Modern Development and Production of a New Live Attenuated Bacterial Vaccine, SCHU S4 ΔclpB, to Prevent Tularemia
Abstract
1. Introduction
2. Results
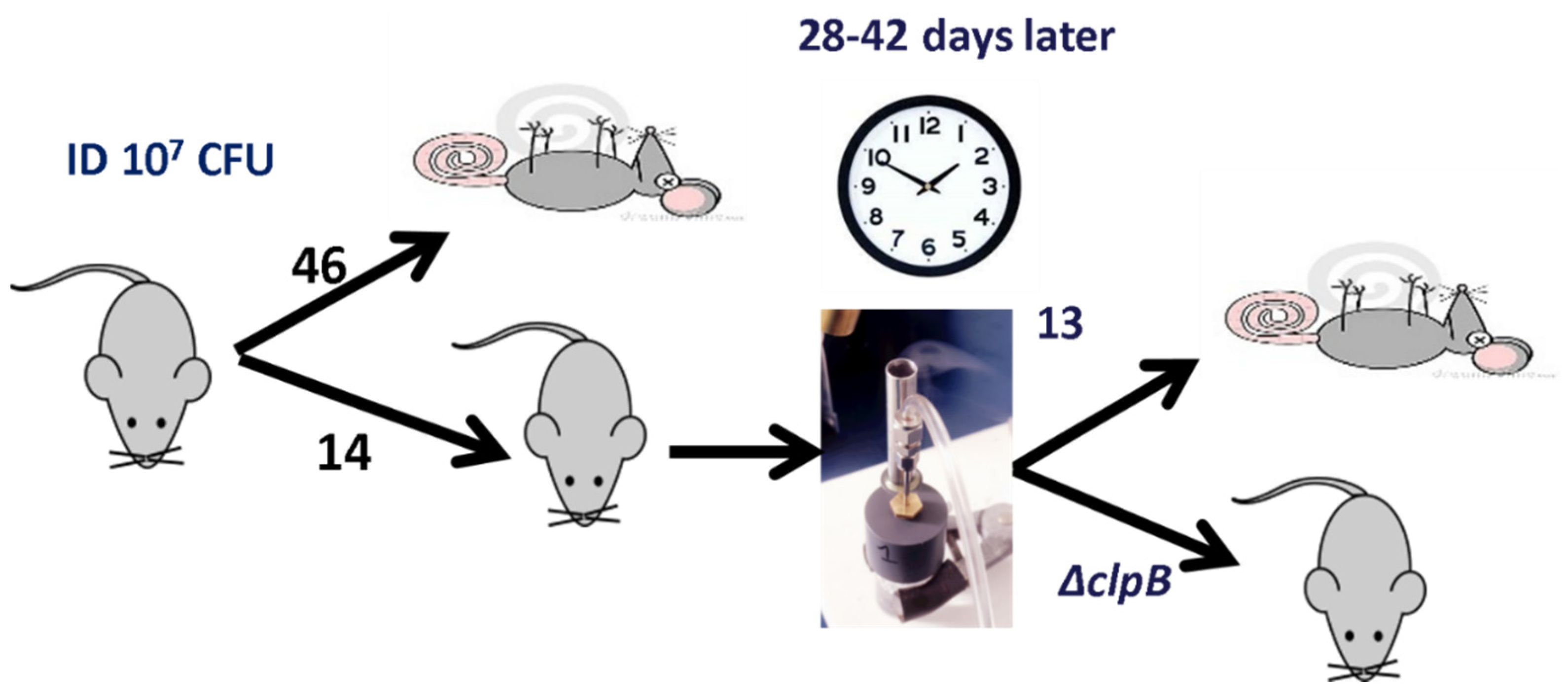
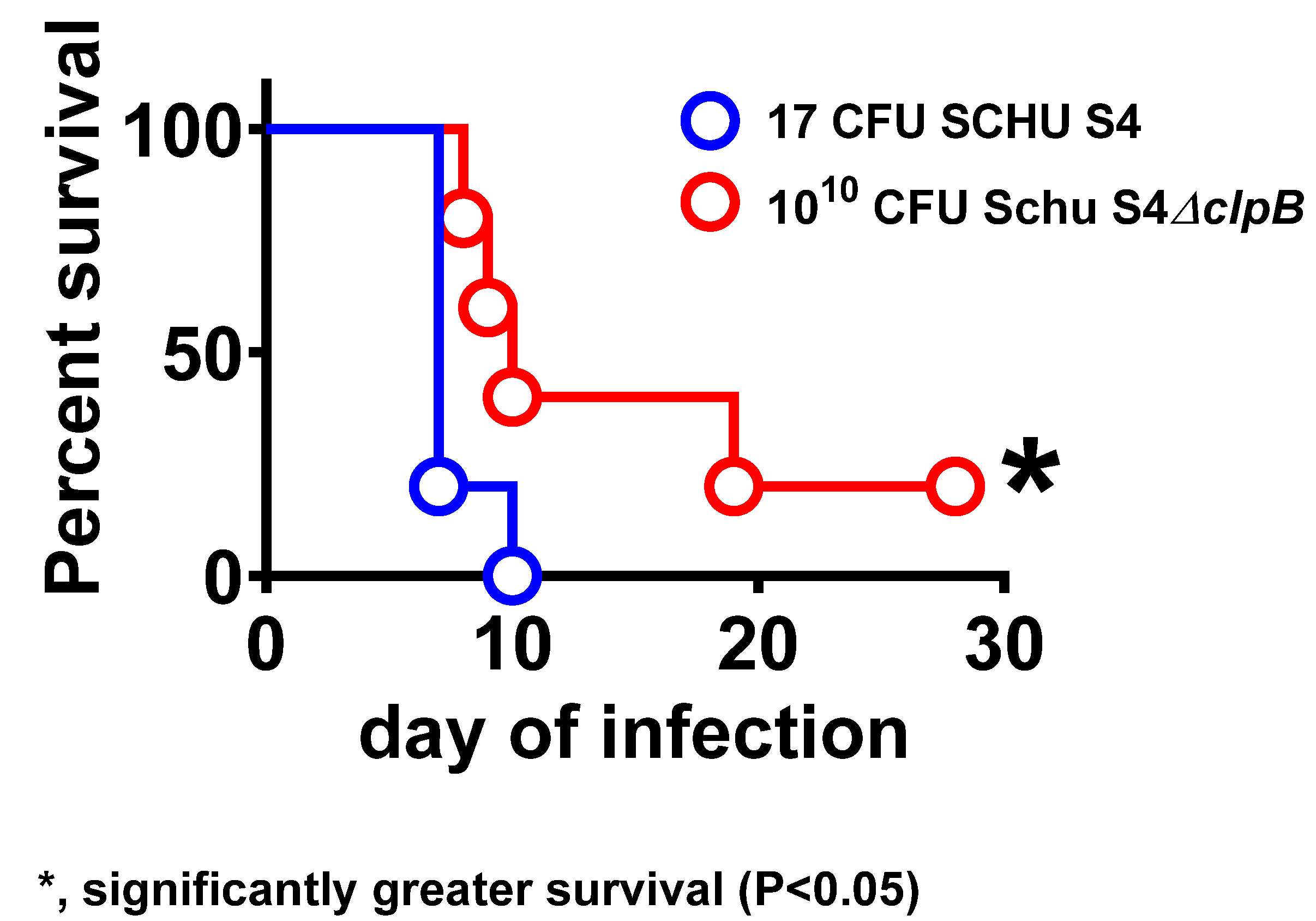
2.1. Studies Supporting Attenuation and Removal of SCHU S4 ΔclpB from the U.S. Select Agent List
2.2. Clearance of ΔclpB from Fischer Rat Tissues
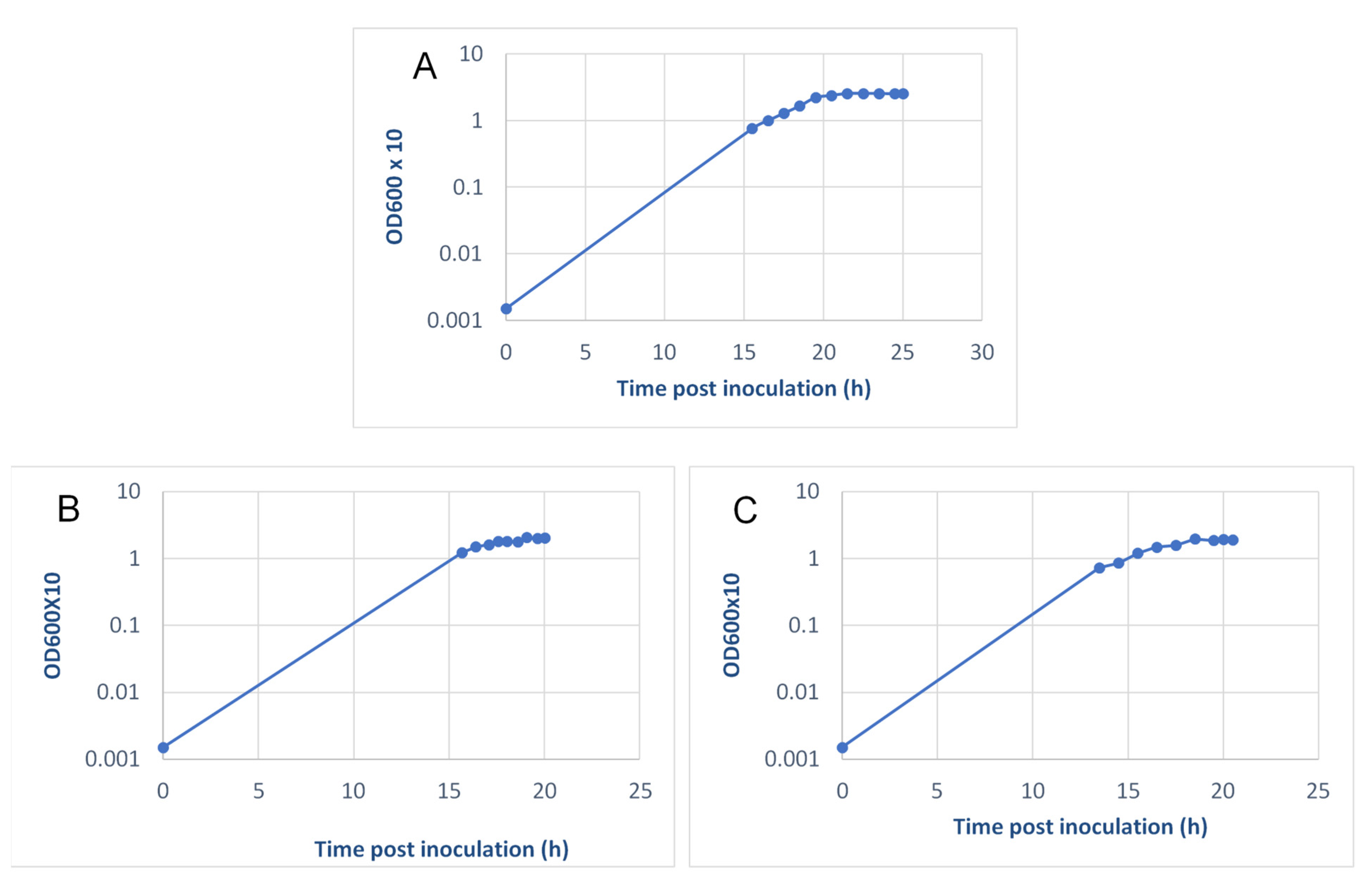
2.3. ΔclpB Vaccine Production Optimization, Scale-Up, and Quality Control Testing
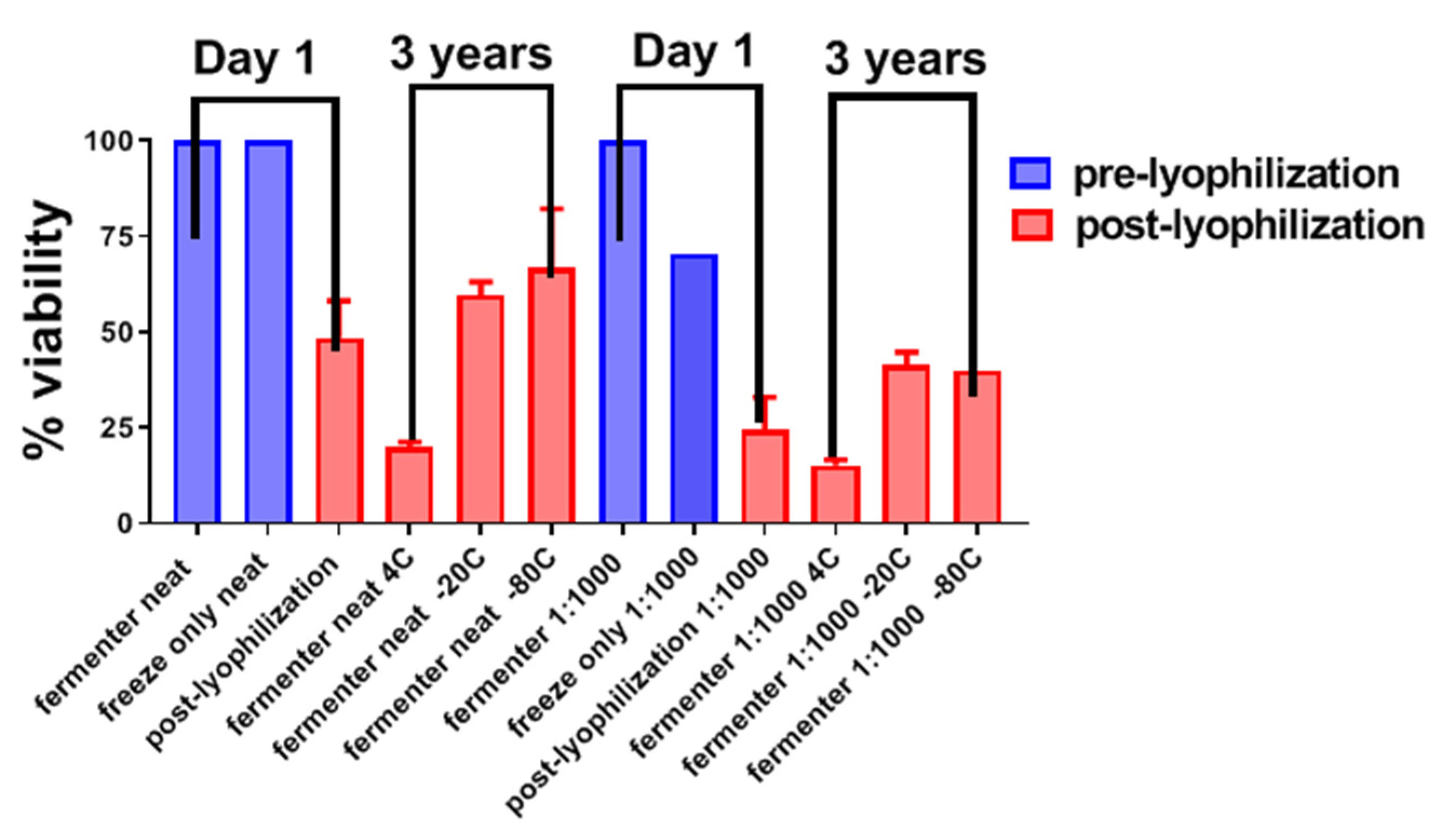
2.4. Long-Term Storage of ΔclpB
2.5. Quality Control and Lot Release Assays for Clinical Lots of ΔclpB
3. Discussion
4. Materials and Methods
4.1. Generation of ΔclpB and Evaluation of Its Potential for Reversion to Wild Type
4.2. Fermenter Growth of ΔclpB at NRC-C
4.3. Manufacturing of ΔclpB at the 25 L Scale at Ology Bioservices
4.4. Lyophilization of ΔclpB Drug Product
4.5. Analytical Assays
4.6. Biological Assays
5. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sjostedt, A. Tularemia: History, epidemiology, pathogen physiology, and clinical manifestations. Ann. N. Y. Acad. Sci. 2007, 1105, 1–29. [Google Scholar] [CrossRef]
- Oyston, P.C.; Sjostedt, A.; Titball, R.W. Tularaemia: Bioterrorism defence renews interest in Francisella tularensis. Nat. Rev. Microbiol. 2004, 2, 967–978. [Google Scholar] [CrossRef] [PubMed]
- Desvars, A.; Furberg, M.; Hjertqvist, M.; Vidman, L.; Sjostedt, A.; Ryden, P.; Johansson, A. Epidemiology and ecology of tularemia in Sweden, 1984–2012. Emerg. Infect. Dis. 2015, 21, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Hestvik, G.; Warns-Petit, E.; Smith, L.A.; Fox, N.J.; Uhlhorn, H.; Artois, M.; Hannant, D.; Hutchings, M.R.; Mattsson, R.; Yon, L.; et al. The status of tularemia in Europe in a one-health context: A review. Epidemiol. Infect. 2015, 143, 2137–2160. [Google Scholar] [CrossRef] [PubMed]
- Oyston, P.C. Francisella tularensis vaccines. Vaccine 2009, 27, D48–D51. [Google Scholar] [CrossRef] [PubMed]
- Kortepeter, M.G.; Parker, G.W. Potential biological weapons threats. Emerg. Infect. Dis. 1999, 5, 523–527. [Google Scholar] [CrossRef]
- Frischknecht, F. The history of biological warfare. Human experimentation, modern nightmares and lone madmen in the twentieth century. EMBO Rep. 2003, 4, S47–S52. [Google Scholar] [CrossRef] [PubMed]
- Griffin, K.F.; Oyston, P.C.; Titball, R.W. Francisella tularensis vaccines. FEMS Immunol. Med. Microbiol. 2007, 49, 315–323. [Google Scholar] [CrossRef]
- Eigelsbach, H.T.; Downs, C.M. Prophylactic effectiveness of live and killed tularemia vaccines. I. Production of vaccine and evaluation in the white mouse and guinea pig. J. Immunol. 1961, 87, 415–425. [Google Scholar]
- Tigertt, W.D. Soviet viable Pasteurella tularensis vaccines. A review of selected articles. Bacteriol. Rev. 1962, 26, 354–373. [Google Scholar] [CrossRef]
- Eigelsbach, H.T.; Tulis, J.J.; McGavran, M.H.; White, J.D. LIVE TULAREMIA VACCINE I: Host-Parasite Relationship in Monkeys Vaccinated Intracutaneously or Aerogenically. J. Bacteriol. 1962, 84, 1020–1027. [Google Scholar] [CrossRef] [PubMed]
- Saslaw, S.; Eigelsbach, H.T.; Prior, J.A.; Wilson, H.E.; Carhart, S. Tularemia vaccine study. II. Respiratory challenge. Arch. Intern. Med. 1961, 107, 702–714. [Google Scholar] [CrossRef] [PubMed]
- Saslaw, S.; Eigelsbach, H.T.; Wilson, H.E.; Prior, J.A.; Carhart, S. Tularemia vaccine study. I. Intracutaneous challenge. Arch. Intern. Med. 1961, 107, 689–701. [Google Scholar] [CrossRef] [PubMed]
- Eigelsbach, H.T.; Hornick, R.B.; Tulis, J.J. Recent studies on live tularemia vaccine. Med. Ann. Dist. Columbia 1967, 36, 282–286. [Google Scholar]
- Burke, D.S. Immunization against tularemia: Analysis of the effectiveness of live Francisella tularensis vaccine in prevention of laboratory-acquired tularemia. J. Infect. Dis. 1977, 135, 55–60. [Google Scholar] [CrossRef]
- McCrumb, F.R. Aerosol Infection of Man with Pasteurella tularensis. Bacteriol. Rev. 1961, 25, 262–267. [Google Scholar] [CrossRef]
- Hornick, R.B.; Eigelsbach, H.T. Aerogenic immunization of man with live Tularemia vaccine. Bacteriol. Rev. 1966, 30, 532–538. [Google Scholar] [CrossRef]
- Pasetti, M.F.; Cuberos, L.; Horn, T.L.; Shearer, J.D.; Matthews, S.J.; House, R.V.; Sztein, M.B. An improved Francisella tularensis live vaccine strain (LVS) is well tolerated and highly immunogenic when administered to rabbits in escalating doses using various immunization routes. Vaccine 2008, 26, 1773–1785. [Google Scholar] [CrossRef] [PubMed]
- Larsen, J.C.; Disbrow, G.L. Project BioShield and the Biomedical Advanced Research Development Authority: A ten year progress report on meeting U.S. preparedness objectives for threat agents. Clin. Infect. Dis. 2017, 64, 1430–1434. [Google Scholar] [CrossRef] [PubMed]
- Popescu, S. Infection Prevention and Control: A Biodefense Measure. In Defense Against Biological Attacks: Volume I; Singh, S.K., Kuhn, J.H., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 145–169. [Google Scholar]
- Conlan, J.W. Tularemia vaccines: Recent developments and remaining hurdles. Future Microbiol. 2011, 6, 391–405. [Google Scholar] [CrossRef]
- Marohn, M.E.; Barry, E.M. Live attenuated tularemia vaccines: Recent developments and future goals. Vaccine 2013, 31, 3485–3491. [Google Scholar] [CrossRef]
- Sunagar, R.; Kumar, S.; Franz, B.J.; Gosselin, E.J. Tularemia vaccine development: Paralysis or progress? Vaccine 2016, 6, 9–23. [Google Scholar] [CrossRef] [PubMed]
- Twine, S.; Bystrom, M.; Chen, W.; Forsman, M.; Golovliov, I.; Johansson, A.; Kelly, J.; Lindgren, H.; Svensson, K.; Zingmark, C.; et al. A mutant of Francisella tularensis strain SCHU S4 lacking the ability to express a 58-kilodalton protein is attenuated for virulence and is an effective live vaccine. Infect. Immun. 2005, 73, 8345–8352. [Google Scholar] [CrossRef] [PubMed]
- Golovliov, I.; Twine, S.M.; Shen, H.; Sjostedt, A.; Conlan, W. A ΔclpB Mutant of Francisella tularensis Subspecies holarctica Strain, FSC200, Is a More Effective Live Vaccine than F. tularensis LVS in a Mouse Respiratory Challenge Model of Tularemia. PLoS ONE 2013, 8, e78671. [Google Scholar] [CrossRef]
- Golovliov, I.; Sjostedt, A.; Mokrievich, A.; Pavlov, V. A method for allelic replacement in Francisella tularensis. FEMS Microbiol. Lett. 2003, 222, 273–280. [Google Scholar] [CrossRef]
- Salomonsson, E.; Kuoppa, K.; Forslund, A.L.; Zingmark, C.; Golovliov, I.; Sjostedt, A.; Noppa, L.; Forsberg, A. Reintroduction of two deleted virulence loci restores full virulence to the live vaccine strain of Francisella tularensis. Infect. Immun. 2009, 77, 3424–3431. [Google Scholar] [CrossRef] [PubMed]
- Kadzhaev, K.; Zingmark, C.; Golovliov, I.; Bolanowski, M.; Shen, H.; Conlan, W.; Sjöstedt, A. Identification of genes contributing to the virulence of Francisella tularensis SCHU S4 in a mouse intradermal infection model. PLoS ONE 2009, 4, e5463. [Google Scholar] [CrossRef] [PubMed]
- Ryden, P.; Twine, S.; Shen, H.; Harris, G.; Chen, W.; Sjostedt, A.; Conlan, W. Correlates of protection following vaccination of mice with gene deletion mutants of Francisella tularensis subspecies tularensis strain, SCHU S4 that elicit varying degrees of immunity to systemic and respiratory challenge with wild-type bacteria. Mol. Immunol. 2013, 54, 58–67. [Google Scholar] [CrossRef]
- Honn, M.; Lindgren, H.; Bharath, G.K.; Sjostedt, A. Lack of OxyR and KatG Results in Extreme Susceptibility of Francisella tularensis LVS to Oxidative Stress and Marked Attenuation In Vivo. Front. Cell. Infect. Microbiol. 2017, 7, 14. [Google Scholar] [CrossRef]
- Lindgren, M.; Tancred, L.; Golovliov, I.; Conlan, W.; Twine, S.M.; Sjostedt, A. Identification of Mechanisms for Attenuation of the FSC043 Mutant of Francisella tularensis SCHU S4. Infect. Immun. 2014, 82, 3622–3635. [Google Scholar] [CrossRef] [PubMed]
- Ozanic, M.; Marecic, V.; Lindgren, M.; Sjostedt, A.; Santic, M. Phenotypic characterization of the Francisella tularensis DeltapdpC and DeltaiglG mutants. Microbes Infect. 2016, 18, 768–776. [Google Scholar] [CrossRef]
- Binesse, J.; Lindgren, H.; Lindgren, L.; Conlan, W.; Sjostedt, A. Roles of reactive oxygen species-degrading enzymes of Francisella tularensis SCHU S4. Infect. Immun. 2015, 83, 2255–2263. [Google Scholar] [CrossRef]
- Forslund, A.L.; Salomonsson, E.N.; Golovliov, I.; Kuoppa, K.; Michell, S.; Titball, R.; Oyston, P.; Noppa, L.; Sjöstedt, A.; Forsberg, A. The type IV pilin, PilA, is required for full virulence of Francisella tularensis subspecies tularensis. BMC Microbiol. 2010, 10, 227. [Google Scholar] [CrossRef] [PubMed]
- Lindgren, M.; Eneslatt, K.; Broms, J.E.; Sjostedt, A. Importance of PdpC, IglC, IglI, and IglG for modulation of a host cell death pathway induced by Francisella tularensis LVS. Infect. Immun. 2013, 81, 2076–2084. [Google Scholar] [CrossRef] [PubMed]
- Twine, S.M.; Vinogradov, E.; Lindgren, H.; Sjostedt, A.; Conlan, J.W. Roles for wbtC, wbtI, and kdtA Genes in Lipopolysaccharide Biosynthesis, Protein Glycosylation, Virulence, and Immunogenicity in Francisella tularensis Strain SCHU S4. Pathogens 2012, 1, 12–29. [Google Scholar] [CrossRef]
- Conlan, J.W.; Shen, H.; Golovliov, I.; Zingmark, C.; Oyston, P.C.; Chen, W.; House, R.V.; Sjöstedt, A. Differential ability of novel attenuated targeted deletion mutants of Francisella tularensis subspecies tularensis strain SCHU S4 to protect mice against aerosol challenge with virulent bacteria: Effects of host background and route of immunization. Vaccine 2010, 28, 1824–1831. [Google Scholar] [CrossRef] [PubMed]
- Shen, H.; Harris, G.; Chen, W.; Sjostedt, A.; Ryden, P.; Conlan, W. Molecular immune responses to aerosol challenge with Francisella tularensis in mice inoculated with live vaccine candidates of varying efficacy. PLoS ONE 2010, 5, e13349. [Google Scholar] [CrossRef]
- Allio, T. The FDA Animal Rule and its role in protecting human safety. Expert Opin. Drug Saf. 2018, 17, 971–973. [Google Scholar] [CrossRef]
- Beasley, D.W.C.; Brasel, T.L.; Comer, J.E. First vaccine approval under the FDA Animal Rule. NPJ Vaccines 2016, 1, 16013. [Google Scholar] [CrossRef]
- Jemski, J.V. Respiratory tularemia: Comparison of selected routes of vaccination in Fischer 344 rats. Infect. Immun. 1981, 34, 766–772. [Google Scholar] [CrossRef]
- Wu, T.H.; Zsemlye, J.L.; Statom, G.L.; Hutt, J.A.; Schrader, R.M.; Scrymgeour, A.A.; Lyons, C.R. Vaccination of Fischer 344 rats against pulmonary infections by Francisella tularensis type A strains. Vaccine 2009, 27, 4684–4693. [Google Scholar] [CrossRef] [PubMed]
- Ray, H.J.; Chu, P.; Wu, T.H.; Lyons, C.R.; Murthy, A.K.; Guentzel, M.N.; Klose, K.E.; Arulanandam, B.P. The Fischer 344 rat reflects human susceptibility to francisella pulmonary challenge and provides a new platform for virulence and protection studies. PLoS ONE 2010, 5, e9952. [Google Scholar] [CrossRef]
- Chamberlain, R.E. Evaluation of Live Tularemia Vaccine Prepared in a Chemically Defined Medium. Appl. Microbiol. 1965, 13, 232–235. [Google Scholar] [CrossRef] [PubMed]
- Hutt, J.A.; Lovchik, J.A.; Dekonenko, A.; Hahn, A.C.; Wu, T.H. The Natural History of Pneumonic Tularemia in Female Fischer 344 Rats after Inhalational Exposure to Aerosolized Francisella tularensis Subspecies tularensis Strain SCHU S4. Am. J. Pathol. 2017, 187, 252–267. [Google Scholar] [CrossRef]
- De Pascalis, R.; Hahn, A.; Brook, H.M.; Ryden, P.; Donart, N.; Mittereder, L.; Frey, B.; Wu, T.H.; Elkins, K.L. A panel of correlates predicts, vaccine-induced protection of rats against respiratory challenge with virulent Francisella tularensis. PLoS ONE 2018, 13, e0198140. [Google Scholar] [CrossRef]
- Marshall, L.E.; Nelson, M.; Davies, C.H.; Whelan, A.O.; Jenner, D.C.; Moule, M.G.; Denman, C.; Cuccui, J.; Atkins, T.P.; Wren, B.W.; et al. An O-Antigen Glycoconjugate Vaccine Produced Using Protein Glycan Coupling Technology Is Protective in an Inhalational Rat Model of Tularemia. J. Immunol. Res. 2018, 2018, 8087916. [Google Scholar] [CrossRef] [PubMed]
- Vinogradov, E.; Perry, M.B.; Conlan, J.W. Structural analysis of Francisella tularensis lipopolysaccharide. Eur. J. Biochem. 2002, 269, 6112–6118. [Google Scholar] [CrossRef] [PubMed]
- Mulligan, M.J.; Stapleton, J.T.; Keitel, W.A.; Frey, S.E.; Chen, W.H.; Rouphael, N.; Edupuganti, S.; Beck, A.; Winokur, P.L.; El Sahly, H.M.; et al. Tularemia vaccine: Safety, reactogenicity, "Take" skin reactions, and antibody responses following vaccination with a new lot of the Francisella tularensis live vaccine strain—A phase 2 randomized clinical Trial. Vaccine 2017, 35, 4730–4737. [Google Scholar] [CrossRef]
- Cherwonogrodzky, J.W.; Knodel, M.H.; Spence, M.R. Increased encapsulation and virulence of Francisella tularensis live vaccine strain (LVS) by subculturing on synthetic medium. Vaccine 1994, 12, 773–775. [Google Scholar] [CrossRef]
- Sandstrom, G.; Sjostedt, A.; Johansson, T.; Kuoppa, K.; Williams, J.C. Immunogenicity and toxicity of lipopolysaccharide from Francisella tularensis LVS. FEMS Microbiol. Immunol. 1992, 5, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Eneslatt, K.; Rietz, C.; Ryden, P.; Stoven, S.; House, R.V.; Wolfraim, L.A.; Tärnvik, A.; Sjöstedt, A. Persistence of cell-mediated immunity three decades after vaccination with the live vaccine strain of Francisella tularensis. Eur. J. Immunol. 2011, 41, 974–980. [Google Scholar] [CrossRef]
- Eneslatt, K.; Golovliov, I.; Ryden, P.; Sjostedt, A. Vaccine-Mediated Mechanisms Controlling Replication of Francisella tularensis in Human Peripheral Blood Mononuclear Cells Using a Co-culture System. Front. Cell. Infect. Microbiol. 2018, 8, 27. [Google Scholar] [CrossRef] [PubMed]
- Lindgren, H.; Eneslatt, K.; Golovliov, I.; Gelhaus, C.; Ryden, P.; Wu, T.; Sjöstedt, A. Vaccine-Mediated Mechanisms Controlling Francisella tularensis SCHU S4 Growth in a Rat Co-Culture System. Pathogens 2020, 9, 338. [Google Scholar] [CrossRef]
- Ohtake, S.; Martin, R.A.; Saxena, A.; Lechuga-Ballesteros, D.; Santiago, A.E.; Barry, E.M.; Truong-Le, V. Formulation and stabilization of Francisella tularensis live vaccine strain. J. Pharm. Sci. 2011, 100, 3076–3087. [Google Scholar] [CrossRef][Green Version]
- Staples, J.E.; Kubota, K.A.; Chalcraft, L.G.; Mead, P.S.; Petersen, J.M. Epidemiologic and molecular analysis of human tularemia, United States, 1964–2004. Emerg. Infect. Dis. 2006, 12, 1113–1118. [Google Scholar] [CrossRef] [PubMed]
- Overholt, E.L.; Tigertt, W.D.; Kadull, P.J.; Ward, M.K.; Charkes, N.D.; Rene, R.M.; Salzman, T.E.; Stephens, M. An analysis of forty-two cases of laboratory-acquired tularemia. Treatment with broad spectrum antibiotics. Am. J. Med. 1961, 30, 785–806. [Google Scholar] [CrossRef]
- Matyas, B.T.; Nieder, H.S.; Telford, S.R., III. Pneumonic tularemia on Martha’s Vineyard: Clinical, epidemiologic, and ecological characteristics. Ann. N. Y. Acad. Sci. 2007, 1105, 351–377. [Google Scholar] [CrossRef] [PubMed]
- Feodorova, V.A.; Sayapina, L.V.; Corbel, M.J.; Motin, V.L. Russian vaccines against especially dangerous bacterial pathogens. Emerg. Microbes Infect. 2014, 3, e86. [Google Scholar] [CrossRef]
- Ma, Y.; Vigouroux, G.; Kalantari, Z.; Goldenberg, R.; Destouni, G. Implications of Projected Hydroclimatic Change for Tularemia Outbreaks in High-Risk Areas across Sweden. Int. J. Environ. Res. Public Health 2020, 17, 6786. [Google Scholar] [CrossRef] [PubMed]
- Hennebique, A.; Boisset, S.; Maurin, M. Tularemia as a waterborne disease: A review. Emerg. Microbes Infect. 2019, 8, 1027–1042. [Google Scholar] [CrossRef]
- Singh, A. Eliciting B cell immunity against infectious diseases using nanovaccines. Nat. Nanotechnol. 2021, 16, 16–24. [Google Scholar] [CrossRef]
- Vetter, V.; Denizer, G.; Friedland, L.R.; Krishnan, J.; Shapiro, M. Understanding modern-day vaccines: What you need to know. Ann. Med. 2018, 50, 110–120. [Google Scholar] [CrossRef] [PubMed]
- Sandstrom, G. The tularaemia vaccine. J. Chem. Technol. Biotechnol. 1994, 59, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Vosti, K.L.; Ward, M.K.; Tigertt, W.D. Agar gel precipitin analyses in laboratory-acquired tularemia. J. Clin. Investig. 1962, 41, 1436–1445. [Google Scholar] [CrossRef] [PubMed]
- El Sahly, H.M.; Atmar, R.L.; Patel, S.M.; Wells, J.M.; Cate, T.; Ho, M.; Guo, K.; Pasetti, M.F.; Lewis, D.E.; Sztein, M.B.; et al. Safety, reactogenicity and immunogenicity of Francisella tularensis live vaccine strain in humans. Vaccine 2009, 27, 4905–4911. [Google Scholar] [CrossRef]
- Elkins, K.L.; Kurtz, S.L.; De Pascalis, R. Progress, challenges, and opportunities in Francisella vaccine development. Expert Rev. Vaccines 2016, 15, 1183–1196. [Google Scholar] [CrossRef]
- Twine, S.M.; Shen, H.; Kelly, J.F.; Chen, W.; Sjostedt, A.; Conlan, J.W. Virulence comparison in mice of distinct isolates of type A Francisella tularensis. Microb. Pathog. 2006, 40, 133–138. [Google Scholar] [CrossRef]
- Twine, S.; Shen, H.; Harris, G.; Chen, W.; Sjostedt, A.; Ryden, P.; Conlana, W. BALB/c mice, but not C57BL/6 mice immunized with a ΔclpB mutant of Francisella tularensis subspecies tularensis are protected against respiratory challenge with wild-type bacteria: Association of protection with post-vaccination and post-challenge immune responses. Vaccine 2012, 30, 3634–3645. [Google Scholar]
- Chen, W.; Shen, H.; Webb, A.; KuoLee, R.; Conlan, J.W. Tularemia in BALB/c and C57BL/6 mice vaccinated with Francisella tularensis LVS and challenged intradermally, or by aerosol with virulent isolates of the pathogen: Protection varies depending on pathogen virulence, route of exposure, and host genetic background. Vaccine 2003, 21, 3690–3700. [Google Scholar]
- Bosio, C.M.; Elkins, K.L. Susceptibility to secondary Francisella tularensis live vaccine strain infection in B-cell-deficient mice is associated with neutrophilia but not with defects in specific T-cell-mediated immunity. Infect. Immun. 2001, 69, 194–203. [Google Scholar] [CrossRef]
- Bradford, M.K.; Elkins, K.L. Immune lymphocytes halt replication of Francisella tularensis LVS within the cytoplasm of infected macrophages. Sci. Rep. 2020, 10, 12023. [Google Scholar] [CrossRef] [PubMed]
- De Pascalis, R.; Chou, A.Y.; Ryden, P.; Kennett, N.J.; Sjostedt, A.; Elkins, K.L. Models derived from in vitro analyses of spleen, liver, and lung leukocyte functions predict vaccine efficacy against the Francisella tularensis Live Vaccine Strain (LVS). mBio 2014, 5, e00936. [Google Scholar] [CrossRef] [PubMed]
- Golovliov, I.; Lindgren, H.; Eneslatt, K.; Conlan, W.; Mosnier, A.; Henry, T.; Sjöstedt, A. An In Vitro Co-culture Mouse Model Demonstrates Efficient Vaccine-Mediated Control of Francisella tularensis SCHU S4 and Identifies Nitric Oxide as a Predictor of Efficacy. Front. Cell. Infect. Microbiol. 2016, 6, 152. [Google Scholar] [CrossRef] [PubMed]
- De Pascalis, R.; Chou, A.Y.; Bosio, C.M.; Huang, C.Y.; Follmann, D.A.; Elkins, K.L. Development of functional and molecular correlates of vaccine-induced protection for a model intracellular pathogen, F. tularensis LVS. PLoS Pathog. 2012, 8, e1002494. [Google Scholar] [CrossRef]
- Lindgren, H.; Honn, M.; Golovlev, I.; Kadzhaev, K.; Conlan, W.; Sjostedt, A. The 58-kilodalton major virulence factor of Francisella tularensis is required for efficient utilization of iron. Infect. Immun. 2009, 77, 4429–4436. [Google Scholar] [CrossRef][Green Version]
- Karlsson, J.; Prior, R.G.; Williams, K.; Lindler, L.; Brown, K.A.; Chatwell, N.; Hjalmarsson, K.; Loman, N.; Mack, K.A.; Pallen, M.; et al. Sequencing of the Francisella tularensis strain SCHU 4 genome reveals the shikimate and purine metabolic pathways, targets for the construction of a rationally attenuated auxotrophic vaccine. Microb. Comp. Genom. 2000, 5, 25–39. [Google Scholar] [CrossRef]


| ID Virulence for BALB/c Mice of 60 Distinct Single Gene Deletion Mutants of SCHU S4 | ||
|---|---|---|
| ID LD50 <30 CFUa ΔFtt | ID LD50 >102 but <106 CFU ΔFtt: | ID LD50 ≥ 107 CFU ΔFtt |
| ahp b, capB, chiX, fadAD2, fadD2, feoB, gpx, hfq, katG, mdaB, oppD, oxyR c, pckA-L d, pdpC c,e, pdpD, pepO, PI1 c,g, PI2 b,g, PilAEV f, pilB, pilC, pilQ, PilT, pmrA c, pyrB, qseC b, RD5, RD8, recA, relA, rimK, sodC, tet, usp, 0023, 0024, 0029, 0069, 0086, fupB, 1023 c, 1149 b, 1564 b | pckA-S d, fupA c, ggt f | iglB, iglC, iglD, gplX, wbtC, wbtI, clpB f kdtA, lpcC, purF, sspA, mglA, FLT0439 g,h FTT0085, |
| Criterion | LVS | ΔclpB | FSC033 a, SCHU S4 a (MTD) b |
|---|---|---|---|
| ID LD50 | >107 CFU | >107 CFU | <10 CFU (7) |
| IN LD50 | ~103 CFU c | 104–106 CFU d | <10 CFU (6) |
| % deaths following ~105 CFU ID e | 2.1 (n = 185) f | 1.4 (n = 560) f | 100 |
| Necrosis score at site of injection | 2–3 g | 0–1 g | 4 g |
| SCID mice MTD ID 103 CFU ID | 15 | 17 h | ND |
| SCID mice MTD IN 102 CFU IN | 14 | 19 | ND |
| Clinical signs given at 105 ID | Mild | Mild | severe |
| Survival SCHU S4 20–100 CFU IN i | ≤20% | 60–100% i | NA |
| Source of ΔclpB | % Survival after IN Inoculation with ~104 CFU | % Survival after IN Challenge with ~100 CFU SCHU S4 42 Days Later |
|---|---|---|
| Original stock | 100% | 100% |
| 10× in vitro 1 | 100% | 100% |
| 5× in vivo 2 | 100% | 100% |
| Original stock | 100% | 100% |
| 5× in CDM 3,4 | 60% | 100% |
| Fermenter CDM 5 | 40% | 100% |
| Characteristic | |
|---|---|
| Time of harvest from flask | 20.75 h |
| CFU/ml at harvest a | 3.9 × 109 |
| Cryopreservative | Sucrose 10% w/v |
| Colony morphology b | Typical of Ftt and Fth |
| Gram stain c | Typical of Ftt and Fth |
| Lytic phage | Negative |
| Lysogenic phage | Negative |
| Contaminant bacteria d | Negative |
| Genomic sequence e | Identical to original mutant |
| 42-day survival of mice after 104 CFU IN administration (original stock/new stock) f | 100%/60% at day 42; NS h |
| 42-day survival of mice following 105 CFU ID administration (original stock/new stock) | 100%/100% |
| Clinical signs g (original vs. new stock) | Significantly greater vs. old stock on days 3, 4, and 5 |
| Skin reactogenicity g (original vs new stock) | NS h |
| ΔclpB organ load (skin, spleen, liver, lung) 4 days after ID vaccination with 105 CFU of original vs. new stock. | ΔclpB lung burden was significantly higher (p = 0.016) for new vs. original stock |
| Day 4 serum cytokine/chemokine levels (21-plex assay) (original vs. new stock) | NS h |
| 28-day survival against IN challenge with ~100 CFU SCHU S4 after IN vaccination (original/new stock) | 100%/100% |
| Protection against IN challenge with ~100 CFU SCHU S4 after ID vaccination original/new stock (MTD in days) | 60% (28)/0% (16). NS h,i |
| Protection against ID challenge with 105 CFU SCHU S4 or FSC033 after ID vaccination | 100%/100% |
| Date of Run | Flask Starting Inoculum CFU/mL | Flask Harvest Concentration CFU/mL (Culture Time, h) | #Doublings (Doubling Time, h) | Fermenter Inoculum CFU/mL | Fermenter Harvest Time, h (CFU/mL) | #Doublings (Doubling Time, h) | Total CFU × 1014 (# Doses × 106) 1 | Biomass g |
|---|---|---|---|---|---|---|---|---|
| December 2014 | 4.0 × 107 | 5.2 × 109 (18.5) | 7 (2.6) | 3.90 × 106 | 22 (1.1 × 1010) | 12 (1.85) | 242 (24) | 177.3 |
| September 2015 | 2.6 × 107 | 9.0 × 109 (18.25) | 8.4 (2.1) | 1.40 × 107 | 20.5 (1.1 × 1010) | 10 (2.3) | 242 (24) | 204.1 |
| June 2017 | 7.8 × 106 | 9.0 × 109 (18.5) | 10.2 (1.8) | 1.43 × 107 | 26 (1.1 × 1010) | 10 (2.9) | 242 (24) | 74.9 2 |
| Parameter | Test Method | Specification |
|---|---|---|
| clpB specific PCR | Identity confirmed a | |
| Purity | Absence of contaminating organisms b | |
| CFU/mL | Report result | |
| Gram Stain | Gram negative coccobacillus | |
| TBD c | Round, smooth and slightly mucoid single colonies | |
| CFU/Ml d | Report result | |
| LAL e | <5 EU/kg/dose | |
| Susceptible to tetracycline, levofloxacin, gentamycin, chloramphenicol, ciprofloxacin, streptomycin, rifampin f | Susceptible | |
| Karl Fisher g | Report Result | |
| Appearance of cake h | Report result |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Conlan, J.W.; Sjöstedt, A.; Gelhaus, H.C.; Fleming, P.; McRae, K.; Cobb, R.R.; De Pascalis, R.; Elkins, K.L. Modern Development and Production of a New Live Attenuated Bacterial Vaccine, SCHU S4 ΔclpB, to Prevent Tularemia. Pathogens 2021, 10, 795. https://doi.org/10.3390/pathogens10070795
Conlan JW, Sjöstedt A, Gelhaus HC, Fleming P, McRae K, Cobb RR, De Pascalis R, Elkins KL. Modern Development and Production of a New Live Attenuated Bacterial Vaccine, SCHU S4 ΔclpB, to Prevent Tularemia. Pathogens. 2021; 10(7):795. https://doi.org/10.3390/pathogens10070795
Chicago/Turabian StyleConlan, J. Wayne, Anders Sjöstedt, H. Carl Gelhaus, Perry Fleming, Kevan McRae, Ronald R. Cobb, Roberto De Pascalis, and Karen L. Elkins. 2021. "Modern Development and Production of a New Live Attenuated Bacterial Vaccine, SCHU S4 ΔclpB, to Prevent Tularemia" Pathogens 10, no. 7: 795. https://doi.org/10.3390/pathogens10070795
APA StyleConlan, J. W., Sjöstedt, A., Gelhaus, H. C., Fleming, P., McRae, K., Cobb, R. R., De Pascalis, R., & Elkins, K. L. (2021). Modern Development and Production of a New Live Attenuated Bacterial Vaccine, SCHU S4 ΔclpB, to Prevent Tularemia. Pathogens, 10(7), 795. https://doi.org/10.3390/pathogens10070795







