The Attenuated Pseudorabies Virus Vaccine Strain Bartha K61: A Brief Review on the Knowledge Gathered during 60 Years of Research
Abstract
1. Introduction
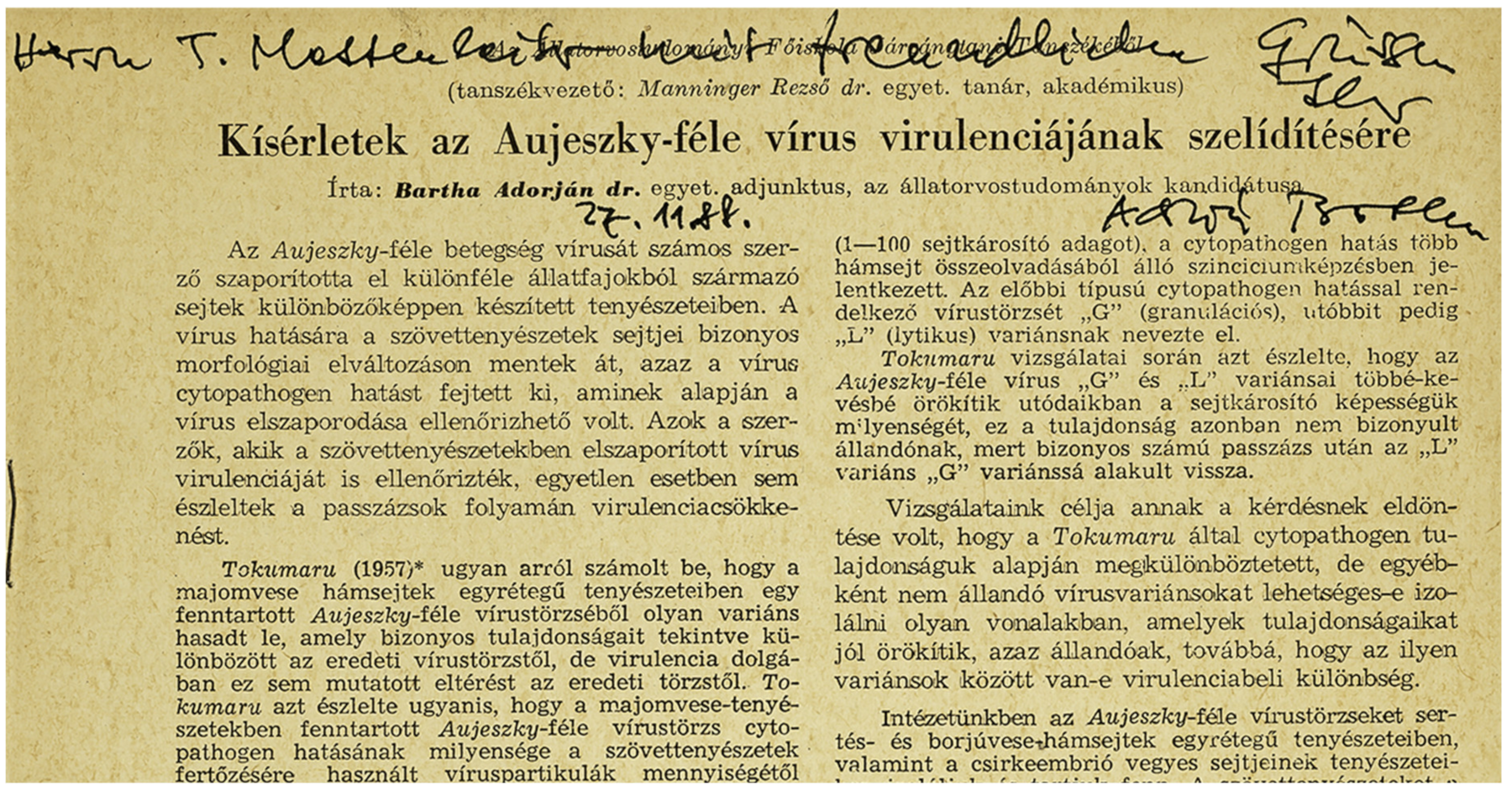
2. History of Aujesky’s Disease Vaccines
3. History of the Bartha K61 Strain
4. Genetic Background of the Bartha K61 Strain
5. The Bartha K61 Strain as a Neuronal Tracer
6. The Bartha K61 Strain as a Vector Vaccine
7. Immunogenicity of the Bartha K61 Strain
8. Concluding Remarks
Author Contributions
Funding
Conflicts of Interest
References
- Roizmann, B.; Desrosiers, R.C.; Fleckenstein, B.; Lopez, C.; Minson, A.C.; Studdert, M.J. The family Herpesviridae: An update. Arch. Virol. 1992, 123, 425–449. [Google Scholar] [CrossRef] [PubMed]
- Nandi, S.; Kumar, M.; Manohar, M.; Chauhan, R.S. Bovine herpes virus infections in cattle. Anim. Health Res. Rev. 2009, 10, 85–98. [Google Scholar] [CrossRef] [PubMed]
- Thiry, E.; Addie, D.; Belák, S.; Boucraut-Baralon, C.; Egberink, H.; Frymus, T.; Gruffydd-Jones, T.; Hartmann, K.; Hosie, M.J.; Lloret, A.; et al. Feline Herpesvirus Infection: ABCD Guidelines on Prevention and Management. J. Feline Med. Surg. 2009, 11, 547–555. [Google Scholar] [CrossRef] [PubMed]
- Dunowska, M. A review of equid herpesvirus 1 for the veterinary practitioner. Part A: Clinical presentation, diagnosis and treatment. New Zealand Vet. J. 2014, 62, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Nauwynck, H.J.; Glorieux, S.; Favoreel, H.; Pensaert, M. Cell biological and molecular characteristics of pseudorabies virus infections in cell cultures and in pigs with emphasis on the respiratory tract. Vet. Res. 2007, 38, 229–241. [Google Scholar] [CrossRef] [PubMed]
- Kritas, S.K.; Pensaert, M.B. Role of gp63 and gIII of Aujeszky’s disease virus in the invasion of the olfactory nervous pathway in neonatal pigs. J. Gen. Virol. 1994, 75, 2319–2327. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.A.; Pomeranz, L.; Gross, S.P.; Enquist, L. Local modulation of plus-end transport targets herpesvirus entry and egress in sensory axons. Proc. Natl. Acad. Sci. USA 2004, 101, 16034–16039. [Google Scholar] [CrossRef]
- Richards, A.L.; Sollars, P.J.; Pitts, J.D.; Stults, A.M.; Heldwein, E.E.; Pickard, G.E.; Smith, G.A. The pUL37 tegument protein guides alpha-herpesvirus retrograde axonal transport to promote neuroinvasion. PLoS Pathog. 2017, 13, e1006741. [Google Scholar] [CrossRef]
- Zaichick, S.V.; Bohannon, K.P.; Hughes, A.; Sollars, P.J.; Pickard, G.E.; Smith, G.A. The herpesvirus VP1/2 protein is an effector of dynein-mediated capsid transport and neuroinvasion. Cell Host Microbe 2013, 13, 193–203. [Google Scholar] [CrossRef]
- Cheung, A.K. Investigation of pseudorabies virus DNA and RNA in trigeminal ganglia and tonsil tissues of latently infected swine. Am. J. Vet. Res. 1995, 56, 45–50. [Google Scholar]
- Mengeling, W.L.; Lager, K.M.; Volz, D.M.; Brockmeier, S.L. Effect of various vaccination procedures on shedding, latency, and reactivation of attenuated and virulent pseudorabies virus in swine. Am. J. Vet. Res. 1992, 53, 2164–2173. [Google Scholar] [PubMed]
- Pomeranz, L.E.; Reynolds, A.E.; Hengartner, C.J. Molecular Biology of Pseudorabies Virus: Impact on Neurovirology and Veterinary Medicine. Microbiol. Mol. Biol. Rev. 2005, 69, 462–500. [Google Scholar] [CrossRef]
- Mettenleiter, T.C.; Ehlers, B.; Müller, T.; Yoon, K.-J.; Teifke, J.P. Viral diseases, Herpesviruses. In Diseases of Swine; Zimmerman, J., Karriker, L., Ramirez, A., Schwartz, K., Stevenson, G., Eds.; John Wiley & Sons: Chichester, West Sussex, UK, 2012; pp. 421–434. [Google Scholar]
- Nauwynck, H.J.; Pensaert, M.B. Abortion induced by cell-associated pseudorabies virus in vaccinated sows. Am. J. Vet. Res. 1992, 53, 489–493. [Google Scholar] [PubMed]
- Wittmann, G. Aujeszky’s disease. Rev. Sci. Tech. Off. Int. Epiz. 1986, 5, 959–977. [Google Scholar] [CrossRef] [PubMed]
- Muller, T.; Bätza, H.-J.; Schlüter, H.; Conraths, F.J.; Mettenleiter, T.C. Eradication of Aujeszky’s Disease in Germany. J. Vet. Med. Ser. B 2003, 50, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Freuling, C.; Müller, T.; Mettenleiter, T. Vaccines against pseudorabies virus (PrV). Vet. Microbiol. 2017, 206, 3–9. [Google Scholar] [CrossRef]
- Müller, T.; Hahn, E.C.; Tottewitz, F.; Kramer, M.; Klupp, B.G.; Mettenleiter, T.C.; Freuling, C. Pseudorabies virus in wild swine: A global perspective. Arch. Virol. 2011, 156, 1691–1705. [Google Scholar] [CrossRef] [PubMed]
- Wu, R.; Bai, C.; Sun, J.; Chang, S.; Zhang, X. Emergence of virulent pseudorabies virus infection in Northern China. J. Vet. Sci. 2013, 14, 363–365. [Google Scholar] [CrossRef]
- McFerran, J.B.; McCracken, R.M.; Dow, C. Comparative studies with inactivated and attenuated vaccines for protection of fattening pigs. In Proceedings of the Seminar in the Animal Pathology Series of the CEC Programme of Coordination of Agricultural Research, Tübingen, Germany, 9–10 June 1981; pp. 163–170. [Google Scholar]
- Van Rooij, E.; De Bruin, M.; De Visser, Y.E.; Boersma, W.; Bianchi, A.T. Analysis of protective immunity against PRV infection in pigs using attenuated and inactivated PRV vaccines. Vet. Res. 2000, 31, 135. [Google Scholar] [CrossRef]
- Bartha, A. Experiments to reduce the virulence of Aujeszky’s virus. Magy. Allatorv. Lapja 1961, 16, 42–45. [Google Scholar]
- Skoda, R.; Brauner, I.; Sadecky, E.; Mayer, V. Immunization against Aujeszky’s Disease with Live Vaccine. I. Attenuation of Virus and Some Properties of Attenuated Strains. Acta Virol. 1964, 8, 1–9. [Google Scholar] [PubMed]
- Mettenleiter, T.C.; Lukàcs, N.; Rziha, H.J. Pseudorabies virus avirulent strains fail to express a major glycoprotein. J. Virol. 1985, 56, 307–311. [Google Scholar] [CrossRef] [PubMed]
- Quint, W.; Gielkens, A.; Van Van Oirschot, J.; Berns, A.; Cuypers, H.T. Construction and Characterization of Deletion Mutants of Pseudorabies Virus: A New Generation of ’Live’ Vaccines. J. Gen. Virol. 1987, 68, 523–534. [Google Scholar] [CrossRef] [PubMed]
- Moormann, R.J.M.; De Rover, T.; Briaire, J.; Peeters, B.P.H.; Gielkens, A.L.J.; Van Oirschot, J.T. Inactivation of the thymidine kinase gene of a gI deletion mutant of pseudorabies virus generates a safe but still highly immunogenic vaccine strain. J. Gen. Virol. 1990, 71, 1591–1595. [Google Scholar] [CrossRef]
- Van Oirschot, J. Diva vaccines that reduce virus transmission. J. Biotechnol. 1999, 73, 195–205. [Google Scholar] [CrossRef]
- Bartha, A.; Kojnok, J. Active immunisation against Aujeszky’s disease. In Proceedings of the 17th World Veterinary Congress, Hannover, Germany, 14–21 August 1963; Volume 1. [Google Scholar]
- Bartha, A. Immunization experiments with the attenuated, K’strain of Aujeszky virus. Magy. Allatorv. Lapja 1962, 17, 321–323. [Google Scholar]
- McFerran, J.; Dow, C. Studies on immunisation of pigs with the Bartha strain of Aujeszky’s disease virus. Res. Vet. Sci. 1975, 19, 17–22. [Google Scholar] [CrossRef]
- De Leeuw, P.W.; Van Oirschot, J.T. Vaccines against Aujeszky’s disease: Evaluation of their efficacy under standardized laboratory conditions. Vet. Q. 1985, 7, 191–197. [Google Scholar] [CrossRef]
- An, T.-Q.; Peng, J.-M.; Tian, Z.-J.; Zhao, H.-Y.; Li, N.; Liu, Y.-M.; Chen, J.-Z.; Leng, C.-L.; Sun, Y.; Chang, D.; et al. Pseudorabies Virus Variant in Bartha-K61–Vaccinated Pigs, China, 2012. Emerg. Infect. Dis. 2013, 19, 1749–1755. [Google Scholar] [CrossRef]
- Luo, Y.; Li, N.; Cong, X.; Wang, C.-H.; Du, M.; Li, L.; Zhao, B.; Yuan, J.; Liu, D.-D.; Li, S.; et al. Pathogenicity and genomic characterization of a pseudorabies virus variant isolated from Bartha-K61-vaccinated swine population in China. Vet. Microbiol. 2014, 174, 107–115. [Google Scholar] [CrossRef]
- Sun, Y.; Luo, Y.; Wang, C.-H.; Yuan, J.; Li, N.; Song, K.; Qiu, H.-J. Control of swine pseudorabies in China: Opportunities and limitations. Vet. Microbiol. 2016, 183, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.-Q.; Tong, W.; Zheng, H.; Li, L.-W.; Li, G.-X.; Gao, F.; Wang, T.; Liang, C.; Ye, C.; Wu, J.-Q.; et al. Variations in glycoprotein B contribute to immunogenic difference between PRV variant JS-2012 and Bartha-K61. Vet. Microbiol. 2017, 208, 97–105. [Google Scholar] [CrossRef]
- Zhou, J.; Li, S.; Wang, X.; Zou, M.; Gao, S. Bartha-k61 vaccine protects growing pigs against challenge with an emerging variant pseudorabies virus. Vaccine 2017, 35, 1161–1166. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Liu, Y.; Chen, S.; Qiao, Y.; Guo, M.; Zheng, Y.; Xu, M.; Wang, Z.; Hou, J.; Wang, J. A gD&gC-substituted pseudorabies virus vaccine strain provides complete clinical protection and is helpful to prevent virus shedding against challenge by a Chinese pseudorabies variant. BMC Vet. Res. 2019, 15, 1–9. [Google Scholar]
- Zeng, R.; Wang, J.; Torrents, D.; Martinez, C.; Pedrazuela, R.; Galé, I. PRV vaccine AUSKIPRA GN (A3 solvent; Bartha k61 strain) provide quick and strong protection against Chinese PRV variant. In Proceedings of the 7th Asian Pig Veterinary Society Congress, Manila, Philippines, 25–27 October 2015. [Google Scholar]
- Ren, J.; Wang, H.; Zhou, L.; Ge, X.; Guo, X.; Han, J.; Yang, H. Glycoproteins C and D of PRV Strain HB1201 Contribute Individually to the Escape From Bartha-K61 Vaccine-Induced Immunity. Front. Microbiol. 2020, 11, 1–13. [Google Scholar] [CrossRef]
- Lomniczi, B.; Blankenship, M.L.; Ben-Porat, T. Deletions in the genomes of pseudorabies virus vaccine strains and existence of four isomers of the genomes. J. Virol. 1984, 49, 970–979. [Google Scholar] [CrossRef] [PubMed]
- Petrovskis, E.A.; Timmins, J.G.; Gierman, T.M.; Post, L.E. Deletions in vaccine strains of pseudorabies virus and their effect on synthesis of glycoprotein gp63. J. Virol. 1986, 60, 1166–1169. [Google Scholar] [CrossRef] [PubMed]
- Mettenleiter, T.C.; Lomniczi, B.; Sugg, N.; Schreurs, C.; Ben-Porat, T. Host cell-specific growth advantage of pseudorabies virus with a deletion in the genome sequences encoding a structural glycoprotein. J. Virol. 1988, 62, 12–19. [Google Scholar] [CrossRef]
- Zuckermann, F.A.; Mettenleiter, T.C.; Schreurs, C.; Sugg, N.; Ben-Porat, T. Complex between glycoproteins gI and gp63 of pseudorabies virus: Its effect on virus replication. J. Virol. 1988, 62, 4622–4626. [Google Scholar] [CrossRef]
- Mettenleiter, T.C.; Zsak, L.; Kaplan, A.S.; Ben-Porat, T.; Lomniczi, B. Role of a structural glycoprotein of pseudorabies in virus virulence. J. Virol. 1987, 61, 4030–4032. [Google Scholar] [CrossRef]
- Husak, P.J.; Kuo, T.; Enquist, L.W. Pseudorabies Virus Membrane Proteins gI and gE Facilitate Anterograde Spread of Infection in Projection- Specific Neurons in the Rat. J. Virol. 2000, 74, 10975–10983. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tomishima, M.; Enquist, L. A conserved α-herpesvirus protein necessary for axonal localization of viral membrane proteins. J. Cell Biol. 2001, 154, 741–752. [Google Scholar] [CrossRef] [PubMed]
- Pickard, G.E.; Smeraski, C.A.; Tomlinson, C.C.; Banfield, B.W.; Kaufman, J.; Wilcox, C.L.; Enquist, L.W.; Sollars, P.J. Intravitreal Injection of the Attenuated Pseudorabies Virus PRV Bartha Results in Infection of the Hamster Suprachiasmatic Nucleus Only by Retrograde Transsynaptic Transport via Autonomic Circuits. J. Neurosci. 2002, 22, 2701–2710. [Google Scholar] [CrossRef] [PubMed]
- Card, J.; Whealy, M.; Robbins, A.; Moore, R.; Enquist, L. Two α-herpesvirus strains are transported differentially in the rodent visual system. Neuron 1991, 6, 957–969. [Google Scholar] [CrossRef]
- Ben-Porat, T.; Demarchi, J.; Pendrys, J.; Veach, R.A.; Kaplan, A.S. Proteins specified by the short unique region of the genome of pseudorabies virus play a role in the release of virions from certain cells. J. Virol. 1986, 57, 191–196. [Google Scholar] [CrossRef]
- Mettenleiter, T.C.; Schreurs, C.; Zuckermann, F.; Ben-Porat, T. Role of pseudorabies virus glycoprotein gI in virus release from infected cells. J. Virol. 1987, 61, 2764–2769. [Google Scholar] [CrossRef]
- Johnson, D.C.; Webb, M.; Wisner, T.W.; Brunetti, C. Herpes Simplex Virus gE/gI Sorts Nascent Virions to Epithelial Cell Junctions, Promoting Virus Spread. J. Virol. 2001, 75, 821–833. [Google Scholar] [CrossRef]
- Kratchmarov, R.; Kramer, T.; Greco, T.M.; Taylor, M.P.; Ch’Ng, T.H.; Cristea, I.M.; Enquist, L.W. Glycoproteins gE and gI Are Required for Efficient KIF1A-Dependent Anterograde Axonal Transport of Alphaherpesvirus Particles in Neurons. J. Virol. 2013, 87, 9431–9440. [Google Scholar] [CrossRef]
- Kang, M.-H.; Banfield, B.W. Pseudorabies Virus Tegument Protein Us2 Recruits the Mitogen-Activated Protein Kinase Extracellular-Regulated Kinase (ERK) to Membranes through Interaction with the ERK Common Docking Domain. J. Virol. 2010, 84, 8398–8408. [Google Scholar] [CrossRef]
- Lyu, C.; Wang, S.; Sun, M.; Tang, Y.; Peng, J.; Tian, Z.; Cai, X. Deletion of pseudorabies virus US2 gene enhances viral titers in a porcine cerebral cortex primary culture system. Virus Genes 2018, 54, 406–413. [Google Scholar] [CrossRef]
- Lomniczi, B.; Watanabe, S.; Ben-Porat, T.; Kaplan, A.S. Genetic basis of the neurovirulence of pseudorabies virus. J. Virol. 1984, 52, 198–205. [Google Scholar] [CrossRef]
- Klupp, B.G.; Lomniczi, B.; Visser, N.; Fuchs, W.; Mettenleiter, T.C. Mutations affecting the UL21 gene contribute to avirulence of pseudorabies virus vaccine strain Bartha. Virology 1995, 212, 466–473. [Google Scholar] [CrossRef][Green Version]
- Lomniczi, B.; Watanabe, S.; Ben-Porat, T.; Kaplan, A.S. Genome location and identification of functions defective in the Bartha vaccine strain of pseudorabies virus. J. Virol. 1987, 61, 796–801. [Google Scholar] [CrossRef] [PubMed]
- Curanovicć, D.; Lyman, M.G.; Bou-Abboud, C.; Card, J.P.; Enquist, L.W. Repair of the UL21 Locus in Pseudorabies Virus Bartha Enhances the Kinetics of Retrograde, Transneuronal Infection In Vitro and In Vivo. J. Virol. 2009, 83, 1173–1183. [Google Scholar] [CrossRef]
- Lyman, M.G.; Demmin, G.L.; Banfield, B.W. The Attenuated Pseudorabies Virus Strain Bartha Fails To Package the Tegument Proteins Us3 and VP22. J. Virol. 2003, 77, 1403–1414. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Michael, K.; Klupp, B.G.; Karger, A.; Mettenleiter, T.C. Efficient Incorporation of Tegument Proteins pUL46, pUL49, and pUS3 into Pseudorabies Virus Particles Depends on the Presence of pUL21. J. Virol. 2007, 81, 1048–1051. [Google Scholar] [CrossRef]
- Yan, K.; Liu, J.; Guan, X.; Yin, Y.-X.; Peng, H.; Chen, H.-C.; Liu, Z.-F. The Carboxyl Terminus of Tegument Protein pUL21 Contributes to Pseudorabies Virus Neuroinvasion. J. Virol. 2019, 93, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Mettenleiter, T.C.; Schreurs, C.; Zuckermann, F.; Ben-Porat, T.; Kaplan, A.S. Role of Glycoprotein glll of Pseudorabies Virus in Virulence. J. Virol. 1988, 62, 2712–2717. [Google Scholar] [CrossRef]
- Schreurs, C.; Mettenleiter, T.C.; Zuckermann, F.; Sugg, N.; Ben-Porat, T. Glycoprotein gIII of pseudorabies virus is multifunctional. J. Virol. 1988, 62, 2251–2257. [Google Scholar] [CrossRef] [PubMed]
- Robbins, A.K.; Ryan, J.P.; Whealy, M.E.; Enquist, L.W. The Gene Encoding the glll Envelope Protein of Pseudorabies Virus Vaccine Strain Bartha Contains a Mutation Affecting Protein Localization. J. Virol. 1989, 63, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Dijkstra, J.M.; Mettenleiter, T.C.; Klupp, B.G. Intracellular Processing of Pseudorabies Virus Glycoprotein M (gM): gM of Strain Bartha Lacks N-Glycosylation. Virology 1997, 237, 113–122. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ihara, S.; Feldman, L.; Watanabe, S.; Ben-Porat, T. Characterization of the immediate-early functions of pseudorabies virus. Virology 1983, 131, 437–454. [Google Scholar] [CrossRef]
- Szpara, M.L.; Tafuri, Y.R.; Parsons, L.R.; Shamim, S.R.; Verstrepen, K.J.; Legendre, M.; Enquist, L.W. A Wide Extent of Inter-Strain Diversity in Virulent and Vaccine Strains of Alphaherpesviruses. PLoS Pathog. 2011, 7, e1002282. [Google Scholar] [CrossRef]
- Spear, P.G. Entry of alphaherpesviruses into cells. Semin. Virol. 1993, 4, 167–180. [Google Scholar] [CrossRef]
- Backovic, M.; DuBois, R.M.; Cockburn, J.J.; Sharff, A.J.; Vaney, M.-C.; Granzow, H.; Klupp, B.G.; Bricogne, G.; Mettenleiter, T.C.; Rey, F.A. Structure of a core fragment of glycoprotein H from pseudorabies virus in complex with antibody. Proc. Natl. Acad. Sci. USA 2010, 107, 22635–22640. [Google Scholar] [CrossRef]
- Schröter, C.; Klupp, B.G.; Fuchs, W.; Gerhard, M.; Backovic, M.; Rey, F.A.; Mettenleiter, T.C. The Highly Conserved Proline at Position 438 in Pseudorabies Virus gH Is Important for Regulation of Membrane Fusion. J. Virol. 2014, 88, 13064–13072. [Google Scholar] [CrossRef]
- Okazaki, K. Proteolytic cleavage of glycoprotein B is dispensable for in vitro replication, but required for syncytium formation of pseudorabies virus. J. Gen. Virol. 2007, 88, 1859–1865. [Google Scholar] [CrossRef]
- Oliver, S.L.; Sommer, M.; Zerboni, L.; Rajamani, J.; Grose, C.; Arvin, A.M. Mutagenesis of Varicella-Zoster Virus Glycoprotein B: Putative Fusion Loop Residues Are Essential for Viral Replication, and the Furin Cleavage Motif Contributes to Pathogenesis in Skin Tissue In Vivo. J. Virol. 2009, 83, 7495–7506. [Google Scholar] [CrossRef]
- De Pelsmaeker, S.; Dierick, E.; Klupp, B.; Mettenleiter, T.C.; Cantoni, C.; Vitale, M.; Favoreel, H.W. Expression of the Pseudorabies Virus gB Glycoprotein Triggers NK Cell Cytotoxicity and Increases Binding of the Activating NK Cell Receptor PILRβ. J. Virol. 2019, 93. [Google Scholar] [CrossRef]
- Card, J.P.; Enquist, L.W. Transneuronal Circuit Analysis with Pseudorabies Viruses. Curr. Protoc. Neurosci. 2014, 68, 1.5.1–1.5.39. [Google Scholar] [CrossRef]
- Yang, M.; Card, J.P.; Tirabassi, R.S.; Miselis, R.R.; Enquist, L.W. Retrograde, Transneuronal Spread of Pseudorabies Virus in Defined Neuronal Circuitry of the Rat Brain Is Facilitated by gE Mutations That Reduce Virulence. J. Virol. 1999, 73, 4350–4359. [Google Scholar] [CrossRef]
- O’Donnell, P.; Lavín, A.; Enquist, L.W.; Grace, A.A.; Card, J.P. Interconnected Parallel Circuits between Rat Nucleus Accumbens and Thalamus Revealed by Retrograde Transynaptic Transport of Pseudorabies Virus. J. Neurosci. 1997, 17, 2143–2167. [Google Scholar] [CrossRef] [PubMed]
- Aston-Jones, G.; Chen, S.; Zhu, Y.; Oshinsky, M.L. A neural circuit for circadian regulation of arousal. Nat. Neurosci. 2001, 4, 732–738. [Google Scholar] [CrossRef] [PubMed]
- Dong, B.; Zarlenga, D.S.; Ren, X. An Overview of Live Attenuated Recombinant Pseudorabies Viruses for Use as Novel Vaccines. J. Immunol. Res. 2014, 2014, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Qiu, H.-J.; Tian, Z.-J.; Tong, G.; Zhou, Y.-J.; Ni, J.-Q.; Luo, Y.-Z.; Cai, X.-H. Protective immunity induced by a recombinant pseudorabies virus expressing the GP5 of porcine reproductive and respiratory syndrome virus in piglets. Vet. Immunol. Immunopathol. 2005, 106, 309–319. [Google Scholar] [CrossRef] [PubMed]
- Tian, Z.-J.; Zhou, G.-H.; Zheng, B.-L.; Qiu, H.-J.; Ni, J.-Q.; Yang, H.-L.; Yin, X.-N.; Hu, S.-P.; Tong, G.-Z. A recombinant pseudorabies virus encoding the HA gene from H3N2 subtype swine influenza virus protects mice from virulent challenge. Vet. Immunol. Immunopathol. 2006, 111, 211–218. [Google Scholar] [CrossRef]
- Klingbeil, K.; Lange, E.; Blohm, U.; Teifke, J.P.; Mettenleiter, T.C.; Fuchs, W. Protection of pigs against pandemic swine origin H1N1 influenza A virus infection by hemagglutinin- or neuraminidase-expressing attenuated pseudorabies virus recombinants. Virus Res. 2015, 199, 20–30. [Google Scholar] [CrossRef]
- Pol, J.M.; Gielkens, A.L.; Van Oirschot, J.T. Comparative pathogenesis of three strains of pseudorabies virus in pigs. Microb. Pathog. 1989, 7, 361–371. [Google Scholar] [CrossRef]
- Lamote, J.A.S.; Kestens, M.; Van Waesberghe, C.; Delva, J.; De Pelsmaeker, S.; Devriendt, B.; Favoreel, H.W. The Pseudorabies Virus Glycoprotein gE/gI Complex Suppresses Type I Interferon Production by Plasmacytoid Dendritic Cells. J. Virol. 2017, 91, 1–12. [Google Scholar] [CrossRef]
- Kimman, T.; Brouwers, R.; Daus, F.; Van Oirschot, J.; Van Zaane, D. Measurement of isotype-specific antibody responses to Aujeszky’s disease virus in sera and mucosal secretions of pigs. Vet. Immunol. Immunopathol. 1992, 31, 95–113. [Google Scholar] [CrossRef]
- Van Rooij, E.; De Bruin, M.; De Visser, Y.; Middel, W.; Boersma, W.; Bianchi, A. Vaccine-induced T cell-mediated immunity plays a critical role in early protection against pseudorabies virus (suid herpes virus type 1) infection in pigs. Vet. Immunol. Immunopathol. 2004, 99, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Nauwynck, H.J.; Zonnekeyn, V.; Pensaert, M.B. Virological Protection of Sows upon Challenge with Aujeszky’s Disease Virus After Multiple Vaccinations with Attenuated or Inactivated Vaccines. J. Vet. Med. Ser. B 1997, 44, 609–615. [Google Scholar] [CrossRef]
- Sparks-Thissen, R.L.; Enquist, L.W. Differential Regulation of Dk and Kk Major Histocompatibility Complex Class I Proteins on the Cell Surface after Infection of Murine Cells by Pseudorabies Virus. J. Virol. 1999, 73, 5748–5756. [Google Scholar] [CrossRef] [PubMed]
- Denés, A.; Boldogkői, Z.; Hornyák, Á.; Palkovits, M.; Kovács, K.J. Attenuated pseudorabies virus-evoked rapid innate immune response in the rat brain. J. Neuroimmunol. 2006, 180, 88–103. [Google Scholar] [CrossRef] [PubMed]
- Hu, S.; Liu, Q.; Zang, S.; Zhang, Z.; Wang, J.; Cai, X.; He, X. Microglia Are Derived from Peripheral Blood Mononuclear Cells After Pseudorabies Infection in Mice. Viral Immunol. 2018, 31, 596–604. [Google Scholar] [CrossRef]
- Paulus, C.; Sollars, P.J.; Pickard, G.E.; Enquist, L.W. Transcriptome Signature of Virulent and Attenuated Pseudorabies Virus-Infected Rodent Brain. J. Virol. 2006, 80, 1773–1786. [Google Scholar] [CrossRef]
- Brukman, A.; Enquist, L.W. Suppression of the Interferon-Mediated Innate Immune Response by Pseudorabies Virus. J. Virol. 2006, 80, 6345–6356. [Google Scholar] [CrossRef]
- Zeng, H.-L.; Yu, F.-L.; Zhang, Z.; Yang, Q.; Jin, S.; He, X.; Chen, X.; Shen, Y.; Cheng, L.; Guo, L.; et al. Quantitative proteomics study of host response to virulent and attenuated pseudorabies virus infection in mouse brain. Biochim. Biophys. Acta (BBA) Proteins Proteom. 2018, 1866, 307–315. [Google Scholar] [CrossRef]
- Laval, K.; Vernejoul, J.B.; Van Cleemput, J.; Koyuncu, O.O.; Enquist, L.W. Virulent Pseudorabies Virus Infection Induces a Specific and Lethal Systemic Inflammatory Response in Mice. J. Virol. 2018, 92, 1–15. [Google Scholar] [CrossRef]
- Laval, K.; Van Cleemput, J.; Vernejoul, J.B.; Enquist, L.W. Alphaherpesvirus infection of mice primes PNS neurons to an inflammatory state regulated by TLR2 and type I IFN signaling. PLoS Pathog. 2019, 15, 1–21. [Google Scholar] [CrossRef]
- Laval, K.; Enquist, L.W. The Neuropathic Itch Caused by Pseudorabies Virus. Pathogens 2020, 9, 254. [Google Scholar] [CrossRef] [PubMed]
- De Bruin, T.G.M.; van Rooij, E.M.A.; de Visser, Y.E.; Voermans, J.J.M.; Samsom, J.N.; Kimman, T.G.; Bianchi, A.T.J. Discrimination of different subsets of cytolytic cells in pseudorabies virus-immune and naive pigs. J. Gen. Virol. 2000, 81, 1529–1537. [Google Scholar] [CrossRef] [PubMed]
- De Pelsmaeker, S.; Devriendt, B.; De Regge, N.; Favoreel, H.W. Porcine NK Cells Stimulate Proliferation of Pseudorabies Virus-Experienced CD8+ and CD4+CD8+ T Cells. Front. Immunol. 2019, 9. [Google Scholar] [CrossRef] [PubMed]
- Querec, T.; Bennouna, S.; Alkan, S.; Laouar, Y.; Gorden, K.; Flavell, R.; Akira, S.; Ahmed, R.; Pulendran, B. Yellow fever vaccine YF-17D activates multiple dendritic cell subsets via TLR2, 7, 8, and 9 to stimulate polyvalent immunity. J. Exp. Med. 2006, 203, 413–424. [Google Scholar] [CrossRef]
- Pulendran, B. Learning immunology from the yellow fever vaccine: Innate immunity to systems vaccinology. Nat. Rev. Immunol. 2009, 9, 741–747. [Google Scholar] [CrossRef]
- Johnston, C.; Gottlieb, S.L.; Wald, A. Status of vaccine research and development of vaccines for herpes simplex virus. Vaccine 2016, 34, 2948–2952. [Google Scholar] [CrossRef]
- Aschner, C.B.; Herold, B.C. Alphaherpesvirus Vaccines. In Alphaherpesviruses: Molecular Biology, Host Interactions and Control; Caister Academic Press: Norfolk, UK, 2020. [Google Scholar]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delva, J.L.; Nauwynck, H.J.; Mettenleiter, T.C.; Favoreel, H.W. The Attenuated Pseudorabies Virus Vaccine Strain Bartha K61: A Brief Review on the Knowledge Gathered during 60 Years of Research. Pathogens 2020, 9, 897. https://doi.org/10.3390/pathogens9110897
Delva JL, Nauwynck HJ, Mettenleiter TC, Favoreel HW. The Attenuated Pseudorabies Virus Vaccine Strain Bartha K61: A Brief Review on the Knowledge Gathered during 60 Years of Research. Pathogens. 2020; 9(11):897. https://doi.org/10.3390/pathogens9110897
Chicago/Turabian StyleDelva, Jonas L., Hans J. Nauwynck, Thomas C. Mettenleiter, and Herman W. Favoreel. 2020. "The Attenuated Pseudorabies Virus Vaccine Strain Bartha K61: A Brief Review on the Knowledge Gathered during 60 Years of Research" Pathogens 9, no. 11: 897. https://doi.org/10.3390/pathogens9110897
APA StyleDelva, J. L., Nauwynck, H. J., Mettenleiter, T. C., & Favoreel, H. W. (2020). The Attenuated Pseudorabies Virus Vaccine Strain Bartha K61: A Brief Review on the Knowledge Gathered during 60 Years of Research. Pathogens, 9(11), 897. https://doi.org/10.3390/pathogens9110897




