Host-Pathogen Interactions of Mycoplasma mycoides in Caprine and Bovine Precision-Cut Lung Slices (PCLS) Models
Abstract
1. Introduction
2. Results
2.1. Viability and Metabolic Activity of Bovine and Caprine PCLS
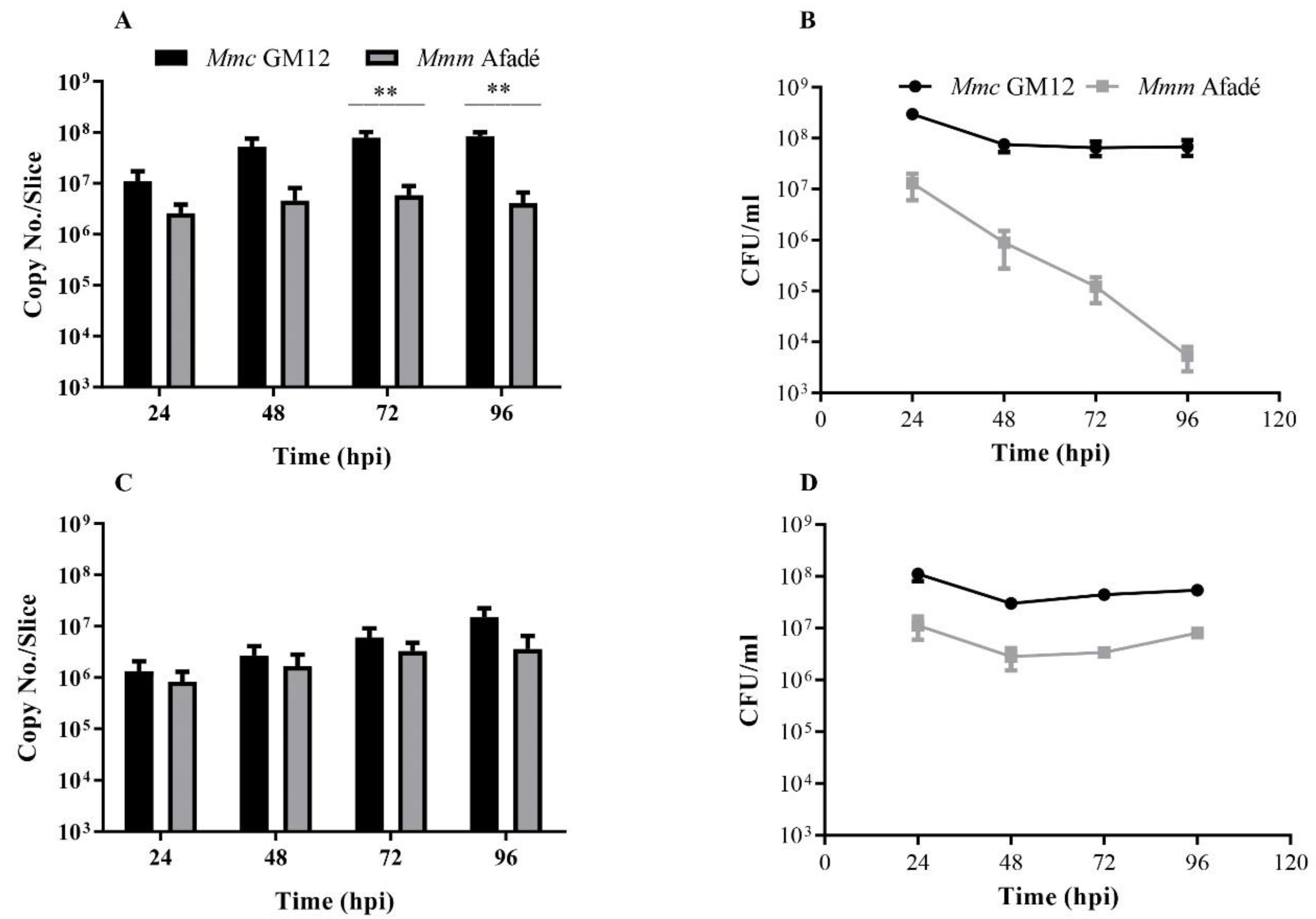
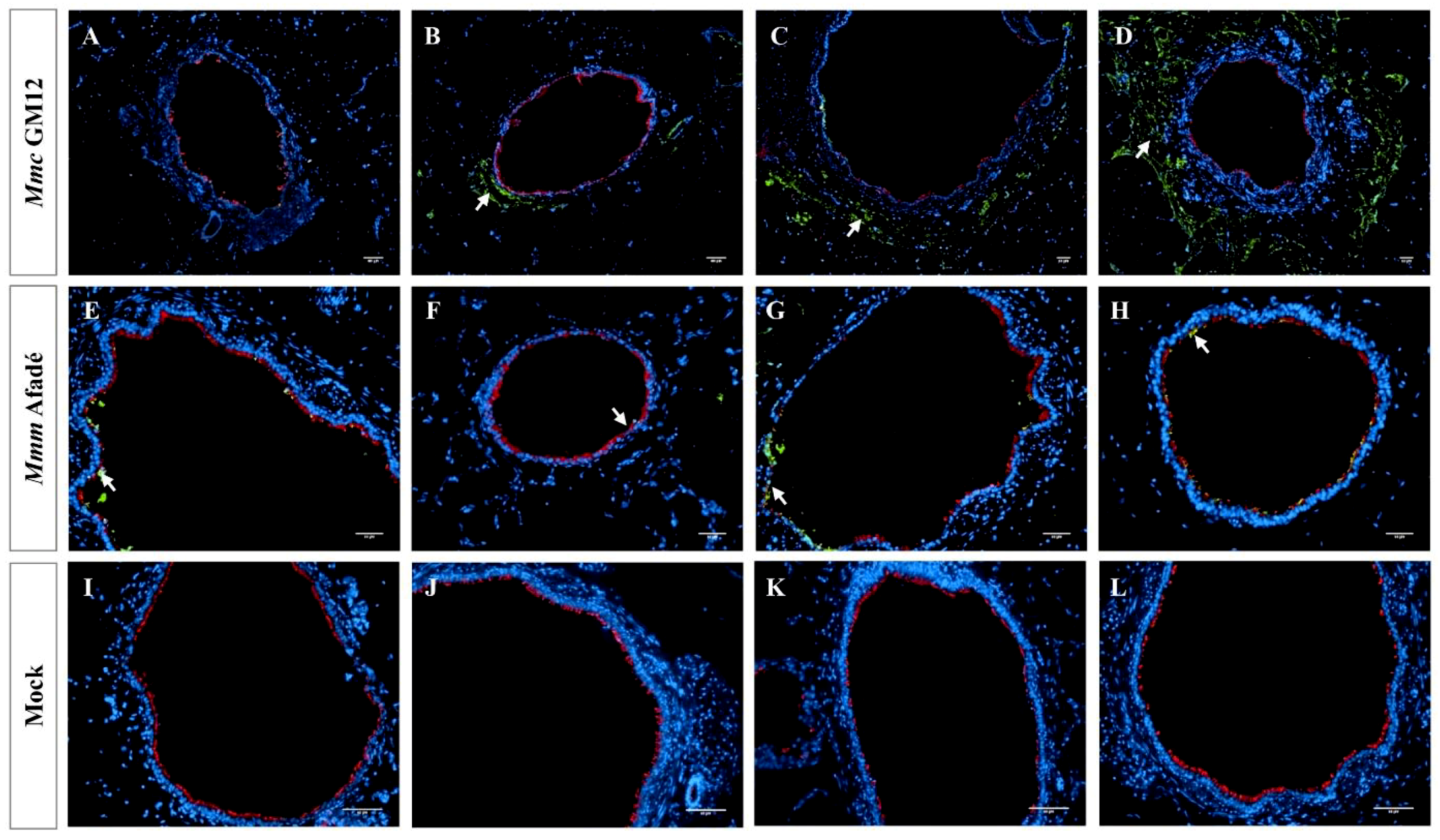
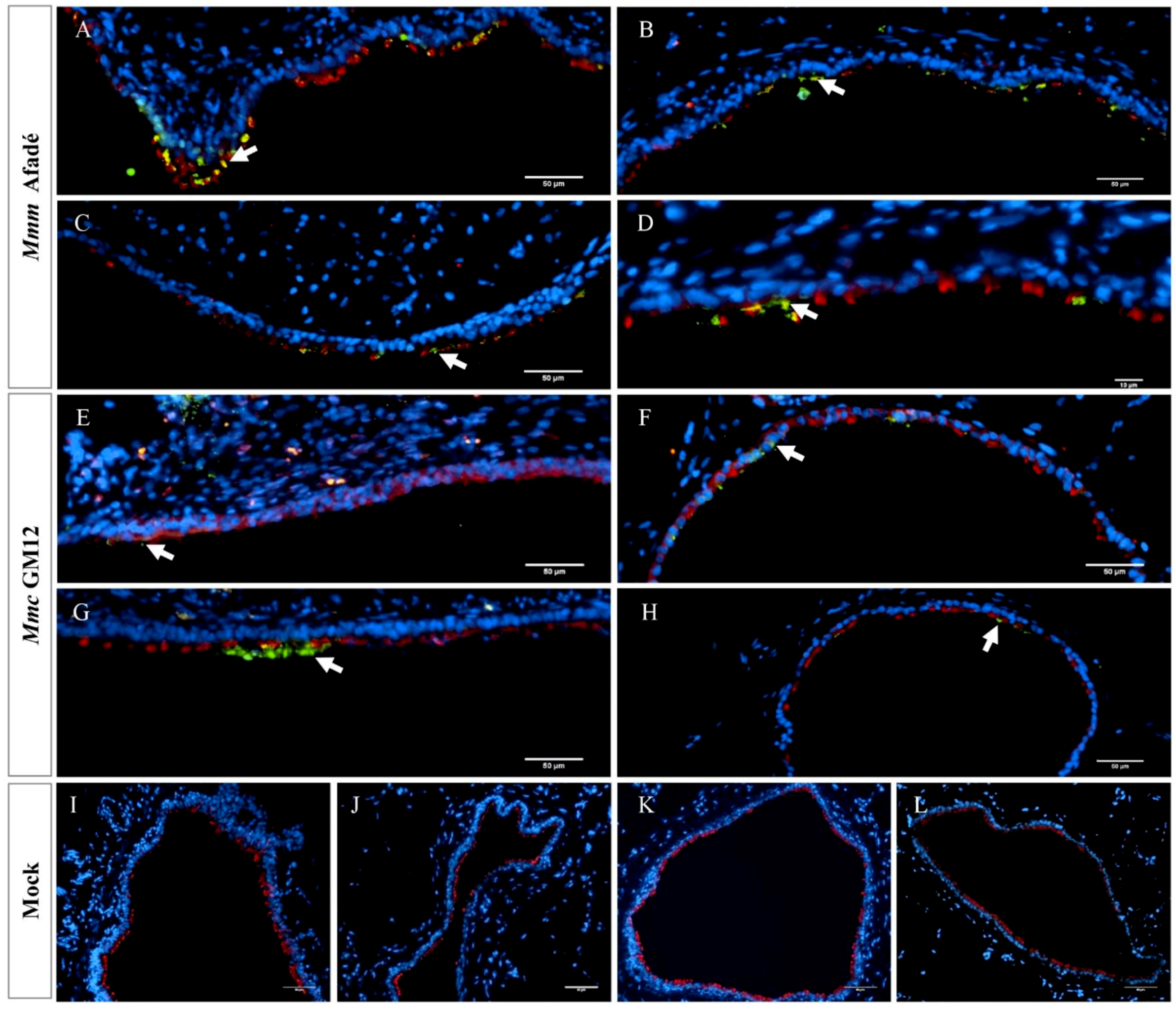
2.2. Adherence of M. mycoides to Caprine PCLS
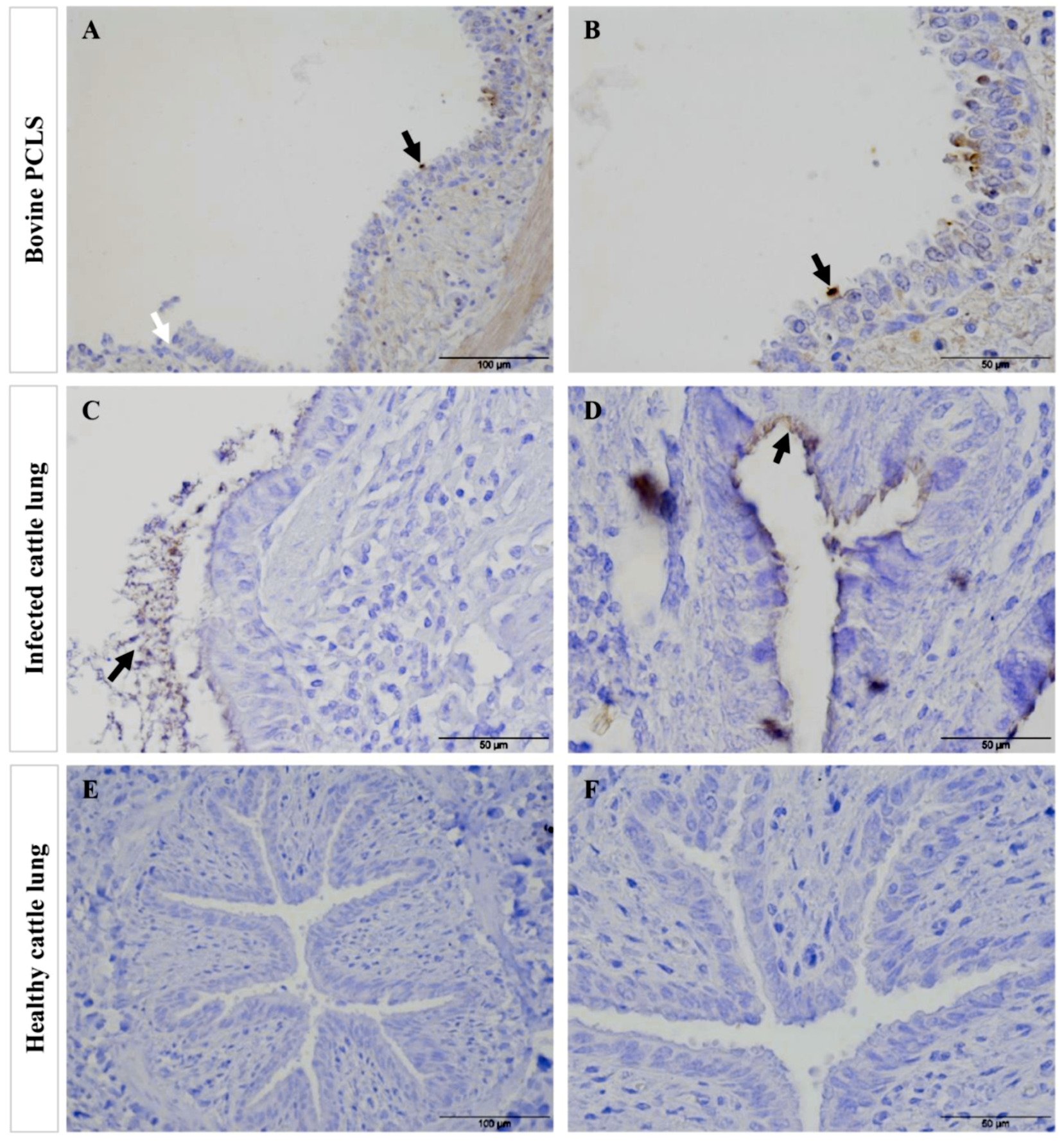
2.3. Adherence of M. mycoides to Bovine PCLS
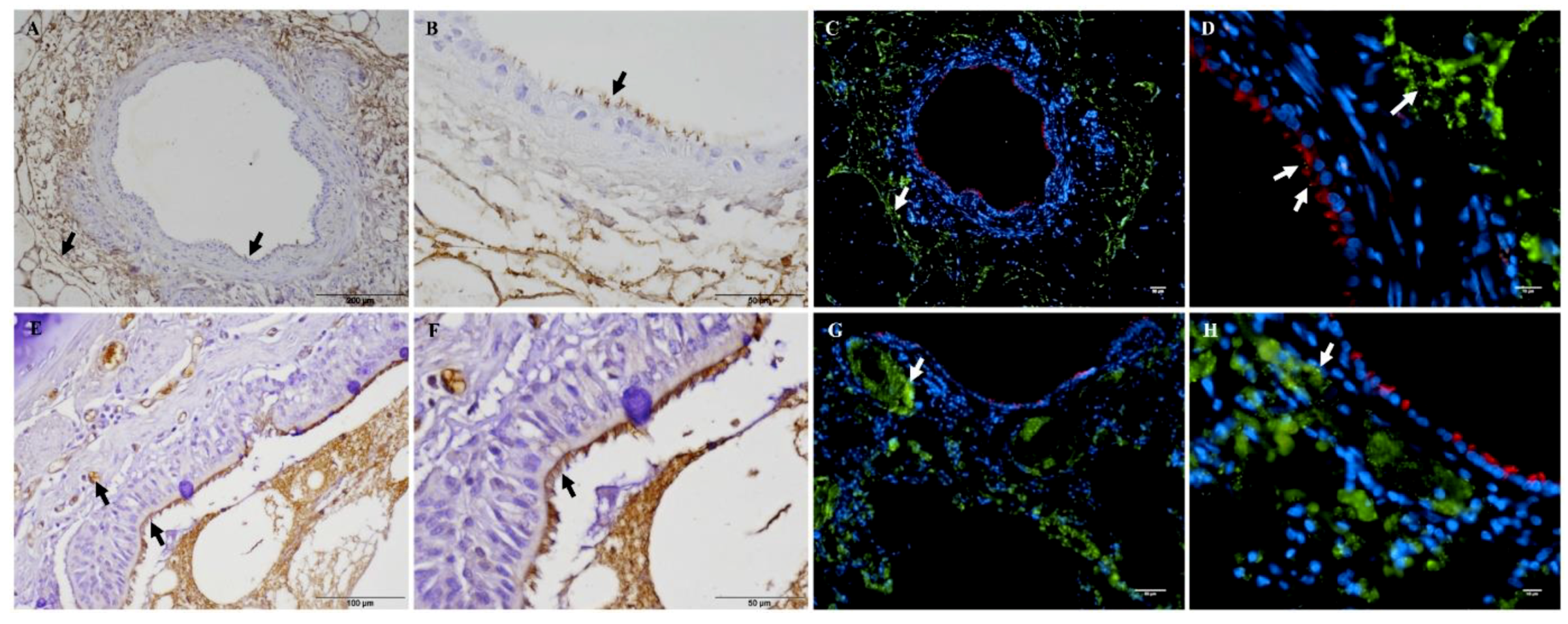
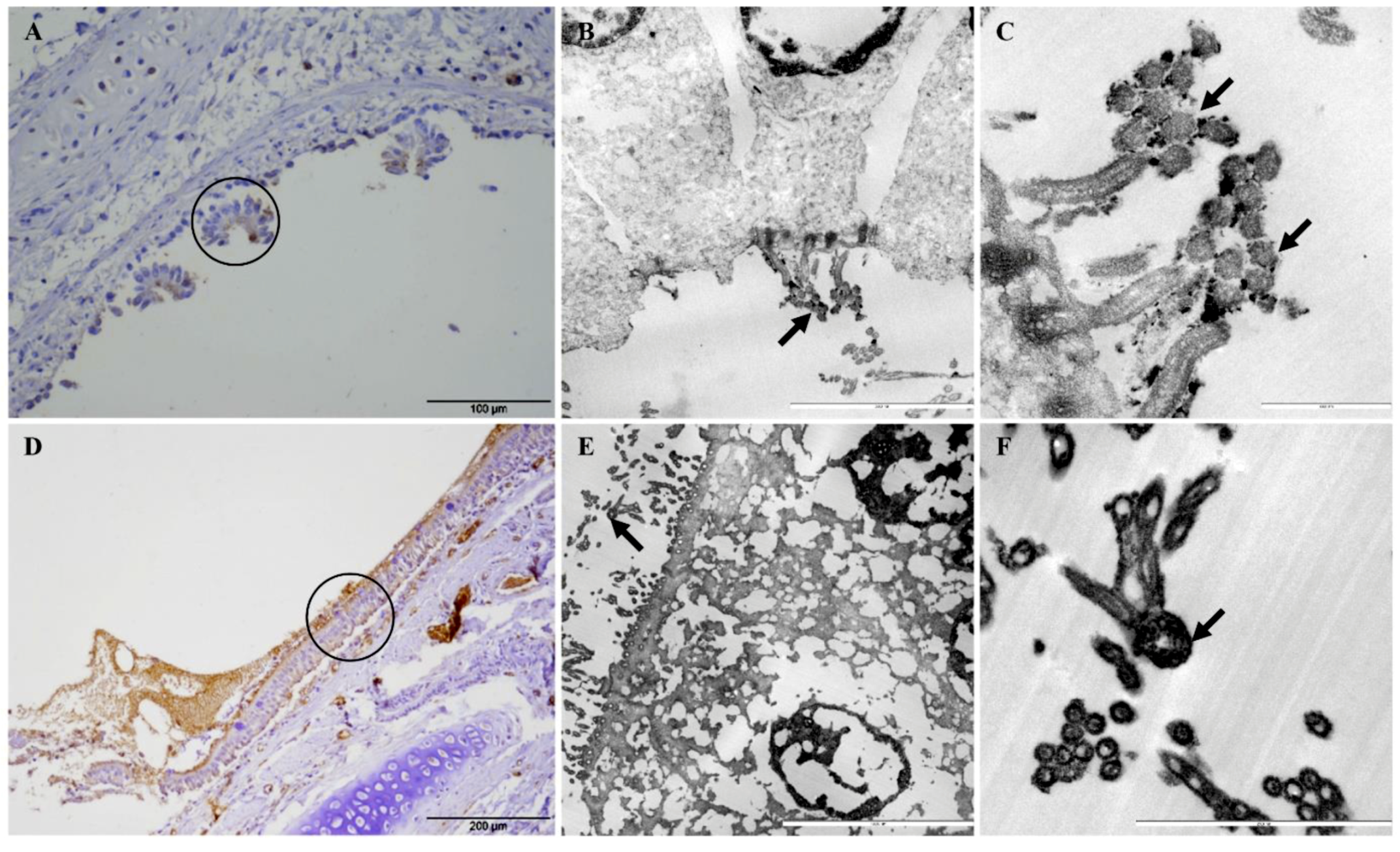
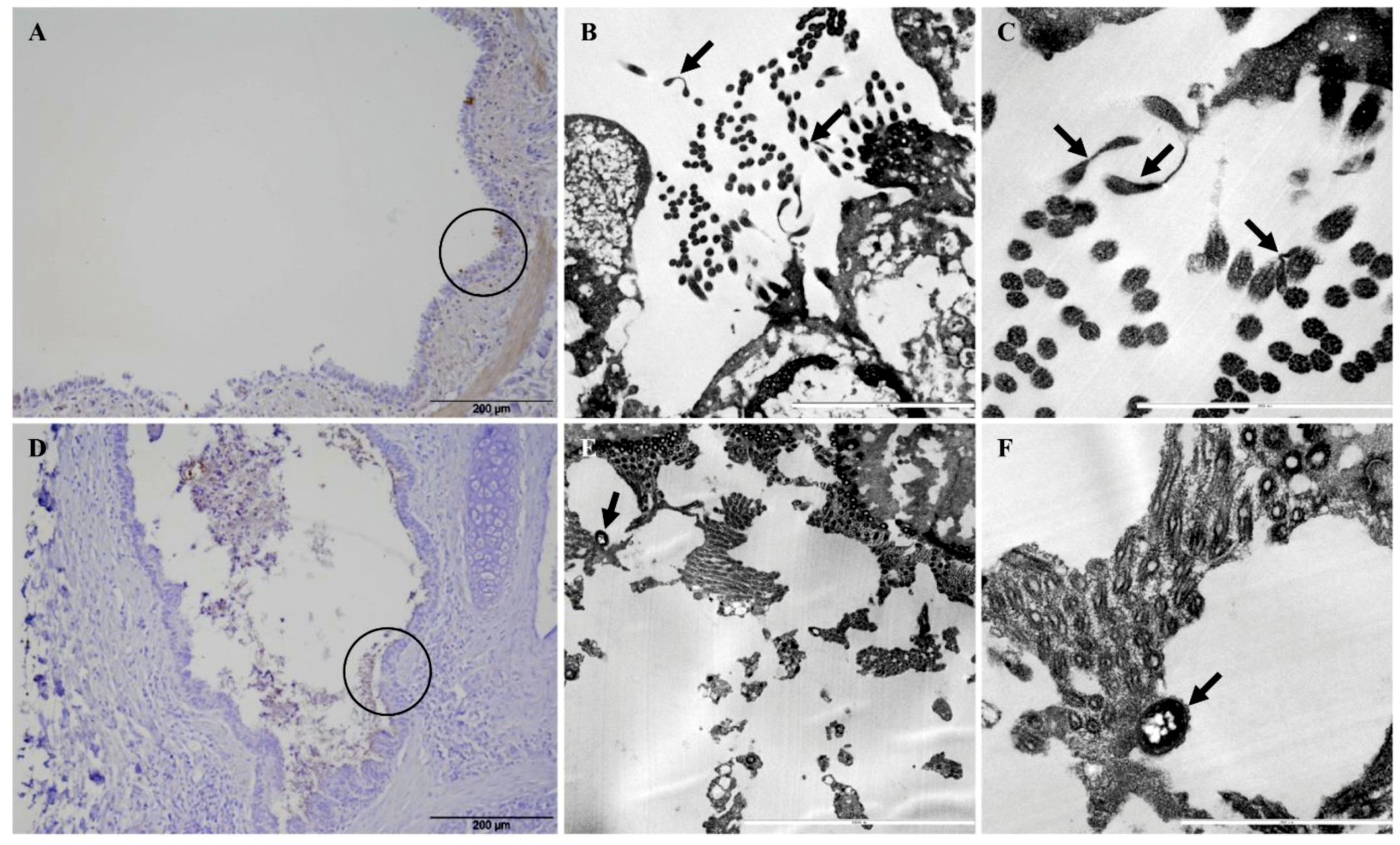
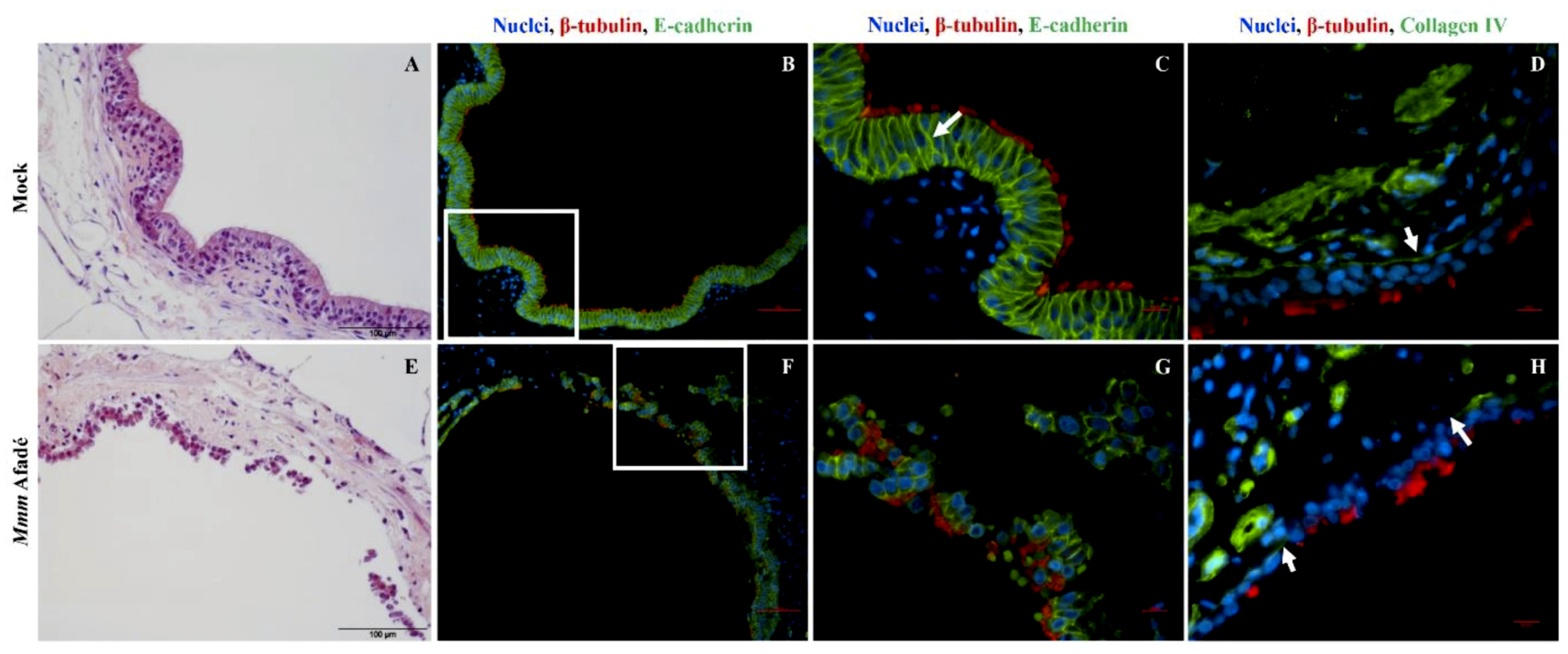
2.4. Colonization and Tissue Tropism of Mycoplasma mycoides
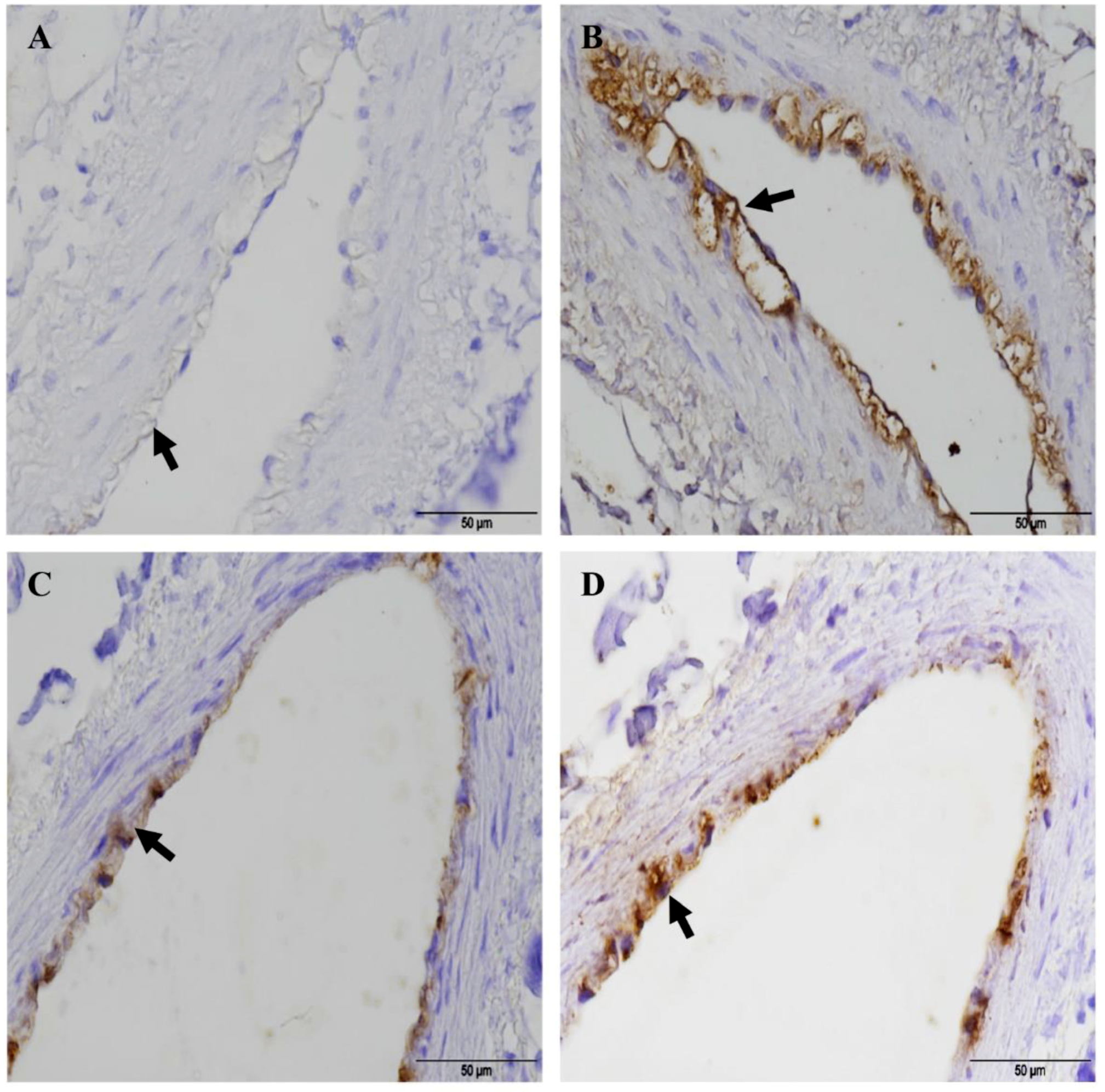
2.5. Histopathological Changes in Long-Term Infected PCLS Resemble the in Vivo Situation
3. Discussion
4. Materials and Methods
4.1. Chemicals, Bacterial Strains and Culture Conditions
4.2. Preparation and Maintenance of PCLS
4.3. Quality Control of PCLS
4.4. Infection of PCLS
4.5. Staining of PCLS
4.6. Electron Microscopy
4.7. DNA Extraction and Quantitative Real-Time PCR (qRT-PCR)
4.8. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Manso-Silvan, L.; Vilei, E.M.; Sachse, K.; Djordjevic, S.P.; Thiaucourt, F.; Frey, J. Mycoplasma leachii sp. nov. as a new species designation for Mycoplasma sp. bovine group 7 of Leach, and reclassification of Mycoplasma mycoides subsp. mycoides LC as a serovar of Mycoplasma mycoides subsp. capri. Int. J. Syst. Evol. Microbiol. 2009, 59, 1353–1358. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A.; Shapiro, B.; Muriuki, C.; Heller, M.; Schnee, C.; Bongcam-Rudloff, E.; Vilei, E.M.; Frey, J.; Jores, J. The origin of the ‘Mycoplasma mycoides cluster’ coincides with domestication of ruminants. PLoS ONE 2012, 7, e36150. [Google Scholar] [CrossRef] [PubMed]
- Cottew, G.S.; Breard, A.; DaMassa, A.J.; Erno, H.; Leach, R.H.; Lefevre, P.C.; Rodwell, A.W.; Smith, G.R. Taxonomy of the Mycoplasma mycoides cluster. Isr. J. Med. Sci. 1987, 23, 632–635. [Google Scholar] [PubMed]
- FAO. Contagious Bovine Pleuropneumonia (CBPP). Available online: http://www.fao.org/ag/againfo/programmes/en/empres/disease_cbpp.asp (accessed on 6 March 2018).
- OIE. Contagious Bovine Pleuropneumonia. Aetiology, Epidemiology, Diagnosis Prevention and Control References. Technical Disease Cards. Available online: http://www.oie.int/en/animal-health-in-the-world/technical-disease-cards/ (accessed on 6 March 2018).
- Tambi, N.E.; Maina, W.O.; Ndi, C. An estimation of the economic impact of contagious bovine pleuropneumonia in Africa. Rev. Sci. Tech. 2006, 25, 999–1011. [Google Scholar] [CrossRef] [PubMed]
- FAO. Recognizing Contagious Bovine Pleuropneumonia. Revised Edition. Available online: www.fao.org/3/a-y4142e.pdf (accessed on 6 March 2018).
- Carter, G.R.; Chengappa, M.M. Microbial Diseases: A Veterinarian’s Guide to Laboratory Diagnosis; Wiley-Blackwell: Hoboken, NJ, USA, 1993; p. 318. [Google Scholar]
- Alemayehu, G.; Leta, S.; Hailu, B. Sero-prevalence of Contagious Bovine Pleuropneumonia (CBPP) in bulls originated from Borena pastoral area of Southern Ethiopia. Trop. Anim. Health Prod. 2015, 47, 983–987. [Google Scholar] [CrossRef] [PubMed]
- Suleiman, A.; Bello, M.; Dzikwi, A.A.; Talba, A.M.; Grema, H.A.; Geidam, Y.A. Serological prevalence of contagious bovine pleuropneumonia in agro-pastoral areas of Nigeria. Trop. Anim. Health Prod. 2015, 47, 1033–1042. [Google Scholar] [CrossRef]
- Sery, A.; Sidibe, C.A.; Cisse, O.; Diallo, M.; Kone, M.; Waret-Szkuta, A.; Roger, F.; Thiaucourt, F.; Niang, M. Seroprevalence of contagious bovine pleuropneumonia (CBPP) in Mali. Trop. Anim. Health Prod. 2015, 47, 395–402. [Google Scholar] [CrossRef]
- Yansambou, M.S.; Diallo, A.A.; Idi, M.; Gagara, H.; Haido, A.M.; Bada Alambedji, R. Serological Prevalence of Contagious Bovine Pleuropneumonia in Niger in 2017. Front. Vet. Sci. 2018, 5, 238. [Google Scholar] [CrossRef]
- Thiaucourt, F.; Bolske, G. Contagious caprine pleuropneumonia and other pulmonary mycoplasmoses of sheep and goats. Rev. Sci. Tech. 1996, 15, 1397–1414. [Google Scholar] [CrossRef]
- Hernandez, L.; Lopez, J.; St-Jacques, M.; Ontiveros, L.; Acosta, J.; Handel, K. Mycoplasma mycoides subsp. capri associated with goat respiratory disease and high flock mortality. Can. Vet. J. 2006, 47, 366–369. [Google Scholar]
- Shah, M.K.; Saddique, U.; Ahmad, S.; Hayat, Y.; Rahman, S.U.; Hassan, M.F.; Ali, T. Isolation rate and antimicrobial susceptibility profiles of Mycoplasma mycoides subspecies capri field isolates from sheep and goats in Pakistan. Short communication. Small Rumin. Res. 2017, 153, 118–122. [Google Scholar] [CrossRef]
- de la Fe, C.; Gomez Martin, A.; Amores, J.; Corrales, J.C.; Sanchez, A.; Poveda, J.B.; Contreras, A. Latent infection of male goats with Mycoplasma agalactiae and Mycoplasma mycoides subspecies capri at an artificial insemination centre. Vet. J. 2010, 186, 113–115. [Google Scholar] [CrossRef]
- Johnson, G.C.; Fales, W.H.; Shoemake, B.M.; Adkins, P.R.; Middleton, J.R.; Williams, F., 3rd; Zinn, M.; Mitchell, W.J.; Calcutt, M.J. An outbreak of Mycoplasma mycoides subspecies capri arthritis in young goats: A case study. J. Vet. Diagn. Investig. 2019, 31, 453–457. [Google Scholar] [CrossRef]
- Mbulu, R.S.; Tjipura-Zaire, G.; Lelli, R.; Frey, J.; Pilo, P.; Vilei, E.M.; Mettler, F.; Nicholas, R.A.; Huebschle, O.J. Contagious bovine pleuropneumonia (CBPP) caused by vaccine strain T1/44 of Mycoplasma mycoides subsp. mycoides SC. Vet. Microbiol. 2004, 98, 229–234. [Google Scholar] [CrossRef]
- Jores, J.; Mariner, J.C.; Naessens, J. Development of an improved vaccine for contagious bovine pleuropneumonia: An African perspective on challenges and proposed actions. Vet. Res. 2013, 44, 122. [Google Scholar] [CrossRef][Green Version]
- Nkando, I.; Perez-Casal, J.; Mwirigi, M.; Prysliak, T.; Townsend, H.; Berberov, E.; Kuria, J.; Mugambi, J.; Soi, R.; Liljander, A.; et al. Recombinant Mycoplasma mycoides proteins elicit protective immune responses against contagious bovine pleuropneumonia. Vet. Immunol. Immunopathol. 2016, 171, 103–114. [Google Scholar] [CrossRef]
- Sada, A.; Tambuwal, F.M.; Egwu, G.O.; Manga, S.B.; Akalusi, Y.; Bello, M.B. Contagious bovine pleuropneumonia (CBPP) vaccination and prevalence (2000–2012) in Katsina state, north-western Nigeria. Vom J. Vet. Sci. 2015, 10, 33–40. [Google Scholar]
- Scacchia, M.; Tjipura-Zaire, G.; Lelli, R.; Sacchini, F.; Pini, A. Contagious bovine pleuropneumonia: Humoral and pathological events in cattle infected by endotracheal intubation or by exposure to infected animals. Vet. Ital. 2011, 47, 407–413. [Google Scholar]
- Revell, S.G. Local reactions following C.B.P.P. vaccination in Zambia. Trop. Anim. Health Prod. 1973, 5, 246–252. [Google Scholar] [CrossRef]
- Muuka, G.M.; Songolo, N.; Kabilika, S.; Fandamu, P.; Buonavoglia, D.; Scacchia, M. Private sector involvement in the control of contagious bovine pleuropneumonia (CBPP) in the Kazungula district of Zambia benefitted the community and the control strategy. Trop. Anim. Health Prod. 2013, 45, 699–703. [Google Scholar] [CrossRef]
- Amanfu, W. Contagious bovine pleuropneumonia (lung sickness) in Africa. Onderstepoort J. Vet. Res. 2009, 76, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.G.; Hao, Y.Q.; Zhang, L.; Hao, R.X.; Liu, X.L.; Huang, Z.Y. Molecular cloning and immune response analysis of putative variable lipoproteins from Mycoplasma mycoides subsp capri. Genet. Mol. Res. 2014, 13, 1527–1539. [Google Scholar] [CrossRef] [PubMed]
- Manimaran, K.; Singh, V.P.; Keduzol, L.T.U.; Sanjoy, D.A.S.; Kumars, A.A.; Srivastava, S.K. Development of lyophilized Mycoplasma mycoides subsp. capri vaccine against caprine pleuropneumonia. Indian J. Anim. Sci. 2006, 76, 900–902. [Google Scholar]
- Russell, W.M.S.; Burch, R.L. The Principles of Humane Experimental Technique; Universities Federation for Animal Welfare: Wheathampstaed, UK, 1959; reprinted 1992. [Google Scholar]
- Hynds, R.E.; Bonfanti, P.; Janes, S.M. Regenerating human epithelia with cultured stem cells: Feeder cells, organoids and beyond. EMBO Mol. Med. 2018, 10, 139–150. [Google Scholar] [CrossRef] [PubMed]
- Henjakovic, M.; Martin, C.; Hoymann, H.G.; Sewald, K.; Ressmeyer, A.R.; Dassow, C.; Pohlmann, G.; Krug, N.; Uhlig, S.; Braun, A. Ex vivo lung function measurements in precision-cut lung slices (PCLS) from chemical allergen-sensitized mice represent a suitable alternative to in vivo studies. Toxicol. Sci. Off. J. Soc. Toxicol. 2008, 106, 444–453. [Google Scholar] [CrossRef] [PubMed]
- Lyons-Cohen, M.R.; Thomas, S.Y.; Cook, D.N.; Nakano, H. Precision-cut Mouse Lung Slices to Visualize Live Pulmonary Dendritic Cells. J. Vis. Exp. 2017. [Google Scholar] [CrossRef]
- Temann, A.; Golovina, T.; Neuhaus, V.; Thompson, C.; Chichester, J.A.; Braun, A.; Yusibov, V. Evaluation of inflammatory and immune responses in long-term cultured human precision-cut lung slices. Hum. Vaccines Immunother. 2017, 13, 351–358. [Google Scholar] [CrossRef]
- Fiorentino, D.F.; Zlotnik, A.; Mosmann, T.R.; Howard, M.; O’Garra, A. IL-10 inhibits cytokine production by activated macrophages. J. Immunol. 1991, 147, 3815–3822. [Google Scholar]
- Olszewska-Pazdrak, B.; Casola, A.; Saito, T.; Alam, R.; Crowe, S.E.; Mei, F.; Ogra, P.L.; Garofalo, R.P. Cell-specific expression of RANTES, MCP-1, and MIP-1alpha by lower airway epithelial cells and eosinophils infected with respiratory syncytial virus. J. Virol. 1998, 72, 4756–4764. [Google Scholar]
- Switalla, S.; Lauenstein, L.; Prenzler, F.; Knothe, S.; Forster, C.; Fieguth, H.G.; Pfennig, O.; Schaumann, F.; Martin, C.; Guzman, C.A.; et al. Natural innate cytokine response to immunomodulators and adjuvants in human precision-cut lung slices. Toxicol. Appl. Pharmacol. 2010, 246, 107–115. [Google Scholar] [CrossRef]
- Henjakovic, M.; Sewald, K.; Switalla, S.; Kaiser, D.; Muller, M.; Veres, T.Z.; Martin, C.; Uhlig, S.; Krug, N.; Braun, A. Ex vivo testing of immune responses in precision-cut lung slices. Toxicol. Appl. Pharmacol. 2008, 231, 68–76. [Google Scholar] [CrossRef]
- Niehof, M.; Hildebrandt, T.; Danov, O.; Arndt, K.; Koschmann, J.; Dahlmann, F.; Hansen, T.; Sewald, K. RNA isolation from precision-cut lung slices (PCLS) from different species. BMC Res. Notes 2017, 10, 121. [Google Scholar] [CrossRef]
- Abd El Rahman, S.; Winter, C.; El-Kenawy, A.; Neumann, U.; Herrler, G. Differential sensitivity of well-differentiated avian respiratory epithelial cells to infection by different strains of infectious bronchitis virus. J. Virol. 2010, 84, 8949–8952. [Google Scholar] [CrossRef]
- Vietmeier, J.; Niedorf, F.; Baumer, W.; Martin, C.; Deegen, E.; Ohnesorge, B.; Kietzmann, M. Reactivity of equine airways—A study on precision-cut lung slices. Vet. Res. Commun. 2007, 31, 611–619. [Google Scholar] [CrossRef]
- Meng, F.; Wu, N.H.; Nerlich, A.; Herrler, G.; Valentin-Weigand, P.; Seitz, M. Dynamic Virus-Bacterium Interactions in a Porcine Precision-Cut Lung Slice Coinfection Model: Swine Influenza Virus Paves the Way for Streptococcus suis Infection in a Two-Step Process. Infect. Immun. 2015, 83, 2806–2815. [Google Scholar] [CrossRef]
- Kirchhoff, J.; Uhlenbruck, S.; Keil, G.M.; Schwegmann-Wessels, C.; Ganter, M.; Herrler, G. Infection of differentiated airway epithelial cells from caprine lungs by viruses of the bovine respiratory disease complex. Vet. Microbiol. 2014, 170, 58–64. [Google Scholar] [CrossRef]
- Kirchhoff, J.; Uhlenbruck, S.; Goris, K.; Keil, G.M.; Herrler, G. Three viruses of the bovine respiratory disease complex apply different strategies to initiate infection. Vet. Res. 2014, 45, 20. [Google Scholar] [CrossRef]
- Goris, K.; Uhlenbruck, S.; Schwegmann-Wessels, C.; Kohl, W.; Niedorf, F.; Stern, M.; Hewicker-Trautwein, M.; Bals, R.; Taylor, G.; Braun, A.; et al. Differential sensitivity of differentiated epithelial cells to respiratory viruses reveals different viral strategies of host infection. J. Virol. 2009, 83, 1962–1968. [Google Scholar] [CrossRef]
- Weldearegay, Y.B.; Pich, A.; Schieck, E.; Liljander, A.; Gicheru, N.; Wesonga, H.; Thiaucourt, F.; Kiirika, L.M.; Valentin-Weigand, P.; Jores, J.; et al. Proteomic characterization of pleural effusion, a specific host niche of Mycoplasma mycoides subsp. mycoides from cattle with contagious bovine pleuropneumonia (CBPP). J. Proteom. 2016, 131, 93–103. [Google Scholar] [CrossRef]
- Nicholas, R.; Ayling, R.; McAuliffe, L. (Eds.) Contagious bovine pleuropneumonia. In Mycoplasma Diseases of Ruminants; CABI: Wallingford, UK, 2008; pp. 69–97. [Google Scholar]
- Nicholas, R.; Ayling, R.; McAuliffe, L. (Eds.) Mycoplasma diseases of ruminants. In Respiratory Diseases of Small Ruminants; CABI: Wallingford, UK, 2008; pp. 169–198. [Google Scholar]
- Tardy, F.; Gaurivaud, P.; Manso-Silvan, L.; Thiaucourt, F.; Pellet, M.P.; Mercier, P.; Le Grand, D.; Poumarat, F. Extended surveillance for CBPP in a free country: Challenges and solutions regarding the potential caprine reservoir. Prev. Vet. Med. 2011, 101, 89–95. [Google Scholar] [CrossRef]
- Yaya, A.; Manso-Silvan, L.; Blanchard, A.; Thiaucourt, F. Genotyping of Mycoplasma mycoides subsp. mycoides SC by multilocus sequence analysis allows molecular epidemiology of contagious bovine pleuropneumonia. Vet. Res. 2008, 39, 14. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, N.C.; Thiaucourt, F.; Singh, V.P.; Sunder, J.; Singh, V.P. Isolation of Mycoplasma mycoides small colony type from contagious caprine pleuropneumonia in India. Vet. Rec. 2000, 147, 520–521. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, P.K.; Garg, D.N.; Mahajan, S.K. Isolation of Mycoplasma mycoides subsp. mycoides (LC variant, Y-Goat) from naturally aborted bovine fetuses. Theriogenology 1989, 32, 683–691. [Google Scholar] [CrossRef]
- Perreau, P.; Bind, J.L. Infection naturelle du veau par Mycoplasma mycoides subsp. mycoides (biotype chèvre). Bull. Acad. Vet. Fr. 1981, 54, 491–496. [Google Scholar] [CrossRef]
- Araake, M. Comparison of ciliostasis by mycoplasmas in mouse and chicken tracheal organ cultures. Microbiol. Immunol. 1982, 26, 1–14. [Google Scholar] [CrossRef]
- Takagi, H.; Arakawa, A. The growth and cilia-stopping effect of Mycoplasma gallisepticum 1RF in chicken tracheal organ cultures. Res. Vet. Sci. 1980, 28, 80–86. [Google Scholar] [CrossRef]
- DeBey, M.C.; Ross, R.F. Ciliostasis and loss of cilia induced by Mycoplasma hyopneumoniae in porcine tracheal organ cultures. Infect. Immun. 1994, 62, 5312–5318. [Google Scholar]
- Aye, R.; Mwirigi, M.K.; Frey, J.; Pilo, P.; Jores, J.; Naessens, J. Cyto-adherence of Mycoplasma mycoides subsp. mycoides to bovine lung epithelial cells. BMC Vet. Res. 2015, 11, 27. [Google Scholar] [CrossRef][Green Version]
- Di Teodoro, G.; Marruchella, G.; Di Provvido, A.; Orsini, G.; Ronchi, G.F.; D’Angelo, A.R.; D’Alterio, N.; Sacchini, F.; Scacchia, M. Respiratory explants as a model to investigate early events of contagious bovine pleuropneumonia infection. Vet. Res. 2018, 49, 5. [Google Scholar] [CrossRef]
- Bertin, C.; Pau-Roblot, C.; Courtois, J.; Manso-Silvan, L.; Thiaucourt, F.; Tardy, F.; Le Grand, D.; Poumarat, F.; Gaurivaud, P. Characterization of free exopolysaccharides secreted by Mycoplasma mycoides subsp. mycoides. PLoS ONE 2013, 8, e68373. [Google Scholar] [CrossRef]
- Gaurivaud, P.; Lakhdar, L.; Le Grand, D.; Poumarat, F.; Tardy, F. Comparison of in vivo and in vitro properties of capsulated and noncapsulated variants of Mycoplasma mycoides subsp. mycoides strain Afade: A potential new insight into the biology of contagious bovine pleuropneumonia. FEMS Microbiol. Lett. 2014, 359, 42–49. [Google Scholar] [CrossRef]
- Clarke, T.B.; Francella, N.; Huegel, A.; Weiser, J.N. Invasive bacterial pathogens exploit TLR-mediated downregulation of tight junction components to facilitate translocation across the epithelium. Cell Host Microbe 2011, 9, 404–414. [Google Scholar] [CrossRef]
- Beisswenger, C.; Coyne, C.B.; Shchepetov, M.; Weiser, J.N. Role of p38 MAP kinase and transforming growth factor-beta signaling in transepithelial migration of invasive bacterial pathogens. J. Biol. Chem. 2007, 282, 28700–28708. [Google Scholar] [CrossRef]
- DaMassa, A.J.; Brooks, D.L.; Adler, H.E. Caprine mycoplasmosis: Widespread infection in goats with Mycoplasma mycoides subsp mycoides (large-colony type). Am. J. Vet. Res. 1983, 44, 322–325. [Google Scholar]
- Jores, J.; Ma, L.; Ssajjakambwe, P.; Schieck, E.; Liljander, A.; Chandran, S.; Stoffel, M.H.; Cippa, V.; Arfi, Y.; Assad-Garcia, N.; et al. Removal of a Subset of Non-essential Genes Fully Attenuates a Highly Virulent Mycoplasma Strain. Front. Microbiol. 2019, 10, 664. [Google Scholar] [CrossRef]
- Sterner-Kock, A.; Haider, W.; Sacchini, F.; Liljander, A.; Meens, J.; Poole, J.; Guschlbauer, M.; Heller, M.; Naessens, J.; Jores, J. Morphological characterization and immunohistochemical detection of the proinflammatory cytokines IL-1beta, IL-17A, and TNF-alpha in lung lesions associated with contagious bovine pleuropneumonia. Trop. Anim. Health Prod. 2016, 48, 569–576. [Google Scholar] [CrossRef][Green Version]
- Steukers, L.; Glorieux, S.; Vandekerckhove, A.P.; Favoreel, H.W.; Nauwynck, H.J. Diverse microbial interactions with the basement membrane barrier. Trends Microbiol. 2012, 20, 147–155. [Google Scholar] [CrossRef]
- Bergmann, S.; Hammerschmidt, S. Fibrinolysis and host response in bacterial infections. Thromb. Haemost. 2007, 98, 512–520. [Google Scholar] [CrossRef]
- Lahteenmaki, K.; Kuusela, P.; Korhonen, T.K. Bacterial plasminogen activators and receptors. FEMS Microbiol. Rev. 2001, 25, 531–552. [Google Scholar] [CrossRef]
- Pilo, P.; Frey, J.; Vilei, E.M. Molecular mechanisms of pathogenicity of Mycoplasma mycoides subsp. mycoides SC. Vet. J. 2007, 174, 513–521. [Google Scholar] [CrossRef][Green Version]
- Bischof, D.F.; Janis, C.; Vilei, E.M.; Bertoni, G.; Frey, J. Cytotoxicity of Mycoplasma mycoides subsp. mycoides small colony type to bovine epithelial cells. Infect. Immun. 2008, 76, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A.; Santana-Cruz, I.; Hegerman, J.; Gourle, H.; Schieck, E.; Lambert, M.; Nadendla, S.; Wesonga, H.; Miller, R.A.; Vashee, S.; et al. High quality draft genomes of the Mycoplasma mycoides subsp. mycoides challenge strains Afade and B237. Stand. Genom. Sci. 2015, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Wise, K.S.; Calcutt, M.J.; Foecking, M.F.; Madupu, R.; DeBoy, R.T.; Roske, K.; Hvinden, M.L.; Martin, T.R.; Durkin, A.S.; Glass, J.I.; et al. Complete genome sequences of Mycoplasma leachii strain PG50T and the pathogenic Mycoplasma mycoides subsp. mycoides small colony biotype strain Gladysdale. J. Bacteriol. 2012, 194, 4448–4449. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kirchhoff, H.; Rosengarten, R. Isolation of a motile mycoplasma from fish. J. Gen. Microbiol. 1984, 130, 2439–2445. [Google Scholar] [CrossRef] [PubMed]
- Jores, J.; Meens, J.; Buettner, F.F.; Linz, B.; Naessens, J.; Gerlach, G.F. Analysis of the immunoproteome of Mycoplasma mycoides subsp. mycoides small colony type reveals immunogenic homologues to other known virulence traits in related Mycoplasma species. Vet. Immunol. Immunopathol. 2009, 131, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, Y.; Assad-Garcia, N.; Kostylev, M.; Noskov, V.N.; Wise, K.S.; Karas, B.J.; Stam, J.; Montague, M.G.; Hanly, T.J.; Enriquez, N.J.; et al. Bacterial genome reduction using the progressive clustering of deletions via yeast sexual cycling. Genome Res. 2015, 25, 435–444. [Google Scholar] [CrossRef] [PubMed]
- Sehl, J.; Hänske, J.; Jores, J.; Liljander, A.; Heller, M.; Schieck, E.; Homeier-Bachmann, T.; Sauter-Louis, C.; Ulrich, U.; Teifke, J.P.; et al. Lungenseuche der Rinder—Pathomorphologie nach experimenteller Infektion. Tierärztliche Praxis Ausgabe G Großtiere Nutztiere 2018, 46, A1–A9. [Google Scholar]
- Punyadarsaniya, D.; Liang, C.H.; Winter, C.; Petersen, H.; Rautenschlein, S.; Hennig-Pauka, I.; Schwegmann-Wessels, C.; Wu, C.Y.; Wong, C.H.; Herrler, G. Infection of differentiated porcine airway epithelial cells by influenza virus: Differential susceptibility to infection by porcine and avian viruses. PLoS ONE 2011, 6, e28429. [Google Scholar] [CrossRef]
- Lehmbecker, A.; Rittinghausen, S.; Rohn, K.; Baumgartner, W.; Schaudien, D. Nanoparticles and pop-off technique for electron microscopy: A known technique for a new purpose. Toxicol. Pathol. 2014, 42, 1041–1046. [Google Scholar] [CrossRef]

| Gene | Primer *** | Primer Sequence (5’-3’) *** | Primer Binding Positions | Acc. No. | Host | |
|---|---|---|---|---|---|---|
| Downstream | Upstream | |||||
| CEACAM18 * | oCC18r-fw | AGCCAAATCTACATCACCCC | 149 to 168 | - | XM_024979463 | Bovine |
| oCC18r-rev | ACCTCTAATGGACACACTTT | - | 364 to 345 | |||
| CEACAM18 * | oCC18z-fw | AGCCAAATCTACATCGCCCC | 406 to 425 | - | XM_018063197 | Caprine |
| oCC18z-rev | ACCTCTAACGGACACACTTT | - | 621 to 602 | |||
| MMS_A0796 ** | oMMS_A0796-fw | AGCTTGTTCTAAAGTTCTTG | 273 to 254 | - | CP002107 | Mmm Gladysdale |
| oMMS_A0796-rev | CTGGTGATTTAATGAGAAAAG | - | 92 to 112 | |||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weldearegay, Y.B.; Müller, S.; Hänske, J.; Schulze, A.; Kostka, A.; Rüger, N.; Hewicker-Trautwein, M.; Brehm, R.; Valentin-Weigand, P.; Kammerer, R.; et al. Host-Pathogen Interactions of Mycoplasma mycoides in Caprine and Bovine Precision-Cut Lung Slices (PCLS) Models. Pathogens 2019, 8, 82. https://doi.org/10.3390/pathogens8020082
Weldearegay YB, Müller S, Hänske J, Schulze A, Kostka A, Rüger N, Hewicker-Trautwein M, Brehm R, Valentin-Weigand P, Kammerer R, et al. Host-Pathogen Interactions of Mycoplasma mycoides in Caprine and Bovine Precision-Cut Lung Slices (PCLS) Models. Pathogens. 2019; 8(2):82. https://doi.org/10.3390/pathogens8020082
Chicago/Turabian StyleWeldearegay, Yenehiwot Berhanu, Sandy Müller, Jana Hänske, Anja Schulze, Aline Kostka, Nancy Rüger, Marion Hewicker-Trautwein, Ralph Brehm, Peter Valentin-Weigand, Robert Kammerer, and et al. 2019. "Host-Pathogen Interactions of Mycoplasma mycoides in Caprine and Bovine Precision-Cut Lung Slices (PCLS) Models" Pathogens 8, no. 2: 82. https://doi.org/10.3390/pathogens8020082
APA StyleWeldearegay, Y. B., Müller, S., Hänske, J., Schulze, A., Kostka, A., Rüger, N., Hewicker-Trautwein, M., Brehm, R., Valentin-Weigand, P., Kammerer, R., Jores, J., & Meens, J. (2019). Host-Pathogen Interactions of Mycoplasma mycoides in Caprine and Bovine Precision-Cut Lung Slices (PCLS) Models. Pathogens, 8(2), 82. https://doi.org/10.3390/pathogens8020082







