Post-Exercise Sweat Loss Estimation Accuracy of Athletes and Physically Active Adults: A Review
Abstract
:1. Introduction
2. Methods
Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Convertino, V.A.; Armstrong, L.E.; Coyle, E.F.; Mack, G.W.; Sawka, M.N.; Senay, L.C., Jr.; Sherman, W.M. American College of Sports Medicine position stand. Exercise and fluid replacement. Med. Sci. Sports Exerc. 1996, 28, i–vii. [Google Scholar] [CrossRef] [PubMed]
- Casa, D.J.; Armstrong, L.E.; Hillman, S.K.; Montain, S.J.; Reiff, R.V.; Rich, B.S.; Roberts, W.O.; Stone, J.A. National Athletic Trainers’ Association position statement: Fluid replacement for athletes. J. Athl. Train. 2000, 35, 212–224. [Google Scholar] [PubMed]
- Sawka, M.N.; Burke, L.M.; Eichner, E.R.; Maughan, R.J.; Montain, S.J.; Stachenfeld, N.S. American College of Sports Medicine position stand. Exercise and fluid replacement. Med. Sci. Sports Exerc. 2007, 39, 377–390. [Google Scholar] [PubMed] [Green Version]
- McDermott, B.P.; Anderson, S.A.; Armstrong, L.E.; Casa, D.J.; Cheuvront, S.N.; Cooper, L.; Kenney, W.L.; O’Connor, F.G.; Roberts, W.O. National Athletic Trainers’ Association position statement: Fluid replacement for the physically active. J. Athl. Train. 2017, 52, 877–895. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cotter, J.D.; Thornton, S.N.; Lee, J.K.; Laursen, P.B. Are we being drowned in hydration advice? Thirsty for more? Extrem. Physiol. Med. 2014, 3, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hew-Butler, T.; Rosner, M.H.; Fowkes-Godek, S.; Dugas, J.P.; Hoffman, M.D.; Lewis, D.P.; Maughan, R.J.; Miller, K.C.; Montain, S.J.; Rehrer, N.J.; et al. Statement of the 3rd international exercise-associated hyponatremia consensus development conference, carlsbad, california, 2015. Br. J. Sports Med. 2015, 49, 1432–1446. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCubbin, A.J.; Allanson, B.A.; Caldwell Odgers, J.N.; Cort, M.M.; Costa, R.J.S.; Cox, G.R.; Crawshay, S.T.; Desbrow, B.; Freney, E.G.; Gaskell, S.K.; et al. Sports Dietitians Australia position statement: Nutrition for exercise in hot environments. Int. J. Sport Nutr. Exerc. Metab. 2020, 30, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Noakes, T.D.; Speedy, D.B. Time for the american college of sports medicine to acknowledge that humans, like all other eartly creatures, do not need to be told how much to drink during exercise. Br. J. Sports Med. 2007, 41, 109–111. [Google Scholar]
- Passe, D.; Horn, M.; Stofan, J.; Horswill, C.; Murray, R. Voluntary dehydration in runners despite favorable conditions for fluid intake. Int. J. Sport Nutr. Exerc. Metab. 2007, 17, 284–295. [Google Scholar] [CrossRef]
- O’Neal, E.K.; Davis, B.A.; Thigpen, L.K.; Caufield, C.R.; Horton, A.D.; McIntosh, J.R. Runners greatly underestimate sweat losses before and after a 1-hr summer run. Int. J. Sport Nutr. Exerc. Metab. 2012, 22, 353–362. [Google Scholar] [CrossRef] [PubMed]
- Shaver, L.N.; O’Neal, E.K.; Hall, E.E.; Nepocatych, S. No performance or affective advantage of drinking versus rinsing with water during a 15-km running session in female runners. Int. J. Exerc. Sci. 2018, 11, 910–920. [Google Scholar] [PubMed]
- Thigpen, L.K.; Green, J.M.; O’Neal, E.K. Hydration profile and sweat loss perception of male and female Division II basketball players during practice. J. Strength Cond. Res. 2014, 28, 3425–3431. [Google Scholar] [CrossRef] [PubMed]
- O’Neal, E.K.; Caufield, C.R.; Lowe, J.B.; Stevenson, M.C.; Davis, B.A.; Thigpen, L.K. 24-h fluid kinetics and perception of sweat losses following a 1-h run in a temperate environment. Nutrients 2014, 6, 37–49. [Google Scholar] [CrossRef] [Green Version]
- Cronin, C.C.; O’Neal, E.; Simpson, J.; Miller, B.L.; Green, M.; Helm Allen, J.A.; Boman, S. Natural training hydration status, sweat rates, and perception of sweat losses during CrossFit training. Int. J. Exerc. Sci. 2016, 9, 4. [Google Scholar]
- Campbell, S.; Pritchett, R.C.; Cederburg, K.; Burnham, T.; Pritchett, K.C. Fluid intake and sweat rate during hot yoga participation. Int. J. Exerc. Sci. 2017, 10, 721–733. [Google Scholar]
- Muth, T.; Pitchett, R.; Pritchett, K.; DePaepe, J.; Blank, R. Hydration status and perception of fluid loss in male and female university rugby union players. Int. J. Exerc. Sci. 2019, 12, 859. [Google Scholar]
- Love, T.D.; Baker, D.F.; Healey, P.; Black, K.E. Measured and perceived indices of fluid balance in professional athletes. The use and impact of hydration assessment strategies. Eur. J. Sport Sci. 2018, 18, 349–356. [Google Scholar] [CrossRef]
- Davis, B.A.; O’Neal, E.; Johnson, S.; Farley, R.S. Hot training conditions inhibit adequate ad libitum recovery fluid intake of runners. Int. J. Exerc. Sci. 2019, 12, 1322–1333. [Google Scholar]
- Baker, L.B. Sweating rate and sweat sodium concentration in athletes: A review of methodology and intra/interindividual variability. Sports Med. 2017, 47, 111–128. [Google Scholar] [CrossRef] [Green Version]
- Cheuvront, S.N.; Montain, S.J. Myths and methodologies: Making sense of exercise mass and water balance. Exp. Physiol. 2017, 102, 1047–1053. [Google Scholar] [CrossRef] [Green Version]
- O’Neal, E.K.; Wingo, J.E.; Richardson, M.T.; Leeper, J.D.; Neggers, Y.H.; Bishop, P.A. Half-marathon and full-marathon runners’ hydration practices and perceptions. J. Athl. Train. 2011, 46, 581–591. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Winger, J.M.; Hoffman, M.D.; Hew-Butler, T.D.; Stuempfle, K.J.; Dugas, J.P.; Fogard, K.; Dugas, L.R. Physiology and hydration beliefs affect race behavior but not post-race sodium in 161-km ultramarathon finishers. Int. J. Sports Physiol. Perform 2013, 8, 536–541. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.; Chiampas, G.; Jaworski, C.; Passe, D. Lack of awareness of fluid needs among participants at a midwest marathon. Sports Health 2011, 3, 451–454. [Google Scholar] [CrossRef] [Green Version]
- O’Neal, E.K.; Poulos, S.P.; Bishop, P.A. Hydration profile and influence of beverage contents on fluid intake by women during outdoor recreational walking. Eur. J. Appl. Physiol. 2012, 112, 3971–3982. [Google Scholar] [CrossRef] [PubMed]
- Backer, H.D.; Shopes, E.; Collins, S.L.; Barkan, H. Exertional heat illness and hyponatremia in hikers. Am. J. Emerg. Med. 1999, 17, 532–539. [Google Scholar] [CrossRef]
- Baker, L.B.; Munce, T.A.; Kenney, W.L. Sex differences in voluntary fluid intake by older adults during exercise. Med. Sci. Sports Exerc. 2005, 37, 789–796. [Google Scholar] [CrossRef] [Green Version]
- Emerson, D.M.; Torres-McGehee, T.M.; Emerson, C.C.; LaSalle, T.L. Individual fluid plans versus ad libitum on hydration status in minor professional ice hockey players. J. Int. Soc. Sports Nutr. 2017, 14, 25. [Google Scholar] [CrossRef] [Green Version]
- Cleary, M.A.; Hetzler, R.K.; Wasson, D.; Wages, J.J.; Stickley, C.; Kimura, I.F. Hydration behaviors before and after an educational and prescribed hydration intervention in adolescent athletes. J. Athl. Train. 2012, 47, 273–281. [Google Scholar] [CrossRef] [Green Version]
- McDermott, B.P.; Casa, D.J.; Yeargin, S.W.; Ganio, M.S.; Lopez, R.M.; Mooradian, E.A. Hydration status, sweat rates, and rehydration education of youth football campers. J. Sport Rehabil. 2009, 18, 535–552. [Google Scholar] [CrossRef]
- McKenzie, A.L.; Munoz, C.X.; Armstrong, L.E. Accuracy of urine color to detect equal to or greater than 2% body mass loss in men. J. Athl. Train. 2015, 50, 1306–1309. [Google Scholar] [CrossRef] [Green Version]
- Peacock, O.J.; Stokes, K.; Thompson, D. Initial hydration status, fluid balance, and psychological affect during recreational exercise in adults. J. Sports Sci. 2011, 29, 897–904. [Google Scholar] [CrossRef] [PubMed]
- MacLeod, H.; Sunderland, C. Fluid balance and hydration habits of elite female field hockey players during consecutive international matches. J. Strength Cond. Res. 2009, 23, 1245–1251. [Google Scholar] [CrossRef] [PubMed]
- Brandenburg, J.P.; Gaetz, M. Fluid balance of elite female basketball players before and during game play. Int. J. Sport Nutr. Exerc. Metab. 2012, 22, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Goulet, E.D.; Hoffman, M.D. Impact of ad libitum versus programmed drinking on endurance performance: A systematic review with meta-analysis. Sports Med. 2019, 49, 221–232. [Google Scholar] [CrossRef] [PubMed]
- Beis, L.Y.; Wright-Whyte, M.; Fudge, B.; Noakes, T.; Pitsiladis, Y.P. Drinking behaviors of elite male runners during marathon competition. Clin. J. Sport Med. 2012, 22, 254–261. [Google Scholar] [CrossRef]
- Lee, J.K.; Nio, A.Q.; Lim, C.L.; Teo, E.Y.; Byrne, C. Thermoregulation, pacing and fluid balance during mass participation distance running in a warm and humid environment. Eur. J. Appl. Physiol. 2010, 109, 887–898. [Google Scholar] [CrossRef]
- Davis, B.A.; Thigpen, L.K.; Hornsby, J.H.; Green, J.M.; Coates, T.E.; O’Neal, E.K. Hydration kinetics and 10-km outdoor running performance following 75% versus 150% between bout fluid replacement. Eur. J. Sport Sci. 2014, 14, 703–710. [Google Scholar] [CrossRef]
- Wilcoxson, M.C.; Johnson, S.L.; Pribyslavska, V.; Green, J.M.; O’Neal, E.K. Fluid retention and utility of practical hydration markers to detect three levels of recovery fluid intake in male runners. Int. J. Sport Nutr. Exerc. Metab. 2017, 27, 178–185. [Google Scholar] [CrossRef]
- O’Neal, E.K.; Johnson, S.L.; Davis, B.A.; Pribyslavska, V.; Stevenson-Wilcoxson, M.C. Urine specific gravity as a practical marker for identifying sub-optimal fluid intake of runners ~12-h post-exercise. Int. J. Sport Nutr. Exerc. Metab. 2019, 29, 32–38. [Google Scholar] [CrossRef]
| Study | Participants | Exercise Condition | Sweat Loss |
|---|---|---|---|
| Sex = n | Modality: Duration (M ± SD; Range) | Actual (L) | |
| Age (Years) | Environmental Conditions (M ± SD; Range) | Predicted (L); Prediction Method | |
| Training Status | Sweat Loss as % of Body Mass | % of Actual | |
| Campbell et al. (2017) [15] | F = 18 M = 3 33 ± 11 Recreational | Hot Hatha yoga; 60 min Dry = 38.7 ± 2.7 °C Relative humidity = 35.8 ± 13.3% 1.11 ± 0.57% | 0.814 ± 0.539 0.512 ± 0.335; 1000 mL bottles 72.5 ± 49.0% |
| Cronin et al. (2016) [14] | F = 20 M = 30 30 ± 9 Recreational | CrossFit™; 34.3 ± 5.5 min WBGT = 20.1 ± 2.8; 16.0–22.7 °C 0.91 ± 0.31% | 0.746 ± 0.305 0.655 ± 0.404; 250 mL bottles 96.0 ± 60.8% |
| Davis et al. (2019) [18] A | M = 12 22 ± 2 Recreational | Treadmill running-temperate environment; 60 min WBGT = 18.1 ± 0.2 °C 1.72 ± 0.29% | 1.348 ± 0.282 0.793 ± 0.333; paper race cups 60.5 ± 26.6% |
| Davis et al. (2019) [18] B | M = 12 22 ± 2 Recreational | Treadmill running-hot environment; 60 min WBGT = 25.6 ± 0.5 °C 2.43 ± 0.56% | 1.907 ± 0.529 1.198 ± 0.550; paper race cups 66.7 ± 35.4% |
| O’Neal et al. (2012) [10] | F = 20 M = 19 41 ± 11 Recreational to collegiate | Outdoor running: 59.14 ± 3.46 min WBGT = 24.1 ± 1.5; 21.3–27.7 °C 2.11 ± 0.52% | 1.468 ± 0.484 0.738 ± 0.470; paper race cups 50.4 ± 23.0% |
| Shaver et al. (2018) [11] | F = 23 (2 trials) 26 ± 6 Recreational | Outdoor running 15-km time trial; 79.98 ± 7.00 min WBGT = 20.0 ± 2.8; 12.8–25.6 °C 2.20 ± 0.48% | 1.306 ± 0.307 0.498 ± 0.516; water bottle reference 39.9 ± 40.9% |
| O’Neal et al. (2014) [13] | F = 8 M = 12 20 ± 2 Recreational to collegiate | Outdoor running; 59.91 ± 3.42 min WBGT = 20.1 ± 2.8; 16.0–22.7 °C 1.96 ± 0.51% | 1.374 ± 0.423 0.697 ± 0.600; paper race cups 50.1 ± 39.1% |
| Thigpen et al. (2014) [12] A | F = 11 M = 11 20 ± 1 NCAA Division II | Collegiate basketball conditioning practice; (F = 95 min, M = 46 min) WBGT F = 20.4, M = 20.0 °C F = 1.47 ± 0.27, M = 1.13 ± 0.27% | F = 1.112 ± 0.271 M = 0.969 ± 0.250 F = 0.394 ± 0.242 M = 1.316 ± 0.847; standard practice water bottle F = 37.5 ± 28.3 M = 142.6 ± 102.4% |
| Thigpen et al. (2014) [12] B | F = 11 M = 11 20 ± 1 NCAA Division II | Collegiate basketball in-season practice; (F = 170 min, M = 170 min) WBGT F = 18.5; M = 17.2 °C F = 2.53 ± 0.43, M = 2.90 ± 0.50% | F = 1.910 ± 0.441 M = 2.471 ± 0.495 F = 0.632 ± 0.284 M = 1.740 ± 1.201; standard practice water bottle F = 35.1 ± 20.1 M = 70.6 ± 56.9% |
| Muth et al. (2019) [16] A | F = 16 20 ± 1 NCAA Rugby Union | Outdoor rugby practice; 95 min Dry = 11.0 ± 1.4 °C Relative humidity = 57.5 ± 3.5% 1.19 ± 0.55% | 0.928 ± 0.446 0.335 ± 0.243; 532 mL cup 53.0 ± 69.2% |
| Muth et al. (2019) [16] B | M = 20 20 ± 1 NCAA Rugby Union | Outdoor rugby practice; 90 min Dry = 8.5.0 ± 2.1 °C Relative humidity = 46.5 ± 9.2% 2.00 ± 0.54% | 1.917 ± 0.516 0.373 ± 0.183; 532 mL cup 20.9 ± 12.5% |
| Love et al. (2018) [17] | M = 20 25 ± 4 Professional | Outdoor rugby practice; 120 min Dry = 35.0 °C Relative humidity = 40% 3.2 ± 0.9% | 3.291 ± 0.948 0.898 ± 0.575; 532 questionnaire 27.4 ± 17.2% |
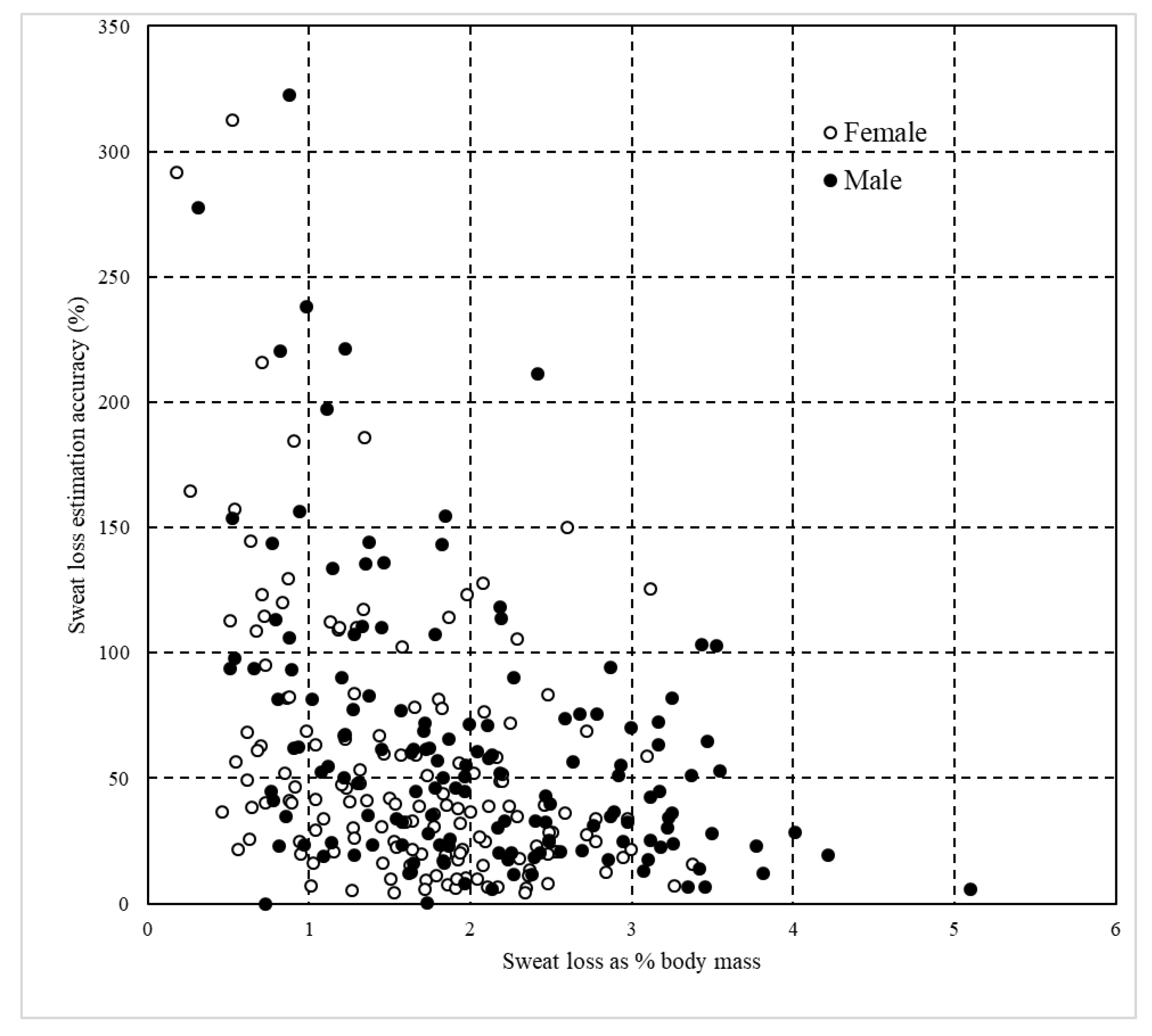
| Female (n = 147 *) | Male (n = 150 **) | All (n = 297) | |
|---|---|---|---|
| Age (years) | 27.3 ± 9.7 | 26.4 ± 9.6 | 26.8 ± 9.7 |
| Weight (kg) | 66.2 ± 11.1 | 87.1 ± 13.5† | 76.7 ± 16.2 |
| Exercise duration (min) | 77 ± 33 | 74 ± 38 | 75 ± 36 |
| Sweat loss | |||
| % body mass | 1.64 ± 0.71 | 2.04 ± 0.92 † | 1.84 ± 0.84 |
| Absolute (L) | 1.072 ± 0.473 ‡ | 1.778 ± 0.907 †‡ | 1.428 ± 0.806 ‡ |
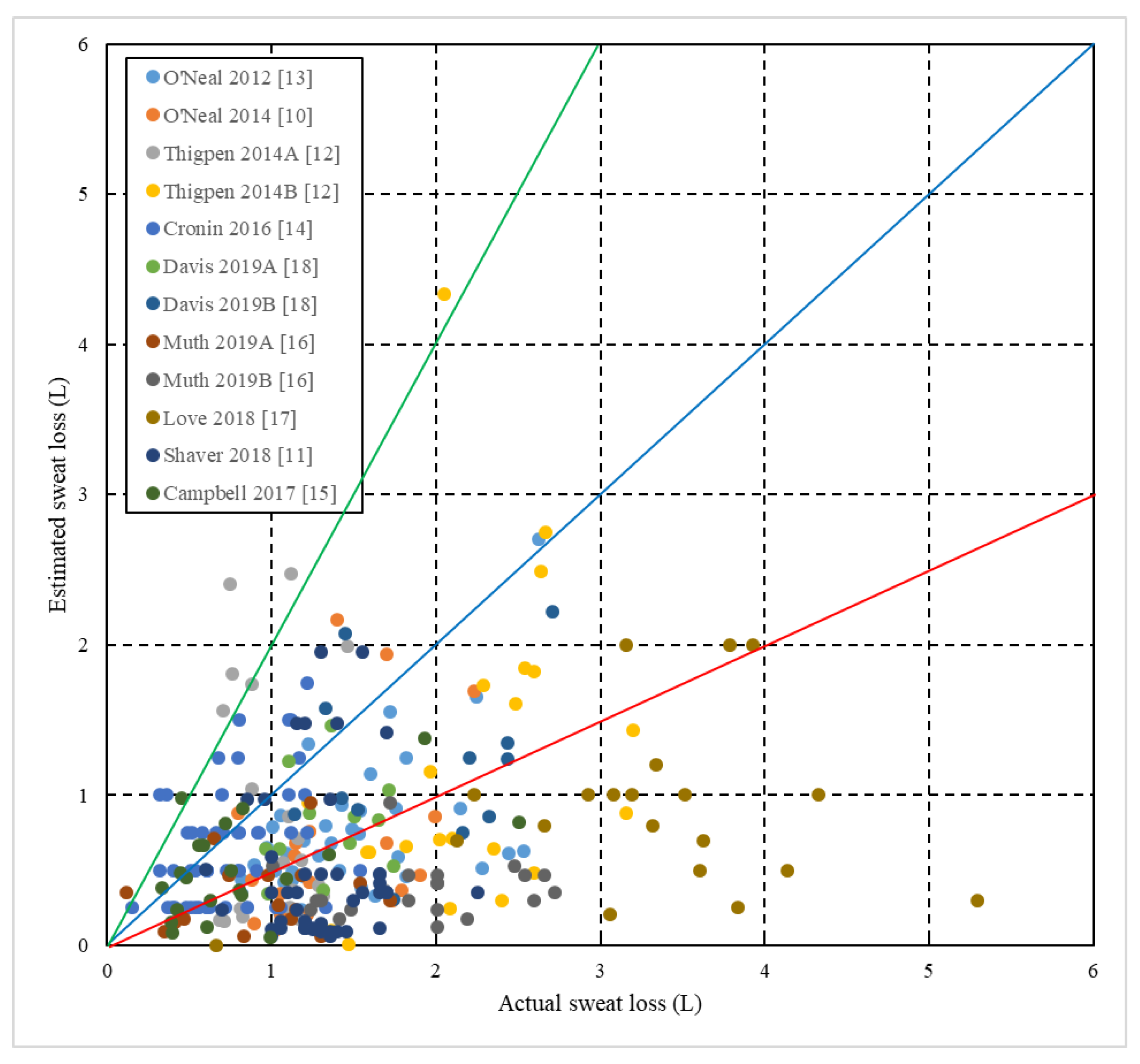
| Estimated (L) | 0.481 ± 0.372 | 0.908 ± 0.666 † | 0.697 ± 0.581 |
| Accuracy (%) | 55.2 ± 51.5 | 62.4 ± 54.5 | 58.9 ± 53.1 |
| Absolute Volume Comparisons | ||||
| Estimated Sweat Loss (L) | Actual Sweat Loss (L) | |||
| 0–1 | 1–2 | 2–3 | 3+ | |
| 0–1 | 82 (27) | 122 (41) | 29 (9) | 12 (4) |
| 1–2 | 7 (2) | 22 (7) | 9 (3) | 5 (1) |
| 2–3 | 1 (0.3) | 3 (1) | 4 (1) | 0 (0) |
| 3+ | 0 (0) | 0 (0) | 1 (0.3) | 0 (0) |
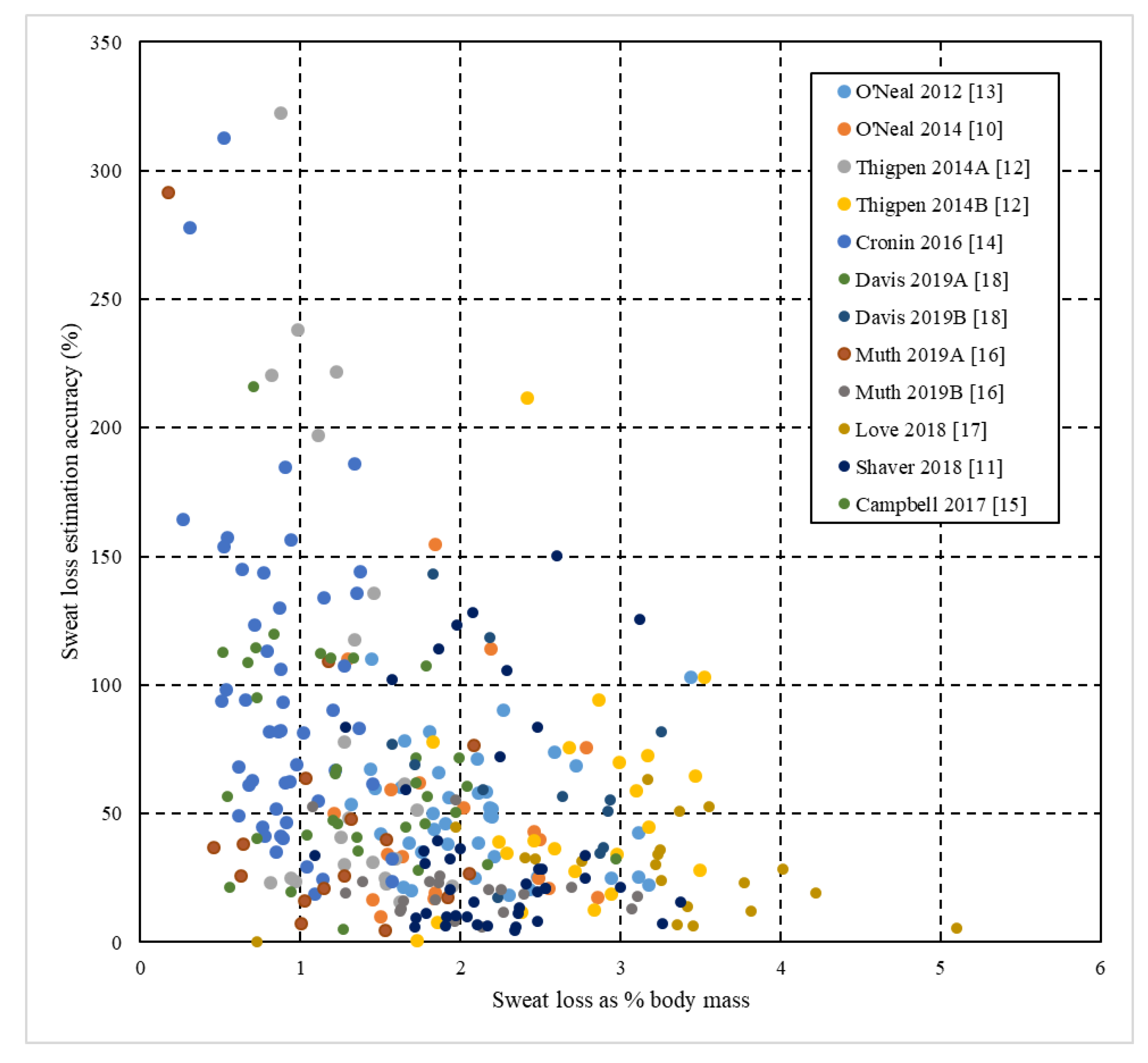
| Relative comparisons | ||||
| Estimation accuracy (%) | Sweat loss as a % of body mass | |||
| 0–1 | 1–2 | 2–3 | 3+ | |
| 0–50 | 17 (5) | 74 (24) | 55 (18) | 22 (7) |
| 50–100 | 16 (5) | 33 (11) | 21 (7) | 7 (2) |
| 100–150 | 10 (3) | 17 (5) | 4 (1) | 3 (1) |
| 150+ | 12 (4) | 4 (1) | 2 (0.6) | 0 (0) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
O’Neal, E.; Boy, T.; Davis, B.; Pritchett, K.; Pritchett, R.; Nepocatych, S.; Black, K. Post-Exercise Sweat Loss Estimation Accuracy of Athletes and Physically Active Adults: A Review. Sports 2020, 8, 113. https://doi.org/10.3390/sports8080113
O’Neal E, Boy T, Davis B, Pritchett K, Pritchett R, Nepocatych S, Black K. Post-Exercise Sweat Loss Estimation Accuracy of Athletes and Physically Active Adults: A Review. Sports. 2020; 8(8):113. https://doi.org/10.3390/sports8080113
Chicago/Turabian StyleO’Neal, Eric, Tara Boy, Brett Davis, Kelly Pritchett, Robert Pritchett, Svetlana Nepocatych, and Katherine Black. 2020. "Post-Exercise Sweat Loss Estimation Accuracy of Athletes and Physically Active Adults: A Review" Sports 8, no. 8: 113. https://doi.org/10.3390/sports8080113
APA StyleO’Neal, E., Boy, T., Davis, B., Pritchett, K., Pritchett, R., Nepocatych, S., & Black, K. (2020). Post-Exercise Sweat Loss Estimation Accuracy of Athletes and Physically Active Adults: A Review. Sports, 8(8), 113. https://doi.org/10.3390/sports8080113




