Multizone Modeling of Airborne SARS-CoV-2 Quanta Transmission and Infection Mitigation Strategies in Office, Hotel, Retail, and School Buildings
Abstract
1. Introduction
2. Methodologies
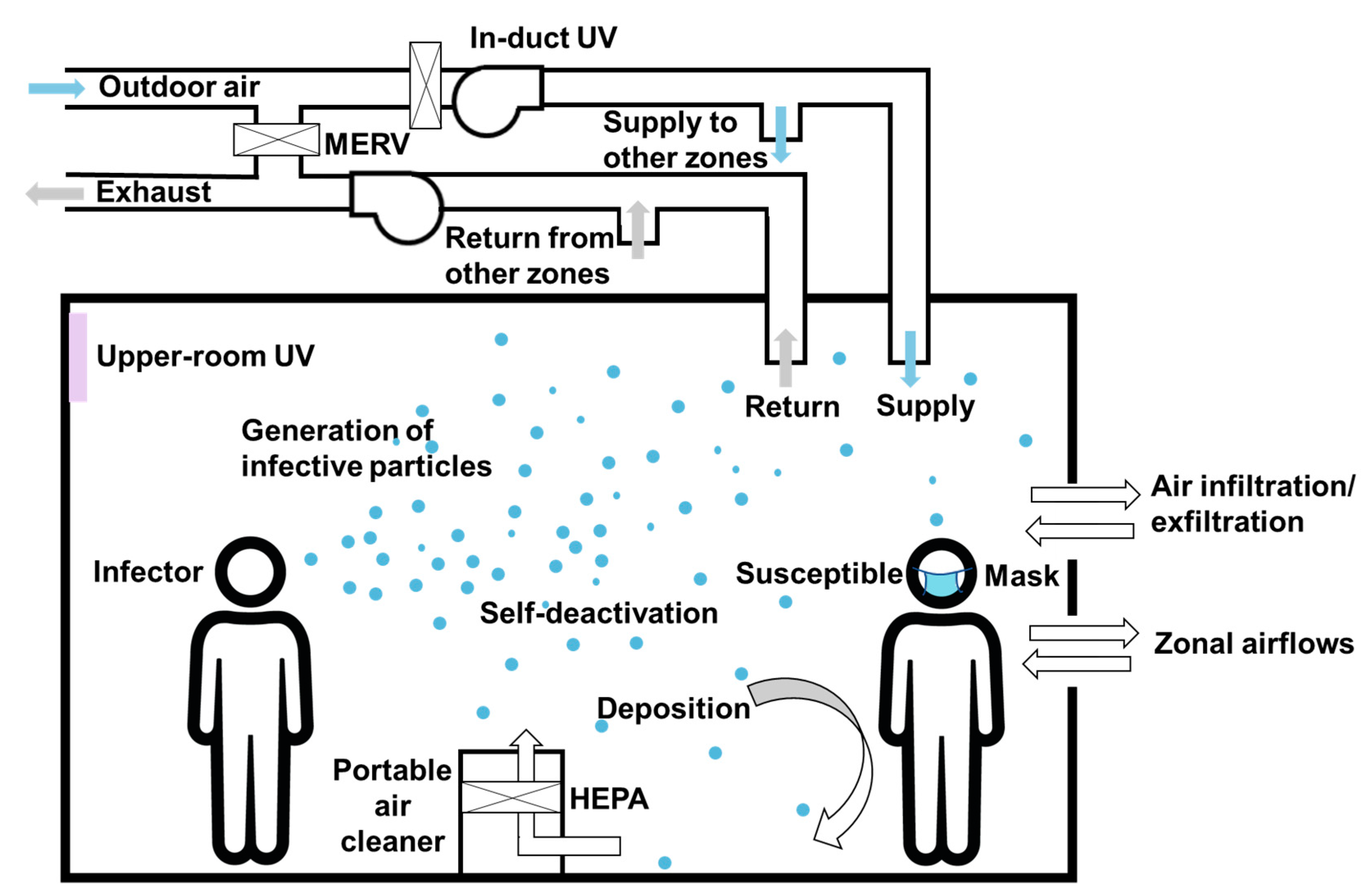
2.1. The CONTAM-Quanta Approach for Evaluating Infection Risks
2.2. Equivalent Air Change Rate
- QOA = outdoor air ventilation rate in [m3/h] divided by the room volume [m3];
- QMERV = recirculated ventilation airflow rate (m3/h) MERV efficiency/Volume (m3);
- QPAC = CADR(m3/h)/Volume (m3);
- QGUVr = airflow rate passing by the in-duct GUV light (m3/h)/Volume (m3), or clean air delivery rate provided by the upper-room germicidal lamp system CADRUV(m3/h)/Volume (m3);
- Qdeposition = Quanta deposition rate (1/h);
- Qdeactivationdec = Viral deactivation rate (1/h).
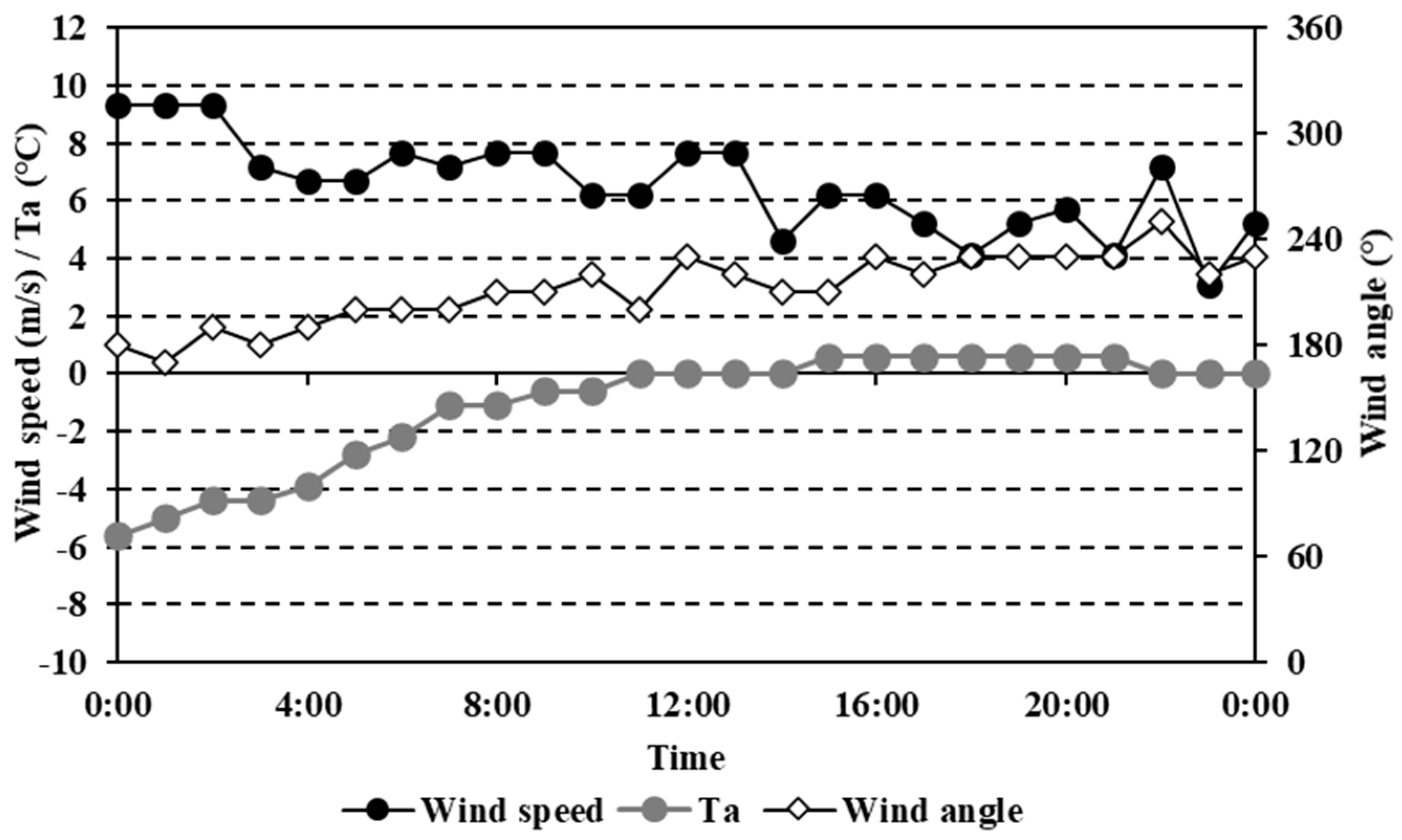
2.3. DOE Prototype Commercial Building Models
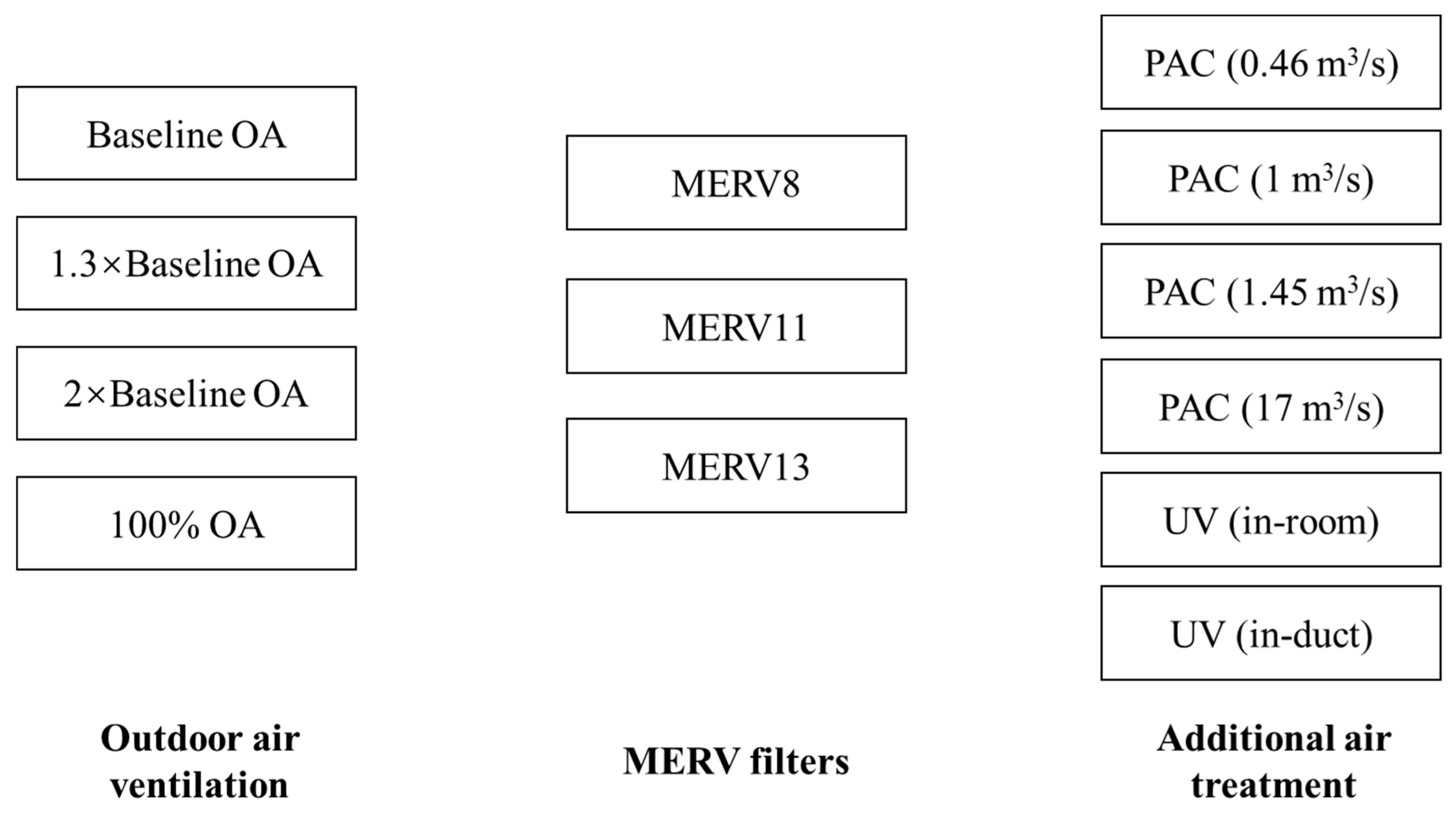
2.4. Baseline Case of Airborne Risk Mitigation Strategies
3. Simulation Results
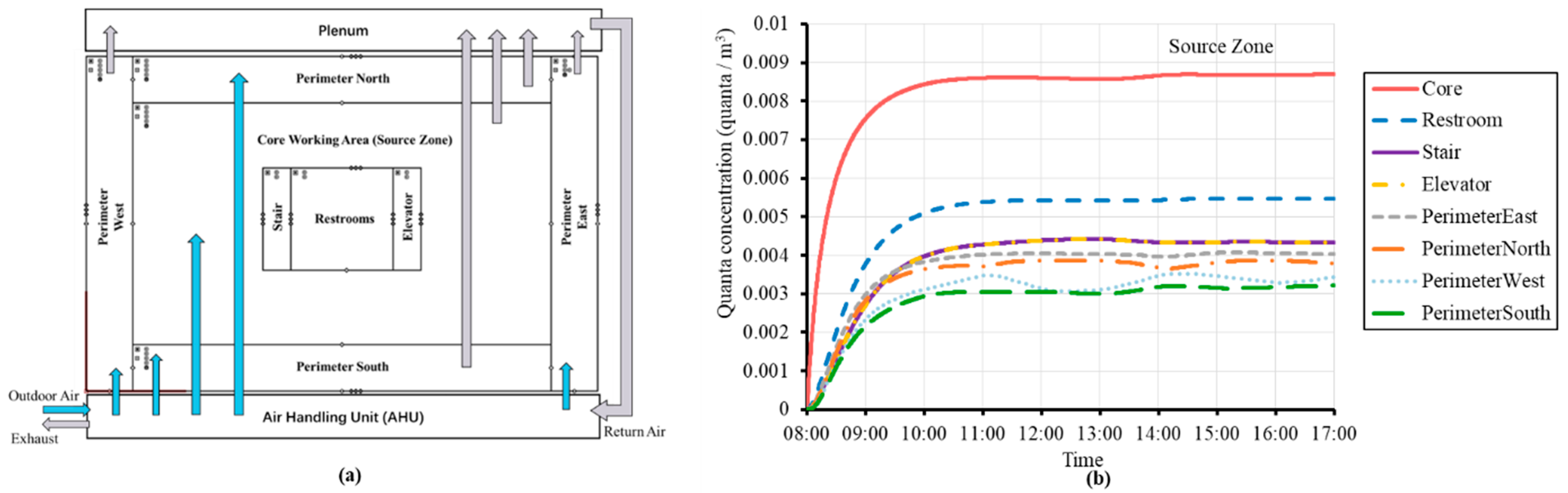
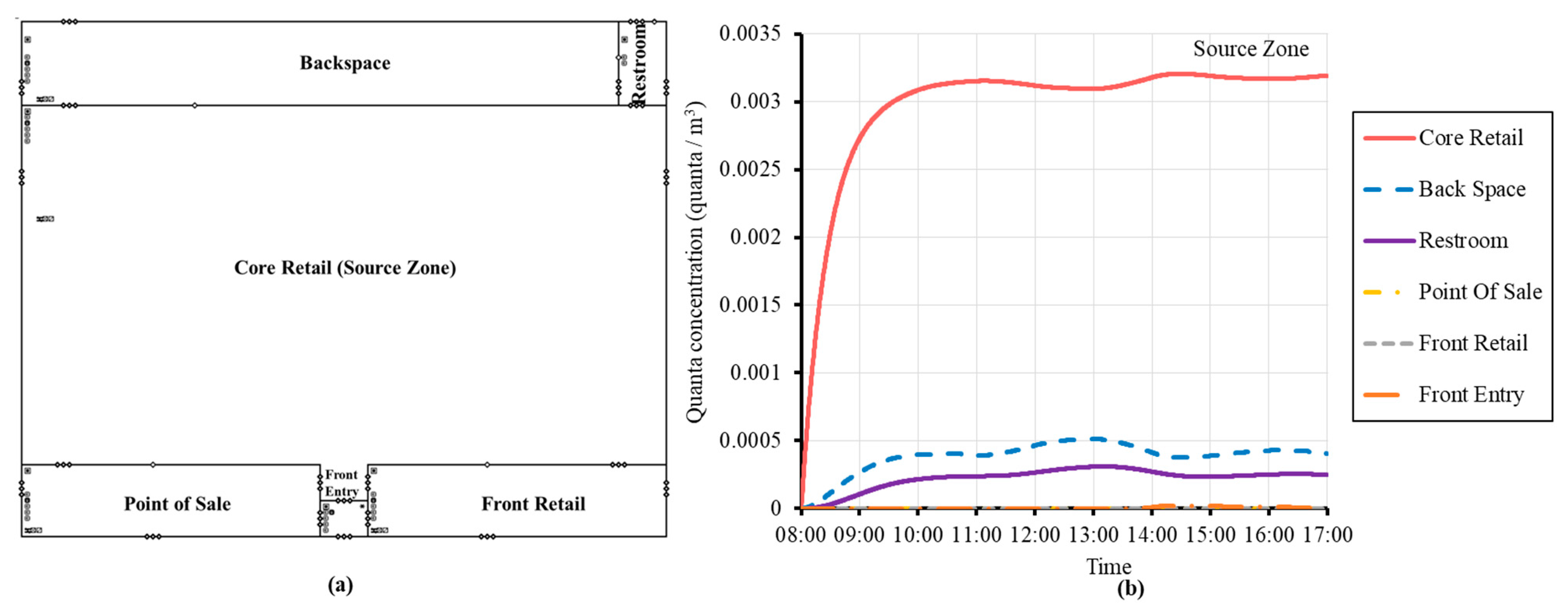
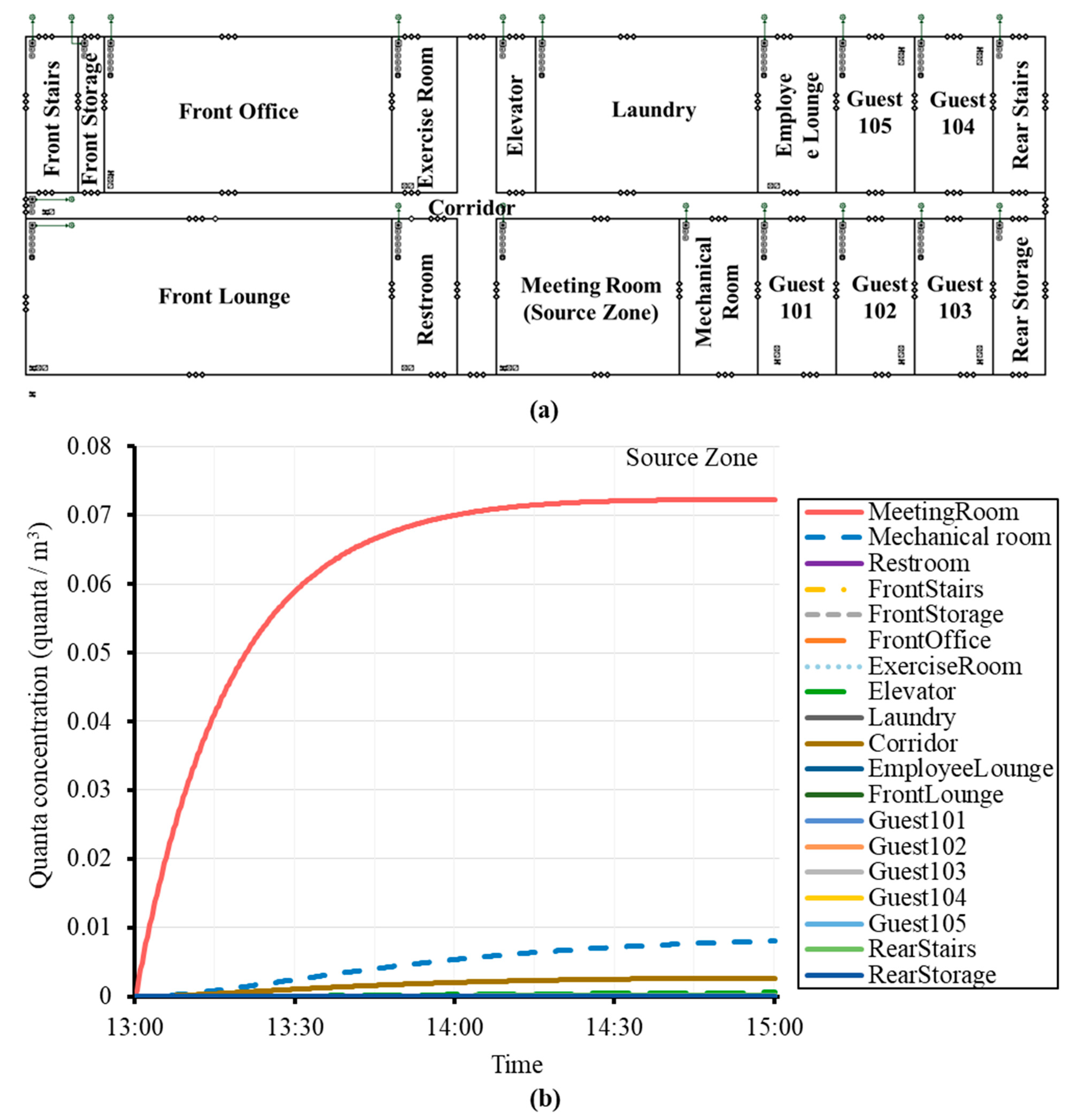
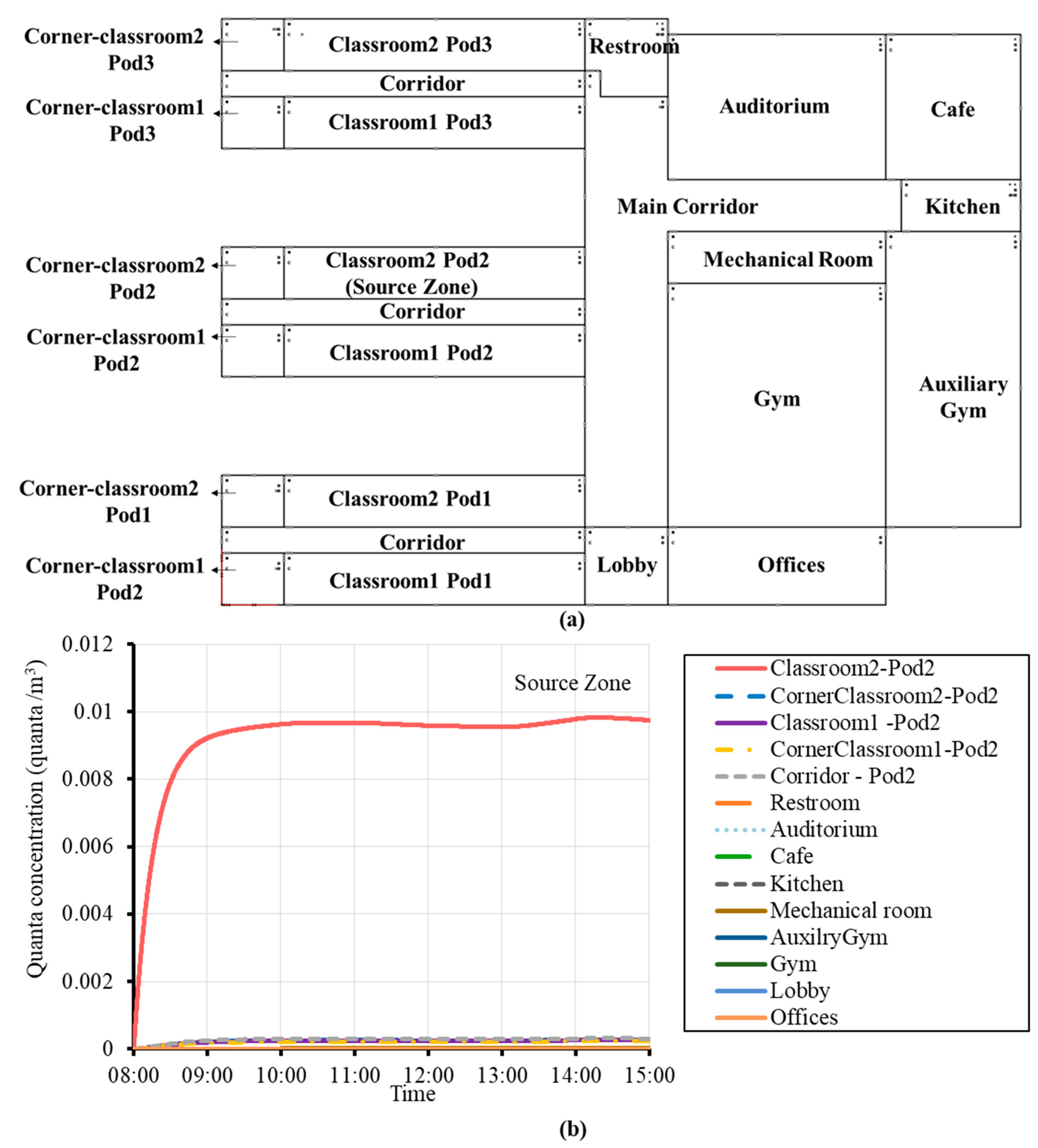
3.1. Zone-to Zone-Transmission
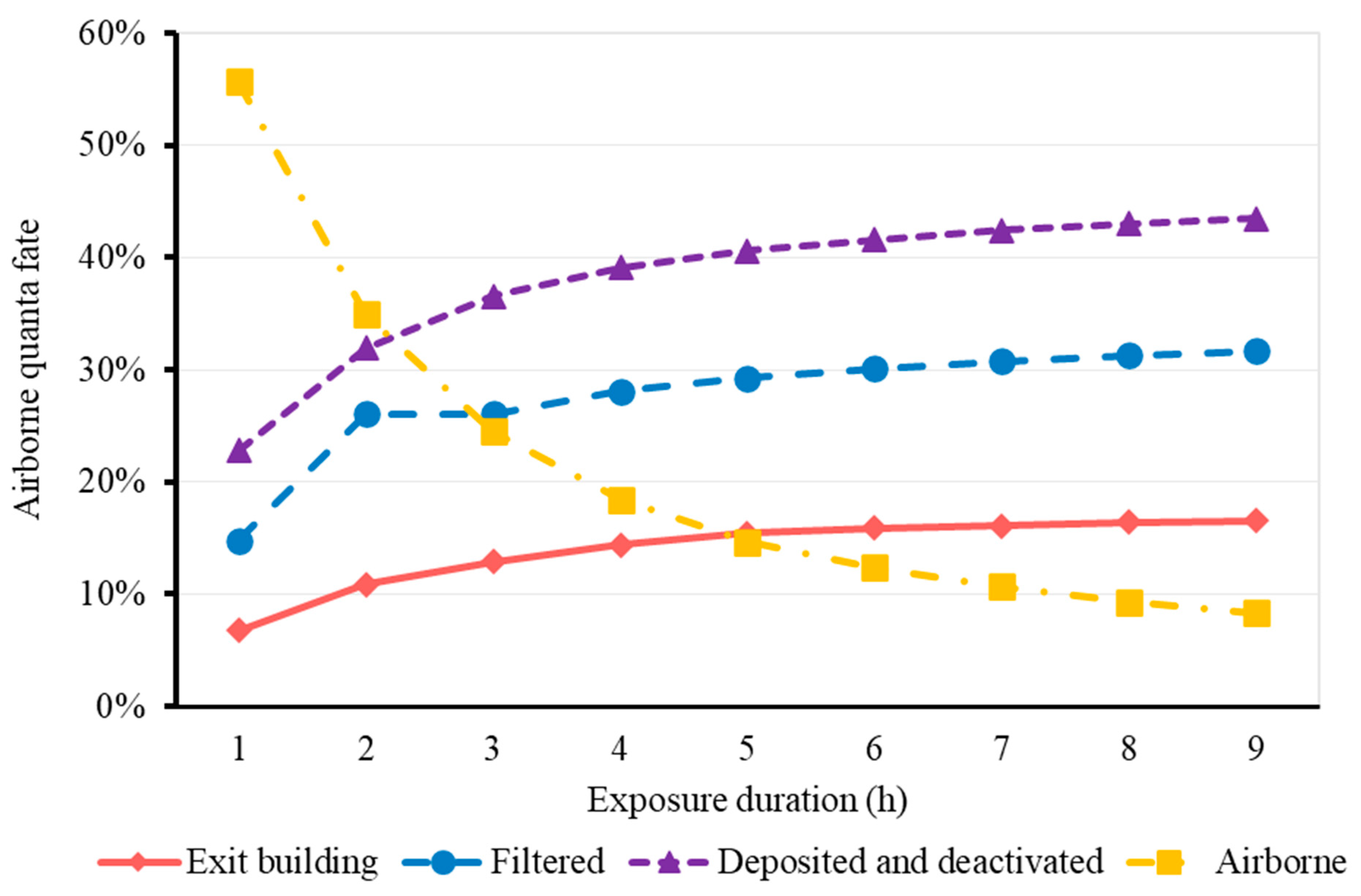
3.2. Fate of Airborne Quanta
3.3. Risk Assessment for Baseline Cases
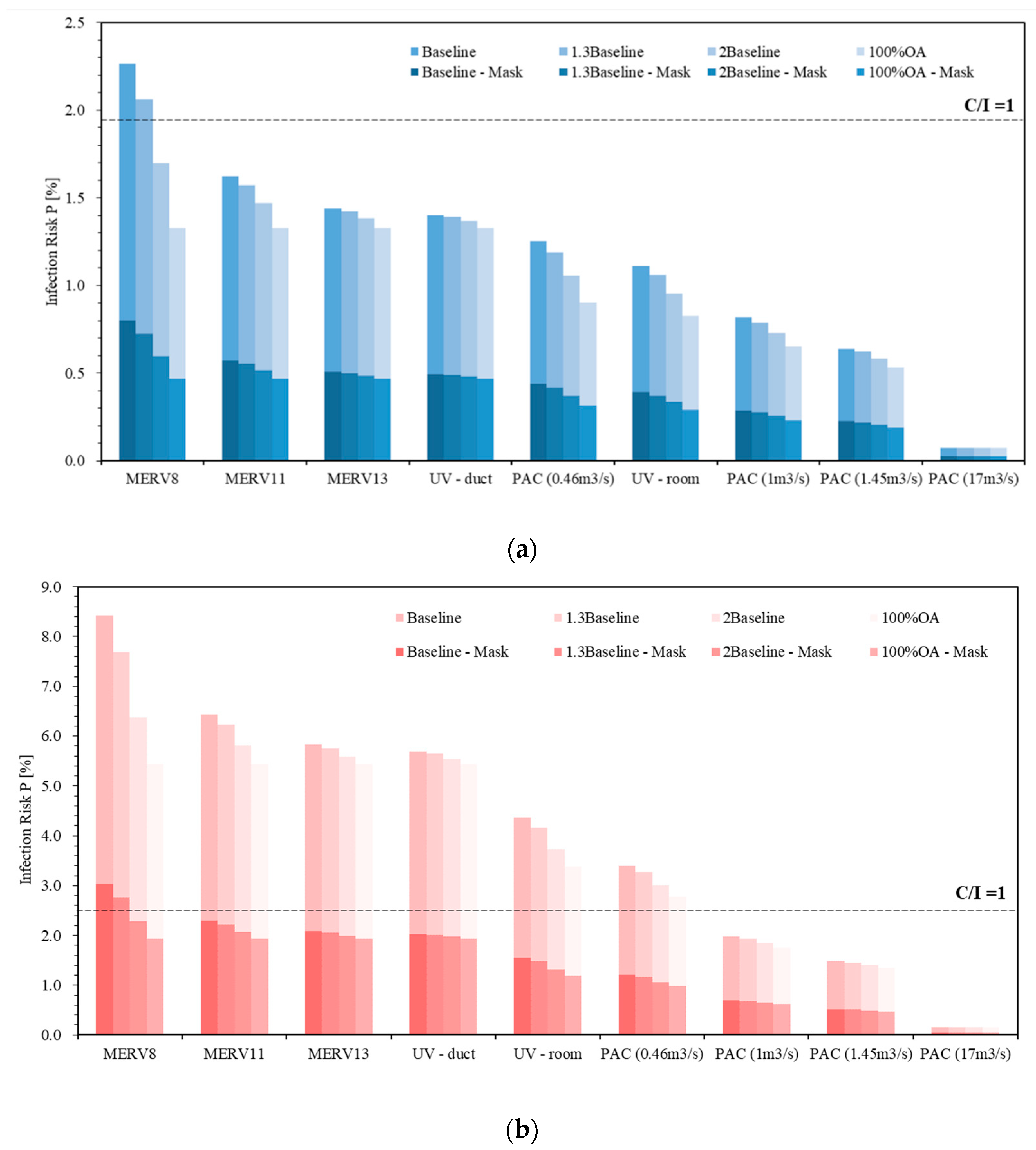
3.4. The Effectiveness of Risk Mitigation Strategies
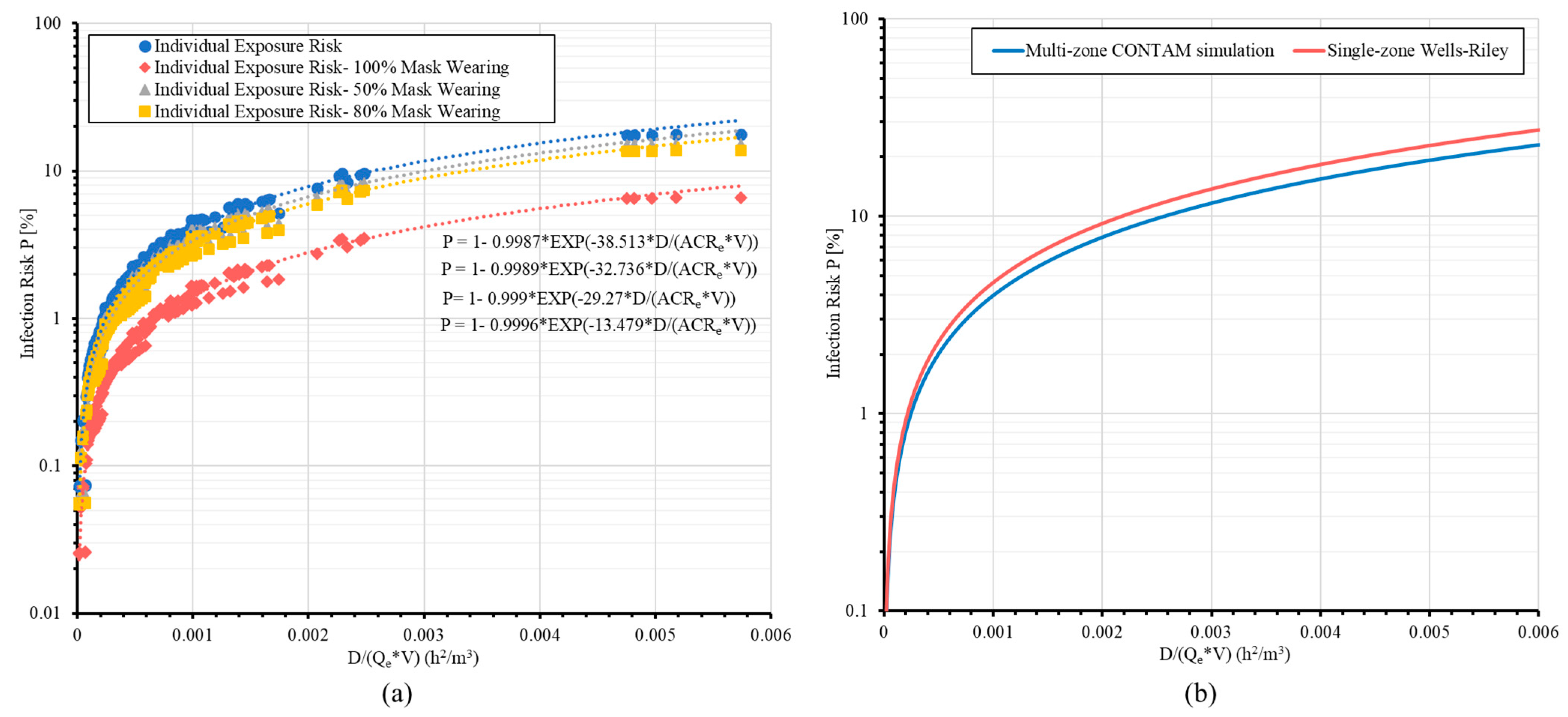
3.5. Association of Infective Risks with Equivalent Air Change Rate Qe
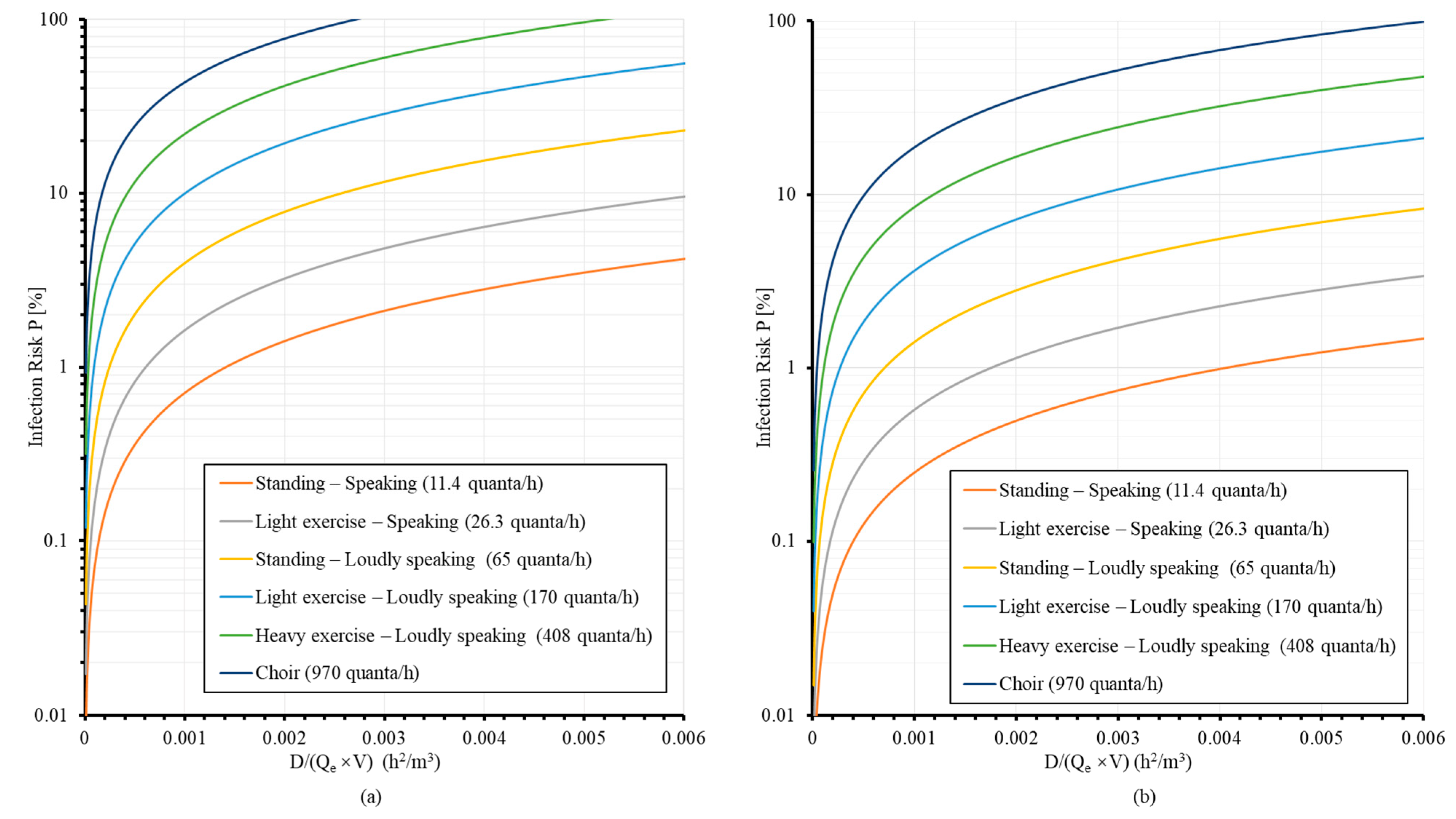
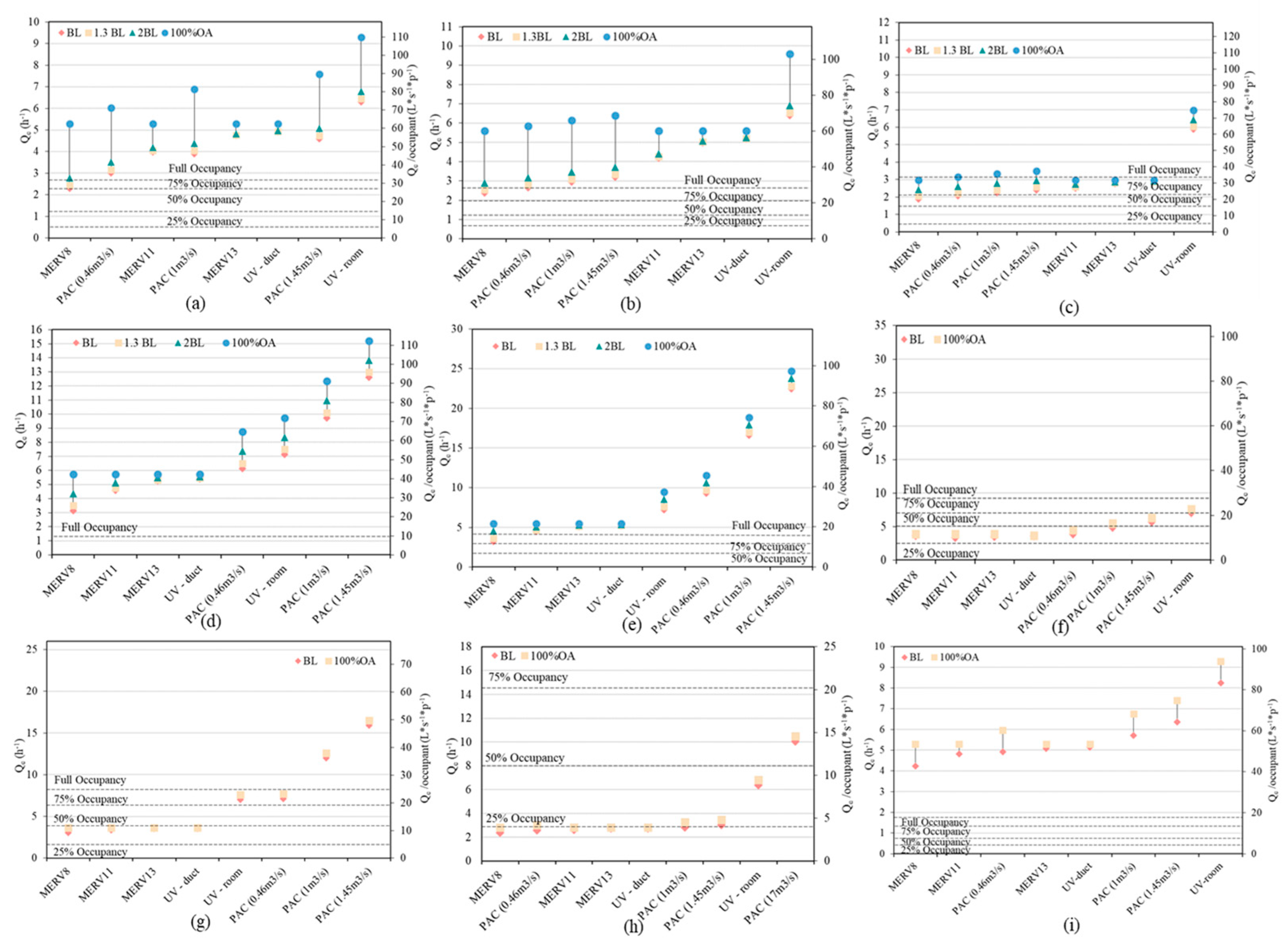
3.6. Mitigation under Different Occupancies
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Nomenclature
| AL | Effective air leakage area (m2) |
| B | Breathing rate (m3/s) |
| C | Number of infection cases |
| Cavg | Average quanta concentration (quanta/m3) |
| CD | Flow discharge coefficient |
| Ci | Contaminant concentration in the infectious zone (quanta/m3) |
| Cj | Contaminant concentration in neighbor zones (quanta/m3) |
| Cs | Contaminant concentration of the supply air (quanta/m3) |
| Crec | Contaminant concentration of the recirculation air (quanta/m3) |
| Coa | Contaminant concentration of the outdoor air (quanta/m3) |
| E | Occupant exposure to contaminants (quanta) |
| Fm | Percentage of mask-wearing occupants |
| G | Generation rate of quanta from the infector (quanta/m3) |
| Minh | Inhale removal efficiency of masks (%) |
| Mexh | Exhale efficiency of masks (%) |
| n | Number of inhaled quanta |
| Q | Volumetric flow rate (m3/s) |
| Qe | Equivalent air change rate (1/h) |
| QOA | Outdoor air ventilation rate (1/h) |
| QMERV | Equivalent air change rate from MERV filters (1/h) |
| QPAC | Equivalent air change rate from portable air cleaner (1/h) |
| QGUV | Equivalent air change rate from in-duct GUV light (1/h) |
| Qdeposition | Quanta deposition rate (1/h) |
| Qdeactivation | Viral deactivation rate (1/h) |
| Qr | Volumetric flow rate of the return air (m3/s) |
| Qlx | Volumetric flow rate of the local exhaust air (m3/s) |
| Qac | Volumetric flow rate of the air cleaner (m3/s) |
| Qrec | Volumetric flow rate of the recirculation air (m3/s) |
| QUVr | Equivalent volumetric flow rate of in-room GUV devices for pathogen inactivation (m3/s) |
| Qdep | Equivalent volumetric flow rate of aerosol deposition (m3/s) |
| Qdec | Equivalent volumetric flow rate of viral aerosol decay/inactivation (m3/s) |
| Qexf | Exfiltration flow rate to neighbor zones (m3/s) |
| Qinf,j | Infiltration from zone j (m3/s) |
| Qexf,j | Exfiltration from zone j (m3/s) |
| The efficiency of MERV filters | |
| The efficiency of in-duct GUV light | |
| The efficiency of portable air cleaner | |
| S | Number of susceptible individuals |
| t | Time (s) |
| V | Volume (m3) |
| Exposure time (h) | |
| Reference pressure difference (Pa) | |
| Pressure difference between zone j and zone i (Pa) |
References
- Comber, L.; Murchu, E.O.; Drummond, L.; Carty, P.G.; Walsh, K.A.; De Gascun, C.F.; Connolly, M.A.; Smith, S.M.; O’Neill, M.; Ryan, M.; et al. Airborne transmission of SARS-CoV-2 via aerosols. Rev. Med. Virol. 2021, 31, e2184. [Google Scholar] [CrossRef] [PubMed]
- Omicron Variant: What You Need to Know. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/coronavirus/2019-ncov/variants/omicron-variant.html (accessed on 10 January 2022).
- Map of COVID-19 Case Trends and Restrictions. Available online: https://www.usatoday.com/storytelling/coronavirus-reopening-america-map/ (accessed on 18 March 2022).
- COVID-19 Restrictions Easing Next Week, Fully Lifted on 21 March. Available online: https://novascotia.ca/news/release/?id=20220223008 (accessed on 18 March 2022).
- COVID-19 in Europe: England Ends all Restrictions and Removes Isolation Rule. Available online: https://www.euronews.com/2022/02/23/covid-19-in-europe-italy-to-end-state-of-emergency-and-ease-restrictions-in-april (accessed on 18 March 2022).
- Kurnitski, J.; Kiil, M.; Wargocki, P.; Boerstra, A.; Seppänen, O.; Olesen, B.; Morawska, L. Respiratory infection risk-based ventilation design method. Build. Environ. 2021, 206, 108387. [Google Scholar] [CrossRef]
- Li, Y.; Leung, G.M.; Tang, J.W.; Yang, X.; Chao, C.Y.H.; Lin, J.Z.; Lu, J.W.; Nielsen, P.V.; Niu, J.; Qian, H.; et al. Role of ventilation in airborne transmission of infectious agents in the built environment—A multidisciplinary systematic review. Indoor Air 2007, 17, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Buonanno, G.; Stabile, L.; Morawska, L. Estimation of airborne viral emission: Quanta emission rate of SARS-CoV-2 for infection risk assessment. Environ. Int. 2020, 141, 105794. [Google Scholar] [CrossRef] [PubMed]
- Riley, E.C.; Murphy, G.; Riley, R.L. Airborne spread of measles in a suburban elementary school. Am. J. Epidemiol. 1978, 107, 421–432. [Google Scholar] [CrossRef]
- Peng, Z.; Rojas, A.P.; Kropff, E.; Bahnfleth, W.; Buonanno, G.; Dancer, S.J.; Kurnitski, J.; Li, Y.; Loomans, M.G.; Marr, L.C. Practical indicators for risk of airborne transmission in shared indoor environments and their application to covid-19 outbreaks. Environ. Sci. Technol. 2022, 56, 1125–1137. [Google Scholar] [CrossRef]
- Dai, H.; Zhao, B. Association of the infection probability of COVID-19 with ventilation rates in confined spaces. Build. Simul. 2020, 13, 1321–1327. [Google Scholar] [CrossRef]
- Shen, J.; Kong, M.; Dong, B.; Birnkrant, M.J.; Zhang, J. A systematic approach to estimating the effectiveness of multi-scale IAQ strategies for reducing the risk of airborne infection of SARS-CoV-2. Build. Environ. 2021, 200, 107926. [Google Scholar] [CrossRef]
- Stabile, L.; Pacitto, A.; Mikszewski, A.; Morawska, L.; Buonanno, G. Ventilation procedures to minimize the airborne transmission of viruses in classrooms. Build. Environ. 2021, 202, 108042. [Google Scholar] [CrossRef]
- Barbosa, B.P.P.; de Carvalho Lobo Brum, N. Ventilation mode performance against airborne respiratory infections in small office spaces: Limits and rational improvements for Covid-19. J. Braz. Soc. Mech. Sci. Eng. 2021, 43, 316. [Google Scholar] [CrossRef]
- Bertone, M.; Mikszewski, A.; Stabile, L.; Riccio, G.; Cortellessa, G.; d′Ambrosio, F.R.; Papa, V.; Morawska, L.; Buonanno, G. Assessment of SARS-CoV-2 airborne infection transmission risk in public buses. Geosci. Front. 2022, 13, 101398. [Google Scholar] [CrossRef]
- Yates, T.A.; Khan, P.Y.; Knight, G.M.; Taylor, J.G.; McHugh, T.D.; Lipman, M.; White, R.G.; Cohen, T.; Cobelens, F.G.; Wood, R.; et al. The transmission of Mycobacterium tuberculosis in high burden settings. Lancet Infect. Dis. 2016, 16, 227–238. [Google Scholar] [CrossRef]
- Shrestha, P.; DeGraw, J.W.; Zhang, M.; Liu, X. Multizonal modeling of SARS-CoV-2 aerosol dispersion in a virtual office building. Build. Environ. 2021, 206, 108347. [Google Scholar] [CrossRef]
- Kennedy, M.; Lee, S.J.; Epstein, M. Modeling aerosol transmission of SARS-CoV-2 in multi-room facility. J. Loss Prev. Process Ind. 2021, 69, 104336. [Google Scholar] [CrossRef]
- Pease, L.F.; Wang, N.; Salsbury, T.I.; Underhill, R.M.; Flaherty, J.E.; Vlachokostas, A.; Kulkarni, G.; James, D.P. Investigation of potential aerosol transmission and infectivity of SARS-CoV-2 through central ventilation systems. Build. Environ. 2021, 197, 107633. [Google Scholar] [CrossRef]
- Cotman, Z.J.; Bowden, M.J.; Richter, B.P.; Phelps, J.H.; Dibble, C.J. Factors affecting aerosol SARS-CoV-2 transmission via HVAC systems; a modeling study. PLOS Comput. Biol. 2021, 17, e1009474. [Google Scholar] [CrossRef]
- ASHRAE. ASHRAE Position Document on Infectious Aerosols; ASHRAE: Atlanta, GA, USA, 2020. [Google Scholar]
- REHVA. REHVA COVID-19 Guidance Document; REHVA: Ixelles, Belgium, 2020. [Google Scholar]
- Guo, M.; Xu, P.; Xiao, T.; He, R.; Dai, M.; Miller, S.L. Review and comparison of HVAC operation guidelines in different countries during the COVID-19 pandemic. Build. Environ. 2021, 187, 107368. [Google Scholar] [CrossRef]
- Axley, J.W. Multi-zone dispersal analysis by element assembly. Build. Environ. 1989, 24, 113–130. [Google Scholar] [CrossRef]
- Walton, G. Airflow and multiroom thermal analysis. ASHRAE Trans. 1982, 88, 78–91. [Google Scholar]
- Li, Y.; Duan, S.; Yu, I.; Wong, T. Multi-zone modeling of probable SARS virus transmission by airflow between flats in Block E, Amoy Gardens. Indoor Air 2005, 15, 96–111. [Google Scholar] [CrossRef]
- Deru, M.; Field, K.; Studer, D.; Benne, K.; Griffith, B.; Torcellini, P.; Liu, B.; Halverson, M.; Winiarski, D.; Rosenberg, M. US Department of Energy Commercial Reference Building Models of the National Building Stock; National Renewable Energy Laboratory: Golden, CO, USA, 2011.
- Ng, L.C.; Musser, A.; Persily, A.K.; Emmerich, S.J. Airflow and Indoor Air Quality Models of DOE Reference Commercial Buildings; National Institute of Standards and Technology: Gaithersburg, MD, USA, 2012; p. 12.
- Dols, W.; Polidoro, B. CONTAM User Guide and Program Documentation; version 3.4; National Institute of Standards and Technology: Gaithersburg, MD, USA, 2020; p. 1887.
- Ng, L.; Musser, A.; Persily, A.; Emmerich, S. Airflow and Indoor Air Quality Models of DOE Prototype Commercial Buildings; Technical Note (NIST TN); National Institute of Standards and Technology: Gaithersburg, MD, USA, 2019. [CrossRef]
- Yan, S.; Wang, L.; Birnkrant, M.J.; Zhai, J.; Miller, S.L. Evaluating SARS-CoV-2 airborne quanta transmission and exposure risk in a mechanically ventilated multizone office building. Build. Environ. 2022, 219, 109184. [Google Scholar] [CrossRef] [PubMed]
- Wells, W.F. Airborne Contagion and Air Hygiene: An Ecological Study of Droplet Infections; Commonwealth Fund: New York, NY, USA, 1955. [Google Scholar]
- Aganovic, A.; Bi, Y.; Cao, G.; Drangsholt, F.; Kurnitski, J.; Wargocki, P. Estimating the impact of indoor relative humidity on SARS-CoV-2 airborne transmission risk using a new modification of the Wells-Riley model. Build. Environ. 2021, 205, 108278. [Google Scholar] [CrossRef] [PubMed]
- Buonanno, G.; Morawska, L.; Stabile, L. Quantitative assessment of the risk of airborne transmission of SARS-CoV-2 infection: Prospective and retrospective applications. Environ. Int. 2020, 145, 106112. [Google Scholar] [CrossRef] [PubMed]
- Thatcher, T.L.; Lai, A.C.K.; Moreno-Jackson, R.; Sextro, R.G.; Nazaroff, W.W. Effects of room furnishings and air speed on particle deposition rates indoors. Atmos. Environ. 2002, 36, 1811–1819. [Google Scholar] [CrossRef]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef]
- Miller, S.L.; MacHer, J.M. Evaluation of a Methodology for Quantifying the Effect of Room Air Ultraviolet Germicidal Irradiation on Airborne Bacteria. Aerosol Sci. Technol. 2000, 33, 274–295. [Google Scholar] [CrossRef]
- Liu, Y.; Ning, Z.; Chen, Y.; Guo, M.; Liu, Y.; Gali, N.K.; Sun, L.; Duan, Y.; Cai, J.; Westerdahl, D.; et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature 2020, 582, 557–560. [Google Scholar] [CrossRef]
- ASHRAE. Method of Testing General Ventilation Air-Cleaning Devices for Removal Efficiency by Particle Size; American Society of Heating, Refrigerating and Air-Conditioning Engineer: Atlanta, GA, USA, 2018. [Google Scholar]
- Miller-Leiden, S.; Lohascio, C.; Nazaroff, W.W.; Macher, J.M. Effectiveness of in-Room Air Filtration and Dilution Ventilation for Tuberculosis Infection Control. J. Air Waste Manag. Assoc. 1996, 46, 869–882. [Google Scholar] [CrossRef]
- Kujundzic, E.; Hernandez, M.; Miller, S.L. Ultraviolet germicidal irradiation inactivation of airborne fungal spores and bacteria in upper-room air and HVAC in-duct configurations. J. Environ. Eng. Sci. 2007, 6, 1–9. [Google Scholar] [CrossRef]
- Pan, J.; Harb, C.; Leng, W.; Marr, L.C. Inward and outward effectiveness of cloth masks, a surgical mask, and a face shield. Aerosol Sci. Technol. 2021, 55, 718–733. [Google Scholar] [CrossRef]
- U.S. EPA. Exposure Factors Handbook 2011 Edition (Final Report); U.S. Environmental Protection Agency: Washington, DC, USA, 2011.
- Chu, D.K.W.; Gu, H.; Chang, L.D.J.; Cheuk, S.S.Y.; Gurung, S.; Krishnan, P.; Ng, D.Y.M.; Liu, G.Y.Z.; Wan, C.K.C.; Tsang, D.N.C.; et al. SARS-CoV-2 Superspread in Fitness Center, Hong Kong, China, March 2021. Emerg. Infect. Dis. 2021, 27, 2230–2232. [Google Scholar] [CrossRef]
- Li, Y.; Qian, H.; Hang, J.; Chen, X.; Cheng, P.; Ling, H.; Wang, S.; Liang, P.; Li, J.; Xiao, S.; et al. Probable airborne transmission of SARS-CoV-2 in a poorly ventilated restaurant. Build. Environ. 2021, 196, 107788. [Google Scholar] [CrossRef]
- Emmerich, S.J.; Heinzerling, D.; Choi, J.-I.; Persily, A.K. Multizone modeling of strategies to reduce the spread of airborne infectious agents in healthcare facilities. Build. Environ. 2013, 60, 105–115. [Google Scholar] [CrossRef]
- Miller, S.L.; Nazaroff, W.W.; Jimenez, J.L.; Boerstra, A.; Buonanno, G.; Dancer, S.J.; Kurnitski, J.; Marr, L.C.; Morawska, L.; Noakes, C. Transmission of SARS-CoV-2 by inhalation of respiratory aerosol in the Skagit Valley Chorale superspreading event. Indoor Air 2020, 31, 314–323. [Google Scholar] [CrossRef]
- Wang, L.; Chen, Q. Validation of a Coupled Multizone-CFD Program for Building Airflow and Contaminant Transport Simulations. HVACR Res. 2007, 13, 267–281. [Google Scholar] [CrossRef]
- Wang, L.L.; Dols, W.S.; Chen, Q. Using CFD Capabilities of CONTAM 3.0 for Simulating Airflow and Contaminant Transport in and around Buildings. HVACR Res. 2010, 16, 749–763. [Google Scholar] [CrossRef]



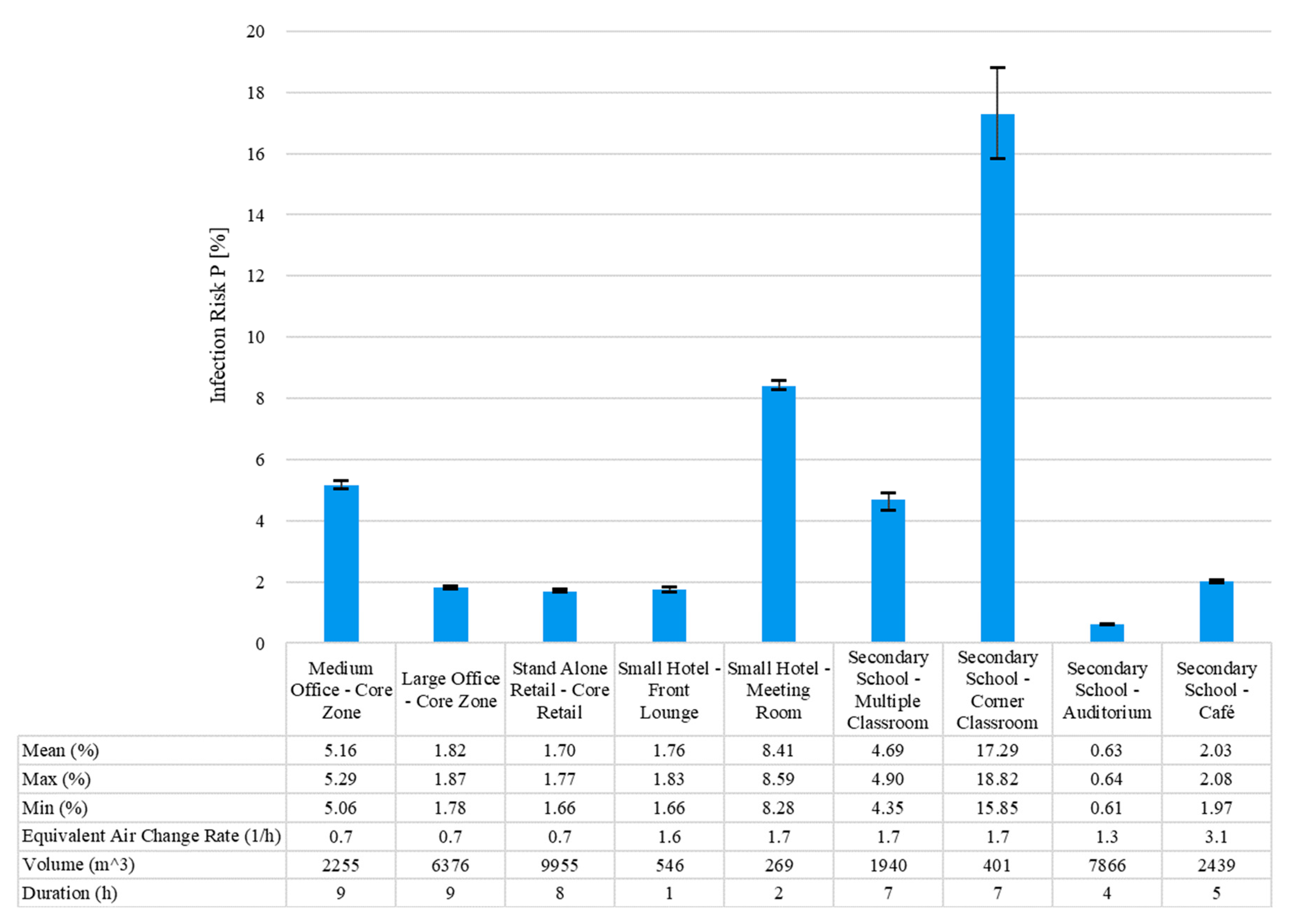


| Building Type | Area (m2) | Volume (m3) | HVAC System Type | Supply Airflow Rates (m3/s) | OA Ratio (%) | Baseline Air Change Rate (1/h) | Maximum Occupancy | Duration of Exposure Modeled |
|---|---|---|---|---|---|---|---|---|
| Medium Office (Core Zone) | 822 | 2255 | variable air volume (VAV) | 2.95 | 14.4 | 0.68 | 53 | 8:00–17:00 (9 h) |
| Large Office (Core Zone) | 2324 | 6376 | variable air volume (VAV) | 8.25 | 14 | 0.65 | 134 | 8:00–17:00 (9 h) |
| Stand-Alone Retail (Core Retail) | 1632 | 9955 | constant-volume single-zone system | 5.67 | 33.3 | 0.68 | 258 | Infector (Staff): 8:00–22:00 Susceptible (Customer): 8:00–16:00 Susceptible |
| Small Hotel (Front Lounge) | 163 | 546 | packaged terminal air conditioner (PTAC) | 0.74 | 32.1 | 1.57 | 53 | Infector (Staff): 5:00–20:00 Susceptible (Guest): 12:00–13:00 (1 h) |
| Small Hotel (Meeting Room) | 80 | 269 | packaged terminal air conditioner (PTAC) | 0.34 | 37 | 1.68 | 43 | Infector: 13:00–15:00 Susceptible: 13:00–15:00 (2 h) |
| Secondary School (Classroom) | 485 | 1940 | variable air volume (VAV) | 1.27 | 73 | 1.72 | 180 | 8:00–15:00 (7 h) |
| Secondary School (Corner Classroom) | 100 | 401 | variable air volume (VAV) | 0.26 | 73 | 1.70 | 37 | 8:00–15:00 (7 h) |
| Secondary School (Auditorium) | 1967 | 7866 | constant air volume (CAV) | 4.10 | 70 | 1.31 | 1596 | 15:00–19:00 (4 h) |
| Secondary School (Café) | 609 | 2439 | constant air volume (CAV) | 2.95 | 70 | 3.05 | 67 | 9:00–14:00 (5 h) |
| Input | Parameters | Reference | |
|---|---|---|---|
| Initial concentration | 0 quanta/m3 | - | |
| Generation rate | 65 quanta/h | [8,34] | |
| Quanta removal | Surface deposition rate | 0.3 h−1 | [35] |
| Quanta deactivation rate | 0.63 h−1 | [36] | |
| UVGI (in-room) Qe | 4 h−1 | [37] | |
| Default quanta particle size | 1–3 μm | [38] | |
| MERV8 removal efficiency | 20% | [39] | |
| MERV11 removal efficiency | 65% | [39] | |
| MERV13 removal efficiency | 85% | [39] | |
| HEPA removal efficiency | 99% | [40] | |
| UVGI (in-duct) removal efficiency | 87% | [41] | |
| PAC1 | 0.46 m3/s | From manufacturer | |
| PAC2 | 1 m3/s | ||
| PAC3 | 1.45 m3/s | ||
| PAC4 | 17 m3/s | ||
| Mask wearing | Mask wearing percentage | 0/100% | - |
| Outward protection effectiveness | 50% | [42] | |
| Inward protection effectiveness | 30% | [42] | |
| Breathing rate | 0.72 m3/h | [43] | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yan, S.; Wang, L.; Birnkrant, M.J.; Zhai, Z.; Miller, S.L. Multizone Modeling of Airborne SARS-CoV-2 Quanta Transmission and Infection Mitigation Strategies in Office, Hotel, Retail, and School Buildings. Buildings 2023, 13, 102. https://doi.org/10.3390/buildings13010102
Yan S, Wang L, Birnkrant MJ, Zhai Z, Miller SL. Multizone Modeling of Airborne SARS-CoV-2 Quanta Transmission and Infection Mitigation Strategies in Office, Hotel, Retail, and School Buildings. Buildings. 2023; 13(1):102. https://doi.org/10.3390/buildings13010102
Chicago/Turabian StyleYan, Shujie, Liangzhu (Leon) Wang, Michael J. Birnkrant, Zhiqiang (John) Zhai, and Shelly L. Miller. 2023. "Multizone Modeling of Airborne SARS-CoV-2 Quanta Transmission and Infection Mitigation Strategies in Office, Hotel, Retail, and School Buildings" Buildings 13, no. 1: 102. https://doi.org/10.3390/buildings13010102
APA StyleYan, S., Wang, L., Birnkrant, M. J., Zhai, Z., & Miller, S. L. (2023). Multizone Modeling of Airborne SARS-CoV-2 Quanta Transmission and Infection Mitigation Strategies in Office, Hotel, Retail, and School Buildings. Buildings, 13(1), 102. https://doi.org/10.3390/buildings13010102









_Wang.png)


