Brain Linac-Based Radiation Therapy: “Test Drive” of New Immobilization Solution and Surface Guided Radiation Therapy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Immobilization Device and Simulation Computed Tomography (Sim-CT)
2.2. Target Volume Definition and Treatment Planning
2.3. CBCT-SGRT Workflow and Data Collections
2.4. Statistical Analysis
3. Results
3.1. Cohort of Study
3.2. Inter-Fraction Reproducibility and Intrafraction Stability
3.3. Technician Aspects, Patient’s and Physician’s Evaluations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hanna, T.P.; Shafiq, J.; Delaney, G.P.; Vinod, S.K.; Thompson, S.R.; Barton, M.B. The population benefit of evidence-based radiotherapy: 5-Year local control and overall survival benefits. Radiother. Oncol. 2018, 126, 191–197. [Google Scholar] [CrossRef] [Green Version]
- Stupp, R.; Mason, W.P.; van den Bent, M.J.; Weller, M.; Fisher, B.; Taphoorn, M.J.B.; Belanger, K.; Brandes, A.A.; Marosi, C.; Bogdahn, U.; et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N. Engl. J. Med. 2005, 352, 987–996. [Google Scholar] [CrossRef]
- Navarria, P.; Minniti, G.; Clerici, E.; Tomatis, S.; Pinzi, V.; Ciammella, P.; Galaverni, M.; Amelio, D.; Scartoni, D.; Scoccianti, S.; et al. Re-irradiation for recurrent glioma: Outcome evaluation, toxicity and prognostic factors assessment. A multicenter study of the Radiation Oncology Italian Association (AIRO). J. Neuro-Oncol. 2018, 142, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Mazzola, R.; Corradini, S.; Gregucci, F.; Figlia, V.; Fiorentino, A.; Alongi, F. Role of Radiosurgery/Stereotactic Radiotherapy in Oligometastatic Disease: Brain Oligometastases. Front. Oncol. 2019, 9, 206. [Google Scholar] [CrossRef]
- Franco, P.; De Bari, B.; Ciammella, P.; Fiorentino, A.; Chiesa, S.; Amelio, D.; Pinzi, V.; Bonomo, P.; Vagge, S.; Fiore, M.; et al. The role of stereotactic ablative radiotherapy in oncological and non-oncological clinical settings: Highlights from the 7th meeting of AIRO—Young Members Working Group (AIRO Giovani). Tumori 2014, 100, 214–219. [Google Scholar] [CrossRef]
- Meduri, B.; Gregucci, F.; D’Angelo, E.; Alitto, A.R.; Ciurlia, E.; Desideri, I.; Marino, L.; Borghetti, P.; Fiore, M.; Fiorentino, A.; et al. Volume de-escalation in radiation therapy: State of the art and new perspectives. J. Cancer Res. Clin. Oncol. 2020, 146, 909–924. [Google Scholar] [CrossRef] [PubMed]
- Babic, S.; Lee, Y.; Ruschin, M.; Lochray, F.; Lightstone, A.; Atenafu, E.; Phan, N.; Mainprize, T.; Tsao, M.; Soliman, H.; et al. To frame or not to frame? Cone-beam CT-based analysis of head immobilization devices specific to linac-based stereotactic radiosurgery and radiotherapy. J. Appl. Clin. Med. Phys. 2018, 19, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Covington, E.L.; Stanley, D.N.; Fiveash, J.B.; Thomas, E.M.; Marcrom, S.R.; Bredel, M.; Willey, C.D.; Riley, K.O.; Popple, R.A. Surface guided imaging during stereotactic radiosurgery with automated delivery. J. Appl. Clin. Med. Phys. 2020, 21, 90–95. [Google Scholar] [CrossRef]
- Niyazi, M.; Brada, M.; Chalmers, A.J.; Combs, S.E.; Erridge, S.C.; Fiorentino, A.; Grosu, A.L.; Lagerwaard, F.J.; Minniti, G.; Mirimanoff, R.-O.; et al. ESTRO-ACROP guideline “target delineation of glioblastomas”. Radiother. Oncol. 2016, 118, 35–42. [Google Scholar] [CrossRef]
- Tsao, M.N.; Rades, D.; Wirth, A.; Lo, S.S.; Danielson, B.L.; Gaspar, L.E.; Sperduto, P.W.; Vogelbaum, M.A.; Radawski, J.; Wang, J.Z.; et al. Radiotherapeutic and surgical management for newly diagnosed brain metastasis(es): An American Society for Radiation Oncology evidence-based guideline. Pract. Radiat. Oncol. 2012, 2, 210–225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seuntjens, J.; Lartigau, E.; Cora, S.; Ding, G.X.; Goetsch, S.; Nuyttens, J. ICRU Report 91. Prescribing, recording, and reporting of stereotactic treatments with small photon beams. J. ICRU 2014, 14, 1–160. [Google Scholar]
- Malmstrom, A.; Gronberg, B.H.; Marosi, C.; Stupp, R.; Frappaz, D.; Schultz, H.; Abacioglu, U.; Tavelin, B.; Lhermitte, B.; Hegi, M.E.; et al. Temozolomide versus standard 6-week radiotherapy versus hypofractionated radiotherapy in patients older than 60 years with glioblastoma: The Nordic randomized, phase 3 trial. Lancet Oncol. 2012, 13, 916–926. [Google Scholar] [CrossRef]
- Gregucci, F.; Fiorentino, A.; Corradini, S.; Figlia, V.; Mazzola, R.; Ricchetti, F.; Ruggieri, R.; Alongi, F. Linac-based radiosurgery or fractionated stereotactic radiotherapy with flattening filter-free volumetric modulated arc therapy in elderly patients: A mono-institutional experience on 110 brain metastases. Strahlenther. Onkol. 2019, 195, 218–225. [Google Scholar] [CrossRef]
- Gregucci, F.; Surgo, A.; Bonaparte, I.; Laera, L.; Ciliberti, M.P.; Carbonara, R.; Gentile, M.A.; Giraldi, D.; Calbi, R.; Caliandro, M.; et al. Poor-Prognosis Patients Affected by Glioblastoma: Retrospective Study of Hypofractionated Radiotherapy with Simultaneous Integrated Boost and Concurrent/Adjuvant Temozolomide. J. Pers. Med. 2021, 11, 1145. [Google Scholar] [CrossRef]
- Alongi, F.; Fiorentino, A.; Mancosu, P.; Navarria, P.; Levra, N.G.; Mazzola, R.; Scorsetti, M. Stereotactic radiosurgery for intracranial metastases: Linac-based and gamma-dedicated unit approach. Expert Rev. Anticancer. Ther. 2016, 16, 731–740. [Google Scholar] [CrossRef] [PubMed]
- Ong, C.L.; Giaj-Levra, N.; Nicosia, L.; Figlia, V.; Tomasini, D.; Franken, E.M.; Alongi, F. Intra-fraction and Inter-fraction analysis of a dedicated immobilization device for intracranial radiation treatment. Radiat. Oncol. 2020, 15, 200. [Google Scholar] [CrossRef]
- Minniti, G.; Scaringi, C.; Clarke, E.; Valeriani, M.; Osti, M.F.; Enrici, R.M. Frameless linacbased stereotactic radiosurgery (SRS) for brain metastases: Analysis of patient repositioning using a mask fixation system and clinical endpoints. Radiat. Oncol. 2011, 6, 158. [Google Scholar] [CrossRef]
- Willner, J.; Flentje, M.; Bratengeier, K. CT simulation in stereotactic brain radiotherapy–analysis of isocenter reproducibility with mask fixation. Radiother. Oncol. 1997, 45, 83–88. [Google Scholar] [CrossRef]
- Karger, C.P.; Jakel, O.; Debus, J.; Kuhn, S.; Hartmann, G.H. Three-dimensional accuracy and inter-fractional reproducibility of patient fixation and positioning using a stereotactic head mask system. Int. J. Radiat. Oncol. Biol. Phys. 2001, 49, 1493–1504. [Google Scholar] [CrossRef]
- Alheit, H.; Dornfeld, S.; Dawel, M.; Alheit, M.; Henzel, B.; Steckler, K.; Blank, H.; Geyer, P. Patient position reproducibility in fractionated stereotactically guided conformal radiotherapy using the BrainLab mask system. Strahlenther. Onkol. 2001, 177, 264–268. [Google Scholar] [CrossRef]
- Kocher, M.; Wittig, A.; Piroth, M.D.; Treuer, H.; Seegenschmiedt, H.; Ruge, M.; Grosu, A.-L.; Guckenberger, M. Stereotactic radiosurgery for treatment of brain metastases. A report of the DEGRO Working Group on Stereotactic Radiotherapy. Strahlenther. Onkol. 2014, 190, 521–532. [Google Scholar] [CrossRef]
- Wilke, L.; Andratschke, N.; Blanck, O.; Brunner, T.B.; Combs, S.E.; Grosu, A.-L.; Moustakis, C.; Schmitt, D.; Baus, W.W.; Guckenberger, M. ICRU report 91 on prescribing, recording, and reporting of stereotactic treatments with small photon beams: Statement from the DEGRO/DGMP working group stereotactic radiotherapy and radiosurgery. Strahlenther. Onkol. 2019, 195, 193–198. [Google Scholar] [CrossRef]
- Yock, A.D.; Pawlicki, T.; Kim, G.Y. Prospective treatment plan-specific action limits for real-time intrafractional monitoring in surface image guided radiosurgery. Med. Phys. 2016, 43, 4342. [Google Scholar] [CrossRef]
- Covington, E.L.; Fiveash, J.B.; Wu, X.; Brezovich, I.; Willey, C.D.; Riley, K.; Popple, R. Optical surface guidance for submillimeter monitoring of patient position during frameless stereotactic radiotherapy. J. Appl. Clin. Med. Phys. 2019, 20, 91–98. [Google Scholar] [CrossRef] [Green Version]
| Total Patients | 69 |
| cRT group | 24 (35%) |
| SRT group | 45 (65%) |
| Total treatment session | 556 |
| cRT treatment session | 397 (71%) |
| SRT treatment session | 159 (29%) |
| Total CBCT | 863 |
| Inter-fraction CBCT | 556 (64%) |
| Intrafraction CBCT | 307 (36%) |
| Sex | |
| Female | 21 (30%) |
| Male | 48 (70%) |
| Median age | 66 years (range 27–89) |
| Diagnosis | |
| Brain Metastases | 32 (46%) |
| Primary brain cancer | 17 (25%) |
| Primary brain cancer recurrence | 10 (14%) |
| Meningioma | 7 (10%) |
| Vascular malformation | 3 (5%) |
| Type of radiation treatment (RT) | |
| Conventional RT | |
| Median dose | 40 Gy (range 20–60 Gy) |
| Median fractions | 15 (5–30) |
| Median target volume | 178.6 cc (range 98.8–470.3 cc) |
| Stereotactic RT | |
| Median dose | 27 Gy (range 12–30 Gy) |
| Median fractions | 3 (range 1–5) |
| Median target volume | 6.15 cc (range 0.7–104 cc) |
| Median coach rotation | 4 (range 0–4) |
| Median monitor units | 2121.7 (range 1037.9–6151.2) |
| Median overall treatment time | 2 min (range 1–5 min) |
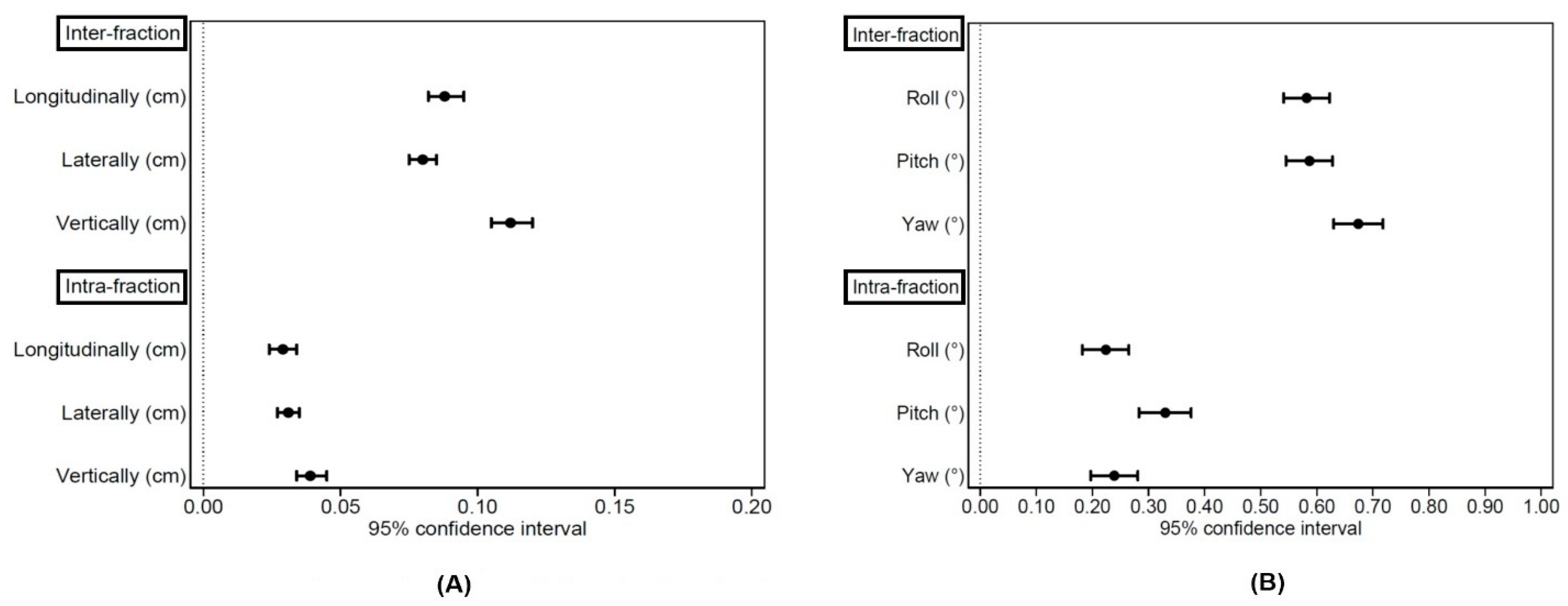
| Population | 69 Patients—556 Treatment Sessions—556 CBCT | |||||
|---|---|---|---|---|---|---|
| Mean | SD | 25% | 50% | 75% | 95% CI | |
| Longitudinally (mm) | 0.9 | 0.8 | 0.3 | 0.7 | 1.2 | 0.82–0.95 |
| Laterally (mm) | 0.8 | 0.6 | 0.4 | 0.7 | 1.1 | 0.82–0.95 |
| Vertically (mm) | 1.1 | 0.9 | 0.5 | 1.0 | 1.6 | 1.05–1.20 |
| Roll (°) | 0.58 | 0.49 | 0.20 | 0.45 | 0.9 | 0.541–0.623 |
| Pitch (°) | 0.59 | 0.49 | 0.20 | 0.40 | 0.80 | 0.545–0.628 |
| Yaw (°) | 0.67 | 0.53 | 0.20 | 0.50 | 1.00 | 0.630–0.718 |
| Population | 45 Patients—159 Treatment Sessions—307 CBCT | |||||
|---|---|---|---|---|---|---|
| Mean | SD | 25% | 50% | 75% | 95% CI | |
| Longitudinally (mm) | 0.3 | 0.3 | 0.1 | 0.2 | 0.4 | 0.24–0.34 |
| Laterally (mm) | 0.3 | 0.3 | 0.1 | 0.2 | 0.4 | 0.27–0.35 |
| Vertically (mm) | 0.4 | 0.3 | 0.1 | 0.3 | 0.6 | 0.34–0.45 |
| Roll (°) | 0.22 | 0.26 | 0.10 | 0.10 | 0.30 | 0.182–0.265 |
| Pitch (°) | 0.33 | 0.29 | 0.10 | 0.30 | 0.40 | 0.283–0.376 |
| Yaw (°) | 0.24 | 0.26 | 0.10 | 0.20 | 0.30 | 0.197–0.281 |
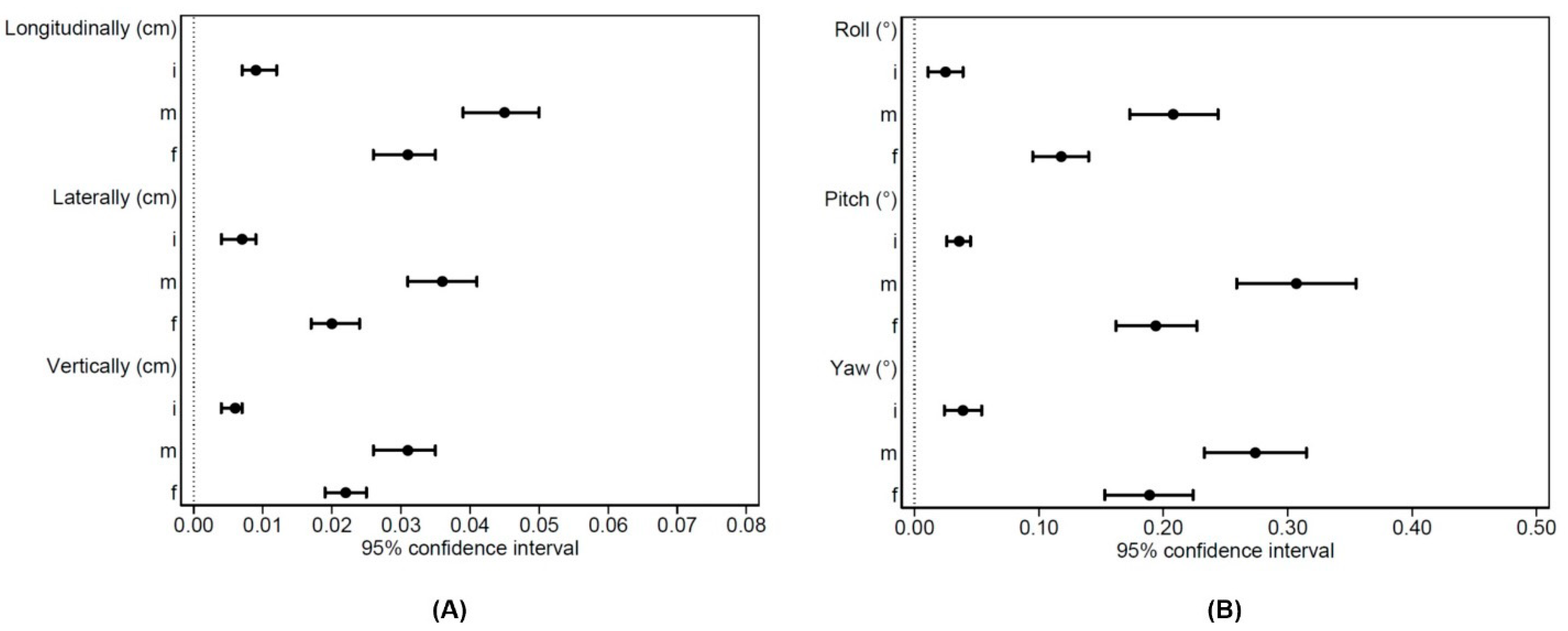
| Population | 45 Patients—159 Treatment Sessions—307 CBCT | ||||||
|---|---|---|---|---|---|---|---|
| Mean | SD | 25% | 50% | 75% | 95% CI | ||
| Longitudinally (mm) | i | 0.09 | 0.18 | 0.00 | 0.00 | 0.10 | 0.07–0.12 |
| m | 0.45 | 0.35 | 0.10 | 0.40 | 0.80 | 0.39–0.50 | |
| f | 0.31 | 0.26 | 0.10 | 0.20 | 0.40 | 0.26–0.35 | |
| Laterally (mm) | i | 0.07 | 0.16 | 0.00 | 0.00 | 0.10 | 0.04–0.09 |
| m | 0.36 | 0.33 | 0.10 | 0.20 | 0.50 | 0.31–0.41 | |
| f | 0.20 | 0.23 | 0.10 | 0.10 | 0.20 | 0.17–0.24 | |
| Vertically (mm) | i | 0.06 | 0.09 | 0.00 | 0.00 | 0.10 | 0.04–0.07 |
| m | 0.31 | 0.31 | 0.10 | 0.20 | 0.40 | 0.26–0.35 | |
| f | 0.22 | 0.20 | 0.10 | 0.20 | 0.30 | 0.19–0.25 | |
| Roll (°) | i | 0.025 | 0.091 | 0.000 | 0.000 | 0.000 | 0.011–0.039 |
| m | 0.208 | 0.228 | 0.000 | 0.100 | 0.300 | 0.173–0.244 | |
| f | 0.118 | 0.144 | 0.000 | 0.100 | 0.200 | 0.095–0.140 | |
| Pitch (°) | i | 0.036 | 0.062 | 0.000 | 0.000 | 0.100 | 0.026–0.045 |
| m | 0.307 | 0.308 | 0.100 | 0.200 | 0.500 | 0.259–0.355 | |
| f | 0.194 | 0.208 | 0.100 | 0.100 | 0.300 | 0.162–0.227 | |
| Yaw (°) | i | 0.039 | 0.097 | 0.000 | 0.000 | 0.100 | 0.024–0.054 |
| m | 0.274 | 0.263 | 0.100 | 0.200 | 0.400 | 0.233–0.315 | |
| f | 0.189 | 0.229 | 0.100 | 0.100 | 0.200 | 0.153–0.224 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gregucci, F.; Bonaparte, I.; Surgo, A.; Caliandro, M.; Carbonara, R.; Ciliberti, M.P.; Aga, A.; Berloco, F.; De Masi, M.; De Pascali, C.; et al. Brain Linac-Based Radiation Therapy: “Test Drive” of New Immobilization Solution and Surface Guided Radiation Therapy. J. Pers. Med. 2021, 11, 1351. https://doi.org/10.3390/jpm11121351
Gregucci F, Bonaparte I, Surgo A, Caliandro M, Carbonara R, Ciliberti MP, Aga A, Berloco F, De Masi M, De Pascali C, et al. Brain Linac-Based Radiation Therapy: “Test Drive” of New Immobilization Solution and Surface Guided Radiation Therapy. Journal of Personalized Medicine. 2021; 11(12):1351. https://doi.org/10.3390/jpm11121351
Chicago/Turabian StyleGregucci, Fabiana, Ilaria Bonaparte, Alessia Surgo, Morena Caliandro, Roberta Carbonara, Maria Paola Ciliberti, Alberto Aga, Francesco Berloco, Marina De Masi, Christian De Pascali, and et al. 2021. "Brain Linac-Based Radiation Therapy: “Test Drive” of New Immobilization Solution and Surface Guided Radiation Therapy" Journal of Personalized Medicine 11, no. 12: 1351. https://doi.org/10.3390/jpm11121351
APA StyleGregucci, F., Bonaparte, I., Surgo, A., Caliandro, M., Carbonara, R., Ciliberti, M. P., Aga, A., Berloco, F., De Masi, M., De Pascali, C., Fragnoli, F., Indellicati, C., Parabita, R., Sanfrancesco, G., Branà, L., Ciocia, A., Curci, D., Guida, P., & Fiorentino, A. (2021). Brain Linac-Based Radiation Therapy: “Test Drive” of New Immobilization Solution and Surface Guided Radiation Therapy. Journal of Personalized Medicine, 11(12), 1351. https://doi.org/10.3390/jpm11121351










