Abstract
Objectives: The incidence of acute cardiac events is one of the main reasons for medical consultation, disembarkation, repatriation, and death among seafarers at sea. Managing cardiovascular risk factors, particularly those that can be modified, is the key to preventing cardiovascular disease. Therefore, this review estimates the pooled prevalence of major CVD risk factors among seafarers. Methods: We conducted a comprehensive search of studies published between 1994 and December 2021 in four international databases, namely PubMed/Medline, Scopus, Google Scholar, and Web of Science (WOS). Each study was evaluated for methodological quality using the Joanna Briggs Institute (JBI) critical appraisal tool for prevalence studies. The DerSimonian–Laird random-effects model with logit transformations was used to estimate the pooled prevalence of major CVD risk factors. The results were reported in accordance with the Preferred Items for Systematic Review and Meta-analysis (PRISMA) guidelines. Results: Out of all 1484 studies reviewed, 21 studies with 145,913 study participants met the eligibility criteria and were included in the meta-analysis. In the pooled analysis, the prevalence of smoking was found to be 40.14% (95% CI: 34.29 to 46.29%) with heterogeneity between studies (I2 = 98%, p < 0.01). The prevalence of hypertension, overweight, obesity, diabetes mellitus, and alcohol consumption was 45.32%, 41.67%, 18.60%, 12.70%, and 38.58%, respectively. However, the sensitivity analysis after excluding studies showed a pooled prevalence of hypertension, overweight, obesity, and diabetes mellitus of 44.86%, 41.87%, 15.99%, and 16.84%, respectively. The subgroup analysis demonstrated that smoking prevalence among seafarers had decreased significantly after 2013. Conclusion: This study demonstrated that CVD risk factors, particularly hypertension, overweight, smoking, alcohol consumption, and obesity, are prevalent among seafarers. These findings may serve as a guide for shipping companies and other responsible bodies in order to prevent CVD risk factors among seafarers. PROSPERO Registration: CRD42022300993.
1. Introduction
Globally, cardiovascular diseases (CVD) account for the majority of disease burden and are attributed to both modifiable and unmodifiable risk factors [1]. CVD are also the number one cause of death from disease on board among seafarers [2,3]. On board a ship, acute cardiac events are one of the leading causes of medical consultation, disembarkation, repatriation, and mortality among seafarers [4,5,6,7,8]. The risk of cardiovascular events among seafarers is higher than that of the general population [9,10]. This may be due to a variety of reasons, including inadequate treatment, no regular monitoring, no immediate response to the emergency despite its severity, delayed resuscitation action, or work-related stress [11].
It is well known that the working conditions of sailors influence their health. A seafarer’s work is characterized by long working hours, lack of sleep and frequent interruptions in their sleep, as well as staying at sea for extended periods of time, which adversely affects their health [12,13,14]. Due to the particular circumstances of their working environment, seafarers can experience different coping strategies such as unhealthy lifestyles (such as smoking, alcohol consumption, etc.) [13,15]. In addition to physical and psychological stresses, these unhealthy lifestyles contribute to CVD on board ships [16]. In order to prevent CVD, risk factors, particularly those that are modifiable, need to be managed.
Modifiable risk factors, such as tobacco use, heavy alcohol consumption, overweight/obesity, and physical inactivity are highly prevalent among seafarers [9,10,17,18,19]. Additionally, the prevalence of modifiable risk factors varies widely among mariners. In a recent systematic review, the prevalence of modifiable risk factors was reported; for smoking, the prevalence was between 37.3% and 72.3%, for overweight between 27.9% and 66.5%, for high blood pressure between 8.2% and 49.7%, and for diabetes mellitus, it ranged from 3.3% to 9.3% [20]. Another systematic review found that the prevalence of alcohol consumption among seafarers varies widely, from 11.5% to 89.5% [21]. As a result, the data presented on the prevalence of modifiable CVD risk factors among seafarers are inconsistent between studies. Inconsistent data on the prevalence of modifiable risk factors for CVD among seafarers may lead decision-makers as well as researchers to consider different figures based on their preferences and the available information. To date, no studies have been reported on the pooled prevalence of CVD risk factors in seafarers. In order to make evidence-based decisions, an analysis of the pooled prevalence of major risk factors for CVD is essential.
The present study aimed to estimate the prevalence of major CVD risk factors (cigarette smoking, high blood pressure, diabetes mellitus, overweight, obesity, and alcohol consumption) among seafarers by reviewing literature available on the topic and analyzing it with a meta-analysis prevalence approach. The results of this study could help international organizations [e.g., International Maritime Organization (IMO), International Labor Office (ILO), World Health Organization (WHO)], national governments, trade unions, shipping companies, and other decision-makers to develop strategies to improve the control of CVD risk factors on board ships among seafarers.
2. Methods
The present systematic review followed the Preferred Items for Systematic Review and Meta-analysis (PRISMA) checklists and diagrams to design and report the results [22], and registered a protocol for this review with the International Prospective Register of Systematic Reviews (PROSPERO) registration number: CRD42022300993).
It is available from https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022300993 (accessed on 8 May 2023).
2.1. Research Questions
This study was guided by the following primary research questions: What is the magnitude of major CVD risk factors among seafarers? Does the distribution of CVD risk factors on-board ships differ according to the time period? How does age affect the distribution of CVD risk factors?
2.2. Search Strategy and Data Sources
In order to identify relevant studies, we conducted a comprehensive systematic search of the literature according to the Meta-Analysis of Observational Studies in Epidemiology (MOOSE) guidelines [23] and the PRISMA statement [22]. We searched the following databases PubMed/Medline, Scopus, Google Scholar, and Web of Science (WOS) for studies reporting the prevalence of CVD risk factors, specifically smoking, high blood pressure, diabetes mellitus, overweight, obesity, and alcohol use, up to November 2021. Further relevant articles were manually reviewed from the retrieved study reference lists. We applied the following key terms for searching in PubMed, Scopus, and WOS for hypertension: “prevalence”, “proportion”, “magnitude”, “high blood pressure”, “hypertension”, “seafarers”, “onboard ships”, “merchant ships”, and “sailors”. To combine the search terms for each outcome of interest, we used Boolean operators such as “AND” and “OR”. The full search strategy in PubMed and Scopus for the prevalence of hypertension, overweight, obesity, smoking, diabetes mellitus, and alcohol use can be found in Supplemental Table S1 (see Supplementary Table S1).
2.3. Inclusion and Exclusion Criteria
The following criteria were considered for eligibility: (1) observational studies (cross-sectional, cohort, and case-control); (2) studies reporting on the prevalence of high blood pressure, overweight, obesity, smoking, diabetes mellitus (DM), and alcohol consumption; (3) studies published between 1994 and December 2021; (4) full-text studies written in English. The following studies were not considered in this study: (1) studies that were not peer-reviewed or were unpublished; (2) studies published as abstracts or conference proceedings; (4) qualitative studies; (5) studies with a small sample size (less than 50 study participants); (6) studies published in languages other than English; (7) review studies, i.e., either systematic or narrative reviews.
In this study, six co-authors (G.G.S., U.A., C.M., G.N., A.S., and G.B.) carried out a literature search and selected the studies independently based on the inclusion criteria. While conducting the literature search and selecting the studies, the two senior co-authors (G.R. and F.A.) resolved any disagreements between the authors.
2.4. Data Extraction and Outcome Variables
After selecting studies, the variables extracted from each study were the first author’s name, publication year, number of cases or reported prevalence, sample size, and study design. These data were entered into an Excel spreadsheet. The primary outcome of the present study was the pooled prevalence of CVD risk factors (high blood pressure, smoking, diabetes, overweight, obesity, alcohol consumption). The five authors (G.G.S., U.A., C.M., G.N., and G.B.) extracted data and compared the results. Any discrepancies between the results were resolved through discussion.
2.5. Quality Assessment
The Joanna Briggs Institute (JBI) critical appraisal tool was used to assess the methodological quality of the studies [24]. The critical appraisal tool contains ten items that were used to evaluate the methodological quality of studies reporting prevalence data (see Supplementary Table S2). A critical appraisal was performed prior to data extraction. Despite the fact that there are four possible responses to each question in the critical appraisal tool (“yes”, “no”, “unclear” or “not applicable”), there is no indication in the document as to how the assessment tool should be interpreted quantitatively in order to rank the studies as low or high quality. Some studies, however, used the mean scores to measure the quality of studies [25,26].
In the present study, the quality of the studies was evaluated using agreed-upon category scores for each study. As a result, the studies were categorized into low, medium, and high quality based on scores ranging from 0 to 10. The studies scoring between 0 and 4 were considered low-quality, the studies scoring between 5 and 6 were considered medium-quality, while studies scoring seven and above (7–10) were considered high-quality.
2.6. Statistical Analysis
The data were entered into a Microsoft Excel spreadsheet version 2019 and analyzed using R-software (Version 4.1.1, The R Foundation for Statistical Computing, Vienna, Austria) [27]. We used the metaprop()functions from R package meta [28] for prevalence and summary meta-analysis and we employed also the escalc(), rma(), and predict() functions from R package metafor [29] along with different arguments to calculate individual effect size (i.e., proportions) and their corresponding sampling variance estimation. A DerSimonian–Laird random-effects model with logit transformations was used to estimate the pooled prevalence of CVD risk factors (high blood pressure, smoking, overweight, obesity, diabetes mellitus, and alcohol consumption) [30]. A random-effect model was used to adjust observed variability [31]. The pooled proportion of each CVD risk factor, considered in the present study with a 95% CI, was generated and visualized using a forest plot.
Begg’s and Egger’s tests were performed to detect the potential publication bias [32,33]. Heterogeneity between studies was assessed using the Cochran’s Q test [34] and I2 test statistics [35]. The degree of heterogeneity was considered as low, moderate, and high based on I2 values of less than 25%, 25% to 75%, and more than 75%, respectively [36]. A univariate meta-regression analysis was conducted based on publication years and sample size to estimate their impact on the prevalence of each CVD risk factor. We also performed a sensitivity analysis using the “Leave-one-out” analysis with a built-in function. Once the outliers were identified, we re-estimated the summary effect (i.e., pooled prevalence) by omitting outliers. Subgroup analyses were also performed according to the year of publication.
3. Results
3.1. Study Characteristics
In total, 1484 records were identified using our search strategy, of which 954 records were excluded because of duplicates. The title and abstract screening excluded 495 articles. The remaining 35 full-text articles were evaluated. Among the 35 full-text papers reviewed, 21 studies with 145,913 study participants met the eligibility criteria and were included in the meta-analysis [9,10,17,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54]. Figure 1 shows the entire process of finding, selecting, and including studies (Figure 1).
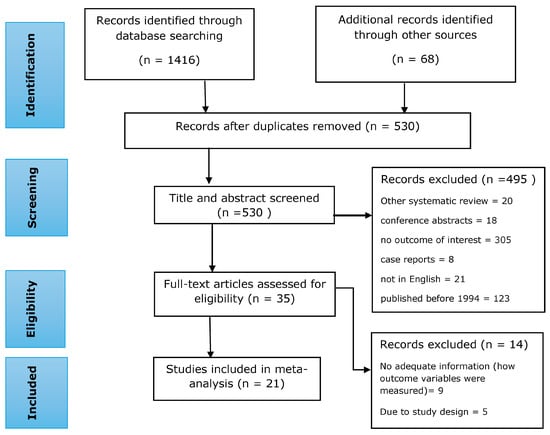
Figure 1.
A flow diagram showing the process of study searching, selection, and inclusion in the present systematic review and meta-analysis.
The studies included in the present systematic review and meta-analysis were conducted between 1994 and 2021. All the included studies were cross-sectional studies (out of 21 studies, 3 were retrospective analyses of cross-sectional studies). The characteristics of the selected studies are summarized in Table 1 along with their methodological quality assessment (Table 1).

Table 1.
Characteristics of selected studies for systematic review and meta-analysis.
3.2. Operational Definition of Outcome Variables in the Included Studies
Four studies defined high blood pressure/hypertension according to the current World Health Organization (WHO) criteria [55]: systolic blood pressure (SBP) ≥ 140 mmHg and/or diastolic blood pressure (DBP) ≥ 90 mmHg and/or taking antihypertensive drugs. In the remaining four studies, high blood pressure was defined as a SBP ≥ 130 mmHg and/or a DBP ≥ 85 mmHg or antihypertensive medication. Smoking status (n = 16) was assessed using a self-reported questionnaire. It was subsequently verified by asking questions such as about the duration of use, age at onset, and the number of cigarettes per day. Overweight (n = 12) and obesity (n = 12) were defined according to current WHO criteria using body mass index (BMI) [56]: 25.0 kg/m2 < BMI < 30.0 kg/m2, and ≥30 kg/m2, respectively, and the BMI was also calculated as weight in kilograms (kg) divided by height in meters (m) squared [Weight (kg)/Height (m)2]. Regarding diabetes mellitus, it was defined as follows: fasting plasma glucose level > 110 mg/dL (n = 1), fasting blood glucose level > 126 mg/dL or blood glucose level 2 h after eating > 200 mg/dL (n = 1), fasting plasma glucose ≥ 5.6 mmol/L or previously diagnosed type two diabetes (n = 1), and fasting glucose level ≥ 110 mg/dL and/or anti-diabetic medication use (n = 2).
3.3. Prevalence of CVD Risk Factors
3.3.1. Prevalence of Smoking
Sixteen studies were selected with a total of 11,511 study participants [9,10,17,38,39,40,41,42,43,45,46,47,48,49,50,52]. In general, the prevalence of smoking varied greatly between the 16 studies, ranging from 23.85% [46] to 67.18% [10]. The pooled prevalence of smoking among seafarers was found to be 40.14% (95% CI: 34.29% to 46.29%), with a high and statistically significant heterogeneity (I2 = 98%, p < 0.01). We took into account the year of publication as a subgroup analysis of smoking prevalence. Thus, seven studies were published between 1994 and 2012, and nine studies were published between 2013 and 2020. The publication year was then categorized into two groups: 2013 and after (2013–2021), and before 2013 (1994–2012). As a result, the pooled proportion of smoking was 34.43% (95% CI: 25.90% to 44.11%, I2 = 98%, p < 0.01) during the 2013 year of publication and after, and 47.85% (95% CI: 41.24% to 54.52%, I2 = 95%, p < 0.01) before 2013. There was a significant decline in smoking prevalence (p < 0.01) in 2013 and subsequent years compared to before 2013 (34.43% vs. 47.85%) (Figure 2).
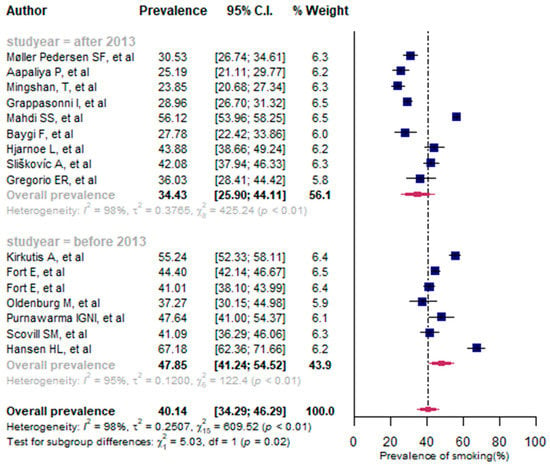
Figure 2.
A forest plot of the prevalence (%) of smoking among seafarers using a random-effects model.
The findings of univariate meta-regression analysis showed that sample size had no impact on the prevalence of smoking among seafarers [QM (test of moderators) (1) = 0.956, p = 0.328]. The year of publication had an impact on the observed prevalence of smoking in seafarers. In fact, there was an association between the prevalence of smoking and year of publication (QM(1) = 9.648, p < 0.001) as well as the significant slope coefficient [−0.059, Z(14) = −3.106, p = 0.002]. The R2 for the publication year shows that 20.47% of the true heterogeneity in the presented effect size can be explained by the year of publication.
The sensitivity analysis indicated no evidence of outliers among the included studies for smoking prevalence (see Supplementary Tables S3 and S4).
3.3.2. Prevalence of High Blood Pressure
The pooled prevalence of high blood pressure among seafarers was 45.32% (95% CI: 36.98% to 53.93%) with significant heterogeneity between the studies (I2 = 96%, p < 0.01) (Figure 3). Overall, eight studies were identified with a total of 3554 study participants [9,17,38,41,42,43,46,48]. The prevalence of high blood pressure varied between the selected studies, ranging from 21.23% [41] to 70.42% [43]. As for the prevalence based on the year of publication, the overall proportion of prevalence of high blood pressure (HBP) was 51.74% (95% CI: 37.90% to 65.32%) after the 2013 year of publication, and 39.02% (95%CI: 29.85 to 49.03%) before 2013 (Figure 3).
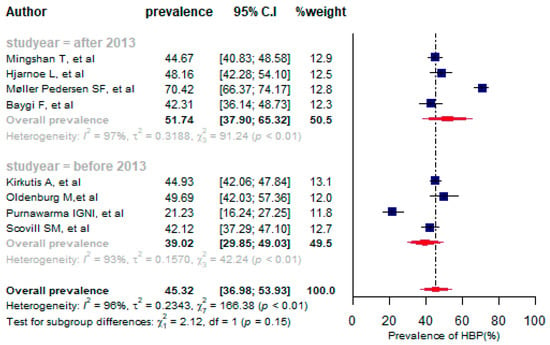
Figure 3.
A forest plot of the prevalence (%) of high blood pressure among seafarers using a random-effects model.
A sensitivity analysis was performed and two outlier studies were identified [41,43], which influenced the pooled estimate of high blood pressure (see Supplementary Tables S5 and S6). After omitting the outlier studies, the overall prevalence of high blood pressure was 44.86% (95%CI: 43.03% to 46.71%) (Supplementary Figure S1), which indicates that the pooled prevalence decreased slightly after removing the outlier studies.
3.3.3. Prevalence of Overweight
Overall, twelve studies reporting the overweight prevalence with a total of 136,710 participants were selected for the meta-analysis [10,17,37,38,41,42,44,46,48,51,53,54]. In selected studies, the prevalence of overweight varied from 28.09% [42] to 51.51% [10]. The pooled prevalence of overweight among seafarers was 41.67% (95% CI: 39.16% to 44.22%, I2 = 85%, p < 0.01). Five of the twelve studies analyzed for combined prevalence were published before 2013 and the remaining seven studies were published after 2013. As a result, the pooled proportion of overweight before the 2013 year of publication was found to be 40.71% (95% CI: 33.67% to 48.16%), and it was 42.15% (95% CI: 39.46% to 44.88%) after 2013. Thus, the prevalence of overweight increased slightly after 2013 compared to before 2013, although the difference was not statistically significant (p = 0.72) (Figure 4).
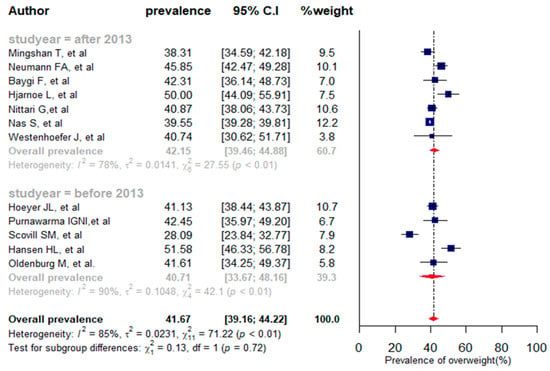
Figure 4.
A forest plot of the prevalence (%) of overweight among seafarers using a random-effects model.
The meta-regression analysis indicated that both sample size [QM(1) = 0.209, p = 0.647] and publication year [QM(1) = 1.495, p = 0.222] were not significantly associated with the proportion of high blood pressure. The sensitivity analysis identified two studies that had influenced the overall prevalence of overweight (Supplementary Tables S7 and S8). After removing the two outlier studies [10,42], the pooled prevalence of overweight was 41.87% (39.88% to 43.89%) with heterogeneity between studies (I2 = 70%, p < 0.01) (see Supplementary Figure S2).
In two studies, the prevalence of overweight was assessed by age group [37,44]. As a result, the overall prevalence of overweight among seafarers aged 16–24 years was 25.64% (95% CI: 18.43% to 34.48%), and 48.84% (95% CI: 43.66% to 54.04%) among those aged 45–66 years (Table 2). The results of our study demonstrated that overweight in seafarers increases significantly with age (x2(2) = 18.46, p < 0.001).

Table 2.
Prevalence of overweight and obesity in terms of age among seafarers.
3.3.4. Prevalence of Obesity
We included 12 studies reporting data on obesity in the present meta-analysis, with a total of 136,710 subjects [10,17,37,38,41,42,44,46,48,51,53,54]. In selected studies, obesity prevalence varied widely, ranging from 8.55% [48] to 61.08% [42]. The pooled prevalence for obesity was 18.60% (95% CI: 13.24% to 25.48%, I2 = 99%, p < 0.01). As for the years of publication, seven studies were published after 2013, and five studies before 2013. Regarding publication-year-specific prevalence, the combined proportion of obesity after 2013 was 15.14% (95% CI: 11.93% to 19.03%), and 23.84% (95%CI: 11.61% to 42.72%) before 2013. The magnitude of obesity before 2013 was higher than after 2013 (23.84% vs. 15.14%), but the difference was not statistically significant (p = 0.23) (Figure 5).
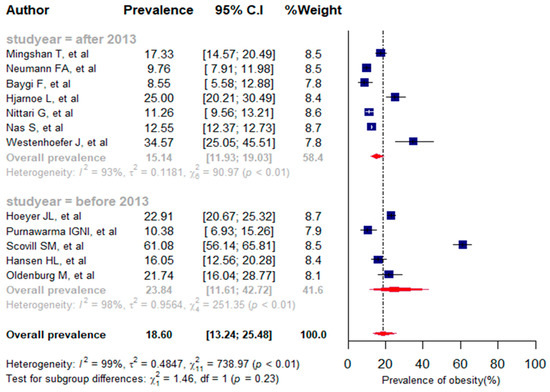
Figure 5.
A forest plot of the prevalence (%) of obesity among seafarers using a random-effects model.
Among the 12 studies included in the meta-analysis for the prevalence of obesity in seafarers, only 2 studies [37,44] reported the obesity prevalence stratified by the age group of the seafarers. As a result, the pooled prevalence of obesity among seafarers aged from 16 to 24 years was 5.10% (95%CI: 2.05% to 12.10%), and 26.74% (95%CI: 20.13% to 34.59%) in seafarers aged between 45 and 66 years (Table 2). According to these findings, obese seafarers aged 45 to 66 years had a higher prevalence, and the difference between the age groups was statistically significant as well (X2 (2) = 16.37, p < 0.001).
According to the univariate meta-regression analysis results, both sample size [QM(1) = 0.344, p = 0.557] and publication year [QM(1) = 0.280, p = 0.596] were not significantly associated with the proportion of obesity. By conducting sensitivity analysis, one outlier study was identified (Supplementary Tables S9 and S10), which influenced the pooled prevalence of obesity. After omitting the outlier study [42], the overall prevalence of obesity was found to be 15.99% (95% CI: 12.88% to 19.68%), with substantial heterogeneity between studies (I2 = 95%, p < 0.01) (Supplementary Figure S3).
3.3.5. Prevalence of Diabetes Mellitus
A total of 1519 participants were included in five studies that investigated the prevalence of diabetes mellitus [38,41,42,43,48]. The overall proportion of diabetes mellitus in the five studies included in the meta-analysis varied from 3.30% [41] to 23.08%. The pooled prevalence for diabetes mellitus was 12.70% (95%CI: 7.88% to 19.85%, I2 = 92%, p < 0.001). Among the five studies, three studies were published before 2013 and the remaining two studies were published after 2013. The combined proportion for diabetes mellitus from papers published after 2013 was 20.10% (95%CI: 15.60% to 25.51%, I2 = 63%, p < 0.01). However, the prevalence of DM before 2013 was 7.62% (95%CI: 1.84% to 26.69%, I2 = 95%, p < 0.01) (Figure 6).
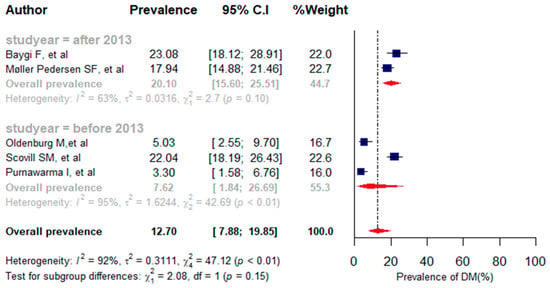
Figure 6.
A forest plot of the prevalence (%) of diabetes mellitus among seafarers using a random-effects model.
Using sensitivity analysis, one outlier study was identified (Supplementary Tables S11 and S12). After excluding the outlier study [41], the combined prevalence of diabetes mellitus (DM) was 16.84% (11.75% to 23.53%, I2 = 86%, p < 0.01) (Supplementary Figure S4). Consequently, the overall prevalence of DM was increased after omitting the outlier study.
3.3.6. Prevalence of Alcohol Consumption
A total of ten studies with 8093 participants provided data on alcohol consumption prevalence [9,38,40,43,45,46,47,49,50,52]. Overall, among the ten studies included in the meta-analysis, alcohol consumption proportion varied widely, ranging from 8.05% [40] to 82.56% [9]. A pooled prevalence of alcohol consumption was 38.56% (95%CI: 19.68% to 61.69%, I2 = 100%, p < 0.001) (Supplementary Figure S5). In terms of the publication years, seven studies were published after 2013, and three studies were published before 2013. Taking into account publication-year-specific prevalence, alcohol use prevalence after 2013 was 33.42% (95% CI: 17.11% to 54.98%), and 51.32% (95%CI: 6.48% to 94.14%) before 2013. The prevalence of alcohol use before 2013 was higher than after 2013 (51.32% vs. 33.42%), but the difference was not statistically significant (p = 0.61) (Supplementary Figure S5).
We conducted a sensitivity analysis in order to identify outliers among the included studies in the meta-analysis. The sensitivity analysis, however, did not reveal any evidence of outliers among the included studies (see Supplementary Tables S13 and S14).
3.4. Publication Bias
As for the publication bias, neither Egger’s (p = 0.690) nor Begg’s (p = 0.571) tests were statistically significant, indicating that no publication bias occurred.
4. Discussion
In the present systematic review and meta-analysis, we estimated the magnitude of CVD risk factors (smoking, high blood pressure, overweight, obesity, diabetes mellitus, and alcohol consumption) among seafarers. We synthesized the findings of 21 published studies with a total of 145,913 study participants between 1994 and 2021 that met the eligibility criteria to estimate the prevalence of major CVD risk factors. We considered the literature from 1994 and onwards in our study search, since we did not find any relevant studies on CVD risk factor prevalence before 1994 based on our preliminary search of different worldwide databases when looking for studies on seafarers. In addition, we searched for peer-reviewed studies on CVD risk factor prevalence from 1994 until 31 December 2021, in the databases we selected because this study began in January 2022. As for the methodological quality assessment of the included studies, 14.3% (n = 3), 38.1% (n = 8), and 47.6% (n = 10) of the studies were of low, medium, and high methodological quality (Table 1). Among the major CVD risk factors considered in this study, high blood pressure (HBP) was the most common risk factor (45.32%), with high and significant heterogeneity (I2 = 96%, p < 0.01). After the sensitivity analysis, HBP (44.86%) was also the main common CVD risk factor compared to the other risk factors included in this study. In a study conducted among seafarers, high blood pressure was identified as a leading cause of cardiovascular disease and accounted for 89% of all CVD diagnosed between 2010 and 2018 on board ships [57].
For the purpose of comparing the magnitude of CVD risk factors, we created two groups based on the study period (before and after 2013). The year 2013 was utilized as a cut-off point because different initiatives related to seafarers’ health were implemented or amended in 2013 and thereafter [58,59]. Therefore, we were interested in studying changes in the magnitude of common CVD risk factors over time. According to the sub-group analysis, the pooled prevalence of HBP was higher after the 2013 year of publication than before 2013 (51.74% vs. 39.02%), indicating an increase in the magnitude of HBP on board ships. After 2013, different measures were undertaken to improve the health of seafarers at sea. As an example, the 2010 International Convention on Standards of Training, Certification, and Watchkeeping for Seafarers (STCW) [58] and the 2006 Maritime Labor Convention (MLC) entered into force on 20 August 2013 [60]. The MLC 2006 outlined numerous health services for seafarers, including physical examination, health monitoring, mandatory limits on board ships, and lifestyle management. Nevertheless, CVD and its risk factors, most notably HBP, were estimated to be more prevalent among seafarers after 2013. Perhaps this is due to the ineffective implementation of measures specified by STCW 2010 and MLC 2006 in relation to the health protection of seafarers after 2013. On the other hand, the IMO, shipping companies, and other responsible bodies need to pay close attention to the implementation of the above conventions and health services for seafarers.
A study conducted on board ships reported that overweight and obesity increased, by 6.70 and 16.75 times, respectively, the risk of high blood pressure among seafarers [61]. Other studies also reported that the prevalence of high blood pressure increases with augmented body mass index, job duration at sea, working hours per week, and age of seafarers [9,62]. The application of specific interventions targeting risk factors such as weight management, limiting daily and weekly working hours in accordance with the MLC 2006 convention, and the regular monitoring and application of prevention measures targeting older seafarers would help to reduce the risk of high blood pressure on board ships.
In this study, we found overweight to be the second most prevalent modifiable risk factor for CVD in seafarers (41.67% with I2 = 85%, p < 0.01). We performed the sensitivity analysis and omitted two outlier studies among the studies included in the meta-analysis for overweight prevalence. We then re-estimated the prevalence of overweight (41.87%) and it was slightly higher than the estimated prevalence before sensitivity analysis. Based on the subgroup analysis, the prevalence of overweight was found to be higher after the 2013 year of publication compared to before 2013 (42.15% vs. 40.71%). We also stratified the proportion of overweight by age group, and accordingly the prevalence of overweight significantly increased with an increase in the age of seafarers. The results obtained are consistent with previous studies conducted among seafarers [61,62]. The possibilities of physical activity on board ships are limited due to the working conditions and the lack of access to a gymnasium on some merchant ships at sea [37]. Consequently, overweight becomes one of the most prevalent risk factors for CVD and can cause relevant health problems at sea. To reduce body weight and the likelihood of CVD, preventive measures such as nutrition management, physical training, and gyms on board ships should be considered. The popularity and diffusion of gyms are increasing on modern cargo ships. It is imperative to follow a physical activity plan under the supervision of a physician and/or trainer in order to maximize the benefits of physical activity to prevent CVDs. During the pre-employment examination, body weight and BMI should be considered as relevant recruitment criteria for seafarers.
Smoking was found to be the third most common modifiable risk factor for CVD among seafarers in the present study (40.14%). Our study demonstrated that smoking was significantly reduced after 2013 compared to years before 2013 (34.43% vs. 47.85%). This could be due to the application of certain mandatory limits related to smoking on board ships and the awareness of the consequences of smoking among seafarers after 2013. Similarly, Pougnet R and his colleagues [20] reported that smoking prevalence was significantly lower in the 2000s compared to the 1990s (45.4% vs. 61.3%, p < 0.01). We encourage applying effective preventive measures and mandatory limits for other common risk factors also, such as high blood pressure, overweight, and alcohol consumption, in order to reduce their prevalence. In general, smoking prevalence is still higher among seafarers. Mandatory limits such as prohibiting smoking in some ship areas should be enforced to reduce the proportion of this phenomenon. Health promotion interventions such as conducting smoking cessation campaigns and raising awareness of the consequences of smoking would improve the control of cigarette smoking on board ships. A study conducted on board ships indicated that level of education is significantly correlated with smoking [52]. Hence, specific campaigns directed at the people more vulnerable in this respect should be considered. Another modifiable CVD risk factor prevalent among seafarers was alcohol consumption [38.56% (95%CI: 19.68% to 61.69%)]. Pooled alcohol consumption was lower after 2013 than before 2013, although the difference was not statistically significant (33.42% vs. 51.32%, p = 0.61). This reduction in alcohol use prevalence may be attributed to the update of preventive measures for alcohol and drug abuse by the International Maritime Organization (IMO) in 2010. For example, the International Maritime Organization (IMO) updated the International Convention on Standards of Training, Certification, and Watchkeeping for Seafarers (STCW Convention) in 2010 in order to address the issue of alcohol and drug abuse among seafarers [63]. The magnitude of alcohol consumption on board is still high, and responsible bodies, including the International Maritime Organization (IMO), shipping companies, and other stakeholders, need to develop mitigation strategies to reduce the prevalence of alcohol consumption among seafarers as it is a critical safety issue that should be addressed. The IMO should also evaluate whether the amended STCW convention regarding alcohol use has been fully implemented.
Obesity and diabetes mellitus were also important risk factors for CVD among seafarers. The estimated prevalence of obesity and diabetes mellitus was 18.60% and 12.70%, respectively. However, the sensitivity analysis, after omitting outliers, showed that the combined prevalence of obesity and diabetes mellitus was 15.99% and 16.84%, respectively. We found that the prevalence of obesity increased with the increasing age of seafarers. In addition, the highest prevalence of obesity was observed among older sailors [26.74%, with significant heterogeneity between studies (I2 = 94%, p <0.001)]. Some shipping companies have taken body weight, particularly obesity, into account in their recruitment criteria. In the pre-employment examination of Danish seafarers, a BMI of 40 kg per square meter or more results in exclusion from working on board ships [64]. Norway too have introduced some limitations for the recruitment of seafarers with a BMI of 35 kg/m2 or above [37]. Obesity not only increases the risk of diabetes mellitus, high blood pressure, and the burden of CVD, but also renders seafarers unfit for work on board ships. Seafarers often experience a sedentary lifestyle on board. Consequently, it is important to encourage regular exercise, to plan physical activity and health education through telemedicine, and to provide smart offline mobile applications to guide seafarers in improving their physical activity. Lifestyle changes such as physical activity, a healthy diet, and the availability of a gymnasium on board ships could positively influence the body weight of seafarers. The prevalence of diabetes mellitus has increased in parallel with the increase in work experience at sea, age, and weekly working hours. In other words, long job duration at sea, long working hours per week, and older age increase the risk of high blood glucose levels in seafarers [62].
4.1. Strengths and Limitations
This is the first review to estimate a pooled prevalence in the context of major risk factors for cardiovascular disease among seafarers at sea. We registered this review protocol initially with the International Prospective Register of Systematic Reviews (PROSPERO) and adhered to the PRISMA guidelines when designing, conducting, and reporting our findings to ensure the validity of the methods used.
Even though most of the included studies were of a low risk of bias, this review found substantial heterogeneity among the included studies, which affected the quality of the overall evidence. Perhaps this is due to poor methodological approaches employed by the various studies. There are a few studies on the health of seafarers centered on their cardiovascular diseases, and data on CVD risk factor prevalence are in general limited. Almost all of the studies included in this review were cross-sectional and some of them had poor methodological quality. In addition, we did not find studies that stratified the prevalence of modifiable CVD risk factors by the rank, nationality, and workplace of seafarers; therefore, we did not take into consideration rank, nationality, and worksite differences in the distribution of prevalence of risk factors for CVD. The magnitude of hypercholesterolemia was not considered in this study due to a lack of studies, despite being one of the major CVD risk factors. We, therefore, encourage future studies to take into account these variables and evaluate their prevalence in a pooled analysis. Despite the above limitations, the estimated proportion of the most common risk factors of CVD is relevant for evidence-based decision making, and for the development of prevention initiatives and control strategies to mitigate the burden of CVD at sea.
4.2. Implications for Practice
Modifiable risk factors are precursors to cardiovascular disease, which results in morbidity, mortality, and the need to divert ships from their intended course at sea. Seafarers experience more cardiovascular events than the general population. Moreover, the prognosis after CVD at sea is also worse than ashore [5]. Cardiovascular diseases have received less attention among maritime seafarers in comparison to the general population, although the magnitude of cardiovascular diseases at sea is growing. However, medical emergencies on all types of ships were caused most often by cardiovascular diseases [65]. It is estimated that the shipping industry incurs approximately EUR 253 million in costs as a result of ships diverting from their courses due to medical emergencies, and the total cost for the whole shipping industry is estimated to be around EUR 760 million [66]. The average cost of a ship diverting due to medical emergencies is EUR 2200 per hour [66].
In order to improve seafarers’ health and reduce the economic and other consequences due to cardiac emergencies on board ships, modifiable risk factors should be managed. Our study is the first review reporting the pooled prevalence of modifiable risk factors, and highlighting the high prevalence of modifiable CVD risk factors among seafarers. It is also pointed out in this review that overweight and obesity are prevalent among seafarers, and this poses a safety hazard on board a ship. An overweight or obese seafarer may find it difficult to perform emergency operations such as using the emergency exits or climbing onto a rescue boat. Therefore, this review informs telemedical maritime assistance services (TMAS) physicians who provide teleconsultation services to seafarers by providing prevention advice or scheduled counseling on lifestyle changes in order to reduce modifiable risk factors, especially high body mass index. As a result, seafarers with high BMIs (25 kg/sqm and over) should be advised through telemedicine to engage in lifestyle measures, including exercise and dietary modification.
Furthermore, the results of our study alert telemedicine case managers or specially trained maritime officers who work with seafarers on board ships to monitor their blood pressure and blood glucose levels regularly. The working conditions of seafarers make monitoring regular blood pressure, blood glucose levels, and other lipid profile tests on board ships very challenging. However, thanks to telemedicine technologies, it is now possible to track seafarers’ physiological parameters regularly and report the data to the TMAS doctors. Consequently, the TMAS doctors will contact the telemedicine case manager or the person responsible for healthcare services on board, or, if possible, they will contact the user directly. A real-time consultation via telemedicine is recommended for patients with elevated blood pressure or abnormal parameters.
Moreover, our study provides information to shipping companies to implement policies prohibiting smoking because smoking is not only a health problem but also a risky habit and a cause of fires on ships. The review findings, in general, urge shipping companies, and other responsible bodies, such as the IMO, MLC, and maritime health policymakers to focus on prevention programs in order to reduce modifiable CVD risk factors on board ships. We recommend that future studies take into account the causes of the modifiable risk factors on board ships.
5. Conclusions
The present study has demonstrated that seafarers have a high prevalence of CVD risk factors, particularly high blood pressure (45.32%), overweight (41.67%), smoking (40.14%), obesity (18.60%), and alcohol consumption (38.58%). This review found substantial heterogeneity between the included studies, although most of the included studies had a low risk of bias, which affected the certainty of the overall evidence. The present study also indicated that the pooled prevalence of overweight and obesity increased along with seafarers’ age. The findings of this review will help the IMO, shipping companies, and other stakeholders to develop and implement telemedicine prevention strategies that address the common CVD risk factors considered in this study.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jpm13050861/s1, Figure S1: A forest plot of the prevalence (%) of high blood pressure among seafarers after omitting the outlier studies; Figure S2: A forest plot of the prevalence (%) of overweight among seafarers after omitting the outlier studies; Figure S3: A forest plot of the prevalence (%) of obesity among seafarers after omitting the outlier studies; Figure S4: A forest plot of the prevalence (%) of diabetes mellitus among seafarers after omitting the outlier studies; Figure S5: A forest plot of the prevalence (%) of alcohol use among seafarers using a random effect model; Table S1: Literature Search strategies and results; Table S2: The Joanna Briggs Institute (JBI) Prevalence Critical Appraisal Tool; Table S3: Leave-one-out analysis for prevalence of smoking in seafarers; Table S4: Leave-one-out diagnostics with a built-in function in smoking prevalence among seafarers; Table S5: Leave-one-out analysis for prevalence of high blood pressure in seafarers; Table S6: Leave-one-out diagnostics with a built-in function in high blood pressure among seafarers; Table S7: Leave-one-out analysis for prevalence of overweight in seafarers; Table S8: Leave-one-out diagnostics with a built-in function in overweight prevalence among seafarers; Table S9: Leave-one-out analysis for prevalence of obesity in seafarers; Table S10: Leave-one-out diagnostics with a built-in function in obesity prevalence among seafarers; Table S11: Leave-one-out analysis for prevalence of diabetes mellitus in seafarers; Table S12: Leave-one-out diagnostics with a built-in function in diabetes mellitus prevalence among seafarers; Table S13: Leave-one-out analysis for prevalence of alcohol consumption in seafarers. Table S14: Leave-one-out diagnostics with a built-in function in alcohol consumption prevalence in seafarers.
Author Contributions
G.G.S. conceived and designed the study, performed analysis, extracted data, interpreted results, selected studies, and drafted the initial manuscript. U.A., C.M., G.N., A.S. and G.B. contributed to data extraction, literature review, study selection, and to drafting the manuscript. G.R. and F.A. reviewed, guided, and approved the study. All authors have read and agreed to the final version of the manuscript.
Funding
This work was supported by Italian Ministry of Health (2021), grant number J59J21011210001, for the development of an Observatory on the Pathologies of Seafarers.
Institutional Review Board Statement
In this systematic review, all data were taken from published articles, and so no ethical approval was required.
Informed Consent Statement
Not applicable.
Data Availability Statement
All relevant data are included in the article or provided as supplementary materials. All extracted data are available upon request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Baddour, L.M.; Addolorato, G.; Ammirati, E.; Mensah, G.; Johnson, C.; Rwegerera, G.M.; Roth, G.A. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar]
- Roberts, S.E.; Jaremin, B. Cardiovascular disease mortality in British merchant shipping and among British seafarers ashore in Britain. Int. Marit. Health 2010, 62, 107–116. [Google Scholar] [PubMed]
- Grappasonni, I.; Petrelli, F.; Amenta, F. Deaths on board ships assisted by the Centro Internazionale Radio Medico in the last 25 years. Travel. Med. Infect. Dis. 2012, 10, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Hansen, H.L. Surveillance of deaths on board Danish merchant ships, 1986-93: Implications for prevention. Occup. Environ. Med. 1996, 53, 269–275. [Google Scholar] [CrossRef]
- Bogdan, J.; Kotulak, E. Myocardial infarction (MI) at the work-site among Polish seafarers. The risk and the impact of occupational factors. Int. Marit. Health 2003, 54, 26–39. [Google Scholar]
- Jaremin, B.; Kotulak, E.; Starnawska, M.; Tomaszunas, S. Causes and circumstances of deaths of polish seafarers during sea voyages. J. Travel. Med. 1996, 3, 91–95. [Google Scholar] [CrossRef]
- Roberts, S.E. Mortality from disease among seafarers in British merchant shipping (1976–1995). Int. Marit. Health 2002, 53, 43–58. [Google Scholar]
- Jensen, O.C.; Laursen, F.V.; Sørensen, F.L. International surveillance of seafarers’ health and working environment. A pilot study of the method. Preliminary report. Int. Marit. Health 2001, 52, 59–67. [Google Scholar]
- Kirkutis, A.; Norkiene, S.; Griciene, P.; Gricius, J.; Yang, S.; Gintautas, J. Prevalence of hypertension in Lithuanian mariners. Proc. West. Pharmacol. Soc. 2004, 47, 71–75. [Google Scholar]
- Hansen, H.L.; Dahl, S.; Bertelsen, B.; Brix, J. Lifestyle, nutritional status and working conditions of Danish sailors. Travel Med. Int. 1994, 12, 139–143. [Google Scholar]
- Kivimäki, M.; Kawachi, I. Work Stress as a Risk Factor for Cardiovascular Disease. Curr. Cardiol. Rep. 2015, 17, 74. [Google Scholar] [CrossRef] [PubMed]
- Sagaro, G.G.; Dicanio, M.; Battineni, G.; Samad, M.A.; Amenta, F. Incidence of occupational injuries and diseases among seafarers: A descriptive epidemiological study based on contacts from onboard ships to the Italian Telemedical Maritime Assistance Service in Rome, Italy. BMJ Open. 2021, 11, e044633. [Google Scholar] [CrossRef] [PubMed]
- Oldenburg, M.; Jensen, H.J. Stress and strain among seafarers related to the occupational groups. Int. J. Environ. Res. Public. Health 2019, 16, 1153. [Google Scholar] [CrossRef] [PubMed]
- Oldenburg, M.; Jensen, H.J.; Latza, U.; Baur, X. Seafaring stressors aboard merchant and passenger ships. Int. J. Public Health 2009, 54, 96–105. [Google Scholar] [PubMed]
- Slišković, A.; Penezić, Z. Occupational stressors, risks and health in the seafaring population. Rev. Psychol. 2016, 22, 29–39. [Google Scholar] [CrossRef]
- Oldenburg, M.; Baur, X.; Schlaich, C. Occupational Risks and Challenges of Seafaring. 2010. Available online: https://www.jstage.jst.go.jp/article/joh/advpub/0/advpub_K10004/_article/-char/ja/ (accessed on 22 November 2021).
- Hjarnoe, L.; Leppin, A. A risky occupation? (Un) healthy lifestyle behaviors among Danish seafarers. Health Promot. Int. 2014, 29, 720–729. [Google Scholar] [CrossRef]
- Filikowski, J.; Rzepiak, M.; Renke, W.; Winnicka, A.; Smolińska, D. Selected risk factors of ischemic heart disease in Polish seafarers. Preliminary report. Int. Marit. Health 2003, 54, 40–46. [Google Scholar]
- Geving, I.H.; Jorgensen, K.U.; Le Thi, M.S.; Sandsund, M. Physical activity levels among offshore fleet seafarers. Int. Marit. Health 2007, 58, 103–114. [Google Scholar]
- Pougnet, R.; Pougnet, L.; Loddé, B.L.; Canals-Pol, M.L.; Jegaden, D.; Lucas, D.; Dewitte, J.D. Cardiovascular risk factors in seamen and fishermen: Review of literature. Int. Marit. Health 2013, 64, 107–113. [Google Scholar]
- Stoll, E.; Püschel, K.; Harth, V.; Oldenburg, M. Prevalence of alcohol consumption among seafarers and fishermen. Int. Marit. Health 2020, 71, 265–274. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of Observational Studies in Epidemiology: A Proposal for Reporting. JAMA 2000, 283, 2008–2012. [Google Scholar]
- Munn, Z.; Moola, S.; Riitano, D.; Lisy, K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int. J. Health Policy Manag. 2014, 3, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Kassa, G.M. Mother-to-child transmission of HIV infection and its associated factors in Ethiopia: A systematic review and meta-analysis. BMC Infect. Dis. 2018, 18, 216. [Google Scholar] [CrossRef] [PubMed]
- Kassa, G.M.; Abajobir, A.A. Prevalence of common mental illnesses in Ethiopia: A systematic review and meta-analysis. Neurol. Psychiatry Brain Res. 2018, 30, 74–85. [Google Scholar]
- R Core Team, R. R: A Language and Environment for Statistical; Computing Foundation for Statistical Computing: Vienna, Austria, 2013. [Google Scholar]
- Balduzzi, S.; Rücker, G.; Schwarzer, G. How to perform a meta-analysis with R: A practical tutorial. Evid. Based Ment. Health 2019, 22, 153–160. [Google Scholar] [CrossRef]
- Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synth. Methods 2010, 1, 97–111. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Begg, C.B.; Mazumdar, M. Operating Characteristics of a Rank Correlation Test for Publication Bias. Biometrics 1994, 50, 1088. [Google Scholar] [CrossRef]
- Cochran, W.G. The Combination of Estimates from Different Experiments. Biometrics 2016, 10, 101–129. [Google Scholar] [CrossRef]
- Grant, J.; Hunter, A. Measuring inconsistency in knowledgebases. J. Intell. Inf. Syst. 2006, 27, 159–184. [Google Scholar] [CrossRef]
- Goto, A.; Arah, O.A.; Goto, M.; Terauchi, Y.; Noda, M. Severe hypoglycaemia and cardiovascular disease: Systematic review and meta-analysis with bias analysis. BMJ 2013, 347, 103. [Google Scholar] [CrossRef] [PubMed]
- Hoeyer, J.L.; Hansen, H.L. Obesity among Danish seafarers. Int. Marit. Health 2005, 56, 48–55. [Google Scholar] [PubMed]
- Oldenburg, M.; Jensen, H.J.; Latza, U.; Baur, X. Coronary risks among seafarers aboard German-flagged ships. Int. Arch. Occup. Environ. Health 2008, 81, 735–741. [Google Scholar] [CrossRef]
- Fort, E.; Massardier-Pilonchery, A.; Bergeret, A. Alcohol and nicotine dependence in French seafarers. Int. Marit. Health 2009, 60, 18–28. [Google Scholar]
- Fort, E.; Massardier-Pilonchéry, A.; Bergeret, A. Psychoactive substances consumption in French fishermen and merchant seamen. Int. Arch. Occup. Environ. Health 2010, 83, 497–509. [Google Scholar] [CrossRef]
- Purnawarma Irwin, G.N.I.; Jensen, O.C.; Canals, M.L.; García Bercedo, R.; Castaños Urkullu, A. Prevalence of cardiovascular risks factors and 10 year predictions of coronary heart disease in seafarers of Pertamina shipping (Indonesia). Med. Marit. 2011, 11, 49–60. [Google Scholar]
- Scovill, S.M.; Roberts, T.K.; McCarty, D.J. Health characteristics of inland waterway merchant marine captains and pilots. Occup. Med. 2012, 62, 638–641. [Google Scholar] [CrossRef]
- Møller Pedersen, S.F.; Jepsen, J.R. The metabolic syndrome among Danish seafarers. Int. Marit. Health 2013, 64, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Nas, S.; Fışkın, R. A research on obesity among Turkish seafarers. Int. Marit. Health 2014, 65, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Aapaliya, P.; Shinde, K.; Deswal, A.K.; Mohapatra, S.; Saleem, S.; Mangal, R.; Bithu, A.; Bithu, A.S.; Maurya, S.P.; Sanadhya, S.; et al. Assessment of oral health among seafarers in Mundra Port, Kutch, Gujarat: A cross-sectional study. Int. Marit. Health 2015, 66, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Mingshan, T.; Jepsen, J.R. Hypertension among Danish Seafarers. Available online: https://journals.viamedica.pl/international_maritime_health/article/view/48265 (accessed on 11 June 2020).
- Mahdi, S.S.; Sibilio, F.; Amenta, F. Dental hygiene habits and oral health status of seafarers. Int. Marit. Health 2016, 67, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Baygi, F.; Jensen, O.C.; Qorbani, M.; Farshad, A.; Salehi, S.A.; Mohammadi-Nasrabadi, F.; Asayesh, H.; Shidfar, F. Prevalence and associated factors of cardio-metabolic risk factors in Iranian seafarers. Int. Marit. Health 2016, 67, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Gregorio, E.R., Jr.; Kobayashi, J.; Medina, J.R.C.; Simbulan, N.P. Knowledge, attitudes, and related practices of Filipino seafarers regarding cardiovascular diseases. Int. Marit. Health 2016, 67, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Sliškovíc, A.; Penezíc, Z. Lifestyle factors in Croatian seafarers as relating to health and stress on board. Work 2017, 56, 371–380. [Google Scholar] [CrossRef]
- Westenhoefer, J.; von Katzler, R.; Jensen, H.J.; Zyriax, B.C.; Jagemann, B.; Harth, V.; Oldenburg, M. Cultural differences in food and shape related attitudes and eating behavior are associated with differences of Body Mass Index in the same food environment: Cross-sectional results from the Seafarer Nutrition Study of Kiribati and European seafarers on merchant ships. BMC Obes. 2018, 5, 1. [Google Scholar] [CrossRef]
- Grappasonni, I.; Scuri, S.; Petrelli, F.; Nguyen, C.T.T.; Sibilio, F.; Di Canio, M.; Samad, M.A.; Amenta, F. Survey on smoking habits among seafarers. Acta Biomed. 2019, 90, 497–505. [Google Scholar]
- Nittari, G.; Tomassoni, D.; Di Canio, M.; Traini, E.; Pirillo, I.; Minciacchi, A.; Amenta, F. Overweight among seafarers working on board merchant ships. BMC Public Health 2019, 19, 45. [Google Scholar] [CrossRef]
- Neumann, F.A.; Belz, L.; Dengler, D.; Harth, V.; von Münster, T.; Westenhöfer, J.; Oldenburg, M.; Zyriax, B.C. Eating behaviour and weight development of European and Asian seafarers during stay on board and at home. J. Occup. Med. Toxicol. 2021, 16, 41. [Google Scholar] [CrossRef] [PubMed]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L., Jr.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.T., Jr.; et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003, 42, 1206–1252. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity: Preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ.—Tech. Rep. Ser. 2000, 894, 252. [Google Scholar]
- Sagaro, G.G.; Battineni, G.; Di Canio, M.; Minciacchi, A.; Nittari, G.; Amenta, F. A descriptive epidemiological study of cardiovascular diseases among seafarers. Int. Marit. Health 2021, 72, 252–258. [Google Scholar] [CrossRef]
- The International Convention on Standards of Training, Certification and Watchkeeping for Seafarers (STCW). International Convention on Standards of Training, Certification and Watchkeeping for Seafarers (STCW). 1978. Available online: https://www.imo.org/en/About/Conventions/Pages/International-Convention-on-Standards-of-Training,-Certification-and-Watchkeeping-for-Seafarers-(STCW).aspx (accessed on 25 October 2021).
- ILO Labour Convention. Convention MLC, 2006—Maritime Labour Convention, 2006 (MLC, 2006). 2006. Available online: https://www.ilo.org/dyn/normlex/en/f?p=NORMLEXPUB:12100:0::NO::P12100_ILO_CODE:C186 (accessed on 29 May 2020).
- ILO Labour Convention. Health Protection and Medical Care (Seafarers) Convention, 2006 (No. 164). 2006. Available online: https://www.ilo.org/dyn/normlex/en/f?p=1000:12100:::NO:12100:P12100_INSTRUMENT_ID:312309 (accessed on 6 October 2019).
- Sagaro, G.G.; Di Canio, M.; Amenta, F. Correlation between body mass index and blood pressure in seafarers. Clin. Exp. Hypertens. 2021, 43, 189–195. [Google Scholar] [CrossRef]
- Sagaro, G.G.; Battineni, G.; Di Canio, M.; Amenta, F. Self-reported modifiable risk factors of cardiovascular disease among seafarers: A cross-sectional study of prevalence and clustering. J. Pers. Med. 2021, 11, 512. [Google Scholar] [CrossRef]
- The International Convention on Standards of Training, Certification and Watchkeeping for Seafarers (STCW). Stcw a Guide For Seafarers Taking into Account the 2010 Manila Amendments. Available online: https://www.mptusa.com/pdf/STCW_guide_english.pdf (accessed on 8 May 2023).
- Hansen, H.L.; Hjarnoe, L.; Jepsen, J.R. Obesity continues to be a major health risk for Danish seafarers and fishermen. Int. Marit. Health 2011, 62, 98–103. [Google Scholar]
- Oldenburg, M.; Rieger, J.; Sevenich, C.; Harth, V. Nautical officers at sea: Emergency experience and need for medical training. J. Occup. Med. Toxicol. 2014, 9, 19. [Google Scholar] [CrossRef]
- Henny, C.; Hartington, K.; Scott, S.; Tveiten, A.; Canals, L. The business case for telemedicine. Int. Marit. Health 2013, 64, 129–135. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).