1. Introduction
Against the backdrop of accelerating global aging and frequent outbreaks of public health emergencies, traditional healthcare facilities are facing unprecedented pressure in resource allocation, service efficiency, and response capabilities [
1]. Especially at the community level, these challenges have driven the transformation of healthcare services from a “centralized” model to a “distributed” and “smart” one, spurring the emergence of community smart health spaces. Take Wuhan during the 2020 COVID-19 pandemic as an example: some communities lacked smart health monitoring and triage systems, leading to severe shortages of public healthcare resources in the early stages [
2]. However, in pilot regions like Hangzhou, smart health spaces integrating telemedicine, health big data management, and elderly-friendly facilities effectively alleviated the pressure on offline medical services [
3]. It is evident that community smart health spaces, as an indispensable part of community public services, lessen the pressure on large hospitals and provide essential basic medical services. However, the current community smart health spaces model is still relatively traditional and has not truly achieved “zero-distance” health services. Therefore, enhancing the smart service capabilities of community smart health spaces is critical.
In terms of policy, the Chinese government has successively issued policy documents such as “Healthy China 2030,” clearly stating that the coverage rate of “Internet + healthcare” services should reach 80% [
4,
5]. This policy provides strong policy support for the integration of “Internet + Healthcare” and smart communities [
6,
7].
In practice, current research on smart health spaces has made some progress. Korzun proposed a mobile health system that uses mobile communication devices to deliver healthcare services [
8]. Rajaei et al. explored the attributes of smart hospitals and proposed a definition based on this approach, considering both the academic and industrial perspectives [
9]. Lu et al. established an objective and comprehensive assessment system and evaluation method to guide the design of innovative health products [
10]. However, most existing studies focus on a single dimension and lack a systematic theoretical framework from strategic planning to spatial design. This limitation restricts the’ overall optimization and practical application of smart health spaces.
This paper takes the community intelligent health space as the research object in this context. It proposes a “SWOT–four orders of design–AHP–TOPSIS” quadratic fusion hybrid model to realize the whole process path from a strategic environmental analysis, space logic construction, user needs assessment, and design preference. It seeks to discover the entire process path from a strategic environmental analysis, space logic construction, and user needs assessment to design optimization. Unlike the traditional practice of relying only on empirical judgment or a single technical model, the model integrates qualitative and quantitative methods to open up the logically closed loop from macro policy to micro-spatial design, which is systematic, scientific, and replicable.
The innovations of this study are that for the first time, SWOT strategy identification, the four orders of design spatial logic, AHP assessment tool, and TOPSIS preference model are integrated to realize the closed-loop process from a pre-design assessment, spatial element construction, and user cognitive weight extraction to multi-scenario screening; meanwhile, the modularized and intelligent movable healthcare unit is introduced to validate its responsive adaptability in high-risk scenarios, which provides paradigm support for an intelligent health infrastructure for cross-scenario applications. The research objectives of this study include the following:
Analyzing the characteristics of community residents’ demand for health services;
Constructing smart health spaces with modular and movable features;
Validating the feasibility of the “SWOT–four orders of design–AHP–TOPSIS” model in design practice.
In summary, the “SWOT–four orders of design–AHP–TOPSIS” comprehensive assessment model constructed in this study not only provides a systematic, quantitative, and replicable solution for the design of smart health spaces but also provides a theoretical framework and practical paradigm that can be popularized for the construction of smart health spaces in multiple scenarios, such as elderly care, rehabilitation, and emergency responses. It also provides a theoretical framework and practical paradigm for the future construction of a smart health space in multiple scenarios, such as elderly care, rehabilitation, and emergency responses, which is of great practical significance in promoting the high-quality development of an innovative health service system [
11]. Subsequent chapters will be organized as follows: the second part is the literature review, the third part is the research methodology, the fourth part is the research findings, and the fifth part is the conclusions.
2. Literature Review
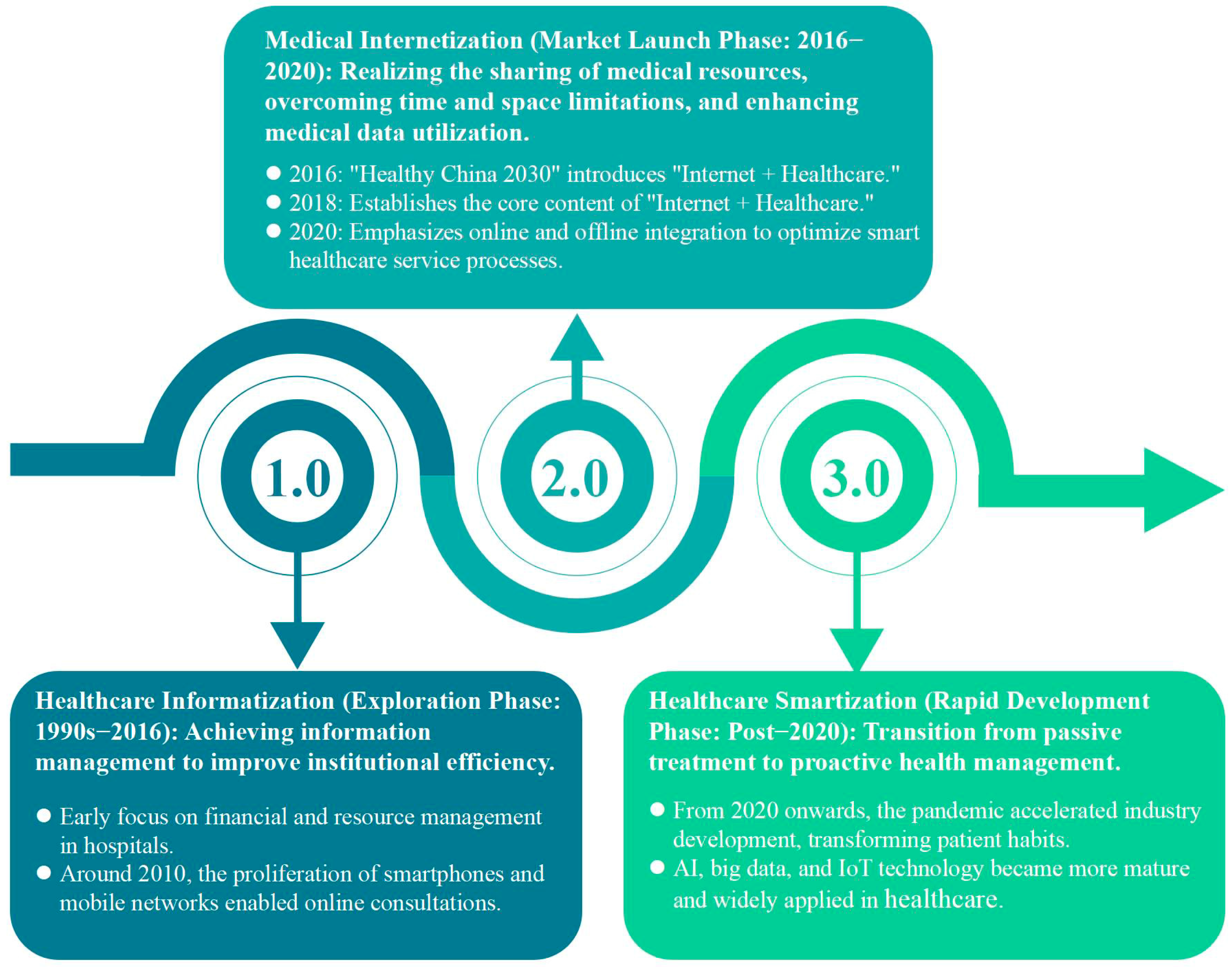
2.1. Smart Healthy Spaces in China: Current Status
With China’s sustained economic growth and rising living standards, the public’s demand for healthcare services is becoming increasingly diverse, and their expectations for the quality of healthcare services are also increasing [
12,
13]. Especially in the post-pandemic era, community healthcare is undergoing a profound shift in residents’ lifestyles and health management concepts [
14]. Competent healthcare has built a digital service platform by integrating community healthcare services with information technology, realizing the sharing of health information and the online and offline collaboration of healthcare services [
15,
16]. This improves the healthcare experience, alleviates the disparities caused by an uneven distribution of healthcare resources [
17,
18], and promotes healthcare equity and public health literacy [
19]. Based on this background, this paper takes the opportunities and challenges of community healthcare development in China as an entry point. It proposes the research idea of constructing a mobile intelligent health space to cope with the sustainable upgrading of the future healthcare service system [
20] (
Figure 1).
2.2. Theoretical Framework
2.2.1. SWOT Analysis
In the system design process of a smart community health space, choosing the appropriate analysis method is crucial to improving the scientificity and user satisfaction of the program [
21,
22]. To solve the complex multidimensional problems in the design, this paper comprehensively adopts SWOT analysis, four orders of design theory, AHP hierarchical analysis, and TOPSIS preference model to form a closed-loop path of “qualitative analysis–spatial construction–weighted decision-making–program ranking.” The closed-loop path of “qualitative analysis–space construction–weighting decision-making–scheme ranking” is formed to realize whole-process guidance for smart health spaces from strategy identification to space execution.
A SWOT analysis is often used in a pre-design feasibility analysis [
23,
24]. Beyhan and Alagoz, through a SWOT analysis, aim to identify strengths, weaknesses, opportunities, and threatening aspects of the current approach to designing building envelopes. Attempts were made to transform weaknesses into strengths. Gontier, J.C. et al., to determine the current state of immersive technology adoption in buildings, conducted a systematic overview and thematic analysis using the SWOT tool [
25]. In their research, identifying strengths, weaknesses, opportunities, and threatening factors was considered critical for the success of the smart campus transformation. Awuzie, B et al., considered the SWOT analysis methodology an effective decision-making aid that facilitates the sequencing of matters [
26].
In the design of community smart and healthy spaces, a SWOT analysis can identify key development directions in terms of macro policies, market trends, resource conditions, and other dimensions. However, it mainly provides directional judgments and lacks a refined implementation path; so, it needs to be used in conjunction with other quantitative methods [
27].
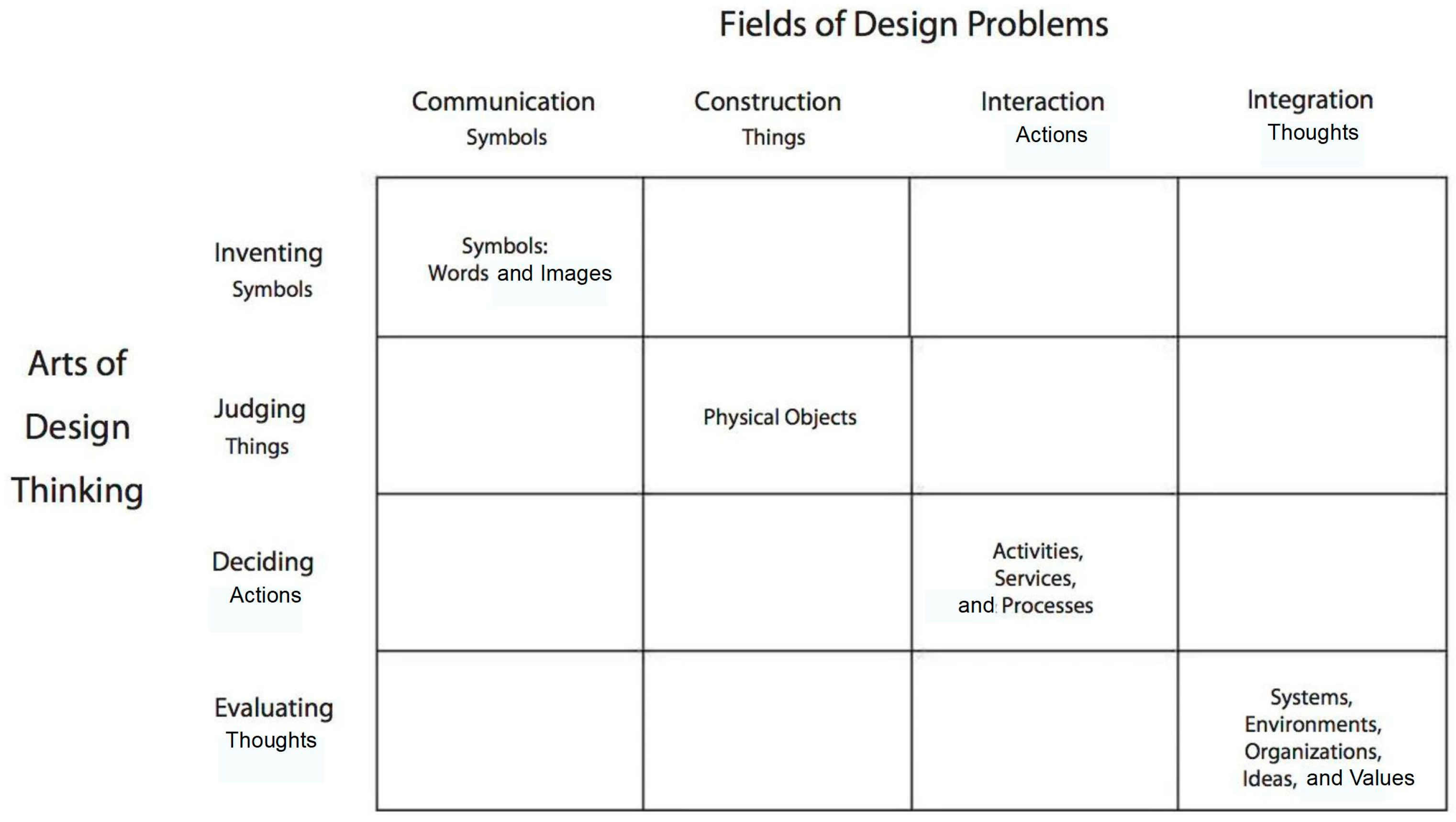
2.2.2. Designing the Four-Order Concept
Richard Buchanan proposed the concept of the “four orders of design,” also known as the “four stages of design.” It defines the four main categories of design: symbols, tangibles, actions and events, and systems and environments (
Figure 2).
Regarding the development history, the theoretical approach first appeared in Buchanan’s 1992 article “The Spooky Problem in Design Thinking” [
28]. With the rapid development of design education and design practice in the 20th century, the theoretical system of the four orders of design evolved and improved. In 1995, Buchanan elaborated on the theoretical system of the four orders of design in the form of a matrix from a rhetorical point of view [
29]. In 2019, Buchanan interpreted the four orders of design again, emphasizing that “environment” refers to the “larger” environment of human activity [
30]. In addition, Richard Buchanan’s presentation at the IxD Interaction Design Conference in 2011 also showed the “four orders of design” concept to the public again. However, through the search of three major repositories, the theory is mainly found in theoretical research but less in practice, and thus this thesis will fill the theory gap in design application.
In the smart health space, the four orders of design help systematically dismantle the coupling relationship between service processes and spatial carriers and provide structured logic for constructing spatial elements. Since the theory is a cognitive framework tool, it needs to be combined with a decision model to clarify the priority of each component before it can be implemented in the actual design.
2.2.3. AHP Method
AHP (Analytical Hierarchical Process) is a multi-criteria decision analysis methodology created by American mathematician and operations researcher Thomas L. Saaty in the 1970s [
31].
In space creation design, AHP theoretical models are often used as a systematic analysis method to sort out design elements. Yaralioglu and Kara identified the necessary parameters required for a sustainable public space design model based on expert opinion in a methodological analysis of the sustainable urban design of public spaces [
32]. Ersoz et al., an AHP was adopted by experts and residents for spatial characterization, resulting in a successful design strategy [
33]. Hu et al. used the methodology to analyze the livability hierarchy of an aging residential area, providing an apparent reference for policymakers and city managers [
34]. Girija et al.’s use of the AHP methodology and the Self-Determination Theoretical Framework advances the understanding of shared office space users’ key motivations [
35].
In summary, through hierarchical decomposition and expert scoring, AHP can systematize, index, and quantify the priority of design elements. It compensates for the shortcomings of the intense subjectivity and lack of weight control in SWOT. It designs a four-order approach applicable to indicator screening and weight allocation scenarios in the clinical health space design.
2.2.4. TOPSIS Method
TOPSIS (Technique for Order Preference by Similarity to the Ideal Solution) is a multi-criteria decision analysis (MCDM) method proposed by Hwang and Yoon in 1981. It is suitable for solving multi-attribute decision problems by calculating the relative proximity of each solution to the ideal solution and the negative ideal solution to rank the solutions [
36].
Shohda et al. used the superiority similarity ranking method based on the ideal solution of TOPSIS to evaluate some Egyptian decorative stones, which provided strategic indicators for stakeholders [
37]. Cheng used four urban parks in Jinan City as case study samples. Subjective perceptions were transformed into objective data through the TOPSIS model, which provided scientific bases for developing urban parks and green spaces. A scientific basis was provided for the development of urban park green space [
38]. Cheng and Li, to avoid decision-making errors caused by subjective factors, applied TOPSIS to perform weighted ranking, which successfully verified the scientific validity and feasibility of the evaluation system [
39]. Zoghi et al. selected the optimal alternative using the multi-criteria decision framework [
40].
Numerous studies have found that the TOPSIS model is well suited for comprehensively evaluating multiple quantitative indicators and can objectively reflect each program’s strengths and weaknesses. Combined with AHP, it can enhance the transparency and scientificity of decision-making [
41].
To summarize, SWOT provides strategic judgment, the four orders of design provide spatial logic, AHP realizes weight allocation, TOPSIS completes the program preference, and the four synergistically construct a systematic path from problem identification to design landing for smart health spaces.
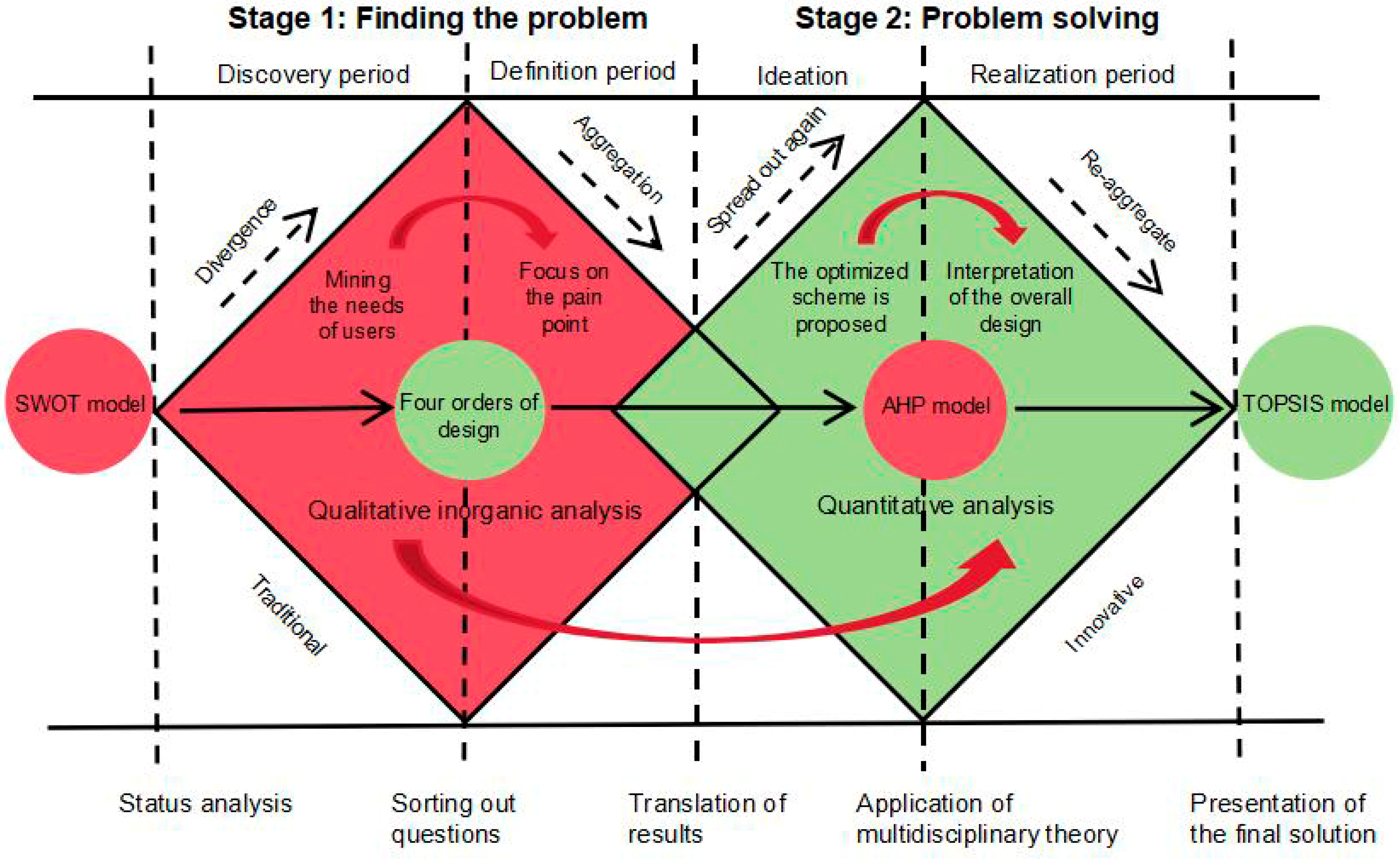
2.3. Conceptual Framework
This study names the model the “Four-Dimensional Integrated Model” based on the organic integration of its four dimensions, strategic analysis, spatial logic, decision-making weights, and optimal ranking, forming a complete and closed structural logic. “Four-Dimensional Integration” refers to integrating four highly complementary methodological tools into a closed-loop design decision-making system, specifically, 1. The SWOT analysis method as a strategic identification layer, providing qualitative assessments of the macro policy environment and opportunities/challenges; 2. the four orders of design Theory as a spatial logic layer, constructing a spatial cognitive and design structure from “symbols, tangible objects, and behavioral events to a system environment”; 3. The AHP method as an indicator evaluation layer, achieving quantitative modeling and weight allocation of user demand indicators; and 4. the TOPSIS optimal selection model as a decision ranking layer, which is used for quantitative comparisons and proximity assessments of multiple schemes.
The four components correspond functionally to the strategic, spatial, weighting, and decision-making stages, forming a complete closed-loop system encompassing design logic, user weighting, evaluation methods, and optimization results. This is called “Four-Dimensional Integration,” emphasizing its multidimensional integration, hierarchical progression, and logically closed structure.
Additionally, this model can be mathematically defined through function nesting and decision process mapping. It reflects its systematic, hierarchical, and scientific nature and is formally expressed as M = TOPSIS × AHP × four orders of design × SWOT (X), where SWOT (X) represents the macro-strategic identification of input data and the output of strategic directions; the four orders of design represents the transformation of strategies into spatial and behavioral dimensions; AHP represents the construction of an evaluation indicator system and the quantification of weights; TOPSIS represents the ranking and selection of multiple design schemes based on weights and indicator values; and M represents the final output as the optimal design decision result. This model has a clear input–processing–output chain and can be formally constructed as a composite function system, where each layer is a mathematically expressible process with a mathematical foundation.
The whole research process consists of two major parts: firstly, the analysis of the problem and then problem solving. The latter consists of four sub-steps: 1. identifying the issue using the SWOT model; 2. thinking about the issue using the concept of the four orders of design; 3. analyzing the problem and proposing a solution using the AHP model; and 4. selecting the optimal solution using the TOPSIS model.
Step 1: After reviewing the literature, users’ experiences, user interviews, and other research methods, we use the SWOT model’s analytical framework to conduct a preliminary analysis of the community smart health space’s current situation and clarify the direction of future optimization.
Step 2: We apply the concept of the four orders of design to analyze intelligent performance and consumers’ experiences and develop an optimization plan.
Step 3: We combine the requirement data obtained from the AHP model to derive an importance ranking and a final improvement strategy.
Step 4: We compare and contrast with other available options and select the best choice.
The conceptual framework utilizes the double-diamond model, which plays on the divergent and focused thinking styles to distill the whole process and present it in a visualization mode. The research steps and mind map are shown below (
Figure 3).
4. Research Findings and Methodological Risks
4.1. Research Findings
Based on each scheme’s positive ideal solution, negative ideal solution, and relative closeness (
Table 13), Option 1 has the highest relative closeness ranking and is therefore rated as the best community smart health space design scheme. The data shows that the contextual scores of the existing solutions are lower than the smart health space design proposed in this study. The study suggests that the SWOT–four orders of design–AHP–TOPSIS hybrid model has a high design guidance value.
In addition, the main findings from the application and evaluation of the hybrid model constructed in this study in the design of innovative and healthy spaces in the community are as follows:
- (1)
Multidimensional Hybrid Model to Enhance the Systematic and Scientific Nature of Intelligent Health Designs
The quadratic fusion model of “SWOT–four orders of design–AHP–TOPSIS” constructed in this study effectively integrates qualitative strategic analysis, design logic, and decision-making tools, significantly improving the logical clarity and operability of community intelligent health space design. Among the AHP results, the behavioral experience (weight = 0.470) has the highest priority among the four types of level 1 indicators, which is much higher than the hardware facilities (weight = 0.094), highlighting the dominant value of user participation and service process in imaginative health scenarios. The TOPSIS assessment results show that the relative proximity of the innovative health space program designed based on the model of the present study (Ci = 0.844) is significantly higher than other existing scenarios (Ci = 0.436 for Scenario 2 and Ci = 0.307 for Scenario 3), which verifies the hybrid model’s preference ability and design-oriented efficacy in practical applications.
- (2)
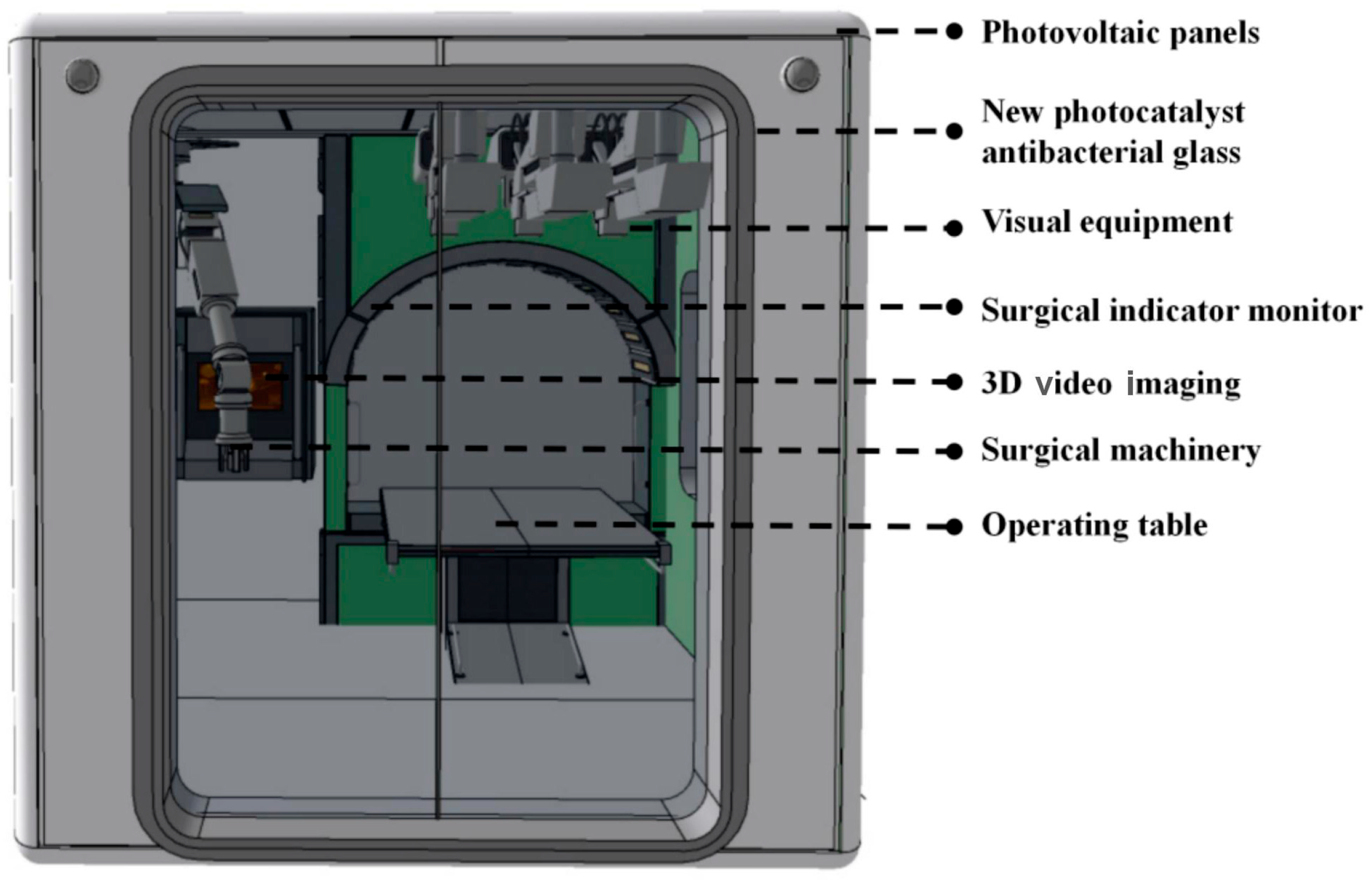
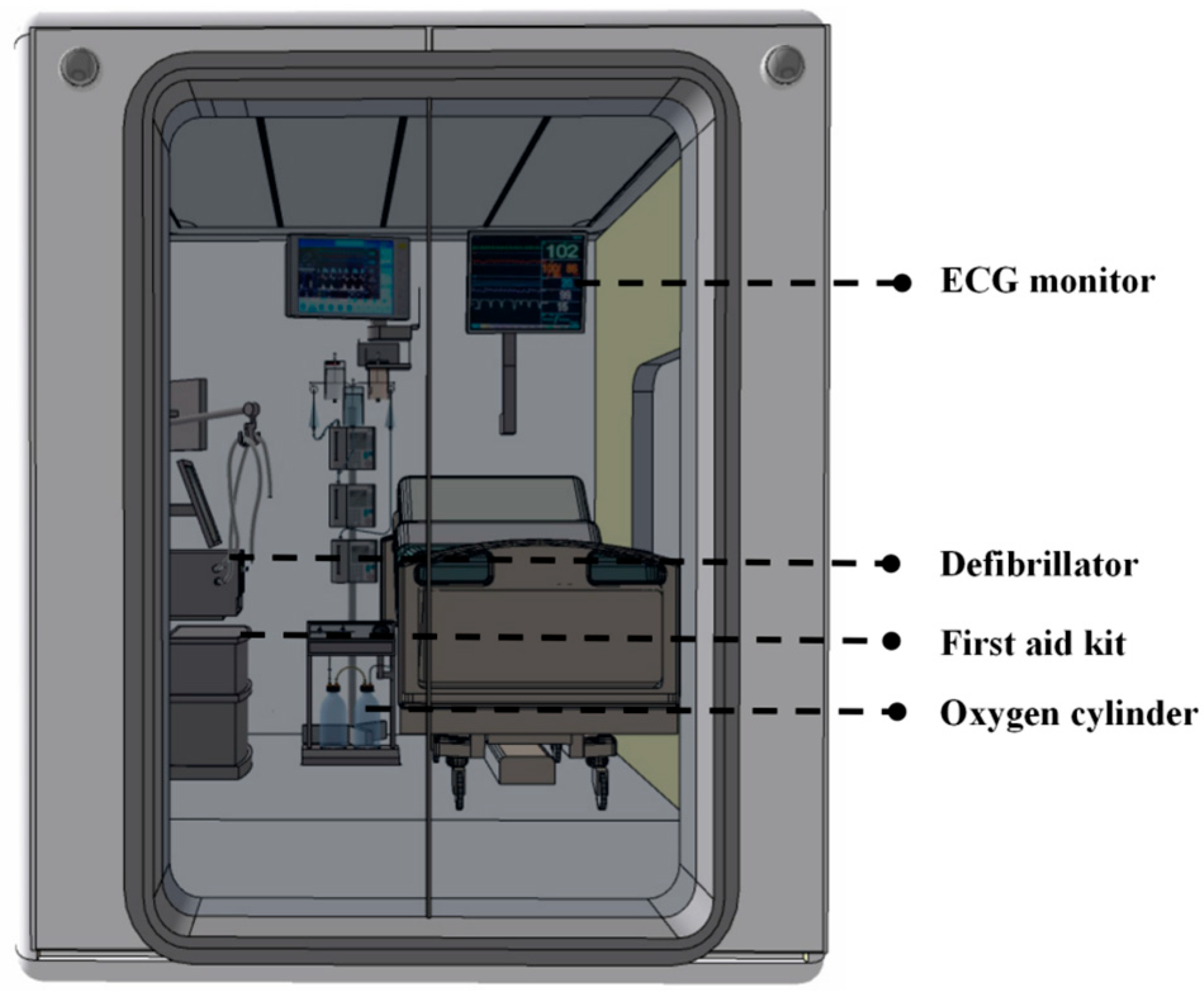
A human-oriented design order promotes the optimization of the healthcare space experience
The theory of the “four orders of design” was first applied to the practice of intelligent health space design, effectively realizing the structural translation from an abstract strategy to spatial elements. In the modules of diagnosis and treatment, first aid, and physical examination, the four-order structural design principle of “symbolic identification–tangible configuration–behavioral process–environmental regulation” is introduced, and through the optimization of color psychology and spatial behavioral path planning, the psychological comfort and functional identification efficiency of patients are enhanced. The optimization of color psychology and spatial behavioral path planning enhances patients’ psychological comfort and functional recognition efficiency. For example, the green diagnosis and treatment module significantly relieves patients’ anxiety, and the beige first aid cabin enhances the response stability of the first aid providers on the scene, reflecting the adaptation and deepening of the human-oriented strategy in the intelligent health environment.
- (3)
Quantitative decision support significantly improves program comparability and objectivity
By combining the AHP and the TOPSIS optimization method, this study constructed an evaluation system covering 16 indicators, in which “remote expert consultation” (combined weight = 0.197) and the “unmanned” function (combined weight = 0.121) became the core decision-making factors, which clarified the focus direction of the future design of the innovative health module. The TOPSIS ranking, calculated based on the dataset scored by 20 domain experts, forms a scientific, quantitative, and replicable evaluation mechanism, providing a robust basis for the assisted judgment of complex space design tasks.
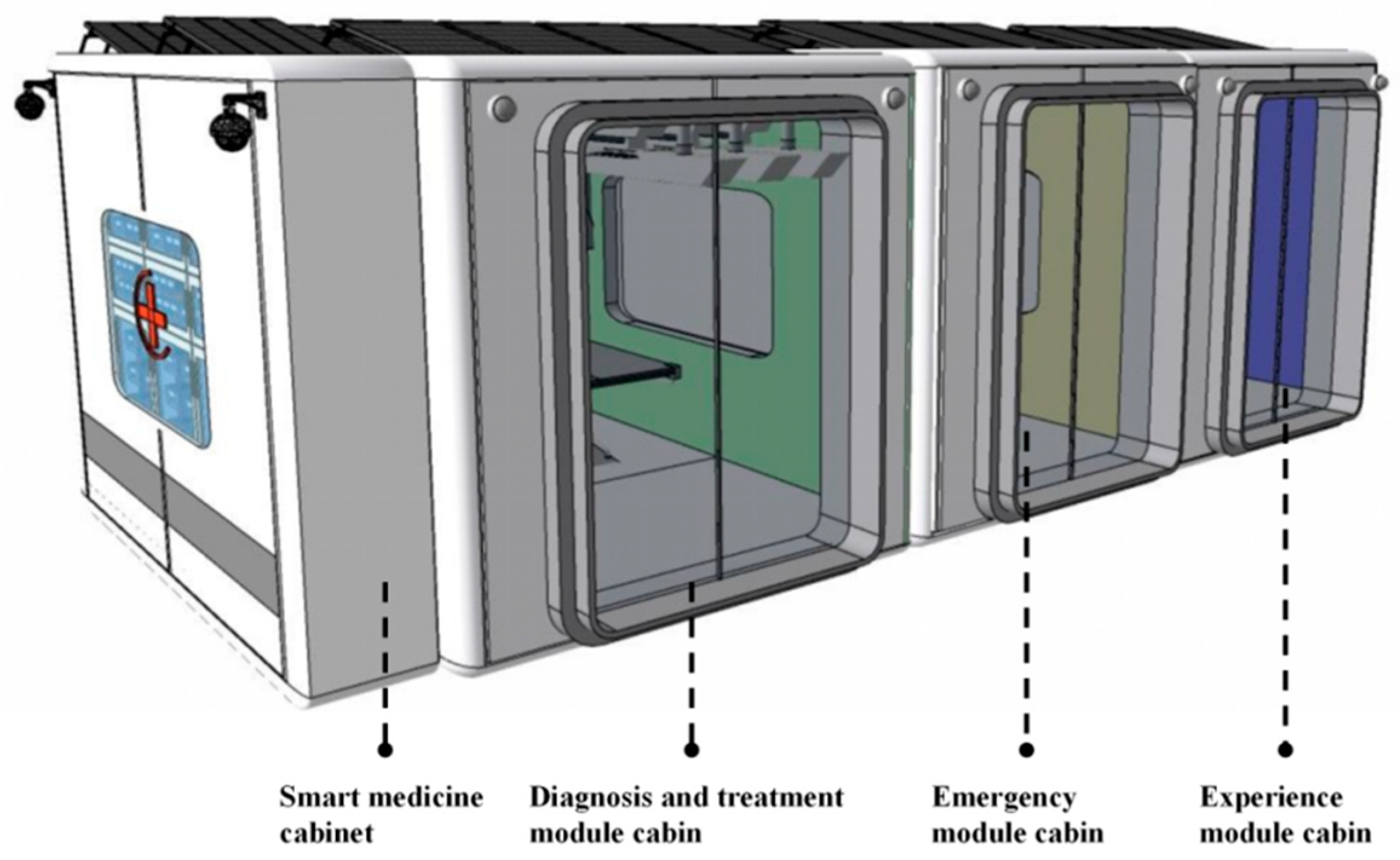
- (4)
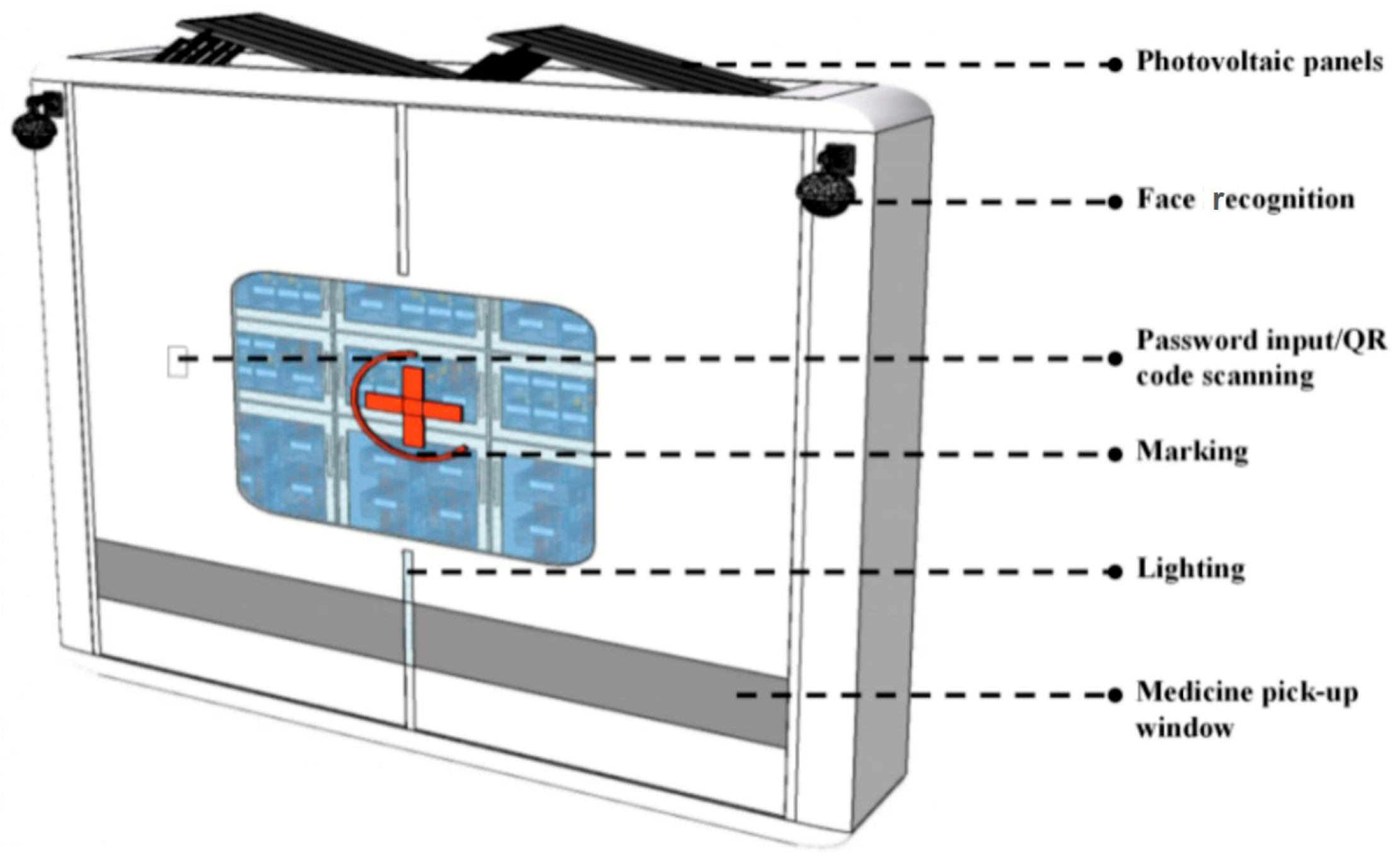
Modularity and the Movable Design Expand the Boundaries of Community Healthcare Response
The intelligent health space adopts a modularized detachable structure and photovoltaic energy system, realizing a four-in-one movable combination unit of “diagnosis, first aid, medical checkup, and medicine collection”. The diagnosis and treatment module integrates a 5G remote surgery system and antibacterial photocatalyst glass, the first aid module is equipped with complete life-supporting equipment, and the medical checkup module is equipped with self-service testing and online consultation functions. This structural design improves the community’s ability to respond to public health emergencies. It provides technical and product support for the future allocation of healthcare resources in rural, remote, and other grassroots areas.
- (5)
The hybrid modeling methodology has the potential for cross-domain replication
The proposed “SWOT–four orders of design–AHP–TOPSIS” multi-disciplinary integration model effectively breaks through the limitations of traditional community healthcare space design, which were characterized by “strong policy orientation, weak user participation, and a single evaluation method”. It establishes a closed-loop decision-making mechanism spanning the entire process from strategic insights (SWOT), system configuration (four orders of design), and indicator balancing (AHP) to optimal solution selection (TOPSIS). This model has validated its methodological efficacy in constructing community smart health spaces and possesses the theoretical foundation and structural flexibility to be extended to other public health scenarios.
To enhance its practicality and promotional value, this paper further proposes a contextual adaptability adjustment mechanism for the model to address differences in target audiences, core functions, and constraints across various usage scenarios.
- (1)
Elderly care service spaces (e.g., senior day care centers and care stations)
Adjustment strategy: Introduce “physical deterioration of the elderly population, digital exclusion, and psychological safety” as disadvantage dimensions in the SWOT analysis phase; emphasize spatial accessibility and emotional support systems (such as interactive voice guidance and cognitive-friendly icon systems) in the “four orders of design” framework; and appropriately increase the weights of the “emotional comfort” and “operational simplicity” indicators in the AHP phase.
Expected outcomes: Enhance the physical and psychological friendliness of spaces for elderly users, promoting their proactive health management and willingness to participate in daily activities.
- (2)
Rehabilitation centers or mobile rehabilitation spaces (e.g., mobile rehabilitation vehicles, community therapy pods)
Adjustment strategy: Strengthen the “rehabilitation assessment—intervention feedback” closed-loop mechanism in module system design; add dimensions such as “muscle function recovery efficiency”, “treatment precision”, and “device intelligence level” in indicator construction; prioritize the dynamic allocation capability and customized service adaptability of the space in TOPSIS evaluation.
Expected outcomes: Enhance rehabilitation facilities’ mobility deployment flexibility and precision treatment capabilities, supporting multi-community collaboration and frequent service provision.
- (3)
Health Education Kiosks and Public Education Spaces
Adjustment strategy: Strengthen the “symbol recognition—interaction trigger—knowledge conversion” path logic in design order; incorporate “cognitive incentive” and “multi-sensory experience dimensions” as evaluation factors in the AHP system; use TOPSIS to select the most interactive and communicative spatial prototypes.
Expected Outcomes: Improve residents’ understanding and internalization of health knowledge and promote the widespread dissemination of preventive health behaviors.
In summary, the “SWOT–four orders of design–AHP–TOPSIS” model, as a hybrid methodology with an adjustable structure, expandable logic, and transferable application, can be flexibly adjusted through modularization to support the entire process optimization from spatial planning to system evaluation in various types of smart health scenarios. In future smart city development, this model is expected to serve as a key methodological pillar for the intelligent transformation of health infrastructure, providing a paradigm demonstration integrating institutional, spatial, and behavioral dimensions.
4.2. Method Applicability Risk
Although the “SWOT–four orders of design–AHP–TOPSIS” quadruple integration model demonstrates strong systematicity and adaptability in theoretical construction and case analysis, it still faces the following potential risks and limitations in practical applications:
Subjective judgment risk—The AHP method relies on expert experience for a pairwise comparisons of indicators. Although this study enhanced objectivity using the geometric mean method to integrate 20 expert questionnaires, indicator weighting inevitably remains influenced by individual biases, potentially affecting the model’s neutrality and reproducibility.
Static results issue—The current model generates optimal solutions based on single expert inputs and scenario assumptions, lacking real-time feedback mechanisms for dynamic changes (such as policy adjustments or evolving user behaviors). This may lead to the results becoming obsolete over time. Future research should introduce dynamic update mechanisms or simulation mechanisms to enhance robustness.
Overreliance on model risks—This model should be used as an auxiliary decision-making tool in conjunction with professional judgment and field research. Suppose that the model conclusions are relied upon as the sole basis for decision-making. In that case, it may lead to systemic misjudgments that overlook irrational user behaviors, cultural context differences, or the impacts of unforeseen events.
5. Conclusions
This study proposes a “quadruple integration” hybrid model framework for the design of community-based intelligent health spaces, innovatively integrating the SWOT strategic analysis, the theory of design order, the Analytical Hierarchical Process (AHP), and the Technique for Order Preference with Similarity to the Ideal Solution (TOPSIS) model. Using a mobile modular intelligent health unit as a prototype, the framework completes a closed-loop process from strategic diagnosis to functional construction and multidimensional evaluation. The study addresses the urgent need for the innovative restructuring of community intelligent health spaces at the conceptual, mechanistic, and systemic levels in the context of an aging population, rising public health risks, and strained primary healthcare systems.
This study achieves a theoretical breakthrough in existing community healthcare space design paradigms. Traditional designs primarily focus on the functional space configuration, lacking an integrated response to behavioral experiences, system interconnectivity, and strategic objectives. This paper introduces the “four orders of design” theory as a spatial structuring method for the first time, implementing the layered design of symbolic systems, tangible configurations, behavioral pathways, and environmental systems to strengthen healthcare spaces’ cognitive guidance and usage interaction logic. The proposed “SWOT–four orders of design–AHP–TOPSIS” integrated model establishes a cross-level, cross-dimensional, and quantifiable design evaluation framework, infusing healthcare space research with systems thinking and decision science support.
Methodologically, this study breaks through the limitations of previous healthcare space designs, which were dominated by qualitative approaches, subjective evaluations, and insufficient user participation. It establishes a multi-level decision-making system comprising four dimensions—behavioral experience, perceived environment, facility configuration, and platform support—with 16 indicators. The AHP analysis clarifies the weights of each indicator, with behavioral experience (weight = 0.470) and software facilities (weight = 0.273) identified as key variables, highlighting the importance of synergy among “space–behavior–technology”; the TOPSIS optimal selection model validated the comprehensive advantages of this design scheme in terms of spatial efficiency and user adaptability with a proximity index Ci = 0.844.
In practical terms, the mobile modular intelligent health unit developed based on the model guidance in this study features comprehensive functions such as telemedicine, routine health checkups, and medication management, making it suitable for daily community health services and emergency response scenarios. It can effectively alleviate the shortage of primary healthcare resources and improve service response efficiency. This scheme emphasizes a human-centered experience, interactive convenience, and system interoperability. It is expected to provide modular deployment templates and methodological frameworks for smart health communities, elderly care stations, rehabilitation pods, and emergency medical units.
Additionally, the model architecture proposed in this study has high scalability. Chapter 4 further explores its adaptation strategies and adjustment paths in different scenarios, such as elderly care spaces, rehabilitation facilities, and health exhibition pavilions, demonstrating the method’s universality and the flexibility of spatial strategies.
This study proposes an innovative mechanism for coupling spatial design and service decision-making in theory. It constructs a decision-making model that integrates assessments and the optimization of the methodology. Furthermore, it provides concrete and feasible spatial prototypes in practice. This research promotes the transformation of community healthcare spaces from a “function-oriented” approach to an “experience-oriented” and “system-oriented” approach, providing spatial support and methodological guarantees for the systematic development of urban health infrastructure under the “Healthy China” strategic goal.
Although this study has achieved certain breakthroughs in method integration and prototype design, the following limitations remain:
First, the current design scheme is still in the prototype modeling and indicator verification stage, lacking systematic user on-site behavior data and service performance evaluations. It is recommended that future research further refine the design adaptability and service efficiency verification through multiple rounds of on-site deployment, user feedback analysis, and lifecycle data tracking. Second, with the rapid development of AI and health technology, future research could integrate generative design tools with ergonomics and environmental psychology to explore personalized growth mechanisms, emotional sensing systems, and sustainable material integration strategies for medical spaces. Third, a health space service network composed of “points–lines–networks” could be constructed at the urban scale, forming a distributed health security system comprising modular units, community hubs, and regional medical centers.
To promote the implementation of the “SWOT–four orders of design–AHP–TOPSIS” model proposed by this research institute in the field of intelligent health spaces, this paper offers the following operational recommendations for policymakers, engineering and technical personnel, and operations and maintenance managers:
- (1)
Recommendations for decision-makers
1. Establish a multi-stakeholder collaborative decision-making mechanism by encouraging the inclusion of resident representatives, community doctors, technology companies, and government departments in the preliminary assessment and strategy formulation stages to establish a user-centric co-construction mechanism for healthy spaces, thereby enhancing the social acceptance and effectiveness of public projects.
2. Strengthen policy resource integration; it is recommended that policy resources related to healthcare, elderly care, smart cities, and digital governance be integrated into the construction of smart, healthy spaces, establishing a unified planning indicator system and performance evaluation framework to avoid duplicate investments and functional overlaps caused by departmental fragmentation.
3. Establish a model-driven investment assessment mechanism that incorporates the model from this study into the project pre-assessment phase as a reference for scientific and differentiated resource allocation by the government, particularly for project types such as urban renewal, community improvement, and expansion of primary healthcare facilities.
- (2)
Recommendations for engineering implementation and operations personnel
1. The modular design should balance standardization and localization. When deploying mobile health units and spatial modules, adhere to unified interface standards (e.g., power supply, network, and data format) to enhance universality while flexibly adjusting based on community demographics and transportation conditions to ensure adaptability and operational convenience.
2. Emphasize the integration of information systems and medical processes. It is recommended to conduct information platform integration and hospital-end system interoperability testing in advance to ensure smooth synchronization of user data between the health cloud platform, offline terminals, and doctor systems, avoiding the phenomenon of “equipment in place but systems ineffective”.
3. Establish a professional maintenance team mechanism. For smart devices (such as remote diagnostic systems and health data collection terminals), an experienced team with composite software and hardware skills should be assigned to perform daily maintenance and user guidance. Introducing local healthcare personnel as the first responders in community health spaces may also be considered.
4. Develop a feedback mechanism and continuous assessment system. Monitor system performance through multidimensional data such as resident usage frequency, satisfaction surveys, and health intervention effectiveness. These provide the dynamic basis for facility adjustments, functional updates, and service optimizations, establishing a closed-loop model of “design–use–redesign.”