GOING GREEN: The Effectiveness of a 40-Day Green Exercise Intervention for Insufficiently Active Adults
Abstract
:1. Introduction
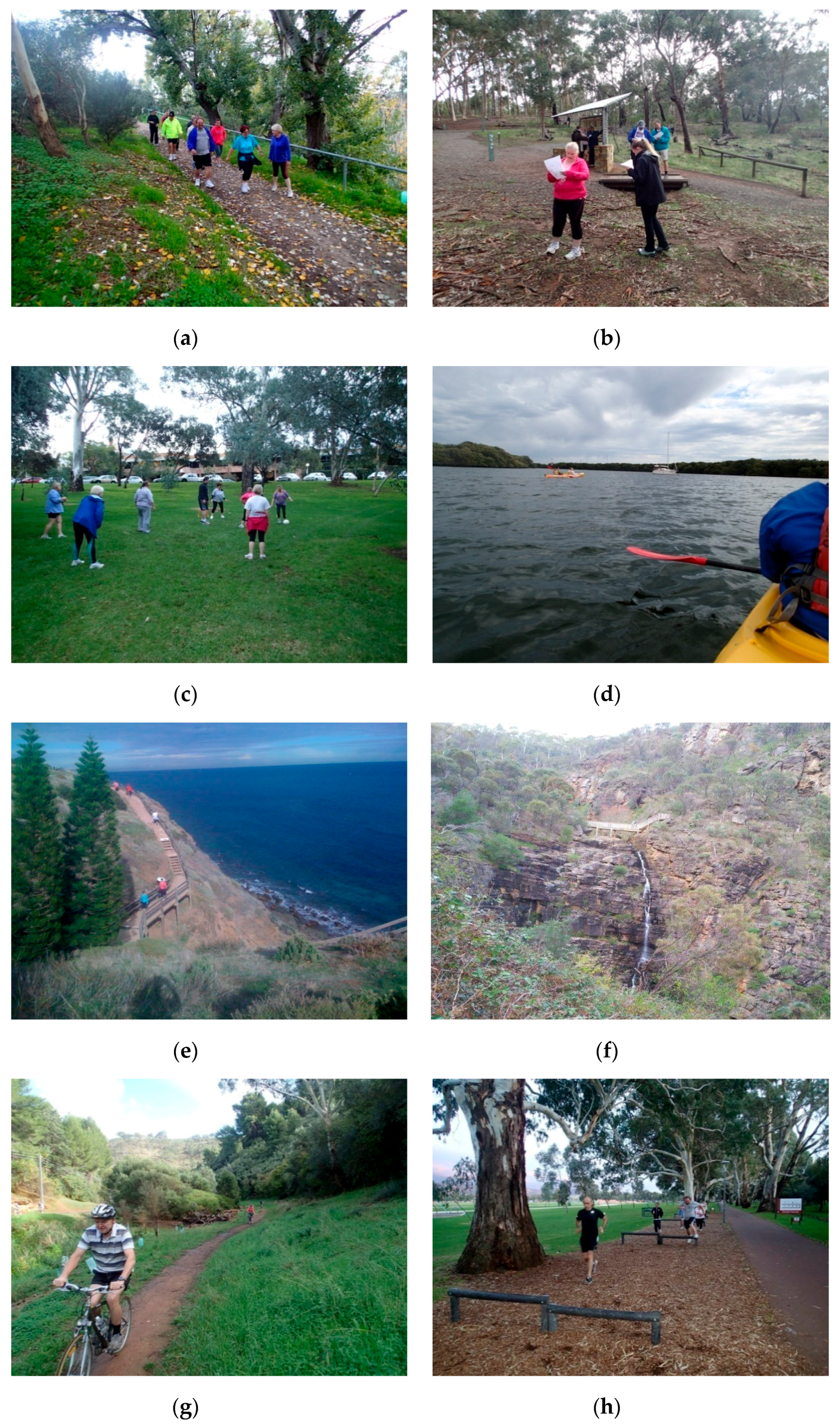
2. Materials and Methods
3. Results
3.1. Participants
3.2. Adherence and Compliance
3.3. Physical Activity
3.4. Changes to Physical and Physiological Health Following the Intervention
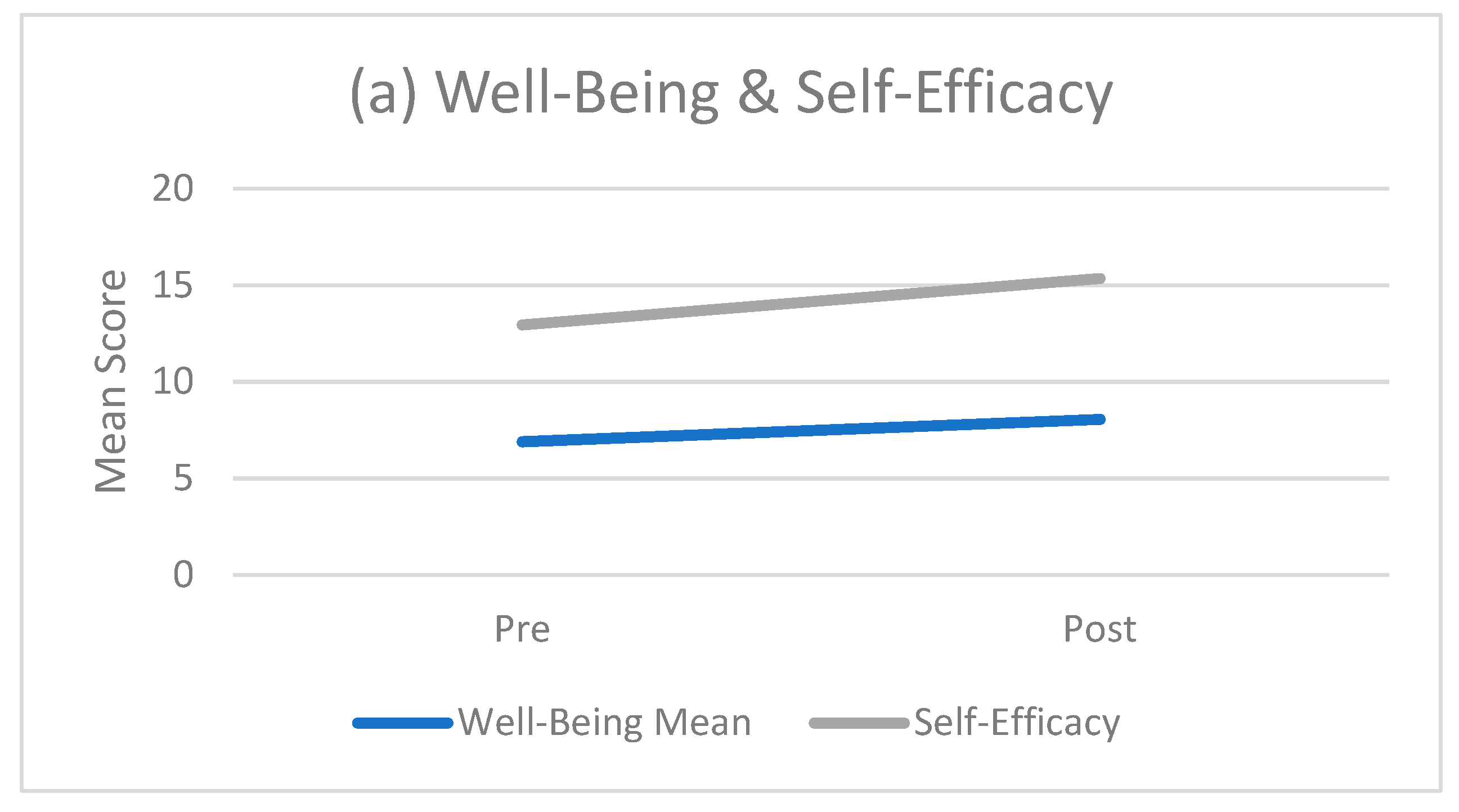
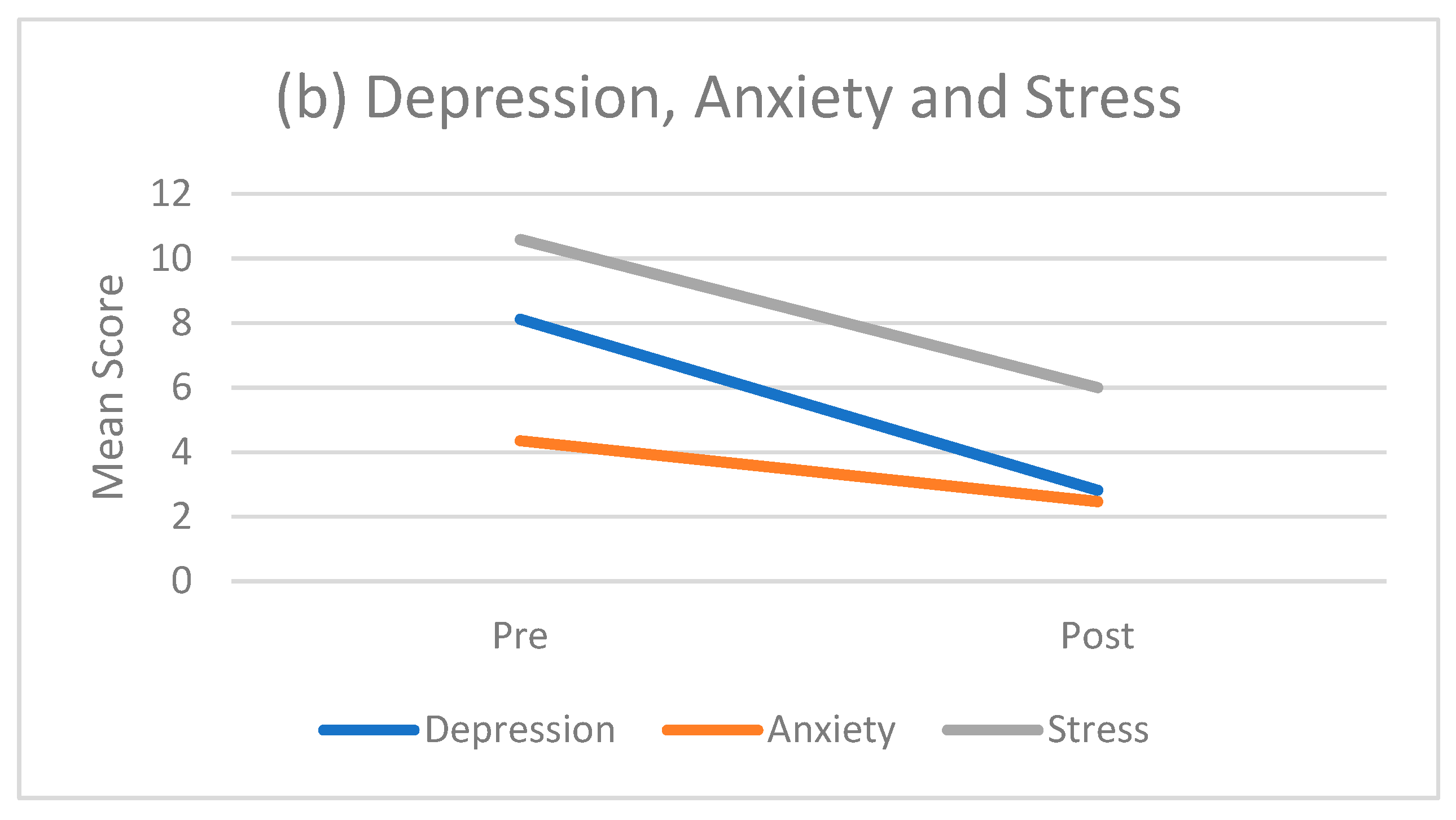
3.5. Changes to Mental Health and Well-Being Following the Intervention
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Physiological Variable | Mean | SD | %TEM |
|---|---|---|---|
| SBP (mmHg) | 119 | 3 | 3.1 |
| DBP (mmHg) | 75 | 2 | 4.1 |
| Height (cm) | 180.9 | 0 | 0.0 |
| Weight (kg) | 86.1 | 0 | 0.0 |
| Hip girth (cm) | 105.5 | 0.5 | 0.4 |
| Waist girth (cm) | 88.3 | 0.5 | 0.6 |
| Mean grip strength left (kg) | 47.5 | 1 | 3.6 |
| Mean grip strength right (kg) | 50.5 | 1.5 | 3.5 |
| Total cholesterol (mmol/L) | 4.38 | 0.08 | 2.3 |
| VO2max (mL·kg−1·min−1) | 40.9 | 3.8 | 10.8 |
References
- O’Keefe, J.H.; Vogel, R.; Lavie, C.J.; Cordain, L. Exercise like a hunter-gatherer: A prescription for organic physical fitness. Prog. Cardiovasc. Dis. 2011, 53, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; Esliger, D.W.; Copeland, J.L.; Barnes, J.D.; Bassett, D.R. Moving forward by looking back: Lessons learned from long-lost lifestyles. Appl. Physiol. Nutr. Metab. 2008, 33, 836–842. [Google Scholar] [CrossRef]
- World Health Organisation. Non-Communicable Diseases: Progress Monitor 2015; World Health Organisation: Geneva, Switzerland, 2015. [Google Scholar]
- Hammer, M.; Stamatakis, E.; Steptoe, A. Dose-response relationship between physical activity and mental health: The Scottish health survey. Br. J. Sports Med. 2009, 43, 1111–1114. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Fact Sheet N°369: Depression. Available online: http://www.who.int/mediacentre/factsheets/fs369/en/ (accessed on 4 March 2014).
- Australian Bureau of Statistics. Australian Health Survey: Physical Activity, 2011–2012. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4364.0.55.004Chapter1002011-12 (accessed on 1 February 2014).
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Kahn, E.B.; Ramsey, L.T.; Brownson, R.C.; Heath, G.W.; Howze, E.H.; Powell, K.E.; Stone, E.J.; Rajab, M.W.; Corso, P. The effectiveness of interventions to increase physical activity. A systematic review. Am. J. Prev. Med. 2002, 22 (Suppl. 4), 73–107. [Google Scholar] [CrossRef]
- Müller-Riemenschneider, F.; Reinhold, T.; Nocon, M.; Willich, S.N. Long-term effectiveness of interventions promoting physical activity: A systematic review. Prev. Med. 2008, 47, 354–368. [Google Scholar] [CrossRef] [PubMed]
- Thompson Coon, J.; Boddy, K.; Stein, K.; Whear, R.; Barton, J.; Depledge, M.H. Does participating in physical activity in outdoor natural environments have a greater effect on physical and mental wellbeing than physical activity indoors? A systematic review. Environ. Sci. Technol. 2011, 45, 1761–1772. [Google Scholar] [CrossRef] [PubMed]
- Conn, V.S.; Hafdahl, A.R.; Mehr, D.R. Interventions to increase physical activity among healthy adults: Meta-analysis of outcomes. Am. J. Public Health 2011, 101, 751–758. [Google Scholar] [CrossRef]
- Van der Bij, A.K.; Laurant, M.G.H.; Wensing, M. Effectiveness of physical activity interventions for older adults: A review. Am. J. Prev. Med. 2002, 22, 120–133. [Google Scholar] [CrossRef]
- Marin, T.S.; Kourbelis, C.; Foote, J.; Newman, P.; Brown, A.; Daniel, M.; Coffee, N.; Nicholls, S.; Ganesan, A.; Versace, V.; et al. Examining adherence to activity monitoring devices to improve physical activity in adults with cardiovascular disease: A systematic review. Eur. J. Prev. Cardiol. 2019, 26, 382–397. [Google Scholar] [CrossRef]
- Stockwell, S.; Schofield, P.; Fisher, A.; Firth, J.; Jackson, S.E.; Stubbs, B.; Smith, L. Digital behavior change interventions to promote physical activity and/or reduce sedentary behavior in older adults: A systematic review and meta-analysis. Exp. Gerontol. 2019, 120, 68–87. [Google Scholar] [CrossRef]
- Barton, J.; Pretty, J. What is the best dose of nature and green exercise for improving mental health? A multi-study analysis. Environ. Sci. Technol. 2010, 44, 3947–3955. [Google Scholar] [CrossRef] [PubMed]
- Bauman, A.; Smith, B.; Stoker, L.; Bellew, B.; Booth, M. Geographical influences upon physical activity participation: Evidence of a “coastal effect”. Aust. N. Z. J. Public Health 1999, 23, 322–324. [Google Scholar] [CrossRef] [PubMed]
- Akers, A.; Barton, J.; Cossey, R.; Gainsford, P.; Griffin, M.; Micklewright, D. Visual color perception in green exercise: Positive effects on mood and perceived exertion. Environ. Sci. Technol. 2012, 46, 8661–8666. [Google Scholar] [CrossRef] [PubMed]
- Bowler, D.E.; Buyung-Ali, L.M.; Knight, T.M.; Pullin, A.S. A systematic review of evidence for the added benefits to health of exposure to natural environments. BMC Public Health 2010, 10, 456. [Google Scholar] [CrossRef] [PubMed]
- Duncan, M.J.; Clarke, N.D.; Birch, S.L.; Tallis, J.; Hankey, J.; Bryant, E.; Eyre, E.L. The effect of green exercise on blood pressure, heart rate and mood state in primary school children. Int. J. Environ. Res. Public Health 2014, 11, 3678–3688. [Google Scholar] [CrossRef]
- Gladwell, V.F.; Brown, D.K.; Wood, C.; Sandercock, G.R.; Barton, J.L. The great outdoors: How a green exercise environment can benefit all. Extrem. Physiol. Med. 2013, 2, 3. [Google Scholar] [CrossRef] [PubMed]
- Hartig, T.; Marcus, C.C. Healing gardens—Places for nature in health care. Lancet 2006, 368, S36–S37. [Google Scholar] [CrossRef]
- Hartig, T.; Evans, G.W.; Jamner, L.D.; Davis, D.S.; Gärling, T. Tracking restoration in natural and urban field settings. J. Environ. Psychol. 2003, 23, 109–123. [Google Scholar] [CrossRef]
- Li, Q.; Morimoto, K.; Kobayashi, M.; Inagaki, H.; Katsumata, M.; Hirata, Y.; Hirata, K.; Suzuki, H.; Li, Y.J.; Wakayama, Y.; et al. Visiting a forest, but not a city, increases human natural killer activity and expression of anti-cancer proteins. Int. J. Immunopathol. Pharmacol. 2008, 21, 117–127. [Google Scholar] [CrossRef] [PubMed]
- Park, B.-J.; Tsunetsugu, Y.; Kasetani, T.; Hirano, H.; Kagawa, T.; Sato, M.; Miyazaki, Y. Physiological effects of Shinrin-yoku (taking in the atmosphere of the forest)-using salivary cortisol and cerebral activity as indicators. J. Physiol. Anthropol. 2007, 26, 123–128. [Google Scholar] [CrossRef]
- Pretty, J. How nature contributes to mental and physical health. Spiritual. Health Int. 2004, 5, 68–78. [Google Scholar] [CrossRef]
- Pretty, J.; Murray, G.; Sellens, M.; Pretty, C. Green Exercise: Complementary Roles of Nature, Exercise and Diet in Physical and Emotional Well-Being and Implications for Public Health Policy; University of Essex: Colchester, UK, 2003. [Google Scholar]
- Sugiyama, T.; Leslie, E.; Giles-Corti, B.; Owen, N. Associations of neighbourhood greenness with physical and mental health: Do walking, social coherence and local social interaction explain the relationships? J. Epidemiol. Community Health 2008, 62, e9. [Google Scholar] [CrossRef] [PubMed]
- Bodin, M.; Hartig, T. Does the outdoor environment matter for psychological restoration gained through running? Psychol. Sport Exerc. 2003, 4, 141–153. [Google Scholar] [CrossRef]
- Butryn, T.M.; Furst, D.M. The effects of park and urban settings on the moods and cognitive strategies of female runners. J. Sport Behav. 2003, 26, 335–355. [Google Scholar]
- Focht, B.C. Brief walks in outdoor and laboratory environments: Effects on affective responses, enjoyment, and intentions to walk for exercise. Res. Q. Exerc. Sport 2009, 80, 611–620. [Google Scholar] [CrossRef] [PubMed]
- Kerr, J.H.; Fujiyama, H.; Sugano, A.; Okamura, T.; Chang, M.; Onouha, F. Psychological responses to exercising in laboratory and natural environments. Psychol. Sport Exerc. 2006, 7, 345–359. [Google Scholar] [CrossRef]
- Mackay, G.J.; Neill, J.T. The effect of “green exercise” on state anxiety and the role of exercise duration, intensity, and greenness: A quasi-experimental study. Psychol. Sport Exerc. 2010, 11, 238–245. [Google Scholar] [CrossRef]
- Peacock, J.; Hine, R.; Pretty, J. The Mental Health Benefits of Green Exercise Activities and Green Care; University of Essex: Colchester, UK, 2007. [Google Scholar]
- Plante, T.G.; Gores, C.; Brecht, C.; Carrow, J.; Imbs, A.; Willemsen, E. Does exercise environment enhance the psychological benefits of exercise for women? Int. J. Stress Manag. 2007, 14, 88–98. [Google Scholar] [CrossRef]
- Yamaguchi, M.; Deguchi, M.; Miyazaki, Y. The effects of exercise in forest and urban environments on sympathetic nervous activity of normal young adults. J. Int. Med. Res. 2006, 34, 152–159. [Google Scholar] [CrossRef]
- Chao, D.; Foy, C.G.; Farmer, D. Exercise adherence among older adults: Challenges and strategies. Control. Clin. Trials 2000, 21, S212–S217. [Google Scholar] [CrossRef]
- Dishman, R.K. The problem of exercise adherence: Fighting sloth in nations with market economies. Quest 2001, 53, 279–294. [Google Scholar] [CrossRef]
- Hamlin, M.; Yule, E.; Elliot, C.; Stoner, L.; Kathiravel, Y. Long-term effectiveness of the New Zealand green prescription primary health care exercise initiative. Public Health 2016, 140, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Husebø, A.M.L.; Dyrstad, S.M.; Søreide, J.A.; Bru, E. Predicting exercise adherence in cancer patients and survivors: A systematic review and meta-analysis of motivational and behavioural factors. J. Clin. Nurs. 2013, 22, 4–21. [Google Scholar] [CrossRef] [PubMed]
- Harte, J.L.; Eifert, G.H. The effects of running, environment, and attentional focus on athletes’ catecholamine and cortisol levels and mood. Psychophysiology 1995, 32, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Teas, J.; Hurley, T.; Ghumare, S.; Ogoussan, K. Walking outside improves mood for healthy postmenopausal women. Clin. Med. Oncol. 2007, 1, 35–43. [Google Scholar] [CrossRef]
- Rogerson, M.; Gladwell, V.F.; Gallagher, D.J.; Barton, J.L. Influences of green outdoors versus indoors environmental settings on psychological and social outcomes of controlled exercise. Int. J. Environ. Res. Public Health 2016, 13, 363. [Google Scholar] [CrossRef] [PubMed]
- Hillsdon, M.; Thorogood, M. A systematic review of physical activity promotion strategies. Br. J. Sports Med. 1996, 30, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Kellert, S.R.; Wilson, E.O. (Eds.) The Biophilia Hypothesis; Island Press: Washington, DC, USA, 1993; 484p. [Google Scholar]
- Norton, L.H.; Norton, K.I.; Lewis, N.; Dollman, J. A comparison of two short-term intensive physical activity interventions: Methodological considerations. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 133. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. The Active Australia Survey: A Guide and Manual for Implementation, Analysis and Reporting; Australian Institute of Health and Welfare: Canberra, Australia, 2003. [Google Scholar]
- Pickering, T.G.; Hall, J.E.; Appel, L.J.; Falkner, B.E.; Graves, J.; Hill, M.N.; Jones, D.W.; Kurtz, T.; Sheps, S.G.; Roccella, E.J. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: Blood pressure measurement in humans: A statement for professionals from the subcommittee of professional and public education of the american heart association council on high blood pressure research. Hypertension 2005, 45, 142–161. [Google Scholar]
- Norton, K.; Olds, T. Anthropometrica: A Textbook of Body Measurement for Sports and Health Courses; UNSW Press: Sydney, Australia, 1996. [Google Scholar]
- Eston, R.; Williams, J. Reliability of ratings of perceived effort regulation of exercise intensity. Br. J. Sports Med. 1988, 22, 153–155. [Google Scholar] [CrossRef]
- Polar Electro. S610 ™ Heart Rate Monitor User’s Manual; Polar Electro, Inc.: Kempele, Finland, 2004. [Google Scholar]
- Crouter, S.E.; Albright, C.; Bassett, J.; David, R. Accuracy of polar S410 heart rate monitor to estimate energy cost of exercise. Med. Sci. Sports Exerc. 2004, 36, 1433–1439. [Google Scholar] [CrossRef] [PubMed]
- Dishman, R.K. Increasing and maintaining exercise and physical activity. Behav. Ther. 1991, 22, 345–378. [Google Scholar] [CrossRef]
- International Wellbeing Group. Personal Wellbeing Index. Available online: http://www.deakin.edu.au/research/acqol/instruments/wellbeing-index/pwi-a-english.pdf (accessed on 19 April 2013).
- Schwarzer, R.; Renner, B. Health-Specific Self-Efficacy Scales. Available online: http://userpage.fu-berlin.de/health/healself.pdf (accessed on 19 April 2013).
- Lovibond, S.H.; Lovibond, P.F. Manual for the Depression Anxiety Stress Scales, 2nd ed.; Psychology Foundation of Australia: Sydney, Australia, 1996. [Google Scholar]
- The Department of Health. Australia’s Physical Activity and Sedentary Behaviour Guidelines. Available online: http://www.health.gov.au/internet/main/publishing.nsf/Content/health-pubhlth-strateg-phys-act-guidelines#apaadult (accessed on 30 March 2019).
- Australian Bureau of Statistics. National Health Survey: First Results, 2017–2018; Australian Bureau of Statistics: Canberra, Australia, 2019.
- Population Research and Outcome Studies Unit. Physical Activity among South Australian Adults; SA Health: Adelaide, Australia, 2010. [Google Scholar]
- Australian Institute of Health and Welfare. Overweight and Obesity. 2013. Available online: http://www.aihw.gov.au/diabetes-indicators/overweight-and-obesity/ (accessed on 20 May 2014).
- Ng, F.; Trauer, T.; Dodd, S.; Callaly, T.; Campbell, S.; Berk, M. The validity of the 21-item version of the depression anxiety stress scales as a routine clinical outcome measure. Acta Neuropsychiatr. 2007, 19, 304–310. [Google Scholar] [CrossRef] [PubMed]
- Frühauf, A.; Niedermeier, M.; Elliott, L.R.; Ledochowski, L.; Marksteiner, J.; Kopp, M. Acute effects of outdoor physical activity on affect and psychological well-being in depressed patients—A preliminary study. Ment. Health Phys. Act. 2016, 10, 4–9. [Google Scholar] [CrossRef]
- Mantler, A.; Logan, A.C. Natural environments and mental health. Adv. Integr. Med. 2015, 2, 5–12. [Google Scholar] [CrossRef]
- Mitchell, R. Is physical activity in natural environments better for mental health than physical activity in other environments? Soc. Sci. Med. 2013, 91, 130–134. [Google Scholar] [CrossRef] [PubMed]
- Pasanen, T.P.; Tyrväinen, L.; Korpela, K.M. The relationship between perceived health and physical activity indoors, outdoors in built environments, and outdoors in nature. Appl. Psychol. Health Well-Being 2014, 6, 324–346. [Google Scholar] [CrossRef]
- Weng, P.-Y.; Chiang, Y.-C. Psychological restoration through indoor and outdoor leisure activities. J. Leis. Res. 2014, 46, 203–215. [Google Scholar] [CrossRef]

| Week | Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday |
|---|---|---|---|---|---|---|---|
| Week 1 800 kJ * | WALK Easy grade walk at River Torrens Linear Park; Includes ice-breakers | Individual | GAITs Group initiative challenges in Victoria Park | Individual | Individual | KAYAK Introductory Kayaking session at Garden Island | |
| Week 2 1000 kJ * | Individual | CYCLING Introductory cycling session at linear park | Individual | STRENGTH & STRETCH Low impact strength exercises, stretching & yoga at Victoria Park | Individual | Individual | CYCLING Introductory trail riding at Brownhill Creek |
| Week 3 1200 kJ * | Individual | WALK Moderate grade walk at River Torrens Linear Park | Individual | TEAM GAMES soccer at Victoria Park | Individual | Individual | WALK Moderate walk at Marino Rocks |
| Week 4 1400 kJ * | Individual | WALK Moderate/challenging walk at River Torrens Linear Park | Individual | CIRCUIT Sweat track circuit in Victoria Park | Individual | Individual | EXPLORING MORIALTA Hike to the waterfalls; rock climbing and abseiling at Morialta CP |
| Week 5 1600 kJ * | Individual | ORIENTEERING Orienteering session in North Adelaide | Individual | STRENGTH & STRETCH Strength, stretching & yoga at Victoria Park | Individual | Individual | ORIENTEERING Orienteering session at Belair National Park |
| Week 6 1800 kJ * | Individual | WALK Challenging walk on Torrens Linear Park | Individual | GAITs Group initiative challenges in Victoria Park | Individual | Individual |
| Variable | Mean | SD | Range |
|---|---|---|---|
| Males (n = 8) | |||
| Age (years) | 48.8 | 9.9 | 28.7–59.3 |
| Height (cm) | 178.2 | 5.0 | 167.5–183.4 |
| Weight (kg) | 93.3 | 16.9 | 71.0–120.5 |
| Unweighted PA (min/week) | 69 | 34 | 30–125 |
| Females (n = 9) | |||
| Age (years) | 47.8 | 11.0 | 28.4–59.1 |
| Height (cm) | 161.3 | 4.4 | 153.2–168.4 |
| Weight (kg) | 80.5 | 17.7 | 60.7–117.6 |
| Unweighted PA (min/week) | 73 | 44 | 0–134 |
| All participants (n = 17) | |||
| Age (years) | 48.3 | 10.2 | 28.4–59.3 |
| Height (cm) | 169.2 | 9.8 | 153.2–183.4 |
| Weight (kg) | 86.5 | 18.0 | 60.7–120.5 |
| Unweighted PA (min/week) | 71 | 38 | 0–134 |
| Week | Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | Sunday |
|---|---|---|---|---|---|---|---|
| 1 | Pre-program | WALK | Individual Day | INITIATIVE TASKS | Individual Day | Individual Day | KAYAK |
| HR119 1088 kJ | HR115 938 kJ | HR126 1410 kJ | HR123 1184 kJ | HR125 1135 kJ | HR112 1256 kJ | ||
| 2 | Individual Day | CYCLING | Individual Day | STRENGTH & STRETCH | Individual Day | Individual Day | CYCLING |
| HR 120 1033 kJ | HR128 1649 kJ | HR138 1094 kJ | HR109 1949 kJ | HR121 915 kJ | HR118 875 kJ | HR128 2066 kJ | |
| 3 | Individual Day | WALK | Individual Day | TEAM GAMES | Individual Day | Individual Day | COASTAL WALK |
| HR 111 1049 kJ | HR119 1565 kJ | HR115 1213 kJ | HR119 1123 kJ | HR115 922 kJ | HR128 1513 kJ | HR132 2470 kJ | |
| 4 | Individual Day | WALK | Individual Day | CIRCUIT | Individual Day | Individual Day | EXPLORING MORIALTA |
| HR 121 1181 kJ | HR119 1296 kJ | HR131 874 kJ | HR134 1368 kJ | HR114 958 kJ | HR114 1100 kJ | HR109 1886 kJ | |
| 5 | Individual Day | ORIENTEERING | Individual Day | STRENGTH & STRETCH | Individual Day | Individual Day | ORIENTEERING |
| HR 121 1225 kJ | HR110 1299 kJ | HR114 792 kJ | HR103 1366 kJ | HR102 707 kJ | HR113 1129 kJ | HR124 1256 kJ | |
| 6 | Individual Day | WALK | Individual Day | INITIATIVE TASKS | Individual Day | Individual Day | Post-program |
| HR 122 1068 kJ | HR115 1334 kJ | HR122 991 kJ | HR122 1776 kJ | HR123 1501 kJ | HR124 1351 kJ |
| Variable | n | Pre Mean | Pre SD | Post Mean | Post SD | p (Paired t-Test) |
|---|---|---|---|---|---|---|
| Anthropometric | ||||||
| Hip girth (cm) | 17 | 110.2 | 14.3 | 109.2 | 14.3 | 0.036 |
| Cardio-Metabolic | ||||||
| Total cholesterol (mmol/L) | 17 | 5.0 | 1.2 | 4.7 | 1.1 | 0.026 |
| Fitness | ||||||
| Aerobic fitness (mL·kg−1·min−1) | 17 | 25.4 | 10.6 | 30.8 | 13.3 | 0.002 |
| Dynamic stability # | 17 | 2.7 | 1.5 | 3.1 | 1.6 | 0.038 |
| Physical Activity | ||||||
| Moderate PA (min/week) | 17 | 55 | 45 | 266 | 132 | <0.001 |
| Vigorous PA (min/week) | 17 | 13 | 20 | 179 | 150 | <0.001 |
| Weighted PA (min/week) | 17 | 84 | 43 | 624 | 367 | <0.001 |
| Psychological # | ||||||
| Well-being | 14 ǂ | 6.9 | 2.1 | 8.1 | 2.4 | <0.001 |
| Depression | 17 | 8.1 | 7.2 | 2.8 | 3.7 | <0.001 |
| Anxiety | 17 | 4.4 | 3.3 | 2.5 | 3.0 | 0.042 |
| Stress | 17 | 10.6 | 5.8 | 6.0 | 3.9 | 0.004 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Glover, N.; Polley, S. GOING GREEN: The Effectiveness of a 40-Day Green Exercise Intervention for Insufficiently Active Adults. Sports 2019, 7, 142. https://doi.org/10.3390/sports7060142
Glover N, Polley S. GOING GREEN: The Effectiveness of a 40-Day Green Exercise Intervention for Insufficiently Active Adults. Sports. 2019; 7(6):142. https://doi.org/10.3390/sports7060142
Chicago/Turabian StyleGlover, Nicholas, and Scott Polley. 2019. "GOING GREEN: The Effectiveness of a 40-Day Green Exercise Intervention for Insufficiently Active Adults" Sports 7, no. 6: 142. https://doi.org/10.3390/sports7060142
APA StyleGlover, N., & Polley, S. (2019). GOING GREEN: The Effectiveness of a 40-Day Green Exercise Intervention for Insufficiently Active Adults. Sports, 7(6), 142. https://doi.org/10.3390/sports7060142





