The Relationship Between Ventilation and Building-Related Symptoms in Modern High-Performance Japanese Houses: A Cross-Sectional Study Using Building-Specification Data
Abstract
1. Introduction
2. Materials and Methods
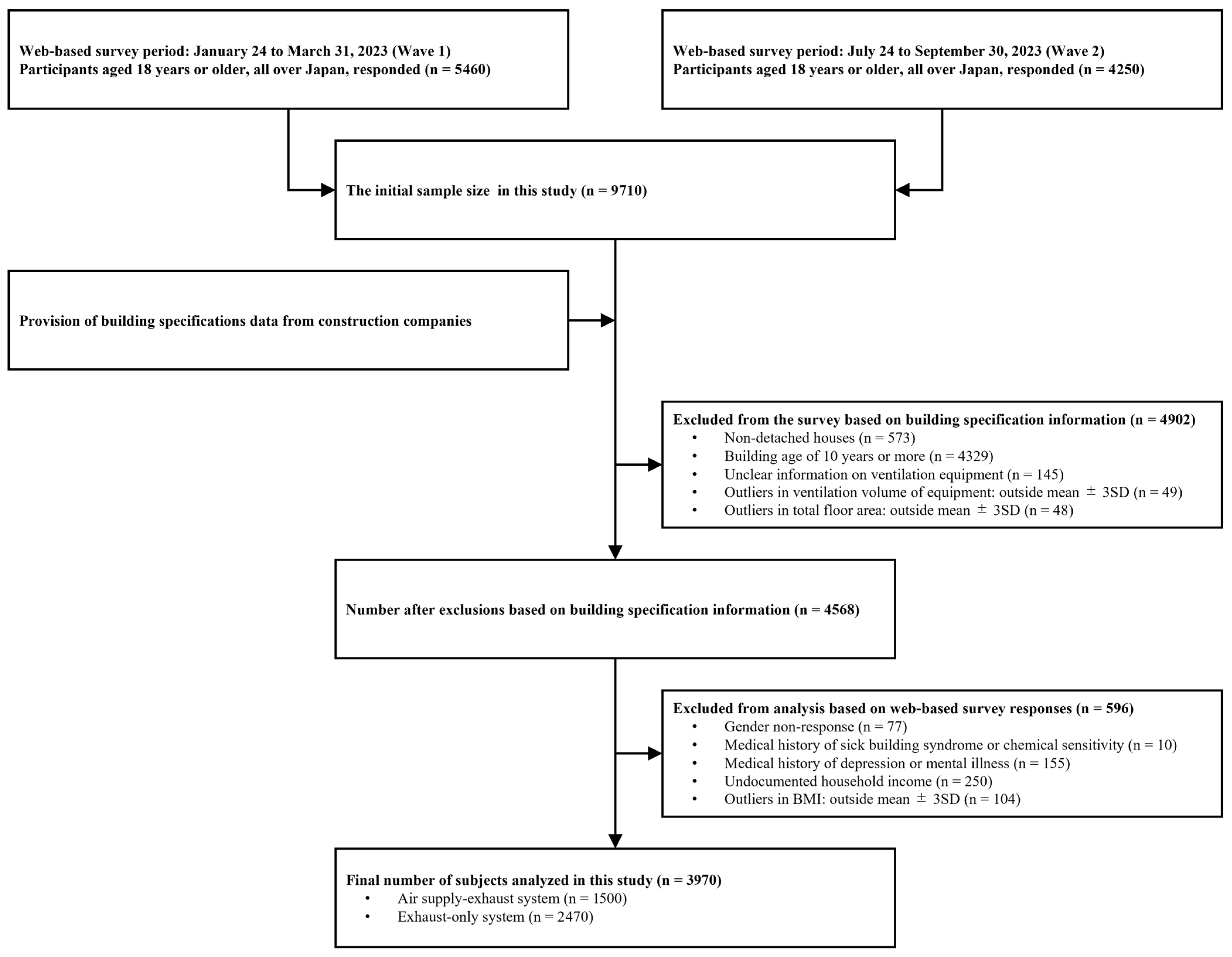
2.1. Study Design, Setting, Participants, and Period
2.2. Outcome Variables
2.3. Ventilation
- Qf: the ventilation volume by floor area (m3/(h·m2));
- Q: the ventilation capacity of ventilation systems (m3/h);
- Atot: total floor area (m2).
- γ: the ratio of the living area to the total floor area (%);
- Aliv: the living area (m2).
- Qliv: the ventilation volume of the living room.
- Qp: the ventilation volume per person (m3/(h·person));
- N: the number of occupants (persons).
2.4. Independent Variables
2.5. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Dwelling Characteristics of ASE and EO Systems
3.3. BRSs for ASE and EO Systems
3.4. The Relationship Between Ventilation Volume per Floor Area and BRSs
3.5. Relationship Between Ventilation Volume per Person and BRSs
4. Discussion
4.1. Ventilation Systems
4.2. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nordin, S. Mechanisms underlying nontoxic indoor air health problems: A review. Int. J. Hyg. Environ. Health 2020, 226, 113489. [Google Scholar] [CrossRef] [PubMed]
- Burge, P.S. Sick building syndrome. Occup. Environ. Med. 2004, 61, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Joshi, S. The sick building syndrome. Indian J. Occup. Environ. Med. 2008, 12, 61–64. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC2796751/ (accessed on 18 August 2025). [CrossRef] [PubMed]
- Cedeño-Laurent, J.; Williams, A.; MacNaughton, P.; Cao, X.; Eitland, E.; Spengler, J.; Allen, J. Building Evidence for Health: Green Buildings, Current Science, and Future Challenges. Annu. Rev. Public Health 2018, 39, 291–308. [Google Scholar] [CrossRef]
- Maung, T.Z.; Bishop, J.E.; Holt, E.; Turner, A.M.; Pfrang, C. Indoor Air Pollution and the Health of Vulnerable Groups: A Systematic Review Focused on Particulate Matter (PM), Volatile Organic Compounds (VOCs) and Their Effects on Children and People with Pre-Existing Lung Disease. Int. J. Environ. Res. Public Health 2022, 19, 8752. [Google Scholar] [CrossRef]
- Vu, T.V.; Stewart, G.B.; Kitwiroon, N.; Lim, S.; Barratt, B.; Kelly, F.J.; Thompson, R.; Smith, R.B.; Toledano, M.B.; Beevers, S.D. Assessing the contributions of outdoor and indoor sources to air quality in London homes of the SCAMP cohort. Build. Environ. 2022, 222, 109359. [Google Scholar] [CrossRef]
- Chen, C.; Zhao, B. Review of relationship between indoor and outdoor particles: I/O ratio, infiltration factor and penetration factor. Atmos. Environ. 2011, 45, 275–288. [Google Scholar] [CrossRef]
- Gupta, S.; Khare, M.; Goyal, R. Sick building syndrome—A case study in a multistory centrally air-conditioned building in the Delhi City. Build. Environ. 2007, 42, 2797–2809. [Google Scholar] [CrossRef]
- Hou, J.; Zhang, Y.; Sun, Y.; Wang, P.; Zhang, Q.; Kong, X.; Sundell, J. Air change rates at night in northeast Chinese homes. Build. Environ. 2018, 132, 273–281. [Google Scholar] [CrossRef]
- Gonzalo Fdel, A.; Griffin, M.; Laskosky, J.; Yost, P.; González-Lezcano, R.A. Assessment of Indoor Air Quality in Residential Buildings of New England through Actual Data. Sustainability 2022, 14, 739. [Google Scholar] [CrossRef]
- Chen, Q. Ventilation performance prediction for buildings: A method overview and recent applications. Build. Environ. 2009, 44, 848–858. [Google Scholar] [CrossRef]
- Li, Y.; Leung, G.M.; Tang, J.W.; Yang, X.; Chao, C.Y.H.; Lin, J.Z.; Lu, J.W.; Nielsen, P.V.; Niu, J.; Qian, H.; et al. Role of ventilation in airborne transmission of infectious agents in the built environment? A multidisciplinary systematic review. Indoor Air 2007, 17, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Lin, Z.; Wang, T.; Norback, D.; Kan, H.; Sundell, J.; Zhao, Z. Sick building syndrome, perceived odors, sensation of air dryness and indoor environment in Urumqi, China. Chin. Sci. Bull. 2014, 59, 5153–5160. [Google Scholar] [CrossRef]
- Sun, Y.; Hou, J.; Cheng, R.; Sheng, Y.; Zhang, X.; Sundell, J. Indoor air quality, ventilation and their associations with sick building syndrome in Chinese homes. Energy Build. 2019, 197, 112–119. [Google Scholar] [CrossRef]
- Kishi, R.; Saijo, Y.; Kanazawa, A.; Tanaka, M.; Yoshimura, T.; Chikara, H.; Takigawa, T.; Morimoto, K.; Nakayama, K.; Shibata, E. Regional differences in residential environments and the association of dwellings and residential factors with the sick house syndrome: A nationwide cross-sectional questionnaire study in Japan. Indoor Air 2009, 19, 243–254. [Google Scholar] [CrossRef]
- Kanazawa, A.; Saito, I.; Araki, A.; Takeda, M.; Ma, M.; Saijo, Y.; Kishi, R. Association between indoor exposure to semi-volatile organic compounds and building-related symptoms among the occupants of residential dwellings. Indoor Air 2010, 20, 72–84. [Google Scholar] [CrossRef]
- Kishi, R.; Ketema, R.M.; Bamai, Y.A.; Araki, A.; Kawai, T.; Tsuboi, T.; Saito, I.; Yoshioka, E.; Saito, T. Indoor environmental pollutants and their association with sick house syndrome among adults and children in elementary school. Build. Environ. 2018, 136, 293–301. [Google Scholar] [CrossRef]
- Lim, A.-Y.; Yoon, M.; Kim, E.-H.; Kim, H.-A.; Lee, M.J.; Cheong, H.-K. Effects of mechanical ventilation on indoor air quality and occupant health status in energy-efficient homes: A longitudinal field study. Sci. Total Environ. 2021, 785, 147324. [Google Scholar] [CrossRef]
- Smedje, G.; Wang, J.; Norbäck, D.; Nilsson, H.; Engvall, K. SBS symptoms in relation to dampness and ventilation in inspected single-family houses in Sweden. Int. Arch. Occup. Environ. Health 2017, 90, 703–711. [Google Scholar] [CrossRef]
- Engvall, K.; Norrby, C.; Norbäck, D. Ocular, nasal, dermal and respiratory symptoms in relation to heating, ventilation, energy conservation, and reconstruction of older multi-family houses. Indoor Air 2003, 13, 206–211. [Google Scholar] [CrossRef]
- Andersson, K. Epidemiological Approach to Indoor Air Problems. Indoor Air 1998, 8, 32–39. [Google Scholar] [CrossRef]
- Mizoue, T. Environmental Tobacco Smoke Exposure and Overtime Work as Risk Factors for Sick Building Syndrome in Japan. Am. J. Epidemiol. 2001, 154, 803–808. [Google Scholar] [CrossRef]
- Suzuki, N.; Nakayama, Y.; Nakaoka, H.; Takaguchi, K.; Tsumura, K.; Hanazato, M.; Hayashi, T.; Mori, C. Risk factors for the onset of sick building syndrome: A cross-sectional survey of housing and health in Japan. Build Environ. 2021, 202, 107976. [Google Scholar] [CrossRef]
- Chen, C.-F.; Hsu, C.-H.; Chang, Y.-J.; Lee, C.-H.; Lee, D.L. Efficacy of HEPA Air Cleaner on Improving Indoor Particulate Matter 2.5 Concentration. Int. J. Environ. Res. Public Health 2022, 19, 11517. [Google Scholar] [CrossRef]
- Gao, X.; Xu, Y.; Cai, Y.; Shi, J.; Chen, F.; Lin, Z.; Chen, T.; Xia, Y.; Shi, W.; Zhao, Z. Effects of filtered fresh air ventilation on classroom indoor air and biomarkers in saliva and nasal samples: A randomized crossover intervention study in preschool children. Environ. Res. 2019, 179, 108749. [Google Scholar] [CrossRef]
- Batterman, S.; Godwin, C.; Jia, C. Long Duration Tests of Room Air Filters in Cigarette Smokers’ Homes. Environ. Sci. Technol. 2005, 39, 7260–7268. [Google Scholar] [CrossRef]
- Shin, D.; Kim, Y.; Hong, K.-J.; Lee, G.; Park, I.; Kim, H.-J.; Kim, S.; Hwang, C.-H.; Noh, K.-C.; Han, B. The Effectiveness of a Mechanical Ventilation System for Indoor PM2.5 in Residential Houses. Toxics 2023, 11, 912. [Google Scholar] [CrossRef]
- Lee, D.; Kim, Y.; Hong, K.-J.; Lee, G.; Kim, H.-J.; Shin, D.; Han, B. Strategies for Effective Management of Indoor Air Quality in a Kindergarten: CO2 and Fine Particulate Matter Concentrations. Toxics 2023, 11, 931. [Google Scholar] [CrossRef]
- Antonopoulos, C.; Dillon, H.E.; Gall, E. Experimental and Modeled Assessment of Interventions to Reduce PM2.5 in a Residence during a Wildfire Event. Pollutants 2024, 4, 26–41. [Google Scholar] [CrossRef]
- Bokkers, E.A.M.; van Zanten, H.H.E.; van den Brand, H. Field study on effects of a heat exchanger on broiler performance, energy use, and calculated carbon dioxide emission at commercial broiler farms, and the experiences of farmers using a heat exchanger. Poult. Sci. 2010, 89, 2743–2750. [Google Scholar] [CrossRef] [PubMed]
- Coskun, A.; Yalin, H.; Atmaca, I. Analysis of direct expansion heat recovery ventilation devices by orthogonal optimization method. J. Therm. Anal. Calorim. 2023, 148, 5625–5635. [Google Scholar] [CrossRef]
- Grisoli, P.; Albertoni, M.; Rodolfi, M. Application of Airborne Microorganism Indexes in Offices, Gyms, and Libraries. Appl. Sci. 2019, 9, 1101. [Google Scholar] [CrossRef]
- Hiipakka, D.W.; Buffington, J.R. Resolution of Sick Building Syndrome in a High-Security Facility. Appl. Occup. Environ. Hyg. 2000, 15, 635–643. [Google Scholar] [CrossRef]
- Mendell, M.J.; Lei-Gomez, Q.; Mirer, A.G.; Seppnen, O.; Brunner, G. Risk factors in heating, ventilating, and air-conditioning systems for occupant symptoms in US office buildings: The US EPA BASE study. Indoor Air 2008, 18, 301–316. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labour and Welfare. Manual for Measuring Indoor Airborne Chemicals. Available online: https://www.mhlw.go.jp/content/11120000/001376419.pdf (accessed on 11 March 2025).
- Tomoaki, S.; Ngo Thi Thu, H. A case study on the room temperature and residents’ choice of living space in the home in summer. J. Fac. Edu. Saga Univ. 2016, 20, 73–82. Available online: https://saga-u.repo.nii.ac.jp/records/21614 (accessed on 28 June 2025).
- Falkenberg, H.K.; Kvikstad, T.M.; Eilertsen, G. Improved indoor lighting improved healthy aging at home—An intervention study in 77-year-old Norwegians. J. Multidiscip. Healthc. 2019, 12, 315–324. [Google Scholar] [CrossRef]
- Ministry of Land, Infrastructure and Transport. The Amended Building Standard Law on Sick House Issues. 2003. Available online: https://www.mlit.go.jp/english/housing_bureau/law/index.html (accessed on 18 August 2025).
- Ministry of Land, Infrastructure, Transport and Tourism. Sick House Measures Based on the Building Standard Law. 2003. Available online: https://www.mlit.go.jp/jutakukentiku/build/jutakukentiku_house_tk_000043.html (accessed on 29 March 2025).
- UNECE. About the GHS. Available online: https://unece.org/about-ghs (accessed on 12 March 2025).
- Ministry of Health, Labour and Welfare. Building Environmental Hygiene Management Standards. Available online: https://www.mhlw.go.jp/bunya/kenkou/seikatsu-eisei10/ (accessed on 9 March 2025).
- Ministry of Health, Labour and Welfare. Required Ventilation Volume for Indoor Air Quality. Available online: https://www.mhlw.go.jp/content/11130500/000771220.pdf (accessed on 9 March 2025).
- Umweltbundesamt (German Environment Agency). German Committee on Indoor Air Guide Values. 2025. Available online: https://www.umweltbundesamt.de/en/topics/health/commissions-working-groups/german-committee-on-indoor-air-guide-values#definition-of-039indoor-environment039- (accessed on 28 June 2025).
- ASHRAE Standard 62.1: Ventilation for Acceptable Indoor Air Quality. Available online: https://www.ashrae.org/technical-resources/bookstore/standards-62-1-62-2 (accessed on 11 March 2025).
- Gosling, S.D.; Rentfrow, P.J.; Swann, W.B. A very brief measure of the Big-Five personality domains. J. Res. Pers. 2003, 37, 504–528. [Google Scholar] [CrossRef]
- Barmark, M. Social determinants of the sick building syndrome: Exploring the interrelated effects of social position and psychosocial situation. Int. J. Environ. Health Res. 2015, 25, 490–507. [Google Scholar] [CrossRef] [PubMed]
- Oshio, A.; Abe, S.; Cutrone, P. Development, Reliability, and Validity of the Japanese Version of Ten Item Personality Inventory (TIPI-J). Jpn. J. Personal. 2012, 21, 40–52. [Google Scholar] [CrossRef]
- Japan Meteorological Agency. General Information on Climate of Japan. Available online: https://www.data.jma.go.jp/gmd/cpd/longfcst/en/tourist.html (accessed on 18 August 2025).
- Umishio, W.; Ikaga, T.; Kario, K.; Fujino, Y.; Kagi, N.; Suzuki, M.; Ando, S.; Saeki, K.; Murakami, S. Effect of living in well-insulated warm houses on hypertension and cardiovascular diseases based on a nationwide epidemiological survey in Japan: A modelling and cost-effectiveness analysis. BMJ Public Health 2024, 2, e001143. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare. Recommended Ventilation Method for Resolving ‘Poorly Ventilated Closed Spaces’. Available online: https://www.mhlw.go.jp/content/000678601.pdf (accessed on 12 March 2025).
- Seppänen, O.A. Association of ventilation rates and CO2 concentrations with health and other responses in commercial and institutional buildings. Indoor Air 1999, 9, 226–252. [Google Scholar] [CrossRef] [PubMed]
- Fisk, W.J.; Mirer, A.G.; Mendell, M.J. Quantitative relationship of sick building syndrome symptoms with ventilation rates. Indoor Air 2009, 19, 159–165. [Google Scholar] [CrossRef]
- Sundell, J.; Levin, H.; Nazaroff, W.W.; Cain, W.S.; Fisk, W.J.; Grimsrud, D.T.; Gyntelberg, F.; Li, Y.; Persily, A.K.; Pickering, A.C.; et al. Ventilation rates and health: Multidisciplinary review of the scientific literature. Indoor Air 2011, 21, 191–204. [Google Scholar] [CrossRef]
- Maula, H.; Hongisto, V.; Naatula, V.; Haapakangas, A.; Koskela, H. The effect of low ventilation rate with elevated bioeffluent concentration on work performance, perceived indoor air quality, and health symptoms. Indoor Air 2017, 27, 1141–1153. [Google Scholar] [CrossRef]
- Petersen, S.; Jensen, K.L.; Pedersen, A.L.S.; Rasmussen, H.S. The effect of increased classroom ventilation rate indicated by reduced CO2 concentration on the performance of schoolwork by children. Indoor Air 2016, 26, 366–379. [Google Scholar] [CrossRef]
- ANSES. Concentrations de CO2 Dans L’air Intérieur et Effets Sur la Santé. 2013. Available online: https://www.anses.fr/fr/system/files/AIR2012sa0093Ra.pdf (accessed on 18 August 2025).
- Naclerio, R.M.; Bachert, C.; Baraniuk, J.N. International Journal of General Medicine Pathophysiology of Nasal Congestion. 2010. Available online: https://www.dovepress.com/ (accessed on 18 August 2025).
- Watanabe, T.; Takahashi, N.; Minaguchi, J.; Mochizuki, A.; Hiramatsu, K. Three-Dimensional Analysis of the Nasolacrimal Duct and Nasal Cavity and Arrangement of Mucosal Tissue in Chickens. J. Poult. Sci. 2020, 57, 303–309. [Google Scholar] [CrossRef]
- Japan Weather Association. JWA 2024 Spring Pollen Dispersion Forecast (Part 1) ~The Cedar Pollen Season to Start Soon, Peaking from Late February~. 2024. Available online: https://www.jwa.or.jp/wp-content/uploads/2024/03/Pollen-Dispersion-Forecasts_2024_01-1.pdf (accessed on 18 August 2025).
- Jung, C.-R.; Chen, W.-T.; Nakayama, S.F. A National-Scale 1-km Resolution PM2.5 Estimation Model over Japan Using MAIAC AOD and a Two-Stage Random Forest Model. Remote Sens. 2021, 13, 3657. [Google Scholar] [CrossRef]
- Kuramochi, M.; Kajino, M.; Ueda, H. Interannual Variability of Dust Deposition in Japan during Spring Season and Related Atmospheric Circulation Fields. J. Meteorol. Soc. Jpn. Ser. II 2023, 101, 255–270. [Google Scholar] [CrossRef]
- Qiao, R.; Lou, X.; Sun, Y.; Liu, Y. Effects of occupant behaviors on perceived dormitory air quality and sick building syndrome symptoms among female college students. Indoor Air 2022, 32, e13153. [Google Scholar] [CrossRef] [PubMed]
- Azuma, K.; Ikeda, K.; Kagi, N.; Yanagi, U.; Osawa, H. Evaluating prevalence and risk factors of building-related symptoms among office workers: Seasonal characteristics of symptoms and psychosocial and physical environmental factors. Environ. Health Prev. Med. 2017, 22, 1–14. [Google Scholar] [CrossRef]
- Takada, S. Influence of temperature and humidity of ambient air on sensation of dryness during respiration. J. Hum. Environ. Syst. 2020, 23, 31–43. [Google Scholar] [CrossRef]
- Goad, N.; Gawkrodger, D.J. Ambient humidity and the skin: The impact of air humidity in healthy and diseased states. J. Eur. Acad. Dermatol. Venereol. 2016, 30, 1285–1294. [Google Scholar] [CrossRef] [PubMed]
- Japan Meteorological Agency. Climate of Japan. Available online: https://www.data.jma.go.jp/stats/data/en/index.html (accessed on 12 March 2025).
| ASE System (n = 1500) | EO System (n = 2470) | |||
|---|---|---|---|---|
| Number (%) | ||||
| Gender | ||||
| Male | 1068 | (71.2) | 1714 | (69.4) |
| Female | 432 | (28.8) | 756 | (30.6) |
| Age group | ||||
| 20–29 | 128 | (8.5) | 65 | (2.6) |
| 30–39 | 684 | (45.6) | 778 | (31.5) |
| 40–49 | 391 | (26.1) | 805 | (32.6) |
| 50–59 | 164 | (10.9) | 415 | (16.8) |
| ≥60 | 133 | (8.9) | 407 | (16.5) |
| BMI a | ||||
| <18.5 | 93 | (6.2) | 171 | (6.9) |
| 18.5−<25 | 1064 | (70.9) | 1790 | (72.5) |
| ≥25 | 343 | (22.9) | 509 | (20.6) |
| Medical history | ||||
| Yes | 745 | (49.7) | 1180 | (47.8) |
| Household income (million yen) | ||||
| <400 | 60 | (4.0) | 182 | (7.4) |
| 400–<800 | 854 | (56.9) | 1450 | (58.7) |
| ≥800 | 586 | (39.1) | 838 | (33.9) |
| Smoker | ||||
| Yes | 197 | (13.1) | 298 | (12.1) |
| Neuroticism tendency | ||||
| ≤7 | 656 | (43.7) | 1075 | (43.5) |
| 8–9 | 515 | (34.3) | 919 | (37.2) |
| ≥10 | 329 | (21.9) | 476 | (19.3) |
| Number of household members b | ||||
| Single | 15 | (1.0) | 35 | (1.4) |
| 2 | 388 | (25.9) | 531 | (21.5) |
| 3 | 490 | (32.7) | 625 | (25.3) |
| 4 | 422 | (28.1) | 839 | (34.0) |
| 5 | 158 | (6.4) | 397 | (16.1) |
| 6 | 27 | (1.1) | 43 | (1.7) |
| Building age | ||||
| <3 | 1212 | (80.8) | 553 | (22.4) |
| 3–<5 | 124 | (8.3) | 663 | (26.8) |
| 5–<10 | 164 | (10.9) | 1254 | (50.8) |
| Regional classification | ||||
| ≤3 | 79 | (5.3) | 4 | (0.2) |
| 4 | 163 | (10.9) | 36 | (1.5) |
| 5 | 278 | (18.5) | 296 | (12.0) |
| 6 | 861 | (57.4) | 1858 | (75.2) |
| 7 | 119 | (7.9) | 276 | (11.2) |
| Insulation grade | ||||
| 4 | 53 | (3.5) | 513 | (20.8) |
| 5 | 1437 | (95.8) | 1938 | (78.5) |
| 6 | 10 | (0.7) | 19 | (0.8) |
| Structure | ||||
| Steel frame | 946 | (63.1) | 1542 | (62.4) |
| Wooden | 554 | (36.9) | 928 | (37.6) |
| Season | ||||
| Winter | 941 | (62.7) | 1533 | (62.1) |
| Summer | 559 | (37.3) | 937 | (37.9) |
| mean (SD) | ||||
| Total floor area (m2) | 129.4 | (31.0) | 130.1 | (30.6) |
| Living room area (m2) | 35.1 | (7.0) | 31.6 | (7.1) |
| Ventilation volume (m3/h) | 153.3 | (34.3) | 139.3 | (34.1) |
| ASE System | EO System | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year-Round | Winter | Summer | Year-Round | Winter | Summer | |||||||
| General symptoms a,b | 103 | (6.9) | 60 | (6.4) | 43 | (7.7) | 153 | (6.2) | 101 | (6.6) | 52 | (5.5) |
| Fatigue | 61 | (4.1) | 31 | (3.3) | 30 | (5.4) | 95 | (3.8) | 61 | (4.0) | 34 | (3.6) |
| Heaviness in the head | 38 | (2.5) | 25 | (2.7) | 13 | (2.3) | 61 | (2.5) | 41 | (2.7) | 20 | (2.1) |
| Headache | 37 | (2.5) | 23 | (2.4) | 14 | (2.5) | 69 | (2.8) | 48 | (3.1) | 21 | (2.2) |
| Nausea/dizziness | 8 | (0.5) | 5 | (0.5) | 3 | (0.5) | 28 | (1.1) | 16 | (1.0) | 12 | (1.3) |
| Difficulty concentrating | 46 | (3.1) | 29 | (3.1) | 17 | (3.0) | 74 | (3.0) | 48 | (3.1) | 26 | (2.8) |
| Mucosal irritation symptoms a,b | 169 | (11.3) | 115 | (12.2) | 54 | (9.7) | 259 | (10.5) | 173 | (11.3) | 86 | (9.2) |
| Itchy eyes | 55 | (3.7) | 36 | (3.8) | 19 | (3.4) | 96 | (3.9) | 69 | (4.5) | 27 | (2.9) |
| Runny/stuffy nose | 107 | (7.1) | 75 | (8.0) | 32 | (5.7) | 176 | (7.1) | 109 | (7.1) | 67 | (7.2) |
| Cough | 99 | (6.6) | 69 | (7.3) | 30 | (5.4) | 132 | (5.3) | 94 | (6.1) | 38 | (4.1) |
| Skin dryness symptoms a,b | 333 | (22.2) | 251 | (26.7) | 82 | (14.7) | 428 | (17.3) | 328 | (21.4) | 100 | (10.7) |
| Dry throat | 235 | (15.7) | 170 | (18.1) | 65 | (11.6) | 281 | (11.4) | 209 | (13.6) | 72 | (7.7) |
| Dryness of the face | 103 | (6.9) | 89 | (9.5) | 14 | (2.5) | 122 | (4.9) | 96 | (6.3) | 26 | (2.8) |
| Dryness of the scalp/ears | 79 | (5.3) | 65 | (6.9) | 14 | (2.5) | 115 | (4.7) | 85 | (5.5) | 30 | (3.2) |
| Dry hands | 176 | (11.7) | 153 | (16.3) | 23 | (4.1) | 226 | (9.1) | 182 | (11.9) | 44 | (4.7) |
| ASE System | EO System | |||
|---|---|---|---|---|
| χ2 | p | χ2 | p | |
| General symptoms | 0.76 | 0.385 | 0.91 | 0.341 |
| Mucosal irritation symptoms | 2.05 | 0.152 | 2.53 | 0.112 |
| Skin dryness symptoms | 28.57 | <0.001 | 45.94 | <0.001 |
| General Symptoms | Mucosal Irritation Symptoms | Skin Dryness Symptoms | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | ||
| ASE system (m3/(h·m2)) | ||||||||||
| Low | <0.43 | 1.00 | 1.00 | 1.00 | ||||||
| Middle | 0.43–<0.52 | 0.73 | (0.44–1.19) | 0.201 | 1.13 | (0.82–1.57) | 0.455 | 0.95 | (0.69–1.31) | 0.753 |
| High | ≥0.52 | 0.55 | (0.33–0.92) | 0.024 | 1.04 | (0.75–1.46) | 0.802 | 1.36 | (1.00–1.87) | 0.054 |
| p for trend | 0.019 | 0.919 | 0.032 | |||||||
| EO system (m3/(h·m2)) | ||||||||||
| Low | <0.41 | 1.00 | 1.00 | 1.00 | ||||||
| Middle | 0.41–<0.46 | 0.72 | (0.48–1.09) | 0.117 | 1.03 | (0.67–1.59) | 0.886 | 0.85 | (0.65–1.11) | 0.219 |
| High | ≥0.46 | 0.79 | (0.52–1.18) | 0.251 | 1.50 | (0.99–2.26) | 0.055 | 0.92 | (0.71–1.21) | 0.562 |
| p for trend | 0.376 | 0.030 | 0.568 | |||||||
| General Symptoms | Mucosal Irritation Symptoms | Skin Dryness Symptoms | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | ||
| ASE system (m3/(h·person)) | ||||||||||
| Low | <15.68 | 1.00 | 1.00 | 1.00 | ||||||
| Middle | 15.68–<22.08 | 0.52 | (0.32–0.86) | 0.011 | 0.84 | (0.55–1.28) | 0.416 | 1.02 | (0.74–1.41) | 0.911 |
| High | ≥22.08 | 0.46 | (0.27–0.77) | 0.003 | 0.93 | (0.61–1.41) | 0.728 | 1.31 | (0.95–1.81) | 0.104 |
| p for trend | 0.007 | 0.384 | 0.147 | |||||||
| EO system (m3/(h·person)) | ||||||||||
| Low | <11.71 | 1.00 | 1.00 | 1.00 | ||||||
| Middle | 11.71–<16.90 | 0.97 | (0.66–1.43) | 0.881 | 1.60 | (1.15–2.21) | 0.005 | 1.13 | (0.87–1.47) | 0.364 |
| High | ≥16.90 | 0.71 | (0.46–1.10) | 0.121 | 1.41 | (1.00–2.00) | 0.051 | 1.13 | (0.86–1.49) | 0.386 |
| p for trend | 0.135 | 0.050 | 0.379 | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iwayama, R.; Shimatani, K.; Nakayama, Y.; Takaguchi, K.; Nakaoka, H.; Suzuki, N.; Sakurai, K. The Relationship Between Ventilation and Building-Related Symptoms in Modern High-Performance Japanese Houses: A Cross-Sectional Study Using Building-Specification Data. Buildings 2025, 15, 3013. https://doi.org/10.3390/buildings15173013
Iwayama R, Shimatani K, Nakayama Y, Takaguchi K, Nakaoka H, Suzuki N, Sakurai K. The Relationship Between Ventilation and Building-Related Symptoms in Modern High-Performance Japanese Houses: A Cross-Sectional Study Using Building-Specification Data. Buildings. 2025; 15(17):3013. https://doi.org/10.3390/buildings15173013
Chicago/Turabian StyleIwayama, Ryotaro, Keiichi Shimatani, Yoshitake Nakayama, Kohki Takaguchi, Hiroko Nakaoka, Norimichi Suzuki, and Kenichi Sakurai. 2025. "The Relationship Between Ventilation and Building-Related Symptoms in Modern High-Performance Japanese Houses: A Cross-Sectional Study Using Building-Specification Data" Buildings 15, no. 17: 3013. https://doi.org/10.3390/buildings15173013
APA StyleIwayama, R., Shimatani, K., Nakayama, Y., Takaguchi, K., Nakaoka, H., Suzuki, N., & Sakurai, K. (2025). The Relationship Between Ventilation and Building-Related Symptoms in Modern High-Performance Japanese Houses: A Cross-Sectional Study Using Building-Specification Data. Buildings, 15(17), 3013. https://doi.org/10.3390/buildings15173013









