Multicomponent Training and Optimal Dosing Strategies for Adults with Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Eligibility Criteria
2.3. Search Strategy
2.4. Data Collection and Synthesis
2.5. Data Extraction and Study Quality
2.6. Statistical Analysis
3. Results
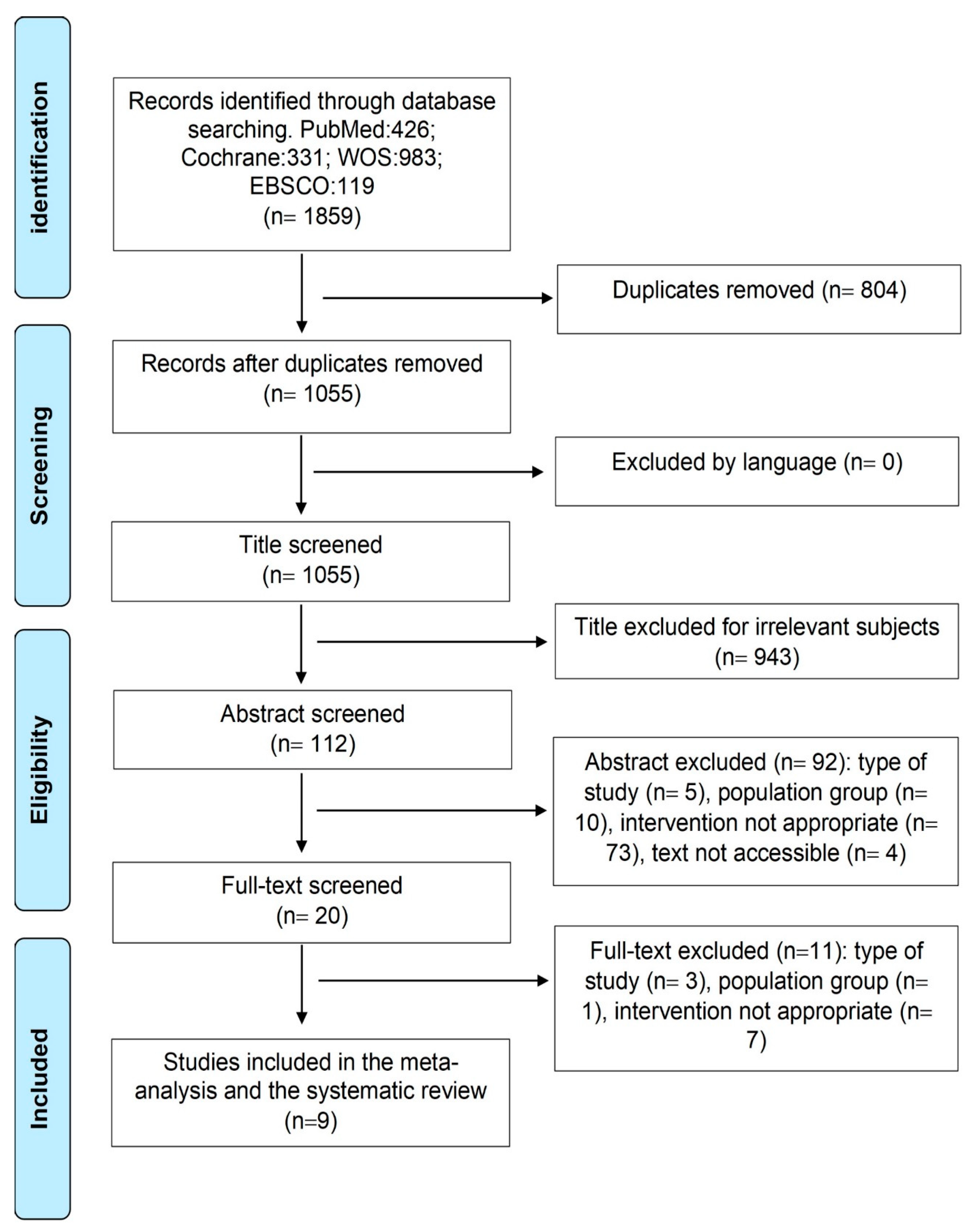
3.1. Search Results and Study Characteristics
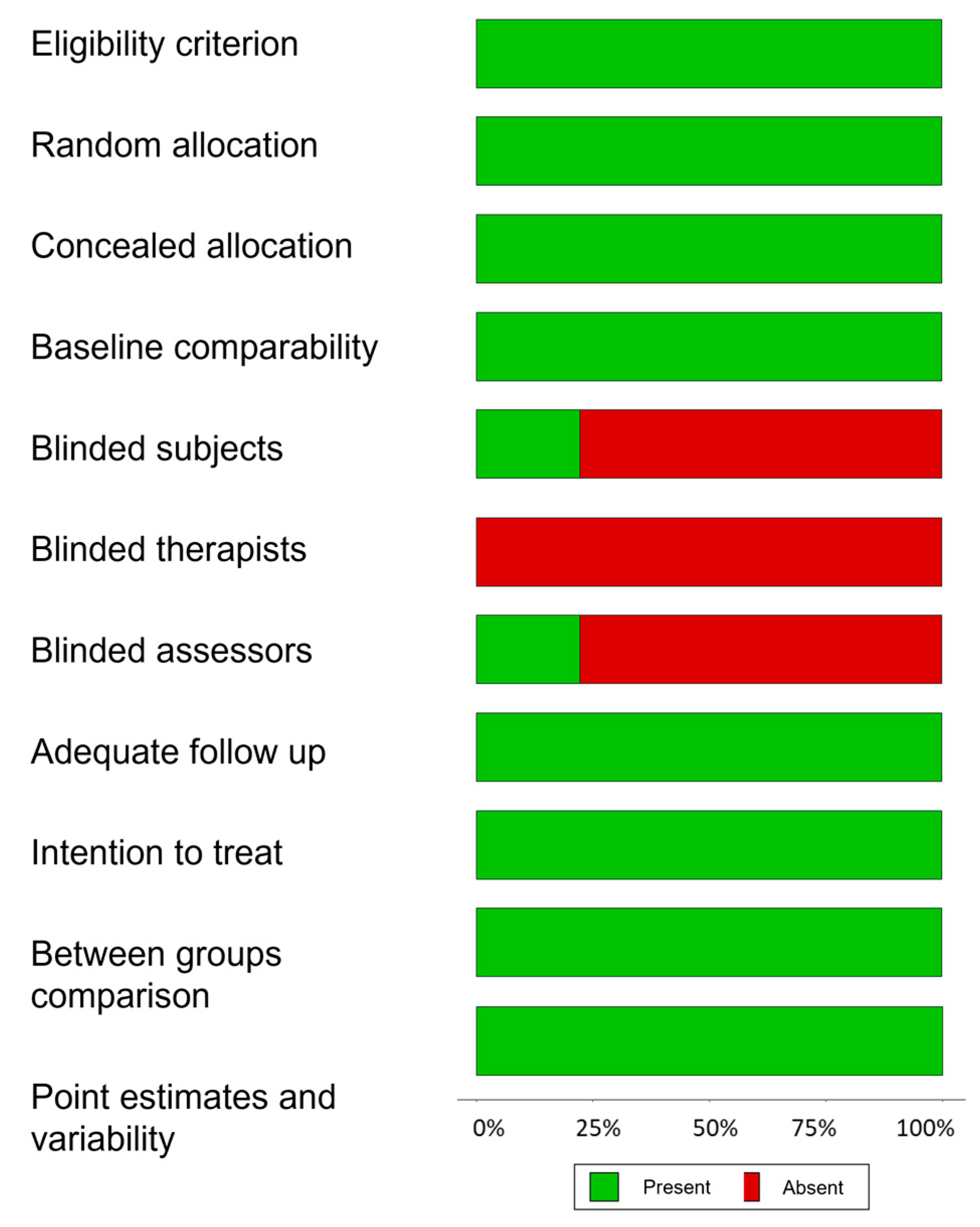
3.2. Risk of Bias
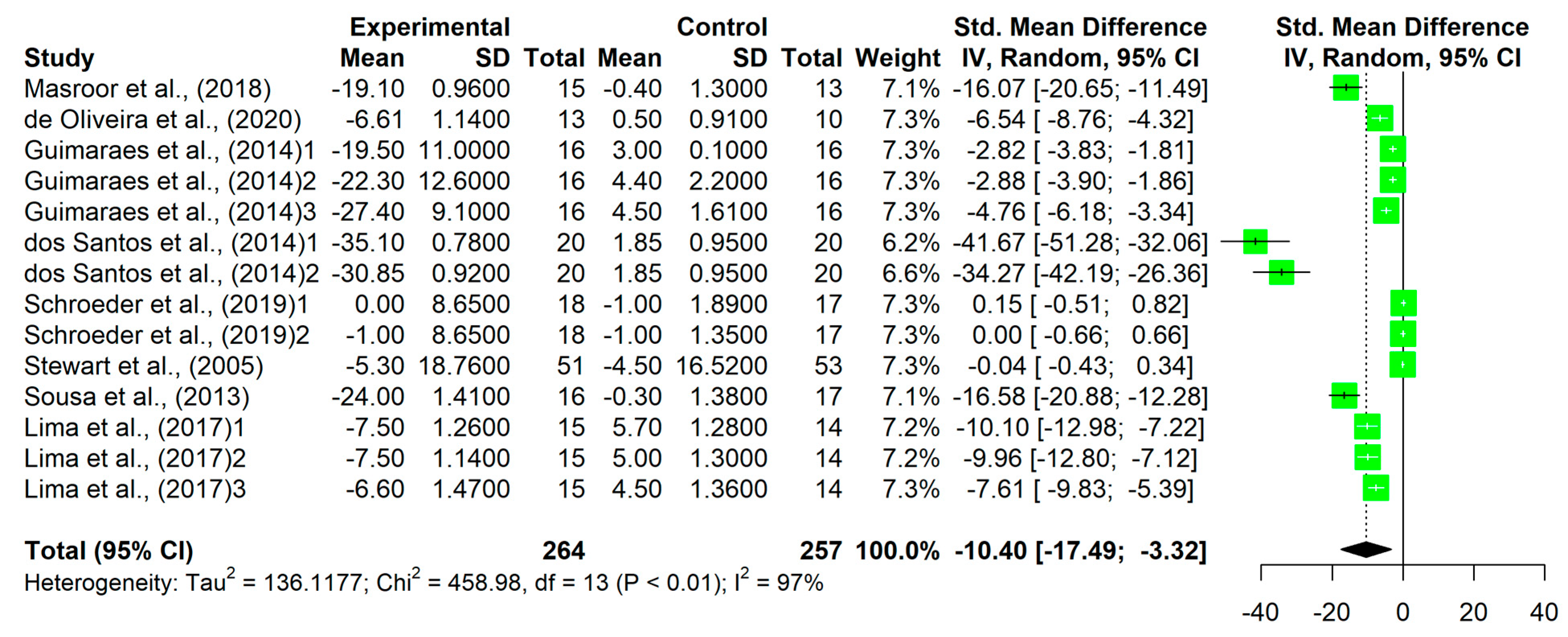
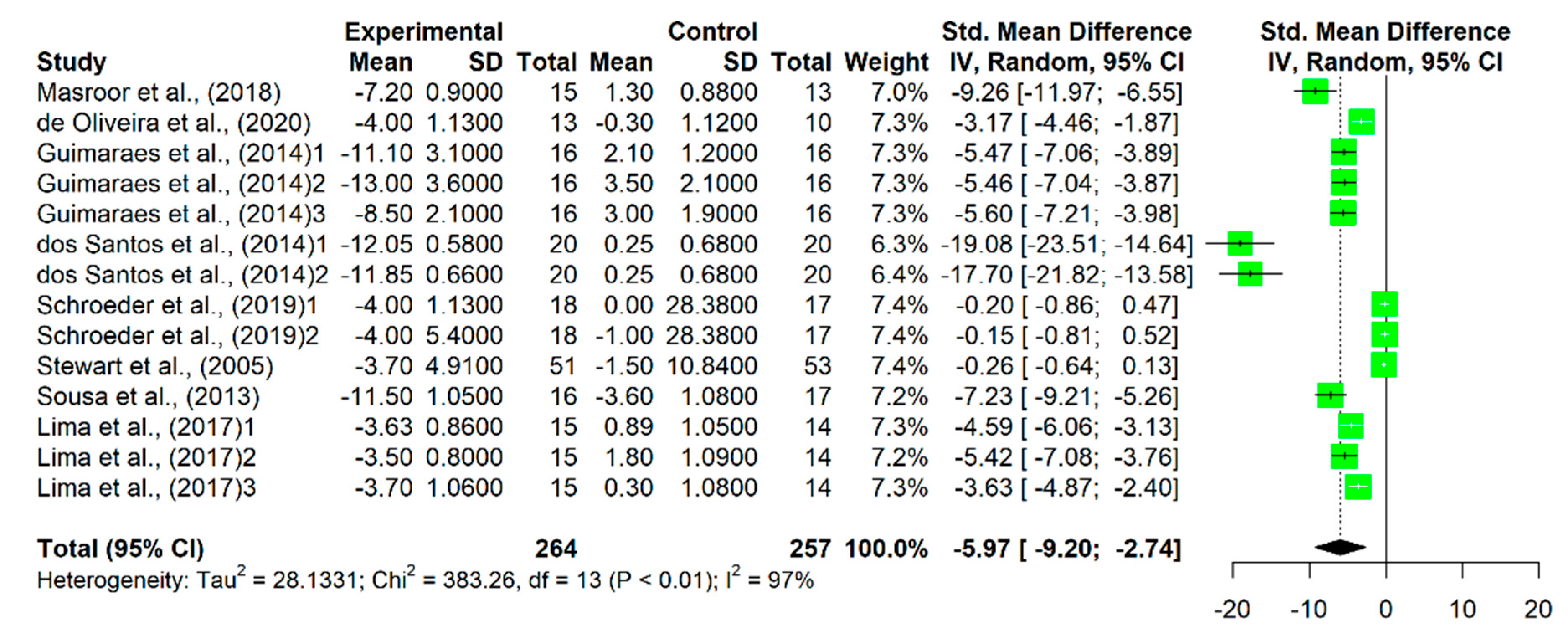
3.3. Effect of the Interventions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stanaway, J.D.; Afshin, A.; Gakidou, E.; Lim, S.S.; Abate, D.; Abate, K.H.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar] [CrossRef]
- Roth, G.A.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef] [PubMed]
- Unger, T.; Borghi, C.; Charchar, F.; Khan, N.A.; Poulter, N.R.; Prabhakaran, D.; Ramirez, A.; Schlaich, M.; Stergiou, G.S.; Tomaszewski, M.; et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020, 75, 1334–1357. [Google Scholar] [CrossRef] [PubMed]
- Gómez, J.F.; Camacho, P.A.; López-López, J.; López-Jaramillo, P. Control y tratamiento de la hipertensión arterial: Programa 20-20. Rev. Colomb. De Cardiol. 2019, 26, 99–106. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Hanssen, H.; Boardman, H.; Deiseroth, A.; Moholdt, T.; Simonenko, M.; Kränkel, N.; Niebauer, J.; Tiberi, M.; Abreu, A.; Solberg, E.E.; et al. Personalized exercise prescription in the prevention and treatment of arterial hypertension: A Consensus Document from the European Association of Preventive Cardiology (EAPC) and the ESC Council on Hypertension. Eur. J. Prev. Cardiol. 2021, 29, 205–215. [Google Scholar] [CrossRef]
- Rossi, F.E.; Fortaleza, A.C.; Neves, L.M.; Buonani, C.; Picolo, M.R.; Diniz, T.A.; Kalva-Filho, C.A.; Papoti, M.; Lira, F.S.; Freitas Junior, I.F. Combined Training (Aerobic Plus Strength) Potentiates a Reduction in Body Fat but Demonstrates No Difference on the Lipid Profile in Postmenopausal Women When Compared With Aerobic Training With a Similar Training Load. J. Strength Cond. Res. 2016, 30, 226–234. [Google Scholar] [CrossRef]
- Dent, E.; Morley, J.E.; Cruz-Jentoft, A.J.; Woodhouse, L.; Rodríguez-Mañas, L.; Fried, L.P.; Woo, J.; Aprahamian, I.; Sanford, A.; Lundy, J.; et al. Physical Frailty: ICFSR International Clinical Practice Guidelines for Identification and Management. J. Nutr. Health Aging 2019, 23, 771–787. [Google Scholar] [CrossRef]
- Pardo, P.J.M.; Gálvez, N.G.; Cristobal, R.V.; Romero, L.S.; Vivancos, A.L.; Díaz, D.V.; García, G.M.G.; González, J.G.P.; Cornejo, I.E.; Pavón, D.J. Programa de Intervención Multidominio Healthy-Age: Recomendaciones para un envejecimiento saludable: Porla red Healthy-Age. Cult. Cienc. Y Deporte 2021, 16, 311–320. [Google Scholar]
- Li, Y.; Hanssen, H.; Cordes, M.; Rossmeissl, A.; Endes, S.; Schmidt-Trucksäss, A. Aerobic, resistance and combined exercise training on arterial stiffness in normotensive and hypertensive adults: A review. Eur. J. Sport Sci. 2015, 15, 443–457. [Google Scholar] [CrossRef]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007, 39, 1435–1445. [Google Scholar] [CrossRef]
- Corso, L.M.; Macdonald, H.V.; Johnson, B.T.; Farinatti, P.; Livingston, J.; Zaleski, A.L.; Blanchard, A.; Pescatello, L.S. Is Concurrent Training Efficacious Antihypertensive Therapy? A Meta-analysis. Med. Sci. Sports Exerc. 2016, 48, 2398–2406. [Google Scholar] [CrossRef]
- Herrod, P.J.J.; Doleman, B.; Blackwell, J.E.M.; O’Boyle, F.; Williams, J.P.; Lund, J.N.; Phillips, B.E. Exercise and other nonpharmacological strategies to reduce blood pressure in older adults: A systematic review and meta-analysis. J. Am. Soc. Hypertens. 2018, 12, 248–267. [Google Scholar] [CrossRef]
- Pescatello, L.S.; Buchner, D.M.; Jakicic, J.M.; Powell, K.E.; Kraus, W.E.; Bloodgood, B.; Campbell, W.W.; Dietz, S.; Dipietro, L.; George, S.M.; et al. Physical Activity to Prevent and Treat Hypertension: A Systematic Review. Med. Sci. Sports Exerc. 2019, 51, 1314–1323. [Google Scholar] [CrossRef]
- Stewart, K.J.; Bacher, A.C.; Turner, K.L.; Fleg, J.L.; Hees, P.S.; Shapiro, E.P.; Tayback, M.; Ouyang, P. Effect of exercise on blood pressure in older persons: A randomized controlled trial. Arch. Intern. Med. 2005, 165, 756–762. [Google Scholar] [CrossRef]
- Sousa, N.; Mendes, R.; Abrantes, C.; Sampaio, J.; Oliveira, J. A randomized 9-month study of blood pressure and body fat responses to aerobic training versus combined aerobic and resistance training in older men. Exp. Gerontol. 2013, 48, 727–733. [Google Scholar] [CrossRef]
- Dos Santos, E.S.; Asano, R.Y.; Filho, I.G.; Lopes, N.L.; Panelli, P.; Nascimento Dda, C.; Collier, S.R.; Prestes, J. Acute and chronic cardiovascular response to 16 weeks of combined eccentric or traditional resistance and aerobic training in elderly hypertensive women: A randomized controlled trial. J. Strength Cond. Res. 2014, 28, 3073–3084. [Google Scholar] [CrossRef]
- Guimaraes, G.V.; de Barros Cruz, L.G.; Fernandes-Silva, M.M.; Dorea, E.L.; Bocchi, E.A. Heated water-based exercise training reduces 24-hour ambulatory blood pressure levels in resistant hypertensive patients: A randomized controlled trial (HEx trial). Int. J. Cardiol. 2014, 172, 434–441. [Google Scholar] [CrossRef]
- Son, W.M.; Sung, K.D.; Cho, J.M.; Park, S.Y. Combined exercise reduces arterial stiffness, blood pressure, and blood markers for cardiovascular risk in postmenopausal women with hypertension. Menopause 2016, 24, 262–268. [Google Scholar] [CrossRef]
- Lima, L.G.; Bonardi, J.T.M.; Campos, G.O.; Bertani, R.F.; Scher, L.M.L.; Moriguti, J.C.; Ferriolli, E.; Lima, N.K.C. Combined aerobic and resistance training: Are there additional benefits for older hypertensive adults? Clinics 2017, 72, 363–369. [Google Scholar] [CrossRef]
- Masroor, S.; Bhati, P.; Verma, S.; Khan, M.; Hussain, M.E. Heart Rate Variability following Combined Aerobic and Resistance Training in Sedentary Hypertensive Women: A Randomised Control Trial. Indian Heart J. 2018, 70 (Suppl. S3), S28–S35. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, E.C.; Franke, W.D.; Sharp, R.L.; Lee, D.C. Comparative effectiveness of aerobic, resistance, and combined training on cardiovascular disease risk factors: A randomized controlled trial. PLoS ONE 2019, 14, e0210292. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, S.N.; Pereira Moro, A.R.; Polito, M.D.; Helena de Jesus, J.; de Souza Bezerra, E. Effects of Concurrent Training with Elastic Tubes in Hypertensive Patients: A Blind Controlled Randomized Clinical Trial. Exp. Aging Res. 2019, 46, 68–82. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Green, S. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; Version 5.1.0; The Cochrane Collaboration: London, UK, 2011; Available online: https://www.cochrane-handbook.org (accessed on 1 February 2021).
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Rosenthal, R. The file drawer problem and tolerance for null results. Psychol. Bull. 1979, 86, 638–641. [Google Scholar] [CrossRef]
- De Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Sterne, J.A.; Sutton, A.J.; Ioannidis, J.P.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Higgins, J.P.; Thompson, S.G. Controlling the risk of spurious findings from meta-regression. Stat. Med. 2004, 23, 1663–1682. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: New York, NY, USA, 1988. [Google Scholar]
- Cornelissen, V.A.; Smart, N.A. Exercise training for blood pressure: A systematic review and meta-analysis. J. Am. Heart Assoc. 2013, 2, e004473. [Google Scholar] [CrossRef]
- Saco-Ledo, G.; Valenzuela, P.L.; Ruiz-Hurtado, G.; Ruilope, L.M.; Lucia, A. Exercise Reduces Ambulatory Blood Pressure in Patients With Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Am. Heart Assoc. 2020, 9, e018487. [Google Scholar] [CrossRef]
- Valenzuela, P.L.; Ruilope, L.M.; Santos-Lozano, A.; Wilhelm, M.; Kränkel, N.; Fiuza-Luces, C.; Lucia, A. Exercise benefits in cardiovascular diseases: From mechanisms to clinical implementation. Eur. Heart J. 2023, 44, 1874–1889. [Google Scholar] [CrossRef]
- Bullard, T.; Ji, M.; An, R.; Trinh, L.; Mackenzie, M.; Mullen, S.P. A systematic review and meta-analysis of adherence to physical activity interventions among three chronic conditions: Cancer, cardiovascular disease, and diabetes. BMC Public Health 2019, 19, 636. [Google Scholar] [CrossRef]
- Spiering, B.A.; Kraemer, W.J.; Anderson, J.M.; Armstrong, L.E.; Nindl, B.C.; Volek, J.S.; Maresh, C.M. Resistance exercise biology: Manipulation of resistance exercise programme variables determines the responses of cellular and molecular signalling pathways. Sports Med. 2008, 38, 527–540. [Google Scholar] [CrossRef]
- Taipale, R.S.; Häkkinen, K. Acute hormonal and force responses to combined strength and endurance loadings in men and women: The “order effect”. PLoS ONE 2013, 8, e55051. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Pescatello, L.S.; Franklin, B.A.; Fagard, R.; Farquhar, W.B.; Kelley, G.A.; Ray, C.A. American College of Sports Medicine position stand. Exercise and hypertension. Med. Sci. Sports Exerc. 2004, 36, 533–553. [Google Scholar] [CrossRef]
- Anandita, M.; Mehta, A.; Yang, E.; Parapid, B. Older Adults and Hypertension: Beyond the 2017 Guideline for Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults; American College of Cardiology: Washington, DC, USA, 2020; Volume 26. [Google Scholar]
- Pedersen, B.K.; Saltin, B. Exercise as medicine—Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports 2015, 25 (Suppl. S3), 1–72. [Google Scholar] [CrossRef]
- Zaleski, A. Exercise for the Prevention and Treatment of Hypertension–Implications and Application; American College of Sports Medicine: Indianapolis, IN, USA, 2019. [Google Scholar]
- Zhang, Y.; Zhang, Y.J.; Zhang, H.W.; Ye, W.B.; Korivi, M. Low-to-Moderate-Intensity Resistance Exercise Is More Effective than High-Intensity at Improving Endothelial Function in Adults: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 6723. [Google Scholar] [CrossRef]
- Eklund, D.; Schumann, M.; Kraemer, W.J.; Izquierdo, M.; Taipale, R.S.; Häkkinen, K. Acute Endocrine and Force Responses and Long-Term Adaptations to Same-Session Combined Strength and Endurance Training in Women. J. Strength Cond. Res. 2016, 30, 164–175. [Google Scholar] [CrossRef] [PubMed]
- Schumann, M.; Küüsmaa, M.; Newton, R.U.; Sirparanta, A.I.; Syväoja, H.; Häkkinen, A.; Häkkinen, K. Fitness and lean mass increases during combined training independent of loading order. Med. Sci. Sports Exerc. 2014, 46, 1758–1768. [Google Scholar] [CrossRef] [PubMed]
- Wilhelm, E.N.; Rech, A.; Minozzo, F.; Botton, C.E.; Radaelli, R.; Teixeira, B.C.; Reischak-Oliveira, A.; Pinto, R.S. Concurrent strength and endurance training exercise sequence does not affect neuromuscular adaptations in older men. Exp. Gerontol. 2014, 60, 207–214. [Google Scholar] [CrossRef] [PubMed]
| Studies | Sample | Age | Treatment | Inclusion Criteria | Main Variables |
|---|---|---|---|---|---|
| Oliveira et al. [23] | EG = 13 CG = 10 | 62.65 ± 6.0 years | Diuretics; ARBs II; ACE inhibitors | Age ≥ 50 years; controlled HTN; medical clearance for exercise; no physical activity in the last 6 months; no serious medical conditions | BP; isometric maximal strength; body composition; VO2 |
| Schoeder et al. [22] | EG (MCT) = 18; (AT), (ST) and (CG) = 17 | 45–74 years 58 ± 7 | Untreated | SBP 120–149 and DBP 80–99 mm Hg without medication; BMI 25–40 kg/m2; sedentary; no serious medical conditions; non-smoker; non-pregnant | BP; HR; BMI; body composition; cardiorespiratory fitness; strength |
| Masroor et al. [21] | EG = 15 CG = 13 | 30–50 years 40.45 ± 4.2 | A drug (not specified) | Sedentary women; premenopausal; stage 1 or 2 HTN; no serious medical conditions; no physical activity in the last 6 months | BP; HRV |
| Lima et al. [20] | EG (MCT) and (AT)= 15; CG = 14 | 60–75 years | Hydrochlorothiazide; ACE inhibitors; ARBs II | Antihypertensive medication; SBP < 160 mm Hg and DBP 105 mm Hg; non-smokers; no serious medical conditions; not obese II or III | BP; blood markers; cardiac hypertrophy; body composition; VO2max |
| Son et al. [19] | EG = 10; CG = 10 | 72–85 years 75 ± 2 | Untreated | Postmenopausal women; stage 1 HTN; non-obese; non-smokers; sedentary; non-medicated | BP; body composition; functional capacity; VO2max; arterial stiffness; endothelin-1; nitrate |
| Guimaraes et al. [18] | EG = 16; CG = 16 | 40–65 years 53.7 ± 6.0 | Diuretics; CCBs; ACE inhibitors; ARBs II; Beta-blockers | HBP >5 years; use of three antihypertensive drugs; no serious medical conditions; no physical activity in the last 6 months; non-smokers | BP; VO2max |
| Dos Santos et al. [17] | EG (TST) = 20; (EST) and CG = 20 | 60–65 years 63.1 ± 2.3 | CCBs; ACE inhibitors; ARBs II | Female; HTN; SBP < 180 and DBP < 110 mm Hg; sedentary; not diabetic; not on drugs and/or alcohol | BP; biochemical parameters |
| Sousa et al. [16] | EG (MCT) = 16 (AT) = 15, CG = 17 | 65–75 years (69.1 ± 5.0) | A drug (not specified) | Older men; no diabetes; no severe obesity; no severe hypertension; no neurological; mental or cognitive impairment; no physical impairment | BP; strength; lower limb aerobic endurance; body fatness |
| Stewart et al. [15] | EG = 51; CG = 53 | 55–75 years 63.6 ± 5.7 | Untreated | Untreated mild hypertension; no physical activity in the last 6 months; non-smokers; no diabetes; no serious diseases | BP; VO2 max; strength; body composition; arterial stiffness |
| Studies | Start | Training | Finish | T, F, D |
|---|---|---|---|---|
| Oliveira et al. [23] | 10′ running and S | Aerobic: 25′ on treadmill, progressing the intensity by 5% every two weeks from 70% HRR to 80% HRR. Strength: 6 exercises (rowing, standing bench press, arm curl, knee extension, knee flexion, forward march with a resistance band) × 2 sets × 15 repetitions × 30″ between sets and exercises. Intensity measured with OMNI-Resistance exercise scale (RES), progressing from 5 RPE progressing to 7 RPE and with the elastic bands from low extensions to high tensions. | 10′ S and ME | 8 wks, 3 days/wk, 70′ |
| Schoeder et al. [22] | - | Aerobic: 30′ on treadmill or cycle ergometer at 40% HRR, progressing to 70% HRR. Strength: 30′ with 8 exercises (chest press, shoulder press, pull-down, lumbar extension, abdominal crunches, torso rotation, biceps curl, triceps extension, leg press, quadriceps extension, leg flexion and hip abduction) × 2 sets of 18–20 reps max until progressing to 3 sets of 10–14 reps max, with 1–2′ rest between sets. | - | 8 wks, 3 days/wk, 60′ |
| Masroor et al. [21] | 5′ treadmill at 40% of HRmax | Aerobic: 20′ treadmill at 50–80% HRmax (intensity increased gradually over 4 weeks) Strength: 5 exercises (bicep curls, triceps extensions, abdominal crunches, leg curls, and knee extensions) × 3 sets × 10 reps at an intensity of 50–80% of 1 RM (intensity was gradually increased over 4 weeks). | 5′ treadmill at 40% of HRmax | 4 wks, 5 days/wk, 50′–60′ |
| Lima et al. [20] | 5′ | Strength: 9 strength exercises (leg press, 45° leg press or bench press, bench extensor, front bench with handle, seated bench press, upright rowing, plantar flexion, seated rowing and crunches) × 15 repetitions (upper limbs) and 20 repetitions (lower limbs and trunk) with an intensity of 50–60% 1 RM. From week 1 to 4, they performed 1 round, and from week 5 to 10, 2 rounds. Aerobic: 20′ on treadmill from week 1 to 4 and 30′ from week 5 to 10. The intensity of the exercise was based on the physical condition of each participant. | - | 10 wks, 3 days/wk, 40′–60′ |
| Son et al. [19] | 5′ SS | Strength: 20′ exercises with elastic bands; 10 exercises (seated row, bicep curl, shoulder flexion, elbow flexion, push-up; hip flexion, hip extension, calf raise, leg press, and squats). Aerobic: 30′ of walking at an exercise intensity of 40% to 50% HRR from weeks 1 to 4 and 60% to 70% HRR from weeks 9–12. | 5′ SS | 12 wks, 3 days/wk 60′ |
| Guimaraes et al. [18] | 5′ | Strength: 20′ calisthenics in water (upper and lower limbs). Aerobic: 30′ walking in water between 11 and 13 on the Borg scale. | 5′ S | 12 wks, 3 days/wk, 60′ |
| Dos Santos et al. [17] | TST | Strength: 7 exercises (bench press with barbell, leg press, trunk extension, leg extension, arm curl, dorsiflexion, and lateral raises). Week 1 to 5 at 70% 10 RM, week 6 to 11 at 80% of 10 RM, and week 12 to 16 at 90% of 10 RM. 3 sets × 10 reps. Aerobic: 20′ on a treadmill at 65–75% HRR. | - | 16 wks, 3 days/wk, 50′–60′ |
| EST | Strength: work 30% 1 RM more than in EFT. Same resistance work. | - | ||
| Sousa et al. [16] | 10′ walking and S | Two days of training on land and one day in the water. Aerobic: 30′ with a choice between walking, jogging, or dancing with moderate intensity; in addition, 10′ of muscle resistance with 3 exercises (with own body weight, and upper and lower body), 3 sets, 15–20 repetitions. The aquatic session: relay races, water volleyball, and water polo. Strength: 6 exercises (bench press, leg press, lateral leg extension, leg extension, leg curl, military press, leg curl, and arm curl) at 65%R 1 RM × 3 sets × 10–12 reps (MC1); 75%RM. 24 × 3 sets × 8–10 reps (MC2); 70%RM × 3 sets × 8–10 reps (MC3); 65%RM × 3 sets × 10–12 reps (MC4). | 5′ S | 32 wks, 3 days/wk, 60′ |
| Stewart et al. [15] | S | Strength: 7 exercises (latissimus dorsi pull down, leg extension, leg curl, bench press, leg press, shoulder press, and seated mid-row) × 2 sets × 10–15 reps at 50% 1 RM. Aerobic: 45′ with a choice of treadmill, exercise bike, or stair climber. Intensity between 60 and 90% HRmax. | - | 24 wks, 3 days/wk, >60′ |
| C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 | C9 | C10 | C11 | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Oliveira et al. [23] | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 9 |
| Schroeder et al. [22] | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 9 |
| Masroor et al. [21] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 10 |
| Lima et al. [20] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 8 |
| Son et al. [19] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 8 |
| Guimaraes et al. [18] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 8 |
| Dos Santos et al. [17] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 8 |
| Sousa et al. [16] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 8 |
| Stewart et al. [15] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 8 |
| Authors | G | MD | 95% CI | p | MD | 95% CI | p | |
|---|---|---|---|---|---|---|---|---|
| Age | ||||||||
| <65 years | Masroor et al. [21], de Oliveira et al. [23], Guimaraes et al. [18], dos Santos et al. [17]_1_TRT, dos Santos et al. [17]_2_ERT, and Schroeder et al. [22] | 6 | −2.2 | −3.63; −0.78 | 0.002 | −0.17 | −0.58; 0.23 | 0.400 |
| ≥65 years | Sousa et al. [16] and Lima et al. [20] | 2 | −1.06 | −1.93; 0.2 | 0.016 | |||
| Weeks | ||||||||
| <14 weeks | Masroor et al. [21], de Oliveira et al. [23], Guimaraes et al. [18], Schroeder et al. [22], and Lima et al. [20] | 5 | −0.97 | −1.74; 0.21 | 0.012 | 0.36 | −0.01; 0.70 | 0.043 |
| ≥14 weeks | dos Santos et al. [17]_1_TRT, dos Santos et al. [17]_2_ERT, and Sousa et al. [16] | 3 | −3.51 | −5.74; −1.27 | 0.002 | |||
| Frequency | ||||||||
| 3 days/weeks | de Oliveira et al. [23], Guimaraes et al. [18], dos Santos et al. [17], Schroeder et al. [22], Sousa et al. [16], and Lima et al. [20] | 6 | −1.47 | −2.53; −0.40 | 0.006 | 0.42 | 0.97; −0.12 | 0.130 |
| >3 days/weeks | Masroor et al. [21] | 1 | −2.63 | −3.63; −1.64 | ˂0.001 | |||
| Intensity Aerobic Training | ||||||||
| ≤75% HRR | Masroor et al. [21], Guimaraes et al. [18], dos Santos et al. [17]_1_TRT, dos Santos et al. [17]_2_ERT, and Schroeder et al. [22] | 5 | −1.51 | −4.26; −0.77 | 0.004 | −0.05 | −0.47; 0.37 | 0.819 |
| >75% HRR | de Oliveira et al. [23] and Sousa et al. [16] | 2 | −1.15 | −1.87; −0.43 | 0.001 | |||
| Duration Aerobic Training | ||||||||
| <30 min | de Oliveira et al. [23], dos Santos et al. [17]_1_TRT, dos Santos et al. [17]_2_ERT, and Lima et al. [20] | 4 | −2.58 | −4.61; −0.55 | 0.012 | 0.46 | 0.16; 0.76 | 0.002 |
| ≥30 min | Masroor et al. [21], Guimaraes et al. [18], Schroeder et al. [22], Stewart et al. [15], and Sousa et al. [16] | 5 | −5.25 | −8.14; 2.35; | <0.001 | |||
| Intensity Strength Training | ||||||||
| ≤75% 1 RM | Schroeder et al. [22], Sousa et al. [16], and Lima et al. [20] | 3 | −0.69 | −1.55; 0.16 | 0.112 | 0.56 | 0.12;1 | 0.013 |
| >75% 1 RM | Masroor et al. [21] and dos Santos et al. [17]_1_TRT | 2 | −4.03 | −6.86; −1.21 | 0.005 | |||
| Repetitions Strength Training | ||||||||
| ≤10 | Masroor et al. [21] and dos Santos et al. [17]_1 TRT | 2 | −4.03 | −6.86; −1.21 | 0.005 | −0.61 | −1.03; −0.18 | 0.005 |
| >10 | de Oliveira et al. [23], Schroeder et al. [22], Sousa et al. [16], and Lima et al. [20] | 4 | −0.71 | −1.33; −0.08 | 0.026 | |||
| Order Training Components | ||||||||
| Aerobic + Strength | Masroor et al. [21], de Oliveira et al. [23], and Schroeder et al. [22] | 3 | −1.10 | −2.52; 0.33 | 0.131 | 0.22 | −0.16; 0.59 | 0.256 |
| Strength + Aerobic | Guimaraes et al. [18], dos Santos et al. [17]_1_TRT, dos Santos et al. [17]_2_ERT, and Lima et al. [20] | 4 | −2.65 | −4.59; −0.71 | 0.007 | |||
| Authors | G | MD | 95% CI | p | MD | 95% CI | p | |
|---|---|---|---|---|---|---|---|---|
| Age | ||||||||
| <65 years | Masroor et al. [21], de Oliveira et al. [23], Guimaraes et al. [18], dos Santos et al. [17]_1_TRT, dos Santos et al. [17]_2_ERT, and Schroeder et al. [22] | 6 | −1.79 | −2.67; −0.91 | <0.001 | −0.20 | −0.60; 0.2 | 0.326 |
| ≥65 years | Sousa et al. [16] and Lima et al. [20] | 2 | −0.97 | −1.60; −0.34 | 0.002 | |||
| Weeks | ||||||||
| <14 weeks | Masroor et al. [21], de Oliveira et al. [23], Guimaraes et al. [18], Schroeder et al. [22], and Lima et al. [20] | 5 | −1.04 | −1.55; 0.54 | <0.001 | 0.40 | 0.75; 0.05 | 0.024 |
| ≥14 weeks | dos Santos et al. [17] _1_TRT, dos Santos et al. [17] _2_ERT, and Sousa et al. [16] | 3 | −2.51 | −3.83; −1.18 | <0.001 | |||
| Frequency | ||||||||
| 3 days/weeks | de Oliveira et al. [23], Guimaraes et al. [18], dos Santos et al. [17] _1_TRT, Schroeder et al. [22], Sousa et al. [16], and Lima et al. [20] | 6 | −1.46 | −2.26; 0.66 | <0.001 | −0.08 | 0.47; −0.62 | 0.784 |
| >3 days/weeks | Masroor et al. [21] | 1 | −1.17 | −1.95; 0.39 | 0.003 | |||
| Intensity Aerobic training | ||||||||
| ≤75% HRR | Masroor et al. [21], de Oliveira et al. [23], Guimaraes et al. [18], dos Santos et al. [17] _1_TRT, dos Santos et al. [17] _2_ERT, and Schroeder et al. [22] | 6 | 1.79 | −2.67; 0.91 | <0.001 | −0.06 | −0.58; 0.47 | 0.832 |
| >75% HRR | Sousa et al. [16] | 1 | −1.3 | −2.07; −0.53 | <0.001 | |||
| Intensity Strength Training | ||||||||
| ≤75% 1 RM | Schroeder et al. [22], Sousa et al. [16], and Lima et al. [20] | 3 | −1.3 | −2.06; −0.55 | <0.001 | 0.21 | 0.64; −0.23 | 0.346 |
| >75% 1 RM | Masroor et al. [21] and dos Santos et al. [17]_1_TRT | 2 | −2.35 | −4.71; 0.01 | 0.050 | |||
| Duration Aerobic training | ||||||||
| <30 min | de Oliveira et al. [23], dos Santos et al. [17]_1_TRT, dos Santos et al. [17] _2_ERT, and Lima et al. [20] | 4 | −1.84 | −3.28; −0.39 | 0.012 | 0.21 | −0.09; 0.51; | 0.173 |
| ≥30 min | Masroor et al. [21], Guimaraes et al. [18], Schroeder et al. [22], Stewart et al. [15], and Sousa et al. [16] | 5 | −3.05 | −5.26; −0.85 | 0.006 | |||
| Repetitions Strength Training | ||||||||
| ≤10 | Masroor et al. [21] and dos Santos et al. [17]_1_TRT | 2 | −2.35 | −4.71; 0.01 | 0.050 | −0.26 | 0.15; −0.68 | 0.216 |
| >10 | de Oliveira et al. [23], Schroeder et al. [22], Sousa et al. [16], and Lima et al. [20] | 4 | −1.10 | −1.76; 0.44 | 0.001 | |||
| Order Training Components | ||||||||
| Aerobic + Strength | Masroor et al. [21], de Oliveira et al. [23], and Schroeder et al. [22] | 3 | −1.21 | −2.07; −0.36 | 0.005 | 0.16 | −0.21; 0.53 | 0.398 |
| Strength + Aerobic | Guimaraes et al. [18], dos Santos et al. [17] _1_TRT, dos Santos et al. [17] _2_ERT, and Lima et al. [20] | 4 | −1.95 | −3.27; −0.64 | 0.003 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Ruiz, I.; Lozano, F.; Masia, M.D.; González-Gálvez, N. Multicomponent Training and Optimal Dosing Strategies for Adults with Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Sports 2023, 11, 115. https://doi.org/10.3390/sports11060115
López-Ruiz I, Lozano F, Masia MD, González-Gálvez N. Multicomponent Training and Optimal Dosing Strategies for Adults with Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Sports. 2023; 11(6):115. https://doi.org/10.3390/sports11060115
Chicago/Turabian StyleLópez-Ruiz, Isabel, Fernando Lozano, María Dolores Masia, and Noelia González-Gálvez. 2023. "Multicomponent Training and Optimal Dosing Strategies for Adults with Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials" Sports 11, no. 6: 115. https://doi.org/10.3390/sports11060115
APA StyleLópez-Ruiz, I., Lozano, F., Masia, M. D., & González-Gálvez, N. (2023). Multicomponent Training and Optimal Dosing Strategies for Adults with Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Sports, 11(6), 115. https://doi.org/10.3390/sports11060115







