Occlusal Scheme Effect on the Biomechanical Response of Full-Arch Dental Prosthesis Supported by Titanium Implants: A Systematic Review
Abstract
:1. Introduction
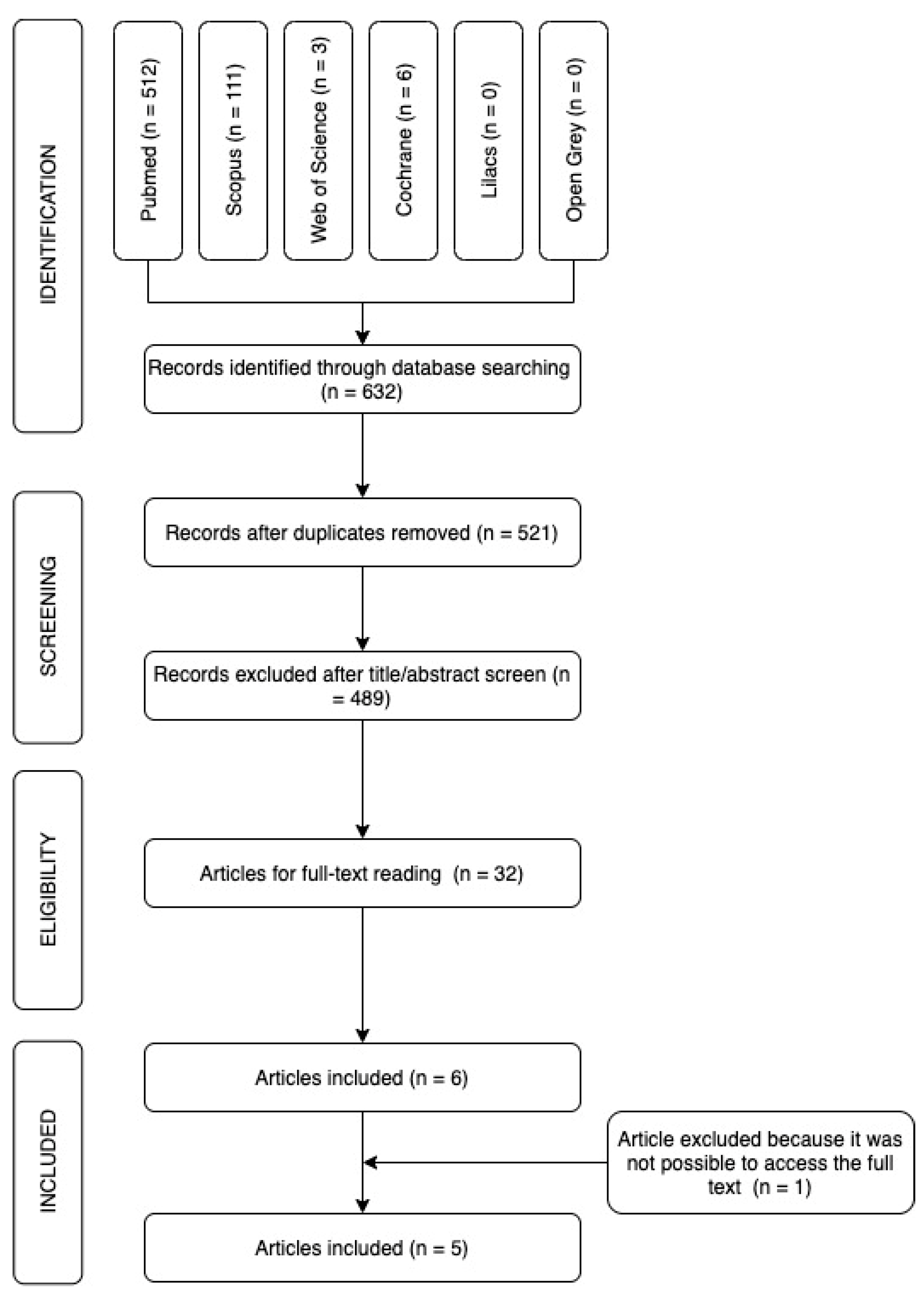
2. Materials and Methods
2.1. Protocol Registration
2.2. Focus Question
- Population (patients)—Dental implants/dental prosthesis, implant supported/edentulous mouth;
- Intervention—occlusal scheme/dental occlusion/Implant-protected occlusion/occlusal stability;
- Comparison—none;
- Outcome—dental stress distribution/ mouth rehabilitation.
2.3. Literature Search
- Inclusion: Dental rehabilitation with titanium implant, Implant-protected occlusion, edentulous mouth, full-arch rehabilitation.
- Exclusion: Rehabilitation without dental implant. Single implant rehabilitation.
| PubMed = 512 * |
| P = (((((“Dental implants”[MeSH Terms]) OR (“Dental implants”[Title/Abstract])) OR (“Dental Implant”[Title/Abstract])) OR (Surgical Dental Prostheses[Title/Abstract])) OR (Edentulous Mouth[MeSH Terms])) OR (Edentulous Mouth[Title/Abstract]) AND I = ((((((((“Dental occlusion”[MeSH Terms]) OR (“Dental occlusion”[Title/Abstract])) OR (“Occlusion, Dental”[Title/Abstract])) OR (“Canine Guidance”[Title/Abstract])) OR (“Occlusal Guidance”[Title/Abstract])) OR (“Occlusal Plane”[Title/Abstract])) OR (“Occlusal scheme”[Title/Abstract])) OR (Implant-protected occlusion[Title/Abstract])) OR (“Occlusal stability”[Title/Abstract]) AND O = ((((“Dental stress analysis”[MeSH Terms]) OR (Dental stress distribution [Title/Abstract])) OR (“Prosthesis Failure”[MeSH Terms])) OR (“Mouth rehabilitation”[MeSH Terms])) OR (rehabilitations, mouth [Title/Abstract]) |
| Scopus = 111 |
| TITLE-ABS-KEY (“Dental implants” OR “Dental Implant” OR “Surgical Dental Prostheses” OR “Edentulous Mouth”)) AND (TITLE-ABS-KEY (“Dental occlusion” OR “Occlusion, Dental” OR “Canine Guidance” OR “Occlusal Guidance” OR “Occlusal Plane” OR “Occlusal scheme” OR “Implant-protected occlusion” OR “Occlusal stability”)) AND (TITLE-ABS-KEY (“Dental stress analysis” OR “Dental stress distribution” OR “Prosthesis Failure” OR “Mouth rehabilitation” OR “rehabilitations, mouth”)) |
| Web of Science = 3 |
| TS = (“Dental implants” OR “Dental implants” OR “Dental Implant” OR “Surgical Dental Prostheses” OR “Edentulous Mouth” OR “Edentulous Mouth”) AND TS = (“Dental occlusion” OR “Occlusion, Dental” OR “Canine Guidance” OR “Occlusal Guidance” OR “Occlusal Plane” OR “Occlusal scheme” OR “Implant-protected occlusion” OR “Occlusal stability”) AND TS = (“Dental stress analysis” OR “Dental stress distribution” OR “Prosthesis Failure” OR “Mouth rehabilitation” OR “rehabilitations, mouth”) |
| Cochrane Library = 6 |
| #1 MeSH descriptor: [Dental Implants] explode all trees 1481 #2 (“Dental implants” OR “Dental implant” OR “Surgical Dental Prostheses”):ti,ab,kw #3 #1 OR #2 #4 MeSH descriptor: [Mouth, Edentulous] explode all trees #5 (“Edentulous Mouth”):ti,ab,kw #6 #4 OR #5 #7 #3 OR #6 #8 MeSH descriptor: [Dental Occlusion] explode all trees #9 (“Dental occlusion” OR “Canine Guidance” OR “Occlusal Guidance” OR “Occlusal Plane” OR “Occlusal scheme” OR “Implant-protected occlusion” OR “Occlusal stability”):ti,ab,kw #10 #8 OR #9 #11 MeSH descriptor: [Dental Stress Analysis] explode all trees #12 (“Dental stress distribution”):ti,ab,kw #13 #11 OR #12 #14 MeSH descriptor: [Prosthesis Failure] explode all trees #15 MeSH descriptor: [Mouth Rehabilitation] explode all trees #16 (“rehabilitations, mouth”):ti,ab,kw 0 #17 #15 OR #16 #18 #13 OR #14 OR #17 #19 #7 AND #10 AND #18 |
| Lilacs = 0 |
| (MH: “Dental implants” OR “Dental implants” OR “Implantes Dentários” OR “Implantes Dentales” OR “dental implant” OR “Implante dentário” OR “Implante Dental” OR “Surgical Dental Prostheses” OR “Prótese Dentária Cirúrgica” OR “Prótesis Dental Quirúrgica” OR MH: “Edentulous Mouth” OR “Edentulous Mouth” OR “Boca Edêntula” OR “Boca Edéntula”) AND (MH: “Dental occlusion” OR “Dental occlusion” OR “Oclusão Dentária” OR “Oclusión Dental” OR “Canine Guidance” OR “Orientação de Canino” OR “Orientación Canina” OR “Occlusal Guidance” OR “Orientação Oclusal” OR “Orientación Oclusal” OR “Occlusal Plane” OR “Plano Oclusal” OR “Occlusal scheme” OR “Esquema oclusal” OR “Occlusal stability” OR “Estabilidade oclusal” OR “Estabilidad oclusal” OR “Implant-protected occlusion” OR “Oclusão protegida por implante” OR “Oclusión protegida por implantes”) AND (MH: “Dental stress analysis” OR “Dental stress distribution” OR “Distribuição de estresse dentário” OR “Distribución del estrés dental” OR MH: “Prosthesis Failure” OR MH: “Mouth rehabilitation” OR “Rehabilitations, mouth” OR “Reabilitações, boca” OR “Rehabilitaciones, boca”) |
| Open Grey = 0 |
2.4. Quality Assessment of Risk of Bias
3. Results
Quality Assessment of Risk of Bias
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Adell, R.; Lekholm, U.; Rockler, B.; Brånemark, P.-I. A 15-Year Study of Osseointegrated Implants in the Treatment of the Edentulous Jaw. Int. J. Oral Surg. 1981, 10, 387–416. [Google Scholar] [CrossRef]
- Taylor, T.D.; Agar, J.R. Twenty Years of Progress in Implant Prosthodontics. J. Prosthet. Dent. 2002, 88, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Hirsch, J.; Lekholm, U.; Thomsen, P. Differential Diagnosis and Treatment Strategies for Biologic Complications and Failing Oral Implants: A Review of the Literature. Int. J. Oral Maxillofac. Implant. 1999, 14, 473–490. [Google Scholar]
- Vervaeke, S.; Collaert, B.; Cosyn, J.; Deschepper, E.; De Bruyn, H. A Multifactorial Analysis to Identify Predictors of Implant Failure and Peri-Implant Bone Loss. Clin. Implant Dent. Relat. Res. 2015, 17, e298–e307. [Google Scholar] [CrossRef] [PubMed]
- Isidor, F. Loss of Osseointegration Caused by Occlusal Load of Oral Implants. A Clinical and Radiographic Study in Monkeys. Clin. Oral Implant. Res. 1996, 7, 143–152. [Google Scholar] [CrossRef]
- Adell, R. Tissue Integrated Prostheses in Clinical Dentistry. Int. Dent. J. 1985, 35, 259–265. [Google Scholar]
- Schwarz, M.S. Mechanical Complications of Dental Implants. Clin. Oral Implant. Res. 2000, 11, 156–158. [Google Scholar] [CrossRef]
- Rangert, B.R.; Sullivan, R.M.; Jemt, T.M. Load Factor Control for Implants in the Posterior Partially Edentulous Segment. Int. J. Oral Maxillofac. Implant. 1997, 12, 360–370. [Google Scholar]
- Koyano, K.; Esaki, D. Occlusion on Oral Implants: Current Clinical Guidelines. J. Oral Rehabil. 2015, 42, 153–161. [Google Scholar] [CrossRef]
- Nikolopoulou, F.; Ktena-agapitou, P. Rationale for Choices of Occlusal Schemes for Complete Dentures Supported by Implants. J. Oral Implantol. 2006, XXXII, 200–203. [Google Scholar] [CrossRef]
- Wismeijer, D.; van Waas, M.A.J.; Kalk, W. Factors to Consider in Selecting an Occlusal Concept for Patients with Implants in the Edentulous Mandible. J. Prosthet. Dent. 1995, 74, 380–384. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, 1–9. [Google Scholar] [CrossRef]
- Türker, N.; Alkiş, H.T.; Sadowsky, S.J.; Şebnem Büyükkaplan, U. Effects of Occlusal Scheme on All-on-Four Abutments, Screws, and Prostheses: A Three-Dimensional Finite Element Study. J. Oral Implantol. 2021, 47, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Falk, H.; Laurell, L.; Lundgren, D. Occlusal Interferences and Cantilever Joint Stress in Implant-Supported Prostheses Occluding with Complete Dentures. Int. J. Oral Maxillofac. Implant. 1990, 5, 70–77. [Google Scholar]
- Linkevicius, T.; Vladimirovas, E.; Grybauskas, S.; Puisys, A.; Rutkunas, V. Veneer Fracture in Implant-Supported Metal-Ceramic Restorations. Part I: Overall Success Rate and Impact of Occlusal Guidance. Stomatol. Balt. Dent. Maxilofac. J. 2008, 10, 133–139. [Google Scholar]
- Block, J.; Matalon, S.; Tanase, G.; Ormianer, Z. Effect of Restorative Configurations and Occlusal Schemes on Strain Levels in Bone Surrounding Implants. Implant. Dent. 2017, 26, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Greco, G.D.; de Las Casas, E.; Cornacchia, T.P.M.; de Magalhaes, C.S.; Moreira, A.N. Standard of Disocclusion in Complete Dentures Supported by Implants without Free Distal Ends: Analysis by the Finite Elements Method. J. Appl. Oral Sci. 2012, 20, 64–69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Türker, N.; Büyükkaplan, U.S.; Sadowsky, S.J.; Özarslan, M.M. Finite Element Stress Analysis of Applied Forces to Implants and Supporting Tissues Using the “All-on-Four” Concept with Different Occlusal Schemes. J. Prosthodont. 2019, 28, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Swaminathan, Y.; Rao, G. Implant Protected Occlusion. J. Dent. Med. Sci. 2013, 11, 20–25. [Google Scholar] [CrossRef]
- Misch, C.E.; Bides, M.W. Implant-Protected Occlusion. Int. J. Dent. Symp. 1994, 2, 32–37. [Google Scholar]
- Chen, Y.Y.; Kuan, C.L.; Wang, Y.B. Implant Occlusion: Biomechanical Considerations for Implant-Supported Prostheses. J. Dent. Sci. 2008, 3, 65–74. [Google Scholar]
- Kim, Y.; Oh, T.-J.; Misch, C.E.; Wang, H.-L. Occlusal Considerations in Implant Therapy: Clinical Guidelines with Biomechanical Rationale. Clin. Oral Implant. Res. 2005, 16, 26–35. [Google Scholar] [CrossRef]
- Felice, P.; Checchi, L.; Barausse, C.; Pistilli, R.; Sammartino, G.; Masi, I.; Ippolito, D.R.; Esposito, M. Posterior jaws rehabilitated with partial prostheses supported by 4.0 × 4.0 mm2 or by longer implants: One-year post-loading results from a multicenter randomised controlled trial. Eur. J. Oral Implantol. 2016, 9, 35–45. [Google Scholar]
- Cannizzaro, G.; Felice, P.; Gherlone, E.; Barausse, C.; Ferri, V.; Leone, M.; Trullenque-Eriksson, A.; Esposito, M. Immediate loading of two (fixed-on-2) vs four (fixed-on-4) implants placed with a flapless technique supporting mandibular cross-arch fixed prostheses: 3-year results from a pilot randomised controlled trial. Eur. J. Oral Implantol. 2017, 10, 133–145. [Google Scholar]
- Wie, H. Registration of Localization, Occlusion and Occluding Materials for Failing Screw Joints in the Brånemark Implant System. Clin. Oral Implant. Res. 1995, 6, 47–53. [Google Scholar] [CrossRef]
- Ogawa, T.; Ogimoto, T.; Koyano, K. Pattern of Occlusal Contacts in Lateral Positions: Canine Protection and Group Function Validity in Classifying Guidance Patterns. J. Prosthet. Dent. 1998, 80, 67–74. [Google Scholar] [CrossRef]
- Chaichanasiri, E.; Nanakorn, P.; Tharanon, W.; Sloten, J. Vander Finite Element Analysis of Bone around a Dental Implant Supporting a Crown with a Premature Contact. J. Med. Assoc. Thail. 2009, 92, 1336–1344. [Google Scholar]
- Valente, F.; Scarano, A.; Murmura, G.; Varvara, G.; Sinjari, B.; Mandelli, F.; Piattelli, M.; Caputi, S.; Traini, T. Collagen Fibres Orientation in the Bone Matrix around Dental Implants: Does the Implant’s Thread Design Play a Role? Int. J. Mol. Sci. 2021, 22, 7860. [Google Scholar] [CrossRef] [PubMed]
- Silveira, M.P.M.; Campaner, L.M.; Bottino, M.A.; Nishioka, R.S.; Borges, A.L.S.; Tribst, J.P.M. Influence of the dental implant number and load direction on stress distribution in a 3-unit implant-supported fixed dental prosthesis. Dent. Med. Probl. 2021, 58, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; Dal Piva, A.M.D.O.; Gonçalves, N.I.Ê.; Borges, A.L.S.; Bottino, M.A.; Kleverlaan, C.J. Polymerization shrinkage and push-out bond strength of different composite resins for sealing the screw-access hole on implant-supported crowns. J. Adhes. Dent. 2020, 22, 523–530. [Google Scholar] [PubMed]
- Bottino, M.A.; de Oliveira, F.R.; Sabino, C.F.; Dinato, J.C.; Silva-Concílio, L.R.; Tribst, J.P.M. Survival Rate and Deformation of External Hexagon Implants with One-Piece Zirconia Crowns. Metals 2021, 11, 1068. [Google Scholar] [CrossRef]
| First Author (Year) [Reference] | n | Patients Characteristics | Observation Time | Type of Analysis | Ethical Comitêe |
|---|---|---|---|---|---|
| Linkevicius et al. (2008) [15] | 251-(21) | Male and Female with the average age of 42.1 ± 11.3 years (range from 19 to 76 years old) | 1–48 months | Clinical inspection—Ceramic failure | All the patients included into the study gave informed content to use |
| Falk et al. (1990) [14] | 8 | Six men and two women participated in this study. Their mean age was 56 years (range 43 to 65) | Immediately evaluation | Force recording. Mingograf jet recorder (Elema Schönander, Solna, Sweden) via a 9-V battery-powered bridge amplifier. The occlusal forces were then measured according to a standardized test program. | Ethical disclosure not mentioned. Patients from Department of Prosthodontics at The Institute for Postgraduate Dental Education, Jönköping, Sweden. |
| Part A | |||||||
| First Author (Year) [Reference] | Country | Study Type | Purpose of Study | Analyzed Groups | Analyzed Occlusion | Test Type | Results |
| Greco et al. (2010) [17] | Brazil | FEA | Compared the stresses generated by the disocclusion in the canine guide occlusion (CGO) and bilateral balanced occlusion (BBO) on the implants and metallic infrastructure of a modified Brånemark protocol | (1) Nodal load of 15 N with an angle of 45° to the canine tooth—CGO (2) Nodal load of 15 N with a angle of 45° distributed across three teeth—BBO | Not mentioned | Linear elastic static analysis (maximum stress) | The disocclusion in BBO induced lower tensions than those in CGO in a mandibular complete denture supported by implants without free distal ends |
| Türker et al. (2019) [13] | Turkey and USA | FEA | Evaluate stress distributions on implants and alveolar bone due to occlusal load produced during chewing by prostheses prepared according to the All-on-Four concept with different occlusal schemes | (1) CGO: occlusal scheme prepared according to canine-guided occlusion (2) GFO: occlusal scheme prepared according to group function occlusion (3) BBO: occlusal scheme prepared according to bilateral balanced occlusion (4) LO: occlusal scheme prepared according to lingualized occlusion (5) MO: occlusal scheme prepared according to monoplane occlusion | Maximum intercuspation (450 N) Lateral movement (93 N to CGO; 200 N to GFO; 400 N to BBO, LO and MO) Protrusive movement (94 N to CGO and CFO; 400 N to BBO, LO and MO) | Stress outputs for the maxilla and mandible were taken as maximum principal stress (Pmax) and minimum principal stress (Pmin). Von Mises stress values were obtained for the implants | The highest stress values on alveolar bone occurred around the neck region of the implants in cortical bone, and the highest stress values on implants occurred at the neck region of the implants The highest stress values were observed in maximum intercuspation with monoplane occlusion, during protrusive movement with BBO, and during lateral movement with bilateral balanced and monoplane occlusion The lowest stress values were observed with canine- guided occlusion in all conditions and on all structures |
| Block et al. (2017) [16] | Israel | In vitro | Investigate the effect of implant insertion on the strain levels in bovine bone and to evaluate the effect of simulated mastication cycles on the strain levels around implants, in splinted and nonsplinted restorations with different occlusal schemes. | Full splint (FS) loading: complete cross-arch splint force on entire metal plate. Segmented cross-arch splint (SS) loading: metal plate cut in the midline and force applied on the entire metal plate. 3. Canine loading (CL): disconnecting right canine from distal teeth while maintaining proximal contact with adjacent premolar. Metal plate also cut accordingly. Load applied on tooth 6. Premolar loading:Premolar loading (PL): splinted group function restoration in same configuration as in CL (teeth 4 and 3 connected). Load applied on teeth 5 and 4.Premolar-segmented loading (PSL): nonsplinted group function disconnecting second premolar from first molar while maintaining proximal contacts with adjacent teeth. Metal plate also cut accordingly. Load applied on teeth 5 and 4. Single implant loading (SL): loading of first molars full separation of tooth 3 from adjacent teeth. Load applied only on tooth 3. | Canine guidance, and group function configurations. | The restoration was loaded by an Instron machine (model 4502; Instron Corp., Buckinghamshire, United Kingdom) with a force amplitude of 135 N at a sinus of 1 Hz for 300 cycles, simulating 5 min of mastication. Strain was measured during loading, and residual strain measurements were recorded after loading stopped | Comparing the 3 different guidance configurations, PL presented the most favorable strain results both in loading, showing the best distribution of vertical compared with horizontal strain, and in residual strain with the lowest horizontal strain values (p < 0.05). The least favorable strain results were in CL where there were the highest levels of horizontal strain in loading and even higher levels of horizontal residual strain (p < 0.05) Premolar loading guidance presented the most favorable loading and residual strain results (p < 0.05) |
| Linkevicius et al. (2008) [15] | Lithuania | Clinical Trials | Define the fracture rate of implant supported metal-ceramic restorations delivered in private practice, and to identify if a restoration’s contact during eccentric mandible movements has any influence on ceramic fracture rates | A regular occlusal scheme was applied. Habitual occlusal position,occlusal contacts were not positioned on oblique planes and posterior prostheses did not have contact during eccentric mandible movements 3 types of rehabilitations: - single crowns - fixed partial dentures - full cross-arch reconstructions 4 follow up time groups: - 1 year - 1–2 years - 2–3 years - Over 3 years | Eccentric mandibular movements | Clinical Inspected for the presence of mechanical complications, namely ceramic fractures. They were distinguished as: adhesive co-adhesive | Full-arch metal-ceramic restorations experienced 38.1% chipping.The majority of the failures in the current study were of co-adhesive kind The difference between the full-arch restorations and single or partial fixed crown groups was found to be statistically significant. It was concluded that 54.2%) of all failures occurred in guiding restorations Consequently, contact during eccentric mandibular movements significantly increases the possibility of veneer complication |
| Falk et al. (1990) [14] | Sweden | Clinical Trials | The aim of this study was to determine whether a small, experimentally introduced, premature occlusal contact on the distal cantilever unit in dentitions with fixture-supported prostheses occluding with complete dentures would further amplify the unfavorable distribution of axially directed occlusal forces | Basic occlusion with simultaneous occlusal contacts in habitual occlusion interfered occlusion in habitual occlusion Basic occlusion in preferred chewing side.Interfered occlusion with a 100-µm-high premature occlusal contact on the second cantilever unit of the preferred chewing side. | Closing forces in habitual occlusion and chewing movements and preferred and non-preferred side. | Local and total maximal closing forces in habitual occlusion Mean local and total chewing forces calculated from one randomly selected chewing sequence.For force recording, the transducers were connected to a Mingograf jet recorder (Elema Schönander, Solna, Sweden) via a 9-V battery-powered bridge amplifier. The occlusal forces were then measured according to a standardized test program. | The premature occlusal contact of the preferred chewing side had no influence on the total maximal closing forces as compared to basic occlusion. The group mean local closing force at the interfered was significantly increased (p < 0.05). The interfered occlusion resulted in a slight, although nonsignificant, increase of the vertical bending stress during closing but had no effect on the chewing vertical bending stress |
| Part B | |||||||
| First Author (Year) [Reference] | Region of Study | Number of Implants | Feature of the Implants | Materials Type | Antagonist Type | ||
| Greco et al. (2010) [17] | A model simulating a jaw | 5 installed between the mental foramen, with a distance of 4 mm between their platforms and 2 located at the midpoint of the occlusal surface of the first molar | All implants were cylindrical. The dimension of 13 mm in height and 3.75 mm in diameter is about the 5 implants in anterior area; 5 mm in height and 5 mm in diameter is about the 2 implantes in posterior area | Implants anterior area: (Brånemark System® Mk III Groovy; Nobel® Biocare, Zürich-Flughafen, Switzerland); Posterior area: (Titamax WS®; Neodent®, Curitiba, PR, Brazil) Prosthetic components made of titanium were 3 mm in height (Multi-unit Abutment®; Nobel Biocare®) A nickel-chromium infrastructure (Wiron® BEGO, Goldschlangerar, Bremen, Germany) with a thickness of 6 mm, a height of 4 mm and a total length of 112 mm with free distal ends 12 dental elements in acrylic resin with a range of 2 mm of gingival | Not applicable | ||
| Türker et al. (2019) [13] | Human maxilla and jaw | 4 implants in maxilla: distance from the midline to the anterior implant in the was 15.4 mm, the distance between the two implants was 30.8 mm, and the distance between the anterior and posterior implants was 31 mm 4 implants in jaw: the distance from the midline to the anterior implant was 14.2 mm, the distance between the anterior two implants was 28.4 mm, and the distance between the anterior and posterior implants was 30.2 mm | The implants were internal hexagon type. Distal sloping of posterior region implants was performed at 40° for both the maxilla and mandible Dimension of 4 × 10 mm2 for the anterior region and 4 × 13 mm2 for the posterior region | Implants: OsseoSpeed tx 4.0 S Astra Tech; Dentsply Sirona, York, PA Flat abutment for the anterior region (20° UniAbutment 3.5/4.0; Astra Tech), and angulated abutment (Angled Abutment 3.5/4.0; Astra Tech) The bar structure in the maxilla was 5 mm wide, 3 mm high, and 95.8 mm long. The bar structure in the mandible was 94.8 mm long, and despite variation in different regions, it was 5 mm wide and 3 mm long on average (not mentioned the material) Teeth with sim- ilar crown sizes and crown widths were chosen for all occlusal concepts (Ivostar; Ivoclar Vivadent) | All-on-Four protocols | ||
| Block et al. (2017) [16] | Bovine jaw and maxillary teeth was set up | 8 Implants, teeth location numbers: 2, 3, 4, 6, and 11, 13, 14, 15 (position of canines, second premolars, first and second molars). | Not mentioned | Titanium-alloy abutments were connected to the implant analogs.(SPI;Alpha-BioTec, Petah-Tiqwa, Israel). A full-arch cast metal restoration were placed on the abutments. This restoration consisted of a metal framework with 5 dental units on each side of the arch. | Not applicable | ||
| Linkevicius et al. (2008) [15] | Maxillary and jaw | Not mentioned | Not mentioned | Titanium implants (BioHorizons, Ala, USA) Metal- ceramic. frameworks alloy Co-Cr was used as base metal. Different ceramics were used for layering in fabrication of prostheses GC Initial (GC, Japan), Inspiration (Heimerle-Meule, Germany) Design (Ivoclar, Liechtenstein) Vita VM7 (Vita Zahnfabrik, Germany) | Full arch rehabilitation | ||
| Falk et al. (1990) [14] | Anterior region of the jaw, between the mental foramina | 5 or 6 titanium implants | The shape of the cantilever joints was roughly elliptic, and the dimensions of the joints as well as the whole metal framework of the construction were approximately 5 mm high and 4 mm wide. The yield strength for hardened type III gold alloy is approximately 440 N/mm2, and for unhardened it is approximately 310 N/mm2 | Titanium fixtures. The metal frameworks were cast in type III dental gold alloy | Complete dentures | ||
| Sample Calculation or Numerical Model Validation | Sample Randomization | The Number (n) of Specimens/ Patients Is Clear | Parameters for Clinical Analysis Standardized or Boundary Conditions with Proper References | Ethical Committee | Blind Analysis | Parameters for the Mechanical Test | Overall Risk of Bias | |
|---|---|---|---|---|---|---|---|---|
| Linkevicius et al. (2008) [15] |  |  |  |  |  |  | N/A |  |
| Falk et al. (1990) [14] |  |  |  |  |  |  | N/A |  |
| Block et al. (2017) [16] |  | N/A |  |  | N/A | N/A |  |  |
| Greco et al. (2010) [17] |  | N/A |  |  | N/A | N/A |  |  |
| Türker et al. (2019) [13] |  | N/A |  |  | N/A | N/A |  |  |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gomes, L.C.L.; Pierre, F.Z.; Tribst, J.P.M.; Ramos, N.d.C.; Bresciani, E.; de Araújo, R.M.; Júnior, L.N.; Bottino, M.A. Occlusal Scheme Effect on the Biomechanical Response of Full-Arch Dental Prosthesis Supported by Titanium Implants: A Systematic Review. Metals 2021, 11, 1574. https://doi.org/10.3390/met11101574
Gomes LCL, Pierre FZ, Tribst JPM, Ramos NdC, Bresciani E, de Araújo RM, Júnior LN, Bottino MA. Occlusal Scheme Effect on the Biomechanical Response of Full-Arch Dental Prosthesis Supported by Titanium Implants: A Systematic Review. Metals. 2021; 11(10):1574. https://doi.org/10.3390/met11101574
Chicago/Turabian StyleGomes, Laís Carolina Landim, Fernanda Zapater Pierre, João Paulo Mendes Tribst, Nathália de Carvalho Ramos, Eduardo Bresciani, Rodrigo Máximo de Araújo, Lafayette Nogueira Júnior, and Marco Antonio Bottino. 2021. "Occlusal Scheme Effect on the Biomechanical Response of Full-Arch Dental Prosthesis Supported by Titanium Implants: A Systematic Review" Metals 11, no. 10: 1574. https://doi.org/10.3390/met11101574
APA StyleGomes, L. C. L., Pierre, F. Z., Tribst, J. P. M., Ramos, N. d. C., Bresciani, E., de Araújo, R. M., Júnior, L. N., & Bottino, M. A. (2021). Occlusal Scheme Effect on the Biomechanical Response of Full-Arch Dental Prosthesis Supported by Titanium Implants: A Systematic Review. Metals, 11(10), 1574. https://doi.org/10.3390/met11101574







