Babesia divergens: A Drive to Survive
Abstract
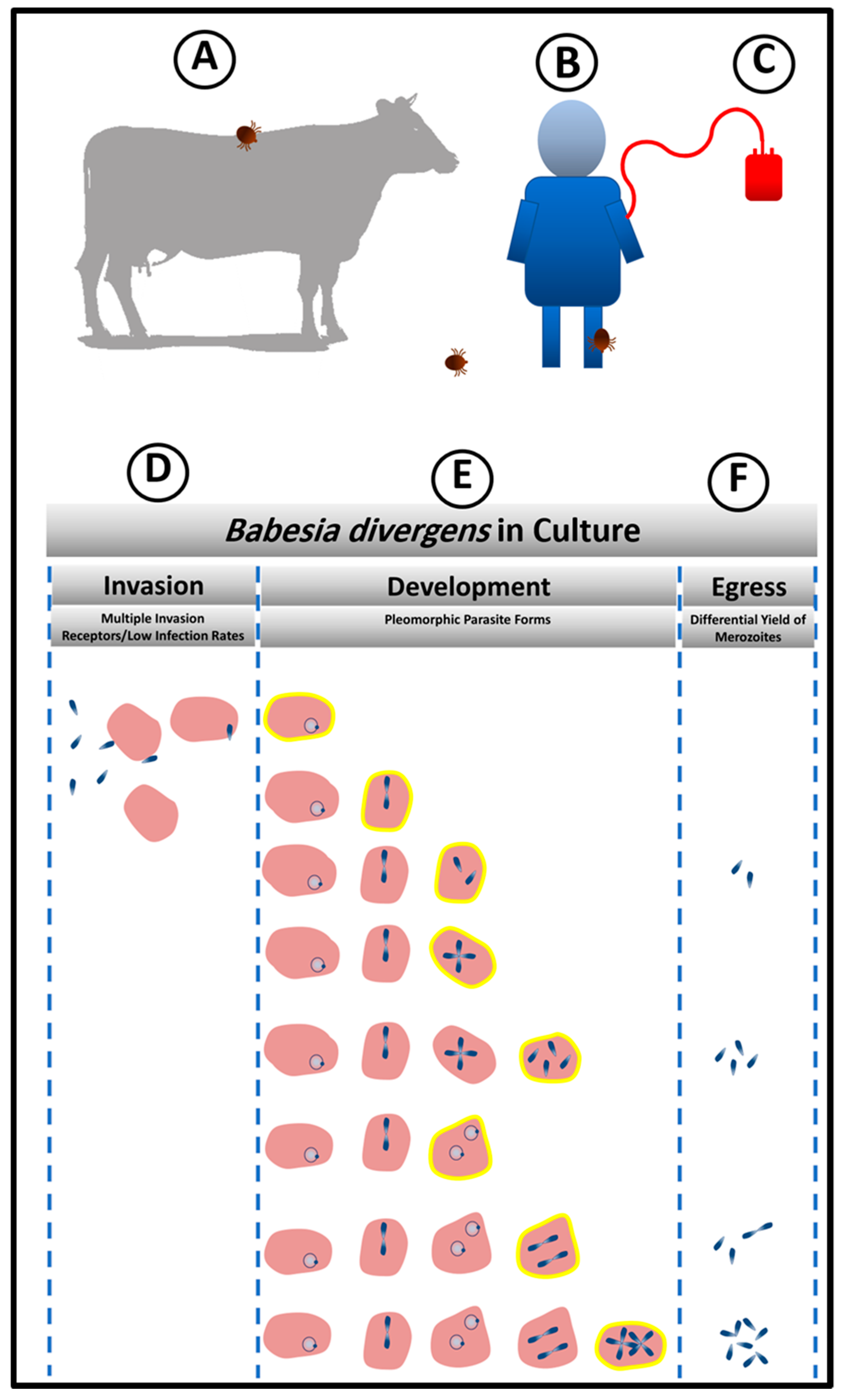
:1. Modes of Transmission
2. Babesia divergens as a Zoonotic Agent
3. Features of the Babesia divergens Lifecycle that Dictate Parasitism Success
4. Efficient Invasion Is the First Step of Establishing Successful Parasitism
5. Babesia divergens Flexible Intra-Erythrocytic Life Cycle Leads to Pleomorphic Life Forms
6. Maintenance of Babesia divergens Population Structure to Enable Quick Adaptation to Changing Environment through Egress and the Release of Different Numbers of Infective Units
7. Persistence and Implications for Pathogen Inactivation Strategies
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Krause, P.J.; Telford, S.R., 3rd; Ryan, R.; Hurta, A.B.; Kwasnik, I.; Luger, S.; Niederman, J.; Gerber, M.; Spielman, A. Geographical and temporal distribution of babesial infection in Connecticut. J. Clin. Microbiol. 1991, 29, 1–4. [Google Scholar] [PubMed]
- Lantos, P.M.; Krause, P.J. Babesiosis: Similar to malaria but different. Pediatr. Ann. 2002, 31, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Hunfeld, K.P.; Hildebrandt, A.; Gray, J.S. Babesiosis: Recent insights into an ancient disease. Int. J. Parasitol. 2008, 38, 1219–1237. [Google Scholar] [CrossRef] [PubMed]
- Gorenflot, A.; Moubri, K.; Precigout, E.; Carcy, B.; Schetters, T.P. Human babesiosis. Ann. Trop. Med. Parasitol. 1998, 92, 489–501. [Google Scholar] [CrossRef] [PubMed]
- Gray, J.; Zintl, A.; Hildebrandt, A.; Hunfeld, K.P.; Weiss, L. Zoonotic babesiosis: Overview of the disease and novel aspects of pathogen identity. Ticks Tick-Borne Dis. 2010, 1, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Hildebrandt, A.; Gray, J.S.; Hunfeld, K.P. Human babesiosis in Europe: What clinicians need to know. Infection 2013, 41, 1057–1072. [Google Scholar] [CrossRef] [PubMed]
- de la Fuente, J.; Estrada-Pena, A.; Venzal, J.M.; Kocan, K.M.; Sonenshine, D.E. Overview: Ticks as vectors of pathogens that cause disease in humans and animals. Front. Biosci. J. Virtual Libr. 2008, 13, 6938–6946. [Google Scholar] [CrossRef]
- Mehlhorn, H.; Shein, E. The piroplasms: Life cycle and sexual stages. Adv. Parasitol. 1984, 23, 37–103. [Google Scholar] [PubMed]
- Yabsley, M.J.; Shock, B.C. Natural history of Zoonotic Babesia: Role of wildlife reservoirs. Int. J. Parasitol. Parasites Wildlife 2013, 2, 18–31. [Google Scholar] [CrossRef]
- Leiby, D.A. Transfusion-associated babesiosis: shouldn’t we be ticked off? Ann. Intern. Med. 2011, 155, 556–557. [Google Scholar] [CrossRef]
- Leiby, D.A. Transfusion-transmitted Babesia spp.: Bull’s-eye on Babesia microti. Clin. Microbiol. Rev. 2011, 24, 14–28. [Google Scholar] [CrossRef] [PubMed]
- Gubernot, D.M.; Nakhasi, H.L.; Mied, P.A.; Asher, D.M.; Epstein, J.S.; Kumar, S. Transfusion-transmitted babesiosis in the United States: Summary of a workshop. Transfusion 2009, 49, 2759–2771. [Google Scholar] [CrossRef] [PubMed]
- Yager, P.H.; Luginbuhl, L.M.; Dekker, J.P. Case records of the Massachusetts General Hospital. Case 6-2014. A 35-day-old boy with fever, vomiting, mottled skin, and severe anemia. N. Engl. J. Med. 2014, 370, 753–762. [Google Scholar] [CrossRef] [PubMed]
- Aderinboye, O.; Syed, S.S. Congenital babesiosis in a four-week-old female infant. Pediatr. Infect. Dis. J. 2010, 29, 188. [Google Scholar] [CrossRef] [PubMed]
- New, D.L.; Quinn, J.B.; Qureshi, M.Z.; Sigler, S.J. Vertically transmitted babesiosis. J. Pediatr. 1997, 131, 163–164. [Google Scholar] [CrossRef]
- Sethi, S.; Alcid, D.; Kesarwala, H.; Tolan, R.W., Jr. Probable congenital babesiosis in infant, new jersey, USA. Emerg. Infect. Dis. 2009, 15, 788–791. [Google Scholar] [CrossRef] [PubMed]
- Hildebrandt, A.; Hunfeld, K.P.; Baier, M.; Krumbholz, A.; Sachse, S.; Lorenzen, T.; Kiehntopf, M.; Fricke, H.J.; Straube, E. First confirmed autochthonous case of human Babesia microti infection in Europe. Eur. J. Clin. Microbiol. Infect. Dis. 2007, 26, 595–601. [Google Scholar] [CrossRef]
- Skrabalo, Z.; Deanovic, Z. Piroplasmosis in man; report of a case. Documenta de medicina geographica et tropica 1957, 9, 11–16. [Google Scholar]
- Homer, M.J.; Aguilar-Delfin, I.; Telford, S.R., 3rd; Krause, P.J.; Persing, D.H. Babesiosis. Clin. Microbiol. Rev. 2000, 13, 451–469. [Google Scholar] [CrossRef]
- Herwaldt, B.L.; Linden, J.V.; Bosserman, E.; Young, C.; Olkowska, D.; Wilson, M. Transfusion-associated babesiosis in the United States: A description of cases. Ann. Intern. Med. 2011, 155, 509–519. [Google Scholar] [CrossRef]
- Vannier, E.; Krause, P.J. Human babesiosis. N. Engl. J. Med. 2012, 366, 2397–2407. [Google Scholar] [CrossRef] [PubMed]
- Jalovecka, M.; Sojka, D.; Ascencio, M.; Schnittger, L. Babesia Life Cycle—When Phylogeny Meets Biology. Trends Parasitol. 2019, 35, 356–368. [Google Scholar] [CrossRef] [PubMed]
- Montero, E.; Rafiq, S.; Heck, S.; Lobo, C.A. Inhibition of human erythrocyte invasion by Babesia divergens using serine protease inhibitors. Mol. Biochem. Parasitol. 2007, 153, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Montero, E.; Rodriguez, M.; Gonzalez, L.M.; Lobo, C.A. Babesia divergens: Identification and characterization of BdHSP-20, a small heat shock protein. Exp. Parasitol. 2008, 119, 238–245. [Google Scholar] [CrossRef]
- Montero, E.; Rodriguez, M.; Oksov, Y.; Lobo, C.A. Babesia divergens apical membrane antigen 1 and its interaction with the human red blood cell. Infect. Immunity 2009, 77, 4783–4793. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, M.; Alhassan, A.; Ord, R.L.; Cursino-Santos, J.R.; Singh, M.; Gray, J.; Lobo, C.A. Identification and characterization of the RouenBd1987 Babesia divergens Rhopty-Associated Protein 1. PLoS ONE 2014, 9, e107727. [Google Scholar] [CrossRef] [PubMed]
- Repnik, U.; Gangopadhyay, P.; Bietz, S.; Przyborski, J.M.; Griffiths, G.; Lingelbach, K. The apicomplexan parasite Babesia divergens internalizes band 3, glycophorin A and spectrin during invasion of human red blood cells. Cell. Microbiol. 2015, 17, 1052–1068. [Google Scholar] [CrossRef] [PubMed]
- Cursino-Santos, J.R.; Halverson, G.; Rodriguez, M.; Narla, M.; Lobo, C.A. Identification of binding domains on red blood cell glycophorins for Babesia divergens. Transfusion 2014, 54, 982–989. [Google Scholar] [CrossRef] [PubMed]
- Lobo, C.A. Babesia divergens and Plasmodium falciparum use common receptors, glycophorins A and B, to invade the human red blood cell. Infect. Immunity 2005, 73, 649–651. [Google Scholar] [CrossRef] [PubMed]
- Cursino-Santos, J.R.; Singh, M.; Pham, P.; Rodriguez, M.; Lobo, C.A. Babesia divergens builds a complex population structure composed of specific ratios of infected cells to ensure a prompt response to changing environmental conditions. Cell. Microbiol. 2016, 18, 859–874. [Google Scholar] [CrossRef] [PubMed]
- Lobo, C.A.; Rodriguez, M.; Cursino-Santos, J.R. Babesia and red cell invasion. Curr. Opin. Hematol. 2012, 19, 170–175. [Google Scholar] [CrossRef] [PubMed]
- Cursino-Santos, J.R.; Singh, M.; Pham, P.; Lobo, C.A. A novel flow cytometric application discriminates among the effects of chemical inhibitors on various phases of Babesia divergens intraerythrocytic cycle. Cytometry Part A 2017, 91, 216–231. [Google Scholar] [CrossRef] [PubMed]
- Sevilla, E.; Gonzalez, L.M.; Luque, D.; Gray, J.; Montero, E. Kinetics of the invasion and egress processes of Babesia divergens, observed by time-lapse video microscopy. Sci. Rep. 2018, 8, 14116. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.M.; Fairhurst, R.M. Malaria parasites and red cell variants: When a house is not a home. Curr. Opin. Hematol. 2014, 21, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Nishi, M.; Hu, K.; Murray, J.M.; Roos, D.S. Organellar dynamics during the cell cycle of Toxoplasma gondii. J. Cell Sci. 2008, 121, 1559–1568. [Google Scholar] [CrossRef]
- Valentin, A.; Rigomier, D.; Precigout, E.; Carcy, B.; Gorenflot, A.; Schrevel, J. Lipid trafficking between high density lipoproteins and Babesia divergens-infected human erythrocytes. Biol. Cell 1991, 73, 63–70. [Google Scholar] [CrossRef]
- Rossouw, I.; Maritz-Olivier, C.; Niemand, J.; van Biljon, R.; Smit, A.; Olivier, N.A.; Birkholtz, L.M. Morphological and Molecular Descriptors of the Developmental Cycle of Babesia divergens Parasites in Human Erythrocytes. PLoS Negl. Trop. Dis. 2015, 9, e0003711. [Google Scholar] [CrossRef]
- Cursino-Santos, J.R.; Alhassan, A.; Singh, M.; Lobo, C.A. Babesia: Impact of cold storage on the survival and the viability of parasites in blood bags. Transfusion 2014, 54, 585–591. [Google Scholar] [CrossRef]

© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lobo, C.A.; Cursino-Santos, J.R.; Singh, M.; Rodriguez, M. Babesia divergens: A Drive to Survive. Pathogens 2019, 8, 95. https://doi.org/10.3390/pathogens8030095
Lobo CA, Cursino-Santos JR, Singh M, Rodriguez M. Babesia divergens: A Drive to Survive. Pathogens. 2019; 8(3):95. https://doi.org/10.3390/pathogens8030095
Chicago/Turabian StyleLobo, Cheryl A, Jeny R Cursino-Santos, Manpreet Singh, and Marilis Rodriguez. 2019. "Babesia divergens: A Drive to Survive" Pathogens 8, no. 3: 95. https://doi.org/10.3390/pathogens8030095
APA StyleLobo, C. A., Cursino-Santos, J. R., Singh, M., & Rodriguez, M. (2019). Babesia divergens: A Drive to Survive. Pathogens, 8(3), 95. https://doi.org/10.3390/pathogens8030095



