Applying Ecological Momentary Assessment (EMA) to Understand Overweight and Obesity: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
((ema) OR (“ecological momentary assessment”) OR (“mobile health”) OR (“experience sampling method”) OR (“ambulatory assessment”) OR (“personal digital assistant”) OR (“ambulatory monitoring”) OR (“real-time data capture”) OR (“real-time monitoring”) OR (“real-time interventions”) OR (“electronic diary”) OR (“repeated observations”) OR (“diary data”) OR (“time series”)) AND ((obes*) OR (“binge eating disorder”) OR (“overweight”)).
2.2. Inclusion and Exclusion Criteria
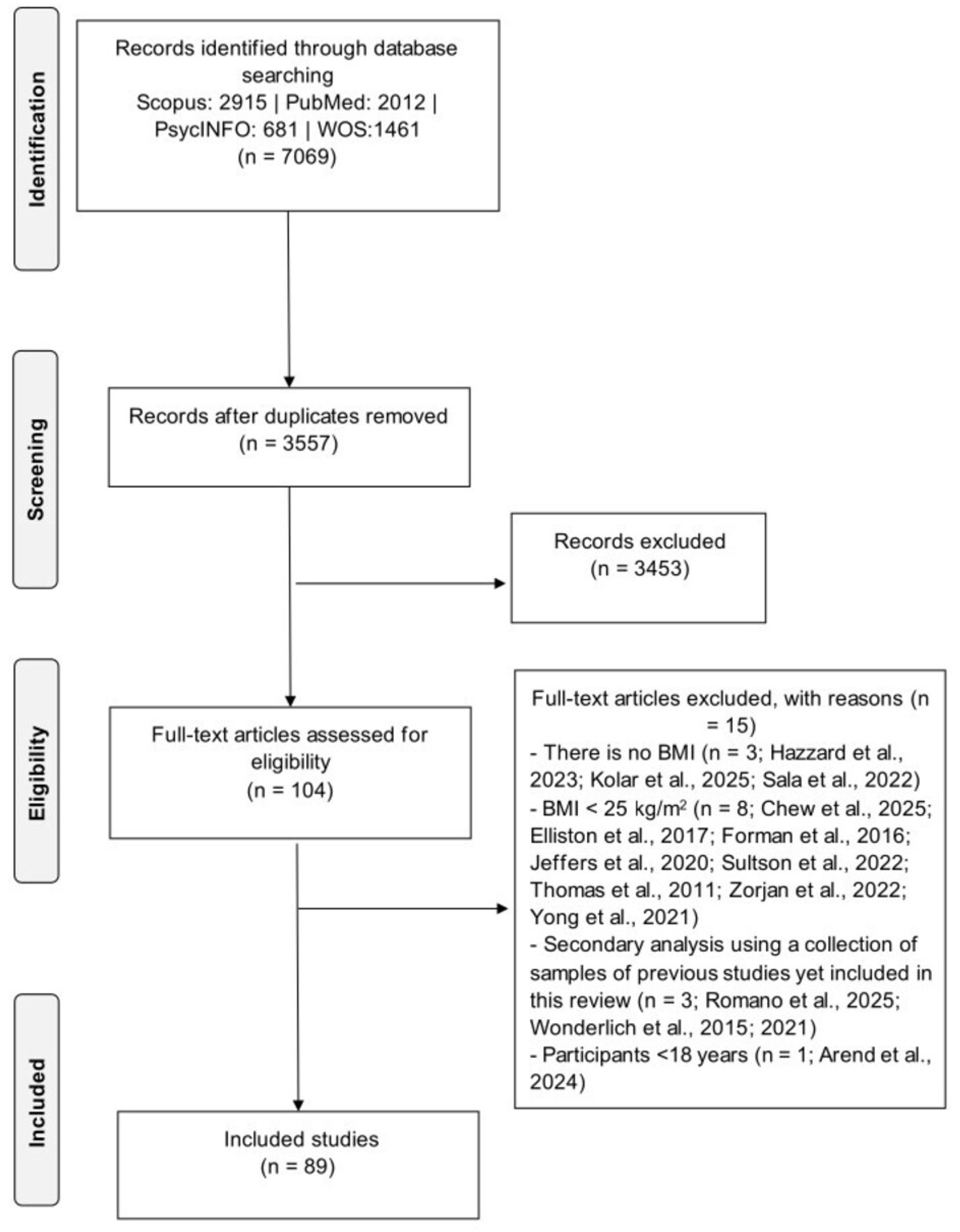
2.3. Study Selection
2.4. Data Extraction and Synthesis
2.5. Quality Appraisal
2.6. Data Synthesis
3. Results
3.1. Study Characteristics
3.2. Description of Participants
3.3. Description of Study Aims
3.4. Description of EMAs
3.5. Description of Measures
3.5.1. Clinical Measures
3.5.2. Predictor Variables
3.5.3. Outcomes Variables
3.6. Description of Main Findings
3.6.1. Eating Behavior and BE Episodes
3.6.2. Temptation and Lapses in Dietary or Exercise Behavior
3.6.3. Food Craving
3.6.4. Weight Stigma
3.6.5. Sleep and Physical Exercise
3.7. Quality Appraisal Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aziz, R.; Sherwani, A.Y.; Al Mahri, S.; Malik, S.S.; Mohammad, S. Why are obese people predisposed to severe disease in viral respiratory infections? Obesities 2023, 3, 46–58. [Google Scholar] [CrossRef]
- Chu, D.-T.; Nguyet, N.T.M.; Nga, V.T.; Lien, N.V.T.; Vo, D.D.; Lien, N.; Ngoc, V.T.N.; Le, D.-H.; Nga, V.B.; Van Tu, P. An update on obesity: Mental consequences and psychological interventions. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Puhl, R.M.; Heuer, C.A.; Brownell, K.D. Stigma and social consequences of obesity. Clin. Obes. Adults Child. 2009, 25–40. [Google Scholar]
- Haththotuwa, R.N.; Wijeyaratne, C.N.; Senarath, U. Worldwide epidemic of obesity. In Obesity and Obstetrics; Elsevier: Amsterdam, The Netherlands, 2020; pp. 3–8. [Google Scholar]
- Phelps, N.H.; Singleton, R.K.; Zhou, B.; Heap, R.A.; Mishra, A.; Bennett, J.E.; Paciorek, C.J.; Lhoste, V.P.F.; Carrillo-Larco, R.M.; Stevens, G.A. Worldwide trends in underweight and obesity from 1990 to 2022: A pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet 2024, 403, 1027–1050. [Google Scholar] [CrossRef]
- Marcozzi, B.; Lo Noce, C.; Vannucchi, S.; Di Lonardo, A.; Damiano, C.; Galeone, D.; Bellisario, P.; Palmieri, L.; Donfrancesco, C. Measured obesity and overweight in adults: The Italian Health Examination Survey 2023-CUORE Project. Eur. J. Public Health 2024, 34 (Suppl. S3), ckae144-1441. [Google Scholar] [CrossRef]
- Castelnuovo, G.; Pietrabissa, G.; Manzoni, G.M.; Cattivelli, R.; Rossi, A.; Novelli, M.; Varallo, G.; Molinari, E. Cognitive behavioral therapy to aid weight loss in obese patients: Current perspectives. Psychol. Res. Behav. Manag. 2017, 10, 9. [Google Scholar] [CrossRef]
- Scott, K.M.; Bruffaerts, R.; Simon, G.E.; Alonso, J.; Angermeyer, M.; De Girolamo, G.; Demyttenaere, K.; Gasquet, I.; Haro, J.M.; Karam, E. Obesity and mental disorders in the general population: Results from the world mental health surveys. Int. J. Obes. 2008, 32, 192–200. [Google Scholar] [CrossRef]
- Pickering, R.P.; Grant, B.F.; Chou, S.P.; Compton, W.M. Are Overweight, Obesity, and Extreme Obesity Associated With Psychopathology? Results From the National Epidemiologic Survey on Alcohol and Related Conditions (CME). J. Clin. Psychiatry 2007, 68, 998–1009. [Google Scholar] [CrossRef]
- Manzoni, G.M.; Cribbie, R.A.; Villa, V.; Arpin-Cribbie, C.A.; Gondoni, L.; Castelnuovo, G. Psychological well-being in obese inpatients with ischemic heart disease at entry and at discharge from a four-week cardiac rehabilitation program. Front. Psychol. 2010, 1, 38. [Google Scholar] [CrossRef]
- Hudson, J.I.; Hiripi, E.; Pope Jr, H.G.; Kessler, R.C. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol. Psychiatry 2007, 61, 348–358. [Google Scholar] [CrossRef]
- Bennett, J.; Greene, G.; Schwartz-Barcott, D. Perceptions of emotional eating behavior. A qualitative study of college students. Appetite 2013, 60, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Van Strien, T.; Frijters, J.E.R.; Bergers, G.P.A.; Defares, P.B. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int. J. Eat. Disord. 1986, 5, 295–315. [Google Scholar] [CrossRef]
- Leehr, E.J.; Krohmer, K.; Schag, K.; Dresler, T.; Zipfel, S.; Giel, K.E. Emotion regulation model in binge eating disorder and obesity—A systematic review. Neurosci. Biobehav. Rev. 2015, 49, 125–134. [Google Scholar] [CrossRef]
- Guerrini-Usubini, A.; Cattivelli, R.; Scarpa, A.; Musetti, A.; Varallo, G.; Franceschini, C.; Castelnuovo, G. The interplay between emotion dysregulation, psychological distress, emotional eating, and weight status: A path model. Int. J. Clin. Health Psychol. 2023, 23, 100338. [Google Scholar] [CrossRef]
- Görlach, M.G.; Kohlmann, S.; Shedden-Mora, M.; Rief, W.; Westermann, S. Expressive suppression of emotions and overeating in individuals with overweight and obesity. Eur. Eat. Disord. Rev. 2016, 24, 377–382. [Google Scholar] [CrossRef]
- Van Strien, T.; Engels, R.C.M.E.; Van Leeuwe, J.; Snoek, H.M. The Stice model of overeating: Tests in clinical and non-clinical samples. Appetite 2005, 45, 205–213. [Google Scholar] [CrossRef]
- Van Strien, T.; Ouwens, M.A. Effects of distress, alexithymia and impulsivity on eating. Eat. Behav. 2007, 8, 251–257. [Google Scholar] [CrossRef]
- Van Strien, T. Causes of emotional eating and matched treatment of obesity. Curr. Diab. Rep. 2018, 18, 35. [Google Scholar] [CrossRef]
- Jackson, J.B.; Pietrabissa, G.; Rossi, A.; Manzoni, G.M.; Castelnuovo, G. Brief strategic therapy and cognitive behavioral therapy for women with binge eating disorder and comorbid obesity: A randomized clinical trial one-year follow-up. J. Consult. Clin. Psychol. 2018, 86, 688. [Google Scholar] [CrossRef]
- Sorgente, A.; Pietrabissa, G.; Manzoni, G.M.; Re, F.; Simpson, S.; Perona, S.; Rossi, A.; Cattivelli, R.; Innamorati, M.; Jackson, J.B. Web-based interventions for weight loss or weight loss maintenance in overweight and obese people: A systematic review of systematic reviews. J. Med. Internet Res. 2017, 19, e229. [Google Scholar] [CrossRef] [PubMed]
- Myin-Germeys, I.; Kasanova, Z.; Vaessen, T.; Vachon, H.; Kirtley, O.; Viechtbauer, W.; Reininghaus, U. Experience sampling methodology in mental health research: New insights and technical developments. World Psychiatry 2018, 17, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Shiffman, S.; Stone, A.A.; Hufford, M.R. Ecological momentary assessment. Annu. Rev. Clin. Psychol. 2008, 4, 1–32. [Google Scholar] [CrossRef]
- Trull, T.J.; Ebner-Priemer, U.W. Using experience sampling methods/ecological momentary assessment (ESM/EMA) in clinical assessment and clinical research: Introduction to the special section. Psychol. Assess. 2009, 21, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Mink, F.; Lutz, W.; Hehlmann, M.I. Ecological Momentary Assessment in psychotherapy research: A systematic review. Clin. Psychol. Rev. 2025, 117, 102565. [Google Scholar] [CrossRef]
- Palmier-Claus, J.E.; Myin-Germeys, I.; Barkus, E.; Bentley, L.; Udachina, A.; Delespaul, P.A.E.G.; Lewis, S.W.; Dunn, G. Experience sampling research in individuals with mental illness: Reflections and guidance. Acta Psychiatr. Scand. 2011, 123, 12–20. [Google Scholar] [CrossRef]
- Engel, S.G.; Crosby, R.D.; Thomas, G.; Bond, D.; Lavender, J.M.; Mason, T.; Steffen, K.J.; Green, D.D.; Wonderlich, S.A. Ecological Momentary Assessment in Eating Disorder and Obesity Research: A Review of the Recent Literature. Curr. Psychiatry Rep. 2016, 18, 37. [Google Scholar] [CrossRef]
- Khan, K.S.; Kunz, R.; Kleijnen, J.; Antes, G. Five steps to conducting a systematic review. J. R. Soc. Med. 2003, 96, 118–121. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Huang, X.; Lin, J.; Demner-Fushman, D. Evaluation of PICO as a knowledge representation for clinical questions. In AMIA Annual Symposium Proceedings; American Medical Informatics Association: Washington, DC, USA, 2006; Volume 2006, p. 359. [Google Scholar]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Smith, V.; Devane, D.; Begley, C.M.; Clarke, M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med. Res. Methodol. 2011, 11, 15. [Google Scholar] [CrossRef]
- Arend, A.K.; Blechert, J.; Yanagida, T.; Voderholzer, U.; Reichenberger, J. Emotional food craving across the eating disorder spectrum: An ecological momentary assessment study. Eat. Weight. Disord.-Stud. Anorex. Bulim. Obes. 2024, 29, 58. [Google Scholar] [CrossRef]
- Chew, H.S.J.; Vashishtha, R.; Du, R.; Liaw, Y.X.; Gneezy, A. Identifying Dietary Triggers Among Individuals with Overweight and Obesity: An Ecological Momentary Assessment Study. Nutrients 2025, 17, 481. [Google Scholar] [CrossRef]
- Elliston, K.G.; Ferguson, S.G.; Schüz, B. Personal and situational predictors of everyday snacking: An application of temporal self-regulation theory. Br. J. Health Psychol. 2017, 22, 854–871. [Google Scholar] [CrossRef]
- Forman, E.M.; Shaw, J.A.; Goldstein, S.P.; Butryn, M.L.; Martin, L.M.; Meiran, N.; Crosby, R.D.; Manasse, S.M. Mindful decision making and inhibitory control training as complementary means to decrease snack consumption. Appetite 2016, 103, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Hazzard, V.M.; Loth, K.A.; Crosby, R.D.; Wonderlich, S.A.; Engel, S.G.; Larson, N.; Neumark-Sztainer, D. Relative food abundance predicts greater binge-eating symptoms in subsequent hours among young adults experiencing food insecurity: Support for the “feast-or-famine” cycle hypothesis from an ecological momentary assessment study. Appetite 2023, 180, 106316. [Google Scholar] [CrossRef]
- Jeffers, A.J.; Mason, T.B.; Benotsch, E.G. Psychological eating factors, affect, and ecological momentary assessed diet quality. Eat. Weight. Disord.-Stud. Anorex. Bulim. Obes. 2020, 25, 1151–1159. [Google Scholar] [CrossRef] [PubMed]
- Kolar, D.R.; Ralph-Nearman, C.; Swanson, T.; Levinson, C.A. Exercise moderates longitudinal group psychopathology networks in individuals with eating disorders. Compr. Psychiatry 2025, 136, 152543. [Google Scholar] [CrossRef] [PubMed]
- Romano, K.A.; Peterson, C.B.; Forester, G.; Wonderlich, J.A.; Wonderlich, S.A.; Engel, S.E.; Crosby, R.D. Momentary Mediational Associations Among Affect, Emotion Dysregulation, and Different Types of Loss of Control Eating Among Adults With Binge Eating Disorder. Int. J. Eat. Disord. 2025, 58, 1072–1084. [Google Scholar] [CrossRef]
- Sala, M.; Linde, J.A.; Crosby, R.D.; Pacanowski, C.R. State body dissatisfaction predicts momentary positive and negative affect but not weight control behaviors: An ecological momentary assessment study. Eat. Weight. Disord.-Stud. Anorex. Bulim. Obes. 2022, 26, 1957–1962. [Google Scholar] [CrossRef]
- Sultson, H.; Kreegipuu, K.; Akkermann, K. Exploring the role of momentary positive and negative affect in overeating and binge eating: Evidence for different associations among men and women. Appetite 2022, 168, 105758. [Google Scholar] [CrossRef]
- Thomas, J.G.; Doshi, S.; Crosby, R.D.; Lowe, M.R. Ecological momentary assessment of obesogenic eating behavior: Combining person-specific and environmental predictors. Obesity 2011, 19, 1574–1579. [Google Scholar] [CrossRef]
- Wonderlich, J.A.; Lavender, J.M.; Wonderlich, S.A.; Peterson, C.B.; Crow, S.J.; Engel, S.G.; Le Grange, D.; Mitchell, J.E.; Crosby, R.D. Examining convergence of retrospective and ecological momentary assessment measures of negative affect and eating disorder behaviors. Int. J. Eat. Disord. 2015, 48, 305–311. [Google Scholar] [CrossRef]
- Wonderlich, J.A.; Crosby, R.D.; Engel, S.G.; Crow, S.J.; Peterson, C.B.; Le Grange, D.; Wonderlich, S.A.; Fischer, S. Negative affect and binge eating: Assessing the unique trajectories of negative affect before and after binge-eating episodes across eating disorder diagnostic classifications. Int. J. Eat. Disord. 2021, 55, 223–230. [Google Scholar] [CrossRef]
- Yong, J.Y.; Tong, E.M.; Liu, J.C. Meal-time smartphone use in an obesogenic environment: Two longitudinal observational studies. JMIR Mhealth Uhealth 2021, 9, e22929. [Google Scholar] [CrossRef]
- Zorjan, S.; Schienle, A. Temporal dynamics of mental imagery, craving and consumption of craved foods: An experience sampling study. Psychol. Health 2022, 38, 1443–1459. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.; Skelton, K.; Dunton, G.; Bruening, M. A systematic review of methods and procedures used in ecological momentary assessments of diet and physical activity research in youth: An adapted STROBE checklist for reporting EMA studies (CREMAS). J. Med. Internet Res. 2016, 18, e151. [Google Scholar] [CrossRef] [PubMed]
- Perski, O.; Keller, J.; Kale, D.; Asare, B.Y.A.; Schneider, V.; Powell, D.; Naughton, F.; ten Hoor, G.; Verboon, P.; Kwasnicka, D. Understanding health behaviours in context: A systematic review and meta-analysis of ecological momentary assessment studies of five key health behaviours. Health Psychol. Rev. 2022, 16, 576–601. [Google Scholar] [CrossRef]
- Armijo-Olivo, S.; Stiles, C.R.; Hagen, N.A.; Biondo, P.D.; Cummings, G.G. Assessment of study quality for systematic reviews: A comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: Methodological research. J. Eval. Clin. Pract. 2012, 18, 12–18. [Google Scholar] [CrossRef]
- Carels, R.A.; Hoffman, J.; Collins, A.; Raber, A.C.; Cacciapaglia, H.; O’Brien, W.H. Ecological momentary assessment of temptation and lapse in dieting. Eat. Behav. 2001, 2, 307–321. [Google Scholar] [CrossRef]
- Kerver, G.A.; Wonderlich, J.A.; Laam, L.A.; Amponsah, T.; Nameth, K.; Steffen, K.J.; Heinberg, L.J.; Safer, D.L.; Wonderlich, S.A.; Engel, S.G. A naturalistic assessment of the relationship between negative affect and loss of control eating over time following metabolic and bariatric surgery. Appetite 2025, 204, 107748. [Google Scholar] [CrossRef]
- Wetzel, K.E.; Himmelstein, M.S.; Ciesla, J.A. Bracing for impact: An intensive longitudinal investigation of weight stigma, vigilant coping, and maladaptive eating. Soc. Sci. Med. 2025, 371, 117904. [Google Scholar] [CrossRef] [PubMed]
- Roordink, E.M.; Joosten, M.M.; Steenhuis, I.H.; Kroeze, W.; Hoekstra, T.; Jacobs, N.; van Stralen, M.M. Affective and cognitive predictors of lapse in exercise and dietary behavior: An ecological momentary assessment study amongst Dutch adults trying to lose weight. Psychol. Health 2025, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Kuipers, E.A.M.; Timmerman, J.G.; van Det, M.J.; Vollenbroek-Hutten, M.M.R. Feasibility and Links Between Emotions, Physical States, and Eating Behavior in Patients After Metabolic Bariatric Surgery: Experience Sampling Study. JMIR Form. Res. 2025, 9, e60486. [Google Scholar] [CrossRef]
- Dougherty, E.N.; Bottera, A.R.; Murray, M.F.; Ekwonu, A.; Wildes, J.E.; Haedt-Matt, A.A. Habitual behavioural control moderates the relation between daily perceived stress and purging. Eur. Eat. Disord. Rev. 2025, 33, 10–19. [Google Scholar] [CrossRef]
- Neal, C.; Pepper, G.V.; Shannon, O.M.; Allen, C.; Bateson, M.; Nettle, D. The daily experience of hunger in UK females with and without food insecurity. Appetite 2025, 204, 107732. [Google Scholar] [CrossRef]
- Morales, J.C.; Smith, K.E.; Mason, T.B. Ecological momentary assessment of weight-related stress predicting eating disorder and affective symptoms. Body Image 2025, 53, 101891. [Google Scholar] [CrossRef]
- Margaryan, L.; Smith, K.E.; Mason, T.B. Daily patterns of loneliness and binge eating and food addiction using ecological momentary assessment. J. Behav. Med. 2025, 48, 616–629. [Google Scholar] [CrossRef]
- Ruf, A.; Neubauer, A.B.; Koch, E.D.; Ebner-Priemer, U.; Reif, A.; Matura, S. Stressed! Grab a bite? Stress eating in adults with Attention-Deficit/Hyperactivity Disorder: An Ecological Momentary Assessment study. Neurosci. Appl. 2025, 4, 105509. [Google Scholar] [CrossRef]
- Pape, M.; Herpertz, S.; Färber, T.; Seiferth, C.; Schoemann, N.; Wolstein, J.; Steins-Loeber, S. Food Addiction in Individuals With Overweight and Obesity Undergoing a 12-Week Long Tailored mHealth Weight Loss Intervention. Eur. Eat. Disord. Rev. 2025, 33, 931–940. [Google Scholar] [CrossRef]
- Boh, B.; Jansen, A.; Clijsters, I.; Nederkoorn, C.; Lemmens, L.H.J.M.; Spanakis, G.; Roefs, A. Indulgent thinking? Ecological momentary assessment of overweight and healthy-weight participants’ cognitions and emotions. Behav. Res. Ther. 2016, 87, 196–206. [Google Scholar] [CrossRef]
- Roefs, A.; Boh, B.; Spanakis, G.; Nederkoorn, C.; Lemmens, L.H.J.M.; Jansen, A. Food craving in daily life: Comparison of overweight and normal-weight participants with ecological momentary assessment. J. Hum. Nutr. Diet. 2019, 32, 765–774. [Google Scholar] [CrossRef] [PubMed]
- Roordink, E.M.; Steenhuis, I.H.M.; Kroeze, W.; Hoekstra, T.; Jacobs, N.; van Stralen, M.M. Social Environmental Predictors of Lapse in Dietary Behavior: An Ecological Momentary Assessment Study Amongst Dutch Adults Trying to Lose Weight. Ann. Behav. Med. 2023, 57, 620–629. [Google Scholar] [CrossRef] [PubMed]
- Latner, J.D.; McLeod, G.; O’Brien, K.S.; Johnston, L. The role of self-efficacy, coping, and lapses in weight maintenance. Eat. Weight Disord. 2013, 18, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Manasse, S.M.; Lampe, E.W.; Srivastava, P.; Payne-Reichert, A.; Mason, T.B.; Juarascio, A.S. Momentary associations between fear of weight gain and dietary restriction among individuals with binge-spectrum eating disorders. Int. J. Eat. Disord. 2022, 55, 541–552. [Google Scholar] [CrossRef]
- Munsch, S.; Meyer, A.H.; Milenkovic, N.; Schlup, B.; Margraf, J.; Wilhelm, F.H. Ecological momentary assessment to evaluate cognitive-behavioral treatment for binge eating disorder. Int. J. Eat. Disord. 2009, 42, 648–657. [Google Scholar] [CrossRef]
- Munsch, S.; Meyer, A.H.; Quartier, V.; Wilhelm, F.H. Binge eating in binge eating disorder: A breakdown of emotion regulatory process? Psychiatry Res. 2012, 195, 118–124. [Google Scholar] [CrossRef]
- Hilbert, A.; Tuschen-Caffier, B. Maintenance of binge eating through negative mood: A naturalistic comparison of binge eating disorder and bulimia nervosa. Int. J. Eat. Disord. 2007, 40, 521–530. [Google Scholar] [CrossRef]
- Svaldi, J.; Werle, D.; Naumann, E.; Eichler, E.; Berking, M. Prospective associations of negative mood and emotion regulation in the occurrence of binge eating in binge eating disorder. J. Psychiatr. Res. 2019, 115, 61–68. [Google Scholar] [CrossRef]
- Seiferth, C.; Fiedler, J.; Farber, T.; Pape, M.; Schroeder, S.; Herpertz, S.; Steins-Loeber, S.; Wolstein, J. Bi-directional associations of core affect and physical activity in adults with higher body weight: An ecological momentary assessment study. J. Health Psychol. 2024, 29, 1115–1128. [Google Scholar] [CrossRef]
- McKee, H.C.; Ntoumanis, N.; Taylor, I.M. An ecological momentary assessment of lapse occurrences in dieters. Ann. Behav. Med. 2014, 48, 300–310. [Google Scholar] [CrossRef]
- Thøgersen-Ntoumani, C.; Dodos, L.A.; Stenling, A.; Ntoumanis, N.; Thogersen-Ntoumani, C.; Dodos, L.A.; Stenling, A.; Ntoumanis, N. Does self-compassion help to deal with dietary lapses among overweight and obese adults who pursue weight-loss goals? Br. J. Health Psychol. 2021, 26, 767–788. [Google Scholar] [CrossRef] [PubMed]
- Keating, L.; Mills, J.S.; Rawana, J.S. Momentary predictors of binge eating: An attachment perspective. Eat. Behav. 2019, 32, 44–52. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, D.E.; Trottier, K.; Cao, L.; Crosby, R.D.; Wonderlich, S.A.; Engel, S.G.; Olmsted, M.P. Momentary skills use predicts decreased binge eating and purging early in day treatment: An ecological momentary assessment study. Int. J. Eat. Disord. 2024, 57, 548–557. [Google Scholar] [CrossRef] [PubMed]
- Alabduljader, K.; Cliffe, M.; Sartor, F.; Papini, G.; Cox, W.M.; Kubis, H.-P. Ecological momentary assessment of food perceptions and eating behavior using a novel phone application in adults with or without obesity. Eat. Behav. 2018, 30, 35–41. [Google Scholar] [CrossRef]
- Nechita, D.M.; David, D. Shame facets as predictors of problematic eating behaviors: An ecological momentary assessment study. Behav. Res. Ther. 2023, 168, 104381. [Google Scholar] [CrossRef]
- Kornacka, M.; Czepczor-Bernat, K.; Napieralski, P.; Brytek-Matera, A. Rumination, mood, and maladaptive eating behaviors in overweight and healthy populations. Eat. Weight Disord. 2021, 26, 273–285. [Google Scholar] [CrossRef]
- Cnudde, K.; De Vylder, F.; Cardon, G.; Maes, I.; Van Dyck, D. Within- and between-person associations of time-varying determinants with snacking in older adults: An EMA study. Br. J. Nutr. 2024, 132, 236–247. [Google Scholar] [CrossRef]
- Booker, J.M.; Cabeza de Baca, T.; Treviño-Alvarez, A.M.; Stinson, E.J.; Votruba, S.B.; Chang, D.C.; Engel, S.G.; Krakoff, J.; Gluck, M.E. Dietary Adherence Is Associated with Perceived Stress, Anhedonia, and Food Insecurity Independent of Adiposity. Nutrients 2024, 16, 526. [Google Scholar] [CrossRef]
- Godfrey, K.M.; Schumacher, L.M.; Butryn, M.L.; Forman, E.M. Physical Activity Intentions and Behavior Mediate Treatment Response in an Acceptance-Based Weight Loss Intervention. Ann. Behav. Med. 2019, 53, 1009–1019. [Google Scholar] [CrossRef]
- Unick, J.L.; Dunsiger, S.I.; Leblond, T.; Hahn, K.; Thomas, J.G.; Abrantes, A.M.; Stroud, L.R.; Wing, R.R. Randomized Trial Examining the Effect of a 12-wk Exercise Program on Hedonic Eating. Med. Sci. Sports Exerc. 2021, 53, 1638–1647. [Google Scholar] [CrossRef]
- Williams, D.M.; Dunsiger, S.; Emerson, J.A.; Gwaltney, C.J.; Monti, P.M.; Miranda, R.J. Self-Paced Exercise, Affective Response, and Exercise Adherence: A Preliminary Investigation Using Ecological Momentary Assessment. J. Sport Exerc. Psychol. 2016, 38, 282–291. [Google Scholar] [CrossRef]
- Bartholomay, J.; Schaefer, L.M.; Forester, G.; Crosby, R.D.; Peterson, C.B.; Crow, S.J.; Engel, S.G.; Wonderlich, S.A. Evaluating dietary restriction as a maintaining factor in binge-eating disorder. Int. J. Eat. Disord. 2024, 57, 1172–1180. [Google Scholar] [CrossRef] [PubMed]
- Peterson, C.B.; Engel, S.G.; Crosby, R.D.; Strauman, T.; Smith, T.L.; Klein, M.; Crow, S.J.; Mitchell, J.E.; Erickson, A.; Cao, L.; et al. Comparing integrative cognitive-affective therapy and guided self-help cognitive-behavioral therapy to treat binge-eating disorder using standard and naturalistic momentary outcome measures: A randomized controlled trial. Int. J. Eat. Disord. 2020, 53, 1418–1427. [Google Scholar] [CrossRef] [PubMed]
- Engel, S.G.; Kahler, K.A.; Lystad, C.M.; Crosby, R.D.; Simonich, H.K.; Wonderlich, S.A.; Peterson, C.B.; Mitchell, J.E. Eating behavior in obese BED, obese non-BED, and non-obese control participants: A naturalistic study. Behav. Res. Ther. 2009, 47, 897–900. [Google Scholar] [CrossRef] [PubMed]
- Goldschmidt, A.B.; Engel, S.G.; Wonderlich, S.A.; Crosby, R.D.; Peterson, C.B.; Le Grange, D.; Tanofsky-Kraff, M.; Cao, L.; Mitchell, J.E. Momentary affect surrounding loss of control and overeating in obese adults with and without binge eating disorder. Obesity 2012, 20, 1206–1211. [Google Scholar] [CrossRef]
- Pollert, G.A.; Engel, S.G.; Schreiber-Gregory, D.N.; Crosby, R.D.; Cao, L.; Wonderlich, S.A.; Tanofsky-Kraff, M.; Mitchell, J.E. The role of eating and emotion in binge eating disorder and loss of control eating. Int. J. Eat. Disord. 2013, 46, 233–238. [Google Scholar] [CrossRef]
- Keith, N.R.; Xu, H.; de Groot, M.; Hemmerlein, K.; Clark, D.O. Identifying Contextual and Emotional Factors to Explore Weight Disparities between Obese Black and White Women. Clin. Med. Insights. Women’s Health 2016, 9, 85–93. [Google Scholar]
- Scherer, E.A.; Metcalf, S.A.; Whicker, C.L.; Bartels, S.M.; Grabinski, M.; Kim, S.J.; Sweeney, M.A.; Lemley, S.M.; Lavoie, H.; Xie, H.; et al. Momentary Influences on Self-Regulation in Two Populations With Health Risk Behaviors: Adults Who Smoke and Adults Who Are Overweight and Have Binge-Eating Disorder. Front. Digit. Health 2022, 4, 798895. [Google Scholar] [CrossRef]
- Williams-Kerver, G.A.; Steffen, K.J.; Smith, K.E.; Cao, L.; Crosby, R.D.; Engel, S.G. Negative Affect and Loss of Control Eating Among Bariatric Surgery Patients: An Ecological Momentary Assessment Pilot Investigation. Obes. Surg. 2020, 30, 2382–2387. [Google Scholar] [CrossRef]
- Goldstein, S.P.; Zhang, F.; Thomas, J.G.; Butryn, M.L.; Herbert, J.D.; Forman, E.M. Application of Machine Learning to Predict Dietary Lapses During Weight Loss. J. Diabetes Sci. Technol. 2018, 12, 1045–1052. [Google Scholar] [CrossRef]
- Srivastava, P.; Michael, M.L.; Manasse, S.M.; Juarascio, A.S. Do momentary changes in body dissatisfaction predict binge eating episodes? An ecological momentary assessment study. Eat. Weight Disord. 2021, 26, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Williams-Kerver, G.A.; Wonderlich, S.A.; Crosby, R.D.; Cao, L.; Smith, K.E.; Engel, S.G.; Crow, S.J.; Peterson, C.B.; Mitchell, J.E.; Le Grange, D. Differences in Affective Dynamics Among Eating Disorder Diagnostic Groups. Clin. Psychol. Sci. Psychol. Sci. 2020, 8, 857–871. [Google Scholar] [CrossRef] [PubMed]
- Carels, R.A.; Hlavka, R.; Selensky, J.C.; Solar, C.; Rossi, J.; Caroline Miller, J. A daily diary study of internalised weight bias and its psychological, eating and exercise correlates. Psychol. Health 2019, 34, 306–320. [Google Scholar] [CrossRef] [PubMed]
- Boswell, R.G.; Potenza, M.N.; Grilo, C.M. The neurobiology of binge-eating disorder compared with obesity: Implications for differential therapeutics. Clin. Ther. 2021, 43, 50–69. [Google Scholar] [CrossRef]
- Goldschmidt, A.B.; Crosby, R.D.; Cao, L.; Engel, S.G.; Durkin, N.; Beach, H.M.; Berg, K.C.; Wonderlich, S.A.; Crow, S.J.; Peterson, C.B. Ecological momentary assessment of eating episodes in obese adults. Psychosom. Med. 2014, 76, 747–752. [Google Scholar] [CrossRef]
- Olson, K.L.; Panza, E.; Lillis, J.; Wing, R.R. Association of Weight-Related Stigmas With Daily Pain Symptoms Among Individuals With Obesity. Ann. Behav. Med. 2023, 57, 269–274. [Google Scholar] [CrossRef]
- Ambwani, S.; Roche, M.J.; Minnick, A.M.; Pincus, A.L. Negative affect, interpersonal perception, and binge eating behavior: An experience sampling study. Int. J. Eat. Disord. 2015, 48, 715–726. [Google Scholar] [CrossRef]
- Schaefer, L.M.; Smith, K.E.; Dvorak, R.; Crosby, R.D.; Wonderlich, S.A. Eating expectancies and reinforcement learning: A state-based test of affect regulation and expectancy models in the natural environment. Eat. Weight Disord. 2021, 26, 2263–2269. [Google Scholar] [CrossRef]
- Parker, M.N.; Michael, M.; Murray, H.B.; Juarascio, A.S.; Manasse, S.M. State emotion modulation and loss-of-control eating in individuals with obesity: A preliminary ecological momentary assessment study. Eat. Behav. 2021, 41, 101478. [Google Scholar] [CrossRef]
- Dougherty, E.N.; Wildes, J.E.; Haedt-Matt, A.A. The role of habit in maintaining binge/purge behaviors: An ecological momentary assessment study. Int. J. Eat. Disord. 2024, 57, 1160–1171. [Google Scholar] [CrossRef]
- Chwyl, C.; Crochiere, R.J.; Forman, E.M. The role of everyday activities on likelihood of dietary lapse: An ecological momentary assessment study. J. Behav. Med. 2023, 46, 532–539. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.O.; Keith, N.R.; Ofner, S.; Hackett, J.; Li, R.; Agarwal, N.; Tu, W. Environments and situations as correlates of eating and drinking among women living with obesity and urban poverty. Obes. Sci. Pract. 2022, 8, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Coffman, D.L.; Oliva, I.B.; Forman, E.M. Does acceptance-based treatment moderate the effect of stress on dietary lapses? Transl. Behav. Med. 2021, 11, 2110–2115. [Google Scholar] [CrossRef] [PubMed]
- Mason, A.E.; Jhaveri, K.; Cohn, M.; Brewer, J.A. Testing a mobile mindful eating intervention targeting craving-related eating: Feasibility and proof of concept. J. Behav. Med. 2018, 41, 160–173. [Google Scholar] [CrossRef]
- Sagui-Henson, S.J.; Radin, R.M.; Jhaveri, K.; Brewer, J.A.; Cohn, M.; Hartogensis, W.; Mason, A.E. Negative Mood and Food Craving Strength Among Women with Overweight: Implications for Targeting Mechanisms Using a Mindful Eating Intervention. Mindfulness 2021, 12, 2997–3010. [Google Scholar] [CrossRef]
- Forester, G.; Schaefer, L.M.; Johnson, J.S.; Richson, B.N.; Dvorak, R.D.; Crosby, R.D.; Peterson, C.B.; Wonderlich, S.A. Evaluating the role of binge planning and binge inevitability within affect regulation models of binge eating. Appetite 2024, 203, 107719. [Google Scholar] [CrossRef]
- Srivastava, P.; Giannone, A.; Lampe, E.W.; Clancy, O.M.; Fitzpatrick, B.; Juarascio, A.S.; Manasse, S.M. A naturalistic examination of feeling fat: Characteristics, predictors, and the relationship with eating disorder behaviors. Int. J. Eat. Disord. 2024, 57, 1756–1768. [Google Scholar] [CrossRef]
- Wonderlich, J.A.; Forester, G.; Crosby, R.D.; Engel, S.G.; Crow, S.J.; Peterson, C.B.; Wonderlich, S.A. An examination of state and trait urgency in individuals with binge-eating disorder. Eur. Eat. Disord. Rev. 2024, 32, 869–879. [Google Scholar] [CrossRef]
- Hagerman, C.J.; Onu, M.C.; Crane, N.T.; Butryn, M.L.; Forman, E.M. Psychological and behavioral responses to daily weight gain during behavioral weight loss treatment. J. Behav. Med. 2024, 47, 492–503. [Google Scholar] [CrossRef]
- Goldstein, S.P.; Hoover, A.; Thomas, J.G. Combining passive eating monitoring and ecological momentary assessment to characterize dietary lapses from a lifestyle modification intervention. Appetite 2022, 175, 106090. [Google Scholar] [CrossRef]
- Carels, R.A.; Douglass, O.M.; Cacciapaglia, H.M.; O’Brien, W.H. An ecological momentary assessment of relapse crises in dieting. J. Consult. Clin. Psychol. 2004, 72, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Vartanian, L.R.; Pinkus, R.T.; Smyth, J.M. The phenomenology of weight stigma in everyday life. J. Context. Behav. Sci. 2014, 3, 196–202. [Google Scholar] [CrossRef]
- Carels, R.A.; Rossi, J.; Solar, C.; Selensky, J.C. An ecological momentary assessment of weight stigma among weight loss participants. J. Health Psychol. 2019, 24, 1155–1166. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, M.L.; Manasse, S.M.; Juarascio, A.S. Affect trajectories surrounding binge eating episodes and heavy drinking episodes in adults with binge-spectrum eating disorders. Eur. Eat. Disord. Rev. 2024, 32, 503–513. [Google Scholar] [CrossRef]
- Forester, G.; Schaefer, L.M.; Dodd, D.R.; Burr, E.K.; Bartholomay, J.; Berner, L.A.; Crosby, R.D.; Peterson, C.B.; Crow, S.J.; Engel, S.G.; et al. Time-of-day and day-of-week patterns of binge eating and relevant psychological vulnerabilities in binge-eating disorder. Int. J. Eat. Disord. 2023, 56, 1694–1702. [Google Scholar] [CrossRef]
- MacIntyre, R.I.; Heron, K.E.; Crosby, R.D.; Engel, S.G.; Wonderlich, S.A.; Mason, T.B. Measurement of the influences of social processes in appetite using ecological momentary assessment. Appetite 2021, 161, 105126. [Google Scholar] [CrossRef]
- Schaefer, L.M.; Forester, G.; Burr, E.K.; Laam, L.; Crosby, R.D.; Peterson, C.B.; Crow, S.J.; Engel, S.G.; Dvorak, R.D.; Wonderlich, S.A. Examining the role of craving in affect regulation models of binge eating: Evidence from an ecological momentary assessment study. J. Psychopathol. Clin. Sci. 2023, 132, 725–732. [Google Scholar] [CrossRef]
- Kalan, R.E.; Smith, A.; Mason, T.B.; Smith, K.E. Independent associations of food addiction and binge eating measures with real-time eating behaviors and contextual factors: An exploratory ecological momentary assessment study. Appetite 2024, 192, 107127. [Google Scholar] [CrossRef]
- Li, S.S.; Kalan, R.E.; Smith, A.; Mason, T.B.; Smith, K.E. Momentary mechanisms of binge-eating symptoms using ecological momentary assessment: The moderating role of food addiction. Eur. Eat. Disord. Rev. 2024, 32, 1105–1116. [Google Scholar] [CrossRef]
- Mason, T.B.; Morales, J.C.; Smith, A.; Smith, K.E. Factor Structure, Reliability, and Convergent Validity of an Ecological Momentary Assessment Binge-Eating Symptoms Scale. Eval. Health Prof. 2024, 48, 189–194. [Google Scholar] [CrossRef]
- Smith, A.; Page, K.A.; Smith, K.E. Associations between affect dynamics and eating regulation in daily life: A preliminary ecological momentary assessment study. Cogn. Emot. 2024, 38, 818–824. [Google Scholar] [CrossRef] [PubMed]
- Sala, M.; Roos, C.R.; Crochiere, R.J.; Butryn, M.L.; Juarascio, A.S.; Manasse, S.M.; Forman, E.M. Real-time fluctuations in mindful awareness, willingness, and values clarity, and their associations with craving and dietary lapse among those seeking weight loss. J. Context. Behav. Sci. 2021, 22, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Goldschmidt, A.B.; Crosby, R.D.; Engel, S.G.; Crow, S.J.; Cao, L.; Peterson, C.B.; Durkin, N. Affect and eating behavior in obese adults with and without elevated depression symptoms. Int. J. Eat. Disord. 2014, 47, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Mason, T.B.; Smith, K.E.; Crosby, R.D.; Dvorak, R.; Engel, S.G.; Crow, S.; Wonderlich, S.A.; Peterson, C.B. Self-discrepancy as a predictor of eating disorder symptoms: Findings from two ecological momentary assessment studies of adults with binge eating. Cognit. Ther. Res. 2022, 46, 580–589. [Google Scholar] [CrossRef]
- Schaefer, L.M.; Smith, K.E.; Anderson, L.M.; Cao, L.; Crosby, R.D.; Engel, S.G.; Crow, S.J.; Peterson, C.B.; Wonderlich, S.A. The role of affect in the maintenance of binge-eating disorder: Evidence from an ecological momentary assessment study. J. Abnorm. Psychol. 2020, 129, 387–396. [Google Scholar] [CrossRef]
- Mason, T.B.; Do, B.; Chu, D.; Belcher, B.R.; Dunton, G.F.; Lopez, N. V Associations among affect, diet, and activity and binge-eating severity using ecological momentary assessment in a non-clinical sample of middle-aged fathers. Eat. Weight Disord. 2022, 27, 543–551. [Google Scholar] [CrossRef]
- Goldstein, S.P.; Dochat, C.; Schumacher, L.M.; Manasse, S.M.; Crosby, R.D.; Thomas, J.G.; Butryn, M.L.; Forman, E.M. Using ecological momentary assessment to better understand dietary lapse types. Appetite 2018, 129, 198–206. [Google Scholar] [CrossRef]
- Goldschmidt, A.B.; Crosby, R.D.; Cao, L.; Pearson, C.M.; Utzinger, L.M.; Pacanowski, C.R.; Mason, T.B.; Berner, L.A.; Engel, S.G.; Wonderlich, S.A.; et al. Contextual factors associated with eating in the absence of hunger among adults with obesity. Eat. Behav. 2017, 26, 33–39. [Google Scholar] [CrossRef]
- Emerson, J.A.; Dunsiger, S.; Williams, D.M. Reciprocal within-day associations between incidental affect and exercise: An EMA study. Psychol. Health 2018, 33, 130–143. [Google Scholar] [CrossRef]
- Crochiere, R.J.; Abber, S.R.; Taylor, L.C.; Sala, M.; Schumacher, L.M.; Goldstein, S.P.; Forman, E.M. Momentary predictors of dietary lapse from a mobile health weight loss intervention. J. Behav. Med. 2022, 45, 324–330. [Google Scholar] [CrossRef]
- Stein, R.I.; Kenardy, J.; Wiseman, C.V.; Dounchis, J.Z.; Arnow, B.A.; Wilfley, D.E. What’s driving the binge in binge eating disorder?: A prospective examination of precursors and consequences. Int. J. Eat. Disord. 2007, 40, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Ralph-Nearman, C.; Hooper, M.A.; Hunt, R.A.; Levinson, C.A. Dynamic relationships among feeling fat, fear of weight gain, and eating disorder symptoms in an eating disorder sample. Appetite 2024, 195, 107181. [Google Scholar] [CrossRef] [PubMed]
- Mason, T.B.; Smith, K.E.; Anderson, L.M.; Schaefer, L.M.; Engel, S.G.; Crow, S.J.; Crosby, R.D.; Peterson, C.B.; Wonderlich, S.A. Affective response to binge eating as a predictor of treatment outcomes for binge-eating disorder. Clin. Psychol. Sci. 2021, 9, 752–760. [Google Scholar] [CrossRef] [PubMed]
- Stein, C.H.; Craft, S.A. Case Managers’ Experiences of Personal Growth: Learning from Consumers. Community Ment. Health J. 2007, 43, 183–195. [Google Scholar] [CrossRef]
- Imes, C.C.; Bizhanova, Z.; Kline, C.E.; Rockette-Wagner, B.; Chasens, E.R.; Sereika, S.M.; Burke, L.E. Bidirectional relationship between sleep and sedentary behavior in adults with overweight or obesity: A secondary analysis. Sleep Adv. J. Sleep Res. Soc. 2021, 2, zpab004. [Google Scholar] [CrossRef]
- Manasse, S.M.; Lampe, E.W.; Gillikin, L.; Trainor, C.M.; Abber, S.R.; Fitzpatrick, B.; Sanchez, H.; Juarascio, A.S. An examination of daily sleep characteristics and subsequent eating disorder behavior among individuals with binge-spectrum eating disorders. Eat. Weight Disord. 2022, 27, 3743–3749. [Google Scholar] [CrossRef]
- Hagerman, C.J.; Ehmann, M.M.; Taylor, L.C.; Forman, E.M. The role of self-compassion and its individual components in adaptive responses to dietary lapses. Appetite 2023, 190, 107009. [Google Scholar] [CrossRef]
- Schumacher, L.M.; Martin, G.J.; Goldstein, S.P.; Manasse, S.M.; Crosby, R.D.; Butryn, M.L.; Lillis, J.; Forman, E.M. Ecological momentary assessment of self-attitudes in response to dietary lapses. Health Psychol. 2018, 37, 148–152. [Google Scholar] [CrossRef]
- Crochiere, R.J.; Zhang, F.Z.; Juarascio, A.S.; Goldstein, S.P.; Thomas, J.G.; Forman, E.M. Comparing ecological momentary assessment to sensor-based approaches in predicting dietary lapse. Transl. Behav. Med. 2021, 11, 2099–2109. [Google Scholar] [CrossRef]
- Srivastava, A.V.; Brown, R.; Newport, D.J.; Rousseau, J.F.; Wagner, K.D.; Guzick, A.; Devargas, C.; Claassen, C.; Ugalde, I.T.; Garrett, A.; et al. The role of resilience in the development of depression, anxiety, and post-traumatic stress disorder after trauma in children and adolescents. Psychiatry Res. 2024, 334, 115772. [Google Scholar] [CrossRef]
- Rancourt, D.; Leahey, T.M.; LaRose, J.G.; Crowther, J.H. Effects of weight-focused social comparisons on diet and activity outcomes in overweight and obese young women. Obesity 2015, 23, 85–89. [Google Scholar] [CrossRef]
- Goldschmidt, A.B.; Crosby, R.D.; Cao, L.; Wonderlich, S.A.; Mitchell, J.E.; Engel, S.G.; Peterson, C.B. A preliminary study of momentary, naturalistic indicators of binge-eating episodes in adults with obesity. Int. J. Eat. Disord. 2018, 51, 87–91. [Google Scholar] [CrossRef]
- Mason, S.M.; Farkas, K.; Friedman, J.K.; Gerlach, A.; Johnson, S.T.; Tavernier, R.E.; Bodnar, L.M.; Neumark-Sztainer, D. Cohort profile: Life-course experiences and pregnancy (LEAP)–A retrospective pregnancy cohort for life-course reproductive health research. PLoS ONE 2024, 19, e0295825. [Google Scholar] [CrossRef]
- Mason, T.B.; Smith, K.E.; Crosby, R.D.; Wonderlich, S.A.; Crow, S.J.; Engel, S.G.; Peterson, C.B. Does the eating disorder examination questionnaire global subscale adequately predict eating disorder psychopathology in the daily life of obese adults? Eat. Weight Disord. 2018, 23, 521–526. [Google Scholar] [CrossRef]
- Potter, L.; Meadows, A.; Smyth, J. Experiences of weight stigma in everyday life: An ecological momentary assessment study. J. Health Psychol. 2021, 26, 2781–2793. [Google Scholar] [CrossRef] [PubMed]
- Fox, J.R.E.; Power, M.J. Eating disorders and multi-level models of emotion: An integrated model. Clin. Psychol. Psychother. An Int. J. Theory Pract. 2009, 16, 240–267. [Google Scholar] [CrossRef] [PubMed]
- Treasure, J.; Duarte, T.A.; Schmidt, U. Eating disorders. Lancet 2020, 395, 899–911. [Google Scholar] [CrossRef]
- Raffone, F.; Atripaldi, D.; Barone, E.; Marone, L.; Carfagno, M.; Mancini, F.; Saliani, A.M.; Martiadis, V. Exploring the Role of Guilt in Eating Disorders: A Pilot Study. Clin. Pract. 2025, 15, 56. [Google Scholar] [CrossRef]
- Polivy, J.; Herman, C.P. Overeating in restrained and unrestrained eaters. Front. Nutr. 2020, 7, 30. [Google Scholar] [CrossRef]
- Boswell, R.G.; Kober, H. Food cue reactivity and craving predict eating and weight gain: A meta-analytic review. Obes. Rev. 2016, 17, 159–177. [Google Scholar] [CrossRef]
- Tapper, K. Mindfulness and craving: Effects and mechanisms. Clin. Psychol. Rev. 2018, 59, 101–117. [Google Scholar] [CrossRef]
- Puhl, R.M.; Heuer, C.A. Obesity stigma: Important considerations for public health. Am. J. Public Health 2010, 100, 1019–1028. [Google Scholar] [CrossRef]
- Durso, L.E.; Latner, J.D. Understanding self-directed stigma: Development of the weight bias internalization scale. Obesity 2008, 16, S80–S86. [Google Scholar] [CrossRef]
- de Jong, K.; Conijn, J.M.; Gallagher, R.A.V.; Reshetnikova, A.S.; Heij, M.; Lutz, M.C. Using progress feedback to improve outcomes and reduce drop-out, treatment duration, and deterioration: A multilevel meta-analysis. Clin. Psychol. Rev. 2021, 85, 102002. [Google Scholar] [CrossRef]
- Giles, E.L.; Robalino, S.; McColl, E.; Sniehotta, F.F.; Adams, J. The effectiveness of financial incentives for health behaviour change: Systematic review and meta-analysis. PLoS ONE 2014, 9, e90347. [Google Scholar] [CrossRef]
- Trull, T.J.; Ebner-Priemer, U.W. Ambulatory assessment in psychopathology research: A review of recommended reporting guidelines and current practices. J. Abnorm. Psychol. 2020, 129, 56. [Google Scholar] [CrossRef] [PubMed]
- Raudenbush, S.W. Hierarchical linear models: Applications and data analysis methods. Adv. Quant. Tech. Soc. Sci. Ser. 2002. [Google Scholar]
- Bolger, N.; Stadler, G.; Laurenceau, J.-P. Power analysis for intensive longitudinal studies. In Handbook of Research Methods for Studying Daily Life; The Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Lafit, G.; Adolf, J.K.; Dejonckheere, E.; Myin-Germeys, I.; Viechtbauer, W.; Ceulemans, E. Selection of the number of participants in intensive longitudinal studies: A user-friendly shiny app and tutorial for performing power analysis in multilevel regression models that account for temporal dependencies. Adv. methods Pract. Psychol. Sci. 2021, 4, 2515245920978738. [Google Scholar] [CrossRef]
 = contextual factors;
= contextual factors;  = emotional factors;
= emotional factors;  = relational factors;
= relational factors;  = gender-related factors;
= gender-related factors;  = psychological or cognitive processes; and
= psychological or cognitive processes; and  = food-related factors.
= food-related factors.
 = contextual factors;
= contextual factors;  = emotional factors;
= emotional factors;  = relational factors;
= relational factors;  = gender-related factors;
= gender-related factors;  = psychological or cognitive processes; and
= psychological or cognitive processes; and  = food-related factors.
= food-related factors.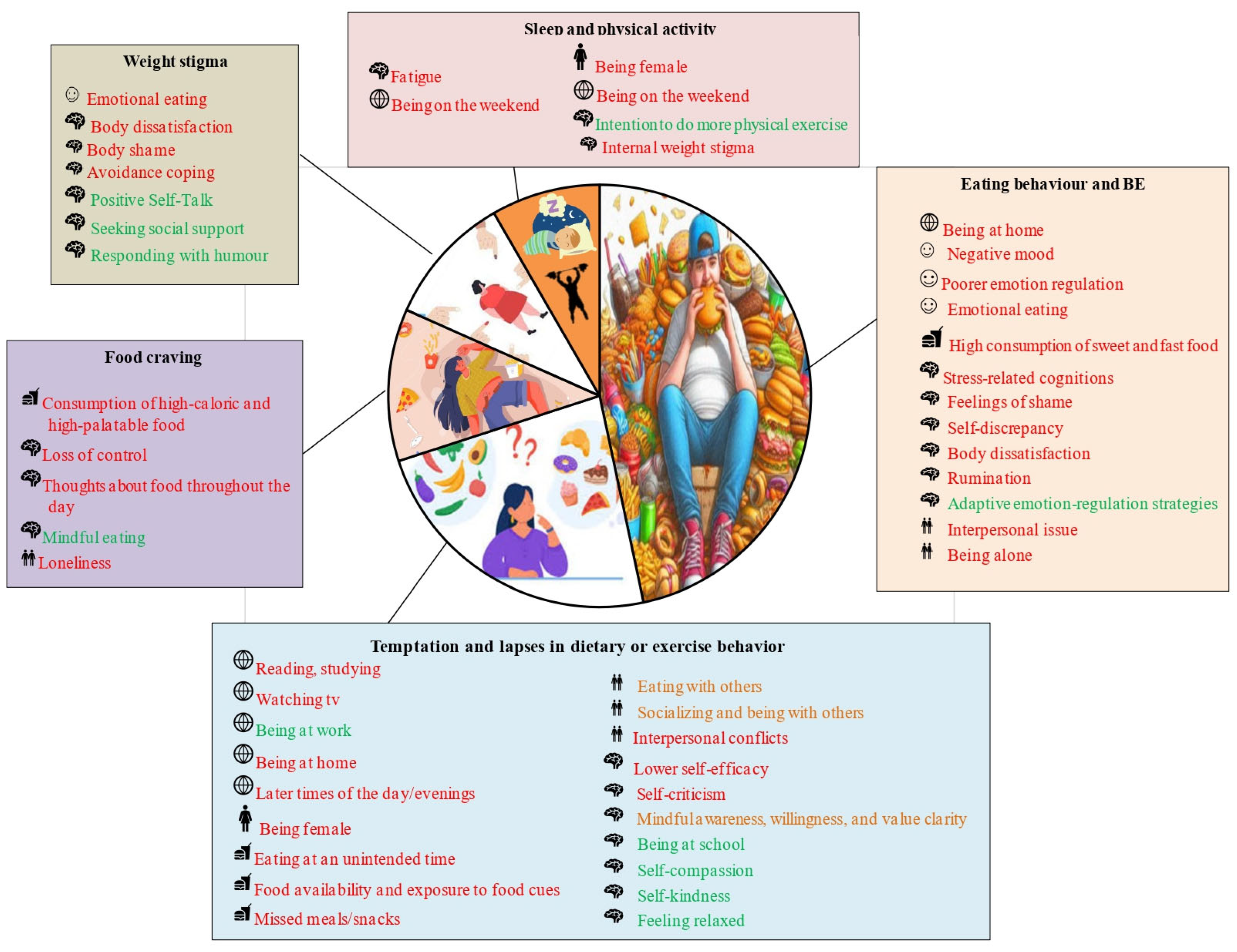
| Author, Year | Quality 1—Rationale for the EMA Design | Quality 2—Whether an a Priori Power Analysis Had Been Conducted | Quality 3—Adherence to the EMAs | Quality 4—Treatment of Missingness | Total |
|---|---|---|---|---|---|
| Alabduljader et al., 2018 [76] | 2 | 1 | 1 | 1 | 5 |
| Ambwani et al., 2015 [99] | 1 | 1 | 1 | 1 | 4 |
| Bartholomay et al., 2024 [84] | 3 | 1 | 2 | 3 | 9 |
| Boh et al., 2016 [62] | 2 | 2 | 2 | 1 | 7 |
| Booker et al., 2024 [80] | 1 | 1 | 1 | 1 | 4 |
| Carels et al., 2001 [51] | 2 | 1 | 1 | 1 | 5 |
| Carels et al., 2004 [113] | 3 | 1 | 2 | 1 | 7 |
| Carels et al., 2019 [95] | 1 | 1 | 2 | 1 | 5 |
| Carels et al., 2019 [80] | 1 | 1 | 1 | 1 | 4 |
| Chwyl et al., 2023 [103] | 2 | 1 | 2 | 1 | 6 |
| Clark et al., 2022 [104] | 1 | 3 | 1 | 2 | 7 |
| Cnudde et al., 2024 [79] | 2 | 3 | 3 | 2 | 10 |
| Coffman et al., 2021 [105] | 1 | 1 | 3 | 1 | 6 |
| Crochiere et al., 2022 [132] | 2 | 1 | 3 | 1 | 7 |
| Dougherty et al., 2024 [102] | 1 | 3 | 1 | 1 | 6 |
| Dougherty et al., 2025 [56] | 1 | 3 | 1 | 1 | 6 |
| Emerson et al., 2018 [131] | 1 | 1 | 2 | 1 | 5 |
| Engel et al., 2009 [86] | 2 | 1 | 1 | 1 | 5 |
| Forester et al., 2023 [117] | 2 | 1 | 1 | 1 | 5 |
| Forester et al., 2024 [108] | 3 | 1 | 3 | 1 | 8 |
| Godfrey et al., 2019 [81] | 2 | 1 | 1 | 1 | 5 |
| Goldschmidt et al., 2012 [87] | 2 | 1 | 2 | 1 | 6 |
| Goldschmidt et al., 2014 [97] | 2 | 1 | 2 | 1 | 6 |
| Goldschmidt et al., 2014 [125] | 1 | 1 | 2 | 1 | 5 |
| Goldschmidt et al., 2017 [130] | 1 | 1 | 2 | 1 | 5 |
| Goldschmidt et al., 2018 [144] | 1 | 1 | 2 | 1 | 5 |
| Goldstein et al., 2018 [92] | 2 | 1 | 2 | 2 | 7 |
| Goldstein et al., 2018 [129] | 2 | 2 | 3 | 3 | 10 |
| Goldstein et al., 2022 [112] | 2 | 3 | 2 | 3 | 10 |
| Hagerman et al., 2023 [139] | 2 | 1 | 2 | 1 | 6 |
| Hagerman et al., 2024 [111] | 1 | 1 | 3 | 2 | 7 |
| Hilbert et al., 2007 [69] | 2 | 1 | 2 | 1 | 6 |
| Imes et al., 2021 [137] | 1 | 1 | 1 | 1 | 4 |
| Kalan et al., 2024 [120] | 1 | 1 | 3 | 1 | 6 |
| Keating et al., 2019 [74] | 3 | 1 | 2 | 3 | 9 |
| Keith et al., 2016 [89] | 1 | 1 | 1 | 1 | 4 |
| Kerver et al., 2025 [52] | 3 | 1 | 3 | 1 | 8 |
| Kornacka et al., 2021 [78] | 1 | 1 | 1 | 1 | 4 |
| Kuipers et al., 2025 [55] | 2 | 1 | 2 | 1 | 6 |
| Latner et al., 2013 [65] | 1 | 1 | 1 | 1 | 4 |
| Li et al., 2024 [121] | 3 | 1 | 3 | 1 | 8 |
| MacDonald et al., 2024 [75] | 1 | 1 | 3 | 1 | 6 |
| MacIntyre et al., 2021 [118] | 1 | 1 | 2 | 1 | 5 |
| Manasse et al., 2022 [138] | 1 | 1 | 3 | 1 | 6 |
| Margaryan et al., 2025 [59] | 1 | 1 | 3 | 1 | 6 |
| Mason et al., 2018 [106] | 1 | 3 | 2 | 2 | 8 |
| Mason et al., 2021 [135] | 2 | 1 | 2 | 2 | 7 |
| Mason et al., 2022 [128] | 2 | 1 | 2 | 1 | 6 |
| Mason et al., 2022 [126] | 3 | 1 | 3 | 1 | 8 |
| Mason et al., 2022 [126] | 3 | 1 | 2 | 1 | 7 |
| Mason et al., 2024 [122] | 3 | 1 | 3 | 1 | 8 |
| Mckee et al., 2014 [72] | 3 | 1 | 1 | 1 | 6 |
| Morales et al., 2025 [58] | 3 | 1 | 2 | 1 | 7 |
| Munsch et al., 2009 [67] | 3 | 1 | 3 | 2 | 9 |
| Munsch et al., 2012 [68] | 3 | 1 | 3 | 1 | 8 |
| Neal et al., 2025 [57] | 2 | 1 | 3 | 1 | 7 |
| Nechita et al., 2023 [77] | 3 | 1 | 1 | 3 | 8 |
| Olson et al., 2023 [98] | 1 | 1 | 3 | 1 | 6 |
| Parker et al., 2021 [101] | 1 | 1 | 1 | 1 | 4 |
| Peterson et al., 2020 [85] | 2 | 3 | 3 | 3 | 11 |
| Pollert et al., 2013 [88] | 1 | 1 | 3 | 1 | 6 |
| Potter et al., 2021 [147] | 2 | 3 | 1 | 1 | 7 |
| Ralph-Nearman et al., 2024 [134] | 1 | 1 | 1 | 2 | 5 |
| Rancourt et al., 2015 [143] | 1 | 1 | 1 | 1 | 4 |
| Roefs et al., 2019 [63] | 3 | 1 | 3 | 1 | 8 |
| Roordink et al., 2023 [54] | 2 | 2 | 3 | 1 | 8 |
| Roordink et al., 2025 [64] | 2 | 2 | 3 | 1 | 8 |
| Ruf et al., 2025 [60] | 3 | 1 | 3 | 2 | 9 |
| Sagui-Henson et al., 2021 [107] | 2 | 3 | 3 | 3 | 11 |
| Sala et al., 2021 [124] | 1 | 3 | 3 | 2 | 9 |
| Schaefer et al., 2020 [127] | 3 | 1 | 2 | 3 | 9 |
| Schaefer et al., 2021 [100] | 3 | 1 | 3 | 1 | 8 |
| Schaefer et al., 2023 [119] | 3 | 1 | 2 | 2 | 8 |
| Scherer et al., 2022 [90] | 3 | 3 | 1 | 1 | 8 |
| Schumacher et al., 2018 [140] | 1 | 1 | 3 | 2 | 7 |
| Seiferth et al., 2024 [71] | 2 | 1 | 1 | 1 | 5 |
| Smith et al., 2024 [123] | 3 | 1 | 3 | 1 | 8 |
| Srivastava et al., 2021 [93] | 1 | 1 | 3 | 1 | 6 |
| Srivastava et al., 2024 [109] | 2 | 1 | 3 | 1 | 7 |
| Stein et al., 2007 [133] | 1 | 1 | 3 | 1 | 6 |
| Svaldi et al., 2019 [70] | 2 | 1 | 3 | 2 | 8 |
| Thøgersen-Ntoumani et al., 2021 [73] | 3 | 1 | 2 | 2 | 8 |
| Unick et al., 2021 [82] | 1 | 3 | 3 | 2 | 9 |
| Vartanian et al., 2014 [114] | 1 | 1 | 1 | 1 | 4 |
| Wetzel et al., 2025 [53] | 3 | 3 | 2 | 2 | 10 |
| Wilkinson et al., 2024 [116] | 3 | 3 | 3 | 1 | 10 |
| Williams-Kerver et al., 2020 [94] | 3 | 2 | 3 | 2 | 10 |
| Williams et al., 2016 [83] | 3 | 1 | 3 | 3 | 10 |
| Wonderlich et al., 2024 [110] | 1 | 1 | 3 | 1 | 6 |
| Weak: 35 (39.32%); Moderate: 28 (31.46%); Strong: 26 (29,21%) | Weak: 70 (78.65%); Moderate: 5 (5.61%); Strong: 14 (15.73%) | Weak: 24 (26.96%); Moderate: 27 (30.33%); Strong: 38 (42.69%) | Weak: 63 (70.78%); Moderate: 17 (19.10%); Strong: 9 (10.11%) | ||
| Legend: 1: Weak, 2: Moderate; and 3: Strong | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rapelli, G.; Spatola, C.A.M.; Landi, G.; Tossani, E.; Grandi, S.; Martino, G.; Castelnuovo, G.; Pietrabissa, G.; Cattivelli, R. Applying Ecological Momentary Assessment (EMA) to Understand Overweight and Obesity: A Systematic Review. J. Pers. Med. 2025, 15, 526. https://doi.org/10.3390/jpm15110526
Rapelli G, Spatola CAM, Landi G, Tossani E, Grandi S, Martino G, Castelnuovo G, Pietrabissa G, Cattivelli R. Applying Ecological Momentary Assessment (EMA) to Understand Overweight and Obesity: A Systematic Review. Journal of Personalized Medicine. 2025; 15(11):526. https://doi.org/10.3390/jpm15110526
Chicago/Turabian StyleRapelli, Giada, Chiara A. M. Spatola, Giulia Landi, Eliana Tossani, Silvana Grandi, Gabriella Martino, Gianluca Castelnuovo, Giada Pietrabissa, and Roberto Cattivelli. 2025. "Applying Ecological Momentary Assessment (EMA) to Understand Overweight and Obesity: A Systematic Review" Journal of Personalized Medicine 15, no. 11: 526. https://doi.org/10.3390/jpm15110526
APA StyleRapelli, G., Spatola, C. A. M., Landi, G., Tossani, E., Grandi, S., Martino, G., Castelnuovo, G., Pietrabissa, G., & Cattivelli, R. (2025). Applying Ecological Momentary Assessment (EMA) to Understand Overweight and Obesity: A Systematic Review. Journal of Personalized Medicine, 15(11), 526. https://doi.org/10.3390/jpm15110526