Personalized Parenteral Nutrition in Critically Ill Patients Undergoing Continuous Renal Replacement Therapy: A Comprehensive Framework for Clinical Practice
Abstract
1. Introduction
2. Methods
3. Pathophysiological Considerations
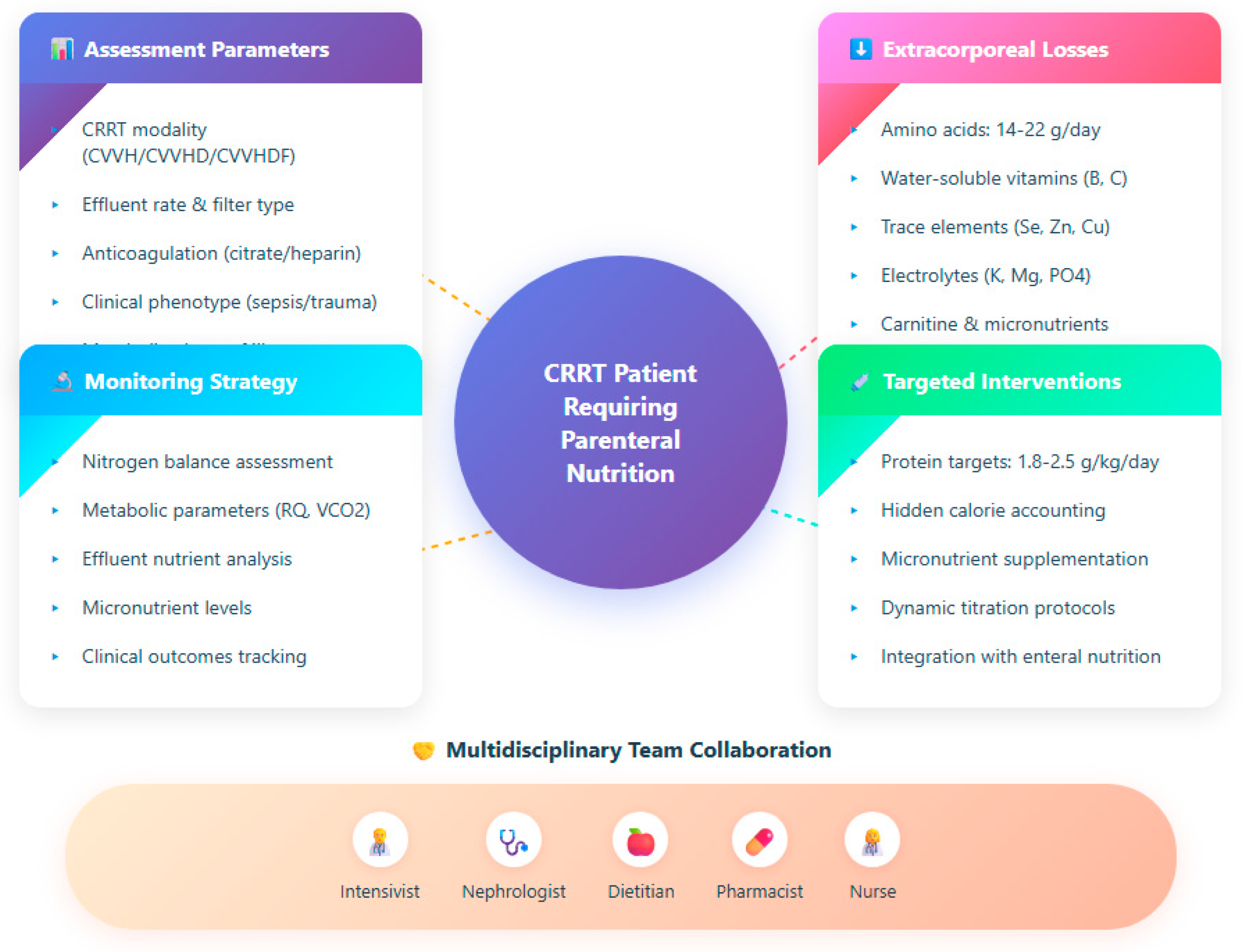
4. Principles of Parenteral Nutrition in CRRT
4.1. Energy Requirements and Substrate Utilization
4.2. Amino Acids and Protein Targets
4.3. Lipids: Role and Tolerance
4.4. Glucose Management and Insulin Needs
4.5. Electrolytes, Micronutrients and Vitamins
4.6. Albumin
5. Personalized Approaches
5.1. Tailoring Nutrition to CRRT Modality and Dose
5.2. Adjustments for Sepsis, Trauma, and Multi-Organ Failure
5.3. Monitoring and Biomarkers of Adequacy
- Nitrogen balance/urea nitrogen appearance: by comparing nitrogen intake with excreted nitrogen (urine + CRRT effluent), one can estimate whether protein supply is sufficient.
- Plasma amino acid levels/profiles: these may reveal substrate depletion or disproportionate clearance.
- Metabolic markers: measures such as respiratory quotient (RQ) from indirect calorimetry, lactate, ketone levels, or substrate oxidation estimates help determine whether energy supply is anabolic or excessive.
- Micronutrient levels (e.g., B vitamins, trace elements): in patients on CRRT, deficiencies may evolve unless explicitly monitored. Wischmeyer et al. argue that in patients at risk (e.g., on RRT), micronutrient evaluation around ICU Day 5–7 should be considered [23].
- Clinical and laboratory parameters: trends in nitrogenous waste, acid–base status, glycemic control, electrolyte shifts, and signs of overfeeding (e.g., hypertriglyceridemia, elevated CO2 production) provide contextual feedback.
5.4. Strategies to Prevent Overfeeding and Underfeeding
- Begin with a ramp-up or stepwise escalation: start at a fraction (e.g., 50–70%) of estimated energy and protein goals, then increase as tolerance is confirmed and metabolic stability ensues. This gradual approach helps prevent sudden metabolic overload. The trend in critical care nutrition supports progressive advances rather than full feeding from day 1 [25].
- Frequent reassessments and dynamic adjustment: daily (or more frequent) review of PN delivery vs. prescribed, biomarker trends, CRRT changes, and clinical course should guide up/down titration.
- Careful accounting of non-nutritional calories: subtract extra calories from citrate, dextrose in replacement solutions or propofol to avoid unintentional overfeeding—a frequent risk in ICU nutrition protocols [26].
- Safety thresholds and triggers: define maximum tolerable glucose infusion rates, lipid doses, total energy ceilings. If parameters (e.g., hyperglycemia, CO2 excess, hypertriglyceridemia) exceed thresholds, the feeding intensity must be reduced.
- Use modular supplementation: rather than remaking entire PN bags, clinicians can adjust individual modules (amino acids, electrolytes, vitamins) to fine-tune without systemic disruption.
- Avoid abrupt large changes: in response to a change in CRRT modality or dose, adjust PN gradually to allow metabolic adaptation rather than inducing shock.
- In patients with unstable multi-organ dysfunction, begin conservatively (slight underfeeding) but with aggressive protein provision, and escalate as the situation stabilizes.
6. Clinical Evidence and Outcomes
6.1. Effects on Mortality, Morbidity, and ICU Stay
6.2. Nutritional Adequacy and Muscle Preservation
6.3. Metabolic Complications and Risk of Infections
7. Practical Aspects and Implementation
7.1. Timing and Initiation of Parenteral Nutrition
7.2. Integration with Enteral Nutrition
7.3. Protocols and Multidisciplinary Collaboration
7.4. Cost-Effectiveness Considerations
8. Future Directions
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PN | Parenteral nutrition |
| AKI | Acute kidney injury |
| CRRT | Continuous renal replacement therapy |
| CVVH | Continuous veno-venous hemofiltration |
| CVVHD | Continuous veno-venous hemodialysis |
| CVVHDF | Continuous veno-venous hemodiafiltration |
| EN | Enteral nutrition |
| ESPEN | European Society for Clinical Nutrition and Metabolism |
| GIR | Glucose infusion rate |
| ICU | Intensive care unit |
| MOF | Multi-organ failure |
| NUTRIC | Nutrition Risk in the Critically Ill |
| PNI | Prognostic nutritional index |
| SANRA | Scale for the Assessment of Narrative Review Articles |
| SPN | Supplemental parenteral nutrition |
| TPN | Total parenteral nutrition |
References
- Nguyen, C.; Singh, G.; Rubio, K.; McLemore, K.; Kuschner, W. Parenteral Nutrition in the Critically Ill Adult: A Narrative Review. J. Intensive Care Med. 2025, 40, 829–838. [Google Scholar] [CrossRef]
- Otis, J.L.; Parker, N.M.; Busch, R.A. Nutrition Support for Patients with Renal Dysfunction in the Intensive Care Unit: A Narrative Review. Nutr. Clin. Pract. 2025, 40, 35–53. [Google Scholar] [CrossRef]
- Ziegler, T.R. Parenteral Nutrition in the Critically Ill Patient. N. Engl. J. Med. 2009, 361, 1088–1097. [Google Scholar] [CrossRef]
- de Man, A.M.; Gunst, J.; Reintam Blaser, A. Nutrition in the Intensive Care Unit: From the Acute Phase to Beyond. Intensive Care Med. 2024, 50, 1035–1048. [Google Scholar] [CrossRef]
- Fishman, G.; Singer, P. Metabolic and Nutritional Aspects in Continuous Renal Replacement Therapy. J. Intensive Med. 2023, 3, 228–238. [Google Scholar] [CrossRef]
- Nystrom, E.M.; Nei, A.M. Metabolic Support of the Patient on Continuous Renal Replacement Therapy. Nutr. Clin. Pract. 2018, 33, 754–766. [Google Scholar] [CrossRef]
- Jonckheer, J.; Vergaelen, K.; Spapen, H.; Malbrain, M.L.N.G.; De Waele, E. Modification of Nutrition Therapy during Continuous Renal Replacement Therapy in Critically Ill Pediatric Patients: A Narrative Review and Recommendations. Nutr. Clin. Pract. 2019, 34, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.M.; Broman, M.; Forni, L.; Ostermann, M.; De Waele, E.; Wischmeyer, P.E. Nutrients and Micronutrients at Risk during Renal Replacement Therapy: A Scoping Review. Curr. Opin. Crit. Care 2021, 27, 367–377. [Google Scholar] [CrossRef] [PubMed]
- Baethge, C.; Goldbeck-Wood, S.; Mertens, S. SANRA—A Scale for the Quality Assessment of Narrative Review Articles. Res. Integr. Peer Rev. 2019, 4, 5. [Google Scholar] [CrossRef] [PubMed]
- Tatsumi, H.; Chihara, S.; Akatsuka, M.; Tani, K.; Kudo, D.; Nakamura, K.; Sato, Y.; Suzuki, K.; Nasu, M.; Hirakawa, M. Evaluation of Amino Acid Kinetics during Low-Dose Continuous Renal Replacement Therapy in Patients with Acute Kidney Injury: A Prospective Single-Center Study. J. Ren. Nutr. 2025, 35, 494–500. [Google Scholar] [CrossRef]
- Lumlertgul, N.; Cameron, L.K.; Bear, D.E.; Ostermann, M. Micronutrient Losses during Continuous Renal Replacement Therapy. Nephron 2023, 147, 759–765. [Google Scholar] [CrossRef]
- Oh, W.C.; Rigby, M.; Harvey, D.; Wei, J.; Tan, C.S.; Choo, J.C.J.; Tay, Z.Y.; Toh, Q.C.; Tee, P.S.; Foo, M.W.Y. Micronutrient and Amino Acid Losses during Renal Replacement Therapy for Acute Kidney Injury. Kidney Int. Rep. 2019, 4, 1094–1108. [Google Scholar] [CrossRef]
- Singer, P.; Blaser, A.R.; Berger, M.M.; Alhazzani, W.; Calder, P.C.; Casaer, M.P.; Hiesmayr, M.; Mayer, K.; Montejo, J.C.; Pichard, C.; et al. ESPEN Guideline on Clinical Nutrition in the Intensive Care Unit. Clin. Nutr. 2019, 38, 48–79. [Google Scholar] [CrossRef]
- Stapel, S.N.; de Boer, R.J.; Thoral, P.J.; Vervloet, M.G.; Girbes, A.R.; Oudemans-van Straaten, H.M. Amino Acid Loss during Continuous Venovenous Hemofiltration in Critically Ill Patients. Blood Purif. 2019, 48, 321–329. [Google Scholar] [CrossRef]
- Davies, S.P.; Reaveley, D.A.; Brown, E.A.; Kox, W.J. Amino acid clearances and daily losses in patients with acute renal failure treated by continuous arteriovenous hemodialysis. Crit. Care Med. 1991, 19, 1510–1515. [Google Scholar] [CrossRef]
- Calder, P.C.; Adolph, M.; Deutz, N.E.P.; Grau, T.; Innes, J.K.; Klek, S. Lipids in the Intensive Care Unit: Recommendations from the ESPEN Expert Group. Clin. Nutr. 2018, 37, 1–18. [Google Scholar] [CrossRef]
- Fiaccadori, E.; Regolisti, G.; Cabassi, A. Specific nutritional problems in acute kidney injury, treated with non-dialysis and dialytic modalities. NDT Plus 2010, 3, 1–7. [Google Scholar] [CrossRef]
- McClave, S.A.; Taylor, B.E.; Martindale, R.G.; Warren, M.M.; Johnson, D.R.; Braunschweig, C. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient. JPEN J. Parenter. Enteral Nutr. 2016, 40, 159–211. [Google Scholar] [CrossRef] [PubMed]
- Lumlertgul, N.; Bear, D.E.; Ostermann, M. Clearance of micronutrients during continuous renal replacement therapy. Crit. Care 2020, 24, 616. [Google Scholar] [CrossRef] [PubMed]
- Vicka, V.; Juknevičius, M.; Juozapavičienė, L.; Galvosas, P.; Stankevičius, E.; Gelman, D.; Mickevičiūtė, D.; Navickas, P.; Dambrauskienė, A.; Jankauskienė, L.; et al. Role of Fat-Free Mass Index on Amino Acid Loss during CRRT in Critically Ill Patients. Medicina 2023, 59, 389. [Google Scholar] [CrossRef] [PubMed]
- Wischmeyer, P.E.; Molinger, J.; Haines, K.; Martindale, R.; Heyland, D.K.; Hurt, R.T.; McClave, S.A.; Preiser, J.C.; Stapleton, R.D.; Bear, D.E.; et al. Personalized Nutrition Therapy in Critical Care: 10 Expert Perspectives. Crit. Care 2023, 27, 261. [Google Scholar] [CrossRef]
- Reintam Blaser, A.; Starkopf, J.; Deane, A.M.; Poeze, M.; Elke, G.; Preiser, J.C.; Casaer, M.P.; Weijs, P.J.M.; Gunst, J.; Schepens, T.; et al. How to Avoid Harm with Feeding Critically Ill Patients: A Synthesis of Viewpoints of a Basic Scientist, Dietitian and Intensivist. Crit. Care 2023, 27, 258. [Google Scholar] [CrossRef]
- Fah, M.; Van Althuis, L.E.; Ohnuma, T.; Winthrop, H.M.; Haines, K.L.; Williams, D.G. Micronutrient Deficiencies in Critically Ill Patients Receiving Continuous Renal Replacement Therapy. Clin. Nutr. ESPEN 2022, 50, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Stoian, M.; Andone, A.; Bândilă, S.R.; Onișor, D.; Babă, D.-F.; Niculescu, R.; Stoian, A.; Azamfirei, L. Personalized Nutrition Strategies for Patients in the Intensive Care Unit: A Narrative Review on the Future of Critical Care Nutrition. Nutrients 2025, 17, 1659. [Google Scholar] [CrossRef] [PubMed]
- Arabi, Y.M.; Aldawood, A.S.; Haddad, S.H.; Al-Dorzi, H.M.; Tamim, H.M.; Jones, G. Permissive underfeeding or standard enteral feeding in critically ill adults. N. Engl. J. Med. 2015, 372, 2398–2408. [Google Scholar] [CrossRef]
- Bousie, E.; van Blokland, D.; Lammers, H.J.; van Zanten, A.R. Relevance of non-nutritional calories in mechanically ventilated critically ill patients. Eur. J. Clin. Nutr. 2016, 70, 1443–1450. [Google Scholar] [CrossRef]
- Heyland, D.K.; Drover, J.W.; Gramlich, L. Total Parenteral Nutrition in the Critically Ill Patient. JAMA 1998, 279, 170–174. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Delgado, J.C.; Muñoz-Del Rio, G.; Flordelís-Lasierra, J.L.; Vidal-Tegedor, B.; Vila-García, A.; Bordejé-Laguna, L.; Zapatero-Gaviria, A.; Fraile-Gutiérrez, V.; Giménez-Esparza, C.; Badenes-Quiles, R.; et al. Parenteral Nutrition: Current Use, Complications, and Efficacy in ICU Patients. Nutrients 2023, 15, 4665. [Google Scholar] [CrossRef]
- Dresen, E.; De Waele, E.; Kiekens, C.; Reynaert, M.; Jochmans, I.; Pirenne, J.; Meersseman, P.; Hermans, G.; Wilmer, A.; Casaer, M.P.; et al. What the Clinician Needs to Know about Medical Nutrition Therapy in Critically Ill Patients in 2023: A Narrative Review. Nutr. Clin. Pract. 2023, 38, 479–498. [Google Scholar] [CrossRef]
- Lee, Y.F.; Huang, K.C.; Tsai, Y.C.; Lin, M.C.; Hsiao, P.J.; Chen, J.S.; Chen, J.B.; Shin, S.J.; Wang, H.H.; Yeh, C.T.; et al. Impact of the prognostic nutritional index on renal replacement therapy–free survival and mortality in patients on continuous renal replacement therapy. Ren. Fail. 2024, 46, 2365394. [Google Scholar] [CrossRef]
- New, A.M.; Nystrom, E.M.; Frazee, E.; Dillon, J.J.; Kashani, K.B.; Miles, J.M.; Markley, B.M.; Bach, K.F.; Miles, A.P.; Palm, C.M.; et al. Continuous Renal Replacement Therapy: A Potential Source of Non-Nutritional Energy Delivery. Am. J. Clin. Nutr. 2017, 105, 1559–1563. [Google Scholar] [CrossRef]
- Al-Zubeidi, D.; Derenoncourt, M.R.; Litchman, T.; McCarthy, M.S.; Seelye, S.M.; Jolicoeur, E.M.; Staley, S.; Dickerson, R.N.; Martindale, R.G.; Hurt, R.T.; et al. Prevention of Complications for Hospitalized Patients Receiving Parenteral Nutrition: A Narrative Review. Nutr. Clin. Pract. 2024, 39, 1037–1053. [Google Scholar] [CrossRef]
- Casaer, M.P.; Mesotten, D.; Hermans, G. Early versus Late Parenteral Nutrition in Critically Ill Adults. N. Engl. J. Med. 2011, 365, 506–517. [Google Scholar] [CrossRef]
- Compher, C.; Bingham, A.L.; McCall, M.; Patel, J.; Rice, T.W.; Braunschweig, C.; McKeever, L. Guidelines for the provision of nutrition support therapy in the adult critically ill patient: The American Society for Parenteral and Enteral Nutrition. JPEN J. Parenter. Enter. Nutr. 2022, 46, 12–41. [Google Scholar] [CrossRef]
- Elke, G.; van Zanten, A.R.H.; Lemieux, M. Enteral versus Parenteral Nutrition in Critically Ill Patients: An Updated Systematic Review and Meta-Analysis of Randomized Controlled Trials. Crit. Care 2016, 20, 117. [Google Scholar] [CrossRef]
- Heidegger, C.P.; Berger, M.M.; Graf, S.; Zingg, W.; Darmon, P.; Costanza, M.C.; Thibault, R.; Pichard, C. Optimization of Energy Provision with Supplemental Parenteral Nutrition in Critically Ill Patients: A Randomized Controlled Trial. Lancet 2013, 381, 385–393. [Google Scholar] [CrossRef]
- Doig, G.S.; Simpson, F.; Finfer, S.; Delaney, A.; Davies, A.R.; Mitchell, I.; Dobb, G.; for the Nutrition Guidelines Investigators of the ANZICS Clinical Trials Group. Effect of evidence-based feeding guidelines on mortality of critically ill adults: A cluster randomized controlled trial. JAMA 2008, 300, 2731–2741. [Google Scholar] [CrossRef]
- Cahill, N.E.; Dhaliwal, R.; Day, A.G. Nutrition Therapy in the Critical Care Setting: What Is “Best Achievable” Practice? Crit. Care Med. 2010, 38, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Elke, G.; Wang, M.; Weiler, N.; Day, A.G.; Heyland, D.K. Close to Recommended Caloric and Protein Intake by Enteral Nutrition Is Associated with Better Clinical Outcome of Critically Ill Septic Patients: Secondary Analysis of a Large International Nutrition Database. Crit. Care 2014, 18, R29. [Google Scholar] [CrossRef] [PubMed]
- Maniaci, A.; Lavalle, S.; Gagliano, C.; Lentini, M.; Masiello, E.; Parisi, F.; Iannella, G.; Cilia, N.D.; Salerno, V.; Cusumano, G.; et al. The Integration of Radiomics and Artificial Intelligence in Modern Medicine. Life 2024, 14, 1248. [Google Scholar] [CrossRef] [PubMed]
- Ridley, E.J.; Davies, A.R.; Parke, R.; Bailey, M.; McArthur, C.; Gillanders, L.; McGuinness, S. Supplemental parenteral nutrition versus usual care in critically ill adults: A pilot randomized controlled study. Crit. Care 2018, 22, 12. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Standard ICU Target | CRRT-Adjusted Target | Rationale for Adjustment | Monitoring |
|---|---|---|---|---|
| Energy | 20–25 kcal/kg/day | 20–25 kcal/kg/day minus hidden calories | Account for citrate (3–4 kcal/mmol), propofol (1.1 kcal/mL), dialysate glucose | Indirect calorimetry, CO2 production, RQ |
| Protein/Amino Acids | 1.2–1.5 g/kg/day | 1.8–2.5 g/kg/day | Compensate for 14–22 g/day effluent losses | Nitrogen balance, effluent amino acid levels, urea appearance |
| Lipids | ≤1.0 g/kg/day | ≤1.5 g/kg/day (max 0.15 g/kg/h) | No significant CRRT clearance; use mixed emulsions | Triglycerides, liver function |
| Glucose | GIR ≤ 4 mg/kg/min | GIR ≤ 5 mg/kg/min adjusted for circuit flux | Variable losses/gains depending on dialysate | Blood glucose q1–2h initially |
| Water-soluble vitamins | Standard dose | 1.5–2× standard dose | High clearance (SC ~1.0) | Serum levels if available |
| Trace elements | Standard dose | Selenium 100–200 μg/day, Zinc 10–15 mg/day | Significant effluent losses | Weekly levels |
| Electrolytes | Per serum levels | Increased supplementation | Continuous removal | Every 4–8 h initially |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sinatra, N.; Maniaci, A.; Cuttone, G.; Senussi Testa, T.; Tutino, S.; Paternò, D.S.; Girombelli, A.; Ippati, G.; Caputo, G.; Sorbello, M.; et al. Personalized Parenteral Nutrition in Critically Ill Patients Undergoing Continuous Renal Replacement Therapy: A Comprehensive Framework for Clinical Practice. J. Pers. Med. 2025, 15, 545. https://doi.org/10.3390/jpm15110545
Sinatra N, Maniaci A, Cuttone G, Senussi Testa T, Tutino S, Paternò DS, Girombelli A, Ippati G, Caputo G, Sorbello M, et al. Personalized Parenteral Nutrition in Critically Ill Patients Undergoing Continuous Renal Replacement Therapy: A Comprehensive Framework for Clinical Practice. Journal of Personalized Medicine. 2025; 15(11):545. https://doi.org/10.3390/jpm15110545
Chicago/Turabian StyleSinatra, Nicola, Antonino Maniaci, Giuseppe Cuttone, Tarek Senussi Testa, Simona Tutino, Daniele Salvatore Paternò, Alessandro Girombelli, Giovanni Ippati, Giorgia Caputo, Massimiliano Sorbello, and et al. 2025. "Personalized Parenteral Nutrition in Critically Ill Patients Undergoing Continuous Renal Replacement Therapy: A Comprehensive Framework for Clinical Practice" Journal of Personalized Medicine 15, no. 11: 545. https://doi.org/10.3390/jpm15110545
APA StyleSinatra, N., Maniaci, A., Cuttone, G., Senussi Testa, T., Tutino, S., Paternò, D. S., Girombelli, A., Ippati, G., Caputo, G., Sorbello, M., & La Via, L. (2025). Personalized Parenteral Nutrition in Critically Ill Patients Undergoing Continuous Renal Replacement Therapy: A Comprehensive Framework for Clinical Practice. Journal of Personalized Medicine, 15(11), 545. https://doi.org/10.3390/jpm15110545









