Molecular Detection and Genetic Characterization of Potential Zoonotic Swine Enteric Viruses in Northern China
Abstract
1. Introduction
2. Results
2.1. Prevalence of PAstV, EMCV, PKV, and PSaV in Pigs Raised on SPF and Conventional Farms
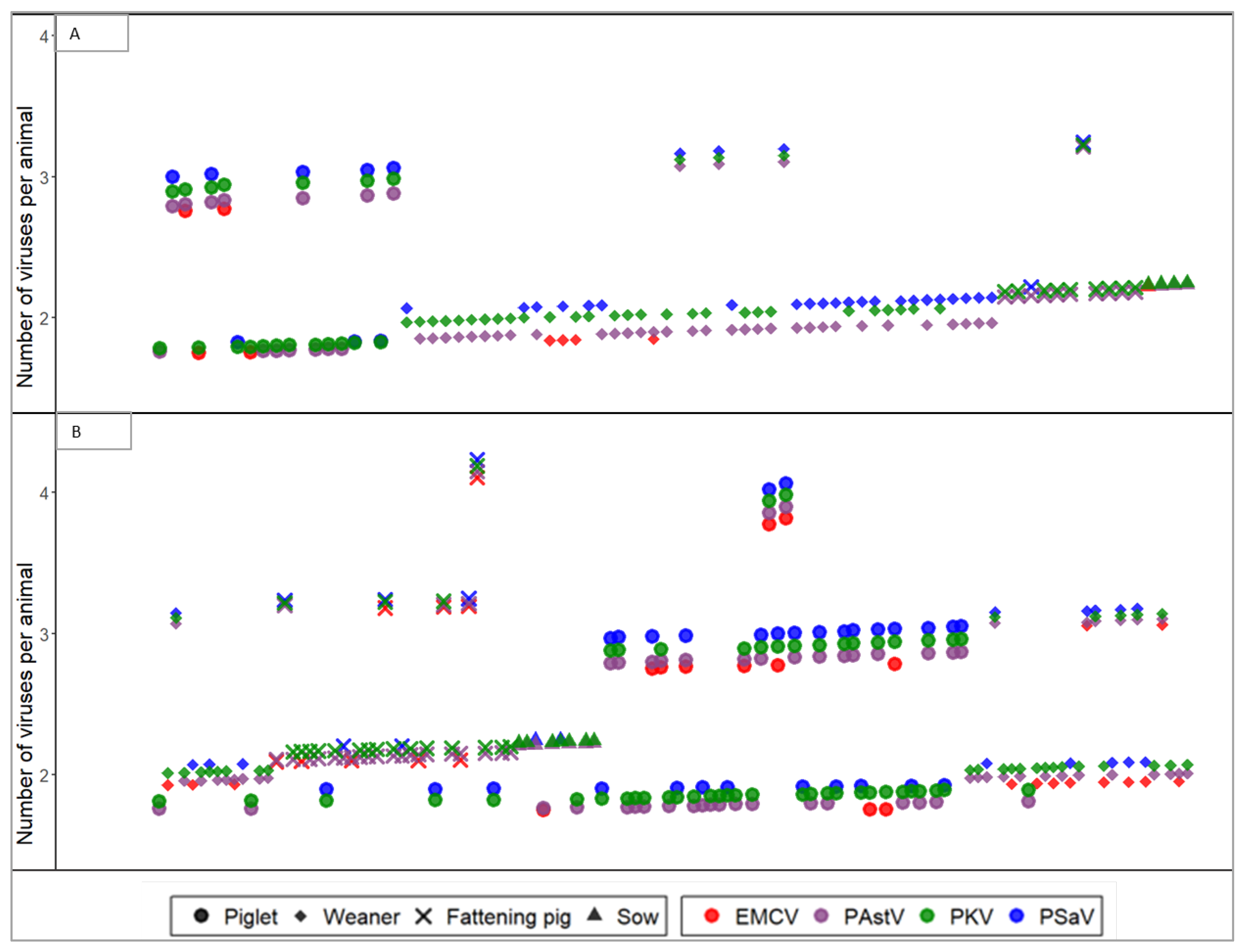
2.2. Prevalence of PAstV, EMCV, PKV, and PSaV in Different Age Groups
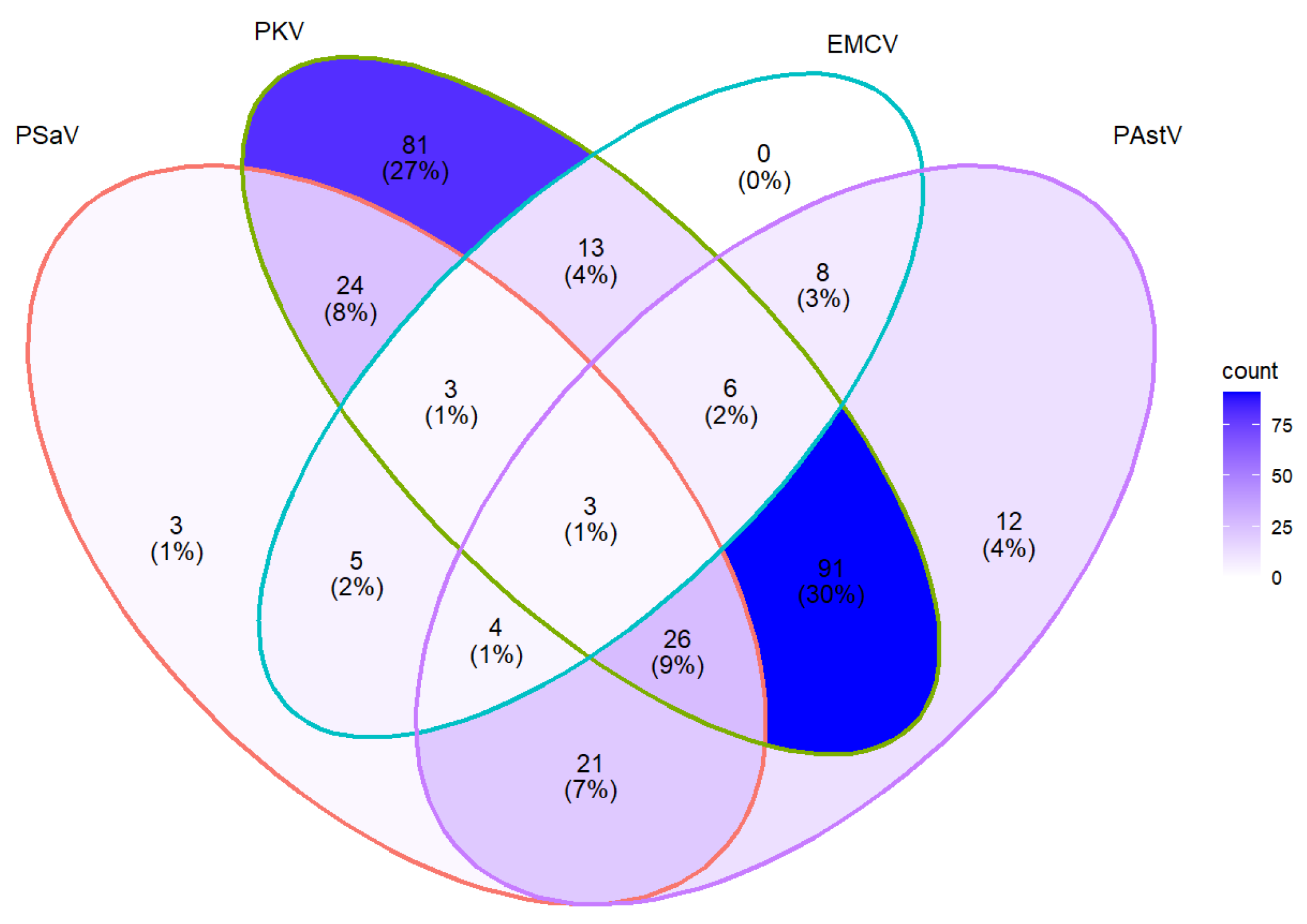
2.3. Coinfection of PAstV, EMCV, PKV, and PSaV
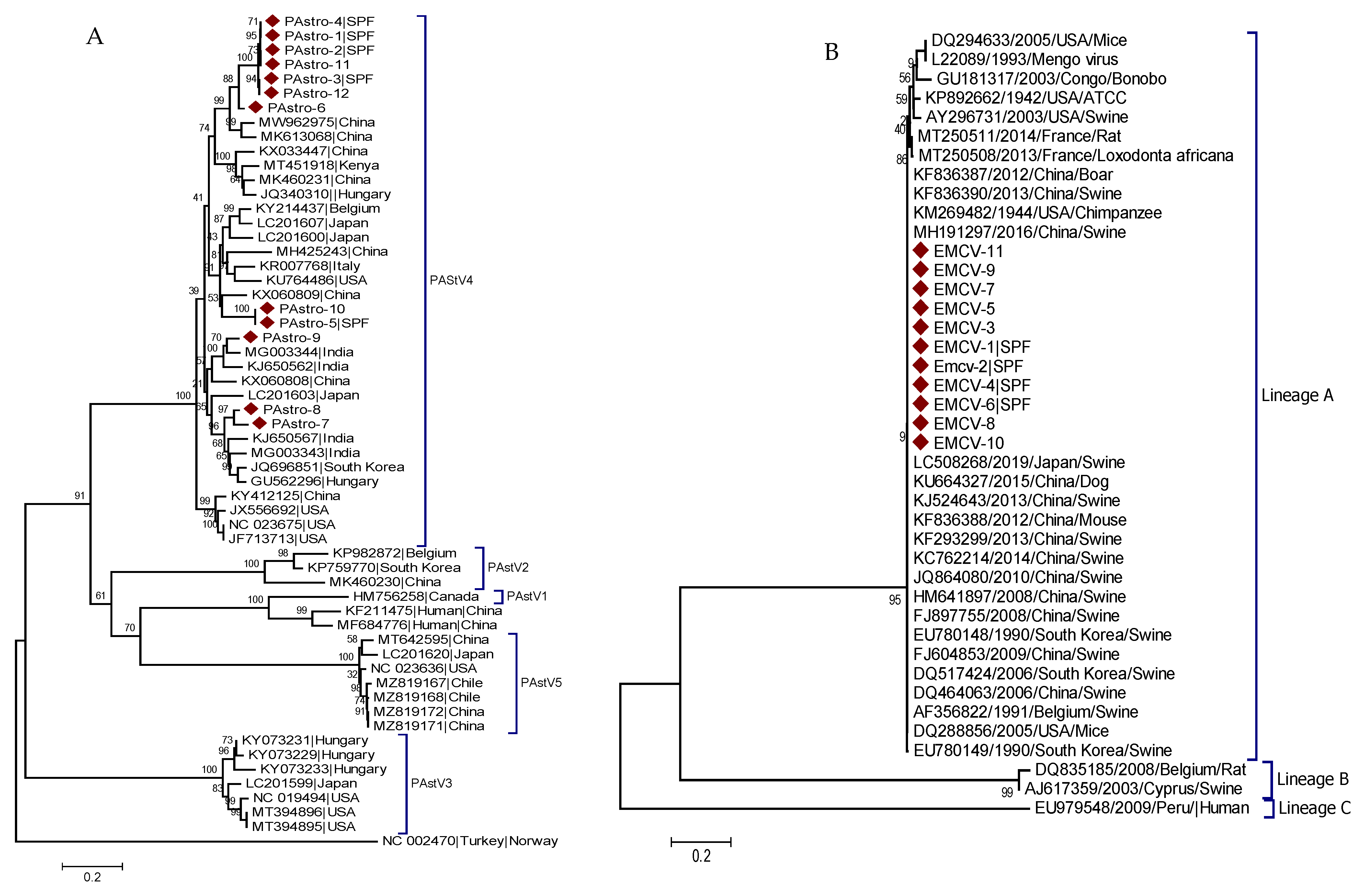
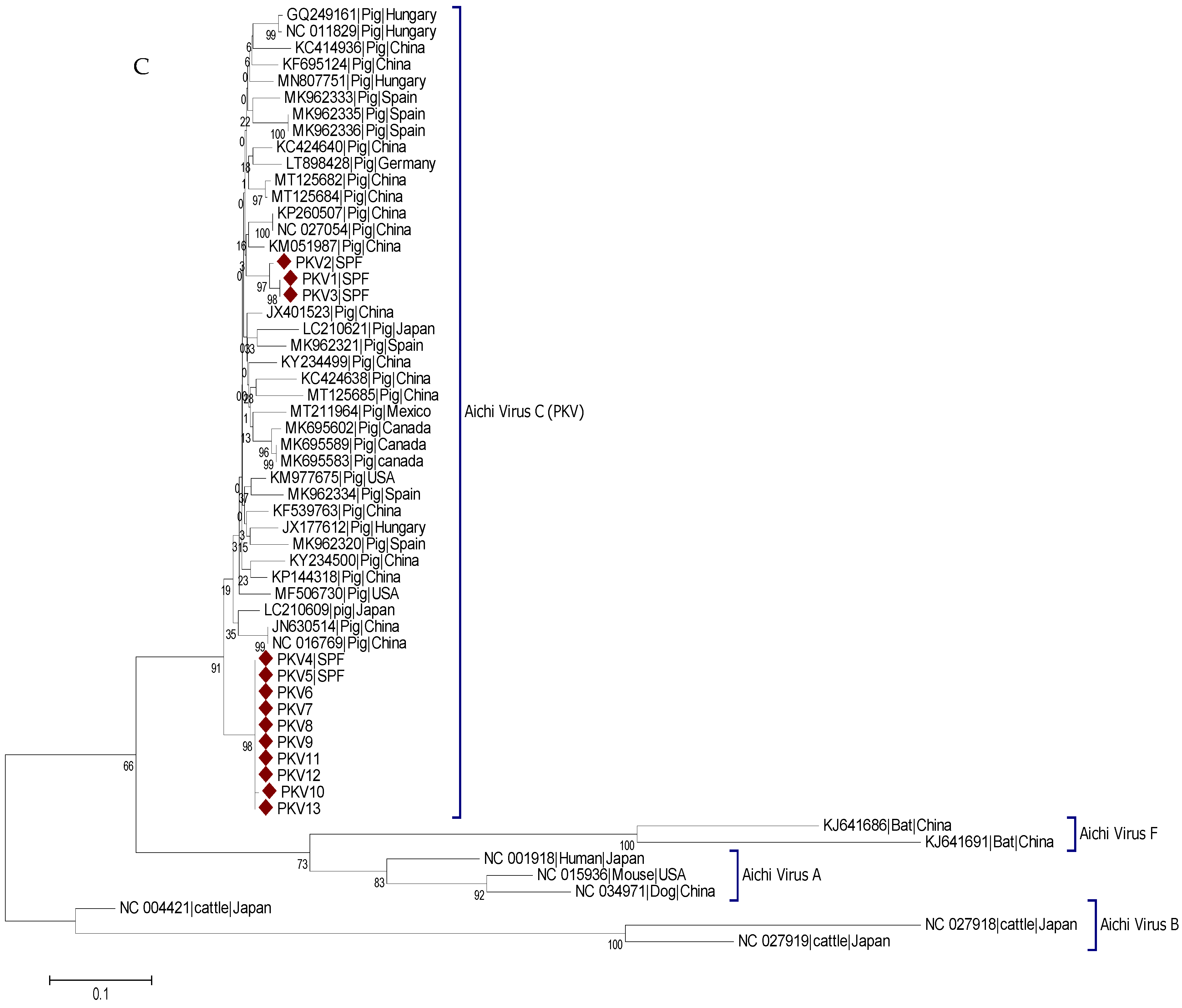
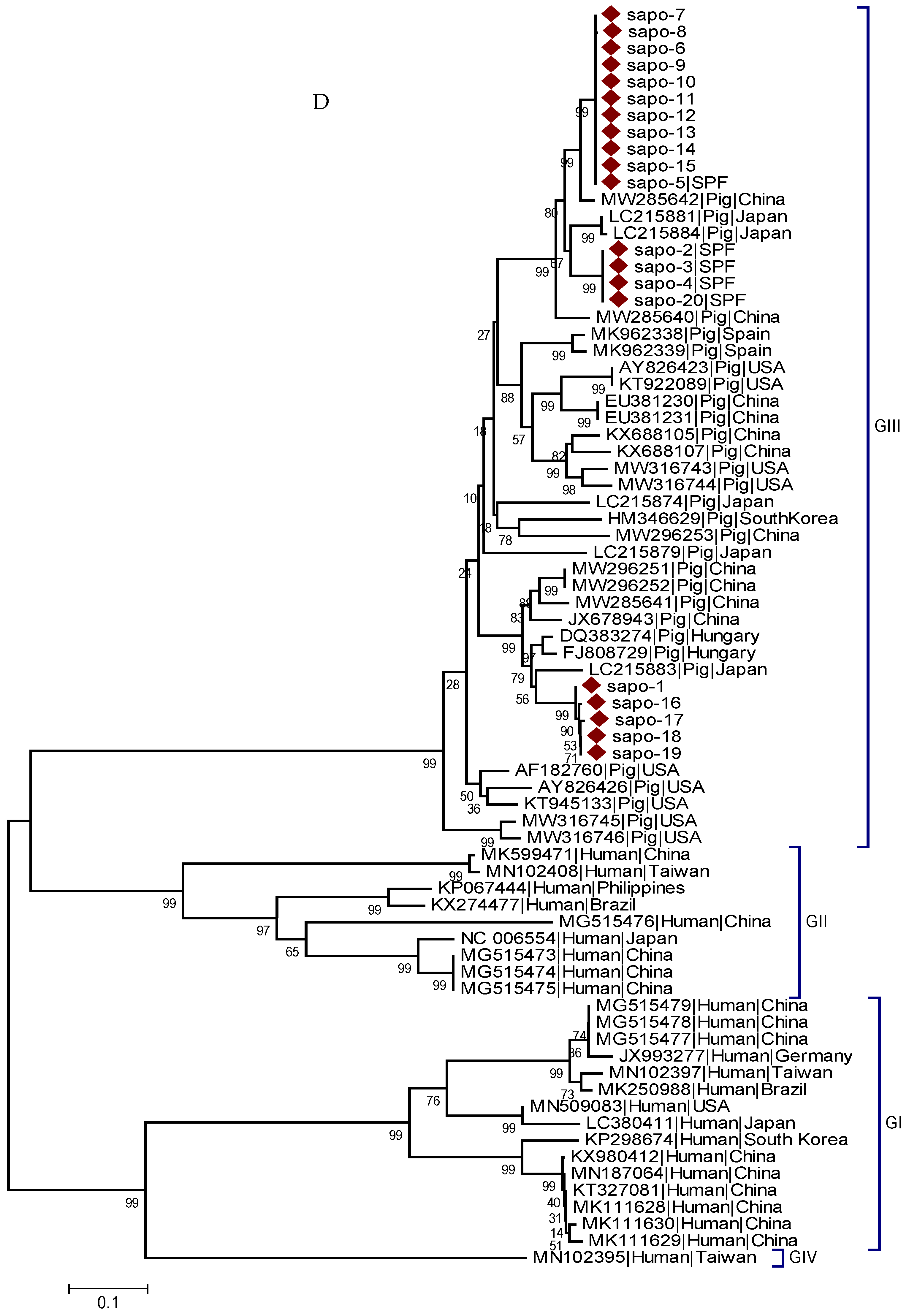
2.4. Sequencing and Phylogenetic Analysis
3. Discussion
4. Materials and Methods
4.1. Specimen Collection
4.2. RNA Extraction and Reverse Transcription
4.3. Primers, PCR Protocols, and Gel Imaging
4.4. DNA Sequences and Phylogenetic Analysis
4.5. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Monini, M.; Di Bartolo, I.; Ianiro, G.; Angeloni, G.; Magistrali, C.F.; Ostanello, F.; Ruggeri, F.M. Detection and molecular characterization of zoonotic viruses in swine fecal samples in Italian pig herds. Arch. Virol. 2015, 160, 2547–2556. [Google Scholar] [CrossRef] [PubMed]
- Kumthip, K.; Khamrin, P.; Saikruang, W.; Kongkaew, A.; Vachirachewin, R.; Ushijima, H.; Maneekarn, N. Detection and genetic characterization of porcine astroviruses in piglets with and without diarrhea in Thailand. Arch. Virol. 2018, 163, 1823–1829. [Google Scholar] [CrossRef] [PubMed]
- Dufkova, L.; Scigalkova, I.; Moutelikova, R.; Malenovska, H.; Prodelalova, J. Genetic diversity of porcine sapoviruses, kobuviruses, and astroviruses in asymptomatic pigs: An emerging new sapovirus GIII genotype. Arch. Virol. 2013, 158, 549–558. [Google Scholar] [CrossRef] [PubMed]
- Machnowska, P.; Ellerbroek, L.; Johne, R. Detection and characterization of potentially zoonotic viruses in faeces of pigs at slaughter in Germany. Vet. Microbiol. 2014, 168, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Martella, V.; Lorusso, E.; Banyai, K.; Decaro, N.; Corrente, M.; Elia, G.; Cavalli, A.; Radogna, A.; Costantini, V.; Saif, L. Identification of a porcine calicivirus related genetically to human sapoviruses. J. Clin. Microbiol. 2008, 46, 1907–1913. [Google Scholar] [CrossRef] [PubMed]
- De Benedictis, P.; Schultz-Cherry, S.; Burnham, A.; Cattoli, G. Astrovirus infections in humans and animals–molecular biology, genetic diversity, and interspecies transmissions. Infect. Genet. Evol. 2011, 11, 1529–1544. [Google Scholar] [CrossRef] [PubMed]
- Wohlgemuth, N.; Honce, R.; Schultz-Cherry, S. Astrovirus evolution and emergence. Infect. Genet. Evol. 2019, 69, 30–37. [Google Scholar] [CrossRef]
- King, A.M.; Adams, M.J.; Carstens, E.B.; Lefkowitz, E.J. Virus taxonomy. In Ninth Report of the International Committee on Taxonomy of Viruses; International Union of Microbiological Societies: Paris, France, 2012; Volume 9. [Google Scholar]
- Luo, M.; Vriend, G.; Kamer, G.; Minor, I.; Arnold, E.; Rossmann, M.G.; Boege, U.; Scraba, D.G.; Duke, G.M.; Palmenberg, A.C. The atomic structure of Mengo virus at 3.0 A resolution. Science 1987, 235, 182–191. [Google Scholar] [CrossRef]
- Carocci, M.; Bakkali-Kassimi, L. The encephalomyocarditis virus. Virulence 2012, 3, 351–367. [Google Scholar] [CrossRef]
- Brewer, L.A.; Lwamba, H.C.; Murtaugh, M.P.; Palmenberg, A.C.; Brown, C.; Njenga, M.K. Porcine encephalomyocarditis virus persists in pig myocardium and infects human myocardial cells. J. Virol. 2001, 75, 11621–11629. [Google Scholar] [CrossRef]
- Acland, H.M.; Littlejohns, I. Encephalomyocarditis virus infection of pigs. An outbreak in New South Wales. Aust. Vet. J. 1975, 51, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Oberste, M.S.; Gotuzzo, E.; Blair, P.; Nix, W.A.; Ksiazek, T.G.; Comer, J.A.; Rollin, P.; Goldsmith, C.S.; Olson, J.; Kochel, T.J. Human febrile illness caused by encephalomyocarditis virus infection, Peru. Emerg. Infect. Dis. 2009, 15, 640. [Google Scholar] [CrossRef] [PubMed]
- Jackova, A.; Sliz, I.; Mandelik, R.; Salamunova, S.; Novotny, J.; Kolesarova, M.; Vlasakova, M.; Vilcek, S. Porcine kobuvirus 1 in healthy and diarrheic pigs: Genetic detection and characterization of virus and co-infection with rotavirus A. Infect. Genet. Evol. 2017, 49, 73–77. [Google Scholar] [CrossRef]
- Di Bartolo, I.; Angeloni, G.; Tofani, S.; Monini, M.; Ruggeri, F.M. Infection of farmed pigs with porcine kobuviruses in Italy. Arch. Virol. 2015, 160, 1533–1536. [Google Scholar] [CrossRef] [PubMed]
- Khamrin, P.; Maneekarn, N.; Hidaka, S.; Kishikawa, S.; Ushijima, K.; Okitsu, S.; Ushijima, H. Molecular detection of kobuvirus sequences in stool samples collected from healthy pigs in Japan. Infect. Genet. Evol. 2010, 10, 950–954. [Google Scholar] [CrossRef] [PubMed]
- Okitsu, S.; Khamrin, P.; Thongprachum, A.; Hidaka, S.; Kongkaew, S.; Kongkaew, A.; Maneekarn, N.; Mizuguchi, M.; Hayakawa, S.; Ushijima, H. Sequence analysis of porcine kobuvirus VP1 region detected in pigs in Japan and Thailand. Virus Genes 2012, 44, 253–257. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Marthaler, D.; Fredrickson, R.; Gauger, P.C.; Zhang, J.; Burrough, E.R.; Petznick, T.; Li, G. Genetically divergent porcine sapovirus identified in pigs, United States. Transbound. Emerg. Dis. 2019, 67, 18–28. [Google Scholar] [CrossRef] [PubMed]
- Reuter, G.; Zimšek-Mijovski, J.; Poljšak-Prijatelj, M.; Di Bartolo, I.; Ruggeri, F.M.; Kantala, T.; Maunula, L.; Kiss, I.; Kecskeméti, S.; Halaihel, N. Incidence, diversity, and molecular epidemiology of sapoviruses in swine across Europe. J. Clin. Microbiol. 2010, 48, 363–368. [Google Scholar] [CrossRef]
- Bank-Wolf, B.R.; König, M.; Thiel, H.-J. Zoonotic aspects of infections with noroviruses and sapoviruses. Vet. Microbiol. 2010, 140, 204–212. [Google Scholar] [CrossRef]
- Reuter, G.; Pankovics, P.; Boros, A. Identification of a novel astrovirus in a domestic pig in Hungary. Arch. Virol. 2011, 156, 125–128. [Google Scholar] [CrossRef]
- Koenen, F.; Vanderhallen, H.; Papadopoulos, O.; Billinis, C.; Paschaleri-Papadopoulou, E.; Brocchi, E.; De Simone, F.; Carra, E.; Knowles, N. Comparison of the pathogenic, antigenic and molecular characteristics of two encephalomyocarditis virus (EMCV) isolates from Belgium and Greece. Res. Vet. Sci. 1997, 62, 239–244. [Google Scholar] [CrossRef]
- Zhou, Y.; Chen, L.; Zhu, L.; Xu, Z. Molecular detection of porcine torovirus in piglets with diarrhea in southwest China. Sci. World J. 2013, 2013, 984282. [Google Scholar] [CrossRef]
- Kim, H.; Cho, H.; Cho, K.; Park, N. Detection and molecular characterization of porcine enteric calicivirus in Korea, genetically related to sapoviruses. J. Vet. Med. Ser. B 2006, 53, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Ulloa, J.C.; Olarte-Aponte, A.M.; Ospina, J.C.; Rincon, M.A. Experimental infection of conventional newly-weaned piglets with porcine astrovirus. Acta Virol. 2019, 63, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Matias Ferreyra, F.S.; Bradner, L.K.; Burrough, E.R.; Cooper, V.L.; Derscheid, R.J.; Gauger, P.C.; Harmon, K.M.; Madson, D.; Pineyro, P.E.; Schwartz, K.J.; et al. Polioencephalomyelitis in Domestic Swine Associated With Porcine Astrovirus Type. Vet. Pathol. 2020, 57, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Boros, A.; Albert, M.; Pankovics, P.; Biro, H.; Pesavento, P.A.; Phan, T.G.; Delwart, E.; Reuter, G. Outbreaks of Neuroinvasive Astrovirus Associated with Encephalomyelitis, Weakness, and Paralysis among Weaned Pigs, Hungary. Emerg. Infect. Dis. 2017, 23, 1982–1993. [Google Scholar] [CrossRef]
- Ulloa, J.C.; Gutiérrez, M.F. Genomic analysis of two ORF2 segments of new porcine astrovirus isolates and their close relationship with human astroviruses. Can. J. Microbiol. 2010, 56, 569–577. [Google Scholar] [CrossRef]
- Xiao, C.-T.; Giménez-Lirola, L.G.; Gerber, P.F.; Jiang, Y.-H.; Halbur, P.G.; Opriessnig, T. Identification and characterization of novel porcine astroviruses (PAstVs) with high prevalence and frequent co-infection of individual pigs with multiple PAstV types. J. Gen. Virol. 2013, 94, 570–582. [Google Scholar] [CrossRef]
- Opriessnig, T.; Xiao, C.T.; Halbur, P.G. Porcine Astrovirus Type 5-Associated Enteritis in Pigs. J. Comp. Pathol. 2020, 181, 38–46. [Google Scholar] [CrossRef]
- Su, M.; Qi, S.; Yang, D.; Guo, D.; Yin, B.; Sun, D. Coinfection and Genetic Characterization of Porcine Astrovirus in Diarrheic Piglets in China From 2015 to 2018. Front. Vet. Sci. 2020, 7, 462. [Google Scholar] [CrossRef]
- Salamunova, S.; Jackova, A.; Mandelik, R.; Novotny, J.; Vlasakova, M.; Vilcek, S. Molecular detection of enteric viruses and the genetic characterization of porcine astroviruses and sapoviruses in domestic pigs from Slovakian farms. BMC Vet. Res. 2018, 14, 313. [Google Scholar] [CrossRef] [PubMed]
- Qin, Y.; Fang, Q.; Li, X.; Li, F.; Liu, H.; Wei, Z.; Ouyang, K.; Chen, Y.; Huang, W. Molecular epidemiology and viremia of porcine astrovirus in pigs from Guangxi province of China. BMC Vet. Res. 2019, 15, 471. [Google Scholar] [CrossRef] [PubMed]
- Xiao, C.-T.; Luo, Z.; Lv, S.-L.; Opriessnig, T.; Li, R.-C.; Yu, X.-L. Identification and characterization of multiple porcine astrovirus genotypes in Hunan province, China. Arch. Virol. 2017, 162, 943–952. [Google Scholar] [CrossRef] [PubMed]
- Cai, Y.; Yin, W.; Zhou, Y.; Li, B.; Ai, L.; Pan, M.; Guo, W. Molecular detection of Porcine astrovirus in Sichuan Province, China. Virol. J. 2016, 13, 6. [Google Scholar] [CrossRef]
- Chen, X.U.; He, Y.; Li, W.; Kalim, U.; Xiao, Y.; Yang, J.; Wang, X.; Yang, S.; Zhang, W. Identification and Characterization of a Novel Recombinant Porcine Astrovirus from Pigs in Anhui, China. Pol. J. Microbiol. 2020, 69, 471–478. [Google Scholar] [CrossRef]
- Lee, M.-H.; Jeoung, H.-Y.; Park, H.-R.; Lim, J.-A.; Song, J.-Y.; An, D.-J. Phylogenetic analysis of porcine astrovirus in domestic pigs and wild boars in South Korea. Virus Genes 2013, 46, 175–181. [Google Scholar] [CrossRef]
- Luo, Z.; Roi, S.; Dastor, M.; Gallice, E.; Laurin, M.-A.; L’Homme, Y. Multiple novel and prevalent astroviruses in pigs. Vet. Microbiol. 2011, 149, 316–323. [Google Scholar] [CrossRef]
- Brnić, D.; Jemeršić, L.; Keros, T.; Prpić, J. High prevalence and genetic heterogeneity of porcine astroviruses in domestic pigs. Vet. J. 2014, 202, 390–392. [Google Scholar] [CrossRef]
- Kattoor, J.J.; Malik, Y.S.; Saurabh, S.; Sircar, S.; Vinodhkumar, O.R.; Bora, D.P.; Dhama, K.; Ghosh, S.; Banyai, K.; Touil, N.; et al. First report and genetic characterization of porcine astroviruses of lineage 4 and 2 in diarrhoeic pigs in India. Transbound. Emerg. Dis. 2019, 66, 47–53. [Google Scholar] [CrossRef]
- Rawal, G.; Ferreyra, F.M.; Macedo, N.R.; Bradner, L.K.; Harmon, K.M.; Allison, G.; Linhares, D.C.L.; Arruda, B.L. Ecology of Porcine Astrovirus Type 3 in a Herd with Associated Neurologic Disease. Viruses 2020, 12, 992. [Google Scholar] [CrossRef]
- Zhao, C.; Chen, C.; Li, Y.; Dong, S.; Tan, K.; Tian, Y.; Zhang, L.; Huang, J.; Zhang, L. Genomic characterization of a novel recombinant porcine astrovirus isolated in northeastern China. Arch. Virol. 2019, 164, 1469–1473. [Google Scholar] [CrossRef] [PubMed]
- Dick, G.; Smithburn, K.; Haddow, A. Mengo encephalomyelitis virus. isolation and immunological properties. Br. J. Exp. Pathol. 1948, 29, 547. [Google Scholar]
- Jungeblut, C.W.; Dalldorf, G. Epidemiological and experimental observations on the possible significance of rodents in a suburban epidemic of poliomyelitis. Am. J. Public Health Nations Health 1943, 33, 169–172. [Google Scholar] [CrossRef] [PubMed]
- Kirkland, P.; Gleeson, A.; Hawkes, R.; Nairn, H.; Boughton, C. Human infection with encephalomyocarditis virus in New South Wales. Med. J. Aust. 1989, 151, 176–178. [Google Scholar] [CrossRef]
- Deutz, A.; Fuchs, K.; Nowotny, N.; Auer, H.; Schuller, W.; Stünzner, D.; Aspöck, H.; Kerbl, U.; Köfer, J. Sero-epidemiological studies of zoonotic infections in hunters--comparative analysis with veterinarians, farmers, and abattoir workers. Wien. Klin. Wochenschr. 2003, 115, 61–67. [Google Scholar]
- Juncker-Voss, M.; Prosl, H.; Lussy, H.; Enzenberg, U.; Auer, H.; Lassnig, H.; Müller, M.; Nowotny, N. Screening for antibodies against zoonotic agents among employees of the Zoological Garden of Vienna, Schönbrunn, Austria. Berl. Munch. Tierarztl. Wochenschr. 2004, 117, 404–409. [Google Scholar]
- Gwathmey, J.K.; Nakao, S.; Come, P.C.; Goad, M.E.; Serur, J.R.; Als, A.V.; Abelmann, W.H. An experimental model of acute and subacute viral myocarditis in the pig. J. Am. Coll. Cardiol. 1992, 19, 864–869. [Google Scholar] [CrossRef]
- Billinis, C.; Leontides, L.; Psychas, V.; Spyrou, V.; Kostoulas, P.; Koenen, F.; Papadopoulos, O. Effect of challenge dose and age in experimental infection of pigs with encephalomyocarditis virus. Vet. Microbiol. 2004, 99, 187–195. [Google Scholar] [CrossRef]
- Yuan, W.; Wang, J.; Sun, M.; Zheng, Y.; Li, L.; Zhang, X.; Sun, J. Rapid detection of encephalomyocarditis virus by one-step reverse transcription loop-mediated isothermal amplification method. Virus Res. 2014, 189, 75–78. [Google Scholar] [CrossRef]
- Yuan, W.; Song, Q.; Zhang, X.; Zhang, L.; Sun, J. Isolation and molecular analysis of porcine encephalomyocarditis virus strain BD2 from northern China. Infect. Genet. Evol. 2014, 21, 303–307. [Google Scholar] [CrossRef]
- Lin, W.; Liu, Y.; Cui, S.; Liu, H. Isolation, molecular characterization, and phylogenetic analysis of porcine encephalomyocarditis virus strain HB10 in China. Infect. Genet. Evol. 2012, 12, 1324–1327. [Google Scholar] [CrossRef] [PubMed]
- Feng, R.; Zhang, H.; Wei, J.; Li, X.; Xie, J.; Li, M.; Qiao, Z.; Feng, Y.; Ma, Z. Isolation, molecular and phylogenetic analysis of encephalomyocarditis virus strain GS01 in China. Infect. Genet. Evol. 2015, 30, 19–26. [Google Scholar] [CrossRef] [PubMed]
- LaRue, R.; Myers, S.; Brewer, L.; Shaw, D.P.; Brown, C.; Seal, B.S.; Njenga, M.K. A wild-type porcine encephalomyocarditis virus containing a short poly(C) tract is pathogenic to mice, pigs, and cynomolgus macaques. J. Virol. 2003, 77, 9136–9146. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Liu, H.; Li, Y.; Zhang, G.; Sang, S.; Wang, C.; Chang, H. Complete genome sequences and phylogenetic analysis of encephalomyocarditis virus strains isolated from pigs and rats origin. Infect. Genet. Evol. 2017, 55, 277–280. [Google Scholar] [CrossRef]
- Zhang, G.Q.; Ge, X.N.; Guo, X.; Yang, H.C. Genomic analysis of two porcine encephalomyocarditis virus strains isolated in China. Arch. Virol. 2007, 152, 1209–1213. [Google Scholar] [CrossRef]
- Canelli, E.; Luppi, A.; Lavazza, A.; Lelli, D.; Sozzi, E.; Martin, A.M.M.; Gelmetti, D.; Pascotto, E.; Sandri, C.; Magnone, W. Encephalomyocarditis virus infection in an Italian zoo. Virol. J. 2010, 7, 64. [Google Scholar] [CrossRef]
- Reddacliff, L.A.; Kirkland, P.D.; Hartley, W.J.; Reece, R.L. Encephalomyocarditis virus infections in an Australian zoo. J. Zoo Wildl. Med. 1997, 28, 153–157. [Google Scholar]
- Wells, S.K.; Gutter, A.E.; Soike, K.F.; Baskin, G.B. Encephalomyocarditis virus: Epizootic in a zoological collection. J. Zoo Wildl. Med. 1989, 20, 291–296. [Google Scholar]
- Knowles, N.; Dickinson, N.; Wilsden, G.; Carra, E.; Brocchi, E.; De Simone, F. Molecular analysis of encephalomyocarditis viruses isolated from pigs and rodents in Italy. Virus Res. 1998, 57, 53–62. [Google Scholar] [CrossRef]
- Seaman, J.; Boulton, J.; Carrigan, M. Encephalomyocarditis virus disease of pigs associated with a plague of rodents. Aust. Vet. J. 1986, 63, 292–294. [Google Scholar] [CrossRef]
- Otomaru, K.; Naoi, Y.; Haga, K.; Omatsu, T.; Uto, T.; Koizumi, M.; Masuda, T.; Yamasato, H.; Takai, H.; Aoki, H. Detection of novel kobu-like viruses in Japanese black cattle in Japan. J. Vet. Med. Sci. 2016, 78, 321–324. [Google Scholar] [CrossRef] [PubMed]
- Reuter, G.; Kecskeméti, S.; Pankovics, P. Evolution of porcine kobuvirus infection, Hungary. Emerg. Infect. Dis. 2010, 16, 696. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Kim, H.K.; Moon, H.J.; Song, D.S.; Rho, S.M.; Han, J.Y.; Nguyen, V.G.; Park, B.K. Molecular detection of porcine kobuviruses in pigs in Korea and their association with diarrhea. Arch. Virol. 2010, 155, 1803–1811. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.P.; Yang, Z.; Lin, W.D.; Wang, W.Y.; Yang, J.; Jin, W.J.; Qin, A.J. The rate of co-infection for piglet diarrhea viruses in China and the genetic characterization of porcine epidemic diarrhea virus and porcine kobuvirus. Acta Virol. 2016, 60, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Van Dung, N.; Anh, P.H.; Van Cuong, N.; Hoa, N.T.; Carrique-Mas, J.; Hien, V.B.; Sharp, C.; Rabaa, M.; Berto, A.; Campbell, J.; et al. Large-scale screening and characterization of enteroviruses and kobuviruses infecting pigs in Vietnam. J. Gen. Virol. 2016, 97, 378–388. [Google Scholar] [CrossRef] [PubMed]
- Di Profio, F.; Ceci, C.; Di Felice, E.; Marsilio, F.; Di Martino, B. Molecular detection of porcine kobuviruses in Italian swine. Res. Vet. Sci. 2013, 95, 782–785. [Google Scholar] [CrossRef]
- Amimo, J.O.; Okoth, E.; Junga, J.O.; Ogara, W.O.; Njahira, M.N.; Wang, Q.; Vlasova, A.N.; Saif, L.J.; Djikeng, A. Molecular detection and genetic characterization of kobuviruses and astroviruses in asymptomatic local pigs in East Africa. Arch. Virol. 2014, 159, 1313–1319. [Google Scholar] [CrossRef]
- Costantini, V.; Loisy, F.; Joens, L.; Le Guyader, F.S.; Saif, L.J. Human and animal enteric caliciviruses in oysters from different coastal regions of the United States. Appl. Environ. Microbiol. 2006, 72, 1800–1809. [Google Scholar] [CrossRef]
- Wang, Q.-H.; Han, M.G.; Funk, J.A.; Bowman, G.; Janies, D.A.; Saif, L.J. Genetic diversity and recombination of porcine sapoviruses. J. Clin. Microbiol. 2005, 43, 5963–5972. [Google Scholar] [CrossRef]
- Liu, G.H.; Li, R.C.; Huang, Z.B.; Yang, J.; Xiao, C.T.; Li, J.; Li, M.X.; Yan, Y.Q.; Yu, X.L. RT-PCR test for detecting porcine sapovirus in weanling piglets in Hunan Province, China. Trop. Anim. Health Prod. 2012, 44, 1335–1339. [Google Scholar] [CrossRef]
- Jiang, C.; He, H.; Zhang, C.; Zhang, X.; Han, J.; Zhang, H.; Luo, Y.; Wu, Y.; Wang, Y.; Ge, B.; et al. One-step triplex reverse-transcription PCR detection of porcine epidemic diarrhea virus, porcine sapelovirus, and porcine sapovirus. J. Vet. Diagn. Investig. 2019, 31, 909–912. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.J.; Yu, J.N.; Nam, H.M.; Bak, H.R.; Lee, J.B.; Park, S.Y.; Song, C.S.; Seo, K.H.; Choi, I.S. Identification of genetic diversity of porcine Norovirus and Sapovirus in Korea. Virus Genes 2011, 42, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Valente, C.S.; Alfieri, A.F.; Barry, A.F.; Leme, R.A.; Lorenzetti, E.; Alfieri, A.A. Age distribution of porcine sapovirus asymptomatic infection and molecular evidence of genogroups GIII and GIX? circulation in distinct Brazilian pig production systems. Trop. Anim. Health Prod. 2016, 48, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.H.; Souza, M.; Funk, J.A.; Zhang, W.; Saif, L.J. Prevalence of noroviruses and sapoviruses in swine of various ages determined by reverse transcription-PCR and microwell hybridization assays. J. Clin. Microbiol. 2006, 44, 2057–2062. [Google Scholar] [CrossRef] [PubMed]
- Jun, Q.; Lulu, T.; Qingling, M.; Xingxing, Z.; Haiting, L.; Shasha, G.; Zibing, C.; Xuepeng, C.; Jinsheng, Z.; Zaichao, Z.; et al. Serological and molecular investigation of porcine sapovirus infection in piglets in Xinjiang, China. Trop. Anim. Health Prod. 2016, 48, 863–869. [Google Scholar] [CrossRef]
- Liu, W.; Yang, B.; Wang, E.; Liu, J.; Lan, X. Complete sequence and phylogenetic analysis of a porcine sapovirus strain isolated from western China. Virus Genes 2014, 49, 100–105. [Google Scholar] [CrossRef]
- Sunaga, F.; Masuda, T.; Aoki, H.; Ito, M.; Sano, K.; Naoi, Y.; Katayama, Y.; Omatsu, T.; Oba, M.; Furuya, T.; et al. Complete genome sequencing and genetic characterization of porcine sapovirus genogroup (G) X and GXI: GVI, GVII, GX, and GXI sapoviruses share common genomic features and form a unique porcine SaV clade. Infect. Genet. Evol. 2019, 75, 103959. [Google Scholar] [CrossRef]
- Salmon, H.; Berri, M.; Gerdts, V.; Meurens, F. Humoral and cellular factors of maternal immunity in swine. Dev. Comp. Immunol. 2009, 33, 384–393. [Google Scholar] [CrossRef]
- Patiño-Galindo, J.Á.; Filip, I.; Rabadan, R. Global patterns of recombination across human viruses. Mol. Biol. Evol. 2021, 38, 2520–2531. [Google Scholar] [CrossRef]
- Kumar, S.; Stecher, G.; Tamura, K. MEGA7: Molecular evolutionary genetics analysis version 7.0 for bigger datasets. Mol. Biol. Evol. 2016, 33, 1870–1874. [Google Scholar] [CrossRef]
| Variable | Number of Pigs (n) | % (Positive/n) | Coinfection Rate | |||
|---|---|---|---|---|---|---|
| PAstV | EMCV | PKV | PSaV | |||
| Conventional farms | 173 | 56.1 (97/173) | 19.1 (33/173) | 72.8 (126/173) | 29.5 (51/173) | 83.2 (124/149) |
| SPF Farms | 310 | 23.9 (74/310) | 2.9 (9/310) | 39 (121/310) | 12 (38/310) | 53.0 (80/151) |
| Piglet | 158 | 32.9 (52/158) | 9.5 (15/158) | 71.5 (113/158) | 24.1 (38/158) | 61.7 (71/115) |
| Weaner | 161 | 45.3 (73/161) | 10.6 (17/161) | 38.5 (62/161) | 25.5 (41/161) | 84.8 (84/99) |
| Fattening pig | 114 | 31.6 (36/114) | 7.9 (9/114) | 45.6 (52/114) | 7 (8/114) | 59.7 (37/62) |
| Sow | 50 | 20 (10/50) | 2 (1/50) | 40 (20/50) | 4 (2/50) | 50.0 (12/24) |
| Overall prevalence | 35 (171/483) | 8.7 (42/483) | 51 (247/483) | 18 (89/483) | 68.0 (204/300) | |
| Virus | Primer Name | Primer Sequence (5′ → 3′) | Target Gene | Amplicon Size | Ref. |
|---|---|---|---|---|---|
| PAstV | PAstV-F | TGACATTTTGTGGATTTACAGTT | ORF1b/ORF2 | 799 | [21] |
| PAstV-R | CACCCAGGGCTGACCA | ||||
| EMCV | ECMV F | GGTGAGAGCAAGCCTCGCAAAGACAG | 3D polymerase gene | 286 | [22] |
| ECMV R | CCCTACCTCACGGAATGG GGCAAAG | ||||
| PKV | PKoV F | TGGATTACAAGTGTTTTGATGC | 3D Polyprotein gene | 351 | [23] |
| PKoV R | TGTCGTAGAACTCCTTGATGAA | ||||
| PSaV | PSaV F | CTCATCAACCCTTTTGAAAC | Capsid protein | 757 | [24] |
| PSaV R | AAAGCATGATGTTGTTAGGC |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Werid, G.M.; Ibrahim, Y.M.; Chen, H.; Fu, L.; Wang, Y. Molecular Detection and Genetic Characterization of Potential Zoonotic Swine Enteric Viruses in Northern China. Pathogens 2022, 11, 417. https://doi.org/10.3390/pathogens11040417
Werid GM, Ibrahim YM, Chen H, Fu L, Wang Y. Molecular Detection and Genetic Characterization of Potential Zoonotic Swine Enteric Viruses in Northern China. Pathogens. 2022; 11(4):417. https://doi.org/10.3390/pathogens11040417
Chicago/Turabian StyleWerid, Gebremeskel Mamu, Yassein M. Ibrahim, Hongyan Chen, Lizhi Fu, and Yue Wang. 2022. "Molecular Detection and Genetic Characterization of Potential Zoonotic Swine Enteric Viruses in Northern China" Pathogens 11, no. 4: 417. https://doi.org/10.3390/pathogens11040417
APA StyleWerid, G. M., Ibrahim, Y. M., Chen, H., Fu, L., & Wang, Y. (2022). Molecular Detection and Genetic Characterization of Potential Zoonotic Swine Enteric Viruses in Northern China. Pathogens, 11(4), 417. https://doi.org/10.3390/pathogens11040417








