van’t Veer, C.; de Vos, A.F.; Wiersinga, W.J. Differential Toll-like receptor-signalling of Burkholderia pseudomallei lipopolysaccharide in murine and human models. PLoS ONE 2015, 10, e0145397. [Google Scholar] [CrossRef] [PubMed]
- Emery, F.D.; Parvathareddy, J.; Pandey, A.K.; Cui, Y.; Williams, R.W.; Miller, M.A. Genetic control of weight loss during pneumonic Burkholderia pseudomallei infection. Pathog. Dis. 2014, 71, 249–264. [Google Scholar] [CrossRef] [PubMed]
- Kager, L.M.; Wiersinga, W.J.; Roelofs, J.J.; de Boer, O.J.; Weiler, H.; van’t Veer, C.; van der Poll, T. A thrombomodulin mutation that impairs active protein C generation is detrimental in severe pneumonia-derived gram-negative sepsis (melioidosis). PLoS Negl. Trop. Dis. 2014, 8, e2819. [Google Scholar] [CrossRef] [PubMed]
- Baker, D.G. Natural pathogens of laboratory mice, rats, and rabbits and their effects on research. Clin. Microbiol. Rev. 1998, 11, 231–266. [Google Scholar] [CrossRef]
- Kline, K.A.; Schwartz, D.J.; Gilbert, N.M.; Lewis, A.L. Impact of host age and parity on susceptibility to severe urinary tract infection in a murine model. PLoS ONE 2014, 9, e97798. [Google Scholar] [CrossRef]
- Han, S.N.; Meydani, S.N. Antioxidants, cytokines, and influenza infection in aged mice and elderly humans. J. Infect. Dis. 2000, 182, S74–S80. [Google Scholar] [CrossRef]
- Lu, J.; Duan, X.; Zhao, W.; Wang, J.; Wang, H.; Zhou, K.; Fang, M. Aged mice are more resistant to influenza virus infection due to reduced inflammation and lung pathology. Aging Dis. 2018, 9, 358–373. [Google Scholar] [CrossRef]
- Pal, S.; Peterson, E.M.; de la Maza, L.M. Susceptibility of mice to vaginal infection with Chlamydia trachomatis mouse pneumonitis is dependent on the age of the animal. Infect. Immun. 2001, 69, 5203–5206. [Google Scholar] [CrossRef][Green Version]
- Puchta, A.; Naidoo, A.; Verschoor, C.P.; Loukov, D.; Thevaranjan, N.; Mandur, T.S.; Nguyen, P.S.; Jordana, M.; Loeb, M.; Xing, Z.; et al. TNF drives monocyte dysfunction with age and results in impaired anti-pneumococcal immunity. PLoS Pathog. 2016, 12, e1005368. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, Y.; Gilmore, X.; Xu, K.; Wyde, P.R.; Mbawuike, I.N. An aged mouse model for RSV infection and diminished CD8+ CTL response. Exp. Biol. Med. 2002, 227, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Ngauy, V.; Lemeshev, Y.; Sadkowski, L.; Crawford, G. Cutaneous melioidosis in a man who was taken as a prisoner of war by the Japanese during World War II. J. Clin. Microbiol. 2005, 43, 970–972. [Google Scholar] [CrossRef] [PubMed]
- Limmathurotsakul, D.; Chaowagul, W.; Chantratita, N.; Wuthiekanun, V.; Biaklang, M.; Tumapa, S.; White, N.J.; Day, N.P.; Peacock, S.J. A simple scoring system to differentiate between relapse and re-infection in patients with recurrent melioidosis. PLoS Negl. Trop. Dis. 2008, 2, e327. [Google Scholar] [CrossRef] [PubMed]
- Jenjaroen, K.; Chumseng, S.; Sumonwiriya, M.; Ariyaprasert, P.; Chantratita, N.; Sunyakumthorn, P.; Hongsuwan, M.; Wuthiekanun, V.; Fletcher, H.A.; Teparrukkul, P.; et al. T-cell responses are associated with survival in acute melioidosis patients. PLoS Negl. Trop. Dis. 2015, 9, e0004152. [Google Scholar] [CrossRef] [PubMed]
- Of mice and men—are mice relevant models for human disease? Available online: https://ec.europa.eu/research/health/pdf/summary-report-25082010_en.pdf (accessed on 29 January 2020).
- Justice, M.J.; Dhillon, P. Using the mouse to model human disease: Increasing validity and reproducibility. Dis. Models Mech. 2016, 9, 101–103. [Google Scholar] [CrossRef]
- Uhl, E.W.; Warner, N.J. Mouse models as predictors of human responses: Evolutionary medicine. Curr. Pathobiol. Rep. 2015, 3, 219–223. [Google Scholar] [CrossRef]
- Kozlowska, J.; Smith, S.; Roberts, J.; Pridgeon, S.; Hanson, J. Prostatic abscess due to Burkholderia pseudomallei: Facilitating diagnosis to optimize management. Am. J. Trop. Med. Hyg. 2018, 98, 227–230. [Google Scholar] [CrossRef]
- Morse, L.P.; Moller, C.C.; Harvey, E.; Ward, L.; Cheng, A.C.; Carson, P.J.; Currie, B.J. Prostatic abscess due to Burkholderia pseudomallei: 81 cases from a 19-year prospective melioidosis study. J. Urol. 2009, 182, 542–547, discussion 7. [Google Scholar] [CrossRef]
- Currie, B.J.; Ward, L.; Cheng, A.C. The epidemiology and clinical spectrum of melioidosis: 540 cases from the 20 year Darwin prospective study. PLoS Negl. Trop. Dis. 2010, 4, e900. [Google Scholar] [CrossRef]
- Chee, Y.C.; Chee, Y.N. An unusual case of primary melioidotic prostatic abscess complicated by perianal abscess. IDCases 2018, 11, 51–52. [Google Scholar] [CrossRef]
- Nernsai, P.; Sophonsritsuk, A.; Lertvikool, S.; Jinawath, A.; Chitasombat, M.N. A case report of Tubo-ovarian abscess caused by Burkholderia pseudomallei. BMC Infect. Dis. 2018, 18, 73. [Google Scholar] [CrossRef] [PubMed]
- Barthold, S.W.; Griffey, S.M.; Percy, D.H. Pathology of Laboratory Rodents and Rabbits, 4th ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2016. [Google Scholar]
- Van Loo, P.L.P.; Van der Meer, E.; Kruitwagen, C.L.J.J.; Koolhaas, J.M.; Van Zutphen, L.F.M.; Baumans, V. Strain-specific aggressive behavior of male mice submitted to different husbandry procedures. Aggress. Behav. 2003, 29, 69–80. [Google Scholar] [CrossRef]
- Kappel, S.; Hawkins, P.; Mendl, M.T. To group or not to group? Good practice for housing male laboratory mice. Animals 2017, 7, 88. [Google Scholar] [CrossRef] [PubMed]
- Dorshkind, K.; Swain, S. Age-associated declines in immune system development and function: Causes, consequences, and reversal. Curr. Opin. Immunol. 2009, 21, 404–407. [Google Scholar] [CrossRef] [PubMed]
- Kishimoto, S.; Tsuyuguchi, I.; Yamamura, Y. Immune responses in aged mice. Clin. Exp. Immunol. 1969, 5, 525–530. [Google Scholar]
- Montecino-Rodriguez, E.; Berent-Maoz, B.; Dorshkind, K. Causes, consequences, and reversal of immune system aging. J. Clin. Investig. 2013, 123, 958–965. [Google Scholar] [CrossRef]
- Myers, C.E.; Mirza, N.N.; Lustgarten, J. Immunity, cancer and aging: Lessons from mouse models. Aging Dis. 2011, 2, 512–523. [Google Scholar]
- Ren, Z.; Gay, R.; Thomas, A.; Pae, M.; Wu, D.; Logsdon, L.; Mecsas, J.; Meydani1, S.N. Effect of age on susceptibility to Salmonella Typhimurium infection in C57BL/6 mice. J. Med. Microbiol. 2009, 58, 1559–1567. [Google Scholar] [CrossRef]
- Shin, J.H.; Gao, Y.; Moore, J.H.; Bolick, D.T.; Kolling, G.L.; Wu, M.; Warren, C.A. Innate immune response and outcome of Clostridium difficile infection are dependent on fecal bacterial composition in the aged host. J. Infect. Dis. 2018, 217, 188–197. [Google Scholar] [CrossRef]
- Fischer, N.; Relman, D.A. Clostridium difficile, Aging, and the gut: Can microbiome rejuvenation keep us young and healthy? J. Infect. Dis. 2018, 217, 174–176. [Google Scholar] [CrossRef]
- Bowen, W.; Batra, L.; Pulsifer, A.R.; Yolcu, E.S.; Lawrenz, M.B.; Shirwan, H. Robust Th1 cellular and humoral responses generated by the Yersinia pestis rF1-V subunit vaccine formulated to contain an agonist of the CD137 pathway do not translate into increased protection against pneumonic plague. Vaccine 2019, 37, 5708–5716. [Google Scholar] [CrossRef] [PubMed]
- Lambert, N.D.; Langfitt, D.M.; Nilles, M.L.; Bradley, D.S. Resistance to Yersinia pestis infection decreases with age in B10.T(6R) mice. Infect. Immun. 2011, 79, 4438–4446. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mecsas, J.; Franklin, G.; Kuziel, W.A.; Brubaker, R.R.; Falkow, S.; Mosier, D.E. Evolutionary genetics: CCR5 mutation and plague protection. Nature 2004, 427, 606. [Google Scholar] [CrossRef] [PubMed]
- Mares, C.A.; Ojeda, S.S.; Li, Q.; Morris, E.G.; Coalson, J.J.; Teale, J.M. Aged mice display an altered pulmonary host response to Francisella tularensis live vaccine strain (LVS) infections. Exp. Gerontol. 2010, 45, 91–96. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lyons, C.R.; Lovchik, J.; Hutt, J.; Lipscomb, M.F.; Wang, E.; Heninger, S.; Berliba, L.; Garrison, K. Murine model of pulmonary anthrax: Kinetics of dissemination, histopathology, and mouse strain susceptibility. Infect. Immun. 2004, 72, 4801–4809. [Google Scholar] [CrossRef] [PubMed]
- Fulton, R.B.; Weiss, K.A.; Pewe, L.L.; Harty, J.T.; Varga, S.M. Aged mice exhibit a severely diminished CD8 T cell response following respiratory syncytial virus infection. J. Virol. 2013, 87, 12694–12700. [Google Scholar] [CrossRef]
- Wong, T.M.; Boyapalle, S.; Sampayo, V.; Nguyen, H.D.; Bedi, R.; Kamath, S.G.; Moore, M.L.; Mohapatra, S.; Mohapatra, S.S. Respiratory syncytial virus (RSV) infection in elderly mice results in altered antiviral gene expression and enhanced pathology. PLoS ONE 2014, 9, e88764. [Google Scholar] [CrossRef]
- Malinczak, C.A.; Fonseca, W.; Rasky, A.J.; Ptaschinski, C.; Morris, S.; Ziegler, S.F.; Lukacs, N.W. Sex-associated TSLP-induced immune alterations following early-life RSV infection leads to enhanced allergic disease. Mucosal Immunol. 2019, 12, 969–979. [Google Scholar] [CrossRef]
- Fang, M.; Roscoe, F.; Sigal, L.J. Age-dependent susceptibility to a viral disease due to decreased natural killer cell numbers and trafficking. J. Exp. Med. 2010, 207, 2369–2381. [Google Scholar] [CrossRef]
- Grove, K.A.; Smith, P.C.; Booth, C.J.; Compton, S.R. Age-associated variability in susceptibility of Swiss Webster mice to MPV and other excluded murine pathogens. J. Am. Assoc. Lab. Anim. Sci. 2012, 51, 789–796. [Google Scholar]
- Compton, S.R.; Paturzo, F.X.; Macy, J.D. Transmission of mouse parvovirus to neonatoal mice. J. Am. Assoc. Lab. Anim. Sci. 2012, 51, 797–802. [Google Scholar] [PubMed]
- Blazquez, A.B.; Escribano-Romero, E.; Martin-Acebes, M.A.; Petrovic, T.; Saiz, J.C. Limited susceptibility of mice to Usutu virus (USUV) infection and induction of flavivirus cross-protective immunity. Virology 2015, 482, 67–71. [Google Scholar] [CrossRef]
- de Oliveira Souza, I.N.; Frost, P.S.; Franca, J.V.; Nascimento-Viana, J.B.; Neris, R.L.S.; Freitas, L.; Pinheiro, D.J.L.L.; Noqueira, C.O.; Neves, G.; Chimelli, L.; et al. Acute and chronic neurological consequences of early-life Zika virus infection in mice. Sci. Transl. Med. 2018, 10, eaar2749. [Google Scholar] [CrossRef] [PubMed]
- Ryman, K.D.; Gardner, C.L.; Meier, K.C.; Biron, C.A.; Johnston, R.E.; Klimstra, W.B. Early restriction of alphavirus replication and dissemination contributes to age-dependent attenuation of systemic hyperinflammatory disease. J. Gen. Virol. 2007, 88, 518–529. [Google Scholar] [CrossRef] [PubMed]
- Zumbrun, E.E.; Abdeltawab, N.F.; Bloomfield, H.A.; Chance, T.B.; Nichols, D.K.; Harrison, P.E.; Kotb, M.; Nalca, A. Development of a murine model for aerosolized ebolavirus infection using a panel of recombinant inbred mice. Viruses 2012, 4, 3468–3493. [Google Scholar] [CrossRef]
- Chua, J.; Bozue, J.A.; Klimko, C.P.; Shoe, J.L.; Ruiz, S.I.; Jensen, C.L.; Tobery, S.A.; Crumpler, J.M.; Chabot, D.J.; Quirk, A.V.; et al. Formaldehyde and glutaraldehyde inactivation of bacterial Tier 1 select agents in tissues. Emerg. Infect. Dis. 2019, 25, 919–926. [Google Scholar] [CrossRef]
- Davis, K.J.; Vogel, P.; Fritz, D.L.; Steele, K.E.; Pitt, M.L.; Welkos, S.L.; Friedlander, A.M.; Byrne, W.R. Bacterial filamentation of Yersinia pestis by beta-lactam antibiotics in experimentally infected mice. Arch. Pathol. Lab. Med. 1997, 121, 865–868. [Google Scholar]
- Hirschberg, J.; Lye, J. A geometric comparison of the delta and Fieller confidence intervals. Am. Stat. 2010, 64, 234–241. [Google Scholar] [CrossRef]
- Finney, D.J. Probit Analysis, 3rd ed.; Cambridge University Press: New York, NY, USA, 1971. [Google Scholar]
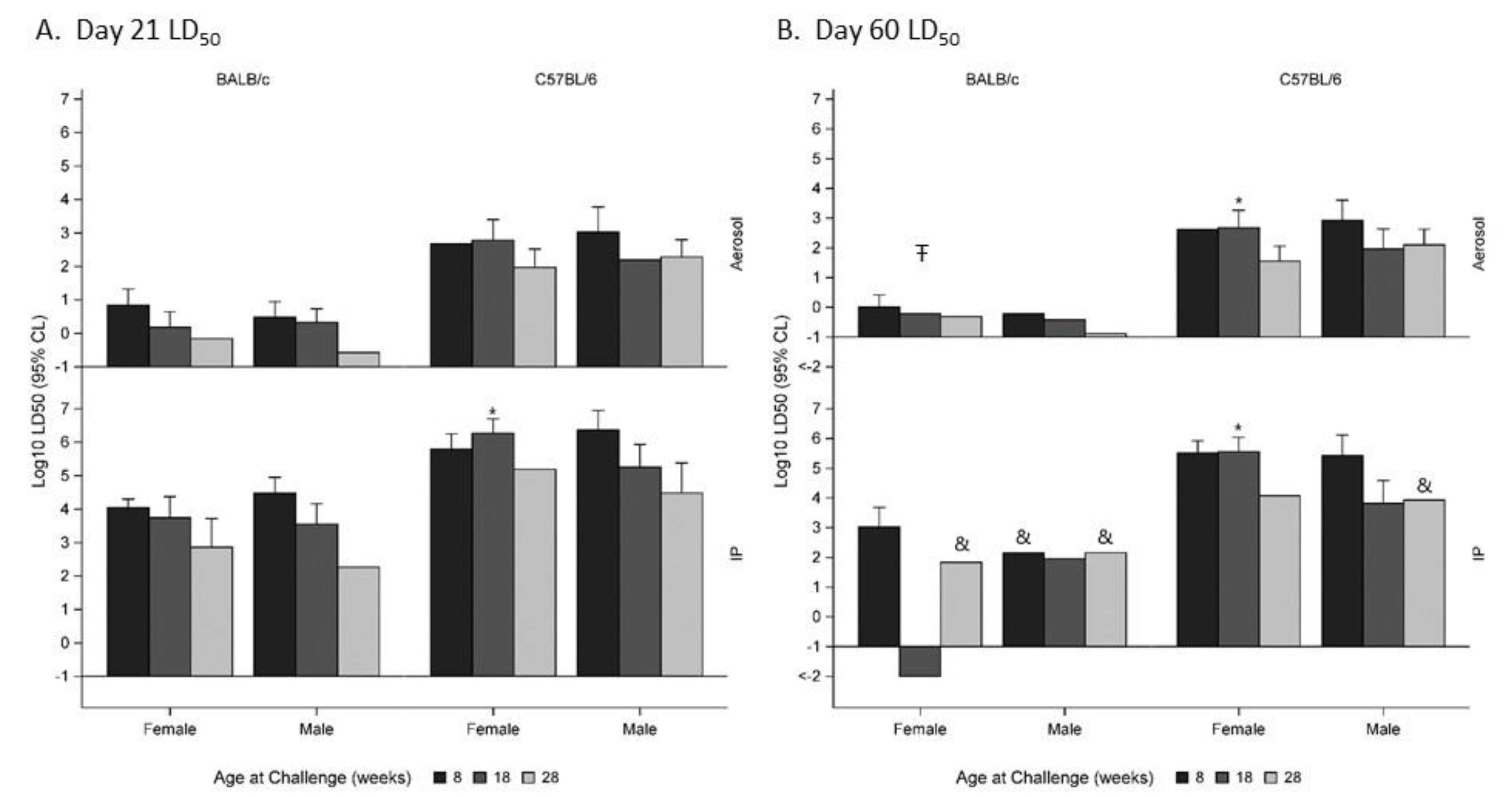



| A. Day 21 LD50 | Age at Exposure (Weeks) | |||||
|---|---|---|---|---|---|---|
| Gender | Exposure Route | Mouse Strain | Dose Range Min, Max | 8 | 18 | 28 |
| Female | Aerosol | BALB/c | −0.16 to 4.00 | 0.84 (0.36, 1.32) | 0.18 (−0.46, 0.64) | −0.16 (−11.14, 0.19) |
| C57BL/6 | −0.19 to 4.02 | 2.67 (− 2) | 2.78 (2.31, 3.40) | 1.97 (1.51, 2.52) | ||
| IP | BALB/c | 1.83 to 5.66 | 4.04 (3.77, 4.29) | 3.74 (3.18, 4.37) | 2.86 (1.04, 3.71) | |
| C57BL/6 | 4.11 to 8.07 | 5.79 (5.32, 6.24) | 6.27 (5.86, 6.70) | 5.19 (− 2) | ||
| Male | Aerosol | BALB/c | −0.18 to 3.26 | 0.48 (0.00, 0.94) | 0.32 (0.04, 0.73) | −0.58 (− 2) |
| C57BL/6 | 0.10 to 4.05 | 3.02 (2.51, 3.77) | 2.19 (− 2) | 2.28 (1.84, 2.80) | ||
| IP | BALB/c | 2.16 to 6.09 | 4.48 (4.05, 4.95) | 3.55 (2.84, 4.16) | 2.26 (−38.27, 3.47) | |
| C57BL/6 | 3.93 to 8.00 | 6.37 (5.87, 6.95) | 5.25 (4.42, 5.93) | 4.48 (1.48, 5.38) | ||
| B. Day 60 LD50 | ||||||
| Female | Aerosol | BALB/c | −0.16 to 4.00 | 0.00 (−1.49, 0.41) | −0.22 (− 2) | −0.32 (− 2) |
| C57BL/6 | −0.19 to 4.02 | 2.62 (− 2) | 2.67 (2.22, 3.26) | 1.55 (1.15, 2.05) | ||
| IP | BALB/c | 1.83 to 5.66 | 3.02 (2.02, 3.68) | −6.47 (− 2) | 1.83 3 | |
| C57BL/6 | 4.11 to 8.07 | 5.51 (5.07, 5.92) | 5.56 (5.07, 6.04) | 4.07 (− 2) | ||
| Male | Aerosol | BALB/c | −0.18 to 3.26 | −0.22 (−19.85, 0.14) | −0.43 (− 2) | −0.89 (− 2) |
| C57BL/6 | 0.10 to 4.05 | 2.92 (2.42, 3.60) | 1.96 (1.36, 2.63) | 2.10 (1.63, 2.63) | ||
| IP | BALB/c | 2.16 to 6.09 | 2.16 3 | 1.95 (− 2) | 2.16 3 | |
| C57BL/6 | 3.93 to 8.00 | 5.42 (4.63, 6.12) | 3.82 (−2.89, 4.59) | 3.93 3 | ||
| . | Age at Exposure (Weeks) | |||||
|---|---|---|---|---|---|---|
| Gender | Exposure Route | Source Vendor | Mouse Strain | 8 | 18 | 28 |
| Female | Aerosol | Charles River | BALB/c | p > 0.05 | ND | ND |
| C57BL/6 | p > 0.05 | ND | ND | |||
| IP | Charles River | BALB/c | p > 0.05 | ND | ND | |
| C57BL/6 | p = 0.037 | ND | ND | |||
| Male | IP | Jackson Laboratory | C57BL/6 | p > 0.05 | p > 0.05 | p > 0.05 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klimko, C.P.; Treviño, S.R.; Moreau, A.M.; Aponte Cuadrado, M.J.; Meyer, J.R.; Fetterer, D.P.; Welkos, S.L.; Worsham, P.L.; Kreiselmeier, N.; Soffler, C.; et al. The Impact of Age and Sex on Mouse Models of Melioidosis. Pathogens 2020, 9, 113. https://doi.org/10.3390/pathogens9020113
Klimko CP, Treviño SR, Moreau AM, Aponte Cuadrado MJ, Meyer JR, Fetterer DP, Welkos SL, Worsham PL, Kreiselmeier N, Soffler C, et al. The Impact of Age and Sex on Mouse Models of Melioidosis. Pathogens. 2020; 9(2):113. https://doi.org/10.3390/pathogens9020113
Chicago/Turabian StyleKlimko, Christopher P., Sylvia R. Treviño, Alicia M. Moreau, Michael J. Aponte Cuadrado, Joshua R. Meyer, David P. Fetterer, Susan L. Welkos, Patricia L. Worsham, Norman Kreiselmeier, Carl Soffler, and et al. 2020. "The Impact of Age and Sex on Mouse Models of Melioidosis" Pathogens 9, no. 2: 113. https://doi.org/10.3390/pathogens9020113
APA StyleKlimko, C. P., Treviño, S. R., Moreau, A. M., Aponte Cuadrado, M. J., Meyer, J. R., Fetterer, D. P., Welkos, S. L., Worsham, P. L., Kreiselmeier, N., Soffler, C., & Cote, C. K. (2020). The Impact of Age and Sex on Mouse Models of Melioidosis. Pathogens, 9(2), 113. https://doi.org/10.3390/pathogens9020113




