Is the Non-Coding RNA miR-195 a Biodynamic Marker in the Pathogenesis of Head and Neck Squamous Cell Carcinoma? A Prognostic Meta-Analysis
Abstract
1. Introduction
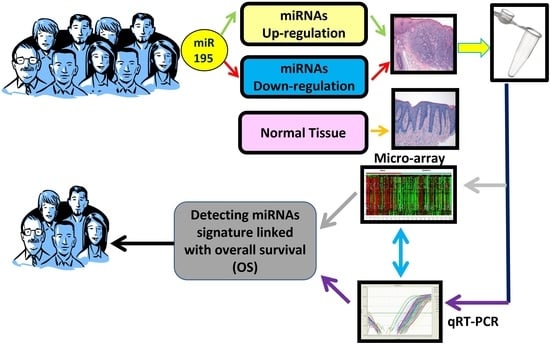
2. Materials and Methods
2.1. Protocol
2.2. Eligibility Criteria
2.3. Sources of Information, Research, and Selection
2.4. Data Collection Process and Data Characteristics
2.5. Risk of Bias in Individual Studies, Summary Measures, Summary of Results, Risk of Bias between Studies, Additional Measures
3. Results
3.1. Selection of Studies
3.2. Data Characteristics
3.3. Risk of Bias
3.4. Meta-Analysis
3.5. Risk of Bias across Study, Publication Bias, Sensitivity Analysis, Subgroup Analysis
3.6. Trial Sequential Analysis, Grade, Additional Measure
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Mathers, C.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int. J. Cancer 2019, 144, 1941–1953. [Google Scholar] [CrossRef] [PubMed]
- Shinohara, S.; Kikuchi, M.; Harada, H.; Hamaguchi, K.; Asato, R.; Tamaki, H.; Mizuta, M.; Hori, R.; Kojima, T.; Honda, K.; et al. Clinicopathological Characteristics and Survival Outcomes of Patients with Buccal Squamous Cell Carcinoma: Results of a Multi-Institutional Study. Medicina 2021, 57, 1361. [Google Scholar] [CrossRef]
- Farhat, M.C.; Dyalram, D.; Ord, R.A.; Lubek, J.E. Oral squamous cell carcinoma in patients aged 45 and younger: Prognosis, survival, and quality of life. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2021, 133, 518–525. [Google Scholar] [CrossRef] [PubMed]
- Berglund, A.; Muenyi, C.; Siegel, E.M.; Ajidahun, A.; Eschrich, S.A.; Wong, D.; Hendrick, L.E.; Putney, R.M.; Kim, S.; Hayes, D.N.; et al. Characterization of epigenomic alterations in HPV16+ head and neck squamous cell carcinomas. Cancer Epidemiol. Biomarkers Prev. 2022, 31, 858–869. [Google Scholar] [CrossRef] [PubMed]
- Muzio, L.L.; Ballini, A.; Cantore, S.; Bottalico, L.; Charitos, I.A.; Ambrosino, M.; Nocini, R.; Malcangi, A.; Dioguardi, M.; Cazzolla, A.P.; et al. Overview of Candida albicans and Human Papillomavirus (HPV) Infection Agents and their Biomolecular Mechanisms in Promoting Oral Cancer in Pediatric Patients. BioMed Res. Int. 2021, 2021, 7312611. [Google Scholar] [CrossRef]
- Bajbouj, K.; Al-Ali, A.; Ramakrishnan, R.K.; Saber-Ayad, M.; Hamid, Q. Histone Modification in NSCLC: Molecular Mechanisms and Therapeutic Targets. Int. J. Mol. Sci. 2021, 22, 11701. [Google Scholar] [CrossRef]
- Hasbullah, H.H.; Musa, M. Gene Therapy Targeting p53 and KRAS for Colorectal Cancer Treatment: A Myth or the Way Forward? Int. J. Mol. Sci. 2021, 22, 11941. [Google Scholar] [CrossRef]
- Hu, J.; Cao, J.; Topatana, W.; Juengpanich, S.; Li, S.; Zhang, B.; Shen, J.; Cai, L.; Cai, X.; Chen, M. Targeting mutant p53 for cancer therapy: Direct and indirect strategies. J. Hematol. Oncol. 2021, 14, 157. [Google Scholar] [CrossRef]
- Kasikci, Y.; Gronemeyer, H. Complexity against current cancer research—Are we on the wrong track? Int. J. Cancer 2021, 150, 1569–1578. [Google Scholar] [CrossRef]
- Liu, M.K.; Sun, X.J.; Gao, X.D.; Qian, Y.; Wang, L.; Zhao, W.L. Methylation alterations and advance of treatment in lymphoma. Front. Biosci.-Landmark 2021, 26, 602–613. [Google Scholar] [CrossRef]
- Otmani, K.; Lewalle, P. Tumor Suppressor miRNA in Cancer Cells and the Tumor Microenvironment: Mechanism of Deregulation and Clinical Implications. Front. Oncol. 2021, 11, 708765. [Google Scholar] [CrossRef] [PubMed]
- Perri, P.; Ponzoni, M.; Corrias, M.V.; Ceccherini, I.; Candiani, S.; Bachetti, T. A Focus on Regulatory Networks Linking MicroRNAs, Transcription Factors and Target Genes in Neuroblastoma. Cancers 2021, 13, 5528. [Google Scholar] [CrossRef] [PubMed]
- Limongelli, L.; Cascardi, E.; Capodiferro, S.; Favia, G.; Corsalini, M.; Tempesta, A.; Maiorano, E. Multifocal Amelanotic Melanoma of the Hard Palate: A Challenging Case. Diagnostics 2020, 10, 424. [Google Scholar] [CrossRef] [PubMed]
- Pisacane, A.; Cascardi, E.; Berrino, E.; Polidori, A.; Sarotto, I.; Casorzo, L.; Panero, M.; Boccaccio, C.; Verginelli, F.; Benvenuti, S.; et al. Real-world histopathological approach to malignancy of undefined primary origin (MUO) to diagnose cancers of unknown primary (CUPs). Virchows Arch. 2022, 8, 1–13. [Google Scholar] [CrossRef]
- Verginelli, F.; Pisacane, A.; Gambardella, G.; D’Ambrosio, A.; Candiello, E.; Ferrio, M.; Panero, M.; Casorzo, L.; Benvenuti, S.; Cascardi, E.; et al. Cancer of unknown primary stem-like cells model multi-organ metastasis and unveil liability to MEK inhibition. Nat. Commun. 2021, 12, 2498. [Google Scholar] [CrossRef]
- Jiang, M.; Liu, F.; Yang, A.-G.; Wang, W.; Zhang, R. The role of long non-coding RNAs in the pathogenesis of head and neck squamous cell carcinoma. Mol. Ther. Oncolytics 2021, 24, 127–138. [Google Scholar] [CrossRef]
- Shiiba, M.; Uzawa, K.; Tanzawa, H. MicroRNAs in Head and Neck Squamous Cell Carcinoma (HNSCC) and Oral Squamous Cell Carcinoma (OSCC). Cancers 2010, 2, 653–669. [Google Scholar] [CrossRef]
- Dioguardi, M.; Spirito, F.; Sovereto, D.; Alovisi, M.; Troiano, G.; Aiuto, R.; Garcovich, D.; Crincoli, V.; Laino, L.; Cazzolla, A.P.; et al. MicroRNA-21 Expression as a Prognostic Biomarker in Oral Cancer: Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 3396. [Google Scholar] [CrossRef]
- Dioguardi, M.; Spirito, F.; Sovereto, D.; Alovisi, M.; Aiuto, R.; Garcovich, D.; Crincoli, V.; Laino, L.; Cazzolla, A.P.; Caloro, G.A.; et al. The Prognostic Role of miR-31 in Head and Neck Squamous Cell Carcinoma: Systematic Review and Meta-Analysis with Trial Sequential Analysis. Int. J. Environ. Res. Public Health 2022, 19, 5334. [Google Scholar] [CrossRef]
- Dioguardi, M.; Spirito, F.; Sovereto, D.; La Femina, L.; Campobasso, A.; Cazzolla, A.P.; Di Cosola, M.; Zhurakivska, K.; Cantore, S.; Ballini, A.; et al. Biological Prognostic Value of miR-155 for Survival Outcome in Head and Neck Squamous Cell Carcinomas: Systematic Review, Meta-Analysis and Trial Sequential Analysis. Biology 2022, 11, 651. [Google Scholar] [CrossRef]
- Lin, X.L.; Zheng, Z.Y.; Zhang, Q.S.; Zhang, Z.; An, Y.Z. Expression of miR-195 and its target gene Bcl-2 in human intervertebral disc degeneration and their effects on nucleus pulposus cell apoptosis. J. Orthop. Surg. Res. 2021, 16, 412. [Google Scholar] [CrossRef] [PubMed]
- Sun, N.; Ye, L.; Chang, T.; Li, X.; Li, X. microRNA-195-Cdc42 axis acts as a prognostic factor of esophageal squamous cell carcinoma. Int. J. Clin. Exp. Pathol. 2014, 7, 6871–6879. [Google Scholar] [PubMed]
- Shuang, Y.; Li, C.; Zhou, X.; Huang, Y.; Zhang, L. MicroRNA-195 inhibits growth and invasion of laryngeal carcinoma cells by directly targeting DCUN1D1. Oncol. Rep. 2017, 38, 2155–2165. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann. Intern. Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Dioguardi, M.; Cantore, S.; Scacco, S.; Quarta, C.; Sovereto, D.; Spirito, F.; Alovisi, M.; Troiano, G.; Aiuto, R.; Garcovich, D.; et al. From Bench to Bedside in Precision Medicine: Diabetes Mellitus and Peri-Implantitis Clinical Indices with a Short-Term Follow-Up: A Systematic Review and Meta-Analysis. J. Pers. Med. 2022, 12, 235. [Google Scholar] [CrossRef]
- Dioguardi, M.; Cantore, S.; Sovereto, D.; La Femina, L.; Caloro, G.A.; Spirito, F.; Scacco, S.; Di Cosola, M.; Lo Muzio, L.; Troiano, G.; et al. Potential Role of miR-196a and miR-196b as Prognostic Biomarkers of Survival in Head and Neck Squamous Cell Carcinoma: A Systematic Review, Meta-Analysis and Trial Sequential Analysis. Life 2022, 12, 1269. [Google Scholar] [CrossRef]
- Dioguardi, M.; Cantore, S.; Sovereto, D.; La Femina, L.; Spirito, F.; Caloro, G.A.; Caroprese, M.; Maci, M.; Scacco, S.; Lo Muzio, L.; et al. Does miR-197 Represent a Valid Prognostic Biomarker in Head and Neck Squamous Cell Carcinoma (HNSCC)? A Systematic Review and Trial Sequential Analysis. J. Pers. Med. 2022, 12, 1436. [Google Scholar] [CrossRef]
- Tierney, J.F.; Stewart, L.A.; Ghersi, D.; Burdett, S.; Sydes, M.R. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 2007, 8, 16. [Google Scholar] [CrossRef]
- Sauerbrei, W.; Taube, S.E.; McShane, L.M.; Cavenagh, M.M.; Altman, D.G. Reporting Recommendations for Tumor Marker Prognostic Studies (REMARK): An Abridged Explanation and Elaboration. J. Natl. Cancer Inst. 2018, 110, 803–811. [Google Scholar] [CrossRef]
- Zhang, Y.; Akl, E.; Schünemann, H. Using systematic reviews in guideline development: The GRADE approach. Res. Synth. Methods 2018, 10, 312–329. [Google Scholar] [CrossRef]
- Ding, D.; Qi, Z. Clinical significance of miRNA-195 expression in patients with laryngeal carcinoma. J. BUON 2019, 24, 315–322. [Google Scholar] [PubMed]
- Jia, L.-F.; Wei, S.-B.; Gong, K.; Gan, Y.-H.; Yu, G.-Y. Prognostic implications of micoRNA miR-195 expression in human tongue squamous cell carcinoma. PloS ONE 2013, 8, e56634. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Niu, R.; Gao, S.; Zhao, F.; Dong, Z.; Zhang, H.; Li, S. Pro-Angiogenesis Role of LINC00662 from Esophageal Squamous Cell Carcinoma Cells-Derived Extracellular Vehicles. Front. Bioeng. Biotechnol. 2022, 10, 772514. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.; Xu, J.L.; Chen, W.Q.; Xu, W.X.; Song, Y.X.; Tang, W.J.; Xu, D.; Jiang, M.P.; Tang, J. Roles and mechanisms of miR-195-5p in human solid cancers. Biomed. Pharmacother. 2022, 150, 112885. [Google Scholar] [CrossRef] [PubMed]
- Riley, R.D.; Hayden, J.A.; Steyerberg, E.W.; Moons, K.G.; Abrams, K.; Kyzas, P.A.; Malats, N.; Briggs, A.; Schroter, S.; Altman, D.G.; et al. Prognosis Research Strategy (PROGRESS) 2: Prognostic factor research. PLoS Med. 2013, 10, e1001380. [Google Scholar] [CrossRef]






| First Author, Data | Country | Study Design | Number of Patients (Male, Female); Staging (I–II, III–IV) | Smoking (Y, N,) | Follow-Up Max | Tumor Type/Tumor Site | Cut-off, Median. | miR | RR miR-195 Low and High Expression (OS, PFS, CSS, DFS, RFS) |
|---|---|---|---|---|---|---|---|---|---|
| [23] Shuang et al., 2017 | China | Prospective | 122 (80, 42); S (23, 99) | 99, 23 | 60 months | LSCC | Median fold change (T/N = 0.436) | miR-195 | OS: RR 0.358 (0.134–0.959) p= 0.041 |
| [31] Ding and Qi, 2019 | China | Prospective | 182 (120, 62); S (130, 50) | / | 60 months | LSCC | Average expression level 0.76 ± 0.38 | miR-195 | OS: RR 0.3616 * (0.2409–0.5428) p = 0.0001 |
| [32] Jia et al., 2013 | China | Prospective | 81 (45, 36); S (48, 33) | / | 48 months | TSCC | Median fold change (T/N = 0.652) | miR-195. | OS: RR 0.322 (0.120–0.865) p = 0.025 |
| First Author, Data | Sample | Clinical Data | Marker Quantification | Prognostication | Statistics | Classical Prognostic Factors | Score |
|---|---|---|---|---|---|---|---|
| [23] Shuang et al., 2017 | 3 | 2 | 3 | 2 | 3 | 2 | 15 |
| [31] Ding and Qi, 2019 | 3 | 2 | 3 | 2 | 3 | 2 | 15 |
| [32] Jia et al.,2013 | 2 | 2 | 3 | 2 | 3 | 2 | 14 |
| Certainty Assessment | No. of Patients | Effect | Certainty | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Studies | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | miR-195 | Placebo | Relative (95% CI) | Absolute (95% CI) | |
| mir-195 HNSCC | |||||||||||
| 3 | Randomized trials | Not serious | Not serious | Not serious | Not serious | Strong association | 385 | -/0 | RR 0.36 (0.25 to 0.51) | 0 fewer per 1.000 (from 1 fewer to 0 fewer) | ⨁⨁⨁⨁High |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dioguardi, M.; Spirito, F.; Caloro, G.A.; Lo Muzio, L.; Cantore, S.; Ballini, A.; Scacco, S.; Malcangi, A.; Sembronio, S.; Cascardi, E.; et al. Is the Non-Coding RNA miR-195 a Biodynamic Marker in the Pathogenesis of Head and Neck Squamous Cell Carcinoma? A Prognostic Meta-Analysis. J. Pers. Med. 2023, 13, 275. https://doi.org/10.3390/jpm13020275
Dioguardi M, Spirito F, Caloro GA, Lo Muzio L, Cantore S, Ballini A, Scacco S, Malcangi A, Sembronio S, Cascardi E, et al. Is the Non-Coding RNA miR-195 a Biodynamic Marker in the Pathogenesis of Head and Neck Squamous Cell Carcinoma? A Prognostic Meta-Analysis. Journal of Personalized Medicine. 2023; 13(2):275. https://doi.org/10.3390/jpm13020275
Chicago/Turabian StyleDioguardi, Mario, Francesca Spirito, Giorgia Apollonia Caloro, Lorenzo Lo Muzio, Stefania Cantore, Andrea Ballini, Salvatore Scacco, Annarita Malcangi, Salvatore Sembronio, Eliano Cascardi, and et al. 2023. "Is the Non-Coding RNA miR-195 a Biodynamic Marker in the Pathogenesis of Head and Neck Squamous Cell Carcinoma? A Prognostic Meta-Analysis" Journal of Personalized Medicine 13, no. 2: 275. https://doi.org/10.3390/jpm13020275
APA StyleDioguardi, M., Spirito, F., Caloro, G. A., Lo Muzio, L., Cantore, S., Ballini, A., Scacco, S., Malcangi, A., Sembronio, S., Cascardi, E., Arrigoni, R., Di Cosola, M., & Nocini, R. (2023). Is the Non-Coding RNA miR-195 a Biodynamic Marker in the Pathogenesis of Head and Neck Squamous Cell Carcinoma? A Prognostic Meta-Analysis. Journal of Personalized Medicine, 13(2), 275. https://doi.org/10.3390/jpm13020275