Effects of Different Orthoses on Neuromuscular Activity of Superficial and Deep Shoulder Muscles during Activities of Daily Living and Physiotherapeutic Exercises in Healthy Participants
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Design
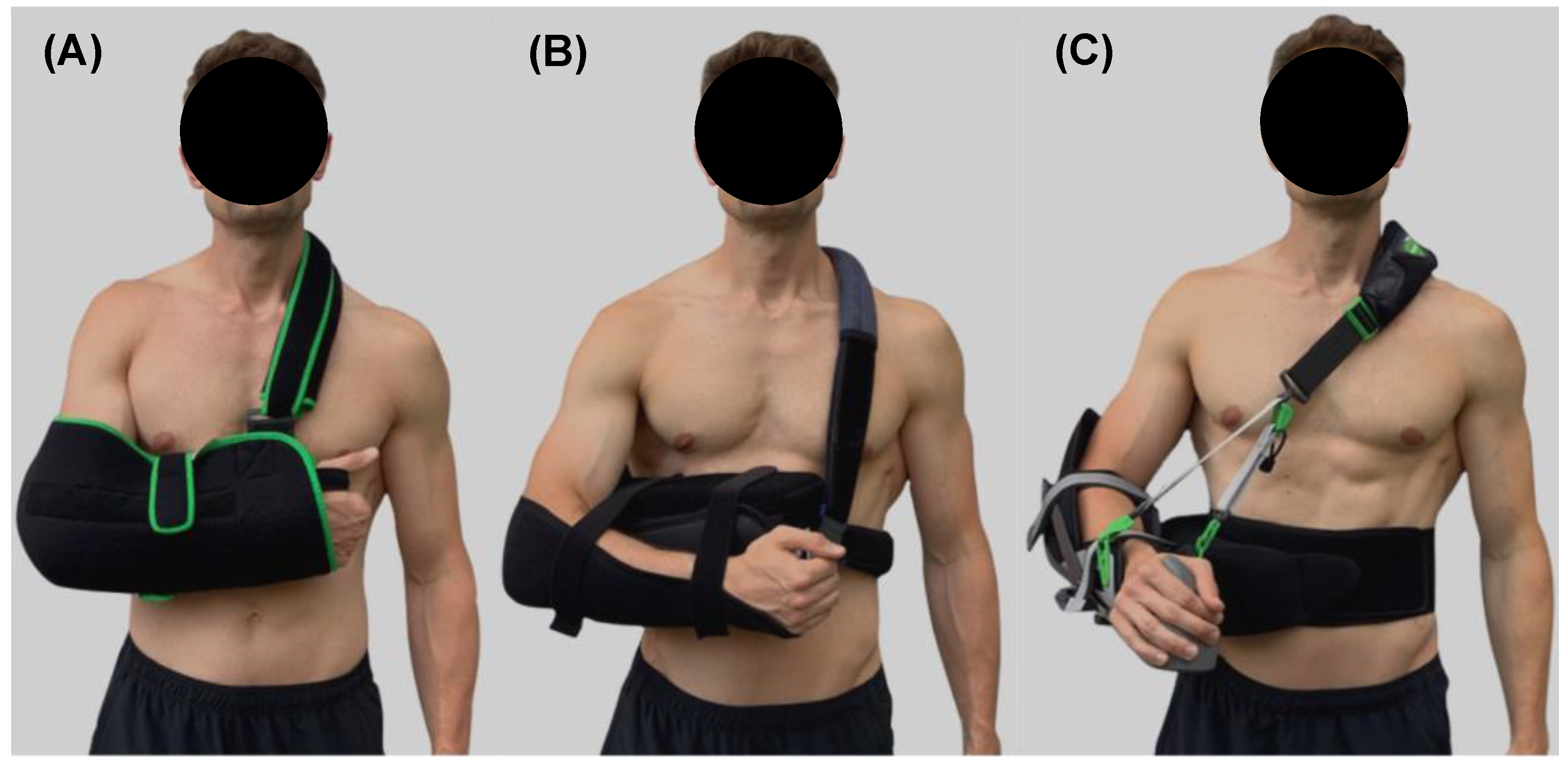
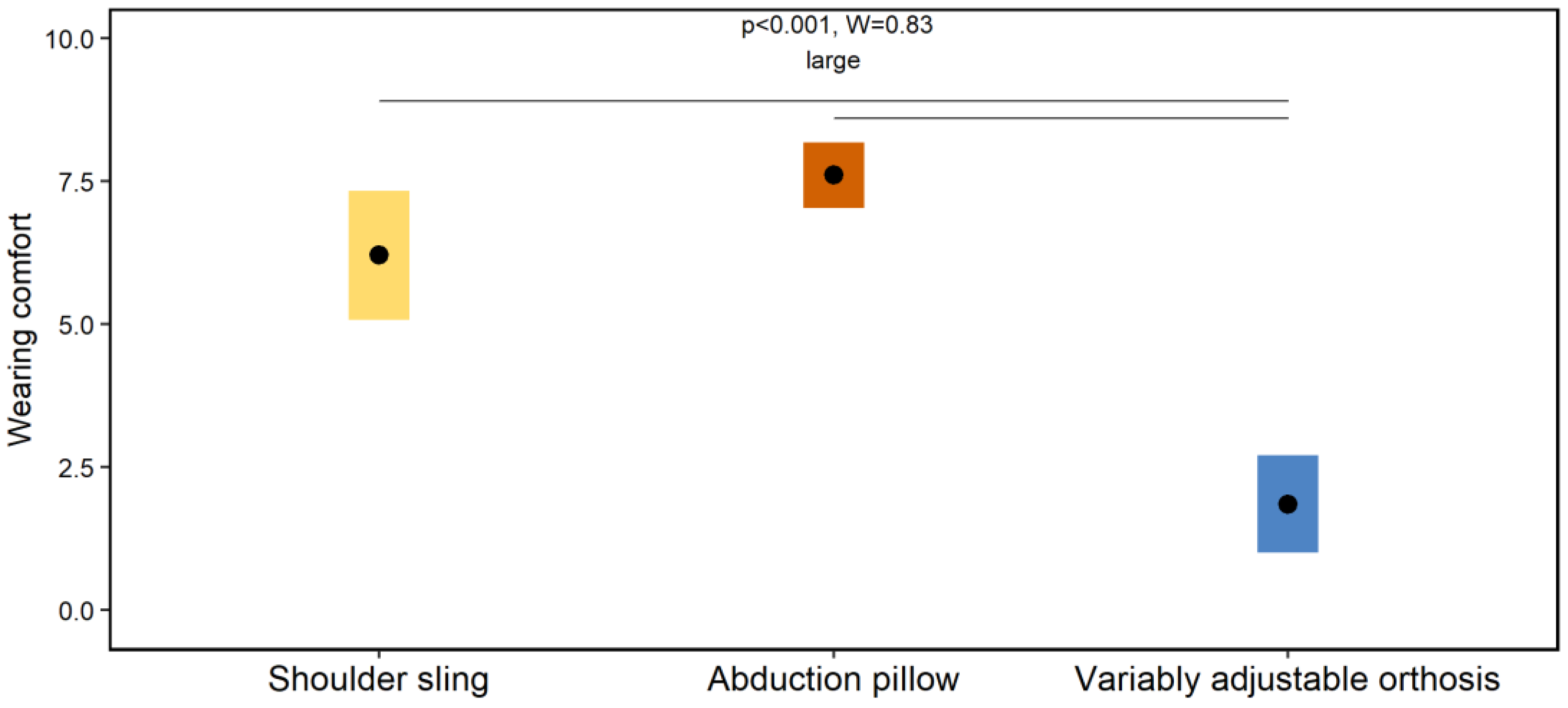
2.3. Shoulder Orthoses
2.4. Activities of Daily Living
2.4.1. Stand Up-Sit Down from a Chair
2.4.2. Open-Close a Water Bottle
2.4.3. Type the Alphabet on a Computer Keyboard
2.4.4. Put On-Take Off a Jacket
2.4.5. Lie Down-Stand Up on a Couch
2.4.6. Walk Slowly over a Short Distance
2.4.7. Put On-Take Off an Orthosis
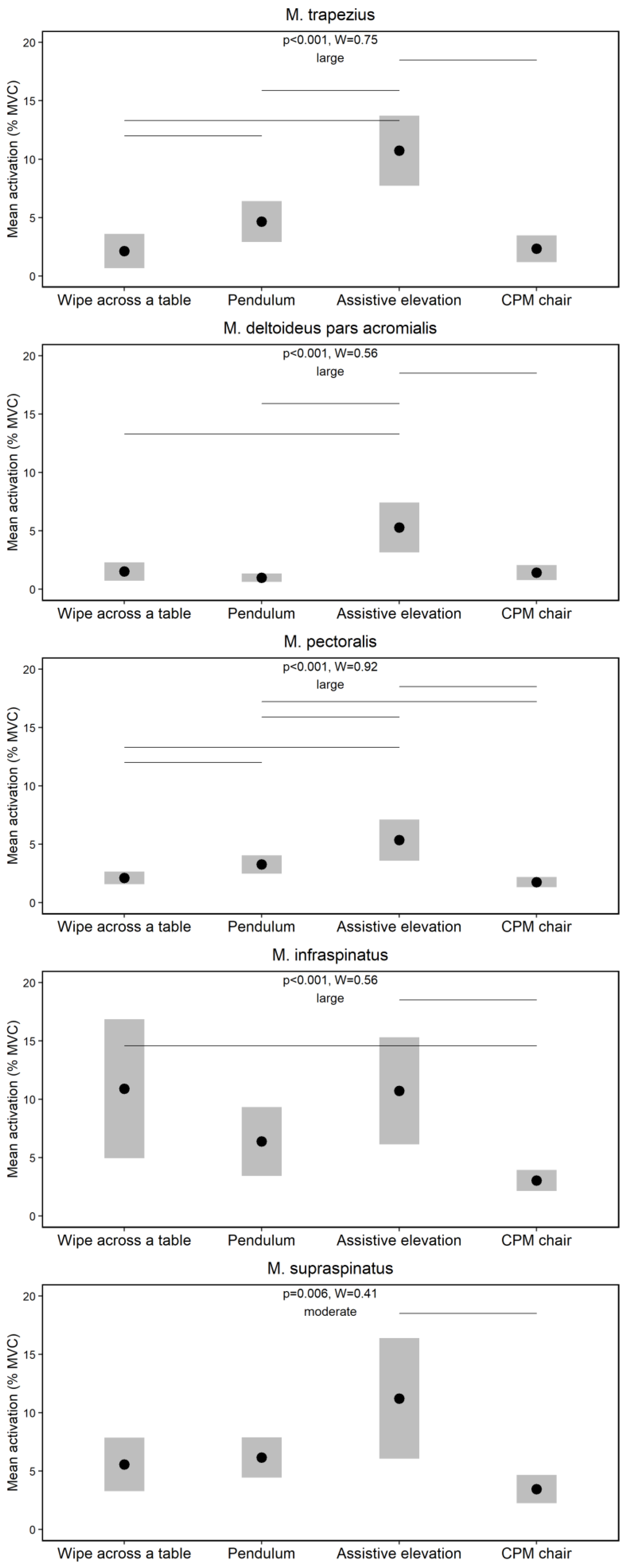
2.5. Physiotherapeutic Exercises
2.5.1. Wipe across a Table
2.5.2. Pendulum
2.5.3. Assistive Elevation
2.5.4. Continuous Passive Motion
2.6. Data Collection
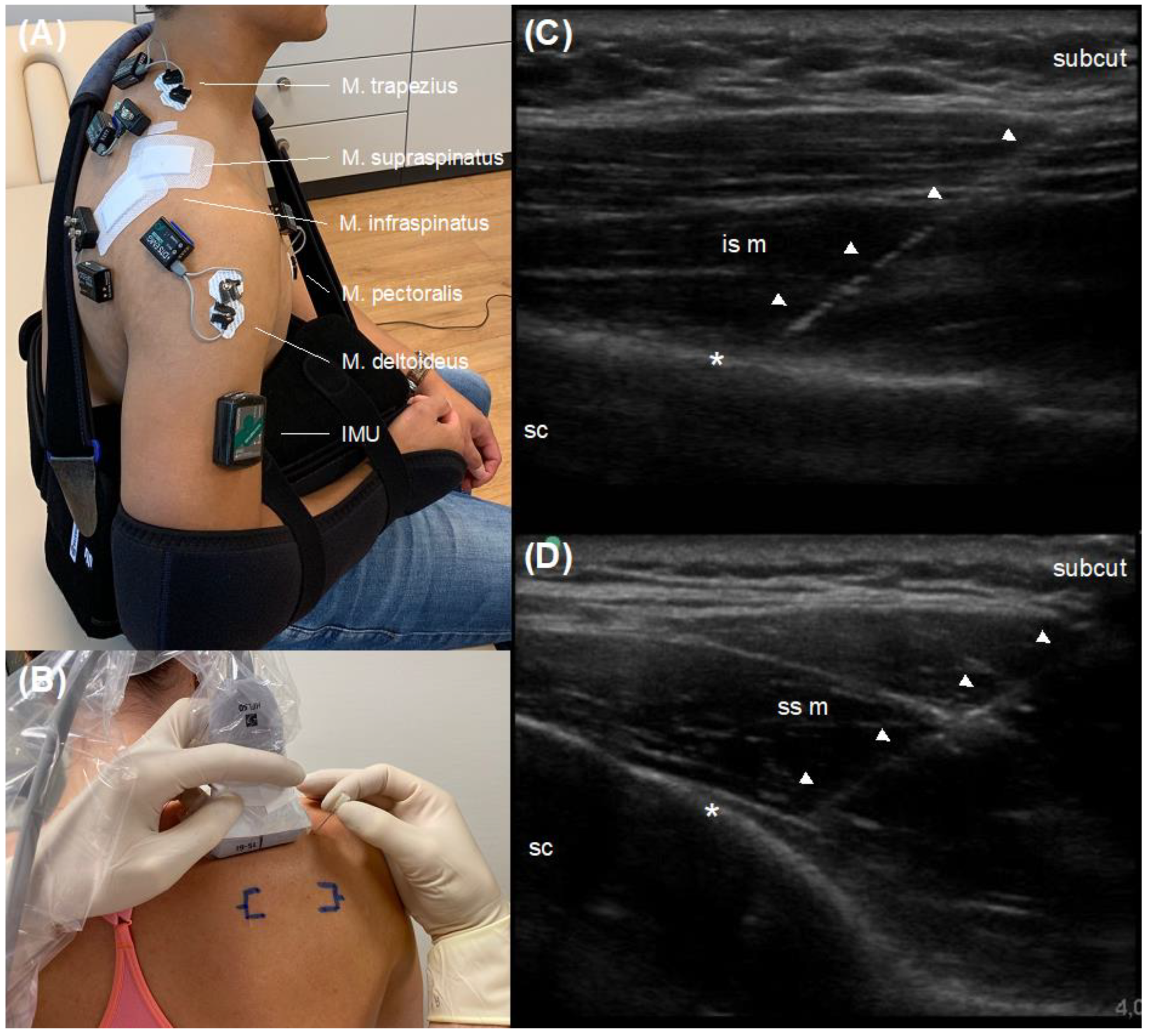
2.6.1. Electromyography
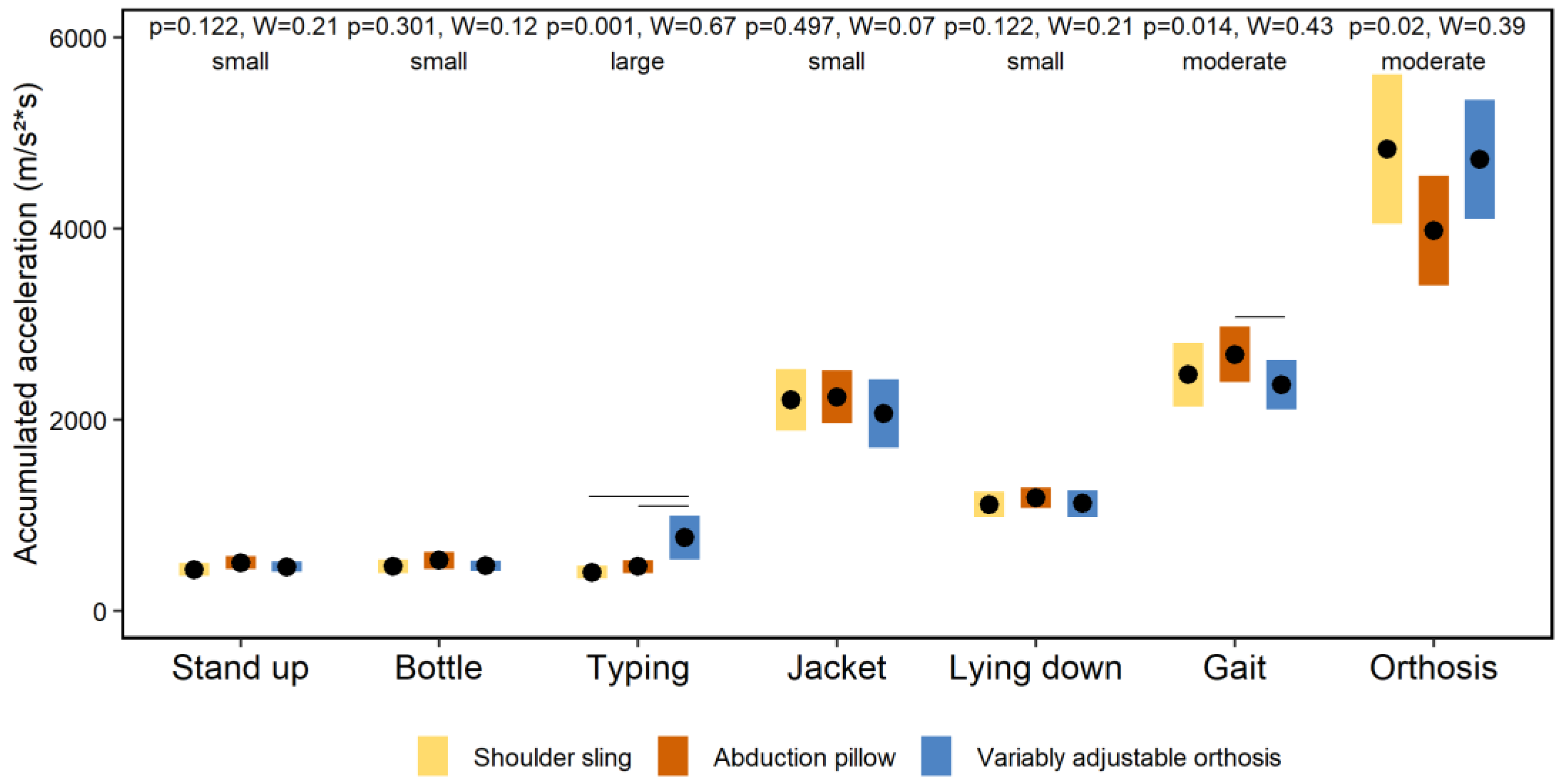
2.6.2. Inertial Measurement Unit
2.6.3. Video Analysis
2.6.4. Visual Analogue Scale
2.7. Statistical Analysis
3. Results
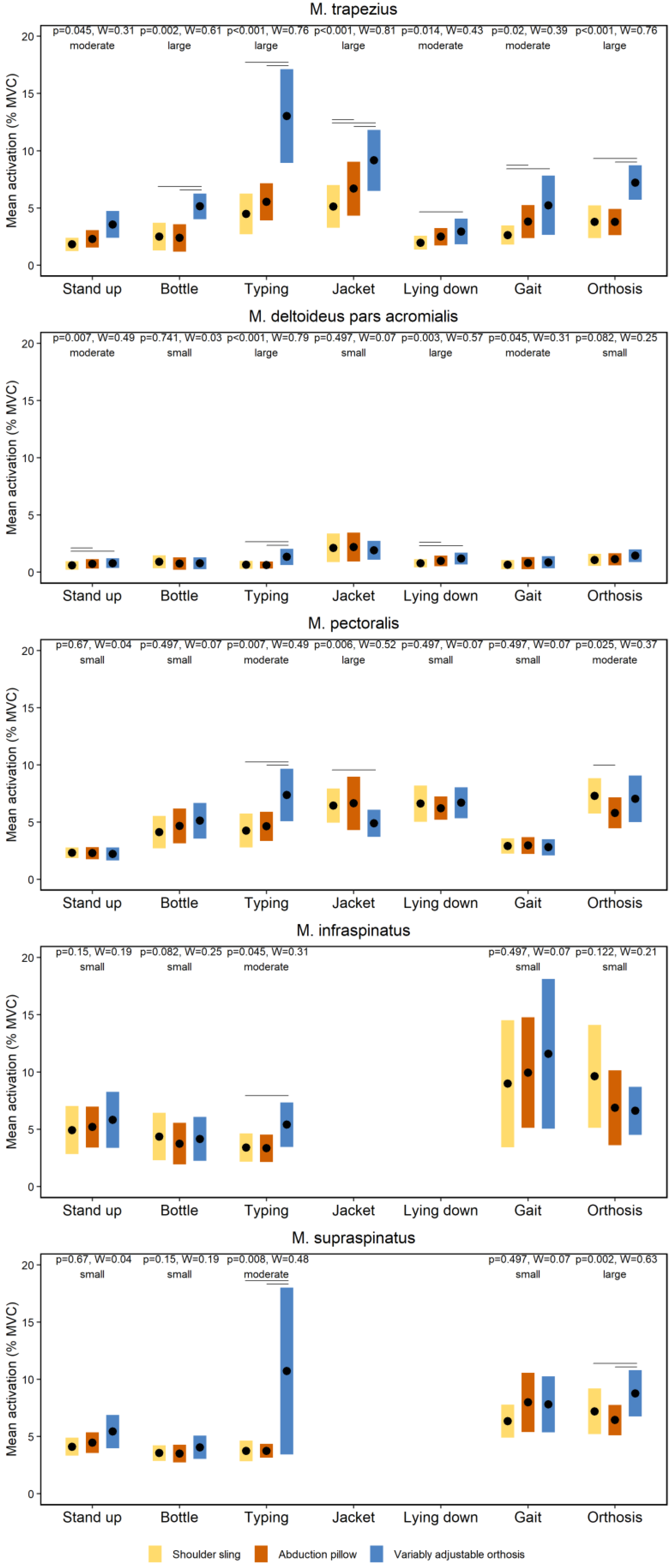
3.1. Effects of Orthoses on Neuromuscular Activity during Activities of Daily Living
3.2. Effects of Physiotherapeutic Exercises on Neuromuscular Activity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Krukenberg, A.; Thierbach, A.; Thiele, K.; Scheibel, M. Aktuelle Entwicklungen und Einsatzgebiete von Schulterorthesen. Obere Extrem. 2016, 11, 10–15. [Google Scholar] [CrossRef]
- Bucksch, S.; Hoffmann, N.; Osterkamp, N.; Yilmaz, S. Heil- und Hilfsmittelreport 2018, BARMER, ed.; 37 Grad Analyse & Beratung: Köln, Germany, 2018; Volume 13. [Google Scholar]
- Greitemann, B.; Maronna, U. Technische Orthopädie: Stellenwert in einem zunehmend operativ ausgerichteten Fach. Orthopäde 2013, 42, 842–853. [Google Scholar] [CrossRef] [PubMed]
- Markets and Markets. Orthopedic Braces & Supports Market by Product (Knee, Ankle, Spine, Shoulder, Neck, Elbow, Wrist, Facial), Category (Soft, Hard), Application (Ligament (ACL, LCL), Preventive, OA), Distribution, and Region—Global Forecast to 2024. Available online: https://www.marketsandmarkets.com/Market-Reports/orthopedic-braces-support-market-24806829.html (accessed on 28 September 2022).
- Sgroi, T.A.; Cilenti, M. Rotator cuff repair: Post-operative rehabilitation concepts. Curr. Rev. Musculoskelet. Med. 2018, 11, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Jung, C.; Tepohl, L.; Tholen, R.; Beitzel, K.; Buchmann, S.; Gottfried, T.; Grim, C.; Mauch, B.; Krischak, G.; Ortmann, H.; et al. Rehabilitation following rotator cuff repair: A work of the Commission Rehabilitation of the German Society of Shoulder and Elbow Surgery e.V. (DVSE) in collaboration with the German Association for Physiotherapy (ZVK) e.V., the Association Physical Therapy, Association for Physical Professions (VPT) e.V. and the Section Rehabilitation-Physical Therapy of the German Society for Orthopaedics and Trauma e.V. (DGOU). Obere Extrem. 2018, 13, 45–61. [Google Scholar] [CrossRef] [PubMed]
- Brislin, K.J.; Field, L.D.; Savoie, F.H., 3rd. Complications after arthroscopic rotator cuff repair. Arthroscopy 2007, 23, 124–128. [Google Scholar] [CrossRef] [PubMed]
- Huberty, D.P.; Schoolfield, J.D.; Brady, P.C.; Vadala, A.P.; Arrigoni, P.; Burkhart, S.S. Incidence and treatment of postoperative stiffness following arthroscopic rotator cuff repair. Arthroscopy 2009, 25, 880–890. [Google Scholar] [CrossRef] [PubMed]
- Peltz, C.D.; Sarver, J.J.; Dourte, L.M.; Wurgler-Hauri, C.C.; Williams, G.R.; Soslowsky, L.J. Exercise following a short immobilization period is detrimental to tendon properties and joint mechanics in a rat rotator cuff injury model. J. Orthop. Res. 2010, 28, 841–845. [Google Scholar] [CrossRef]
- Sarver, J.J.; Peltz, C.D.; Dourte, L.M.; Reddy, S.; Williams, G.R.; Soslowsky, L.J. After rotator cuff repair, stiffness but not the loss in range of motion increased transiently for immobilized shoulders in a rat model. J. Shoulder Elb. Surg. 2008, 17, 108–113. [Google Scholar] [CrossRef]
- Ghodadra, N.S.; Provencher, M.T.; Verma, N.N.; Wilk, K.E.; Romeo, A.A. Open, mini-open, and all-arthroscopic rotator cuff repair surgery: Indications and implications for rehabilitation. J. Orthop. Sports Phys. Ther. 2009, 39, 81–89. [Google Scholar] [CrossRef]
- Millett, P.J.; Wilcox, R.B., 3rd; O’Holleran, J.D.; Warner, J.J. Rehabilitation of the rotator cuff: An evaluation-based approach. J. Am. Acad. Orthop. Surg. 2006, 14, 599–609. [Google Scholar] [CrossRef]
- Gomi, H.; Osu, R. Task-dependent viscoelasticity of human multijoint arm and its spatial characteristics for interaction with environments. J. Neurosci. 1998, 18, 8965–8978. [Google Scholar] [CrossRef] [PubMed]
- Yamazaki, Y.; Suzuki, M.; Ohkuwa, T.; Itoh, H. Coactivation in arm and shoulder muscles during voluntary fixation of a single joint. Brain Res. Bull. 2003, 59, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Cross, J.A.; deVries, J.; Mocarski, M.; Ketchum, N.C.; Compty, E.; Krimmer, M.; Fritz, J.M.; Vetter, C.S. Electromyography of the shoulder musculature during passive rehabilitation exercises. J. Shoulder Elb. Arthroplast. 2020, 4, 2471549220960044. [Google Scholar] [CrossRef]
- Smith, J.; Dahm, D.L.; Kaufman, K.R.; Boon, A.J.; Laskowski, E.R.; Kotajarvi, B.R.; Jacofsky, D.J. Electromyographic activity in the immobilized shoulder girdle musculature during scapulothoracic exercises. Arch. Phys. Med. Rehabil. 2006, 87, 923–927. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.; Dahm, D.L.; Kotajarvi, B.R.; Boon, A.J.; Laskowski, E.R.; Jacofsky, D.J.; Kaufman, K.R. Electromyographic activity in the immobilized shoulder girdle musculature during ipsilateral kinetic chain exercises. Arch. Phys. Med. Rehabil. 2007, 88, 1377–1383. [Google Scholar] [CrossRef] [PubMed]
- Alenabi, T.; Jackson, M.; Tetreault, P.; Begon, M. Electromyographic activity in the immobilized shoulder musculature during ipsilateral elbow, wrist, and finger movements while wearing a shoulder orthosis. J. Shoulder Elb. Surg. 2013, 22, 1400–1407. [Google Scholar] [CrossRef]
- Gurney, A.B.; Mermier, C.; LaPlante, M.; Majumdar, A.; O’Neill, K.; Shewman, T.; Gurney, J.G. Shoulder electromyography measurements during activities of daily living and routine rehabilitation exercises. J. Orthop. Sports Phys. Ther. 2016, 46, 375–383. [Google Scholar] [CrossRef]
- Yoon, S.H.; Lee, D.H.; Jung, M.C.; Park, Y.U.; Lim, S.Y. Electromyographic activities of the rotator cuff muscles during walking, eating, and washing. Am. J. Phys. Med. Rehabil. 2016, 95, e169–e176. [Google Scholar] [CrossRef]
- Seniam. Available online: http://www.seniam.org/ (accessed on 28 September 2022).
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of recommendations for SEMG sensors and sensor placement procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef]
- Menkes, D.L.; Pierce, R. Needle EMG muscle identification: A systematic approach to needle EMG examination. Clin. Neurophysiol. Pr. 2019, 4, 199–211. [Google Scholar] [CrossRef]
- Muller, T.; Martiny, H.; Merz, E.; Doffert, J.; Wustner, M.; Lessel, W.; Heynemann, H.; Enzmann, T.; Dudwiesus, H.; Nuernberg, D.; et al. DEGUM recommendations on infection prevention in ultrasound and endoscopic ultrasound. Ultraschall Med. 2018, 39, 284–303. [Google Scholar] [CrossRef] [PubMed]
- Berckmans, K.; Castelein, B.; Borms, D.; Palmans, T.; Parlevliet, T.; Cools, A. Analysis of scapular kinematics and muscle activity by use of fine-wire electrodes during shoulder exercises. Am. J. Sports Med. 2020, 48, 1213–1219. [Google Scholar] [CrossRef] [PubMed]
- Werin, M.; Maenhout, A.; Palmans, T.; Borms, D.; Cools, A. Does verbal and tactile feedback change EMG activity in shoulder girdle and trunk muscles during plyometric exercise in overhead athletes with and without shoulder pain? Phys. Ther. Sport 2022, 54, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, M.W.; Hotfiel, T.; Stuckradt, A.; Grim, C.; Ueberschar, O.; Freiwald, J.; Baumgart, C. Effects of passive, active, and mixed playing strategies on external and internal loads in female tennis players. PLoS ONE 2020, 15, e0239463. [Google Scholar] [CrossRef] [PubMed]
- RStudio Team. RStudio: Integrated Development Environment for R. RStudio, PBC, Boston, MA. Available online: https://www.rstudio.com/ (accessed on 28 September 2022).
- R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. Available online: https://www.r-project.org/ (accessed on 28 September 2022).
- Tomczak, M.; Tomczak, E. The need to report effect size estimates revisited. An overview of some recommended measures of effect size. Trends Sport Sci. 2014, 1, 19–25. [Google Scholar]
- Sullivan, L.G.; Bailie, R.; Weiss, N.; Miller, B.S. An evaluation of shoulder external rotation braces. Arthrosc. J. Arthrosc. Relat. Surg. 2007, 23, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Edwards, P.K.; Ebert, J.R.; Littlewood, C.; Ackland, T.; Wang, A. A systematic review of electromyography studies in normal shoulders to inform postoperative rehabilitation following rotator cuff repair. J. Orthop. Sports Phys. Ther. 2017, 47, 931–944. [Google Scholar] [CrossRef]
- Long, J.L.; Ruberte Thiele, R.A.; Skendzel, J.G.; Jeon, J.; Hughes, R.E.; Miller, B.S.; Carpenter, J.E. Activation of the shoulder musculature during pendulum exercises and light activities. J. Orthop. Sports Phys. Ther. 2010, 40, 230–237. [Google Scholar] [CrossRef]
- Edwards, P.K.; Kwong, P.W.H.; Ackland, T.; Wang, A.; Donnelly, C.J.; Ebert, J.R. Electromyographic evaluation of early-stage shoulder rehabilitation exercises following rotator cuff repair. Int. J. Sports Phys. Ther. 2021, 16, 1459–1469. [Google Scholar] [CrossRef]
- Reinold, M.M.; Macrina, L.C.; Wilk, K.E.; Fleisig, G.S.; Dun, S.; Barrentine, S.W.; Ellerbusch, M.T.; Andrews, J.R. Electromyographic analysis of the supraspinatus and deltoid muscles during 3 common rehabilitation exercises. J. Athl. Train. 2007, 42, 464–469. [Google Scholar]
- Dockery, M.L.; Wright, T.W.; LaStayo, P.C. Electromyography of the shoulder: An analysis of passive modes of exercise. Orthopedics 1998, 21, 1181–1184. [Google Scholar] [CrossRef] [PubMed]
- Merletti, R.; Farina, D. Analysis of intramuscular electromyogram signals. Philos. Trans. A Math. Phys. Eng. Sci. 2009, 367, 357–368. [Google Scholar] [CrossRef] [PubMed]
- Stokes, I.A.F.; Henry, S.M.; Single, R.M. Surface EMG electrodes do not accurately record from lumbar multifidus muscles. Clin. Biomech. 2003, 18, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Xu, Y.; Han, X.; Wu, W.; Tang, Y.; Wang, C. Functional and morphological changes in the deep lumbar multifidus using electromyography and ultrasound. Sci. Rep. 2018, 8, 6539. [Google Scholar] [CrossRef] [PubMed]
- Arias-Martorell, J. The morphology and evolutionary history of the glenohumeral joint of hominoids: A review. Ecol. Evol. 2019, 9, 703–722. [Google Scholar] [CrossRef]
- Schmidt, M.; Voges, D.; Fischer, M.S. Shoulder movements during quadrupedal locomotion in arboreal primates. Z. Morphol. Anthropol. 2002, 83, 235–242. [Google Scholar] [CrossRef]
- Macintosh, J.E.; Valencia, F.; Bogduk, N.; Munro, R.R. The morphology of the human lumbar multifidus. Clin. Biomech. 1986, 1, 196–204. [Google Scholar] [CrossRef]
- Rathi, S.; Taylor, N.F.; Soo, B.; Green, R.A. Glenohumeral joint translation and muscle activity in patients with symptomatic rotator cuff pathology: An ultrasonographic and electromyographic study with age-matched controls. J. Sci. Med. Sport 2018, 21, 885–889. [Google Scholar] [CrossRef]
| Variable | Mean ± SD |
|---|---|
| Age (years) | 31± 3 |
| Body height (m) | 1.72 ± 0.08 |
| Body mass (kg) | 68.9 ± 14.8 |
| Body mass index (kg/m2) | 23.1 ± 3.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grim, C.; Baumgart, C.; Schlarmann, M.; Hotfiel, T.; Javanmardi, S.; Hoffmann, N.; Kurz, E.; Freiwald, J.; Engelhardt, M.; Hoppe, M.W. Effects of Different Orthoses on Neuromuscular Activity of Superficial and Deep Shoulder Muscles during Activities of Daily Living and Physiotherapeutic Exercises in Healthy Participants. J. Pers. Med. 2022, 12, 2068. https://doi.org/10.3390/jpm12122068
Grim C, Baumgart C, Schlarmann M, Hotfiel T, Javanmardi S, Hoffmann N, Kurz E, Freiwald J, Engelhardt M, Hoppe MW. Effects of Different Orthoses on Neuromuscular Activity of Superficial and Deep Shoulder Muscles during Activities of Daily Living and Physiotherapeutic Exercises in Healthy Participants. Journal of Personalized Medicine. 2022; 12(12):2068. https://doi.org/10.3390/jpm12122068
Chicago/Turabian StyleGrim, Casper, Christian Baumgart, Manuel Schlarmann, Thilo Hotfiel, Sasha Javanmardi, Natalie Hoffmann, Eduard Kurz, Jürgen Freiwald, Martin Engelhardt, and Matthias W. Hoppe. 2022. "Effects of Different Orthoses on Neuromuscular Activity of Superficial and Deep Shoulder Muscles during Activities of Daily Living and Physiotherapeutic Exercises in Healthy Participants" Journal of Personalized Medicine 12, no. 12: 2068. https://doi.org/10.3390/jpm12122068
APA StyleGrim, C., Baumgart, C., Schlarmann, M., Hotfiel, T., Javanmardi, S., Hoffmann, N., Kurz, E., Freiwald, J., Engelhardt, M., & Hoppe, M. W. (2022). Effects of Different Orthoses on Neuromuscular Activity of Superficial and Deep Shoulder Muscles during Activities of Daily Living and Physiotherapeutic Exercises in Healthy Participants. Journal of Personalized Medicine, 12(12), 2068. https://doi.org/10.3390/jpm12122068







