Prospective Evaluation of Two Wall Orbital Fractures Involving the Medial Orbital Wall: PSI Reconstruction versus PDS Repair—Worth the Effort?
Abstract
1. Introduction
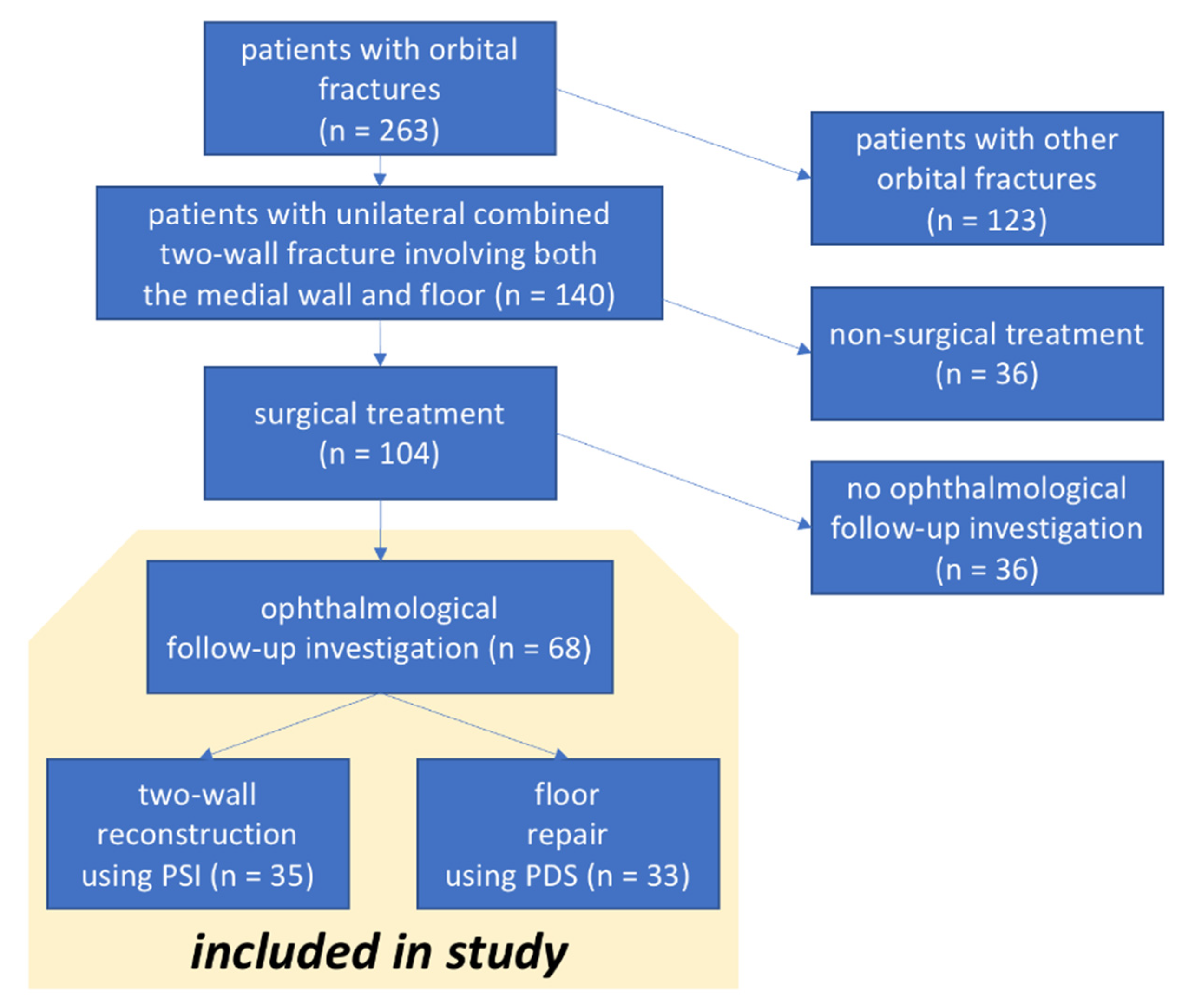
2. Materials and Methods
2.1. Study Protocol
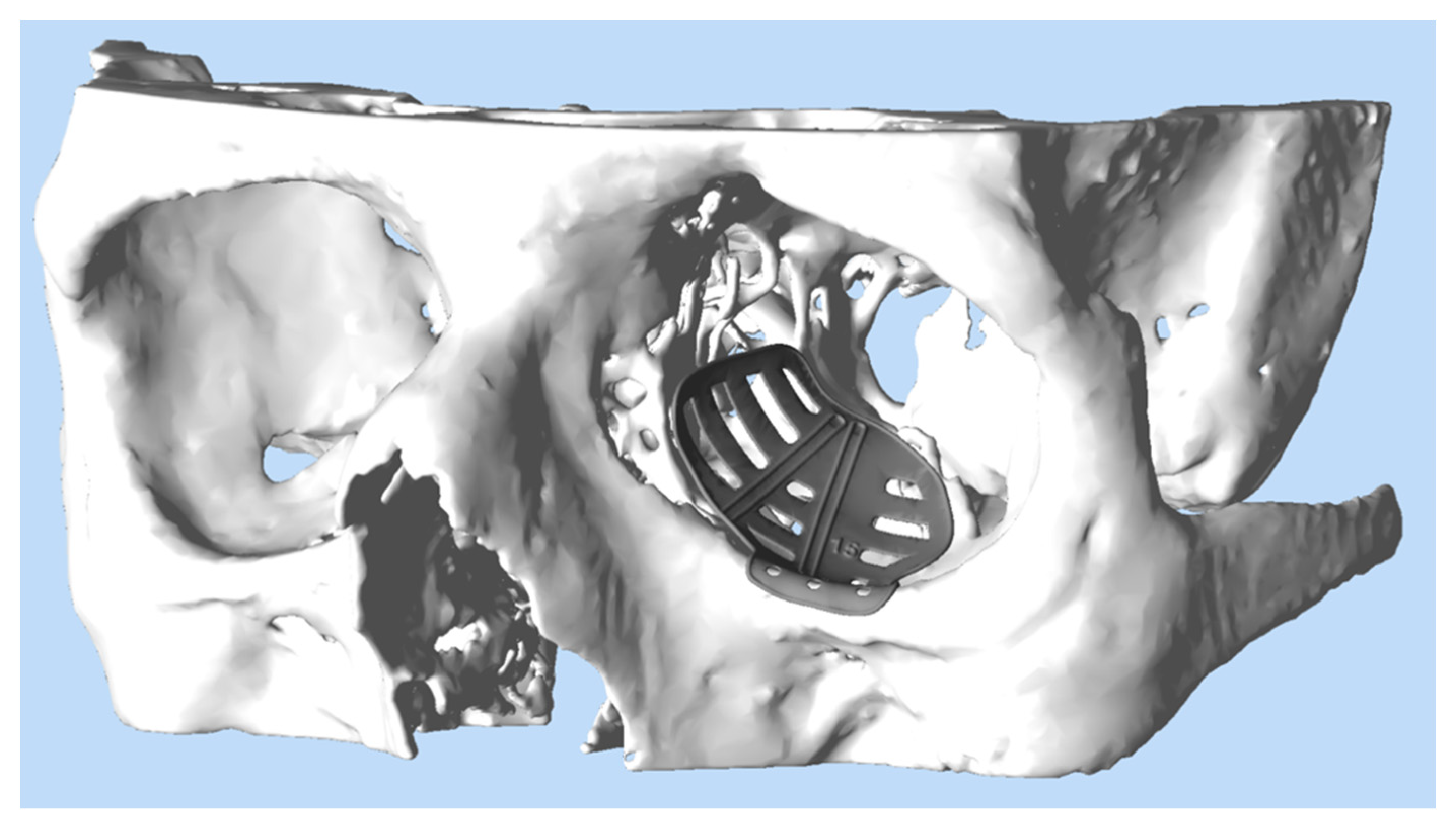
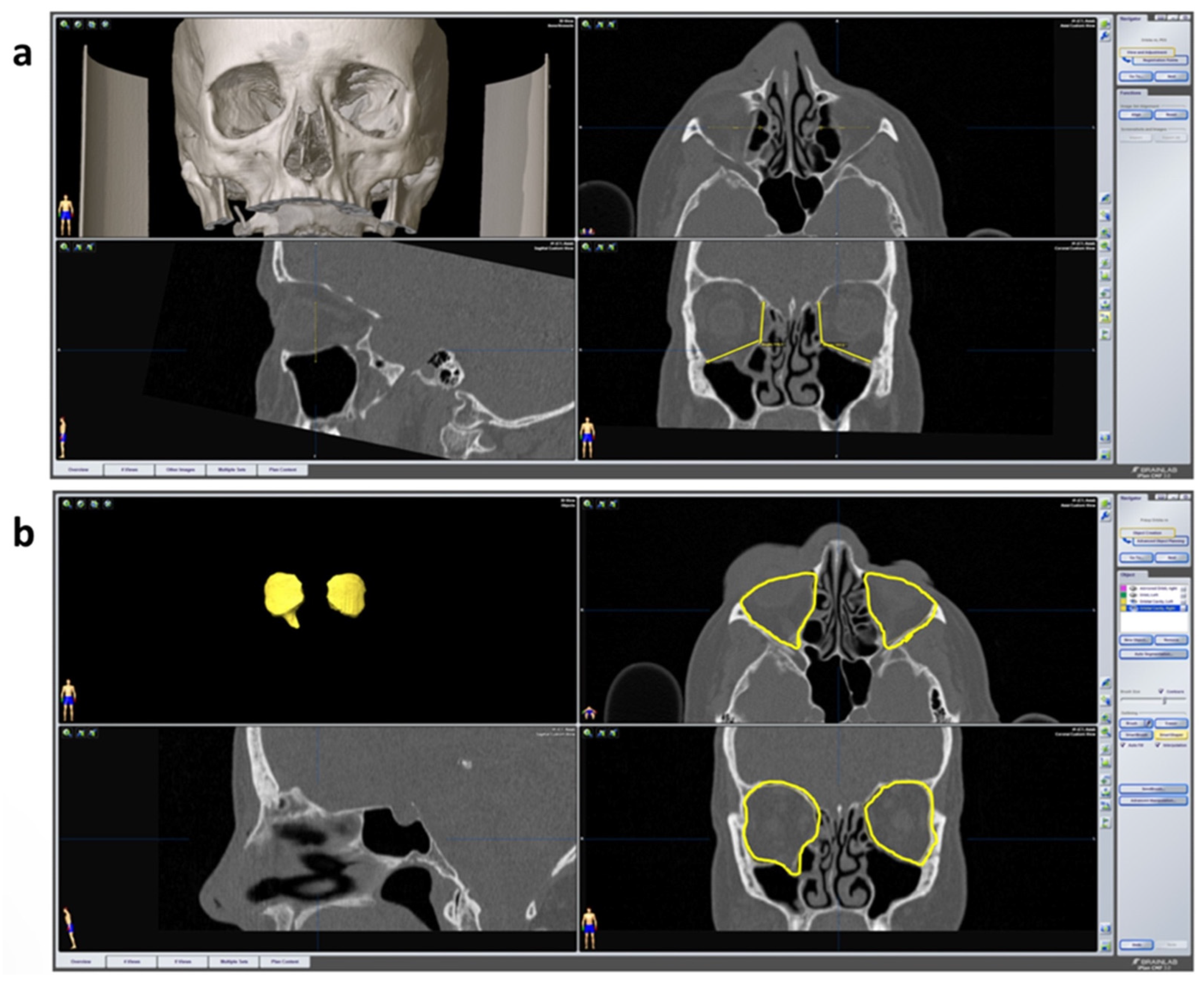
2.2. Work Flow for Orbital Reconstruction with A Patient-Specific Implant
2.3. Work Flow for Orbital Reconstruction with a PDS Foil
2.4. Ophthalmological Examination
2.5. 3D-Data Evaluation
2.6. Statistical Analysis
3. Results
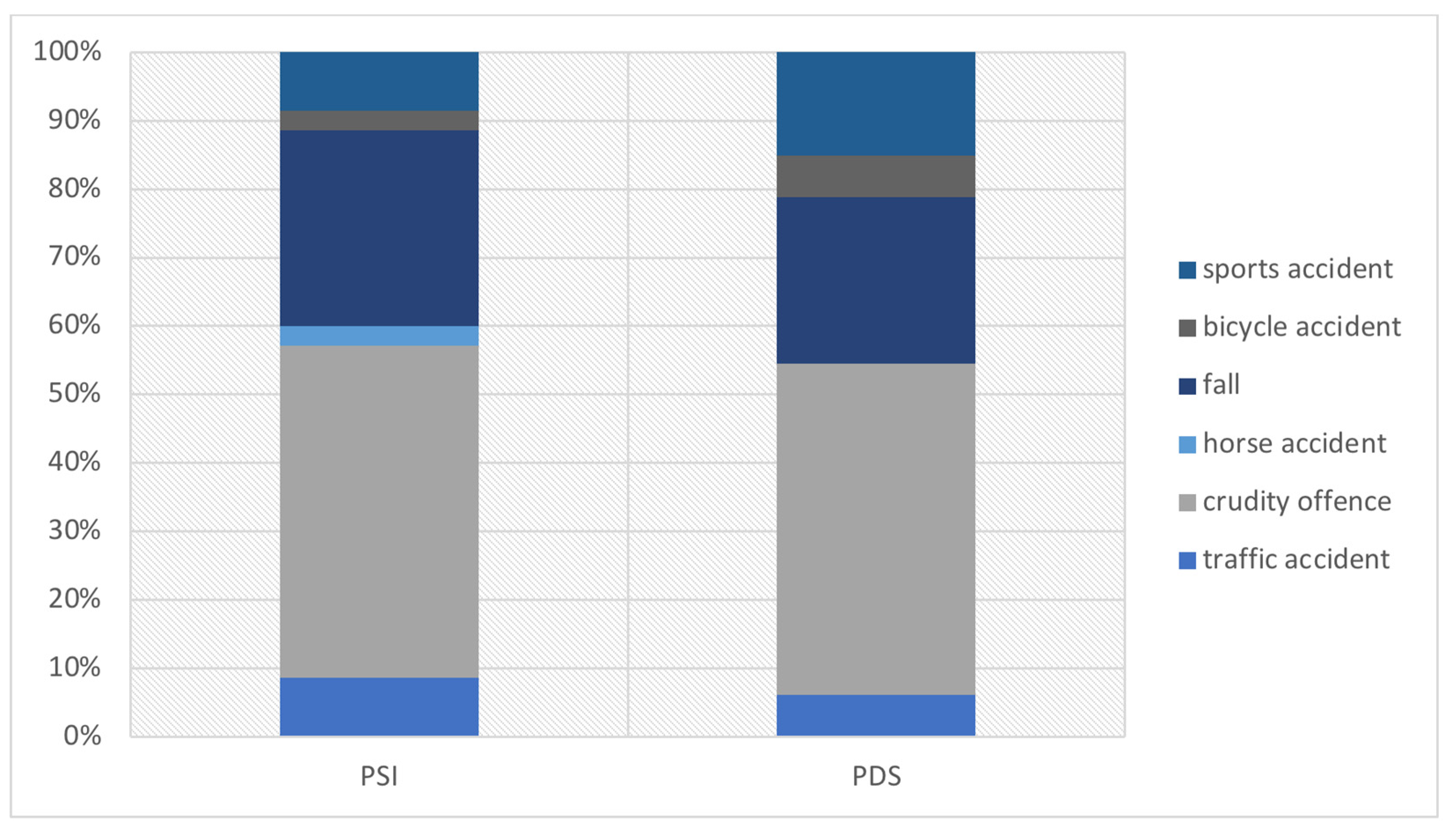
3.1. Demographic
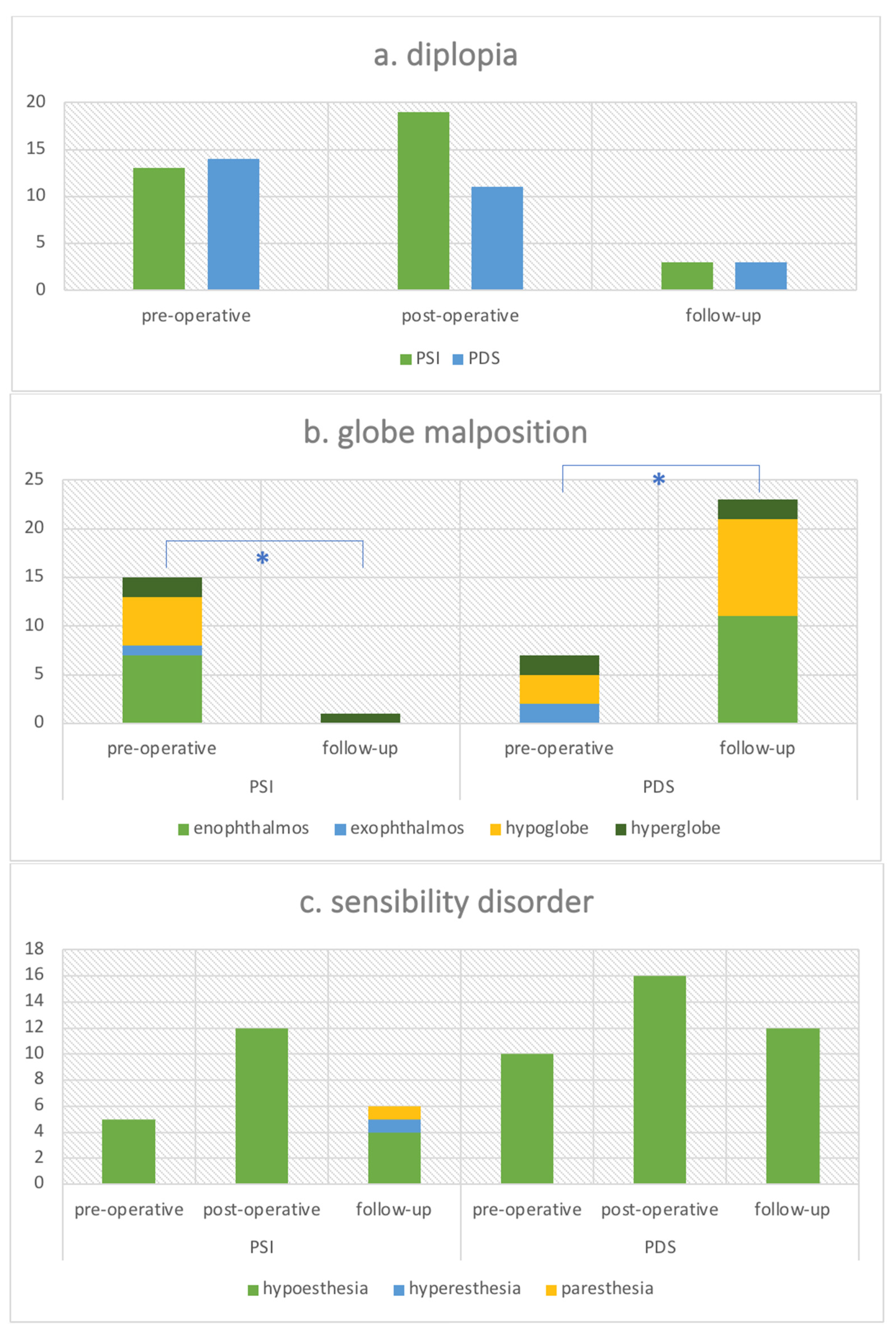
3.2. Clinical Parameters
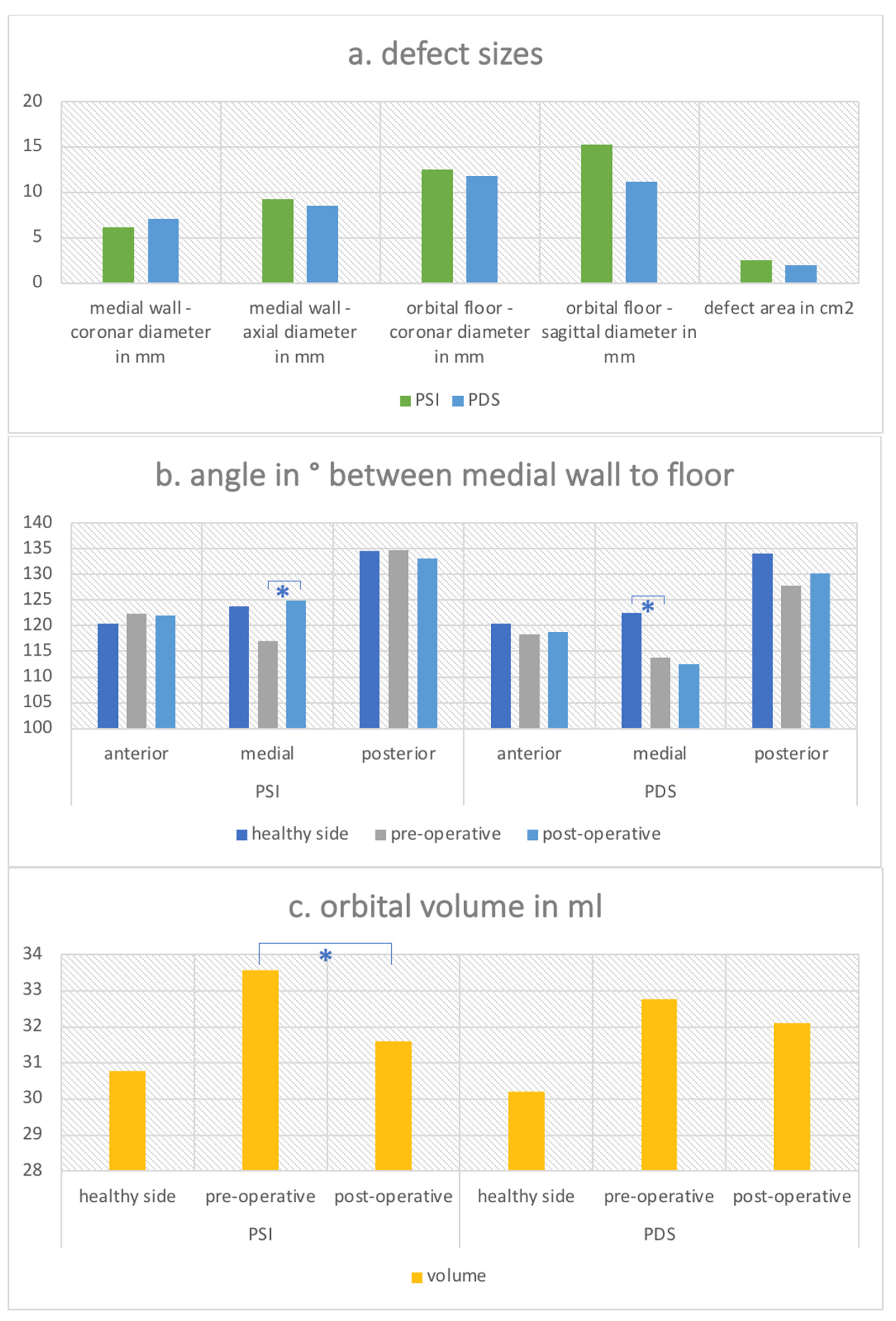
3.3. Radiological Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alafaleq, M.; Roul-Yvonnet, F.; Schouman, T.; Goudot, P. A Retrospective Study of Pure Medial Orbital Wall Fracture Management. J. Français D’ophtalmol. 2019, 42, 592–596. [Google Scholar] [CrossRef]
- Kunz, C.; Sigron, G.R.; Jaquiéry, C. Functional Outcome after Non-Surgical Management of Orbital Fractures-the Bias of Decision-Making According to Size of Defect: Critical Review of 48 Patients. Br. J. Oral Maxillofac. Surg. 2013, 51, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Cornelius, C.-P.; Stiebler, T.; Mayer, P.; Smolka, W.; Kunz, C.; Hammer, B.; Jaquiéry, C.C.; Buitrago-Téllez, C.; Leiggener, C.S.; Metzger, M.C.; et al. Prediction of Surface Area Size in Orbital Floor and Medial Orbital Wall Fractures Based on Topographical Subregions. J. Cranio-Maxillofac. Surg. 2021, 49, 598–612. [Google Scholar] [CrossRef]
- Osguthorpe, J.D. Orbital Wall Fractures: Evaluation and Management. Otolaryngol. Head Neck Surg. 1991, 105, 702–707. [Google Scholar] [CrossRef]
- Dubois, L.; Steenen, S.A.; Gooris, P.J.J.; Mourits, M.P.; Becking, A.G. Controversies in Orbital Reconstruction—I. Defect-Driven Orbital Reconstruction: A Systematic Review. Int. J. Oral Maxillofac. Surg. 2015, 44, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Bowers, J.F. The management of Blow-out fracture of the orbital floor. Surv. Ophthalmol. 1964, 9, 237–243. [Google Scholar] [PubMed]
- Emery, J.M.; Noorden, G.K.; Sclernitzauer, D.A. Orbital Floor Fractures: Long-Term Follow-up of Cases with and without Surgical Repair. Trans. Am. Acad. Ophthalmol. Otolaryngol. 1971, 75, 802–812. [Google Scholar] [PubMed]
- Harris, G.J. Orbital Blow-out Fractures: Surgical Timing and Technique. Eye 2006, 20, 1207–1212. [Google Scholar] [CrossRef]
- Belli, E.; Matteini, C.; Mazzone, N. Evolution in Diagnosis and Repairing of Orbital Medial Wall Fractures. J. Craniofac. Surg. 2009, 20, 191–193. [Google Scholar] [CrossRef]
- Roth, A.; Desmangles, P.; Rossillion, B. Early Treatment of Secondary Muscle Restriction Due to Orbital Blow-out Fractures. J. Fr. D’ophtalmol. 1999, 22, 645–650. [Google Scholar]
- Lee, K.; Snape, L. Efficacy of Transcaruncular Approach to Reconstruct Isolated Medial Orbital Fracture. J. Maxillofac. Oral Surg. 2010, 9, 142–145. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shen, Y.-D.; Paskowitz, D.; Merbs, S.L.; Grant, M.P. Retrocaruncular Approach for the Repair of Medial Orbital Wall Fractures: An Anatomical and Clinical Study. Craniomaxillofac. Trauma Reconstr. 2015, 8, 100–104. [Google Scholar] [CrossRef] [PubMed]
- Gerbino, G.; Zavattero, E.; Viterbo, S.; Ramieri, G. Treatment of Orbital Medial Wall Fractures with Titanium Mesh Plates Using Retrocaruncular Approach: Outcomes with Different Techniques. Craniomaxillofac. Trauma Reconstr. 2015, 8, 326–333. [Google Scholar] [CrossRef] [PubMed]
- Strong, E.B.; Fuller, S.C.; Wiley, D.F.; Zumbansen, J.; Wilson, M.D.; Metzger, M.C. Preformed vs Intraoperative Bending of Titanium Mesh for Orbital Reconstruction. Otolaryngol. Head Neck Surg. 2013, 149, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Rana, M.; Chui, C.H.K.; Wagner, M.; Zimmerer, R.; Rana, M.; Gellrich, N.C. Increasing the Accuracy of Orbital Reconstruction With Selective Laser-Melted Patient-Specific Implants Combined With Intraoperative Navigation. J. Oral Maxillofac. Surg. 2015, 73, 1113–1118. [Google Scholar] [CrossRef]
- Rana, M.; Moellmann, H.L.; Schorn, L.; Lommen, J.; Rana, M.; Wilkat, M.; Hufendiek, K. Primary Orbital Reconstruction with Selective Laser Melting (SLM) of Patient-Specific Implants (PSIs): An Overview of 96 Surgically Treated Patients. J. Clin. Med. 2022, 11, 3361. [Google Scholar] [CrossRef]
- Chepurnyi, Y.; Zhukovtseva, O.; Kopchak, A.; Kanura, O. Clinical application of automated virtual orbital reconstruction for orbital fracture management with patient-specific implants: A prospective comparative study. J. Craniomaxillofac. Surg. 2022; [published online ahead of print, 2022 Jun 3]. [Google Scholar] [CrossRef]
- Burm, J.S.; Chung, C.H.; Oh, S.J. Pure Orbital Blowout Fracture: New Concepts and Importance of Medial Orbital Blowout Fracture. Plast. Reconstr. Surg. 1999, 103, 1839–1849. [Google Scholar] [CrossRef]
- Park, M.S.; Kim, Y.J.; Kim, H.; Nam, S.H.; Choi, Y.W. Prevalence of Diplopia and Extraocular Movement Limitation According to the Location of Isolated Pure Blowout Fractures. Arch. Plast. Surg. 2012, 39, 204–208. [Google Scholar] [CrossRef]
- Hossal, B.M.; Beatty, R.L. Diplopia and Enophthalmos after Surgical Repair of Blowout Fracture. Orbit 2002, 21, 27–33. [Google Scholar] [CrossRef]
- Ploder, O.; Klug, C.; Voracek, M.; Burggasser, G.; Czerny, C. Evaluation of Computer-Based Area and Volume Measurement from Coronal Computed Tomography Scans in Isolated Blowout Fractures of the Orbital Floor. J. Oral Maxillofac. Surg. 2002, 60, 1267–1272; discussion 1273–1274. [Google Scholar] [CrossRef]
- Ploder, O.; Oeckher, M.; Klug, C.; Voracek, M.; Wagner, A.; Burggasser, G.; Baumann, A.; Czerny, C. Follow-up Study of Treatment of Orbital Floor Fractures: Relation of Clinical Data and Software-Based CT-Analysis. Int. J. Oral Maxillofac. Surg. 2003, 32, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Kontio, R.; Suuronen, R.; Salonen, O.; Paukku, P.; Konttinen, Y.T.; Lindqvist, C. Effectiveness of Operative Treatment of Internal Orbital Wall Fracture with Polydioxanone Implant. Int. J. Maxillofac. Oral Surg. 2001, 30, 278–285. [Google Scholar] [CrossRef] [PubMed]
- You, J.P.; Kim, D.W.; Jeon, B.J.; Jeong, S.H.; Han, S.K.; Dhong, E.S.; Kim, W.K. Two-Year Follow-up on the Use of Absorbable Mesh Plates in the Treatment of Medial Orbital Wall Fractures. Arch. Plast. Surg. 2013, 40, 728–734. [Google Scholar] [CrossRef] [PubMed]
- Kontio, R.; Ruuttila, P.; Lindroos, L.; Suuronen, R.; Salo, A.; Lindqvist, C.; Virtanen, I.; Konttinen, Y.T. Biodegradable Polydioxanone and Poly(l/d)Lactide Implants: An Experimental Study on Peri-Implant Tissue Response. Int. J. Maxillofac. Oral Surg. 2005, 34, 766–776. [Google Scholar] [CrossRef] [PubMed]
- Baumann, A.; Burggasser, G.; Gauss, N.; Ewers, R. Orbital Floor Reconstruction with an Alloplastic Resorbable Polydioxanone Sheet. Int. J. Maxillofac. Oral Surg. 2002, 31, 367–373. [Google Scholar] [CrossRef]
- He, Y.; Zhang, Y.; Yu, G.Y.; Guo, C.B.; Shen, G.F.; Peng, X.; Liu, X.J.; Wang, J.; Zhang, W.B.; Liu, Y.P.; et al. Society Of Oral Additionally, Maxillofacial Surgery, Chinese Stomatological Association. Expert Consensus on Navigation-guided Unilateral Orbital Fracture and Orbital Floor Reconstruction Techniques. Chin. J. Dent. Res. 2020, 23, 51–55. [Google Scholar] [CrossRef]
- Bevans, S.E.; Moe, K.S. Advances in the Reconstruction of Orbital Fractures. Facial Plast. Surg. Clin. 2017, 25, 513–535. [Google Scholar] [CrossRef]
- Zimmerer, R.M.; Ellis, E.; Aniceto, G.S.; Schramm, A.; Wagner, M.E.H.; Grant, M.P.; Cornelius, C.P.; Strong, E.B.; Rana, M.; Chye, L.T.; et al. A Prospective Multicenter Study to Compare the Precision of Posttraumatic Internal Orbital Reconstruction with Standard Preformed and Individualized Orbital Implants. J. Craniomaxillofac. Surg. 2016, 44, 1485–1497. [Google Scholar] [CrossRef]
- Novelli, G.; Tonellini, G.; Mazzoleni, F.; Bozzetti, A.; Sozzi, D. Virtual Surgery Simulation in Orbital Wall Reconstruction: Integration of Surgical Navigation and Stereolithographic Models. J. Cranio-Maxillofac. Surg. 2014, 42, 2025–2034. [Google Scholar] [CrossRef]
- Cai, E.Z.; Koh, Y.P.; Hing, E.C.H.; Low, J.R.; Shen, J.Y.; Wong, H.C.; Sundar, G.; Lim, T.C. Computer-Assisted Navigational Surgery Improves Outcomes in Orbital Reconstructive Surgery. J. Craniofac. Surg. 2012, 23, 1567–1573. [Google Scholar] [CrossRef]
- Schmelzeisen, R.; Gellrich, N.C.; Schoen, R.; Gutwald, R.; Zizelmann, C.; Schramm, A. Navigation-Aided Reconstruction of Medial Orbital Wall and Floor Contour in Cranio-Maxillofacial Reconstruction. Injury 2004, 35, 955–962. [Google Scholar] [CrossRef] [PubMed]
- Gander, T.; Essig, H.; Metzler, P.; Lindhorst, D.; Dubois, L.; Rücker, M.; Schumann, P. Patient Specific Implants (PSI) in Reconstruction of Orbital Floor and Wall Fractures. J. Craniomaxillofac. Surg. 2015, 43, 126–130. [Google Scholar] [CrossRef] [PubMed]
- Schönegg, D.; Wagner, M.; Schumann, P.; Essig, H.; Seifert, B.; Rücker, M.; Gander, T. Correlation between Increased Orbital Volume and Enophthalmos and Diplopia in Patients with Fractures of the Orbital Floor or the Medial Orbital Wall. J. Cranio-Maxillofac. Surg. 2018, 46, 1544–1549. [Google Scholar] [CrossRef] [PubMed]
- Zimmerer, R.M.; Gellrich, N.C.; von Bülow, S.; Strong, E.B.; Ellis, E.; Wagner, M.E.H.; Sanchez Aniceto, G.; Schramm, A.; Grant, M.P.; Thiam Chye, L.; et al. Is There More to the Clinical Outcome in Posttraumatic Reconstruction of the Inferior and Medial Orbital Walls than Accuracy of Implant Placement and Implant Surface Contouring? A Prospective Multicenter Study to Identify Predictors of Clinical Outcome. J. Cranio-Maxillofac. Surg. 2018, 46, 578–587. [Google Scholar] [CrossRef] [PubMed]
- Gellrich, N.-C.; Schramm, A.; Hammer, B.; Rojas, S.; Cufi, D.; Lagrèze, W.; Schmelzeisen, R. Computer-Assisted Secondary Reconstruction of Unilateral Posttraumatic Orbital Deformity. Plast. Reconstr. Surg. 2002, 110, 1417–1429. [Google Scholar] [CrossRef]
- Schramm, A.; Suarez-Cunqueiro, M.M.; Rücker, M.; Kokemueller, H.; Bormann, K.H.; Metzger, M.C.; Gellrich, N.C. Computer-Assisted Therapy in Orbital and Mid-Facial Reconstructions. Int. J. Med. Robot. Comput. Assist. Surg. 2009, 5, 111–124. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilkat, M.; Hufendiek, K.; Karahisarlioglu, M.; Borrelli, M.; Sproll, C.; Rana, M. Prospective Evaluation of Two Wall Orbital Fractures Involving the Medial Orbital Wall: PSI Reconstruction versus PDS Repair—Worth the Effort? J. Pers. Med. 2022, 12, 1389. https://doi.org/10.3390/jpm12091389
Wilkat M, Hufendiek K, Karahisarlioglu M, Borrelli M, Sproll C, Rana M. Prospective Evaluation of Two Wall Orbital Fractures Involving the Medial Orbital Wall: PSI Reconstruction versus PDS Repair—Worth the Effort? Journal of Personalized Medicine. 2022; 12(9):1389. https://doi.org/10.3390/jpm12091389
Chicago/Turabian StyleWilkat, Max, Karsten Hufendiek, Merve Karahisarlioglu, Maria Borrelli, Christoph Sproll, and Majeed Rana. 2022. "Prospective Evaluation of Two Wall Orbital Fractures Involving the Medial Orbital Wall: PSI Reconstruction versus PDS Repair—Worth the Effort?" Journal of Personalized Medicine 12, no. 9: 1389. https://doi.org/10.3390/jpm12091389
APA StyleWilkat, M., Hufendiek, K., Karahisarlioglu, M., Borrelli, M., Sproll, C., & Rana, M. (2022). Prospective Evaluation of Two Wall Orbital Fractures Involving the Medial Orbital Wall: PSI Reconstruction versus PDS Repair—Worth the Effort? Journal of Personalized Medicine, 12(9), 1389. https://doi.org/10.3390/jpm12091389






