Abstract
Impaired exercise capacity is the core symptom of heart failure with preserved ejection fraction (HFpEF). We assessed effects of exercise training and Crataegus extract WS 1442 in HFpEF and aimed to identify mechanisms of action in an exploratory trial (German Clinical Trials Register DRKS00000259). 140 sedentary HFpEF NYHA II patients on standard treatment received eight weeks of aerobic endurance training and half were randomized to WS 1442 900 mg/day. Symptoms, 2 km walking time (T2km), parameters of exercise tolerance, cardiac and vascular function, muscular efficiency and skeletal muscular haemoglobin oxygen saturation (SO2) measured during a treadmill protocol were captured at baseline and after eight weeks. Adverse events were recorded during the trial. Mechanisms of action were explored by correlation and path analyses of changes. Symptoms and exercise capacity improved with training, but correlations between improvements were low and path models were rejected. SO2 increased, decreased or undulated with increasing exercise intensity in individual patients and was not altered by training. WS 1442 improved T2km (-12.7% vs. -8.4%, p = 0.019), tended to improve symptoms and to pronounce SO2-decrease with increasing exercise, an indicator of oxygen utilisation. Endurance training and WS 1442 were safe and well tolerated in combination with standard drug treatment.
1. Introduction
At least half of patients with chronic heart failure suffer from diastolic dysfunction with preserved left ventricular ejection fraction (HFpEF) [1]. Typically, these patients are elderly women with a long-standing history of arterial hypertension [1]. Impaired endothelial NO-availability has been implicated in the pathophysiology of HFpEF [2,3,4,5,6]. Current treatment guidelines for this patient population recommend optimal treatment of underlying diseases / risk factors and lifestyle modifications such as moderate exercise training [7,8]. More specific recommendations to improve symptoms, quality of life, and prognosis have not yet been established.
Crataegus extract WS 1442 has been demonstrated to improve symptoms and exercise tolerance in patients with heart failure, New York Heart Association (NYHA) stage II to III [9,10], but no specific trials in patients with HFpEF have been conducted. WS 1442 has been demonstrated to increase thickness and reduce stiffness of the endothelial inner surface layer (the glycocalix), a sensor of blood-flow induced shear stress and modulator of endothelial NO-synthesis [11]. The extract activates endothelial and red blood cell NO-synthase [12,13,14], increases endothelial NO-release and improves endothelium-dependent arterial function in animal models of aging and hypertension [15,16]. The vascular effects are strongly related to the high content of oligomeric procyanidins in the extract [13]. In addition, WS 1442 increases cardiac muscle force of contraction via an ATP-independent mechanism [17], has shown positive effects on remodelling in animal models of increased afterload [18,19,20] and increases skeletal muscle mitochondrial density and fibre diameter [21]. It has not been determined to what extent the reported vascular, cardiac and skeletal muscular effects contribute to the clinical benefit in heart failure patients.
Therefore, the present exploratory study aimed to assess the effects of WS 1442 when added to standard cardiological treatment and exercise training, on symptoms and quality of life, exercise capacity, cardiac, vascular, and muscular function in patients with HFpEF, stage NYHA II. Based on the comprehensive assessment, we aimed to identify mechanisms underlying the clinical benefit.
2. Method, Results, Discussion
2.1. Method
2.1.1. Design
The monocentric prospective randomized controlled open-label phase IV trial (German Clinical Trials Register DRKS00000259; EudraCT 2009-015005-39) was conducted according to ICH-GCP standards and local regulations after favourable opinion from the independent ethics committee of the Landesärztekammer Baden-Württemberg (Baden-Wuerttemberg State Chamber of Physicians), Stuttgart, Germany, and approval by the Federal Institute for Drugs and Medical Devices (BfArM).
2.1.2. Patients
Men and women (1:1, having given written informed consent) with a diagnosis of heart failure NYHA II, echocardiographically assessed resting LVEF > 40%, NT-pro BNP < 450 ng/ml and less than 2 hours of physical activity per week were recruited from a large ambulatory cardiological office in Karlsruhe, Germany. Exclusion criteria included severe or acute cardiac or general diseases, atrial flutter, pacemaker or ICD, significant deterioration of cardiac complaints during the preceding week, treatment with cardiac glycosides, hawthorn or other herbal drugs.
2.1.3. Treatments
All patients were continued on standard cardiological treatment for heart failure with LVEF > 40 % according to the German and European guidelines [7,8] and received eight weeks of exercise training. The training comprised 90 minutes training sessions twice a week according to a detailed written manual conducted by educated trainers from the Institute of Sports and Sport Science, Karlsruhe Institute of Technology. The training sessions included education, warm up, 50 minutes of aerobic exercise (walking), and relaxation. Exercise intensity was individually tailored to a target heart rate corridor using Polar RS800TM heart rate monitors. The target corridor boundaries corresponded to the individual aerobic and anaerobic lactic acid thresholds, determined during the baseline treadmill exercise test and calculated by the software Ergonizer, Version 3.1.0 (Prof. Dr. K. Röcker, Freiburg).
After inclusion patients were randomized 1:1 to training or training and eight weeks open label 450 mg b.i.d. WS® 1442 as film coated tablets (Crataegutt® novo 450 mg). WS 1442 is a dry extract from hawthorn leaves with flowers, drug-extract ratio 4 – 6.6 : 1, extraction solvent ethanol 45% (w/w). The extract is adjusted to 17.3 to 20.1% oligomeric procyanidins (manufacturer: Dr. Willmar Schwabe GmbH & Co. KG, Karlsruhe). Treatment was assigned to included patients by the investigator, opening a sealed randomization envelope with the lowest available randomization number for the patient’s gender. Envelopes were generated by a biometrician, not involved in study conduct, based on two randomization lists (for men and women) generated with software Randomizer (www.randomizer.at) using a block-size of 10.
2.1.4. Outcomes
Symptoms and Quality of Life were captured by the Kansas City Cardiomyopathy Questionnaire (KCCQ [22,23]). Exercise tolerance was assessed (1) for everyday moderate physical activities by the Freiburg Questionnaire of Physical Activity [24] and the 2-km Walking Test [25] and (2) for peak exercise capacity by a treadmill cardiopulmonary exercise protocol. The exercise protocol was performed in two-minute bouts with ascending intensity and a rest of 30 seconds between bouts, and terminated at (1) subjective exhaustion or (2) at a maximal safe heart rate individually determined by the treating cardiologist based on bicycle exercise testing at screening. Time to 2 mmol/l, 4 mmol/l, and individual lactate threshold [26], subjective exertion [27], VO2, VCO2 and end-expiratory CO2 (Cortex MetaMax® 3B spirometer) were assessed during treadmill (Woodway PPS 55med-I) exercise. In addition, a finger pulse plethysmography signal (BMEYE Nexfin HD Monitor) was recorded during treadmill exercise and indices of cardiac and vascular function (heart rate, blood pressure, cardiac output, stroke volume, dP/dt (maximum first derivative of pressure), and peripheral vascular resistance) were automatically calculated from the plethysmography signal. At the end of the exercise testing, a blood sample was drawn from the hyperaemic earlobe to calculate cardiac output from capillary blood and expiratory CO2 concentrations [28]. Muscular efficiency was determined by the ratio of VO2 and workload [29] at maximal exercise. Skeletal muscular haemoglobin oxygen saturation (SO2) was measured during treadmill exercise by a near infrared spectroscopy calf sensor (Hamamatsu Monitor NIRO 100). All outcomes as well as resting NT-pro-BNP were measured at baseline and after eight weeks. Adverse events were recorded to document tolerability and safety of applied treatments. Clinically relevant changes or new abnormal findings in safety laboratory parameters or physical examination were classified as adverse events.
2.1.5. Analysis
In line with the trial’s exploratory nature, no primary endpoint was defined and no formal sample size calculation was performed. A sample size of n = 140 was considered adequate based on previous experience [30] and for a planned path analysis with eight variables and 15 relations [31].
Efficacy analysis was conducted according to the intention-to-treat principle in all patients randomized with any efficacy data after randomization. Efficacy outcomes were analysed descriptively and treatment effects in the training only group were analysed by Wilcoxon rank sum test for change from baseline. Parameters measured at every exercise level (e.g. SO2, Borg’s scale) are reported descriptively until levels with n ≥ 5 in the respective group. Spearman’s rank sum correlation coefficients were calculated between changes in symptoms, parameters derived from treadmill exercise testing, and 2 km walking time as well as correlations between these parameters and training intensity. To identify mechanisms of exercise training, a confirmatory path analysis was conducted for the exercise training only group, based on the correlation matrix and on changes between baseline and eight weeks in efficacy endpoints. Because data did not support the a priori planned path model, exploratory modifications were modelled.
Next, group differences in treatment effects were explored by repeated measurements ANOVA, with significant interactions between treatment and visit indicating treatment differences. To identify mechanisms of WS 1442, necessary modifications of the path model in the group treated with WS 1442 were explored. Analyses were done with SAS version 9.2 (SAS Institute Inc., Cary, NC).
Finger plethysmography data were dominated by movement artefacts, especially at higher exercise levels. Therefore it was decided at blind data review to average data for exercise levels 1 to 3 and to calculate the difference to the average at level 0. Variance was still high and no training effects were detected. Therefore, parameters derived from the plethysmography signal were excluded from path analysis.
The 4 mmol/l lactic acid threshold was only reached by a minority of patients at baseline and after training and was therefore excluded from further analyses.
Descriptive safety analysis was done in all patients receiving treatment at least once.
2.2. Results
2.2.1. Patients and baseline data
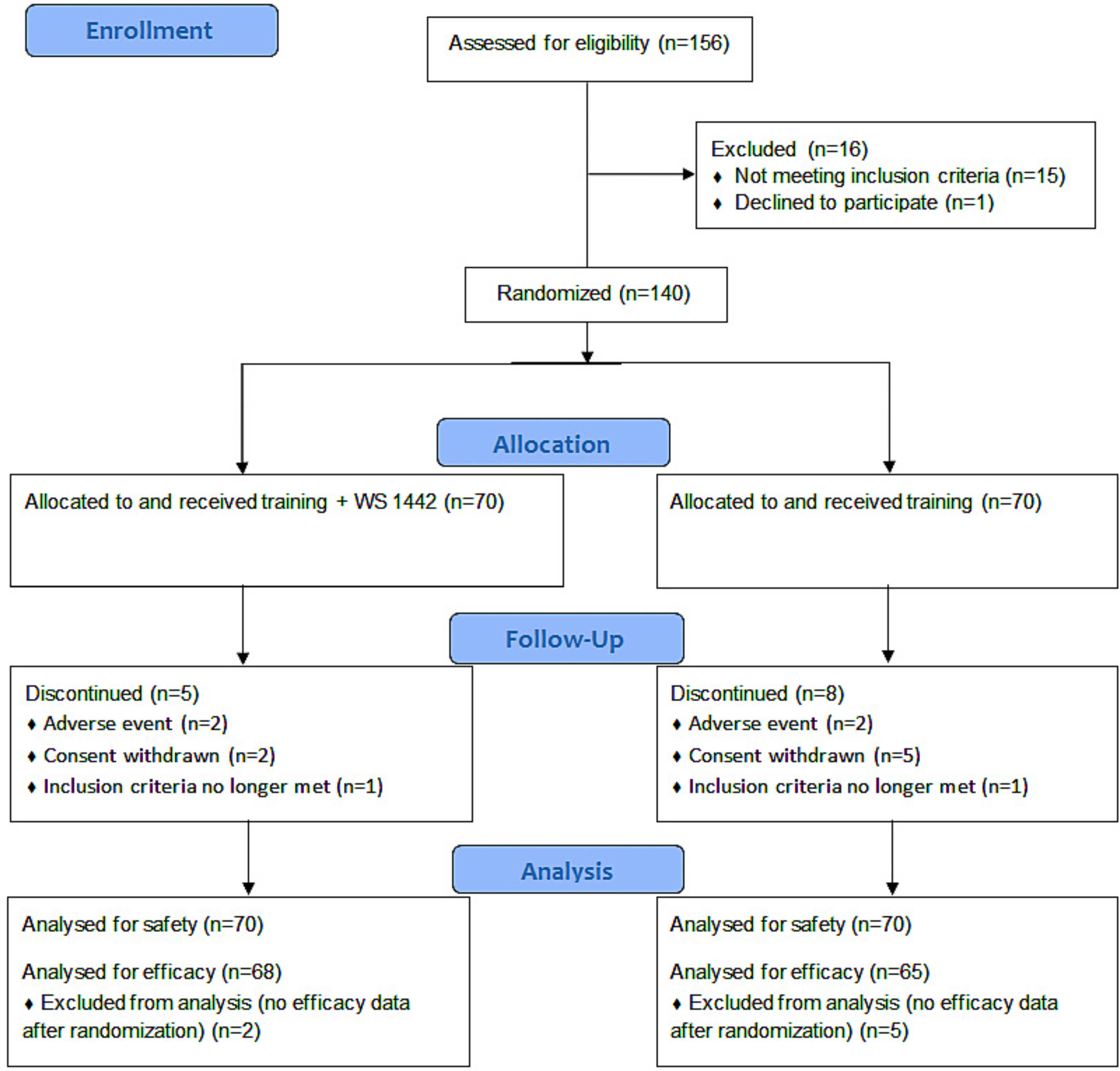
In total, 70 men and 70 women were randomized to study treatment between December 2009 and June 2011. For 7 patients (5 training and WS 1442, 2 training only) no efficacy data were available after randomization, therefore 133 patients were analysed for efficacy (Figure 1). Mean age was 62 years, 90% of patients suffered from arterial hypertension, 40% from ischemic heart disease, 27% had hypercholesterolemia, and 82% were overweight (Table 1). Nearly all patients received cardiovascular baseline medication. Two-thirds were on drugs inhibiting the renin-angiotensin-aldosterone system, about 61% received beta-adrenoceptor antagonists. Baseline symptoms were mild to moderate reflected by a KCCQ sum score of 76 out of 100. NT-proBNP (median 85 ng/l, interquartile range 46 - 170 ng/l) indicated well compensated cardiac status. Treatment groups did not differ significantly in demographics or disease characteristics.
Exercise capacity was moderately limited: Treadmill testing was terminated after 10.3 minutes, with a relative oxygen uptake of 22.0 mlO2/min*kg, a cardiac output of 14.5 l/min, and a muscular efficiency of 17.8 mlO2/min*W at severe subjective exertion (Borg scale 15.7). Individual lactate threshold was reached after 9.5 minutes and patients needed 22.2 minutes for the 2 km walking test (Table 2).
Calf muscle oxygenation showed an unexpected pattern: In some patients, oxygen saturation increased with increasing exercise intensity until termination due to exhaustion, in some it undulated, and in others it decreased (Figure 2).
2.2.2. Study treatment
Patient adherence to exercise training was high but somewhat lower in the group taking WS 1442: 89% of patients in the training only group participated in more than 10 sessions, 79% in the group combined with WS 1442. Mean times in the target heart rate corridor were 391 and 379 minutes. Medication compliance based on pill counting was > 97%.
2.2.3. Treatment effects in training only group
Symptoms and exercise capacity improved after eight weeks of exercise training. KCCQ scores improved significantly as well as exercise time, lactate threshold, muscular efficiency, subjective exertion at exercise level 3, physical activity and 2 km walking time (Table 2). Exercise time during treadmill testing, cardiac output and muscular efficiency at maximal exercise increased, while relative oxygen uptake at maximal exercise remained unchanged at 22.2 ml/min*kg. Subjective exertion at exercise level 5 (from 14.8 to 14.6, p=0.70) and at maximal exercise did not improve significantly.
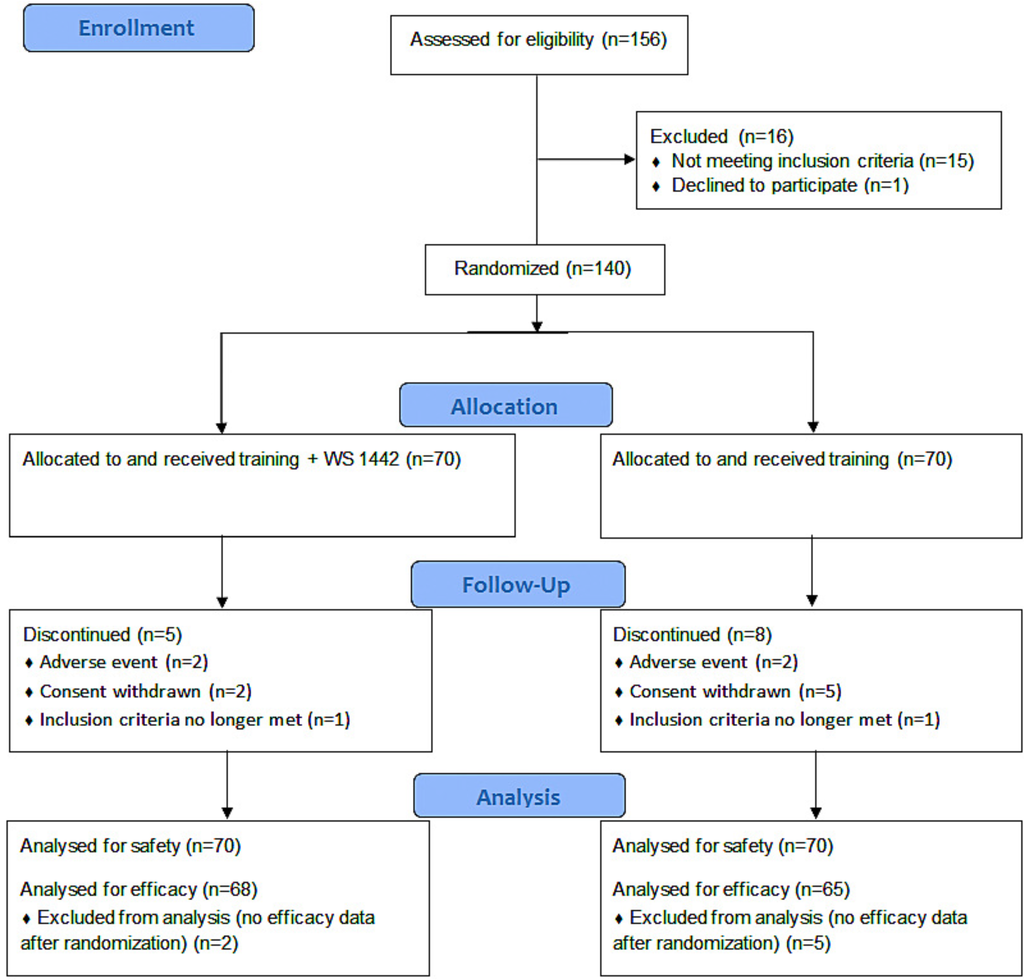
Figure 1.
Patient disposition.
Figure 1.
Patient disposition.
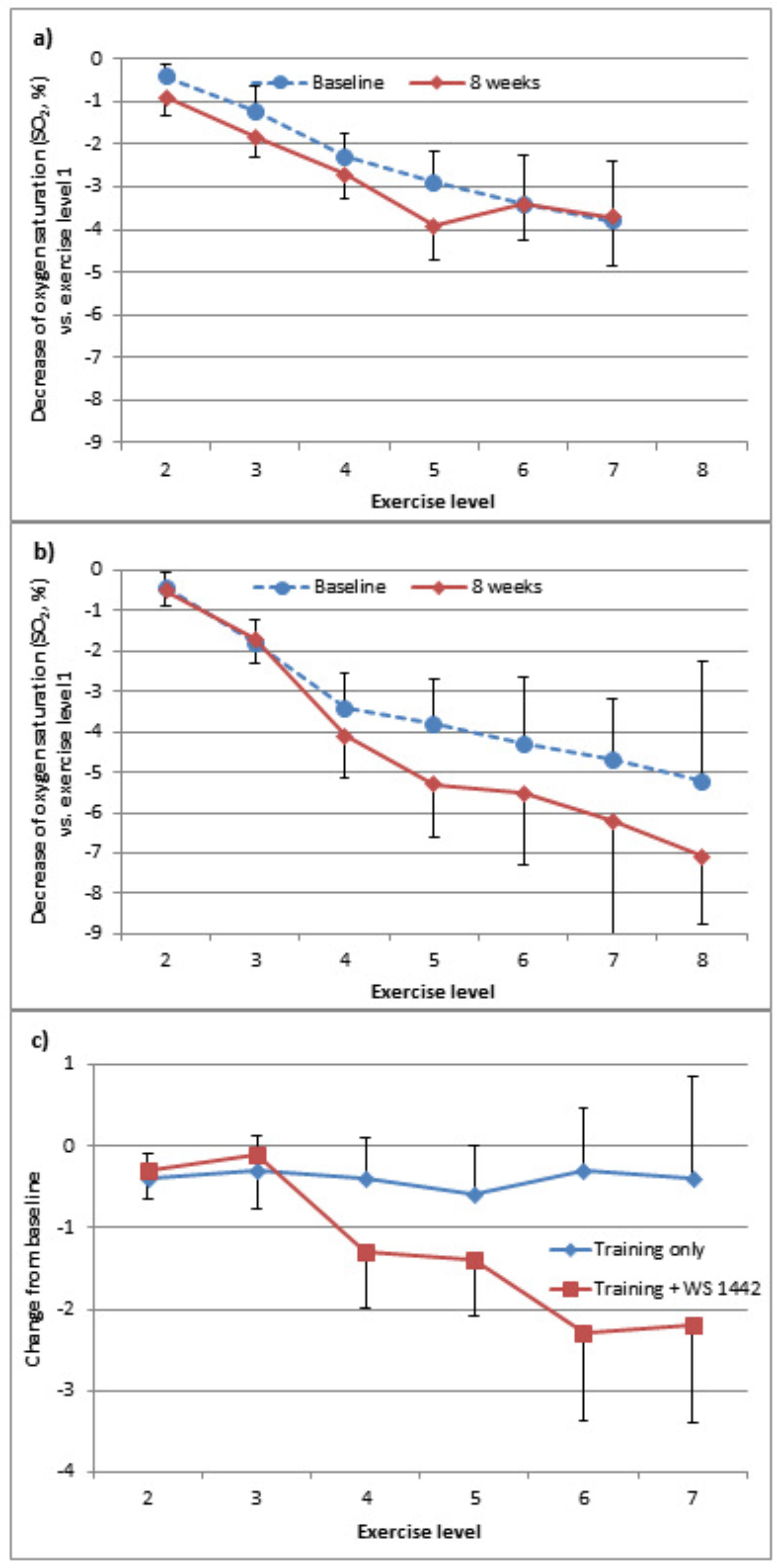
Decrease of skeletal muscle oxygen saturation from exercise level 1 to higher levels was hardly affected by training (Figure 3a). NT-proBNP increased minimally by 18 ng/l (p=0.07).
Correlations between changes in symptoms, parameters derived from treadmill exercise testing, and 2 km walking time were low as were correlations between these parameters and training intensity (Spearman’s rank correlation, nearly all rho < 0.4 and p > 0.05). In line with the low correlations, effects in both, planned and modified path models were generally very small and non-significant.

Table 1.
Study sample characteristics.
| percent of patients or mean value (± SD) | Treatment Group | |
|---|---|---|
| Training + WS 1442 (n=70) | Training (n=70) | |
| Age (years) | 62 ± 9.0 | 62 ± 7.8 |
| Cardiovascular disease/ risk factor | ||
| Hypertension | 91 % | 87 % |
| Ischemic heart disease | 43 % | 36 % |
| Mitral insufficiency | 11 % | 10 % |
| Hyperlipidaemia | 33 % | 33 % |
| Diabetes mellitus | 16 % | 9 % |
| Thyroid disorder | 17 % | 13 % |
| Smoking | 9 % | 9 % |
| Body mass index (kg/m2) | 30.2 ± 5.5 | 29.7 ± 4.7 |
| Concomitant medication | 99 % | 96 % |
| ACE-inhibitors, AT2-antagonists | 69 % | 64 % |
| Beta blockers | 64 % | 57 % |
| Platelet aggregation inhibitors, coumarines | 64 % | 49 % |
| Lipid lowering drugs | 61 % | 56 % |
| Calcium-antagonists | 27 % | 21 % |
| Anti-diabetics | 20 % | 11 % |
| Nitrates, vasodilating drugs, other cardiacs | 19 % | 11 % |
| Diuretics | 17 % | 10 % |
| Thyroid therapeutics | 23 % | 14 % |
2.2.4. Effects of WS 1442
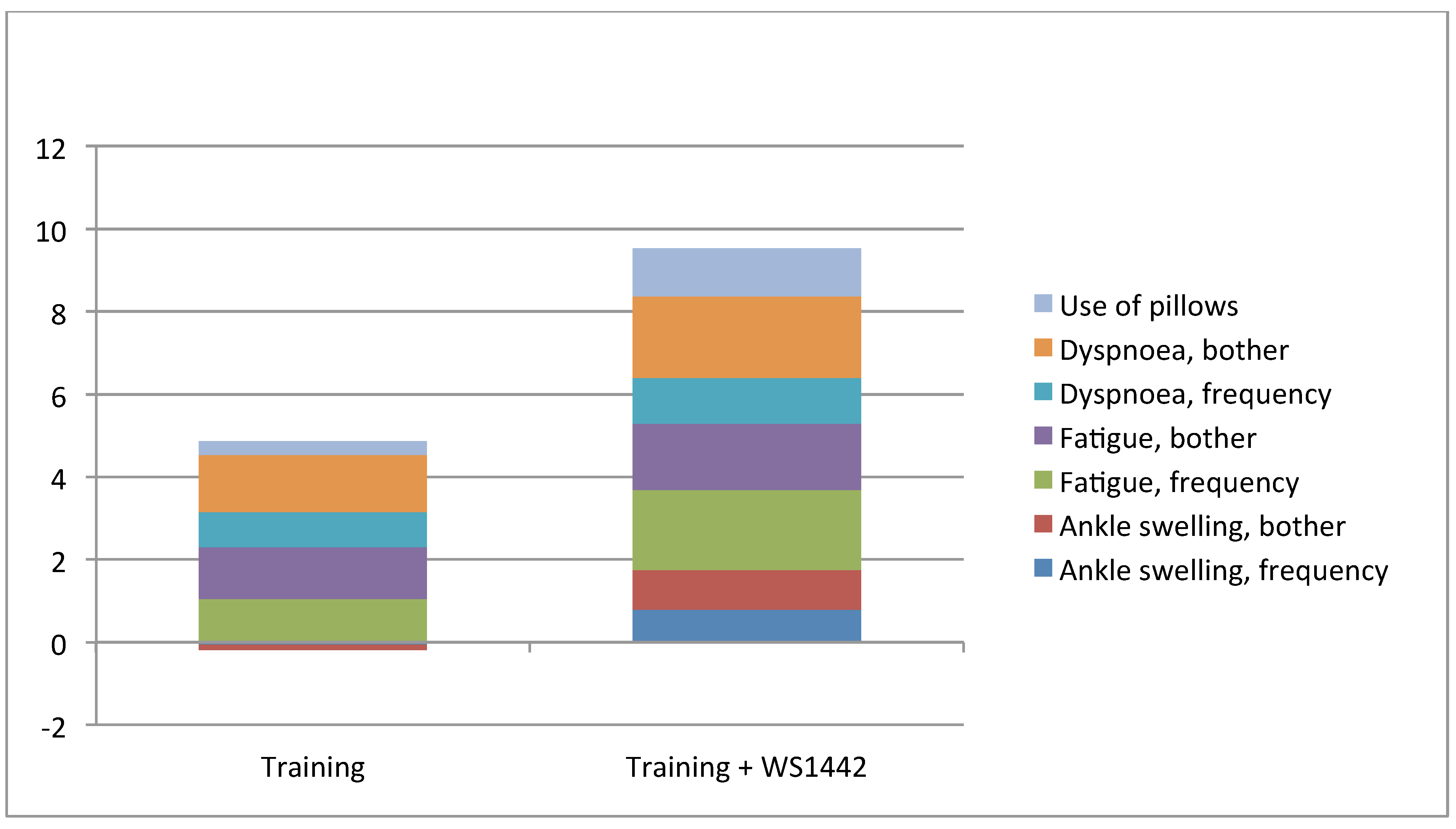
Absolute improvements of symptoms and quality of life tended to be larger with training and WS 1442 compared to training alone (Table 2). The most pronounced difference was in the KCCQ-subscore “Symptoms”, mainly based on improvements in dyspnoea and fatigue (Figure 4).

Table 2.
Effects of 8 weeks treatment on symptoms and exercise capacity.
| Treatment | |||||
|---|---|---|---|---|---|
| Training only | Training + WS 1442 | ||||
| Baseline | Change | Baseline | Change | ||
| KCCQ | |||||
| Physical limitation | 85 ± 17 | 4 ± 15* | 82 ± 17 | 6 ± 15 | |
| Symptom stability | 57 ± 29 | 9 ± 35 | 60 ± 29 | 3 ± 29 | |
| Symptoms | 76 ± 18 | 5 ± 14* | 70 ± 22 | 10 ± 17 | |
| Self-efficacy | 70 ± 21 | 2 ± 17 | 70 ± 20 | 3 ± 15 | |
| Social limitation | 79 ± 23 | 5 ± 16* | 76 ± 25 | 9 ± 20 | |
| Quality of life | 71 ± 24 | 9 ± 17* | 69 ± 23 | 11 ± 18 | |
| Exercise capacity | |||||
| Freiburg Questionnaire of Physical Activity | 27 ± 23 | 14 ± 27* | 27 ± 26 | 14 ± 29 | |
| Time for 2 km walking test (min) | 21.4 ± 2.4 | -1.9 ± 2.0* | 23.0 ± 3.1 | -2.9 ± 2.4† | |
| Treadmill test, time to termination (min) | 11.1 ± 3.0 | 1.3 ± 2.0* | 9.6 ± 3.7 | 1.3 ± 2.7 | |
| Treadmill test, maximum exercise | |||||
| relative O2 uptake (ml/min/kg) | 22.2 ± 4.2 | 0.0 ± 2.5 | 21.9 ± 4.6 | -0.2 ± 2.8 | |
| cardiac output (l/min) | 14.5 ± 3.6 | 0.8 ± 2.4* | 14.4 ± 3.8 | 0.5 ± 2.7 | |
| muscular efficiency (mlO2/W) | 16.9 ± 4.3 | -1.4 ± 4.1* | 18.6 ± 5.4 | -0.8 ± 4.7 | |
| Borg subjective exertion scale | 15.7 ± 2.0 | -0.1 ± 1.7 | 15.5 ± 2.1 | -0.6 ± 2.0 | |
| Time to lactate threshold (min) | 6.8 ± 2.4 | 0.9 ± 2.2* | 5.4 ± 2.8 | 1.1 ± 2.2 | |
* p<0.05, Wilcoxon rank sum test for change from baseline in training only group † p=0.019, repeated measurements ANOVA, interaction visit*treatment in total sample
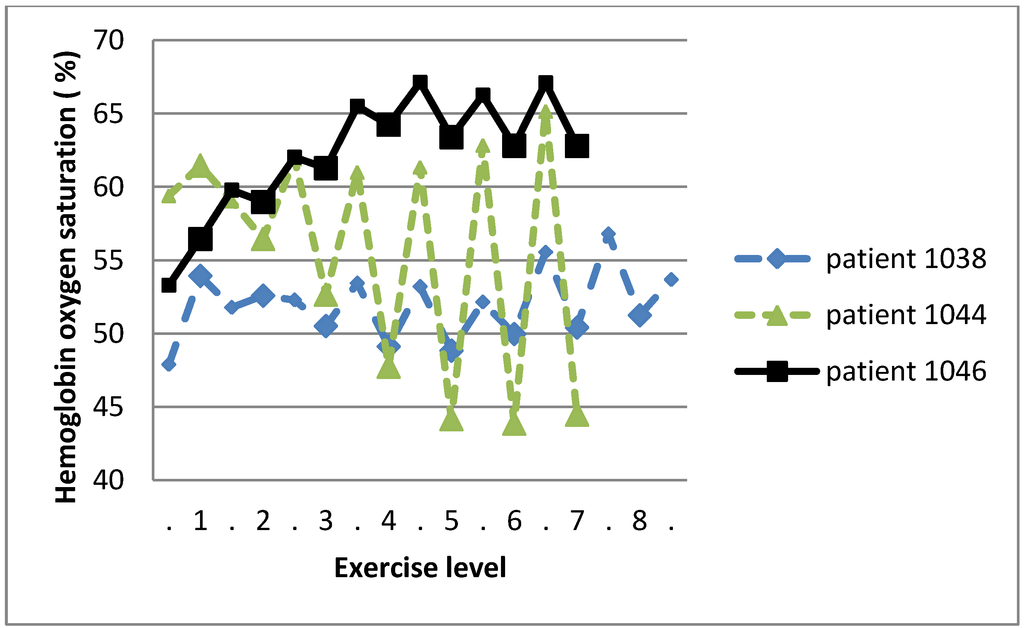
Figure 2.
Haemoglobin oxygen saturation in calf muscle was measured by NIRS during treadmill exercise. The exercise protocol comprised two-minute bouts of increasing intensity (large symbols) and 30 seconds rests between bouts (small symbols). Baseline data from three exemplary patients are displayed.
Figure 2.
Haemoglobin oxygen saturation in calf muscle was measured by NIRS during treadmill exercise. The exercise protocol comprised two-minute bouts of increasing intensity (large symbols) and 30 seconds rests between bouts (small symbols). Baseline data from three exemplary patients are displayed.
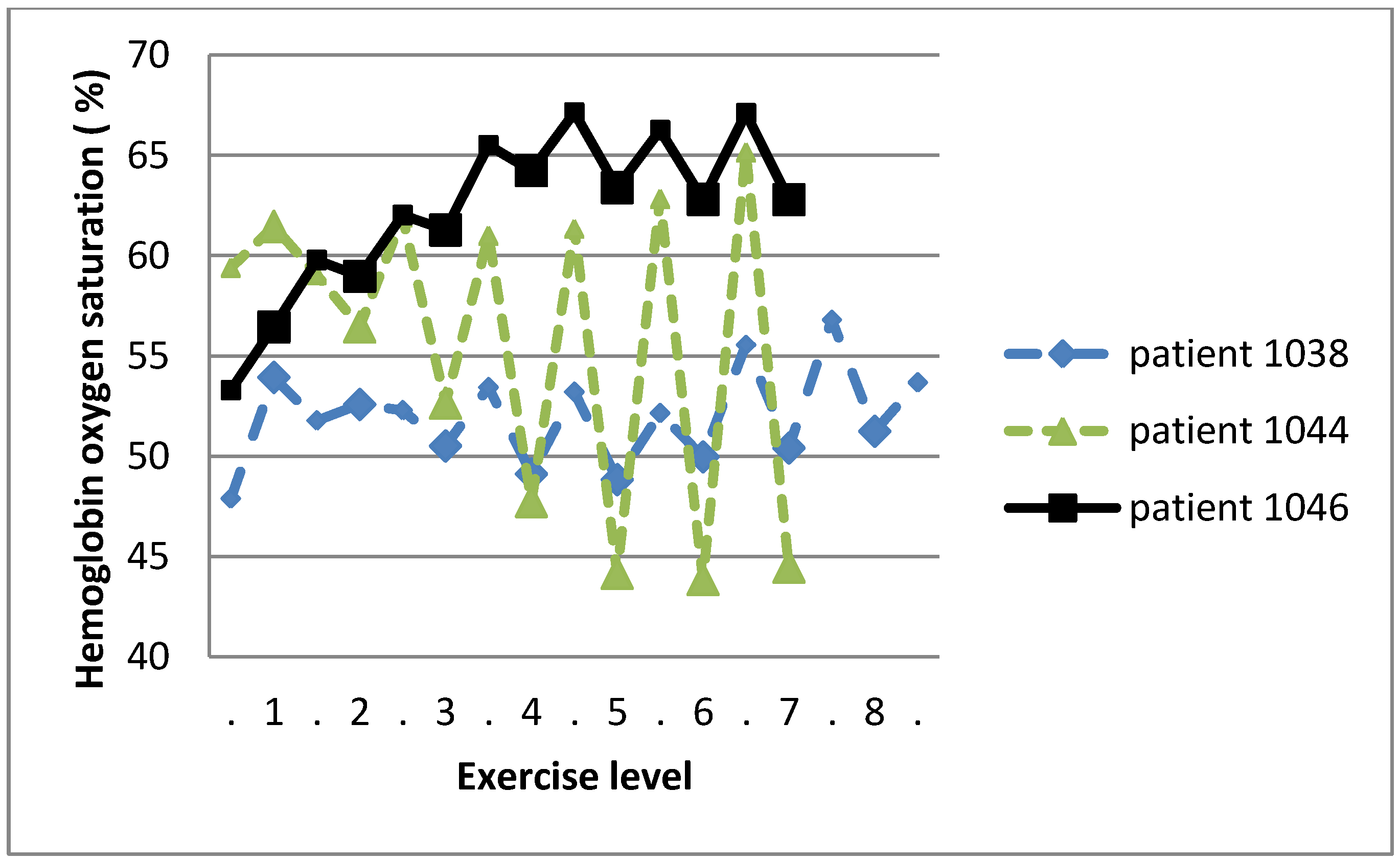
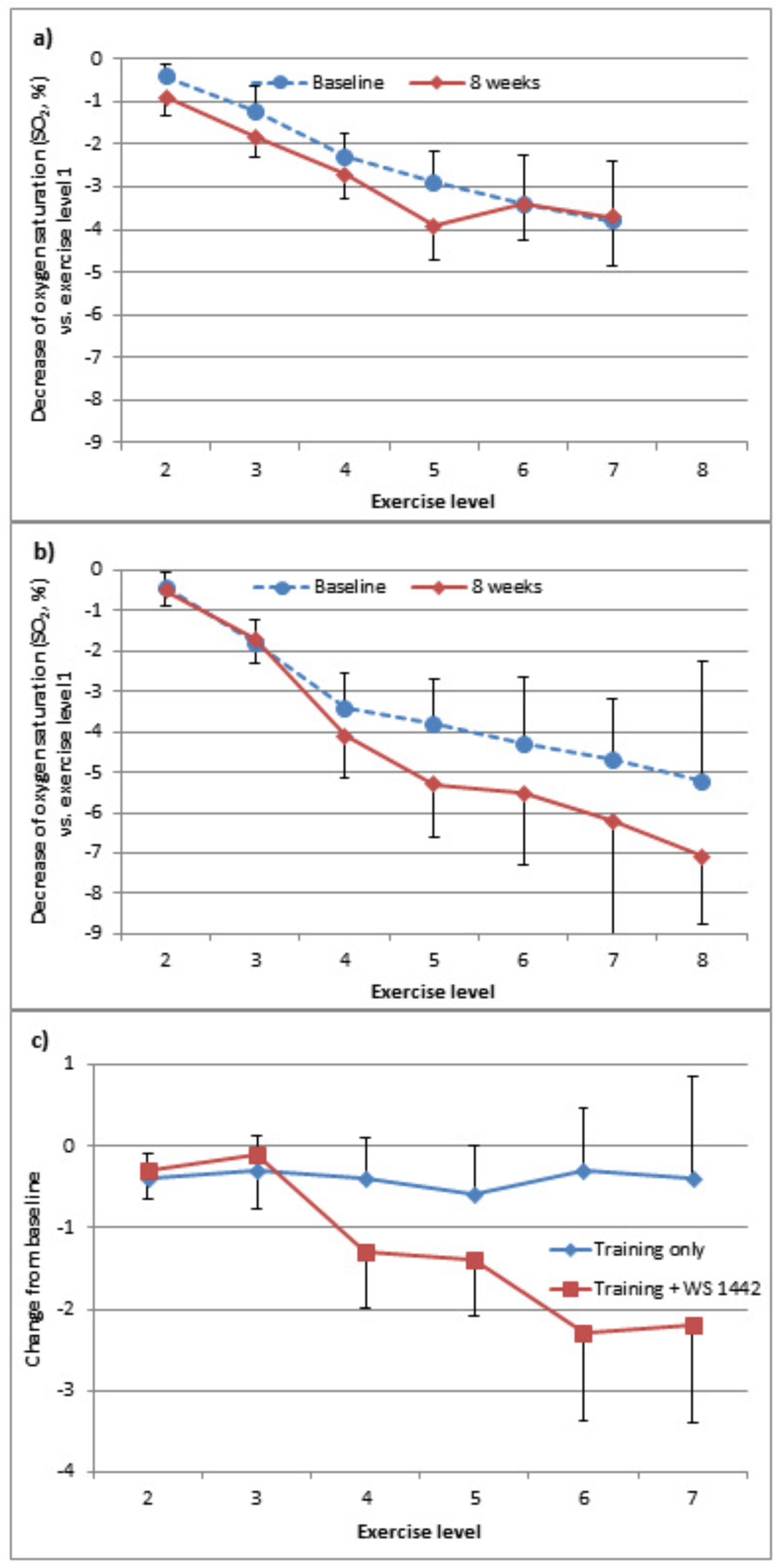
Figure 3.
(a) Effects of interventions on calf muscle oxygenation with increasing exercise. Haemoglobin oxygen saturation (%) in calf muscle was measured by NIRS during treadmill exercise with increasing intensity levels at baseline and after eight weeks of treatment. Absolute decrease of oxygen saturation versus exercise level 1 was calculated for every patient and averaged for the training only group (mean ± SEM). (b) The same data are shown for the group receiving training plus WS 1442. (c) For every patient, the change from baseline in the decrease of oxygen saturation vs. exercise level 1 was calculated for every exercise level. Data were averaged for both groups (mean ± SEM).
Figure 3.
(a) Effects of interventions on calf muscle oxygenation with increasing exercise. Haemoglobin oxygen saturation (%) in calf muscle was measured by NIRS during treadmill exercise with increasing intensity levels at baseline and after eight weeks of treatment. Absolute decrease of oxygen saturation versus exercise level 1 was calculated for every patient and averaged for the training only group (mean ± SEM). (b) The same data are shown for the group receiving training plus WS 1442. (c) For every patient, the change from baseline in the decrease of oxygen saturation vs. exercise level 1 was calculated for every exercise level. Data were averaged for both groups (mean ± SEM).
Mean time required to walk 2 km was significantly reduced by additional intake of WS 1442: It decreased from to 21 to 20 minutes in the training group (-8.4%), and from 23 to 20 minutes in patients taking WS 1442 (-12.7%, p = 0.019 for group difference).
Parameters measured during treadmill exercise improved by a comparable extent in both treatment groups. Subjective exertion ratings tended to improve more with WS 1442 at higher exercise levels (Figure 5).
Decrease of skeletal muscle oxygen saturation from exercise level 1 to higher levels tended to be more pronounced after WS 1442 and training compared to training alone (Figure 3b and c).
Correlations of changes during treatment and effects in path models were generally small and non-significant in the total sample.
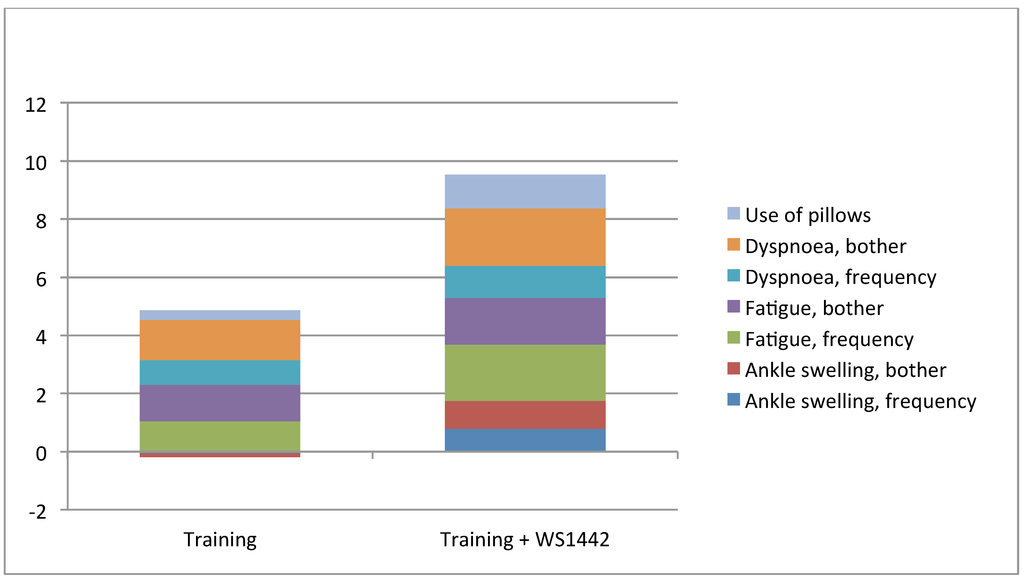
Figure 4.
Absolute change of KCCQ-rated items from the subscore “Symptoms” during eight weeks of treatment.
Figure 4.
Absolute change of KCCQ-rated items from the subscore “Symptoms” during eight weeks of treatment.
2.2.5. Tolerability and Safety
Professionally supervised exercise training for eight weeks was generally safe. The most frequently reported adverse events were related to the musculo-skeletal system and injuries, but none was serious.
Frequency of adverse events was not higher under WS 1442 treatment (13% of patients) than without (17%, Table 3). One serious adverse event (bacterial urogenital infection) occurred; it was considered unrelated to WS 1442 by the investigator. Events probably or possibly related to WS 1442 or drug interactions were not reported throughout the trial.
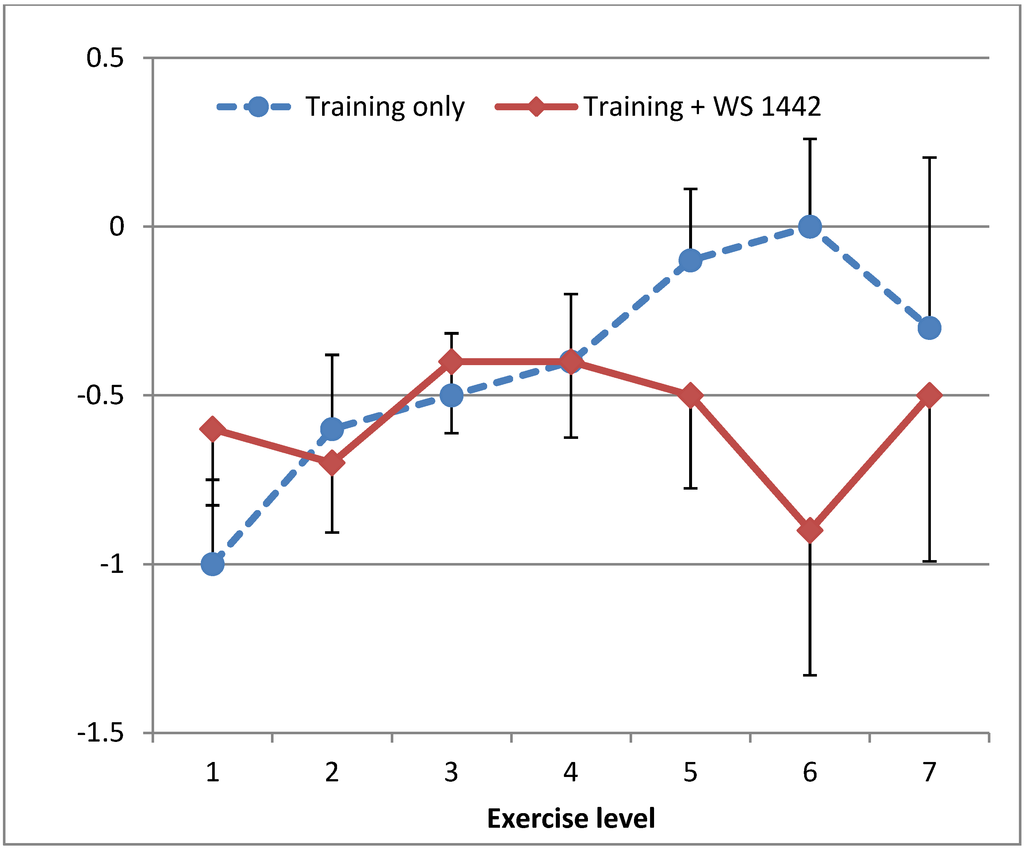
Figure 5.
Decrease of patient rated subjective exertion on Borg’s scale during treadmill exercise with increasing intensity levels from baseline to after eight weeks of treatment (mean ± SEM).
Figure 5.
Decrease of patient rated subjective exertion on Borg’s scale during treadmill exercise with increasing intensity levels from baseline to after eight weeks of treatment (mean ± SEM).
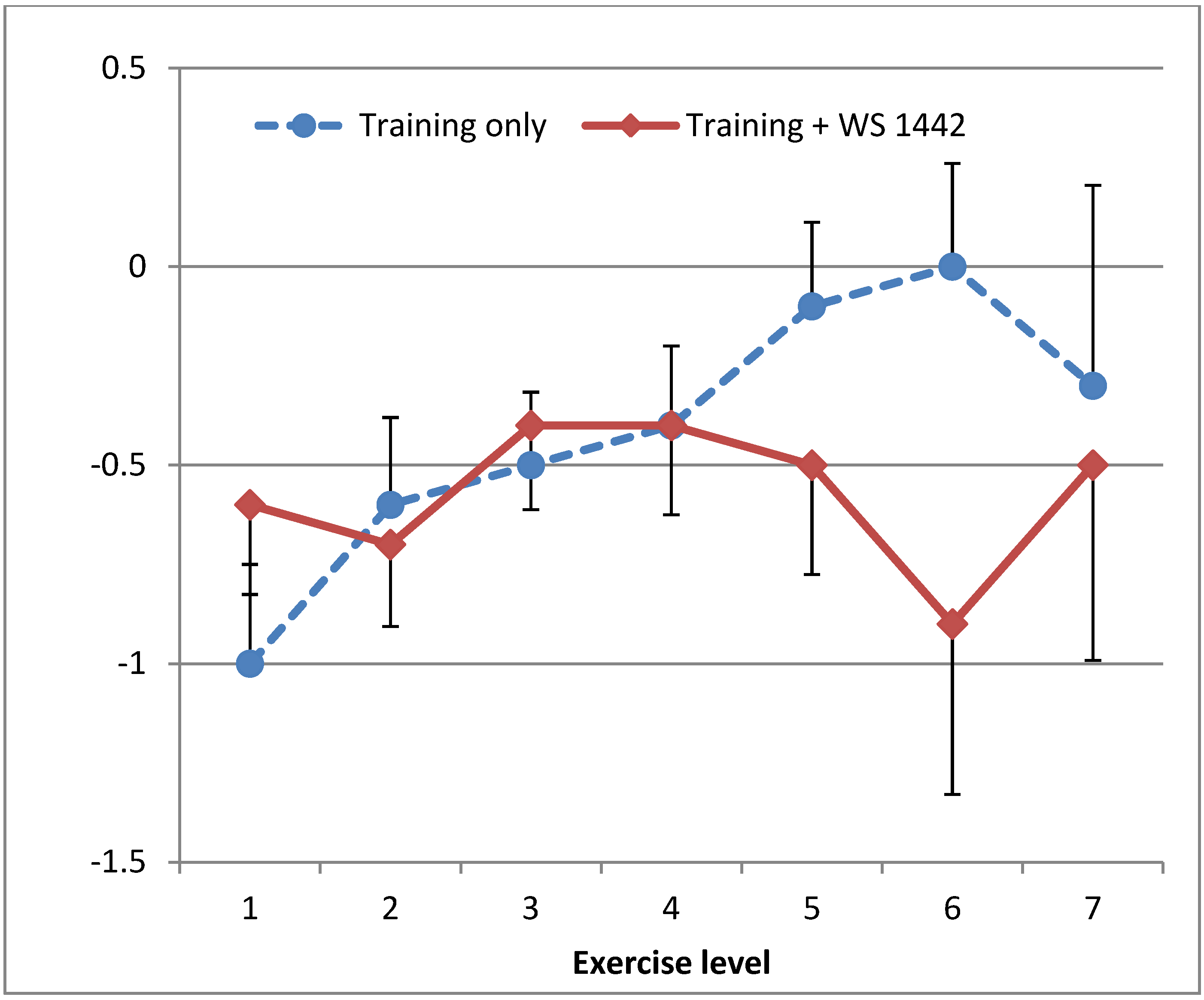

Table 3.
Safety and tolerability.
| percent of patients | Treatment Group | |
|---|---|---|
| Training + WS 1442 (n=70) | Training (n=70) | |
| Adverse events | ||
| total | 13 % | 17 % |
| musculoskeletal and injuries | 7 % | 7 % |
| infections | 6 % | 7 % |
| cardiac | 0 % | 1 % |
| gastrointestinal | 0 % | 1 % |
| psychiatric | 0 % | 1 % |
| serious | 1 % | 0 % |
| fatal | 0 % | 0 % |
| causal relationship to drug likely or possible | 0 % | |
2.3. Discussion
2.3.1. Training effects
Our sample of sedentary patients with HFpEF, already treated according to current guidelines, significantly benefitted in symptoms and quality of life from endurance exercise training. Patients reached a score of 80 to 90 out of 100 in important KCCQ subscales indicating only minimal remaining symptoms. This observation is in line with previous reports and supports the recommendation of endurance exercise training in diastolic heart failure [32,33,34]. Professionally supervised training was generally safe. However, seven per cent of patients experienced non-serious musculo-skeletal events or injuries, highlighting the need of professional supervision to prevent more frequent or serious complications.
Surprisingly, improvements in symptoms, 2 km walking time, and parameters derived from the treadmill protocol were not correlated. Our interpretation is that parameters of exercise capacity developed in healthy trained populations, such as lactate thresholds, are not adequate to describe limitations in everyday physical activities and symptoms in sedentary heart failure patients. Limitations of everyday physical activity probably result from a heterogeneous array of factors beyond cardiovascular markers [35,36]. Therefore we were not able to better describe the modes of action of exercise training by the technologies and analyses employed. Anecdotal reports from the training groups in our study indicated that social interaction, psychological factors and getting used to physical activity are important moderators of symptomatic improvement.
2.3.2. Effects of WS 1442
Efficacy of WS 1442 for symptomatic treatment of heart failure NYHA II has been demonstrated in a number of placebo-controlled trials [9,10]. As our patients already reached a score of 80 to 90 out of 100 in important KCCQ subscales with training only, there was little room for further improvement with WS 1442 and our trial was underpowered to statistically prove the additional symptomatic benefit we observed. In a measure of everyday physical activity that did not have such a ceiling effect, the 2 km walking test, a significant benefit could be demonstrated. The Freiburg questionnaire only reflected the increase in physical activity by participation in the training, and therefore demonstrated no group difference. The exercise protocol was terminated at the pre-specified maximal heart rate in the majority of cases, not for exhaustion. This stopping criterion was not changed during the trial. Therefore improvements in treadmill exercise parameters were moderate without group differences. A trend of less subjective exertion with WS 1442 might indicate that exercise until subjective exhaustion shows a group difference. Finger plethysmography was dominated by movement artefacts preventing meaningful analysis of cardiac and vascular function. More stable and validated techniques should be used in future clinical trials on WS 1442 modes of action.
Adding WS 1442 to standard cardiological drug treatment was safe, no interactions were reported. This is in line with experience during the SPICE trial [37]. In this largest trial ever conducted with crataegus extract, adding WS 1442 to optimal drug treatment in patients with heart failure NYHA II or III and LVEF ≤35% was safe [38].
2.3.3. Skeletal muscle oxygenation
The pattern of skeletal muscle oxygen saturation with increasing exercise in our sample of sedentary treated patients with heart failure was significantly different from the steady decrease that has been reported in healthy trained untreated subjects [39,40]. The observation that a considerable proportion of patients can increase skeletal muscle oxygen saturation with increasing exercise and terminates exercise at high muscle oxygen saturation indicates that oxygen supply to the muscle is not limiting exercise capacity in these patients. Oxygen utilization might be a limiting factor [41]. In line with this observation, a loss of oxidative type-1 muscle fibres and a reduction of capillary to fibre ratio have been reported in HFpEF patients [42,43]. Moreover, in our sample heterogeneity of oxygen saturation patterns with increasing exercise was considerable. Deficits in oxygen supply and oxygen utilization might contribute differentially in individual patients to the limitation in exercise capacity. Therefore, individual patients might respond differentially to treatment strategies. NIRS provides a non-invasive tool to guide treatment strategies in treated patients with HFpEF still suffering from limitations in exercise capacity. We observed that training plus WS 1442 pronounced the average decrease of oxygen saturation with increasing exercise while training alone had no effect on this parameter. Assuming that blood flow to the muscle has not been reduced by training and WS 1442, decrease of oxygen saturation with increasing exercise is an indicator of oxygen utilization. Chronic intake of WS 1442 has been reported to increase skeletal muscle mitochondrial density and to induce a shift towards oxidative type-1 fibres [21]. Therefore we postulate that WS 1442 might improve oxygen utilization in the skeletal muscle.
2.3.4. Limitations
All patients in our trial received exercise training. Therefore we cannot quantify to what extent the observed improvements are due to training or are unspecific (e.g. Hawthorne effect). However, efficacy of exercise training in diastolic heart failure has been reported in controlled trials [32,33,34], and changes in untrained individuals are small. Therefore it is unlikely that the considerable effects we observed are unspecific in nature.
Our control group did not receive placebo because our main interest was the correlation between changes to explore underlying mechanisms, not absolute group differences. While treatments applied in our trial correspond to the setting in routine clinical practice, we cannot exclude that non-specific effects have contributed to the observed group differences. However, the efficacy of WS 1442 has been demonstrated in previous placebo-controlled trials [9,10].
Our trial was not powered to prove treatment effects of WS 1442 and hence is prone to type-II error, i.e. the sample was too small for the observed treatment differences to reach statistical significance. For example, improvements in all but one KCCQ-subscores were larger with WS 1442 than with training alone, for the subscore “symptoms” mean effect was twice as big. Therefore we were not able to finally prove or disprove treatment differences.
We were not able to clarify the mechanisms underlying the clinical benefit of training and WS 1442 with the applied technologies and analyses. Future clinical trials on the mode of action should apply better established and more stable measures of vascular and cardiac function.
4. Conclusion
Treated sedentary patients with heart failure with preserved ejection fraction benefit in symptoms and quality of life from endurance exercise training. Professionally supervised training is safe in this population. WS 1442 tended to further improve symptoms and everyday exercise capacity. This extract can be safely combined with standard drug treatment of heart failure.
Acknowledgments
The trial was financed by Dr. Willmar Schwabe GmbH & Co. KG, Karlsruhe, Germany, manufacturer of WS 1442.
Author Contributions
SH, MB, MK-B and KB designed the trial, SH, CK, EW and MK-B conducted the trial, SH, ML, MK-B, UE-B and KB analysed and interpreted the data, MB wrote the manuscript, all authors critically reviewed, contributed to and approved the manuscript.
Conflicts of Interest
MB is employee of the sponsor, all other authors received investigator honoraria for their contribution to the trial.
References
- Haq, M.A.; Wong, C.; Mutha, V.; Anavekar, N.; Lim, K.; Barlis, P.; Hare, D.L. Therapeutic interventions for heart failure with preserved ejection fraction: A summary of current evidence. World J. Cardiol. 2014, 6, 67–76. [Google Scholar] [PubMed]
- Paulus, W.J.; Tschope, C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J. Am. Coll. Cardiol. 2013, 62, 263–271. [Google Scholar] [PubMed]
- Shibata, K.; Shimokawa, H.; Yanagihara, N.; Otsuji, Y.; Tsutsui, M. Nitric oxide synthases and heart failure - lessons from genetically manipulated mice. J. UOEH. 2013, 35, 147–158. [Google Scholar] [CrossRef] [PubMed]
- Zouein, F.A.; de Castro Bras, L.E.; da Costa, D.V.; Lindsey, M.L.; Kurdi, M.; Booz, G.W. Heart failure with preserved ejection fraction: emerging drug strategies. J. Cardiovasc. Pharmacol. 2013, 62, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Marti, C.N.; Gheorghiade, M.; Kalogeropoulos, A.P.; Georgiopoulou, V.V.; Quyyumi, A.A.; Butler, J. Endothelial dysfunction, arterial stiffness, and heart failure. J. Am. Coll. Cardiol. 2012, 60, 1455–1469. [Google Scholar] [CrossRef] [PubMed]
- Borlaug, B.A. Mechanisms of exercise intolerance in heart failure with preserved ejection fraction. Circ. J. 2013, 78, 20–32. [Google Scholar] [PubMed]
- Bundesärztekammer (BÄK); Kassenärztliche Bundesvereinigung (KBV); Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF). Nationale VersorgungsLeitlinie Chronische Herzinsuffizienz – Langfassung, 1. Auflage Version 7 Dezember 2009, zuletzt geändert: August 2013. 2013. [Google Scholar]
- McMurray, J.J.; Adamopoulos, S.; Anker, S.D.; Auricchio, A.; Bohm, M.; Dickstein, K.; Falk, V.; Filippatos, G.; Fonseca, C.; Gomez-Sanchez, M.A.; Jaarsma, T.; Kober, L.; Lip, G.Y.; Maggioni, A.P.; Parkhomenko, A.; Pieske, B.M.; Popescu, B.A.; Ronnevik, P.K.; Rutten, F.H.; Schwitter, J.; Seferovic, P.; Stepinska, J.; Trindade, P.T.; Voors, A.A.; Zannad, F.; Zeiher, A. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2012, 33, 1787–1847. [Google Scholar]
- Pittler, M.H.; Guo, R.; Ernst, E. Hawthorn extract for treating chronic heart failure. Cochrane. Database. Syst. Rev. 2008, CD005312. [Google Scholar]
- Eggeling, T.; Regitz-Zagrosek, V.; Zimmermann, A.; Burkart, M. Baseline severity but not gender modulates quantified Crataegus extract effects in early heart failure--a pooled analysis of clinical trials. Phytomedicine. 2011, 18, 1214–1219. [Google Scholar] [CrossRef] [PubMed]
- Peters, W.; Drueppel, V.; Kusche-Vihrog, K.; Schubert, C.; Oberleithner, H. Nanomechanics and sodium permeability of endothelial surface layer modulated by hawthorn extract WS 1442. PLoS. One. 2012, 7, e29972. [Google Scholar] [CrossRef] [PubMed]
- Anselm, E.; Socorro, V.F.; Dal-Ros, S.; Schott, C.; Bronner, C.; Schini-Kerth, V.B. Crataegus special extract WS 1442 causes endothelium-dependent relaxation via a redox-sensitive Src- and Akt-dependent activation of endothelial NO synthase but not via activation of estrogen receptors. J. Cardiovasc. Pharmacol. 2009, 53, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Brixius, K.; Willms, S.; Napp, A.; Tossios, P.; Ladage, D.; Bloch, W.; Mehlhorn, U.; Schwinger, R.H. Crataegus special extract WS 1442 induces an endothelium-dependent, NO-mediated vasorelaxation via eNOS-phosphorylation at serine 1177. Cardiovasc. Drugs Ther. 2006, 20, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Rieckeheer, E.; Schwinger, R.H.; Bloch, W.; Brixius, K. Hawthorn special extract WS(R) 1442 increases red blood cell NO-formation without altering red blood cell deformability. Phytomedicine. 2011, 19, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Idris-Khodja, N.; Auger, C.; Koch, E.; Schini-Kerth, V.B. Crataegus special extract WS((R))1442 prevents aging-related endothelial dysfunction. Phytomedicine. 2012, 19, 699–706. [Google Scholar] [CrossRef] [PubMed]
- Schini-Kerth, V.B. The standardized Crataegus extract WS® 1442 prevents systolic hypertension in the DOCA-salt hypertensive rat: Beneficial effects on target organs (blood vessels, heart and kidney). Personal communication, 2013. [Google Scholar]
- Schwinger, R.H.; Pietsch, M.; Frank, K.; Brixius, K. Crataegus special extract WS 1442 increases force of contraction in human myocardium cAMP-independently. J. Cardiovasc. Pharmacol. 2000, 35, 700–707. [Google Scholar] [CrossRef] [PubMed]
- Hwang, H.S.; Bleske, B.E.; Ghannam, M.M.; Converso, K.; Russell, M.W.; Hunter, J.C.; Boluyt, M.O. Effects of hawthorn on cardiac remodeling and left ventricular dysfunction after 1 month of pressure overload-induced cardiac hypertrophy in rats. Cardiovasc. Drugs Ther. 2008, 22, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Hwang, H.S.; Boluyt, M.O.; Converso, K.; Russell, M.W.; Bleske, B.E. Effects of hawthorn on the progression of heart failure in a rat model of aortic constriction. Pharmacotherapy 2009, 29, 639–648. [Google Scholar] [CrossRef] [PubMed]
- Koch, E.; Spörl-Aich, G. Oral treatment with the Crataegus special extract WS(R) 1442 inhibits cardiac hypertrophy in rats with DOCA-salt or aortic banding induced hypertension. Planta Medica 2006, 72, 12–15. [Google Scholar]
- Chen, J.; Brixius, K.; Burkart, M.; Regitz-Zagrosek, V.; Schubert, C. Influence of Crataegus Extract WS1442® on Age-related Alterations in Skeletal Muscle. In Presented at the 78th Annual Meeting of the German Cardiac Society, Mannheim, Germany, 12-4-2012; p. P696.
- Faller, H.; Steinbuchel, T.; Schowalter, M.; Spertus, J.A.; Stork, S.; Angermann, C.E. The Kansas City Cardiomyopathy Questionnaire (KCCQ) -- a new disease-specific quality of life measure for patients with chronic heart failure. Psychother. Psychosom. Med. Psychol. 2005, 55, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Green, C.P.; Porter, C.B.; Bresnahan, D.R.; Spertus, J.A. Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure. J. Am. Coll. Cardiol. 2000, 35, 1245–1255. [Google Scholar] [PubMed]
- Frey, I.; Berg, A.; Grathwohl, D.; Keul, J. Freiburg Questionnaire of physical activity--development, evaluation and application. Soz. Praventivmed. 1999, 44, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Bös, K. Der 2-km-Walking-Test. Alters- und geschlechtsspezifische Normwerte. Gesundheitssport und Sporttherapie 2003, 19, 201–207. [Google Scholar]
- Röcker, K.; Schotte, O.; Niess, A.M.; Horstmann, T.; Huth, H.H. Predicting competition performance in long-distance running by means of a treadmill test. Medicine and Science in Sports and Exercise 1998, 30, 1552–1557. [Google Scholar] [CrossRef] [PubMed]
- Borg, G. Anstrengungsempfinden und körperliche Aktivität. Dtsch. Ärztblatt 2004, 1001, A1016–A1021. [Google Scholar]
- Schardt, F. W. Kardiopulmonale Leistungsdiagnostik, 1st ed.; MKM Marketinginstitut GmbH: Lenggries, Germany, 2005. [Google Scholar]
- Kroidl, F.R.; Schwarz, S.; Lehnigk, B. Kursbuch Spiroergometrie: Technik und Befundung verständlich gemacht; Stuttgart, Germany, 2007. [Google Scholar]
- Westphal, E.; Bös, K. Lebensqualität von Herzinsuffizienz-Patienten beim moderaten Ausdauertraining unter Crataegus-Spezialextrakt WS® 1442. Der Hausarzt 2008, Supp1/08. [Google Scholar]
- Kline, R.B. Principles and practice of structural equation modeling; Guildford Press: New York, 1998. [Google Scholar]
- Gasiorowski, A.; Dutkiewicz, J. Comprehensive rehabilitation in chronic heart failure. Ann. Agric. Environ. Med. 2013, 20, 606–612. [Google Scholar] [PubMed]
- Kitzman, D.W.; Brubaker, P.H.; Herrington, D.M.; Morgan, T.M.; Stewart, K.P.; Hundley, W.G.; Abdelhamed, A.; Haykowsky, M.J. Effect of endurance exercise training on endothelial function and arterial stiffness in older patients with heart failure and preserved ejection fraction: a randomized, controlled, single-blind trial. J. Am. Coll. Cardiol. 2013, 62, 584–592. [Google Scholar] [CrossRef] [PubMed]
- Nolte, K.; Herrmann-Lingen, C.; Wachter, R.; Gelbrich, G.; Dungen, H.D.; Duvinage, A.; Hoischen, N.; von Oehsen, K.; Schwarz, S.; Hasenfuss, G.; Halle, M.; Pieske, B.; Edelmann, F. Effects of exercise training on different quality of life dimensions in heart failure with preserved ejection fraction: the Ex-DHF-P trial. Eur. J. Prev. Cardiol. 2014. Epub ahead of print. [Google Scholar]
- Kitzman, D.W.; Upadhya, B. Heart failure with preserved ejection fraction: a heterogenous disorder with multifactorial pathophysiology. J. Am. Coll. Cardiol. 2014, 63, 457–459. [Google Scholar] [CrossRef] [PubMed]
- Edelmann, F.; Gelbrich, G.; Duvinage, A.; Stahrenberg, R.; Behrens, A.; Prettin, C.; Kraigher-Krainer, E.; Schmidt, A.G.; Dungen, H.D.; Kamke, W.; Tschope, C.; Herrmann-Lingen, C.; Halle, M.; Hasenfuss, G.; Wachter, R.; Pieske, B. Differential interaction of clinical characteristics with key functional parameters in heart failure with preserved ejection fraction - results of the Aldo-DHF trial. Int. J. Cardiol. 2013, 169, 408–417. [Google Scholar] [CrossRef] [PubMed]
- Holubarsch, C.J.; Colucci, W.S.; Meinertz, T.; Gaus, W.; Tendera, M. The efficacy and safety of Crataegus extract WS 1442 in patients with heart failure: the SPICE trial. Eur. J. Heart Fail. 2008, 10, 1255–1263. [Google Scholar] [CrossRef] [PubMed]
- Holubarsch, C.J.F.; Koehler, S.; Malek, F.A.; Gaus, W. Sichere Kombinationstherapie mit Weissdorn-Extrakt WS(R) 1442 bei Herzinsuffizienz NYHA II-III Ergebnisse der SPICE-Studie, der ersten Mortalitaets- und Morbiditaetsstudie mit einem pflanzlichen Arzneimittel. Perfusion 2010, 23, 104–109. [Google Scholar]
- Gerz, E.; Geraskin, D.; Neary, P.; Franke, J.; Platen, P.; Kohl-Bareis, M. Tissue oxygenation during exercise measured with NIRS: a quality control study. In Presented at the Clinical and Biomedical Spectroskopy Meeting, Munich, Germany, 14-6-2009; p. 736816.
- Härtel, S.; Kutzner, C.; Schneider, D.; Grieger, S.; Neumaier, M.; Kohl-Bareis, M. Oxygenation of the calf muscle during an incremental, intermittent walking exercise assessed by NIRS. In Presented at the Diffuse Optical Imaging Meeting III, Munich, Germany, 22-5-2011; Hielscher, A.A., Taroni, P., Eds.; p. 80881G-6.
- Haykowsky, M.J.; Brubaker, P.H.; Morgan, T.M.; Kritchevsky, S.; Eggebeen, J.; Kitzman, D.W. Impaired aerobic capacity and physical functional performance in older heart failure patients with preserved ejection fraction: role of lean body mass. J. Gerontol. A Biol. Sci. Med. Sci. 2013, 68, 968–975. [Google Scholar] [CrossRef] [PubMed]
- Haykowsky, M.J.; Kouba, E.J.; Brubaker, P.H.; Nicklas, B.J.; Eggebeen, J.; Kitzman, D.W. Skeletal muscle composition and its relation to exercise intolerance in older patients with heart failure and preserved ejection fraction. Am. J. Cardiol. 2014, 113, 1211–1216. [Google Scholar] [CrossRef]
- Kitzman, D.W.; Nicklas, B.J.; Kraus, W.E.; Lyles, M.F.; Eggebeen, J.; Morgan, T.M.; Haykowsky, M.J. Skeletal Muscle Abnormalities and Exercise Intolerance in Older Patients with Heart Failure and Preserved Ejection Fraction. Am. J. Physiol Heart Circ. Physiol 2014, 13, 64–70. [Google Scholar]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
