“GONE WITH THE WIND”: The Transitory Effects of COVID-19 on the Gynecological System
Abstract
1. Introduction
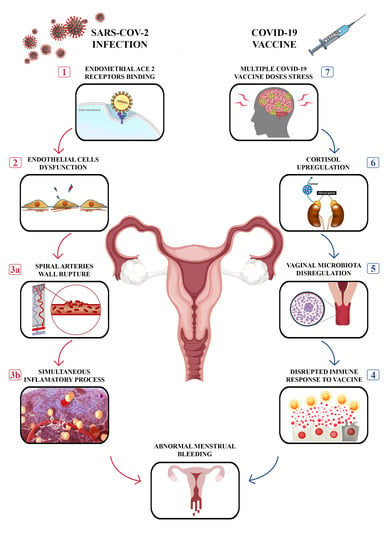
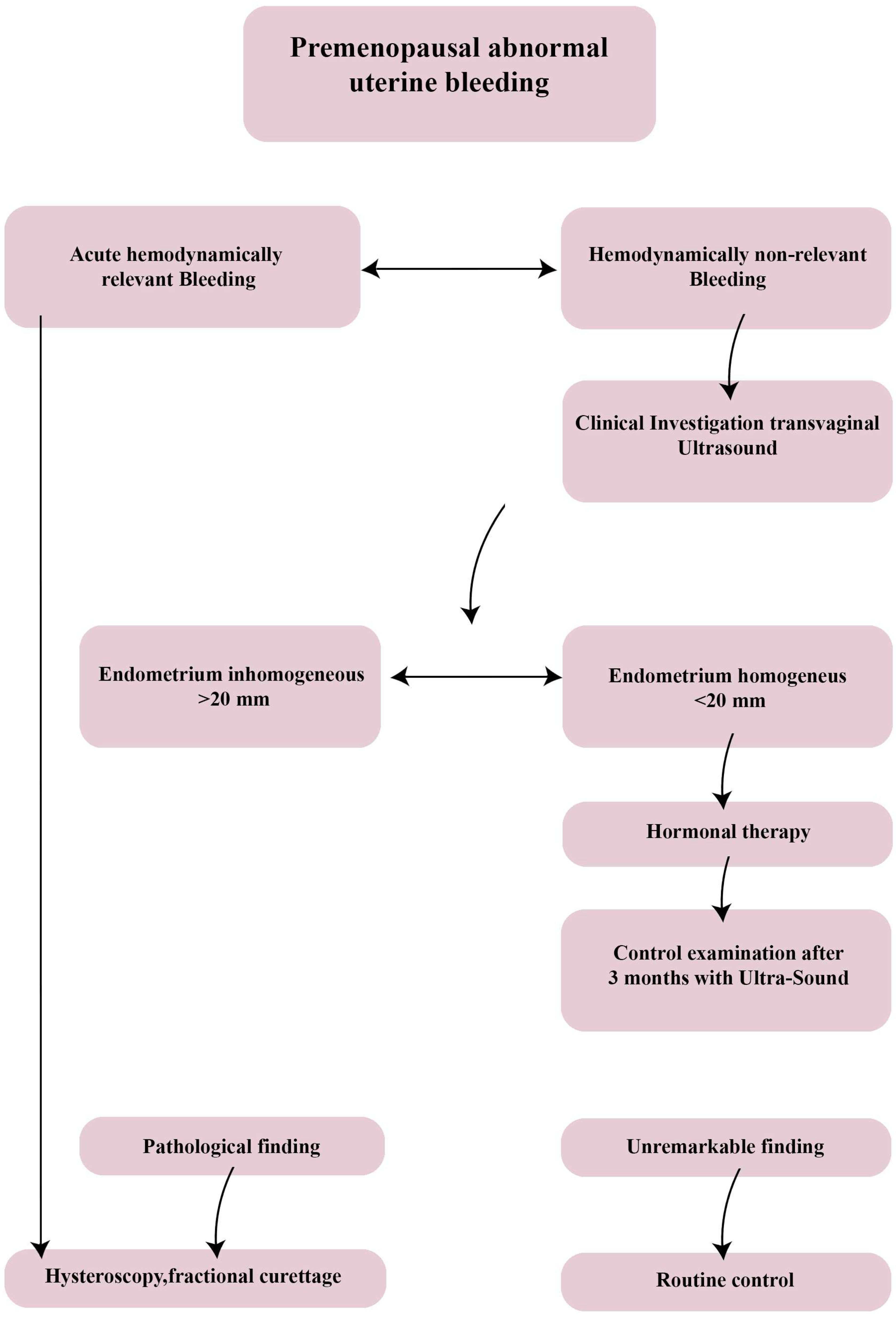
2. Premenopausal Menstrual Cycle Alterations Not COVID-19/VACCINE-Related
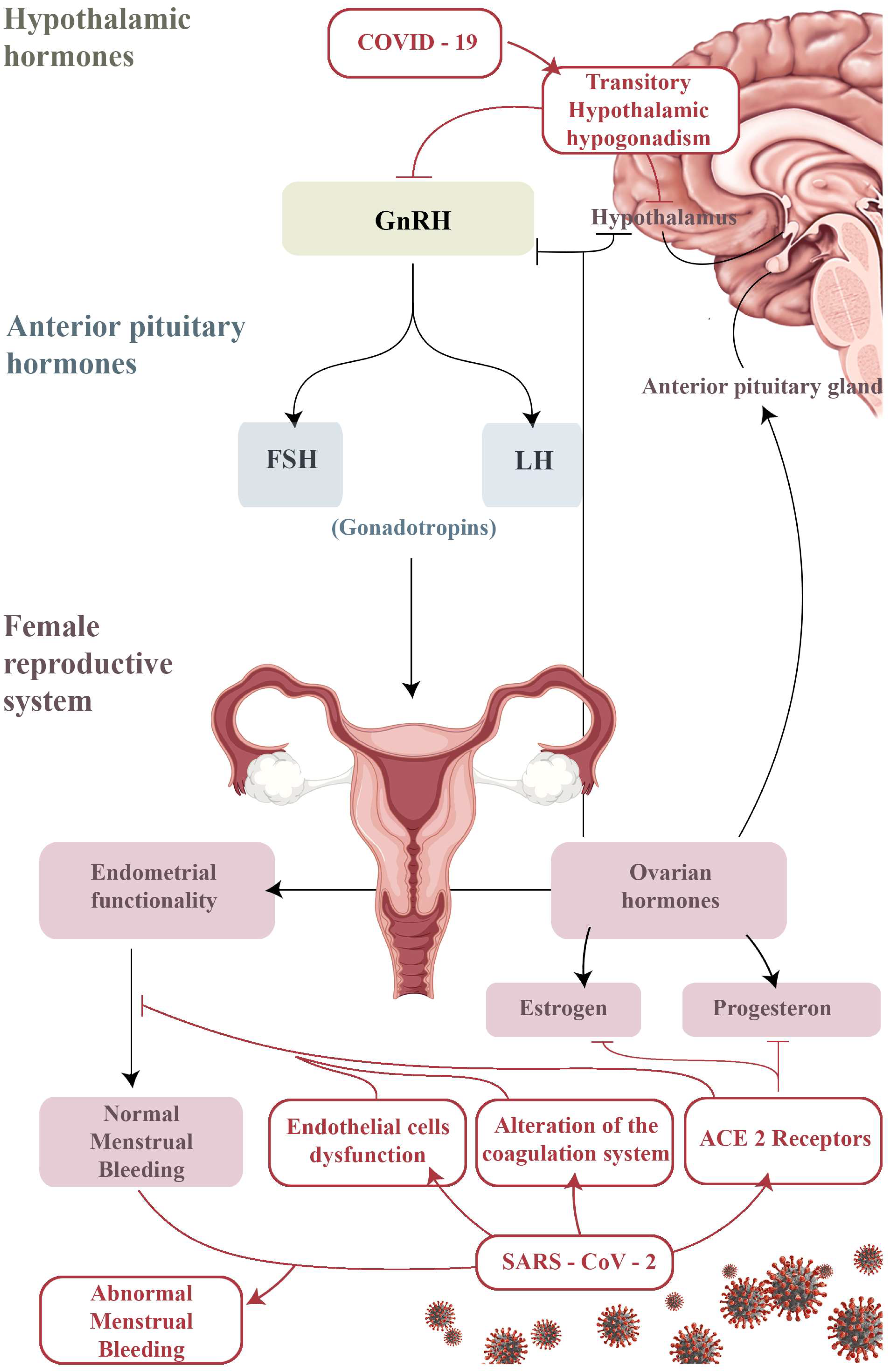
3. Alterations of the Menstrual Cycle as a Result of COVID-19 Infection
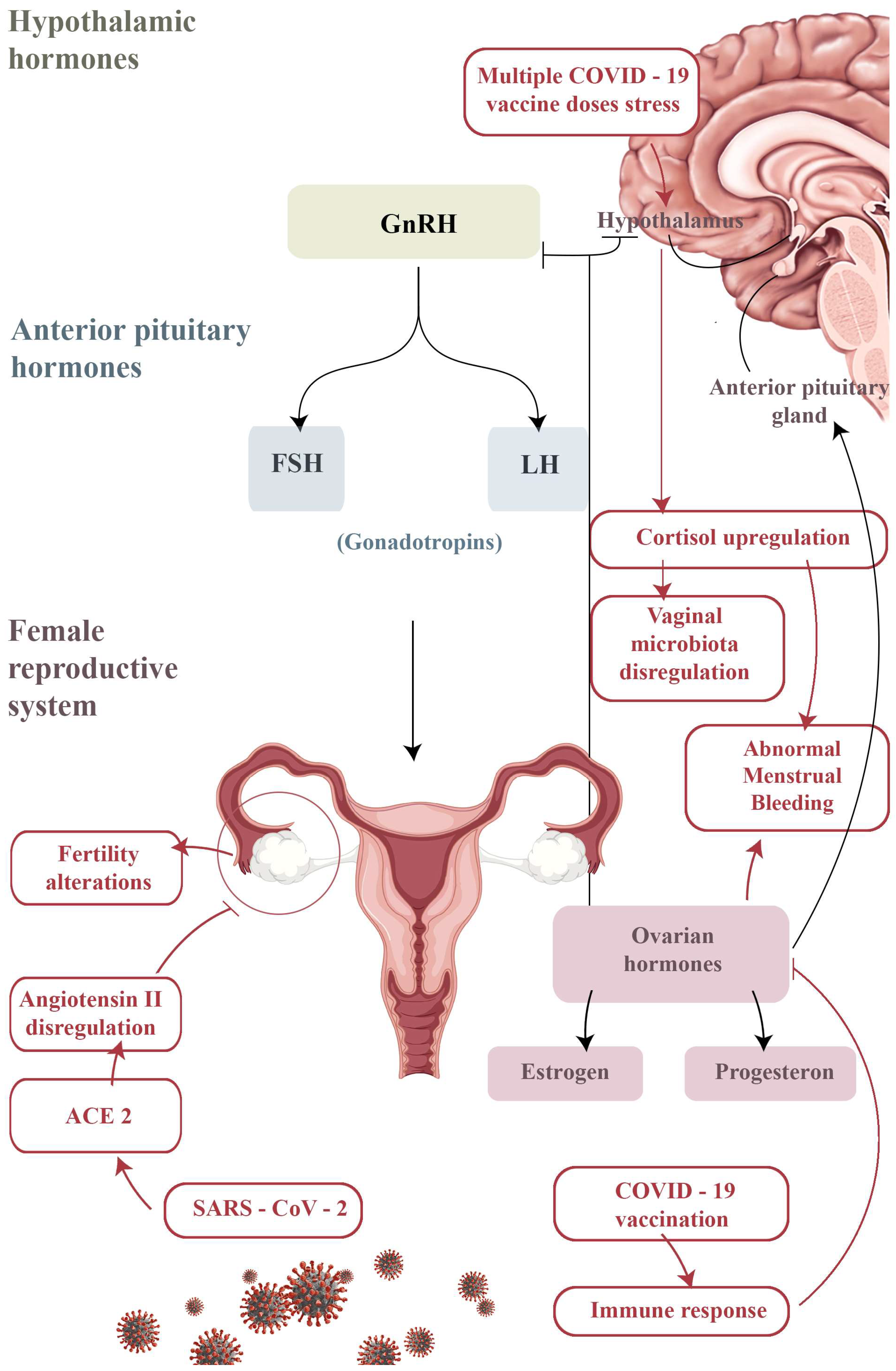
4. Alterations of the Menstrual Cycle after COVID-19 Vaccination
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jukic, A.M.Z.; Weinberg, C.R.; Wilcox, A.J.; McConnaughey, D.R.; Hornsby, P.; Baird, D.D. Accuracy of reporting of menstrual cycle length. Am. J. Epidemiol. 2008, 167, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 105906. [Google Scholar] [CrossRef] [PubMed]
- Sharp, G.C.; Fraser, A.; Sawyer, G.; Kountourides, G.; Easey, K.E.; Ford, G.; Olszewska, Z.; Howe, L.D.; Lawlor, D.A.; Alvergne, A.; et al. The COVID-19 pandemic and the menstrual cycle: Research gaps and opportunities. Int. J. Epidemiol. 2022, 51, 691–700. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Penninger, J.M.; Li, Y.; Zhong, N.; Slutsky, A.S. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: Molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020, 46, 586–590. [Google Scholar] [CrossRef]
- Ye, Q.; Wang, B.; Mao, J. The pathogenesis and treatment of the ‘Cytokine Storm’ in COVID-19. J. Infect. 2020, 80, 607–613. [Google Scholar] [CrossRef]
- Wan, Y.; Shang, J.; Graham, R.; Baric, R.S.; Li, F. Receptor Recognition by the Novel Coronavirus from Wuhan: An Analysis Based on Decade-Long Structural Studies of SARS Coronavirus. J. Virol. 2020, 94, e00127-20. [Google Scholar] [CrossRef]
- Jin, Y.; Yang, H.; Ji, W.; Wu, W.; Chen, S.; Zhang, W.; Duan, G. Virology, Epidemiology, Pathogenesis, and Control of COVID-19. Viruses 2020, 12, 372. [Google Scholar] [CrossRef]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef]
- Zheng, Y.Y.; Ma, Y.T.; Zhang, J.Y.; Xie, X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020, 17, 259–260. [Google Scholar] [CrossRef]
- Long, B.; Brady, W.J.; Koyfman, A.; Gottlieb, M. Cardiovascular complications in COVID-19. Am. J. Emerg. Med. 2020, 38, 1504–1507. [Google Scholar] [CrossRef]
- Zhang, C.; Shi, L.; Wang, F.S. Liver injury in COVID-19: Management and challenges. Lancet Gastroenterol. Hepatol. 2020, 5, 428–430. [Google Scholar] [CrossRef]
- Dellino, M.; Lamanna, B.; Vinciguerra, M.; Tafuri, S.; Stefanizzi, P.; Malvasi, A.; Di Vagno, G.; Cormio, G.; Loizzi, V.; Cazzato, G.; et al. SARS-CoV-2 Vaccines and Adverse Effects in Gynecology and Obstetrics: The First Italian Retrospective Study. Int. J. Environ. Res. Public Health 2022, 19, 13167. [Google Scholar] [CrossRef]
- Cazzato, G.; Cascardi, E.; Colagrande, A.; Foti, C.; Stellacci, A.; Marrone, M.; Ingravallo, G.; Arezzo, F.; Loizzi, V.; Solimando, A.G.; et al. SARS-CoV-2 and Skin: New Insights and Perspectives. Biomolecules 2022, 12, 1212. [Google Scholar] [CrossRef]
- Dellino, M.; Cascardi, E.; Vinciguerra, M.; Lamanna, B.; Malvasi, A.; Scacco, S.; Acquaviva, S.; Pinto, V.; Di Vagno, G.; Cormio, G.; et al. Nutrition as Personalized Medicine against SARS-CoV-2 Infections: Clinical and Oncological Options with a Specific Female Groups Overview. Int. J. Mol. Sci. 2022, 23, 9136. [Google Scholar] [CrossRef]
- Luers, J.C.; Rokohl, A.C.; Loreck, N.; Wawer Matos, P.A.; Augustin, M.; Dewald, F.; Klein, F.; Lehmann, C.; Heindl, L.M. Olfactory and Gustatory Dysfunction in Coronavirus Disease 2019 (COVID-19). Clin. Infect. Dis. 2020, 71, 2262–2264. [Google Scholar] [CrossRef]
- Wiersinga, W.J.; Rhodes, A.; Cheng, A.C.; Peacock, S.J.; Prescott, H.C. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA 2020, 324, 782–793. [Google Scholar] [CrossRef]
- Recalcati, S. Cutaneous manifestations in COVID-19: A first perspective. J. Eur. Acad. Derm. Venereol. 2020, 34, e212–e213. [Google Scholar] [CrossRef]
- Aggarwal, K.; Agarwal, A.; Jaiswal, N.; Dahiya, N.; Ahuja, A.; Mahajan, S.; Tong, L.; Duggal, M.; Singh, M.; Agrawal, R.; et al. Ocular surface manifestations of coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis. PLoS ONE 2020, 15, e0241661. [Google Scholar] [CrossRef]
- Yao, X.H.; Li, T.Y.; He, Z.C.; Ping, Y.F.; Liu, H.W.; Yu, S.C.; Mou, H.M.; Wang, L.H.; Zhang, H.R.; Fu, W.J.; et al. A pathological report of three COVID-19 cases by minimal invasive autopsies. Chin. J. Pathol. 2020, 49, 411–417. [Google Scholar] [CrossRef]
- Resta, L.; Vimercati, A.; Cazzato, G.; Fanelli, M.; Scarcella, S.V.; Ingravallo, G.; Colagrande, A.; Sablone, S.; Stolfa, M.; Arezzo, F.; et al. SARS-CoV-2, Placental Histopathology, Gravity of Infection and Immunopathology: Is There an Association? Viruses 2022, 14, 1330. [Google Scholar] [CrossRef]
- Antonella, V.; De Nola, R.; Battaglia, S.; Di Mussi, R.; Cazzato, G.; Resta, L.; Chironna, M.; Loconsole, D.; Vinci, L.; Chiarello, G.; et al. Adverse Maternal Outcomes in Pregnant Women Affected by Severe-Critical COVID-19 Illness: Correlation with Vaccination Status in the Time of Different Viral Strains’ Dominancy. Vaccines 2022, 10, 2061. [Google Scholar] [CrossRef] [PubMed]
- Charitos, I.A.; Ballini, A.; Lovero, R.; Castellaneta, F.; Colella, M.; Scacco, S.; Cantore, S.; Arrigoni, R.; Mastrangelo, F.; Dioguardi, M. Update on COVID-19 and Effectiveness of a Vaccination Campaign in a Global Context. Int. J. Environ. Res. Public Health 2022, 19, 10712. [Google Scholar] [CrossRef] [PubMed]
- Male, V. Menstrual changes after COVID-19 vaccination. BMJ 2021, 374, n2211. [Google Scholar] [CrossRef] [PubMed]
- Team, C.C.-R.; Food and Drug Administration. Allergic Reactions Including Anaphylaxis After Receipt of the First Dose of Moderna COVID-19 Vaccine—United States, December 21, 2020–January 10, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 125–129. [Google Scholar] [CrossRef]
- Rasmussen, S.A.; Kelley, C.F.; Horton, J.P.; Jamieson, D.J. Coronavirus Disease 2019 (COVID-19) Vaccines and Pregnancy: What Obstetricians Need to Know. Obs. Gynecol. 2021, 137, 408–414. [Google Scholar] [CrossRef]
- Guo, L.; Zhao, S.; Li, W.; Wang, Y.; Li, L.; Jiang, S.; Ren, W.; Yuan, Q.; Zhang, F.; Kong, F.; et al. Absence of SARS-CoV-2 in semen of a COVID-19 patient cohort. Andrology 2021, 9, 42–47. [Google Scholar] [CrossRef]
- Chao, M.; Menon, C.; Elgendi, M. Menstrual cycles during COVID-19 lockdowns: A systematic review and meta-analysis. Front. Reprod. Health 2022, 4, 949365. [Google Scholar] [CrossRef]
- Buran, G.; Gercek Oter, E. Impact of the awareness and fear of COVID-19 on menstrual symptoms in women: A cross-sectional study. Health Care Women Int. 2022, 43, 413–427. [Google Scholar] [CrossRef]
- Nguyen, B.T.; Pang, R.D.; Nelson, A.L.; Pearson, J.T.; Benhar Noccioli, E.; Reissner, H.R.; Kraker von Schwarzenfeld, A.; Acuna, J. Detecting variations in ovulation and menstruation during the COVID-19 pandemic, using real-world mobile app data. PLoS ONE 2021, 16, e0258314. [Google Scholar] [CrossRef]
- Ozimek, N.; Velez, K.; Anvari, H.; Butler, L.; Goldman, K.N.; Woitowich, N.C. Impact of Stress on Menstrual Cyclicity During the Coronavirus Disease 2019 Pandemic: A Survey Study. J. Womens Health 2022, 31, 84–90. [Google Scholar] [CrossRef]
- Phelan, N.; Behan, L.A.; Owens, L. The Impact of the COVID-19 Pandemic on Women’s Reproductive Health. Front. Endocrinol. 2021, 12, 642755. [Google Scholar] [CrossRef]
- Takmaz, T.; Gundogmus, I.; Okten, S.B.; Gunduz, A. The impact of COVID-19-related mental health issues on menstrual cycle characteristics of female healthcare providers. J. Obstet. Gynaecol. Res. 2021, 47, 3241–3249. [Google Scholar] [CrossRef]
- Maher, M.; O’Keeffe, A.; Phelan, N.; Behan, L.A.; Collier, S.; Hevey, D.; Owens, L. Female Reproductive Health Disturbance Experienced during the COVID-19 Pandemic Correlates with Mental Health Disturbance and Sleep Quality. Front. Endocrinol. 2022, 13, 434. [Google Scholar] [CrossRef]
- Edelman, A.; Boniface, E.R.; Benhar, E.; Han, L.; Matteson, K.A.; Favaro, C.; Pearson, J.T.; Darney, B.G. Association Between Menstrual Cycle Length and Coronavirus Disease 2019 (COVID-19) Vaccination: A U.S. Cohort. Obstet. Gynecol. 2022, 139, 481–489. [Google Scholar] [CrossRef]
- Lagana, A.S.; Veronesi, G.; Ghezzi, F.; Ferrario, M.M.; Cromi, A.; Bizzarri, M.; Garzon, S.; Cosentino, M. Evaluation of menstrual irregularities after COVID-19 vaccination: Results of the MECOVAC survey. Open Med. 2022, 17, 475–484. [Google Scholar] [CrossRef]
- Royal College of Obstetricians and Gynaecologists. National Heavy Menstrual Bleeding Audit. 2014. Available online: https://www.hqip.org.uk/wp-content/uploads/2018/02/HwNYNM.pdf (accessed on 1 July 2014).
- Shufelt, C.L.; Torbati, T.; Dutra, E. Hypothalamic amenorrhea and the long-term health consequences. Semin. Reprod. Med. 2017, 35, 256–262. [Google Scholar]
- Munro, M.G. Practical aspects of the two FIGO systems for management of abnormal uterine bleeding in the reproductive years. Best Pract. Res. Clin. Obstet. Gynaecol. 2017, 40, 3–22. [Google Scholar] [CrossRef]
- Care, C.A.H. Menstruation in girls and adolescents: Using the menstrual cycle as a vital sign. Obstet. Gynecol 2015, 126, e143–e146. [Google Scholar]
- Hanson, B.; Johnstone, E.; Dorais, J.; Silver, B.; Peterson, C.M.; Hotaling, J. Female infertility, infertility-associated diagnoses, and comorbidities: A review. J. Assist. Reprod. Genet. 2017, 34, 167–177. [Google Scholar] [CrossRef]
- Bertone-Johnson, E.; Ronnenberg, A.; Houghton, S.; Nobles, C.; Zagarins, S.; Takashima-Uebelhoer, B.; Faraj, J.; Whitcomb, B. Association of inflammation markers with menstrual symptom severity and premenstrual syndrome in young women. Hum. Reprod. 2014, 29, 1987–1994. [Google Scholar] [CrossRef]
- Davies, J.; Kadir, R.A. Endometrial haemostasis and menstruation. Rev. Endocr. Metab. Disord. 2012, 13, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, E.; Van Voorhis, B.J. Coronavirus Disease 2019 (COVID-19) Vaccination in Obstetrics and Gynecology: Addressing Concerns While Paving a Way Forward. Obstet. Gynecol 2022, 139, 479–480. [Google Scholar] [CrossRef] [PubMed]
- Bruinvels, G.; Goldsmith, E.; Blagrove, R.C.; Martin, D.; Shaw, L.; Piasecki, J. How lifestyle changes within the COVID-19 global pandemic have affected the pattern and symptoms of the menstrual cycle. medRxiv 2021. [Google Scholar] [CrossRef]
- Demir, O.; Sal, H.; Comba, C. Triangle of COVID, anxiety and menstrual cycle. J. Obstet. Gynaecol. 2021, 41, 1257–1261. [Google Scholar] [CrossRef] [PubMed]
- Wilson, H.W.; Amo-Addae, M.; Kenu, E.; Ilesanmi, O.S.; Ameme, D.K.; Sackey, S.O. Post-Ebola syndrome among Ebola virus disease survivors in Montserrado County, Liberia 2016. BioMed Res. Int. 2018, 2018, 1909410. [Google Scholar] [CrossRef]
- Hughes, G.C. Progesterone and autoimmune disease. Autoimmun. Rev. 2012, 11, A502–A514. [Google Scholar] [CrossRef]
- Maybin, J.A.; Critchley, H.O. Menstrual physiology: Implications for endometrial pathology and beyond. Hum. Reprod. Update 2015, 21, 748–761. [Google Scholar] [CrossRef]
- Chadchan, S.B.; Popli, P.; Maurya, V.K.; Kommagani, R. The SARS-CoV-2 receptor, angiotensin-converting enzyme 2, is required for human endometrial stromal cell decidualization. Biol. Reprod. 2021, 104, 336–343. [Google Scholar] [CrossRef]
- Kong, S.; Yan, Z.; Yuan, P.; Liu, X.; Chen, Y.; Yang, M.; Chen, W.; Song, S.; Yan, J.; Yan, L. Comprehensive evaluation of ACE2 expression in female ovary by single-cell RNA-seq analysis. BioRxiv 2021. [Google Scholar] [CrossRef]
- Alvergne, A.; Vlajic Wheeler, M.; Högqvist Tabor, V. Do sexually transmitted infections exacerbate negative premenstrual symptoms? Insights from digital health. Evol. Med. Public Health 2018, 2018, 138–150. [Google Scholar] [CrossRef]
- Teuwen, L.-A.; Geldhof, V.; Pasut, A.; Carmeliet, P. COVID-19: The vasculature unleashed. Nat. Rev. Immunol. 2020, 20, 389–391. [Google Scholar] [CrossRef]
- Alvergne, A.; Tabor, V.H. Is female health cyclical? Evolutionary perspectives on menstruation. Trends Ecol. Evol. 2018, 33, 399–414. [Google Scholar] [CrossRef]
- Davis, H.E.; Assaf, G.S.; McCorkell, L.; Wei, H.; Low, R.J.; Re’em, Y.; Redfield, S.; Austin, J.P.; Akrami, A. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 2021, 38, 101019. [Google Scholar] [CrossRef]
- Li, K.; Chen, G.; Hou, H.; Liao, Q.; Chen, J.; Bai, H.; Lee, S.; Wang, C.; Li, H.; Cheng, L. Analysis of sex hormones and menstruation in COVID-19 women of child-bearing age. Reprod. Biomed. Online 2021, 42, 260–267. [Google Scholar] [CrossRef]
- Jing, Y.; Run-Qian, L.; Hao-Ran, W.; Hao-Ran, C.; Ya-Bin, L.; Yang, G.; Fei, C. Potential influence of COVID-19/ACE2 on the female reproductive system. Mol. Hum. Reprod. 2020, 26, 367–373. [Google Scholar] [CrossRef]
- Ding, T.; Wang, T.; Zhang, J.; Cui, P.; Chen, Z.; Zhou, S.; Yuan, S.; Ma, W.; Zhang, M.; Rong, Y. Analysis of ovarian injury associated with COVID-19 disease in reproductive-aged women in Wuhan, China: An observational study. Front. Med. 2021, 8, 635255. [Google Scholar] [CrossRef]
- Iacobucci, G. COVID-19: MHRA is concerned over use of rapid lateral flow devices for mass testing. BMJ 2021, 373, n1090. [Google Scholar] [CrossRef]
- Kwong, A.S.; Pearson, R.M.; Adams, M.J.; Northstone, K.; Tilling, K.; Smith, D.; Fawns-Ritchie, C.; Bould, H.; Warne, N.; Zammit, S. Mental health before and during the COVID-19 pandemic in two longitudinal UK population cohorts. Br. J. Psychiatry 2021, 218, 334–343. [Google Scholar] [CrossRef]
- Aolymat, I. A cross-sectional study of the impact of COVID-19 on domestic violence, menstruation, genital tract health, and contraception use among women in Jordan. Am. J. Trop. Med. Hyg. 2021, 104, 519. [Google Scholar] [CrossRef]
- Morgan, E. Periods: Why women’s menstrual cycles have gone haywire. The Guardian, 25 March 2021. [Google Scholar]
- Freitas, F.D.F.; de Medeiros, A.C.Q.; Lopes, F.d.A. Effects of social distancing during the COVID-19 pandemic on anxiety and eating behavior—A longitudinal study. Front. Psychol. 2021, 12, 645754. [Google Scholar] [CrossRef]
- Ramos-Echevarría, P.M.; Soto-Soto, D.M.; Torres-Reverón, A.; Appleyard, C.B.; Akkawi, T.; Barros-Cartagena, B.D.; López-Rodríguez, V.; Castro-Figueroa, E.M.; Flores-Caldera, I. Impact of the early COVID-19 era on endometriosis patients: Symptoms, stress, and access to care. J. Endometr. Pelvic Pain Disord. 2021, 13, 111–121. [Google Scholar] [CrossRef]
- Silvestris, E.; Dellino, M.; Depalo, R. Fertility preservation in cancer patients at the time of COVID-19 pandemic. J. Gynecol. Obstet. Hum. Reprod. 2020, 49, 101910. [Google Scholar] [CrossRef] [PubMed]
- Bafunno, D.; Romito, F.; Lagattolla, F.; Delvino, V.A.; Minoia, C.; Loseto, G.; Dellino, M.; Guarini, A.; Catino, A.; Montrone, M.; et al. Psychological well-being in cancer outpatients during COVID-19. J. BUON 2021, 26, 1127–1134. [Google Scholar] [PubMed]
- Daniele, A.; Divella, R.; Pilato, B.; Tommasi, S.; Pasanisi, P.; Patruno, M.; Digennaro, M.; Minoia, C.; Dellino, M.; Pisconti, S.; et al. Can harmful lifestyle, obesity and weight changes increase the risk of breast cancer in BRCA 1 and BRCA 2 mutation carriers? A Mini review. Hered. Cancer Clin. Pract. 2021, 19, 45. [Google Scholar] [CrossRef]
- Cascardi, E.; Cazzato, G.; Daniele, A.; Silvestris, E.; Cormio, G.; Di Vagno, G.; Malvasi, A.; Loizzi, V.; Scacco, S.; Pinto, V.; et al. Association between Cervical Microbiota and HPV: Could This Be the Key to Complete Cervical Cancer Eradication? Biology 2022, 11, 1114. [Google Scholar] [CrossRef]
- Vimercati, A.; Dellino, M.; Crupano, F.M.; Gargano, G.; Cicinelli, E. Ultrasonic assessment of cesarean section scar to vesicovaginal fold distance: An instrument to estimate pre-labor uterine rupture risk. J. Matern. Fetal Neonatal Med. 2022, 35, 4370–4374. [Google Scholar] [CrossRef]
- Dellino, M.; Gargano, G.; Tinelli, R.; Carriero, C.; Minoia, C.; Tetania, S.; Silvestris, E.; Loizzi, V.; Paradiso, A.; Casamassima, P.; et al. A strengthening the reporting of observational studies in epidemiology (STROBE): Are HE4 and CA 125 suitable to detect a Paget disease of the vulva? Medicine 2021, 100, e24485. [Google Scholar] [CrossRef]
- GOV. UK. COVID-19 Vaccines: Updates for August 2021. 2021. Available online: https://www.gov.uk/drug-safety-update/covid-19-vaccines-updates-for-august-2021 (accessed on 16 August 2021).
- NIH. Item of Interest: NIH Funds Studies to Assess Potential Effects of COVID-19 Vaccination on Menstruation. 2021. Available online: https://www.nichd.nih.gov/newsroom/news/083021-COVID-19-vaccination-menstruation (accessed on 30 August 2021).
- Bentov, Y.; Beharier, O.; Moav-Zafrir, A.; Kabessa, M.; Godin, M.; Greenfield, C.S.; Ketzinel-Gilad, M.; Ash Broder, E.; Holzer, H.E.; Wolf, D. Ovarian follicular function is not altered by SARS-CoV-2 infection or BNT162b2 mRNA COVID-19 vaccination. Hum. Reprod. 2021, 36, 2506–2513. [Google Scholar] [CrossRef]
- Odeh-Natour, R.; Shapira, M.; Estrada, D.; Freimann, S.; Tal, Y.; Atzmon, Y.; Bilgory, A.; Aslih, N.; Abu-Raya, Y.S.; Shalom-Paz, E. Does mRNA SARS-CoV-2 vaccine in the follicular fluid impact follicle and oocyte performance in IVF treatments? Am. J. Reprod. Immunol. 2022, 87, e13530. [Google Scholar] [CrossRef]
- Minakshi, R.; Rahman, S.; Ayaggari, A.; Dutta, D.; Shankar, A. Understanding the Trauma of Menstrual Irregularity After COVID Vaccination: A Bird’s-Eye View of Female Immunology. Front. Immunol. 2022, 13, 906091. [Google Scholar] [CrossRef]
- Wirtz, C.; Mohamed, Y.; Engel, D.; Sidibe, A.; Holloway, M.; Bloem, P.; Kumar, S.; Brotherton, J.; Reis, V.; Morgan, C. Integrating HPV vaccination programs with enhanced cervical cancer screening and treatment, a systematic review. Vaccine 2021, 40, A116–A123. [Google Scholar] [CrossRef]
| ID | Year | Authors | Title | Study Design | Country | Age (Mean Years Range) | Sample Size |
|---|---|---|---|---|---|---|---|
| [28] | 2022 | Buran and Gercek | Impact of the awareness and fear of COVID-19 on menstrual symptoms in women: A cross-sectional study | Cross-sectional | Turkey | 27.1, 18–42 | 125 |
| [29] | 2021 | Nguyen et al. | Detecting variations in ovulation and menstruation during the COVID-19 pandemic, using real-world mobile app data | Cohort | Great Britain, United States, Sweden, other countries | 32.5, N/A | 18,076 |
| [30] | 2022 | Ozimek et al. | Impact of stress on menstrual cyclicity during the coronavirus disease 2019 pandemic: A survey study | Cohort | United States | 32.5, 18–45 | 210 |
| [31] | 2021 | Phelan et al. | The impact of the COVID-19 pandemic on women’s reproductive health | Cross-sectional | Ireland | 36.7, 15–54 | 1031 |
| [32] | 2021 | Takmaz et al. | The impact of COVID-19-related mental health issues on menstrual cycle characteristics of female healthcare providers | Cross-sectional | Turkey | 29.5, 18–40 | 952 |
| [33] | 2022 | Maher et al. | Female reproductive health disturbance experienced during the COVID-19 pandemic correlates with mental health disturbance and sleep quality | Cross-sectional | Ireland | N/A | 1335 |
| 29–38 |
| ID | Year | Authors | Title | Study Design | Country | Age (Mean Years Range) | Sample Size |
|---|---|---|---|---|---|---|---|
| [34] | 2022 | Edelman et al. | Association Between Menstrual Cycle Length and Coronavirus Disease 2019 (COVID-19) Vaccination: A U.S. Cohort | Cohort | U.S.A. | 27.1, 18–45 | 3959 |
| [35] | 2022 | Laganà et al. | Evaluation of menstrual irregularities after COVID-19 vaccination: Results of the MECOVAC survey | Survey | Italy | 35.8 | 369 |
| 18–45 | |||||||
| [12] | 2022 | Dellino et al. | SARS-CoV-2 Vaccines and Adverse Effects in Gynecology and Obstetrics: The First Italian Retrospective Study | Survey | Italy | 32.5, 18–45 | 100 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dellino, M.; Vimercati, A.; D’Amato, A.; Damiani, G.R.; Laganà, A.S.; Cicinelli, E.; Pinto, V.; Malvasi, A.; Scacco, S.; Ballini, A.; et al. “GONE WITH THE WIND”: The Transitory Effects of COVID-19 on the Gynecological System. J. Pers. Med. 2023, 13, 312. https://doi.org/10.3390/jpm13020312
Dellino M, Vimercati A, D’Amato A, Damiani GR, Laganà AS, Cicinelli E, Pinto V, Malvasi A, Scacco S, Ballini A, et al. “GONE WITH THE WIND”: The Transitory Effects of COVID-19 on the Gynecological System. Journal of Personalized Medicine. 2023; 13(2):312. https://doi.org/10.3390/jpm13020312
Chicago/Turabian StyleDellino, Miriam, Antonella Vimercati, Antonio D’Amato, Gianluca Raffaello Damiani, Antonio Simone Laganà, Ettore Cicinelli, Vincenzo Pinto, Antonio Malvasi, Salvatore Scacco, Andrea Ballini, and et al. 2023. "“GONE WITH THE WIND”: The Transitory Effects of COVID-19 on the Gynecological System" Journal of Personalized Medicine 13, no. 2: 312. https://doi.org/10.3390/jpm13020312
APA StyleDellino, M., Vimercati, A., D’Amato, A., Damiani, G. R., Laganà, A. S., Cicinelli, E., Pinto, V., Malvasi, A., Scacco, S., Ballini, A., Resta, L., Ingravallo, G., Maiorano, E., Cazzato, G., & Cascardi, E. (2023). “GONE WITH THE WIND”: The Transitory Effects of COVID-19 on the Gynecological System. Journal of Personalized Medicine, 13(2), 312. https://doi.org/10.3390/jpm13020312