Abstract
The triathlon is one of the fastest developing sports in the world due to expanding participation and media attention. The fundamental change in Olympic triathlon races from a single to a multistart event is highly demanding in terms of recovery from and prevention of exercise-induced muscle injures. In elite and competitive sports, ultrastructural muscle injuries, including delayed onset muscle soreness (DOMS), are responsible for impaired muscle performance capacities. Prevention and treatment of these conditions have become key in regaining muscular performance levels and to guarantee performance and economy of motion in swimming, cycling and running. The aim of this review is to provide an overview of the current findings on the pathophysiology, as well as treatment and prevention of, these conditions in compliance with clinical implications for elite triathletes. In the context of DOMS, the majority of recovery interventions have focused on different protocols of compression, cold or heat therapy, active regeneration, nutritional interventions, or sleep. The authors agree that there is a compelling need for further studies, including high-quality randomized trials, to completely evaluate the effectiveness of existing therapeutic approaches, particularly in triathletes. The given recommendations must be updated and adjusted, as further evidence emerges.
1. Introduction
The triathlon is a multisport endurance sport in which athletes race sequentially in swimming, cycling, and running over various race distances. Due to an ever-expanding participation base and increased media interest, the triathlon is considered to be one of the fastest growing sports globally [1,2,3]. There are numerous event formats for both competitive and recreational events, ranging from super-sprint to long-distance triathlon, over which the International Triathlon Union (ITU) presides. In addition to the standard distance (Olympic distance) and sprint distance races, the ITU is the Governing Body overseeing the Mixed Team Relay (MTR) [4]; an innovative racing format where athletes complete a super-sprint triathlon, comprising of a 300 m swim, 6.6 km cycle and 1 km run before handing over to a teammate in the given order of female-male-female-male. The Mixed Relay is commonly held within 2–3 days of the individual race embedded within the same event. Having recently been included in the Olympic program, the Mixed Relay will make its debut at the Tokyo 2020 Olympic Games [4]. As well as being an exciting addition for spectators, it alters the demands placed upon the athletes, requiring them to work at higher intensity and greater speed throughout.
Historically, events such as the World Triathlon Series (WTS) or Olympic Games consisted of one intense and exhausting race for each athlete. Subsequently, athletes were able to recover in the days following competition until the resumption of full training or further competition; a second race start during the same competition was usually not performed. The fundamental change in triathlons from a single to multi-start event increases the demands placed upon the athlete in terms of recovery and prevention of exercise-induced muscle damages, which in turn has created a demand for research into optimizing recovery and regeneration. According to previous studies, particularly carbohydrate depletion, dehydration, hypoglycemia, electrolyte imbalance and ultrastructural muscle damage have been estimated to have a key function affecting muscle force output in triathletes [5,6]. As triathlon was established as a traditional endurance sport, common recovery practices focus mainly on the metabolic aspects (i.e., energy and carbohydrate storage, fluid intake, natrium balance [7,8]) and triathletes seem well informed about the necessity of rehydration after exercise [6]. Several studies demonstrated the presence of exercise-induced muscle injuries in triathletes [6,9,10], which is a relevant factor that impairs muscle function in triathlons, and which is known to mainly result from the running leg [6]. It was demonstrated in a recent study that post-exercise myoglobin and creatine kinase levels as indirect markers of muscle damage correlated with countermovement jumps height loss after the race [5,6]. The authors concluded that muscle fiber damage is one of the key factors for muscle fatigue in triathlons and strategies to lessen muscle fatigue during triathlon events should comprise a reduction in muscle damage [6]. However, those strategies have not been developed for triathletes up to now. Due to the adapted Olympic program, there is now a greater demand on athletes to regain high-intensity muscular activity and a high biomechanical output in order to deliver maximum performance for the MTR race [11] (Figure 1).

Figure 1.
Scuffles for positions during cycling. High muscular demands are required. Elite triathletes need to perform i.e., over 1000 watts 3s peak power.
Understanding the benefits of each intervention requires knowledge of the underlying muscle damaging and exhausting mechanisms, pathophysiological processes and treatment interventions [12]. The design of an “ideal” recovery regime is a topic receiving a lot of attention within current elite sports research [13,14,15,16]. Therefore, the aim of this narrative review is to provide an overview of the current literature on the pathophysiology as well as treatment and prevention of muscle soreness and suggesting the clinical implications for elite triathletes.
2. Materials and Methods
This narrative review focusses on the prevention and treatment of exercise-induced muscle injuries in relation to elite level triathletes. The existing literature on the pathogenesis, treatment, and prevention of exercise-induced muscle injuries, including original research reports, systematic and non-systematic reviews, book chapters and case reports was reviewed independently from their level of evidence. No systematic literature search was conducted. The aim of the present work was (1) to update the information about the current findings in pathogenesis of exercise-induced muscle injuries; (2) to apply current evidence for the treatment and prevention of exercise-induced muscle injuries in general; and (3) to discuss and evaluate the current findings by considering clinical and practical implications for triathlon races and competitions. For the purpose of this manuscript, the work done by an interdisciplinary authorship, consisting of biomechanists, sports scientists and sports physicians from the German Olympic Federation (DOSB) and the German Triathlon Union (DTU, Deutsche Triathlon Union), as well as scientists specializing in the field of exercise-induced muscle injuries is highlighted.
3. Results and Discussion
3.1. Mechanisms and Pathogenesis of Exercise-Induced Muscle Injures
3.1.1. Differentiation between Muscle Soreness, Exercise-Induced Muscle Damage (EIMD) and Delayed Onset Muscle Soreness (DOMS)
The clinical progression and manifestation of exercise-induced muscle damage, also known as DOMS, commonly begins 6–12 h post exercise, increasing progressively until peak pain occurs at 48–72hrs and thereafter decreasing until completely imperceptible 5–7 days post exercise [17,18]. DOMS is often accompanied by impaired muscle contraction and reduced force capacity [17,19,20], whilst a local or even global area of increased muscle tone is commonly observed [21,22,23,24]. DOMS is associated with local muscle soreness, reduced range of motion and altered biomechanical function of the adjacent joints [17,19,20,25,26]. Although the precise underlying causes of DOMS remain unknown [27], it is commonly accepted that the main mechanisms are related to ultrastructural damage of skeletal muscle integrity (exercise-induced muscle damage, EIMD) caused by intense and exhausting exercise and/or unfamiliar sporting activity [28,29,30] (Figure 2, Figure 3); for elite triathletes, the first scenario being the most relevant.
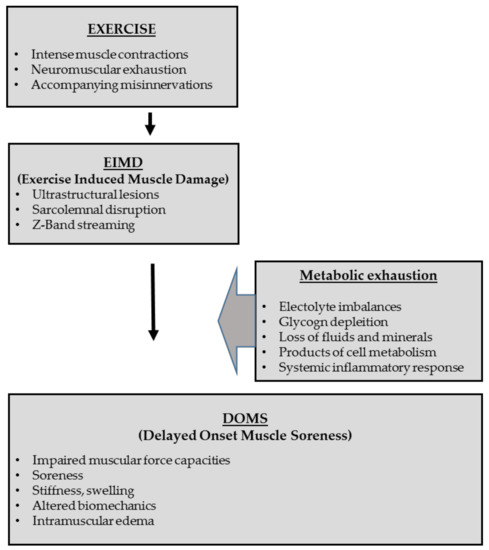
Figure 2.
Illustrating the pathophysiological pathway of exercises, Exercise-induced Muscle Damage (EIMD), Delayed Onset Muscle Soreness (DOMS) and accompanying metabolic exhaustion; adapted from Heiss et al. [12].
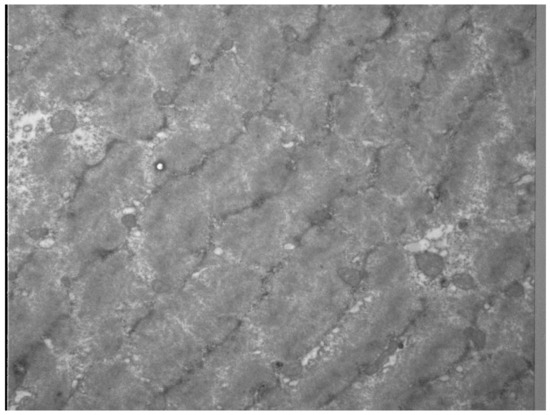
Figure 3.
Z-disk disintegration and myofilament disarrangement as sign of ultrastructural damage was evaluated by electron microscopy of biopsies of human vastus lateralis 24 h after strenuous resistance exercise for 70 s under tension leading to DOMS (With kind permission, Prof. W. Bloch, German Sport University Cologne, Germany).
In the past, eccentric contractions in particular were suspected to play a key role in the development of ultrastructural muscle injuries. In this condition, external loads are greater than the force generated by the muscles fibres under concentric conditions [12,28,31]. The higher muscular force is caused by an increase in recruitment of active cross-bridges [32] and in particular, by “passive-elastic” factors (i.e., Ca2+ triggered increased stiffness of titin and its winding on actin [12,33]), as described in the three-filament model and winding filament by Herzog et al. [34]. However, this hypothesis is not entirely relevant to triathletes, as eccentric contractions may occur solely during running, particularly on inclined surfaces. Several studies demonstrated the presence of exercise-induced muscle injuries in triathletes [6,9,10]. However, the exact cause of muscle damage in endurance sports, in particular in triathletes in triathletes has yet to be elucidated. In triathlons, there are no isolated eccentric contractions that induce a “pure eccentric overload” as applied in several DOMS models. Instead, the disciplines of swimming, cycling, and running are associated with changes of direction and positioning and eccentric contractions are shorter and part of the entire stretch-shortening cycle [35,36]. Swimming and cycling are considered to produce minor muscle damage in the involved muscles. Running however, as weight bearing activity includes concentric and eccentric actions in the lower extremity muscles [6]. During high-intensity races, central neuromuscular exhaustion and accompanying misinnervations can be discussed to reinforce the development of ultrastructural muscle injuries in these conditions. Hence, weariness induced alterations in intra- and intermuscular coordination between the muscle fibres with associated overstressing and damaging single muscle fibers should also be considered a factor [23]. Furthermore, it is unclear if metabolic exhaustion may also reinforce the development of DOMS.
3.1.2. Inflammatory and Healing Responses
Electrolyte imbalances, leukocyte accumulation and infiltration in the exercised muscle, as well as an upregulation of circulating pro-inflammatory cytokines have been found in the context of DOMS as well as after exhausting endurance trials [27,28,29,37]. The released cytokines lead to a higher vascular permeability and microcirculation disturbances as they act as inflammatory mediators [38]. The presence of interstitial fluid associated with intramuscular edema and compartment swelling (Figure 4) as well as the presence of diverse inflammatory substances are described to be responsible for nociceptor activation and pain sensation [39,40]. In response to the loss of sarcolemmal integrity and permeability of the plasma membrane, DOMS is associated with increased creatine kinase (CK) activity levels, which are one of the leading indirect markers of muscle damage [19,38,41,42]. Several further markers such as Interleukin 6 (IL-6), C-reactive protein (CRP) [43], PTX-3 or LDH are upregulated during inflammation within damaged tissues [44]. However, the assessment of these parameters has been studied primarily in a scientific setting, as it is not methodological feasible in the context of triathlon competitions; therefore, generalizability is limited.
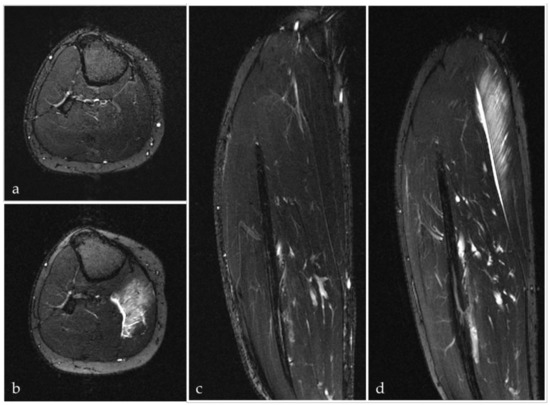
Figure 4.
Axial (a,b) and coronal (c,d) T2-weighted fat-suppressed MRI images of the lower leg before (a,c) and 60 h after eccentric exercise (b,d) in the same participant. The increased signal intensity (b,d) reflects a rising fluid content in the gastrocnemius medialis muscle as equivalent of DOMS.
4. Treatments and Strategies to Target Exercise-Induced Muscle Injuries
It is desirable to prevent athletes from experiencing DOMS, particularly in the context of multi-start events. Based on pathophysiological factors, recovery strategies should focus on various aspects, including (1), the primary prevention of ultrastructural lesions during exercise (prevention of EIMD), (2), the treatment of inflammatory responses leading to DOMS, and (3) – in case of failure of point (1) and (2) the treatment and recovery strategies of reduce signs of DOMS [12]. A range of interventions aiming to either prevent or relieve the symptoms of DOMS, thereby accelerating the recovery process from this performance-limiting condition, have been reported.
4.1. The Role of Sleep
A reduction in total regeneration time at major sporting events containing multiple starts increases the awareness of sleep as a crucial component of the recovery process. Disturbance of sleep can be caused by early morning training, increases in training load, travel departure times, jet lag and altitude [45,46]. Sleep deprivation is associated with lower physical and mental performance [47], whilst optimal levels of sleep (in both quantity and quality) have been linked to increased performance and reduced risk of injury [48]. The greater the demand for speed, tactical awareness and technical skill within a sport, the more sensitive it is to sleep duration manipulation. Further to this, longer-term sleep manipulation is more likely to affect athletic performance than acute sleep manipulation [49]. Some studies showed a positive effect of sleep extension on subsequent performance [50,51]. A promising option in the case of an insufficient night’s sleep could be the introduction of power naps, provided that the recommendation of a 30-min maximum duration is not exceeded [52,53]. For practical suggestions, refer to Table 1.

Table 1.
Recommendations for improving sleep in athletes (Data adapted from Simpson et al. [54]).
4.2. Compression Therapy
In recent years, there has been increasing interest in the efficacy of compression garments for post-exercise treatment in various disciplines. Existing systematic reviews have concluded that compression garments are effective in enhancing recovery from exercise-induced muscle damage [55,56], whilst the majority of previous studies failed to support a performance-enhancing effect of wearing compression garments during exercise. Results are not uniformly accepted. Inconsistent findings may be caused by heterogeneous conditions [55,57] and no consensus for optimal application time, applied pressure, composition as well as shape and design [57] could be provided thus far. Overall there is limited evidence to suggest that compression garments impact athletic performance [58,59,60], but there may be legitimation for its use in terms of recovery [55,57,61,62].
4.2.1. Compression Therapy during Exercise
Bringard et al. suggest that wearing compression garments during exercise may enhance muscle perfusion and decrease muscle oscillation which thereby promotes a lower energy expenditure and an improvement or maintenance in submaximal running speed [63]. Moreover, it is reported that compression garments lead to increased comfort [12,57,64] and support the underlying tissue resulting in reduced microtrauma and muscular damage [62,65]. In contrast, a systematic review by Beliard et al. reported that nine from ten studies did not show any performance enhancing effects [57], nor significant changes in objective physiological variables such as increased oxygen uptake or plasma level related changes of lactate or CK [12,63,64,66]. Only Kemmler et al. could demonstrate a significant performance effect (time under load, total work) for calf compression in male runners [66]. In summary, wearing compression garments during exercise (triathlon) might lead to marginal improvements in performance; however, evidence is inconclusive.
4.2.2. Compression Therapy Post Exercise
For post exercise compression therapy, heterogeneous modalities are discussed. For the prevention of DOMS, several studies have shown positive effects on recovery, function and strength of the treated muscle groups [12,55,57,67]. The decrease of CK levels shown in two studies [15,55,57] and the reduction of lactate level [67,68] could be seen as valid markers for improved regeneration. This could be attributed to an attenuation in the release of CK into the bloodstream, improved clearance from the circulation and enhanced repair of the damaged muscle tissue [12,57]. This theory could however not be confirmed by MRI based investigations which showed no reduction in edema or DOMS in the calf muscles [24]. In the same study, the only parameter shown to be significant was a faster normalization of muscle stiffness.
4.2.3. Intermittent Compression Therapy
A further available treatment strategy is intermittent compression therapy. The NormaTec Pulse Massage Pattern (The NormaTec PULSE recovery Systems, NormaTec, Watertown, Massachusetts, USA) works with a pulsating, dynamic, upwards moving compression with the goal of mobilizing fluids and supporting the outflow out of the extremities [12]. This method is poorly investigated with only one study exists showing local hyperermia [69]. Pneumatic compression pants did not alter the rate of muscle glycogen resynthesis, blood lactate, or blood glucose and insulin concentrations associated with a post-exercise oral glucose load [70]. Further, Haun et al. reported a decrease in DOMS and potential reduction in muscle proteolysis as well as oxidative stress [71]. There is a need for further research related to mechanistic changes.
Practical implications: Based on the evidence reviewed, there is no generalized recommendation for use of compression garments during exercise, but if the athlete reports subjective benefits, then it may have a positive impact. There is evidence suggesting that compression can play a role in enhanced post-exercise recovery, whilst evidence for dynamic compression is inconclusive.
4.3. Thermal Therapy
4.3.1. Cold Water Immersion Therapy (CWI)
Systemic cooling for post-exercise recovery and regeneration has become more widespread in elite sport. Specifically, CWI has established itself as an effective therapy to cope with EIMD and alleviate physiological and functional deficits [72]. There is high level evidence for its clinical effectiveness in regard to an enhanced regeneration [12]. Hohenauer et al. emphasized, that cooling is superior in comparison to passive recovery strategies with CWI achieving the best results in reducing the symptoms of DOMS [73]. This was confirmed by Leeder et al., especially up to 96 hrs post exercise [74]. Various aspects promoting a faster regeneration are suggested, for example, a facilitated removal of metabolites [75]; limitation of inflammation and cell damage [76]; analgesic effects through activation of M8 cation channels (TRPM8), located in a and c fibres [77]; compression through increased hydrostatic pressure [75] and especially a decreased tissue temperature, blood flow and cardiovascular strain [74,76,78]. Referring to the water temperature, the best results were found to be between 11 and 15 °C for 11–15 min. [72]. Also, the efficacy of CWI seems to be depended of the previous type of exercise. CWI is thought to be most effective in attenuating EIMD induced by whole body prolonged endurance-based exercise [79]. Inflammatory processes may be limited through a coldness dependent down regulation of intramuscular metabolism [80]; however, associated adverse effects with regards to glycogen resynthesis or lactate metabolism cannot be assumed and have to be investigated further.
Practical implications: Taking into account the different practical aspects, CWI seems to be an appropriate short-term recovery modality of exercise-induced muscle injuries in triathletes, especially within the new framework that includes mixed relay competition. Beside positive muscle injury related effects, CWI should be viewed critically in regard to glycogen and energy metabolism. The application of CWI should be adjusted to suit the environmental conditions such as climate, local equipment, conditions and, not least, the athlete’s individual preference in order to be most effective.
4.3.2. Heat Therapy
The application of heat therapy is still controversially discussed, and studies have to be regarded cautiously in the examined context. Study protocols vary from experimental designs in isolated mouse soleus muscle to gain information about glycogen and energy metabolism [81], to studies focusing mainly on clinical outcomes like maximal range of movement (ROM) [82] or voluntary contraction and muscle steadiness after sauna [83]. In regards to the acute inflammatory response leading to DOMS (between 48–72hrs), whole-body heat therapy has to be regarded critically [28]. In contrast, after the outlined peak, heat therapy can support soft tissue repair, tissue nutrition and circulation [84,85]. Studies show a positive effect in gaining muscle strength associated with hypertrophy (10 weeks heat therapy without strength training) through provoked gene expression for growth and differentiation [12,86] enhanced recovery after eccentric resistance training with an acceleration of angiogenic factors in human knee extensor muscle [87] and an acceleration of muscle contractility properties and decreased muscle steadiness after whole-body heat therapy by sauna [83]. In contrast Frier et al. emphasizes pre-exercise heat stress may inhibit increases in muscle mass, potentially caused by accumulation of heat shock proteins in lower limbs of rats [88].
Practical implications: For the application of heat therapy in triathlons, no general recommendation can be made at this point. Especially for acute injuries in the first inflammation phase, cooling is the preferred strategy. After the inflammatory response or recovery without muscle injury, heat therapy can support regeneration and improved tissue healing. Unfortunately, there are no available studies with an endurance-based protocol, specifically relating to long-term muscle load such as the duration of a triathlon event.
4.4. Active Regeneration
Conventional strategies such as low intensity exercise and stretching have a long tradition in sports [89], whilst there has been a surge in innovative techniques recently which are yet to be fully investigated. Low intensity training is suggested after eccentric or high-intensity training sessions inducing DOMS, which is associated with muscle pain and tenderness [90], as well as compromised performance and swelling [28]. It has been proposed that the short-term alleviation of pain during exercise is due to the breakup of adhesions in the sore muscles, an increased removal of noxious waste products via an increased blood flow or an increased endorphin release [90]. There are two studies inducing DOMS with an eccentric exercise protocol in upper arm [91] and wrist extensor muscles [92] followed by 8–10 min ergometry; neither was unable to show any clinical advantage [90]. In contrast Hasson et al. reported a significant decrease in DOMS 48 hrs after a high velocity concentric isokinetic exercise of the knee extensors and flexors by performing a stepping exercise 24 hrs after the initial training [90,93]. In summary, study results related to recovery from DOMS are heterogenous, without any clear conclusion.
Furthermore, in regard to fatigue inducing exercise, Vanderthommen et al. were unable to show any superior effect in performance or pain of active compared to passive regeneration after isometric muscle contraction [94]. The same recovery modality of pedaling on a bicycle ergometer with a moderate load had however demonstrated an improvement in the recovery process [94]. These studies showed a superior blood lactate removal following active recovery [95,96] compared to passive recovery. In a randomized controlled trial from 2018 no positive effects of dynamic contract-relax stretching in either strength or in ROM or pain threshold could be confirmed [97]. Moreover, stretching after eccentric exercises failed to prove its efficacy [90], therefore it was concluded that there is insufficient data for stretching as a strategy to enhance recovery [98].A new form of active regeneration is foam rolling, as a method of self-myofascial release, which has become popular in recovery [12] with ubiquitous use through all performance levels. Several studies have examined the effect of post muscle damaging exercise foam rolling. All studies reported a significant reduction of pain, whilst two also showed objective benefits in sprint and jump performance and in ROM [17,99], which was, however, contradicted by the findings of Jay et al. [100]. As another clinical outcome Fleckenstein et al. observed a significant effect of foam rolling on neuromuscular exhaustion as maximal isometric voluntary force of the knee extensors and pain [101]. The only study observing the rate of blood lactate clearance was conducted after a 100 m water-rescue in life guards which was also found to be significant [102]. In conclusion, foam rolling seems to be effective in pain reduction, but further benefits have yet to be conclusively reported. The underlying physiological principles and potential risks also remain unclear [103,104].
Practical implications: As an active recovery strategy, low intensity training in form of 15 min of pedaling directly after exercise might have a recovery enhancing effect, however, there is little evidence of performance enhancement or objective support for muscle healing [12].
4.5. Nutrition
The importance of post-exercise nutrition as a critical component of recovery is widely accepted. However, evidence-based dietary recommendations specifically related to elite triathletes are still lacking. There are many studies evaluating the effects of nutritional expression of DOMS after EIMD. The importance of protein supplementation for endurance triathletes is increasingly accepted. Post-exercise protein supplementation enhances muscle protein synthesis and satellite cell activity for muscle repair, furthermore facilitates muscle glycogen resynthesis [105]. Beside this, branched-chain amino acids (BCAAs) which are mainly metabolized in skeletal muscle [106], are thought to have further positive effects on exercise-related cytokine production in cases of structural and metabolic processes due to exercise damage [12,107]. A review analyzing the effects of branched-chain amino acids (BCAAs) in endurance sports concluded that supplementation with BCAAs lowers the degree of pain and muscle damage, perceived exertion and mental fatigue, but stimulates the anabolic response in recovery and improves the immune response. There was no consensus about the dose and timing, but it seems to be most effective if there is 2–3/1 1g relationship between leucine/ isoleucine and valine amino acids [108]. Doering et al. suggest that masters athletes may have slower recovery rates due to impaired muscle remodeling mechanism, compared to younger, equally trained athletes, after muscle-damaging endurance exercise. Given this fact, masters athletes could benefit from higher doses of post exercise dietary protein intake, especially with leucine [105]. A systematic review showed that a high daily BCAA supplementation (>200 mg kg −1 day −1) for a long period (>10 days) was particularly effective when the extent of muscle damage was low-to-moderate and consumed pre-exercise [12,40,109]. Another important nutritional component targeting a fast and ideal recovery are the omega-3-fatty acids. By limitation of anti-inflammatory responses and oxidative stress, omega-3-fatty acids significantly reduce the DOMS sensations. Therefore, it is recommended to ingest 1.8–3 g of omega-3-fatty acids after exercise [110,111].
5. Conclusions
The present work provides an overview of the pathophysiological pathway, as well as the various treatment strategies in the field of exercise-induced muscle injuries, and evaluates their effectiveness with respect to the existing scientific evidence and practical expertise (Table 2). As a limitation of this review, there are only a few studies dealing with specific interventions in elite triathletes. Most existing investigations focusing on the pathogenesis or interventions in exercise-induced muscle injuries consist of a wide spectrum of athletes and different accompanying metabolic demands. Further, when interpreting triathlon specific data, different metabolic demands in short and long-distance athletes have to be considered, and it is unclear if given general recommendations can be completely transferred to Olympic triathletes. The authors agree that there is a compelling need for further studies, including high-quality randomized trials, to completely evaluate the effectiveness of existing therapeutic approaches. The given recommendations must be updated and adjusted as further evidence emerges.

Table 2.
Overview of discussed interventions in treatment and prevention of exercise-induced muscle damages.
Author Contributions
T.H., M.W.H., C.G. and M.E. designed the manuscript. T.H. and R.H. have made major contributions in section “Results”. I.M., M.H., C.L., K.P. and T.K. have made major contributions in drafting and writing the section “Discussion”. All authors read and approved the final manuscript.
Funding
This research received no external funding.
Acknowledgments
The English language support of Annika Wing is gratefully acknowledged.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kienstra, C.M.; Asken, T.R.; Garcia, J.D.; Lara, V.; Best, T.M. Triathlon Injuries: Transitioning from Prevalence to Prediction and Prevention. Curr. Sports Med. Rep. 2017, 16, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Olcina, G.; Timon, R.; Brazo-Sayavera, J.; Martinez-Guardado, I.; Marcos-Serrano, M.; Crespo, C. Changes in physiological and performance variables in non-professional triathletes after taking part in an Olympic distance triathlon. Res. Sports Med. (Print) 2018, 26, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Neidel, P.; Wolfram, P.; Hotfiel, T.; Engelhardt, M.; Koch, R.; Lee, G.; Zwingenberger, S. Cross-Sectional Investigation of Stress Fractures in German Elite Triathletes. Sports 2019, 7, 88. [Google Scholar] [CrossRef] [PubMed]
- International Triathlon Union. Available online: https://www.triathlon.org/ (accessed on 1 May 2019).
- Jeukendrup, A.E.; Jentjens, R.L.; Moseley, L. Nutritional considerations in triathlon. Sports Med. (Auckl. NZ) 2005, 35, 163–181. [Google Scholar] [CrossRef] [PubMed]
- Del Coso, J.; Gonzalez-Millan, C.; Salinero, J.J.; Abian-Vicen, J.; Soriano, L.; Garde, S.; Perez-Gonzalez, B. Muscle damage and its relationship with muscle fatigue during a half-iron triathlon. PLoS ONE 2012, 7, e43280. [Google Scholar] [CrossRef]
- Hiller, W.D. Dehydration and hyponatremia during triathlons. Med. Sci. Sports Exerc. 1989, 21, S219–S221. [Google Scholar]
- Speedy, D.B.; Noakes, T.D.; Kimber, N.E.; Rogers, I.R.; Thompson, J.M.; Boswell, D.R.; Ross, J.J.; Campbell, R.G.; Gallagher, P.G.; Kuttner, J.A. Fluid balance during and after an ironman triathlon. Clin. J. Sport Med. 2001, 11, 44–50. [Google Scholar] [CrossRef]
- Margaritis, I.; Tessier, F.; Verdera, F.; Bermon, S.; Marconnet, P. Muscle enzyme release does not predict muscle function impairment after triathlon. J. Sports Med. Phys. Fit. 1999, 39, 133–139. [Google Scholar]
- Galan, B.S.; Carvalho, F.G.; Santos, P.C.; Gobbi, R.B.; Kalva-Filho, C.A.; Papoti, M.; da Silva, A.S.; Freitas, E.C. Effects of taurine on markers of muscle damage, inflammatory response and physical performance in triathletes. J. Sports Med. Phys. Fit. 2018, 58, 1318–1324. [Google Scholar] [CrossRef]
- Fernandez-Revelles, A.B. Infographic. Correlation between phases and final result in Men’s triathlon competition at the Olympic Games in Sydney 2000. Br. J. Sports Med. 2018. [Google Scholar] [CrossRef]
- Heiss, R.; Freiwald, J.; Hoppe, M.W.; Lutter, C.; Forst, R.; Grim, C.; Poettgen, K.; Bloch, W.; Huttel, M.; Hotfiel, T. Advances in Delayed-Onset Muscle Soreness (DOMS): Part II: Treatment and Prevention. Sportverletz. Sportschaden 2019, 33, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Crowther, F.; Sealey, R.; Crowe, M.; Edwards, A.; Halson, S. Influence of recovery strategies upon performance and perceptions following fatiguing exercise: A randomized controlled trial. BMC Sports Sci. Med. Rehabil. 2017, 9, 25. [Google Scholar] [CrossRef] [PubMed]
- Hausswirth, C.; Mujika, I. Recovery for Performance in Sport; Human Kinetics: Champaign, IL, USA, 2013. [Google Scholar]
- Meyer, T.; Ferrauti, A.; Kellmann, M.; Pfeiffer, M. Regenerationsmanagement im Spitzensport. REGman-Ergebnisse und Handlungsempfehlungen; Sportverlag Strauß: Hellenthal, Germany, 2016. [Google Scholar]
- Hotfiel, T.; Seil, R.; Bily, W.; Bloch, W.; Gokeler, A.; Krifter, R.M.; Mayer, F.; Ueblacker, P.; Weisskopf, L.; Engelhardt, M. Nonoperative treatment of muscle injuries–recommendations from the GOTS expert meeting. J. Exp. Orthop. 2018, 5, 24. [Google Scholar] [CrossRef] [PubMed]
- Pearcey, G.E.; Bradbury-Squires, D.J.; Kawamoto, J.E.; Drinkwater, E.J.; Behm, D.G.; Button, D.C. Foam rolling for delayed-onset muscle soreness and recovery of dynamic performance measures. J. Athl. Train. 2015, 50, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Valle, X.; Til, L.; Drobnic, F.; Turmo, A.; Montoro, J.B.; Valero, O.; Artells, R. Compression garments to prevent delayed onset muscle soreness in soccer players. Muscles Ligaments Tendons J. 2013, 3, 295–302. [Google Scholar] [CrossRef]
- Kim, S.K.; Kim, M.C. The affect on delayed onset muscle soreness recovery for ultrasound with bee venom. J. Phys. Ther. Sci. 2014, 26, 1419–1421. [Google Scholar] [CrossRef] [PubMed]
- Mizuno, S.; Morii, I.; Tsuchiya, Y.; Goto, K. Wearing Compression Garment after Endurance Exercise Promotes Recovery of Exercise Performance. Int. J. Sports Med. 2016, 37, 870–877. [Google Scholar] [CrossRef]
- Hotfiel, T.; Kellermann, M.; Swoboda, B.; Wildner, D.; Golditz, T.; Grim, C.; Raithel, M.; Uder, M.; Heiss, R. Application of Acoustic Radiation Force Impulse (ARFI) Elastography in Imaging of Delayed Onset Muscle Soreness (DOMS): A Comparative Analysis With 3T MRI. J. Sport Rehabil. 2017, 1–29. [Google Scholar] [CrossRef]
- Pollock, N.; James, S.L.J.; Lee, J.C.; Chakraverty, R. British athletics muscle injury classification: A new grading system. Br. J. Sports Med. 2014, 48. [Google Scholar] [CrossRef]
- Mueller-Wohlfahrt, H.W.; Haensel, L.; Mithoefer, K.; Ekstrand, J.; English, B.; McNally, S.; Orchard, J.; van Dijk, C.N.; Kerkhoffs, G.M.; Schamasch, P.; et al. Terminology and classification of muscle injuries in sport: The Munich consensus statement. Br. J. Sports Med. 2013, 47, 342–350. [Google Scholar] [CrossRef]
- Heiss, R.; Kellermann, M.; Swoboda, B.; Grim, C.; Lutter, C.; May, M.S.; Wuest, W.; Uder, M.; Nagel, A.M.; Hotfiel, T. Effect of Compression Garments on the Development of Delayed-Onset Muscle Soreness: A Multimodal Approach Using Contrast-Enhanced Ultrasound and Acoustic Radiation Force Impulse Elastography. J. Orthop. Sports Phys. Ther. 2018, 48, 887–894. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.Y.; Jeong, J.G.; Lee, B.H. Evaluation of muscle damage using ultrasound imaging. J. Phys. Ther. Sci. 2015, 27, 531–534. [Google Scholar] [CrossRef] [PubMed]
- Kellermann, M.H.M.; Swoboda, B.; Gelse, K.; Freiwald, J.; Grim, C.; Nagel, A.; Uder, M.; Wildner, D.; Hotfiel, T. Intramuscular perfusion response in delayed onset muscle soreness (DOMS): A quantitative analysis with contrast-enhanced ultrasound (CEUS). Int. J. Sports Med. 2017, 38, 833–841. [Google Scholar] [CrossRef] [PubMed]
- Paulsen, G.; Mikkelsen, U.R.; Raastad, T.; Peake, J.M. Leucocytes, cytokines and satellite cells: What role do they play in muscle damage and regeneration following eccentric exercise? Exerc. Immunol. Rev. 2012, 18, 42–97. [Google Scholar] [PubMed]
- Hotfiel, T.; Freiwald, J.; Hoppe, M.W.; Lutter, C.; Forst, R.; Grim, C.; Bloch, W.; Huttel, M.; Heiss, R. Advances in Delayed-Onset Muscle Soreness (DOMS): Part I: Pathogenesis and Diagnostics. Sportverletz. Sportschaden 2018, 32, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Peake, J.; Nosaka, K.; Suzuki, K. Characterization of inflammatory responses to eccentric exercise in humans. Exerc. Immunol. Rev. 2005, 11, 64–85. [Google Scholar] [PubMed]
- Lewis, P.B.; Ruby, D.; Bush-Joseph, C.A. Muscle soreness and delayed-onset muscle soreness. Clin. Sports Med. 2012, 31, 255–262. [Google Scholar] [CrossRef]
- Douglas, J.; Pearson, S.; Ross, A.; McGuigan, M. Eccentric Exercise: Physiological Characteristics and Acute Responses. Sports Med. (Auckl. NZ) 2017, 47, 663–675. [Google Scholar] [CrossRef]
- Linari, M.; Lucii, L.; Reconditi, M.; Casoni, M.E.; Amenitsch, H.; Bernstorff, S.; Piazzesi, G.; Lombardi, V. A combined mechanical and X-ray diffraction study of stretch potentiation in single frog muscle fibres. J. Physiol. 2000, 526 Pt 3, 589–596. [Google Scholar] [CrossRef]
- Nishikawa, K.C.; Monroy, J.A.; Uyeno, T.E.; Yeo, S.H.; Pai, D.K.; Lindstedt, S.L. Is titin a ‘winding filament’? A new twist on muscle contraction. Proc. Biol. Sci. 2012, 279, 981–990. [Google Scholar] [CrossRef]
- Herzog, W. Mechanisms of enhanced force production in lengthening (eccentric) muscle contractions. J. Appl. Physiol. (Bethesda MD 1985) 2014, 116, 1407–1417. [Google Scholar] [CrossRef] [PubMed]
- Nicol, C.; Avela, J.; Komi, P.V. The stretch-shortening cycle: A model to study naturally occurring neuromuscular fatigue. Sports Med. (Auckl. NZ) 2006, 36, 977–999. [Google Scholar] [CrossRef] [PubMed]
- Tesch, P.A.; Fernandez-Gonzalo, R.; Lundberg, T.R. Clinical Applications of Iso-Inertial, Eccentric-Overload (YoYo) Resistance Exercise. Front. Physiol. 2017, 8, 241. [Google Scholar] [CrossRef] [PubMed]
- Pinho, R.A.; Silva, L.A.; Pinho, C.A.; Scheffer, D.L.; Souza, C.T.; Benetti, M.; Carvalho, T.; Dal-Pizzol, F. Oxidative stress and inflammatory parameters after an Ironman race. Clin. J. Sport Med. 2010, 20, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Yanagisawa, O.; Sakuma, J.; Kawakami, Y.; Suzuki, K.; Fukubayashi, T. Effect of exercise-induced muscle damage on muscle hardness evaluated by ultrasound real-time tissue elastography. Springerplus 2015, 4, 308. [Google Scholar] [CrossRef] [PubMed]
- Nie, H.; Madeleine, P.; Arendt-Nielsen, L.; Graven-Nielsen, T. Temporal summation of pressure pain during muscle hyperalgesia evoked by nerve growth factor and eccentric contractions. Eur. J. Pain 2009, 13, 704–710. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Lee, J. A review of nutritional intervention on delayed onset muscle soreness. Part I. J. Exerc. Rehabil. 2014, 10, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Kraemer, W.J.; Bush, J.A.; Wickham, R.B.; Denegar, C.R.; Gomez, A.L.; Gotshalk, L.A.; Duncan, N.D.; Volek, J.S.; Putukian, M.; Sebastianelli, W.J. Influence of compression therapy on symptoms following soft tissue injury from maximal eccentric exercise. J. Orthop. Sports Phys. Ther. 2001, 31, 282–290. [Google Scholar] [CrossRef]
- Ulbricht, A.; Gehlert, S.; Leciejewski, B.; Schiffer, T.; Bloch, W.; Hohfeld, J. Induction and adaptation of chaperone-assisted selective autophagy CASA in response to resistance exercise in human skeletal muscle. Autophagy 2015, 11, 538–546. [Google Scholar] [CrossRef]
- Deme, D.; Telekes, A. Prognostic importance of lactate dehydrogenase (LDH) in oncology. Orv. Hetil. 2017, 158, 1977–1988. [Google Scholar] [CrossRef]
- Del Giudice, M.; Gangestad, S.W. Rethinking IL-6 and CRP: Why They Are More Than Inflammatory Biomarkers, and Why It Matters. Brain Behav. Immun. 2018. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.S.H.; Teo, W.P.; Warmington, S.A. Effects of training and competition on the sleep of elite athletes: A systematic review and meta-analysis. Br. J. Sports Med. 2018. [Google Scholar] [CrossRef] [PubMed]
- Hausswirth, C.; Louis, J.; Aubry, A.; Bonnet, G.; Duffield, R.; Le Meur, Y. Evidence of disturbed sleep and increased illness in overreached endurance athletes. Med. Sci. Sports Exerc. 2014, 46, 1036–1045. [Google Scholar] [CrossRef] [PubMed]
- Halson, S.L. Sleep in elite athletes and nutritional interventions to enhance sleep. Sports Med. (Auckl. NZ) 2014, 44 (Suppl. 1), S13–S23. [Google Scholar] [CrossRef] [PubMed]
- Watson, A.M. Sleep and Athletic Performance. Curr. Sports Med. Rep. 2017, 16, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Kirschen, G.W.; Jones, J.J.; Hale, L. The Impact of Sleep Duration on Performance Among Competitive Athletes: A Systematic Literature Review. Clin. J. Sport Med. 2018. [Google Scholar] [CrossRef] [PubMed]
- Bonnar, D.; Bartel, K.; Kakoschke, N.; Lang, C. Sleep Interventions Designed to Improve Athletic Performance and Recovery: A Systematic Review of Current Approaches. Sports Med. (Auckl. NZ) 2018, 48, 683–703. [Google Scholar] [CrossRef]
- Thun, E.; Bjorvatn, B.; Flo, E.; Harris, A.; Pallesen, S. Sleep, circadian rhythms, and athletic performance. Sleep Med. Rev. 2015, 23, 1–9. [Google Scholar] [CrossRef]
- Milner, C.E.; Cote, K.A. Benefits of napping in healthy adults: Impact of nap length, time of day, age, and experience with napping. J. Sleep Res. 2009, 18, 272–281. [Google Scholar] [CrossRef]
- Waterhouse, J.; Atkinson, G.; Edwards, B.; Reilly, T. The role of a short post-lunch nap in improving cognitive, motor, and sprint performance in participants with partial sleep deprivation. J. Sports Sci. 2007, 25, 1557–1566. [Google Scholar] [CrossRef]
- Simpson, N.S.; Gibbs, E.L.; Matheson, G.O. Optimizing sleep to maximize performance: Implications and recommendations for elite athletes. Scand. J. Med. Sci. Sports 2017, 27, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.; Howatson, G.; van Someren, K.; Leeder, J.; Pedlar, C. Compression garments and recovery from exercise-induced muscle damage: A meta-analysis. Br. J. Sports Med. 2014, 48, 1340–1346. [Google Scholar] [CrossRef] [PubMed]
- Marques-Jimenez, D.; Calleja-Gonzalez, J.; Arratibel, I.; Delextrat, A.; Terrados, N. Are compression garments effective for the recovery of exercise-induced muscle damage? A systematic review with meta-analysis. Physiol. Behav. 2016, 153, 133–148. [Google Scholar] [CrossRef] [PubMed]
- Beliard, S.; Chauveau, M.; Moscatiello, T.; Cros, F.; Ecarnot, F.; Becker, F. Compression garments and exercise: No influence of pressure applied. J. Sports Sci. Med. 2015, 14, 75. [Google Scholar] [PubMed]
- da Silva, C.A.; Helal, L.; da Silva, R.P.; Belli, K.C.; Umpierre, D.; Stein, R. Association of Lower Limb Compression Garments During High-Intensity Exercise with Performance and Physiological Responses: A Systematic Review and Meta-analysis. Sports Med. 2018, 48, 1859–1873. [Google Scholar] [CrossRef] [PubMed]
- Venckunas, T.; Trinkunas, E.; Kamandulis, S.; Poderys, J.; Grunovas, A.; Brazaitis, M. Effect of lower body compression garments on hemodynamics in response to running session. Sci. World J. 2014, 2014, 353040. [Google Scholar] [CrossRef] [PubMed]
- Duffield, R.; Portus, M. Comparison of three types of full-body compression garments on throwing and repeat-sprint performance in cricket players. Br. J. Sports Med. 2007, 41, 409–414; discussion 414. [Google Scholar] [CrossRef]
- Kim, J.; Kim, J.; Lee, J. Effect of compression garments on delayed-onset muscle soreness and blood inflammatory markers after eccentric exercise: A randomized controlled trial. J. Exerc. Rehabil. 2017, 13, 541–545. [Google Scholar] [CrossRef]
- Trenell, M.I.; Rooney, K.B.; Sue, C.M.; Thomspon, C.H. Compression Garments and Recovery from Eccentric Exercise: A (31)P-MRS Study. J. Sports Sci. Med. 2006, 5, 106–114. [Google Scholar]
- Bringard, A.; Perrey, S.; Belluye, N. Aerobic energy cost and sensation responses during submaximal running exercise--positive effects of wearing compression tights. Int. J. Sports Med. 2006, 27, 373–378. [Google Scholar] [CrossRef]
- Ali, A.; Caine, M.P.; Snow, B.G. Graduated compression stockings: Physiological and perceptual responses during and after exercise. J. Sports Sci. 2007, 25, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Sperlich, B.; Born, D.-P.; Kaskinoro, K.; Kalliokoski, K.K.; Laaksonen, M.S. Squeezing the muscle: Compression clothing and muscle metabolism during recovery from high intensity exercise. PLoS ONE 2013, 8, e60923. [Google Scholar] [CrossRef] [PubMed]
- Kemmler, W.; von Stengel, S.; Kockritz, C.; Mayhew, J.; Wassermann, A.; Zapf, J. Effect of compression stockings on running performance in men runners. J. Strength Cond. Res. 2009, 23, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Hamlin, M.J.; Mitchell, C.J.; Ward, F.D.; Draper, N.; Shearman, J.P.; Kimber, N.E. Effect of compression garments on short-term recovery of repeated sprint and 3-km running performance in rugby union players. J. Strength Cond. Res. 2012, 26, 2975–2982. [Google Scholar] [CrossRef]
- Chatard, J.C.; Atlaoui, D.; Farjanel, J.; Louisy, F.; Rastel, D.; Guezennec, C.Y. Elastic stockings, performance and leg pain recovery in 63-year-old sportsmen. Eur. J. Appl. Physiol. 2004, 93, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.S.; Borges, A.R.; Beck, D.T. Peripheral conduit and resistance artery function are improved following a single, 1-h bout of peristaltic pulse external pneumatic compression. Eur. J. Appl. Physiol. 2015, 115, 2019–2029. [Google Scholar] [CrossRef] [PubMed]
- Keck, N.A.; Cuddy, J.S.; Hailes, W.S.; Dumke, C.L.; Ruby, B.C. Effects of commercially available pneumatic compression on muscle glycogen recovery after exercise. J. Strength Cond. Res. 2015, 29, 379–385. [Google Scholar] [CrossRef]
- Haun, C.T.; Roberts, M.D.; Romero, M.A.; Osburn, S.C.; Mobley, C.B.; Anderson, R.G.; Goodlett, M.D.; Pascoe, D.D.; Martin, J.S. Does external pneumatic compression treatment between bouts of overreaching resistance training sessions exert differential effects on molecular signaling and performance-related variables compared to passive recovery? An exploratory study. PLoS ONE 2017, 12, e0180429. [Google Scholar] [CrossRef]
- Machado, A.F.; Ferreira, P.H.; Micheletti, J.K.; de Almeida, A.C.; Lemes, I.R.; Vanderlei, F.M.; Netto Junior, J.; Pastre, C.M. Can Water Temperature and Immersion Time Influence the Effect of Cold Water Immersion on Muscle Soreness? A Systematic Review and Meta-Analysis. Sports Med. (Auckl. NZ) 2016, 46, 503–514. [Google Scholar] [CrossRef]
- Hohenauer, E.; Taeymans, J.; Baeyens, J.P.; Clarys, P.; Clijsen, R. The Effect of Post-Exercise Cryotherapy on Recovery Characteristics: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0139028. [Google Scholar] [CrossRef]
- Leeder, J.; Gissane, C.; van Someren, K.; Gregson, W.; Howatson, G. Cold water immersion and recovery from strenuous exercise: A meta-analysis. Br. J. Sports Med. 2012, 46, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Stocks, J.M.; Patterson, M.J.; Hyde, D.E.; Jenkins, A.B.; Mittleman, K.D.; Taylor, N.A. Effects of immersion water temperature on whole-body fluid distribution in humans. Acta Physiol. Scand. 2004, 182, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Wilcock, I.M.; Cronin, J.B.; Hing, W.A. Physiological response to water immersion: A method for sport recovery? Sports Med. 2006, 36, 747–765. [Google Scholar] [CrossRef] [PubMed]
- Proudfoot, C.J.; Garry, E.M.; Cottrell, D.F.; Rosie, R.; Anderson, H.; Robertson, D.C.; Fleetwood-Walker, S.M.; Mitchell, R. Analgesia mediated by the TRPM8 cold receptor in chronic neuropathic pain. Curr. Biol. 2006, 16, 1591–1605. [Google Scholar] [CrossRef] [PubMed]
- Swenson, C.; Sward, L.; Karlsson, J. Cryotherapy in sports medicine. Scand. J. Med. Sci. Sports 1996, 6, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Ihsan, M.; Watson, G.; Abbiss, C.R. What are the physiological mechanisms for post-exercise cold water immersion in the recovery from prolonged endurance and intermittent exercise? Sports Med. 2016, 46, 1095–1109. [Google Scholar] [CrossRef] [PubMed]
- Merrick, M.A.; Rankin, J.M.; Andres, F.A.; Hinman, C.L. A preliminary examination of cryotherapy and secondary injury in skeletal muscle. Med. Sci. Sports Exerc. 1999, 31, 1516–1521. [Google Scholar] [CrossRef] [PubMed]
- Blackwood, S.J.; Hanya, E.; Katz, A. Effect of post-exercise temperature elevation on post-exercise glycogen metabolism of isolated mouse soleus muscle. J. Appl. Physiol. (1985) 2019. [Google Scholar] [CrossRef] [PubMed]
- Saga, N.; Katamoto, S.; Naito, H. Effect of heat preconditioning by microwave hyperthermia on human skeletal muscle after eccentric exercise. J. Sports Sci. Med. 2008, 7, 176–183. [Google Scholar] [PubMed]
- Cernych, M.; Baranauskiene, N.; Vitkauskiene, A.; Satas, A.; Brazaitis, M. Accelerated muscle contractility and decreased muscle steadiness following sauna recovery do not induce greater neuromuscular fatigability during sustained submaximal contractions. Hum. Mov. Sci. 2019, 63, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Halvorson, G.A. Therapeutic Heat and Cold for Athletic Injuries. Phys. Sportsmed. 1990, 18, 87–94. [Google Scholar] [CrossRef]
- Lohman, E.B., 3rd; Bains, G.S.; Lohman, T.; DeLeon, M.; Petrofsky, J.S. A comparison of the effect of a variety of thermal and vibratory modalities on skin temperature and blood flow in healthy volunteers. Med. Sci. Monit. 2011, 17, MT72–81. [Google Scholar] [CrossRef] [PubMed]
- Goto, K.; Oda, H.; Kondo, H.; Igaki, M.; Suzuki, A.; Tsuchiya, S.; Murase, T.; Hase, T.; Fujiya, H.; Matsumoto, I.; et al. Responses of muscle mass, strength and gene transcripts to long-term heat stress in healthy human subjects. Eur. J. Appl. Physiol. 2011, 111, 17–27. [Google Scholar] [CrossRef]
- Kim, K.; Kuang, S.; Song, Q.; Gavin, T.P.; Roseguini, B.T. Impact of heat therapy on recovery following eccentric exercise in humans. J. Appl. Physiol. (1985) 2019. [Google Scholar] [CrossRef]
- Frier, B.C.; Locke, M. Heat stress inhibits skeletal muscle hypertrophy. Cell Stress Chaperones 2007, 12, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Freiwald, J. Optimales Dehnen: Sport-Prävention-Rehabilitation; Spitta Verlag: Balingen, Germany, 2013. [Google Scholar]
- Cheung, K.; Hume, P.A.; Maxwell, L. Delayed Onset Muscle Soreness. Sports Med. 2003, 33, 145–164. [Google Scholar] [CrossRef]
- Weber, M.D.; Servedio, F.J.; Woodall, W.R. The effects of three modalities on delayed onset muscle soreness. J. Orthop. Sports Phys. Ther. 1994, 20, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Gulick, D.T.; Kimura, I.F.; Sitler, M.; Paolone, A.; Kelly IV, J.D. Various treatment techniques on signs and symptoms of delayed onset muscle soreness. J. Athl. Train. 1996, 31, 145. [Google Scholar]
- Hasson, S.M.; Williams, J.; Signorile, J. Fatigue-induced changes in myoelectric signal characteristics and perceived exertion. Can. J. Sport Sci. 1989, 14, 99–102. [Google Scholar]
- Vanderthommen, M.; Makrof, S.; Demoulin, C. Comparison of active and electrostimulated recovery strategies after fatiguing exercise. J. Sports Sci. Med. 2010, 9, 164–169. [Google Scholar]
- Gupta, S.; Goswami, A.; Sadhukhan, A.K.; Mathur, D.N. Comparative study of lactate removal in short term massage of extremities, active recovery and a passive recovery period after supramaximal exercise sessions. Int. J. Sports Med. 1996, 17, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Bangsbo, J.; Graham, T.; Johansen, L.; Saltin, B. Muscle lactate metabolism in recovery from intense exhaustive exercise: Impact of light exercise. J. Appl. Physiol. (1985) 1994, 77, 1890–1895. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Feng, B.; Chen, K.; Andersen, L.L.; Page, P.; Wang, Y. The Efficacy of Dynamic Contract-Relax Stretching on Delayed-Onset Muscle Soreness Among Healthy Individuals: A Randomized Clinical Trial. Clin. J. Sport Med. 2018, 28, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Torres, R.; Ribeiro, F.; Alberto Duarte, J.; Cabri, J.M. Evidence of the physiotherapeutic interventions used currently after exercise-induced muscle damage: Systematic review and meta-analysis. Phys. Ther. Sport 2012, 13, 101–114. [Google Scholar] [CrossRef]
- Macdonald, G.Z.; Button, D.C.; Drinkwater, E.J.; Behm, D.G. Foam rolling as a recovery tool after an intense bout of physical activity. Med. Sci. Sports Exerc. 2014, 46, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Jay, K.; Sundstrup, E.; Sondergaard, S.D.; Behm, D.; Brandt, M.; Saervoll, C.A.; Jakobsen, M.D.; Andersen, L.L. Specific and cross over effects of massage for muscle soreness: Randomized controlled trial. Int. J. Sports Phys. Ther. 2014, 9, 82–91. [Google Scholar]
- Fleckenstein, J.; Wilke, J.; Vogt, L.; Banzer, W. Preventive and Regenerative Foam Rolling are Equally Effective in Reducing Fatigue-Related Impairments of Muscle Function following Exercise. J. Sports Sci. Med. 2017, 16, 474–479. [Google Scholar] [PubMed]
- Kalen, A.; Perez-Ferreiros, A.; Barcala-Furelos, R.; Fernandez-Mendez, M.; Padron-Cabo, A.; Prieto, J.A.; Rios-Ave, A.; Abelairas-Gomez, C. How can lifeguards recover better? A cross-over study comparing resting, running, and foam rolling. Am. J. Emerg. Med. 2017, 35, 1887–1891. [Google Scholar] [CrossRef] [PubMed]
- Freiwald, J.; Baumgart, C.; Kühnemann, M.; Hoppe, M.W. Foam-Rolling in sport and therapy–Potential benefits and risks. Sports Orthop. Traumatol. 2016, 32, 258–266. [Google Scholar] [CrossRef]
- Freiwald, J.; Baumgart, C.; Kühnemann, M.; Hoppe, M.W. Foam-Rolling in sport and therapy – Potential benefits and risks. Sports Orthopaedics and Traumatology 2016, 32, 267–275. [Google Scholar] [CrossRef]
- Doering, T.M.; Reaburn, P.R.; Phillips, S.M.; Jenkins, D.G. Postexercise Dietary Protein Strategies to Maximize Skeletal Muscle Repair and Remodeling in Masters Endurance Athletes: A Review. Int. J. Sport Nutr. Exerc. Metab. 2016, 26, 168–178. [Google Scholar] [CrossRef] [PubMed]
- Harper, A.E.; Miller, R.H.; Block, K.P. Branched-chain amino acid metabolism. Annu. Rev. Nutr. 1984, 4, 409–454. [Google Scholar] [CrossRef] [PubMed]
- Foure, A.; Bendahan, D. Is Branched-Chain Amino Acids Supplementation an Efficient Nutritional Strategy to Alleviate Skeletal Muscle Damage? A Systematic Review. Nutrients 2017, 9, 1047. [Google Scholar] [CrossRef]
- Salinas-Garcia, M.E.; Martinez-Sanz, J.M.; Urdampilleta, A.; Mielgo-Ayuso, J.; Norte Navarro, A.; Ortiz-Moncada, R. Effects of branched amino acids in endurance sports: A review. Nutr. Hosp. 2014, 31, 577–589. [Google Scholar] [CrossRef] [PubMed]
- Hurley, C.F.; Hatfield, D.L.; Riebe, D.A. The effect of caffeine ingestion on delayed onset muscle soreness. J. Strength Cond. Res. 2013, 27, 3101–3109. [Google Scholar] [CrossRef]
- Jouris, K.B.; McDaniel, J.L.; Weiss, E.P. The Effect of Omega-3 Fatty Acid Supplementation on the Inflammatory Response to eccentric strength exercise. J. Sports Sci. Med. 2011, 10, 432–438. [Google Scholar]
- Su, Q.S.; Tian, Y.; Zhang, J.G.; Zhang, H. Effects of allicin supplementation on plasma markers of exercise-induced muscle damage, IL-6 and antioxidant capacity. Eur. J. Appl. Physiol. 2008, 103, 275–283. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).