Detection of Second Line Drug Resistance among Drug Resistant Mycobacterium Tuberculosis Isolates in Botswana
Abstract
1. Background
2. Methods
2.1. Design and Study Population
2.2. Treatment Outcome Definitions
2.3. DNA Extraction
2.4. Genotyping
2.4.1. Spoligotyping
2.4.2. Hain Genotype MTBDRsl Version 2
2.4.3. Data Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- WHO. Global Tuberculosis Report. Available online: https://www.who.int/tb/publications/global_report/en/ (accessed on 20 July 2019).
- Oudghiri, A.; Karimi, H.; Chetioui, F.; Zakham, F.; Bourkadi, J.E.; Elmessaoudi, M.D.; Laglaoui, A.; Chaoui, I.; El Mzibri, M. Molecular characterization of mutations associated with resistance to second-line tuberculosis drug among multidrug-resistant tuberculosis patients from high prevalence tuberculosis city in Morocco. BMC Infect. Dis. 2018, 18, 98. [Google Scholar] [CrossRef] [PubMed]
- Villegas, L.; Otero, L.; Sterling, T.R.; Huaman, M.A.; Van der Stuyft, P.; Gotuzzo, E.; Seas, C. Prevalence, risk factors, and treatment outcomes of isoniazid-and rifampicin-mono-resistant pulmonary tuberculosis in lima, peru. PLoS ONE 2016, 11, e0152933. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, M. Isoniazid monoresistance: A precursor to multidrug-resistant tuberculosis? Ann. Am. Thorac. Soc. 2018, 15, 306–307. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.B.; Nguyen, N.V.; Tran, H.T.; Nguyen, H.V.; Bui, Q.T. Prevalence of resistance to second-line tuberculosis drug among multidrug-resistant tuberculosis patients in Viet Nam, 2011. Western Pac. Surveill. Response J. 2016, 7, 35–40. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hu, Y.; Hoffner, S.; Wu, L.; Zhao, Q.; Jiang, W.; Xu, B. Prevalence and genetic characterization of second-line drug-resistant and extensively drug-resistant Mycobacterium tuberculosis in Rural China. Antimicrob. Agents Chemother. 2013, 57, 3857–3863. [Google Scholar] [CrossRef]
- Gardee, Y.; Dreyer, A.W.; Koornhof, H.J.; Omar, S.V.; da Silva, P.; Bhyat, Z.; Ismail, N.A. Evaluation of the GenoType MTBDRsl version 2.0 assay for second-line drug resistance detection of mycobacterium tuberculosis isolates in South Africa. J. Clin. Microbiol. 2017, 55, 791–800. [Google Scholar] [CrossRef]
- Farhat, M.R.; Jacobson, K.R.; Franke, M.F.; Kaur, D.; Sloutsky, A.; Mitnick, C.D.; Murray, M. Gyrase mutations are associated with variable levels of fluoroquinolone resistance in mycobacterium tuberculosis. J. Clin. Microbiol. 2016, 54, 727–733. [Google Scholar] [CrossRef]
- Hooper, D.C.; Jacoby, G.A. Mechanisms of drug resistance: Quinolone resistance. Ann. N.Y. Acad. Sci. 2015, 1354, 12–31. [Google Scholar] [CrossRef]
- Jabeen, K.; Shakoor, S.; Malik, F.; Hasan, R. Fluoroquinolone resistance in Mycobacterium tuberculosis isolates from Pakistan 2010–2014: Implications for disease control. Int. J. Mycobacteriol. 2015, 4, 47–48. [Google Scholar] [CrossRef]
- WHO. The Use of Molecular Line Probe Assays for the Detection of Resistance to Second-Line Anti-Tuberculosis Drugs: Policy Guidance; WHO: Geneva, Switzerland, 2016; Available online: https://www.who.int/tb/publications/lpa-mdr-diagnostics/en/ (accessed on 23 July 2019).
- HainLifescience. Instructions for Use for Hain GenoType MTBDRsl, Version 2.0; HainLifescience: Nehren, Germany; Available online: https://www.hain-lifescience.de/en/instructions-for-use.html (accessed on 20 July 2019).
- Tagliani, E.; Cabibbe, A.M.; Miotto, P.; Borroni, E.; Toro, J.C.; Mansjo, M.; Hoffner, S.; Hillemann, D.; Zalutskaya, A.; Skrahina, A.; et al. Diagnostic performance of the new version (v2.0) of genotype mtbdrsl assay for detection of resistance to fluoroquinolones and second-line injectable drugs: A multicenter study. J. Clin. Microbiol. 2015, 53, 2961–2969. [Google Scholar] [CrossRef]
- Ismail, N.; Ismail, F.; Omar, S.V.; Blows, L.; Gardee, Y.; Koornhof, H.; Onyebujoh, P.C. Drug resistant tuberculosis in Africa: Current status, gaps and opportunities. Afr. J. Lab. Med. 2018, 7, 781. [Google Scholar] [CrossRef] [PubMed]
- Nanzaluka, F.H.; Chibuye, S.; Kasapo, C.C.; Langa, N.; Nyimbili, S.; Moonga, G.; Kapata, N.; Kumar, R.; Chongwe, G. Factors associated with unfavourable tuberculosis treatment outcomes in Lusaka, Zambia, 2015: A secondary analysis of routine surveillance data. Pan. Afr. Med. J. 2019, 32, 159. [Google Scholar] [CrossRef]
- Tanue, E.A.; Nsagha, D.S.; Njamen, T.N.; Assob, N.J.C. Tuberculosis treatment outcome and its associated factors among people living with HIV and AIDS in Fako Division of Cameroon. PLoS ONE 2019, 14, e0218800. [Google Scholar] [CrossRef] [PubMed]
- Mogashoa, T.; Melamu, P.; Ley, S.D.; Streicher, E.M.; Iketleng, T.; Kelentse, N.; Mupfumi, L.; Mokomane, M.; Kgwaadira, B.; Novitsky, V.; et al. Genetic diversity of Mycobacterium tuberculosis strains circulating in Botswana. PLoS ONE 2019, 14, e0216306. [Google Scholar] [CrossRef]
- National Tuberculosis Programme Manual 2011. Available online: https://www.who.int/hiv/pub/guidelines/botswana_tb.pdf (accessed on 5 January 2019).
- HainLifescience. Instructions for Use for Hain GenoLyse Kit for Isolation of Genomic Bacterial DNA; HainLifescience: Nehren, Germany; Available online: https://www.hain-lifescience.de/en/instructions-for-use.html (accessed on 20 July 2019).
- Kamerbeek, J.; Schouls, L.; Fau-Kolk, A.; Kolk, A.; Fau-van Agterveld, M.; van Agterveld, M.; Fau-van Soolingen, D.; van Soolingen, D.; Fau-Kuijper, S.; Kuijper, S.; et al. Simultaneous detection and strain differentiation of Mycobacterium tuberculosis for diagnosis and epidemiology. J. Clin. Microbiol. 1997, 35, 907–914. [Google Scholar] [PubMed]
- Cox, H.; Kebede, Y.; Allamuratova, S.; Ismailov, G.; Davletmuratova, Z.; Byrnes, G.; Stone, C.; Niemann, S.; Rusch-Gerdes, S.; Blok, L.; et al. Tuberculosis recurrence and mortality after successful treatment: Impact of drug resistance. PLoS Med. 2006, 3, e384. [Google Scholar] [CrossRef]
- Munang, M.L.; Kariuki, M.; Dedicoat, M. Isoniazid-resistant tuberculosis in Birmingham, United Kingdom, 1999–2010. QJM 2015, 108, 19–25. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kendall, E.A.; Malhotra, S.; Cook-Scalise, S.; Denkinger, C.M.; Dowdy, D.W. Estimating the impact of a novel drug regimen for treatment of tuberculosis: A modeling analysis of projected patient outcomes and epidemiological considerations. BMC Infect. Dis. 2019, 19, 794. [Google Scholar] [CrossRef]
- Saravu, K.; Pai, M. Drug-resistant tuberculosis: Progress towards shorter and safer regimens. Lung India 2019, 36, 373–375. [Google Scholar] [CrossRef]
- GLI. Line Probe Assays for Drug Resistant Tuberculosis Detection. Interpretation and Reporting Guide for Laboratory Staff and Clinicians. Available online: http://www.stoptb.org/wg/gli/assets/documents/LPA_test_web_ready.pdf (accessed on 20 July 2019).
- Maitre, T.; Petitjean, G.; Chauffour, A.; Bernard, C.; El Helali, N.; Jarlier, V.; Reibel, F.; Chavanet, P.; Aubry, A.; Veziris, N. Are moxifloxacin and levofloxacin equally effective to treat XDR tuberculosis? J. Antimicrob. Chemother. 2017, 72, 2326–2333. [Google Scholar] [CrossRef]
- Chien, J.Y.; Chen, Y.T.; Wu, S.G.; Lee, J.J.; Wang, J.Y.; Yu, C.J. Treatment outcome of patients with isoniazid mono-resistant tuberculosis. Clin. Microbiol. Infect. 2015, 21, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Yimer, S.A.; Agonafir, M.; Derese, Y.; Sani, Y.; Bjune, G.A.; Holm-Hansen, C. Primary drug resistance to anti-tuberculosis drugs in major towns of Amhara region, Ethiopia. APMIS 2012, 120, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Asmamaw, D.; Seyoum, B.; Makonnen, E.; Atsebeha, H.; Woldemeskel, D.; Yamuah, L.; Addus, H.; Aseffa, A. Primary drug resistance in newly diagnosed smear positive tuberculosis patients in Addis Ababa, Ethiopia. Ethiop. Med. J. 2008, 46, 367–374. [Google Scholar] [PubMed]
- Vidyaraj, C.K.; Chitra, A.; Smita, S.; Muthuraj, M.; Govindarajan, S.; Usharani, B.; Anbazhagi, S. Prevalence of rifampicin-resistant Mycobacterium tuberculosis among human-immunodeficiency-virus-seropositive patients and their treatment outcomes. J. Epidemiol. Glob. Health 2017, 7, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Haar, C.H.; Cobelens, F.G.; Kalisvaart, N.A.; van der Have, J.J.; van Gerven, P.J.; van Soolingen, D. Tuberculosis drug resistance and HIV infection, the Netherlands. Emerg. Infect. Dis. 2007, 13, 776–778. [Google Scholar] [CrossRef]
- Fenner, L.; Atkinson, A.; Boulle, A.; Fox, M.P.; Prozesky, H.; Zurcher, K.; Ballif, M.; Furrer, H.; Zwahlen, M.; Davies, M.A.; et al. HIV viral load as an independent risk factor for tuberculosis in South Africa: Collaborative analysis of cohort studies. J. Int. AIDS Soc. 2017, 20, 21327. [Google Scholar] [CrossRef]
- Ajileye, A.; Alvarez, N.; Merker, M.; Walker, T.M.; Akter, S.; Brown, K.; Moradigaravand, D.; Schon, T.; Andres, S.; Schleusener, V.; et al. Some synonymous and nonsynonymous gyra mutations in mycobacterium tuberculosis lead to systematic false-positive fluoroquinolone resistance results with the hain genotype mtbdrsl assays. Antimicrob. Agents Chemother. 2017, 61. [Google Scholar] [CrossRef]
- Disratthakit, A.; Prammananan, T.; Tribuddharat, C.; Thaipisuttikul, I.; Doi, N.; Leechawengwongs, M.; Chaiprasert, A. Role of gyrB mutations in pre-extensively and extensively drug-resistant tuberculosis in thai clinical isolates. Antimicrob. Agents Chemother. 2016, 60, 5189–5197. [Google Scholar] [CrossRef]
| n | % | |
|---|---|---|
| Sex | ||
| Male | 29 | 50.9 |
| Female | 28 | 49.1 |
| Age in years | ||
| <20 years | 9 | 16.1 |
| 20–39 years | 28 | 50.0 |
| 40–59 years | 16 | 28.6 |
| >60 years | 3 | 5.4 |
| HIV status | ||
| Negative | 15 | 26.3 |
| Positive | 31 | 54.4 |
| Unknown | 11 | 19.3 |
| Specimen type | ||
| Extra-pulmonary | 1 | 1.8 |
| Pulmonary | 55 | 96.5 |
| Unknown | 1 | 1.8 |
| Smear results | ||
| Negative | 12 | 21.1 |
| Positive | 45 | 79 |
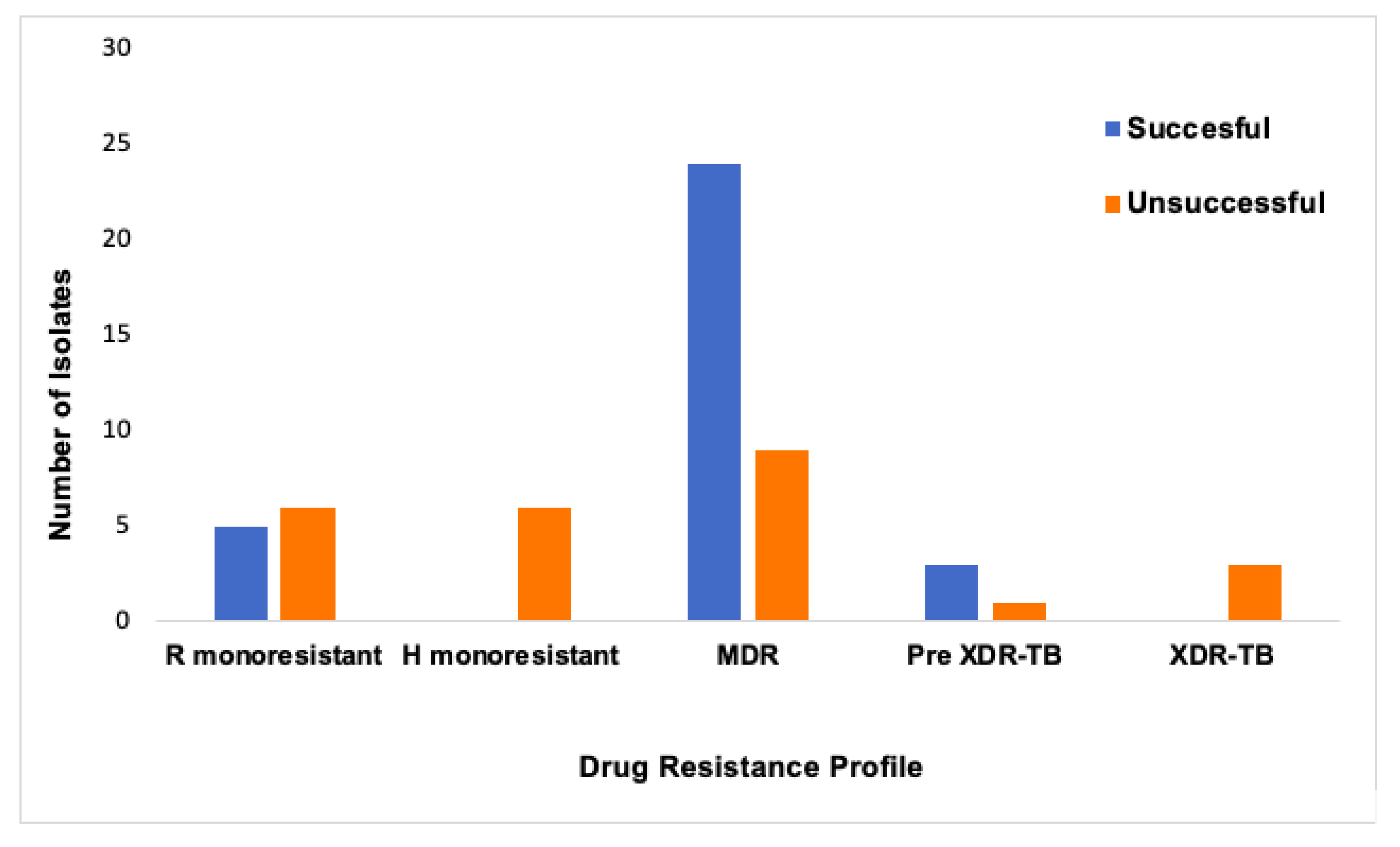
| Drug resistance profile | ||
| Rifampicin monoresistant | 11 | 19.3 |
| Isoniazid monoresistant | 6 | 10.5 |
| Multi-drug resistant (MDR) | 33 | 57.9 |
| Pre-XDR* | 4 | 7.0 |
| XDR** | 3 | 5.3 |
| Region | ||
| Central | 24 | 42.1 |
| South West | 1 | 1.8 |
| North West | 5 | 8.8 |
| Southern | 27 | 47.4 |
| Lineage | ||
| Lineage 1 | 7 | 12.3 |
| Lineage 2 | 11 | 19.3 |
| Lineage 4 | 38 | 66.7 |
| Unknown | 1 | 1.8 |
| MDR N = 50 | 2nd Line Drug Resistance* N = 7 | p-value | |
|---|---|---|---|
| Sex | n (%) | n (%) | 0.253 |
| Male | 27 (54) | 2 (29) | |
| Female | 23 (46) | 5 (71) | |
| Age in years | 0.833 | ||
| <20 years | 8 (16) | 1 (14) | |
| 20–39 years | 23 (47) | 5 (71) | |
| 40–59 years | 15 (31) | 1 (14) | |
| >60 years | 3 (6) | 0 (0) | |
| HIV status | 0.226 | ||
| Negative | 15 (30) | 0 (0) | |
| Positive | 26 (52) | 5 (71) | |
| Unknown | 9 (18) | 2 (29) | |
| Smear results | 0.630 | ||
| Negative | 10 (20) | 2 (29) | |
| Positive | 40 (80) | 5 (71) | |
| Region | 0.866 | ||
| Central | 20 (40) | 4 (57) | |
| South West | 1 (2) | 0 (0) | |
| North West | 24 (48) | 0 (0) | |
| Southern | 5 (10) | 3 (43) | |
| Lineage | 0.066 | ||
| Lineage 1 | 4 (8) | 3 (43) | |
| Lineage 2 | 11 (22) | 0 (0) | |
| Lineage 4 | 34 (68) | 4 (57) | |
| Unknown | 1 (2) | 0 (0) | |
| Case | Age | Sex | Region | HIV Status | FLDs Drug Resistance Pattern | Hybridization Pattern (s) | Codon Mutations | SLDs Drug Resistance Pattern | M.tb Lineage, Spoligo Family | Treatment Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 29 | F | Central | Positive | H; R; S; E | gyrA ΔWT3 + rrs ΔWT1 + rrs MUT1 | Undefined mutation, A1401G | OFL; LFX; KAN; AM; CAP | L4, X3 | Failed |
| 2 | 28 | F | North West | Unknown | H; R; S; E | gyrA ΔWT3 + rrs ΔWT1 + rrs MUT1 | Undefined mutation, A1401G | OFL; LFX; KAN; AM; CAP | L4, X3 | Failed |
| 3 | 32 | M | North West | Positive | H; R; E | gyrA ΔWT2 + gyrA MUT1+ rrs ΔWT1 + rrs MUT1 | A90V, A1401G | OFL; LFX; KAN; AM; CAP | L4, LAM4 | Deceased |
| 4 | 37 | F | Central | Positive | H; R; E | gyrA ΔWT3 + gyrA MUT1 | A90V | OFL; LFX | L1, EAI1_SOM | Completed |
| 5 | 44 | M | Central | Unknown | H; R; S; E | gyrA ΔWT2 + gyrA MUT1 | A90V | OFL; LFX | L1, EAI1_SOM | *Not evaluated |
| 6 | 34 | F | Central | Positive | H; R; S; E | gyrA ΔWT2 + gyrA MUT1 | A90V | OFL; LFX | L1, EAI1_SOM | Completed |
| 7 | 16 | F | South | Positive | H; R; S; E | gyrA ΔWT1 | G88A/G88C | OFL; LFX | L4, LAM3 | Cured |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mogashoa, T.; Melamu, P.; Derendinger, B.; Ley, S.D.; Streicher, E.M.; Iketleng, T.; Mupfumi, L.; Mokomane, M.; Kgwaadira, B.; Rankgoane-Pono, G.; et al. Detection of Second Line Drug Resistance among Drug Resistant Mycobacterium Tuberculosis Isolates in Botswana. Pathogens 2019, 8, 208. https://doi.org/10.3390/pathogens8040208
Mogashoa T, Melamu P, Derendinger B, Ley SD, Streicher EM, Iketleng T, Mupfumi L, Mokomane M, Kgwaadira B, Rankgoane-Pono G, et al. Detection of Second Line Drug Resistance among Drug Resistant Mycobacterium Tuberculosis Isolates in Botswana. Pathogens. 2019; 8(4):208. https://doi.org/10.3390/pathogens8040208
Chicago/Turabian StyleMogashoa, Tuelo, Pinkie Melamu, Brigitta Derendinger, Serej D. Ley, Elizabeth M. Streicher, Thato Iketleng, Lucy Mupfumi, Margaret Mokomane, Botshelo Kgwaadira, Goabaone Rankgoane-Pono, and et al. 2019. "Detection of Second Line Drug Resistance among Drug Resistant Mycobacterium Tuberculosis Isolates in Botswana" Pathogens 8, no. 4: 208. https://doi.org/10.3390/pathogens8040208
APA StyleMogashoa, T., Melamu, P., Derendinger, B., Ley, S. D., Streicher, E. M., Iketleng, T., Mupfumi, L., Mokomane, M., Kgwaadira, B., Rankgoane-Pono, G., Tsholofelo, T. T., Kasvosve, I., Moyo, S., Warren, R. M., & Gaseitsiwe, S. (2019). Detection of Second Line Drug Resistance among Drug Resistant Mycobacterium Tuberculosis Isolates in Botswana. Pathogens, 8(4), 208. https://doi.org/10.3390/pathogens8040208





