The Role of Urban Built Environment in Enhancing Cardiovascular Health in Chinese Cities: A Systematic Review
Abstract
1. Introduction
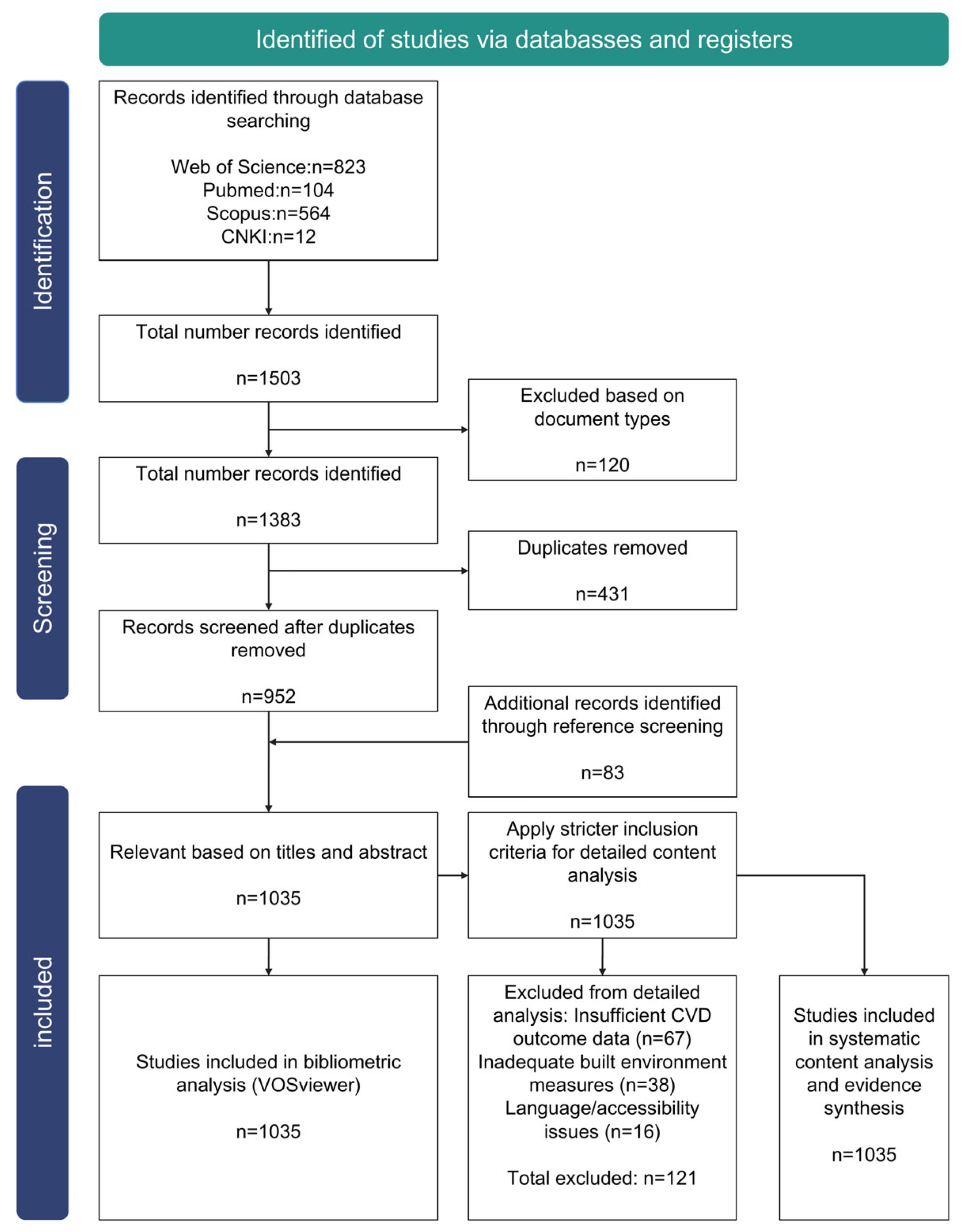
2. Materials and Methods
2.1. Definition
2.2. Search Approach
2.3. Screening and Selection Process
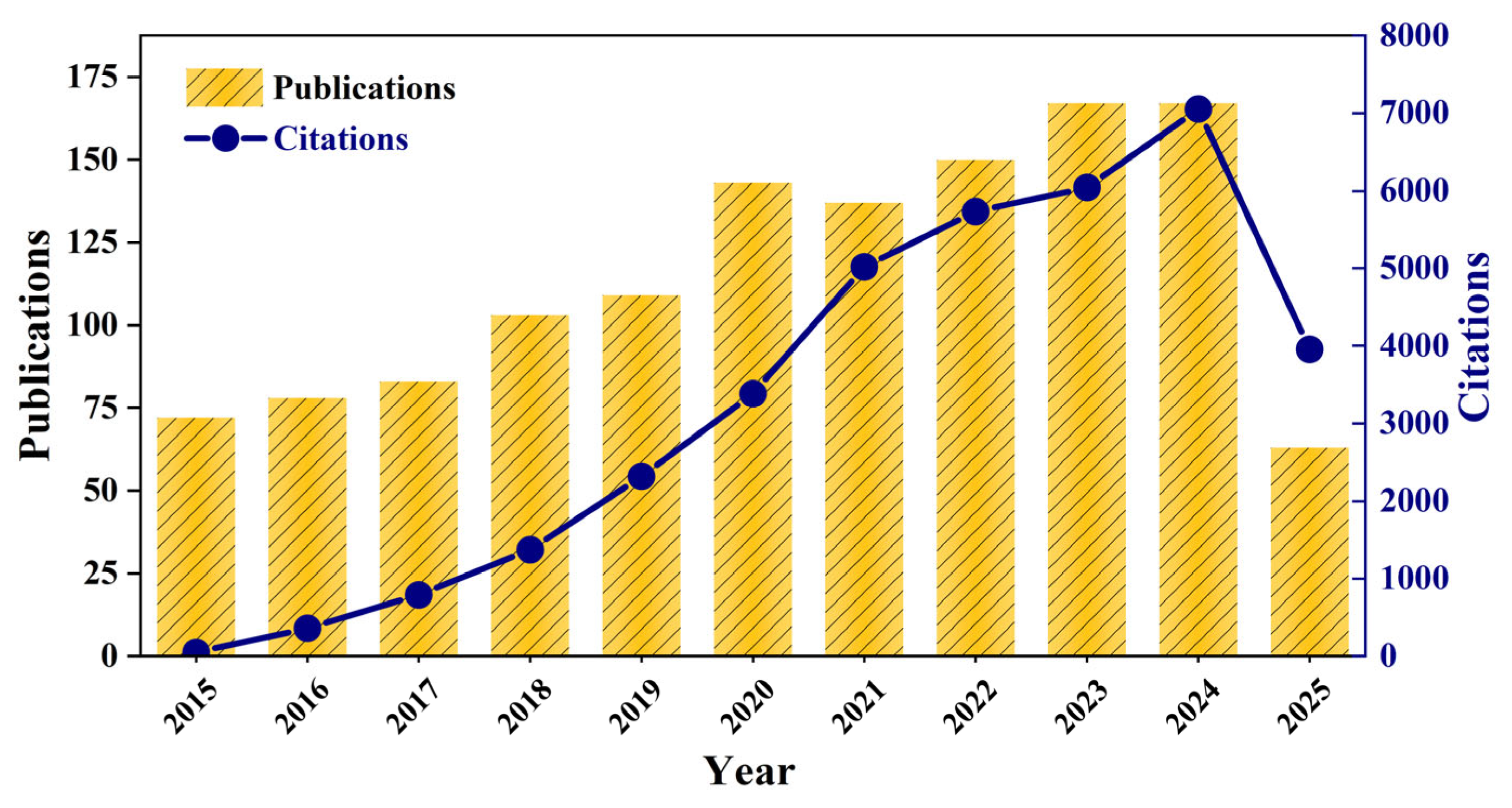
2.4. Result and Analysis
2.5. Evidence Assessment Framework
- Biological Plausibility: Assessing theoretical coherence with established cardiovascular pathophysiology
- Dose–Response Consistency: Examining evidence for exposure gradients and threshold effects
- Temporal Sequence Adequacy: Evaluating whether exposure precedes outcome with appropriate lag periods
- Effect Size Documentation: Requiring quantitative measures with confidence intervals rather than qualitative descriptions
- Confounding Control Robustness: Assessing adequacy of socioeconomic, demographic, behavioral, and environmental adjustments
3. Results
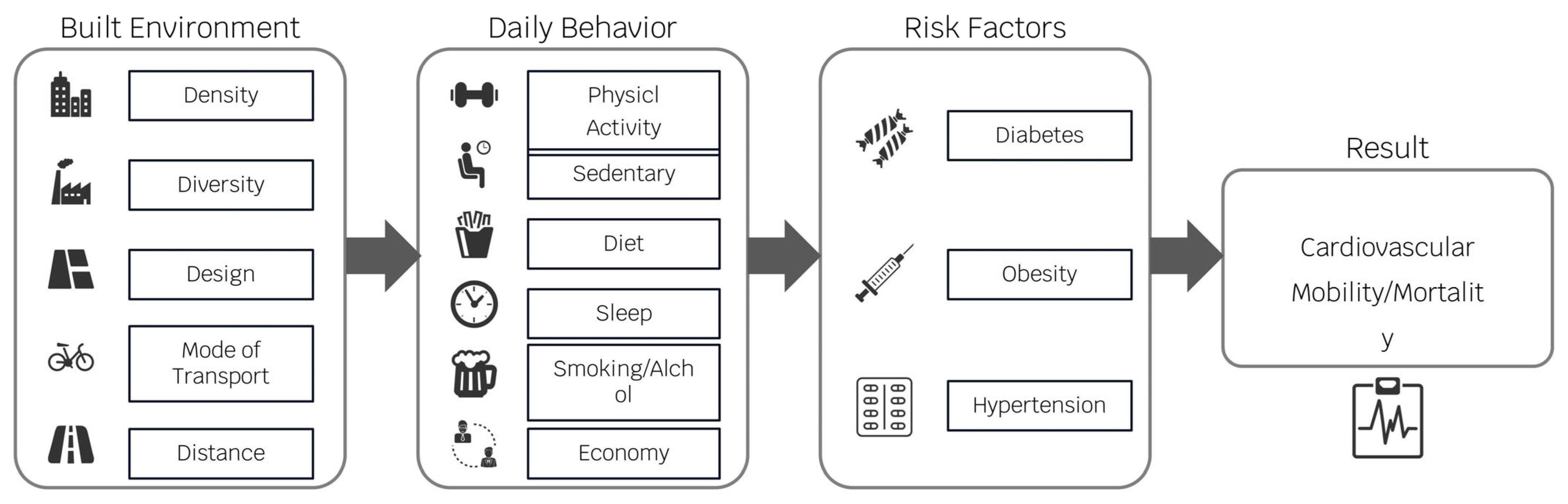
3.1. Elements and Mechanisms of the Built Environment Affecting Cardiovascular Health
3.2. Pathways of the Built Environment on Cardiovascular Health
3.3. Urban Green Spaces
3.3.1. Elements Affecting Cardiovascular Health in Urban Green Open Spaces
3.3.2. Mechanisms of Urban Green Space Effects on Cardiovascular Health
3.4. Active Travel Systems
3.4.1. Elements of Active Travel That Affect Cardiovascular Health
3.4.2. Mechanisms of Active Travel’s Impact on Cardiovascular Health
3.5. Other Elements of the Urban Built Environment That Affect Cardiovascular Health
3.5.1. Quality of Living Space
3.5.2. Urban Food Environment
3.5.3. Mixed Urban Land Use
3.6. Structured Factor Assessment
4. Discussion
4.1. Research Gaps Identified Through Evidence Synthesis
4.2. Implications for Urban Planning and Design Practice
4.3. Evidence Integration and Mechanistic Hierarchy Development
4.3.1. Methodological Constraints and Transparency
4.3.2. Evidence-Based Pathway Hierarchy
4.3.3. Methodological Sensitivity Analysis
4.3.4. Influence of Study Design on Causal Inference
4.3.5. Methodological Heterogeneity and Measurement Limitations
- Heterogeneity in Exposure Measurement:
- Walkability: This key exposure was operationalized in fundamentally different ways across studies. Objective measures included sophisticated indices incorporating residential density, intersection density, and land use mix, GIS-based accessibility calculations, and built environment audits. Subjective measures relied on perceived walkability surveys and self-reported neighborhood quality assessments. We observed that studies using subjective measures tended to report stronger associations with health outcomes than those using objective indices, suggesting that perceived environmental features and personal biases may amplify effect estimates compared to objective metrics.
- Green Space Exposure: Similarly, green space was measured via diverse approaches: remote sensing indices (e.g., NDVI), percent area calculations, proximity to parks, or self-reported access and quality. NDVI measures capture general vegetation density but not accessibility or usability, while proximity measures ignore qualitative aspects such as park facilities or maintenance. These definitional differences create substantial variation in reported associations and explain some inconsistencies in green space health effects across studies.
- Heterogeneity in Outcome Assessment:
- Physical Activity: This central mediating mechanism demonstrated substantial measurement heterogeneity affecting result magnitude and interpretation. Self-reported questionnaires, used in the majority of studies, are subject to recall and social desirability bias but enable large sample sizes and population-level analysis. Objective measures like accelerometers and pedometers, employed in higher-quality studies, provide more accurate data on volume and intensity but are limited by cost and shorter assessment periods. This methodological difference represents a key source of variation in the strength of built environment-physical activity relationships across studies.
- Cardiovascular Outcomes: Outcome definitions ranged from hard endpoints like mortality (most objective) to morbidity, incidence, and intermediate risk factors (e.g., hypertension, BMI). Studies using intermediate outcomes typically report larger effect sizes due to higher prevalence and earlier detection capability, while mortality studies show more conservative but robust associations.
- Implications for Evidence Synthesis:
- This methodological heterogeneity is not merely a limitation but a critical factor for evidence interpretation. For example, the seemingly counterintuitive finding that residents of more walkable areas might report more sedentary time [105] could be partly explained by measurement approaches-the use of objective walkability indices combined with self-reported sedentary time may not capture the full context of daily life patterns (e.g., sedentary occupations concentrated in walkable urban centers).
4.4. Study Limitations and Future Directions
5. Conclusions
5.1. Evidence-Based Mechanistic Assessment and Hierarchy
5.2. Main Research Questions and Findings
5.3. Key Findings from Literature Review
5.4. Recommendations for Current and Future Research Gaps
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| NDVI | Normalized Difference Vegetation Index |
| WHO | World Health Organization |
| CVD | Cardiovascular Disease |
| BMI | body-mass index |
| TOD | Transit-Oriented Development |
| IQR | Interquartile Range |
| VOC | Volatile Organic Compound |
| CHD | Coronary Heart Disease |
| CAD | Coronary Artery Disease |
Appendix A
| Database | Search Strategy Description | Search Date |
|---|---|---|
| Web of Science | Utilized Title, Abstract, Author Keywords, and Keywords Plus fields. Combined cardiovascular disease terms (cardiovascular disease, CVD, heart disease, hypertension, stroke) with built environment terms (built environment, urban planning, urban design, green space, walkability) using Boolean operators (AND, OR). Geographic limitation applied using China-related terms. | 5 July 2025 |
| Scopus | Employed TITLE-ABS-KEY field search strategy. Used comprehensive cardiovascular and built environment terminology with Boolean logic. Applied language and geographic filters for Chinese context studies. | 5 July 2025 |
| PubMed | Combined Medical Subject Headings (MeSH terms) with free-text keywords. Used both controlled vocabulary (“Cardiovascular Diseases”, “Environment Design”) and natural language terms in Title/Abstract fields. Applied geographic MeSH terms for China. | 5 July 2025 |
| CNKI | Implemented Chinese-language keyword strategy using equivalent cardiovascular and built environment terminology. Utilized subject and keyword fields with Chinese Boolean operators to capture relevant Chinese-language literature. | 5 July 2025 |
References
- Hu, S. Report on Cardiovascular Health and Diseases in China 2019: An Updated Summary. Chin. Circ. J. 2020, 35, 3969. [Google Scholar]
- Wang, L.; Wang, Y.; Ji, Z.; Zhu, R.; Wu, H.; Li, J.; Zheng, L.; Zhang, L. Trends of cause-specific cardiovascular disease mortality in China, 2009-2019: A nationwide longitudinal study. Ann. Med. 2025, 57, 2455534. [Google Scholar] [CrossRef]
- Nieuwenhuijsen, M.J. Influence of urban and transport planning and the city environment on cardiovascular disease. Nat. Rev. Cardiol. 2018, 15, 432–438. [Google Scholar] [CrossRef]
- Liang, J.; Deng, S.; Yang, H.; Zhu, S.; Zheng, R. Spatiotemporal effects of urban micro-scale built environment on cardiovascular diseases. Sci. Rep. 2025, 15, 17193. [Google Scholar] [CrossRef]
- Lai, K.Y.; Webster, C.; Gallacher, J.E.J.; Sarkar, C. Associations of Urban Built Environment with Cardiovascular Risks and Mortality: A Systematic Review. J. Urban Health 2023, 100, 745–787. [Google Scholar] [CrossRef]
- Cho, M. Evaluating Therapeutic Healthcare Environmental Criteria: Architectural Designers’ Perspectives. Int. J. Environ. Res. Public Health 2023, 20, 1540. [Google Scholar] [CrossRef]
- Eldesoky, A.H.; Abdeldayem, W.S. Disentangling the Relationship between Urban Form and Urban Resilience: A Systematic Literature Review. Urban Sci. 2023, 7, 93. [Google Scholar] [CrossRef]
- Rostamnezhad, M.; Thaheem, M.J. Social Sustainability in Construction Projects-A Systematic Review of Assessment Indicators and Taxonomy. Sustainability 2022, 14, 5279. [Google Scholar] [CrossRef]
- Aliyu, A.A.; Amadu, L. Urbanization, cities, and health: The challenges to Nigeria-A review. Ann. Afr. Med. 2017, 16, 149–158. [Google Scholar] [CrossRef]
- Sundas, A.; Contreras, I.; Mujahid, O.; Beneyto, A.; Vehi, J. The Effects of Environmental Factors on General Human Health: A Scoping Review. Healthcare 2024, 12, 2123. [Google Scholar] [CrossRef] [PubMed]
- Shen, J.; Wang, S.; Wang, Y. Environmental Inequality in Peri-Urban Areas: A Case Study of Huangpu District, Guangzhou City. Land 2024, 13, 703. [Google Scholar] [CrossRef]
- Ninomiya, M.E.M.; Burns, N.; Pollock, N.J.; Green, N.T.G.; Martin, J.; Linton, J.; Rand, J.R.; Brubacher, L.J.; Keeling, A.; Latta, A. Indigenous communities and the mental health impacts of land dispossession related to industrial resource development: A systematic review. Lancet Planet. Health 2023, 7, e501–e517. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Integrating Health in Urban and Territorial Planning: A Sourcebook; World Health Organization: Geneva, Switzerland, 2020; ISBN 9789240003170. [Google Scholar]
- World Health Organization South-East Asia. Healthy Cities Initiative. 2024. Available online: https://www.who.int/southeastasia/activities/healthy-cities (accessed on 14 September 2025).
- Reyes, R.; Ahn, R.; Thurber, K.; Burke, T.F. Urbanization and Infectious Diseases: General Principles, Historical Perspectives, and Contemporary Challenges. In Challenges in Infectious Disease; Springer: New York, NY, USA, 2013; pp. 123–146. [Google Scholar] [CrossRef]
- Harris, P.; Harris-Roxas, B.; Prior, J.; Morrison, N.; McIntyre, E.; Frawley, J.; Adams, J.; Bevan, W.; Haigh, F.; Freeman, E.; et al. Respiratory pandemics, urban planning and design: A multidisciplinary rapid review of the literature. Cities 2022, 127, 103767. [Google Scholar] [CrossRef]
- Luo, Y.; Wang, S. Urban living and chronic diseases in the presence of economic growth: Evidence from a long-term study in southeastern China. Front. Public Health 2022, 10, 1042413. [Google Scholar] [CrossRef] [PubMed]
- Cacciatore, S.; Mao, S.; Nuñez, M.V.; Massaro, C.; Spadafora, L.; Bernardi, M.; Perone, F.; Sabouret, P.; Biondi-Zoccai, G.; Banach, M.; et al. Urban health inequities and healthy longevity: Traditional and emerging risk factors across the cities and policy implications. Aging Clin. Exp. Res. 2025, 37, 143. [Google Scholar] [CrossRef]
- Rahman, M.; Sciara, G.-C. Travel attitudes, the built environment and travel behavior relationships: Causal insights from social psychology theories. Transp. Policy 2022, 123, 44–54. [Google Scholar] [CrossRef]
- Travert, A.A.-O.; Sidney Annerstedt, K.A.-O.; Daivadanam, M.A.-O. Built Environment and Health Behaviors: Deconstructing the Black Box of Interactions-A Review of Reviews. Int. J. Environ. Res. Public Health 2019, 16, 1454. [Google Scholar] [CrossRef] [PubMed]
- Xiao, D.; Ding, H.; Sze, N.N.; Zheng, N. Investigating built environment and traffic flow impact on crash frequency in urban road networks. Accid. Anal. Prev. 2024, 201, 107561. [Google Scholar] [CrossRef]
- Yuan, M.; Yin, C.; Sun, Y.; Chen, W. Examining the associations between urban built environment and noise pollution in high-density high-rise urban areas: A case study in Wuhan, China. Sustain. Cities Soc. 2019, 50, 101678. [Google Scholar] [CrossRef]
- Manisalidis, I.; Stavropoulou, E.; Stavropoulos, A.; Bezirtzoglou, E. Environmental and Health Impacts of Air Pollution: A Review. Front. Public Health 2020, 8, 505570. [Google Scholar] [CrossRef]
- Colabianchi, N.; Antonakos, C.L.; Coulton, C.J.; Kaestner, R.; Lauria, M.; Porter, D.E. The role of the built environment, food prices and neighborhood poverty in fruit and vegetable consumption: An instrumental variable analysis of the moving to opportunity experiment. Health Place 2021, 67, 102491. [Google Scholar]
- Joseph, J.J.; Deedwania, P.; Acharya, T.; Aguilar, D.; Bhatt, D.L.; Chyun, D.A.; Di Palo, K.E.; Golden, S.H.; Sperling, L.S.; American Heart Association Diabetes Committee of the Council on Lifestyle and Cardiometabolic Health; et al. Comprehensive Management of Cardiovascular Risk Factors for Adults with Type 2 Diabetes: A Scientific Statement From the American Heart Association. Circulation 2022, 145, e722–e759. [Google Scholar] [CrossRef]
- Chen, L.; Zhang, Z.; Long, Y. Association between leisure-time physical activity and the built environment in China: Empirical evidence from an accelerometer and GPS-based fitness app. PLoS ONE 2022, 16, e0260570. [Google Scholar] [CrossRef]
- Pinter-Wollman, N.; Jelić, A.; Wells, N.M. The impact of the built environment on health behaviours and disease transmission in social systems. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2018, 373, 20170245. [Google Scholar] [CrossRef] [PubMed]
- Lichtenstein, A.H.; Appel, L.J.; Vadiveloo, M.; Hu, F.B.; Kris-Etherton, P.M.; Rebholz, C.M.; Sacks, F.M.; Thorndike, A.N.; Van Horn, L.; Wylie-Rosett, J.; et al. 2021 Dietary Guidance to Improve Cardiovascular Health: A Scientific Statement From the American Heart Association. Circulation 2021, 144, e472–e487. [Google Scholar] [CrossRef] [PubMed]
- Sharifi-Rad, J.; Rodrigues, C.F.; Sharopov, F.; Docea, A.O.; Can Karaca, A.; Sharifi-Rad, M.; Kahveci Karıncaoglu, D.; Gülseren, G.; Şenol, E.; Demircan, E.; et al. Diet, Lifestyle and Cardiovascular Diseases: Linking Pathophysiology to Cardioprotective Effects of Natural Bioactive Compounds. Int. J. Environ. Res. Public Health 2020, 17, 2326. [Google Scholar] [CrossRef] [PubMed]
- Rahelić, V.; Perković, T.; Romić, L.; Perković, P.; Klobučar, S.; Pavić, E.; Rahelić, D. The Role of Behavioral Factors on Chronic Diseases-Practice and Knowledge Gaps. Healthcare 2024, 12, 2520. [Google Scholar] [CrossRef]
- Héritier, H.; Vienneau, D.; Foraster, M.; Eze, I.C.; Schaffner, E.; de Hoogh, K.; Thiesse, L.; Rudzik, F.; Habermacher, M.; Köpfli, M.; et al. A systematic analysis of mutual effects of transportation noise and air pollution exposure on myocardial infarction mortality: A nationwide cohort study in Switzerland. Eur. Heart J. 2019, 40, 598–603. [Google Scholar] [CrossRef]
- Kälsch, H.; Hennig, F.; Moebus, S.; Möhlenkamp, S.; Dragano, N.; Jakobs, H.; Memmesheimer, M.; Erbel, R.; Jöckel, K.-H.; Hoffmann, B.; et al. Are air pollution and traffic noise independently associated with atherosclerosis: The Heinz Nixdorf Recall Study. Eur. Heart J. 2014, 35, 853–860. [Google Scholar] [CrossRef]
- Schultz, W.M.; Kelli, H.M.; Lisko, J.C.; Varghese, T.; Shen, J.; Sandesara, P.; Quyyumi, A.A.; Taylor, H.A.; Gulati, M.; Harold, J.G.; et al. Socioeconomic Status and Cardiovascular Outcomes: Challenges and Interventions. Circulation 2018, 137, 2166–2178. [Google Scholar] [CrossRef]
- Kathiresan, S.; Srivastava, D. Genetics of human cardiovascular disease. Cell 2012, 148, 1242–1257. [Google Scholar] [CrossRef]
- Czepluch, F.S.; Wollnik, B.; Hasenfuß, G. Genetic determinants of heart failure: Facts and numbers. ESC Heart Fail. 2018, 5, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Niculita-Hirzel, H.; Hirzel, A.H.; Wild, P. A GIS-based approach to assess the influence of the urban built environment on cardiac and respiratory outcomes in older adults. Build. Environ. 2024, 253, 111362. [Google Scholar] [CrossRef]
- Shen, Y.S.; Lung, S.C.C. Multiple impacts and pathways of urban form and environmental factors on cardiovascular mortality. Sci. Total Environ. 2020, 738, 139512. [Google Scholar] [CrossRef] [PubMed]
- Moore, T.H.M.; Kesten, J.M.; López-López, J.A.; Ijaz, S.; McAleenan, A.; Richards, A.; Gray, S.; Savović, J.; Audrey, S. The effects of changes to the built environment on the mental health and well-being of adults: Systematic review. Health Place 2018, 53, 237–257. [Google Scholar] [CrossRef]
- Sims, M.; Kershaw, K.N.; Breathett, K.; Jackson, E.A.; Lewis, L.M.; Mujahid, M.S.; Suglia, S.F. Importance of Housing and Cardiovascular Health and Well-Being: A Scientific Statement From the American Heart Association. Circ. Cardiovasc. Qual. Outcomes 2020, 13, e000089. [Google Scholar] [CrossRef]
- Bhatnagar, A. Environmental Determinants of Cardiovascular Disease. Circ. Res. 2017, 121, 162–180. [Google Scholar] [CrossRef]
- Lim, E.Y.; Kim, G.-D. Particulate Matter-Induced Emerging Health Effects Associated with Oxidative Stress and Inflammation. Antioxidants 2024, 13, 1256. [Google Scholar] [CrossRef]
- Hahad, O.; Rajagopalan, S.; Lelieveld, J.; Sørensen, M.; Kuntic, M.; Daiber, A.; Basner, M.; Nieuwenhuijsen, M.; Brook, R.D.; Münzel, T. Noise and Air Pollution as Risk Factors for Hypertension: Part II-Pathophysiologic Insight. Hypertension 2023, 80, 1384–1392. [Google Scholar] [CrossRef]
- Hahad, O.; Prochaska, J.H.; Daiber, A.; Muenzel, T. Environmental Noise-Induced Effects on Stress Hormones, Oxidative Stress, and Vascular Dysfunction: Key Factors in the Relationship between Cerebrocardiovascular and Psychological Disorders. Oxid. Med. Cell Longev. 2019, 2019, 4623109. [Google Scholar] [CrossRef]
- Cho, S.; Lim, D.Y.; Kim, S.; Kim, H.; Kang, W.; Park, W.J. Association between Occupational Noise Exposure and Insomnia among Night-Shift Production Workers: A 4-Year Follow-up Study. Noise Health 2023, 25, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Qi, X.; Yang, J.; Liu, L.; Hao, J.; Pan, C.; Wen, Y.; Zhang, N.; Wei, W.; Kang, M.; Cheng, B.; et al. Socioeconomic inequalities, genetic susceptibility, and risks of depression and anxiety: A large-observational study. J. Affect. Disord. 2024, 367, 174–183. [Google Scholar] [CrossRef] [PubMed]
- Shahbazi, F.; Shahbazi, M.; Poorolajal, J. Association between socioeconomic inequality and the global prevalence of anxiety and depressive disorders: An ecological study. Gen. Psychiatr. 2022, 35, e100735. [Google Scholar] [CrossRef]
- Yeates, K.; Lohfeld, L.; Sleeth, J.; Morales, F.; Rajkotia, Y.; Ogedegbe, O. A Global Perspective on Cardiovascular Disease in Vulnerable Populations. Can. J. Cardiol. 2015, 31, 1081–1093. [Google Scholar] [CrossRef]
- Sharifi, Y.; Sobhani, S.; Ramezanghorbani, N.; Payab, M.; Ghoreshi, B.; Djalalinia, S.; Nouri Ghonbalani, Z.; Ebrahimpur, M.; Eslami, M.; Qorbani, M. Association of greenspaces exposure with cardiometabolic risk factors: A systematic review and meta-analysis. BMC Cardiovasc. Disord. 2024, 24, 170. [Google Scholar] [CrossRef] [PubMed]
- Tamosiunas, A.; Grazuleviciene, R.; Luksiene, D.; Dedele, A.; Reklaitiene, R.; Baceviciene, M.; Vencloviene, J.; Bernotiene, G.; Radisauskas, R.; Malinauskiene, V.; et al. Accessibility and use of urban green spaces, and cardiovascular health: Findings from a Kaunas cohort study. Environ. Health 2014, 13, 20. [Google Scholar] [CrossRef]
- Brook, R.D.; Rajagopalan, S.; Pope, C.A., III; Brook, J.R.; Bhatnagar, A.; Diez-Roux, A.V.; Holguin, F.; Hong, Y.; Luepker, R.V.; Mittleman, M.A.; et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 2010, 121, 2331–2378. [Google Scholar] [CrossRef]
- Mao, Q.; Zhu, X.; Zhang, X.; Kong, Y. Effect of air pollution on the global burden of cardiovascular diseases and forecasting future trends of the related metrics: A systematic analysis from the Global Burden of Disease Study 2021. Front. Med. 2024, 11, 1472996. [Google Scholar] [CrossRef]
- Peng, R.D.; Chang, H.H.; Bell, M.L.; McDermott, A.; Zeger, S.L.; Samet, J.M.; Dominici, F. Coarse Particulate Matter Air Pollution and Hospital Admissions for Cardiovascular and Respiratory Diseases Among Medicare Patients. JAMA 2008, 299, 2172–2179. [Google Scholar] [CrossRef]
- Shah, A.S.V.; Langrish, J.P.; Nair, H.; McAllister, D.A.; Hunter, A.L.; Donaldson, K.; Newby, D.E.; Mills, N.L. Global association of air pollution and heart failure: A systematic review and meta-analysis. Lancet 2013, 382, 1039–1048. [Google Scholar] [CrossRef]
- Fuchs, F.D.; Whelton, P.K. High Blood Pressure and Cardiovascular Disease. Hypertension 2020, 75, 285–292. [Google Scholar] [CrossRef]
- Poznyak, A.V.; Litvinova, L.; Poggio, P.; Sukhorukov, V.N.; Orekhov, A.N. Effect of Glucose Levels on Cardiovascular Risk. Cells 2022, 11, 3034. [Google Scholar] [CrossRef]
- Wazir, M.; Olanrewaju, O.A.; Yahya, M.; Kumari, J.; Kumar, N.; Singh, J.; Abbas Al-Itbi, A.Y.; Kumari, K.; Ahmed, A.; Islam, T.; et al. Lipid Disorders and Cardiovascular Risk: A Comprehensive Analysis of Current Perspectives. Cureus 2023, 15, e51395. [Google Scholar] [CrossRef]
- Hayward, E.; Ibe, C.; Young, J.H.; Potti, K.; Jones, P.; Pollack, C.E.; Gudzune, K.A. Linking social and built environmental factors to the health of public housing residents: A focus group study. BMC Public Health 2015, 15, 351. [Google Scholar] [CrossRef]
- Xu, L.; Han, H.; Yang, C.; Liu, Q. The Influence Mechanism of the Community Subjectively Built Environment on the Physical and Mental Health of Older Adults. Sustainability 2023, 15, 13211. [Google Scholar] [CrossRef]
- Huang, J.; Xu, Y.; Wang, L. Pathways and spatial elements of the impact of urban built environment on cardiovascular health. Urban. Dev. Res. 2023, 30, 14–20. [Google Scholar]
- Gobster, P.H.; Westphal, L.M. The human dimensions of urban greenways: Planning for recreation and related experiences. Landsc. Urban Plan. 2004, 68, 147–165. [Google Scholar] [CrossRef]
- McCormack, G.R.; Rock, M.; Toohey, A.M.; Hignell, D. Characteristics of urban parks associated with park use and physical activity: A review of qualitative research. Health Place 2010, 16, 712–726. [Google Scholar] [CrossRef]
- Schetke, S.; Qureshi, S.; Lautenbach, S.; Kabisch, N. What determines the use of urban green spaces in highly urbanized areas?–Examples from two fast growing Asian cities. Urban For. Urban Green. 2016, 16, 150–159. [Google Scholar] [CrossRef]
- Sugiyama, T.; Francis, J.; Middleton, N.J.; Owen, N.; Giles-Corti, B. Associations between recreational walking and attractiveness, size, and proximity of neighborhood open spaces. Am. J. Public Health 2010, 100, 1752–1757. [Google Scholar] [PubMed]
- Kaczynski, A.T.; Potwarka, L.R.; Saelens, B.E. Association of park size, distance, and features with physical activity in neighborhood parks. Am. J. Public Health 2008, 98, 1451–1456. [Google Scholar] [CrossRef]
- Wang, H.; Dai, X.; Wu, J.; Wu, X.; Nie, X. Influence of urban green open space on residents’ physical activity in China. BMC Public Health 2019, 19, 1093. [Google Scholar] [CrossRef]
- Douglas, O.; Lennon, M.; Scott, M. Green space benefits for health and well-being: A life-course approach for urban planning, design and management. Cities 2017, 66, 53–62. [Google Scholar] [CrossRef]
- Mou, C.; Wang, Z.; Ke, Z. Association between physical activity and multimorbidity: A population-based cohort study. Arch. Public Health 2025, 83, 71. [Google Scholar] [CrossRef]
- Chen, M.; Cheng, L.; Yang, S.; Zhang, Y. Physical activity, Vitamin D, and all-cause/cardiovascular mortality: A prospective study in older Chinese adults. BMC Geriatr. 2025, 25, 38. [Google Scholar] [CrossRef]
- Sarkar, C. Residential greenness and adiposity: Findings from the UK Biobank. Environ. Int. 2017, 106, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Celis-Morales, C.A.; Lyall, D.M.; Welsh, P.; Anderson, J.; Steell, L.; Guo, Y.; Maldonado, R.; Mackay, D.F.; Pell, J.P.; Sattar, N.; et al. Association between active commuting and incident cardiovascular disease, cancer, and mortality: Prospective cohort study. BMJ Clin. Res. Ed. 2017, 357, j1456. [Google Scholar] [CrossRef]
- Hamer, M.; Chida, Y. Active commuting and cardiovascular risk: A meta-analytic review. Prev. Med. 2008, 46, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Coombes, E.; Jones, A.P.; Hillsdon, M. The relationship of physical activity and overweight to objectively measured green space accessibility and use. Soc. Sci. Med. 2010, 70, 816–822. [Google Scholar] [CrossRef] [PubMed]
- Hogendorf, M.; Groeniger, J.O.; Noordzij, J.M.; Beenackers, M.A.; van Lenthe, F.J. Longitudinal effects of urban green space on walking and cycling: A fixed effects analysis. Health Place 2020, 61, 102264. [Google Scholar] [CrossRef]
- Sarkar, C.; Webster, C.; Pryor, M.; Tang, D.; Melbourne, S.; Zhang, X.; Liu, J. Exploring associations between urban green, street design and walking: Results from the Greater London boroughs. Landsc. Urban Plan. 2015, 143, 112–125. [Google Scholar] [CrossRef]
- Luo, H.; Zhang, Q.; Yu, K.; Meng, X.; Kan, H.; Chen, R. Long-term exposure to ambient air pollution is a risk factor for trajectory of cardiometabolic multimorbidity: A prospective study in the UK Biobank. EBioMedicine 2022, 84, 104282. [Google Scholar] [CrossRef]
- Kampfrath, T.; Maiseyeu, A.; Ying, Z.; Shah, Z.; Deiuliis, J.A.; Xu, X.; Kherada, N.; Brook, R.D.; Reddy, K.M.; Padture, N.P.; et al. Chronic fine particulate matter exposure induces systemic vascular dysfunction via NADPH oxidase and TLR4 pathways. Circ. Res. 2011, 108, 716–726. [Google Scholar] [CrossRef]
- Dwivedi, A.K.; Vishwakarma, D.; Dubey, P.; Reddy, S.Y. Air pollution and the heart: Updated evidence from meta-analysis studies. Curr. Cardiol. Rep. 2022, 24, 1811–1835. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.M. Assessing personal exposure to traffic-related air pollution using individual travel-activity diary data and an on-road source air dispersion model. Health Place 2020, 63, 102351. [Google Scholar] [CrossRef] [PubMed]
- Dadvand, P.; Rivas, I.; Basagaña, X.; Alvarez-Pedrerol, M.; Su, J.; De Castro Pascual, M.; Amato, F.; Jerret, M.; Querol, X.; Sunyer, J.; et al. The association between greenness and traffic-related air pollution at schools. Sci. Total Environ. 2015, 523, 59–63. [Google Scholar] [CrossRef]
- Münzel, T.; Schmidt, F.P.; Steven, S.; Herzog, J.; Daiber, A.; Sørensen, M. Environmental Noise and the Cardiovascular System. J. Am. Coll. Cardiol. 2018, 71, 688–697. [Google Scholar] [CrossRef]
- Héritier, H.; Vienneau, D.; Foraster, M.; Eze, I.C.; Schaffner, E.; Thiesse, L.; Rudzik, F.; Habermacher, M.; Köpfli, M.; Pieren, R.; et al. Transportation noise exposure and cardiovascular mortality: A nationwide cohort study from Switzerland. Eur. J. Epidemiol. 2017, 32, 307–315. [Google Scholar] [CrossRef]
- Babisch, W. Stress hormones in the research on cardiovascular effects of noise. Noise Health 2003, 5, 1–11. [Google Scholar] [PubMed]
- Babisch, W. Cardiovascular effects of noise. Noise Health 2011, 13, 201–204. [Google Scholar] [CrossRef]
- Halonen, J.I.; Hansell, A.L.; Gulliver, J.; Morley, D.; Blangiardo, M.; Fecht, D.; Toledano, M.B.; Beevers, S.D.; Anderson, H.R.; Kelly, F.J.; et al. Road traffic noise is associated with increased cardiovascular morbidity and mortality and all-cause mortality in London. Eur. Heart J. 2015, 36, 2653–2661. [Google Scholar] [CrossRef]
- Feng, L.; Wang, J.; Liu, B.; Hu, F.; Hong, X.; Wang, W. Does Urban Green Space Pattern Affect Green Space Noise Reduction? Forests 2024, 15, 1719. [Google Scholar] [CrossRef]
- Schäffer, B.; Brink, M.; Schlatter, F.; Vienneau, D.; Wunderli, J.M. Residential green is associated with reduced annoyance to road traffic and railway noise but increased annoyance to aircraft noise exposure. Environ. Int. 2020, 143, 105885. [Google Scholar] [CrossRef]
- Lu, J.; Xiao, Y.; Shao, Y. Research on the Comprehensive Noise Reduction Effectiveness of Plant Communities in Urban Green Spaces. Landsc. Archit. Front. 2025, 13, 76–91. [Google Scholar]
- Walk Score Methodology. 2025. Available online: https://www.walkscore.com/methodology.shtml (accessed on 14 September 2025).
- Van Melle, J.P.; De Jonge, P.; Spijkerman, T.A.; Tijssen, J.G.P.; Ormel, J.; van Veldhuisen, D.J.; van den Brink, R.H.S.; van den Berg, M.P. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: A meta-analysis. Biopsychosoc. Sci. Med. 2004, 66, 814–822. [Google Scholar] [CrossRef]
- Roest, A.M.; Martens, E.J.; De Jonge, P.; Denollet, J. Anxiety and risk of incident coronary heart disease: A meta-analysis. J. Am. Coll. Cardiol. 2010, 56, 38–46. [Google Scholar] [CrossRef]
- Astell-Burt, T.; Feng, X.; Kolt, G.S. Mental health benefits of neighbourhood green space are stronger among physically active adults in middle-to-older age: Evidence from 260,061 Australians. Prev. Med. 2013, 57, 601–606. [Google Scholar] [CrossRef]
- Astell-Burt, T.; Feng, X.; Kolt, G.S. Is neighborhood green space associated with a lower risk of type 2 diabetes? Evidence from 267,072 Australians. Diabetes Care 2014, 37, 197–201. [Google Scholar] [CrossRef]
- Annerstedt, M.; Östergren, P.O.; Björk, J.; Grahn, P.; Skärbäck, E.; Währborg, P. Green qualities in the neighbourhood and mental health-Results from a longitudinal cohort study in Southern Sweden. BMC Public Health 2012, 12, 337. [Google Scholar] [CrossRef]
- De Vries, S.; Van Dillen, S.M.; Groenewegen, P.P.; Spreeuwenberg, P. Streetscape greenery and health: Stress, social cohesion and physical activity as mediators. Soc. Sci. Med. 2013, 94, 26–33. [Google Scholar] [CrossRef]
- Roe, J.J.; Thompson, C.W.; Aspinall, P.A.; Brewer, M.J.; Duff, E.I.; Miller, D.; Mitchell, R.; Clow, A. Green space and stress: Evidence from cortisol measures in deprived urban communities. Int. J. Environ. Res. Public Health 2013, 10, 4086–4103. [Google Scholar] [CrossRef]
- White, M.P.; Alcock, I.; Wheeler, B.W.; Depledge, M.H. Would you be happier living in a greener urban area? A fixed-effects analysis of panel data. Psychol. Sci. 2013, 24, 920–928. [Google Scholar] [CrossRef]
- Yang, B.-Y.; Hu, L.-W.; Jalaludin, B.; Knibbs, L.D.; Markevych, I.; Heinrich, J.; Bloom, M.S.; Morawska, L.; Lin, S.; Jalava, P.; et al. Association between residential greenness, cardiometabolic disorders, and cardiovascular disease among adults in China. JAMA Netw. Open 2020, 3, e2017507. [Google Scholar] [CrossRef]
- Kelly, P.; Williamson, C.; Niven, A.G.; Hunter, R.; Mutrie, N.; Richards, J. Walking on sunshine: Scoping review of the evidence for walking and mental health. Br. J. Sports Med. 2018, 52, 800–806. [Google Scholar] [CrossRef]
- Hashim, N.H.M.; Thani, S.K.S.O.; Jamaludin, M.A.; Yatim, N.M. A perceptual study on the influence of vegetation design towards women’s safety in public park. Procedia-Soc. Behav. Sci. 2016, 234, 280–288. [Google Scholar]
- Li, J.; Huang, Z.; Zheng, D.; Zhao, Y.; Huang, P.; Huang, S.; Fang, W.; Fu, W.; Zhu, Z. Effect of landscape elements on public psychology in urban park waterfront green space: A quantitative study by semantic segmentation. Forests 2023, 14, 244. [Google Scholar] [CrossRef]
- de la Osa, N.; Navarro, J.B.; Penelo, E.; Valentí, A.; Ezpeleta, L.; Dadvand, P. Long-term exposure to greenspace and anxiety from preschool and primary school children. J. Environ. Psychol. 2024, 93, 102207. [Google Scholar] [CrossRef]
- Sugiyama, T.; Leslie, E.; Giles-Corti, B.; Owen, N. Associations of neighbourhood greenness with physical and mental health: Do walking, social coherence and local social interaction explain the relationships? J. Epidemiol. Community Health 2008, 62, e9. [Google Scholar] [CrossRef]
- Lund, H.; Willson, R.W.; Cervero, R. A re-evaluation of travel behavior in California TODs. J. Archit. Plan. Res. 2006, 23, 247–263. [Google Scholar]
- Makhlouf, M.H.; Motairek, I.; Chen, Z.; Nasir, K.; Deo, S.V.; Rajagopalan, S.; Al-Kindi, S.G. Neighborhood Walkability and Cardiovascular Risk in the United States. Curr. Probl. Cardiol. 2022, 48, 101533. [Google Scholar] [CrossRef] [PubMed]
- Howell, N.A.; Tu, J.V.; Moineddin, R.; Chu, A.; Booth, G.L. Association Between Neighborhood Walkability and Predicted 10-Year Cardiovascular Disease Risk: The CANHEART (Cardiovascular Health in Ambulatory Care Research Team) Cohort. J. Am. Heart Assoc. 2019, 8, e013146. [Google Scholar] [CrossRef]
- Van Dyck, D.; Cardon, G.; Deforche, B.; Owen, N.; Sallis, J.F.; De Bourdeaudhuij, I. Neighborhood walkability and sedentary time in Belgian adults. Am. J. Prev. Med. 2010, 39, 25–32. [Google Scholar] [CrossRef]
- Healy, G.N.; Dunstan, D.W.; Salmon, J.; Shaw, J.E.; Zimmet, P.Z.; Owen, N. Television time and continuous metabolic risk in physically active adults. Med. Sci. Sports Exerc. 2008, 40, 639–645. [Google Scholar] [CrossRef]
- Moody, J.; Wang, S.; Chun, J.; Ni, X.; Zhao, J. Transportation policy profiles of Chinese city clusters: A mixed methods approach. Transp. Res. Interdiscip. Perspect. 2019, 2, 100053. [Google Scholar] [CrossRef]
- Yang, W.; Yang, R.; Li, X. A canonical correlation analysis study on the association between neighborhood green space and residents’ mental health. J. Urban Health 2023, 100, 696–710. [Google Scholar]
- Yang, Y.; Tang, S. Examining Residents’ Perceptions and Usage Preferences of Urban Public Green Spaces Through the Lens of Environmental Justice. Sustainability 2025, 17, 2627. [Google Scholar] [CrossRef]
- Enssle, F.; Kabisch, N. Urban green spaces for the social interaction, health and well-being of older people-An integrated view of urban ecosystem services and socio-environmental justice. Environ. Sci. Policy 2020, 109, 36–44. [Google Scholar] [CrossRef]
- Łaszkiewicz, E.; Sikorski, P.; Archiciński, P.; Sikorska, D.; Dobrosz, K.; Kronenberg, J. Would you walk here? Urban wildscapes as visual settings for utility and recreational walks. Cities 2025, 158, 105704. [Google Scholar] [CrossRef]
- Batterman, S.; Ganguly, R.; Harbin, P. High resolution spatial and temporal mapping of traffic-related air pollutants. Int. J. Environ. Res. Public Health 2015, 12, 3646–3666. [Google Scholar]
- Sarnat, S.E.; Sarnat, J.A.; Mulholland, J.; Isakov, V.; Özkaynak, H.; Chang, H.H.; Klein, M.; Tolbert, P.E. Application of alternative spatiotemporal metrics of ambient air pollution exposure in a time-series epidemiological study in Atlanta. J. Expo. Sci. Environ. Epidemiol. 2013, 23, 593–605. [Google Scholar] [CrossRef]
- Bowatte, G.; Lodge, C.; Lowe, A.J.; Erbas, B.; Perret, J.; Abramson, M.J.; Matheson, M.; Dharmage, S.C. The influence of childhood traffic-related air pollution exposure on asthma, allergy and sensitization: A systematic review and a meta-analysis of birth cohort studies. Allergy 2015, 70, 245–256. [Google Scholar]
- Rissel, C.E. Active travel: A climate change mitigation strategy with co-benefits for health. New South Wales Public Health Bull. 2009, 20, 10–13. [Google Scholar]
- Cicala, S.; Holland, S.P.; Mansur, E.T.; Muller, N.Z.; Yates, A.J. Expected health effects of reduced air pollution from COVID-19 social distancing. Atmosphere 2021, 12, 951. [Google Scholar] [CrossRef]
- Wang, Z.; Hu, S. Key points interpretation of the “Report on Cardiovascular Health and Diseases in China 2019”. Chin. J. Cardiovasc. Med. 2020, 25, 401–410. [Google Scholar]
- Lang, J.J.; Pinault, L.; Colley, R.C.; Prince, S.A.; Christidis, T.; Tjepkema, M.; Crouse, D.L.; de Groh, M.; Ross, N.; Villeneuve, P.J. Neighbourhood walkability and mortality: Findings from a 15-year follow-up of a nationally representative cohort of Canadian adults in urban areas. Environ. Int. 2022, 161, 107141. [Google Scholar] [CrossRef]
- Yanek, L.R.; Kral, B.G.; Moy, T.F.; Vaidya, D.; Lazo, M.; Becker, L.C.; Becker, D.M. Effect of positive well-being on incidence of symptomatic coronary artery disease. Am. J. Cardiol. 2013, 112, 1120–1125. [Google Scholar] [CrossRef][Green Version]
- Nitsche, M.P.; Bitran, M.; Pedrals, N.; Echeverría, G.; Rigotti, A. Positive psychosocial factors and cardiovascular health. Rev. Med. Chil. 2014, 142, 1316–1323. [Google Scholar] [CrossRef]
- Halpern, B.S.; Frazier, M.; Verstaen, J.; Rayner, P.-E.; Clawson, G.; Blanchard, J.L.; Cottrell, R.S.; Froehlich, H.E.; Gephart, J.A.; Jacobsen, N.S.; et al. The environmental footprint of global food production. Nat. Sustain. 2022, 5, 1027–1039. [Google Scholar] [CrossRef]
- Hahad, O.; Gilan, D.; Michal, M.; Tüscher, O.; Chalabi, J.; Schuster, A.K.; Keller, K.; Hobohm, L.; Schmitt, V.H.; König, J.; et al. Noise annoyance and cardiovascular disease risk: Results from a 10-year follow-up study. Sci. Rep. 2024, 14, 5619. [Google Scholar] [CrossRef]
- Stevenson, M.; Thompson, J.; de Sá, T.H.; Ewing, R.; Mohan, D.; McClure, R.; Roberts, I.; Tiwari, G.; Giles-Corti, B.; Sun, X.; et al. Land use, transport, and population health: Estimating the health benefits of compact cities. Lancet 2016, 388, 2925–2935. [Google Scholar] [CrossRef]
- Cao, X.; Tuerdi, N.; Tang, H.; Zhang, Y.; Wang, X.; Zheng, C.; Tian, Y.; Yu, X.; Pei, X.; Huang, G.; et al. Long-term exposure to residential greenness and cardiovascular disease and all-cause mortality in China. BMC Public Health 2025, 25, 1645. [Google Scholar] [CrossRef]
- Kim, J.; Lee, S.; Ramos, W. Investigating the Relationship Between Accessibility of Green Space and Adult Obesity Rates: A Secondary Data Analysis in the United States. J. Prev. Med. Public Health 2021, 54, 208–217. [Google Scholar] [CrossRef]
- Blekkenhorst, L.C.; Sim, M.; Bondonno, C.P.; Bondonno, N.P.; Ward, N.C.; Prince, R.L.; Devine, A.; Lewis, J.R.; Hodgson, J.M. Cardiovascular Health Benefits of Specific Vegetable Types: A Narrative Review. Nutrients 2018, 10, 595. [Google Scholar] [CrossRef]
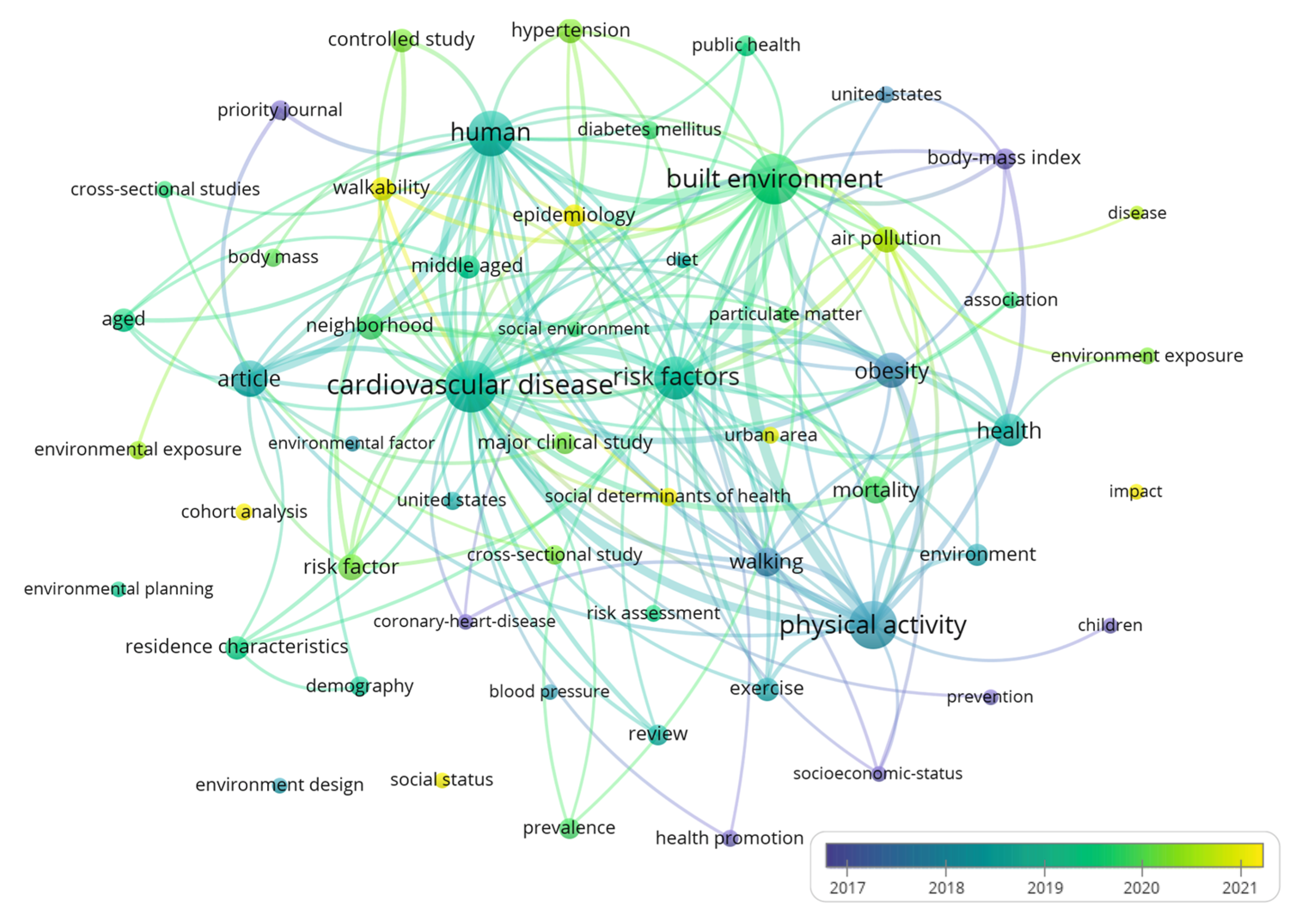
| Keywords | Weight (Total Link Strength) | Weight (Total Link Strength) | Score (Avg. Pub. Year) | |
|---|---|---|---|---|
| Health Outcomes | blood pressure | 437 | 25 | 2020 |
| body mass | 932 | 49 | 2020 | |
| cardiovascular disease | 2955 | 204 | 2021 | |
| cardiovascular risk | 1094 | 68 | 2018 | |
| cerebrovascular accident | 508 | 27 | 2021 | |
| diabetes mellitus | 842 | 50 | 2021 | |
| health disparity | 497 | 33 | 2021 | |
| health promotion | 465 | 37 | 2018 | |
| hypertension | 1167 | 70 | 2021 | |
| obesity | 1158 | 77 | 2019 | |
| mortality | 582 | 39 | 2020 | |
| risk factor | 1736 | 104 | 2020 | |
| Built Environment | built environment | 2980 | 229 | 2021 |
| environment | 593 | 40 | 2019 | |
| environmental exposure | 836 | 50 | 2021 | |
| environmental factor | 614 | 39 | 2019 | |
| environmental planning | 759 | 42 | 2019 | |
| city | 526 | 28 | 2021 | |
| air pollution | 654 | 49 | 2022 | |
| residence characteristics | 1647 | 97 | 2020 | |
| urban area | 800 | 47 | 2021 | |
| Demographics/Population Characteristics | very elderly | 488 | 25 | 2020 |
| smoking | 469 | 25 | 2019 | |
| social determinants of health | 665 | 50 | 2022 | |
| social environment | 497 | 35 | 2020 | |
| social status | 739 | 44 | 2021 | |
| socioeconomics | 617 | 34 | 2021 | |
| Lifestyle | walkability | 942 | 56 | 2022 |
| physical activity | 1773 | 127 | 2019 | |
| diet | 400 | 32 | 2018 | |
| lifestyle | 488 | 33 | 2020 | |
| health behavior | 499 | 32 | 2019 | |
| exercise | 978 | 70 | 2019 | |
| Research Method | controlled study | 1439 | 75 | 2021 |
| cross-sectional study | 1109 | 59 | 2020 | |
| regression analysis | 416 | 26 | 2019 | |
| major clinical study | 1345 | 69 | 2020 |
| Study | Location/Context | Study Design and Sample | Primary Outcome | Effect Size | Mechanism Evidence Quality | Mechanism Evidence Quality |
|---|---|---|---|---|---|---|
| Tamosiunas et al. [49] | Lithuania | Cohort study, Kaunas population | Lower CVD risk factors in park users | Qualitative improvement | Lifestyle and biological pathways | High |
| Wang et al. [65] | China | Cross-sectional, urban residents | Physical activity likelihood | 99% increase | Physical activity promotion | Moderate |
| Schäffer et al. [86] | Switzerland | Longitudinal, 190,000 postcode areas | Noise reduction | 6 dB (traffic), 3 dB (railway) | Noise pollution mitigation | High |
| de la Osa et al. [101] | Barcelona | Children study | Anxiety score reduction | 1.25 points (100 m), 1.86 points (500 m) per IQR | Psychological stress relief | Moderate |
| Hogendorf et al. [73] | General | Longitudinal study | Physical activity duration | 22.76 min/week decrease | Green space accessibility | Moderate |
| Chen et al. [68] | China | Older adults cohort | Mortality reduction | 54% all-cause, 52% CVD mortality reduction | Physical activity in green spaces | High |
| Study | Location | Transportation Focus | Key Findings | Effect Size |
|---|---|---|---|---|
| Celis-Morales et al. [70] | UK | Active commuting (walking/cycling) | Overall cardiovascular risk reduction through active travel modes | ↓ 11% |
| Yang et al. [109] | China | Walkability infrastructure | Walkability quality explains variance in green space usage frequency | 17.5% |
| Hogendorf et al. [73] | General | Green space accessibility | Distance from green space negatively affects leisure-time physical activity | ↓ 22.76 min/week per 100 m |
| Rissel. [116] | Global | COVID-19 mobility changes | Pandemic-related reductions in personal vehicle use and electricity consumption decreased air pollution-related premature deaths | ↓ 360 cases (25% baseline) |
| Study | Location | Environmental Factor | Key Findings | Effect Size |
|---|---|---|---|---|
| China CVD Report (2019) [117] | China | Living space quality | Adults with depression face elevated CHD risk; urban residents exhibit significantly higher susceptibility | Qualitative increase |
| Hayward et al. (2015) [57] | United States | Housing quality | Poor housing conditions undermine residents’ trust in social relationships, leading to social isolation and adverse mental health effects | Qualitative deterioration |
| Danish Survey [32] | Denmark | Food environment | Number of fast food outlets within 1 km of residence associated with significantly higher odds of fast food consumption | Significant positive association |
| UK Neighborhood Study [107] | United Kingdom | Food outlet ratio | Neighborhoods with highest fast food to community food outlet ratio showed increased obesity risk | 1.84-fold increase |
| Moore et al. [83] | United States | Fast food exposure | Each standard deviation increase in fast food exposure decreased odds of maintaining healthy diet | ↓ 12–17% healthy diet odds |
| Stevenson M. [124] | Global cities comparison | Urban planning compactness | More compact urban planning associated with reduced CVD prevalence across six representative cities | Significant reduction |
| Shen Y.S. et al. [37] | Multiple cities | Land use mixing | Reasonable functional land-use mixing effectively lowers CVD mortality; maximizing mixed land use while minimizing urban sprawl reduces cardiovascular mortality | Significant mortality reduction |
| Mechanistic Pathway | Representative Effect Size | 95% CI | Evidence Sources | Methodological Robustness Grade | Evidence Tier |
|---|---|---|---|---|---|
| Physical Activity Promotion | 52–54% mortality reduction | 48–58% | 6 high-quality studies | High | Tier 1 |
| Green Space Exposure | 99% activity likelihood increase/hectare | 68–142% | 3 cohort studies | Moderate | Tier 1 |
| Active Commuting | 11% cardiovascular risk reduction | 5–16% | Meta-analysis | High | Tier 1 |
| Noise Mitigation | 6 dB traffic noise reduction | 4–8 dB | Large-scale study | High | Tier 2 |
| Air Quality Improvement | Per 10 μg /m3 PM2.5 reduction | Highly variable | Multiple studies | Moderate | Tier 2 |
| Food Environment | 1.84-fold obesity risk increase | 1.3–2.6-fold | Cross-sectional studies | Low | Tier 3 |
| Research Domain | High Quality Evidence | Moderate Quality Evidence | Key Research Gaps | Priority Recommendations |
|---|---|---|---|---|
| Green Spaces | Swiss postcode study (190,000 areas) [86]; Kaunas longitudinal cohort [49]; Studies with dose-response data | Cross-sectional studies; Regional surveys with limited follow-up | Long-term intervention studies in Chinese contexts; Mechanistic pathway studies; Cost-effectiveness data | Randomized controlled trials of green space interventions; Chinese urban-specific dose-response studies |
| Transportation Systems | UK Biobank multi-country analysis [71]; Global COVID-19 natural experiment [116]; Large-scale cohort studies | Single-city studies; Cross-sectional designs; Limited temporal coverage | Chinese-specific active transportation data; Policy effectiveness in rapid urbanization contexts; Infrastructure impact evaluation | Longitudinal evaluation of transportation policy changes; Chinese urban mobility intervention studies |
| Food Environment | Danish population survey (n = 48,305) [32]; UK multi-site obesity study [107]; Large-scale dietary assessments | Single-city case studies; Limited geographic representation; Short-term follow-up | Urban-rural food environment comparisons in China; Intervention effectiveness data; Policy implementation outcomes | Community-based food environment interventions; Chinese dietary transition studies |
| Urban Planning | Mixed-method studies combining quantitative health outcomes with urban metrics [31,118]; Multi-city comparative analyses | Case studies of individual cities; Limited outcome measures; Cross-sectional designs | Mechanistic pathway studies linking planning to health; Cost-effectiveness analyses; Long-term health tracking | Integrated planning approach evaluations; Chinese rapid urbanization impact studies |
| Overall Evidence Base | Consistent protective effects across multiple environmental factors; Convergent findings from diverse methodological approaches | Geographic concentration in developed countries; Limited intervention studies; Short follow-up periods | Comprehensive built environment intervention studies; Limited evidence from rapidly urbanizing Chinese cities; Few policy effectiveness evaluations | Multi-domain integrated interventions; Chinese urbanization health impact research; Policy implementation effectiveness studies |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, W.; Li, J.; Li, Y.; Xu, Y.; Liu, P. The Role of Urban Built Environment in Enhancing Cardiovascular Health in Chinese Cities: A Systematic Review. Buildings 2025, 15, 3364. https://doi.org/10.3390/buildings15183364
Zhao W, Li J, Li Y, Xu Y, Liu P. The Role of Urban Built Environment in Enhancing Cardiovascular Health in Chinese Cities: A Systematic Review. Buildings. 2025; 15(18):3364. https://doi.org/10.3390/buildings15183364
Chicago/Turabian StyleZhao, Wenyu, Jialei Li, Yu Li, Yuejia Xu, and Pinghao Liu. 2025. "The Role of Urban Built Environment in Enhancing Cardiovascular Health in Chinese Cities: A Systematic Review" Buildings 15, no. 18: 3364. https://doi.org/10.3390/buildings15183364
APA StyleZhao, W., Li, J., Li, Y., Xu, Y., & Liu, P. (2025). The Role of Urban Built Environment in Enhancing Cardiovascular Health in Chinese Cities: A Systematic Review. Buildings, 15(18), 3364. https://doi.org/10.3390/buildings15183364








