Ultrasound-Guided Needle Aspiration of Peritonsillar Abscesses: Utility of Transoral Pharyngeal Ultrasonography
Abstract
:1. Introduction
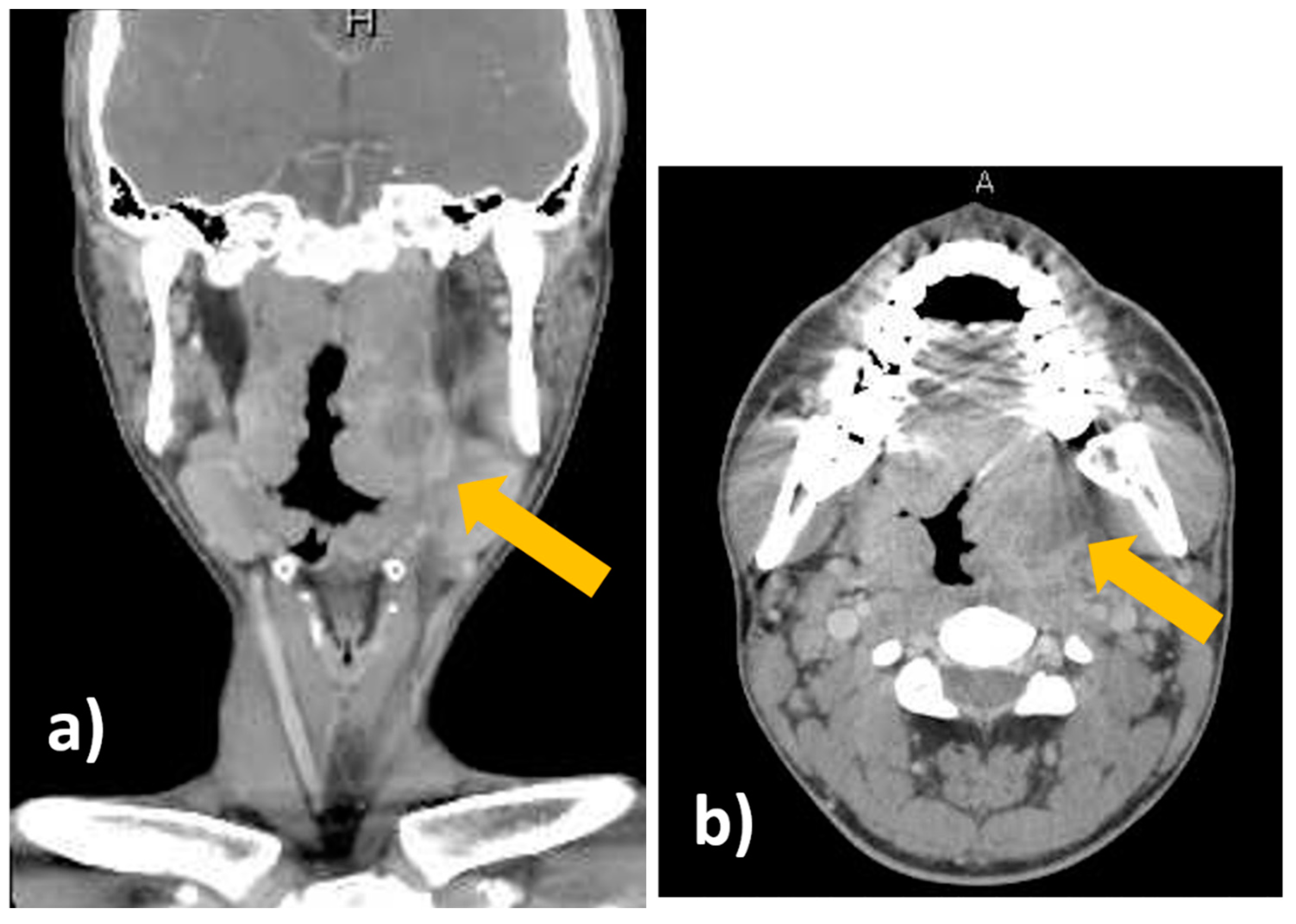
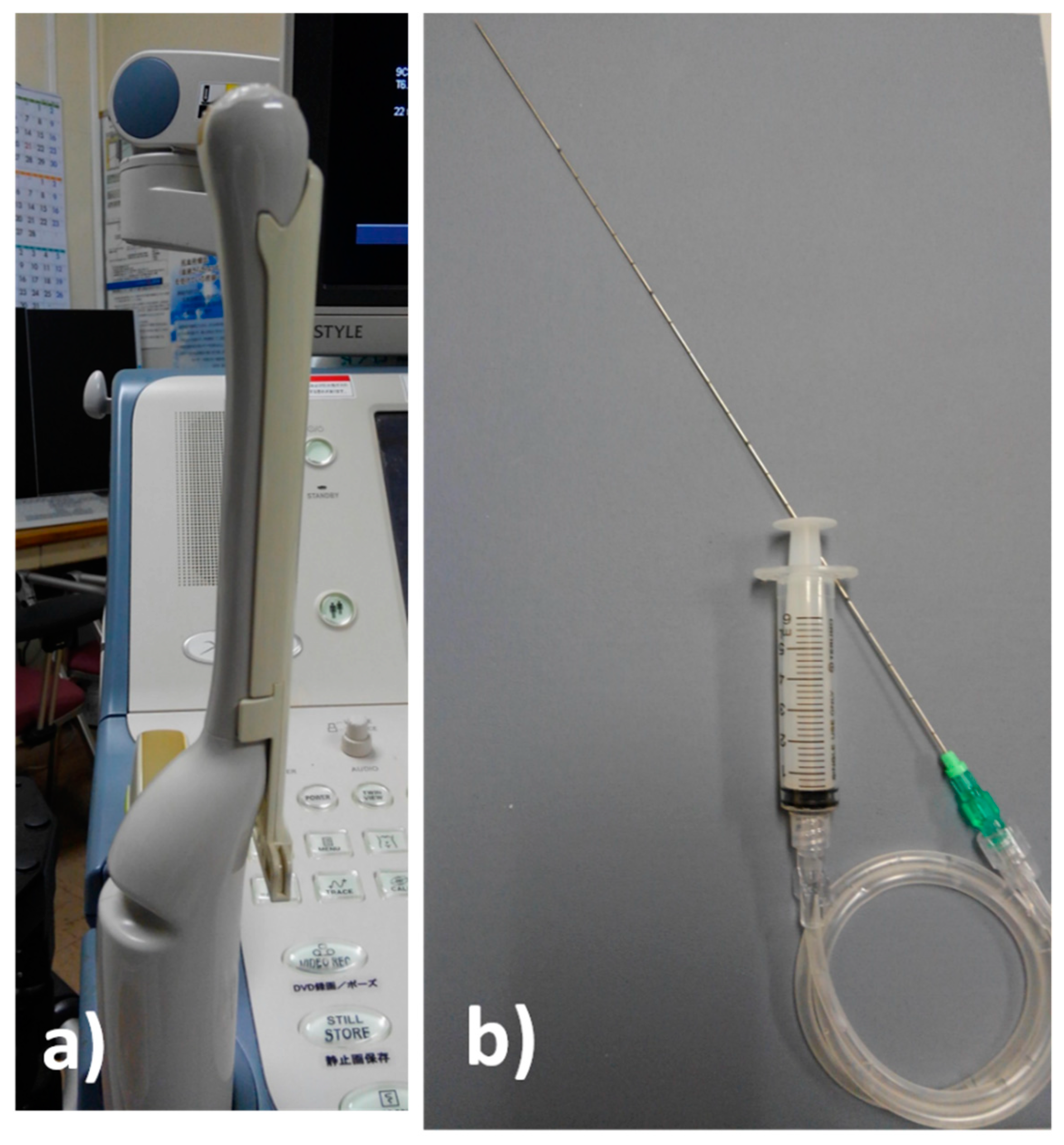
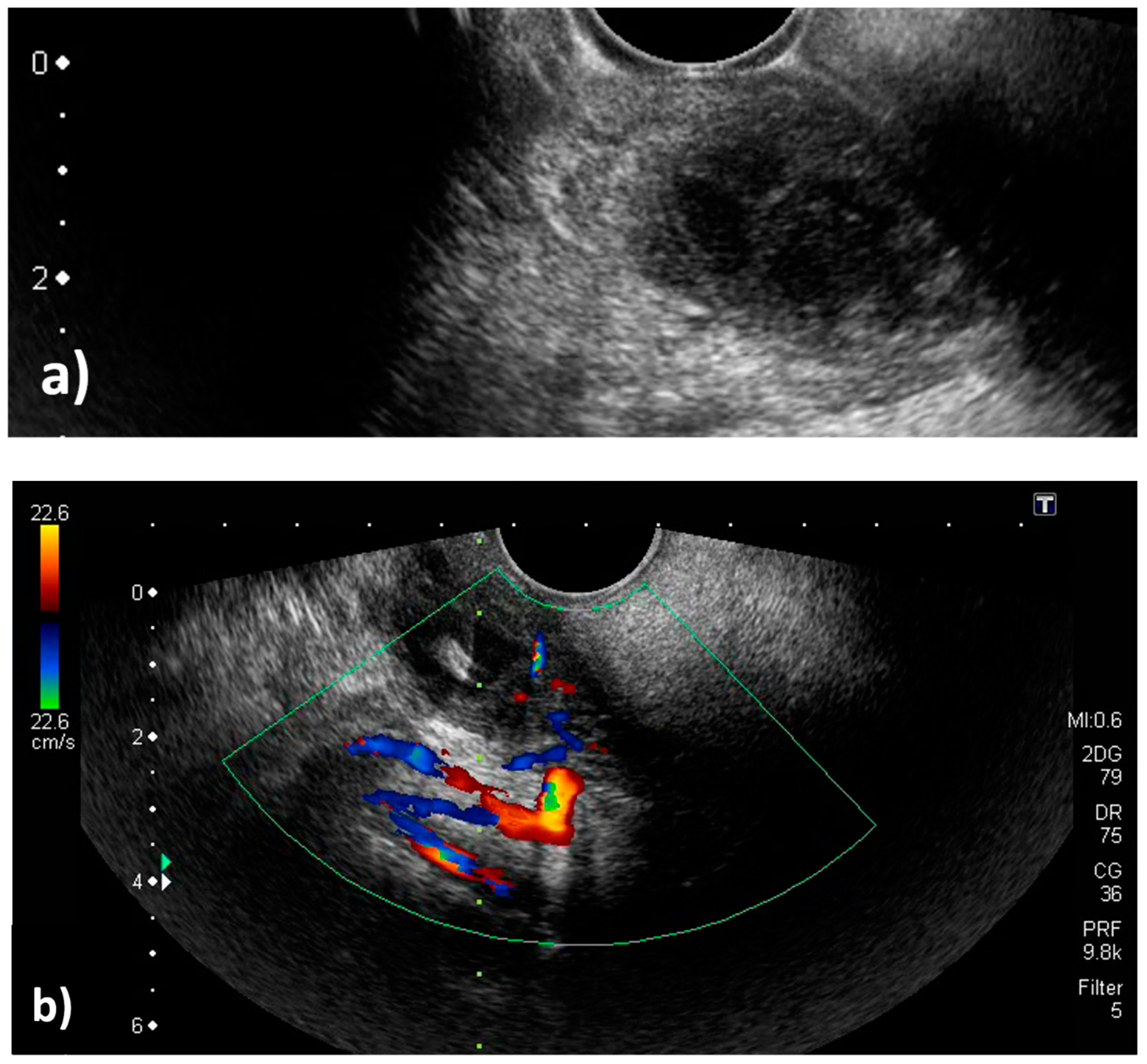
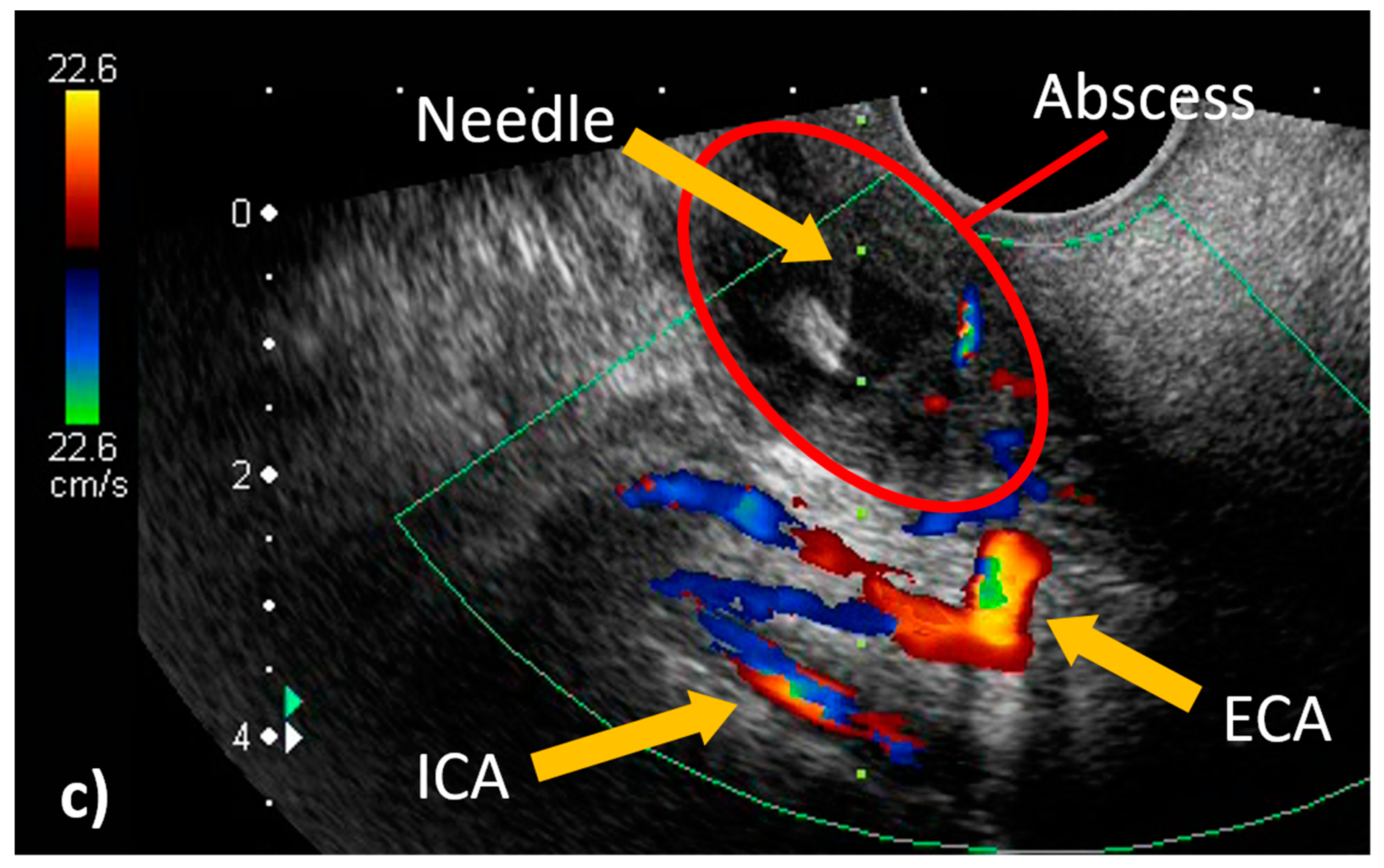
2. Case Report
3. Discussion
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Yasaka, M.; Kimura, K.; Otsubo, R.; Isa, K.; Wada, K.; Nagatsuka, K.; Minematsu, K.; Yamaguchi, T. Transoral carotid ultrasonography. Stroke 1998, 29, 1383–1388. [Google Scholar] [CrossRef] [PubMed]
- Hagiwara, Y.; Yoshie, T.; Shimizu, T.; Fukano, T.; Takada, T.; Ueda, T.; Hasegawa, Y. Contrast-enhanced transoral carotid ultrasonography for the evaluation of plaque protrusion after carotid artery stenting. Clin. Ultrasound. 2018, 46, 598–601. [Google Scholar] [CrossRef] [PubMed]
- Hagiwara, Y.; Shimizu, T.; Hasegawa, Y. Contrast-enhanced transoral carotid ultrasonography for the diagnosis and follow-up of extracranial internal carotid artery dissection: A case report. J. Clin. Ultrasound. 2017, 46, 368–371. [Google Scholar] [CrossRef] [PubMed]
- Hagiwara, Y.; Yoshie, T.; Shimizu, T.; Ogura, H.; Akamatsu, M.; Fukano, T.; Takada, T.; Nogoshi, S.; Ueda, T.; Hasegawa, Y. Contrast-enhanced transoral carotid ultrasonography for the evaluation of a long stenotic lesion in the internal carotid artery. Clin. Case Rep. 2016, 11, 1215–1216. [Google Scholar] [CrossRef] [PubMed]
- Salihoglu, M.; Eroglu, M.; Yildirim, A.; Cakmak, A.; Hardal, U.; Kara, K. Transoral ultrasonography in the diagnosis and treatment of peritonsillar abscess. Clin. Imaging 2013, 37, 465–467. [Google Scholar] [CrossRef] [PubMed]
- Lyon, M.; Blaivas, M. Intraoral ultrasound in the diagnosis and treatment of suspected peritonsillar abscess in the emergency department. Acad Emerg Med. 2005, 12, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Blaivas, M.; Theodoro, D.; Duggal, S. Ultrasound-guided drainage of peritonsillar abscess by the emergency physician. Am. J. Emerg Med. 2003, 21, 155–158. [Google Scholar] [CrossRef] [PubMed]
- Hagiwara, Y.; Araga, T.; Saito, Y.; Sasano, Y.; Tamura, Y.; Shimizu, T.; Hasegawa, Y. Utility of transoral pharyngeal ultrasonography for puncture drainage of peritonsillar abscess. Clin. Case Rep. 2019, 19, 839–840. [Google Scholar] [CrossRef] [PubMed]
- Herzon, F.S.; Harris, P. Peritonsillar abscess: Incidence, current management practices, and a proposal for treatment guidelines. Laryngoscope 1995, 105, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Page, C.; Biet, A.; Zaatar, R.; Strunski, V. Parapharyngeal abscess: Diagnosis and treatment. Eur. Arch. Oto-Rhino-Laryngol. 2008, 265, 681–686. [Google Scholar] [CrossRef] [PubMed]
- Buckley, A.; Moss, E.; Blokmanis, A. Diagnosis of peritonsillar abscess: value of intraoral sonography. AJR 1994, 162, 961–964. [Google Scholar] [CrossRef] [PubMed]
- Spires, J.R.; Ownes, J.J.; Woodson, G.E.; Miller, R.H. Treatment of peritonsillar abscess: a prospective study of aspiration vs incision and drainage. Arch. Otolaryngol. Head Neck Surg. 1987, 113, 984–988. [Google Scholar] [CrossRef] [PubMed]
- Todsen, T.; Stage, M.G.; Holst Hahn, C. A novel technique for intraoral ultrasoundguided aspiration of peritonsillar abscess. Diagnostics 2018, 8, 50. [Google Scholar] [CrossRef] [PubMed]
- Wong, K.T.; Tsang, R.K.; Tse, G.M.; Yuen, E.H.; Ahuja, A.T. Biopsy of deep-seated head and neck lesions under intraoral ultrasound guidance. Am. J. Neuroradiol. 2006, 27, 1654–1657. [Google Scholar] [PubMed]

© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hagiwara, Y.; Saito, Y.; Ogura, H.; Yaguchi, Y.; Shimizu, T.; Hasegawa, Y. Ultrasound-Guided Needle Aspiration of Peritonsillar Abscesses: Utility of Transoral Pharyngeal Ultrasonography. Diagnostics 2019, 9, 141. https://doi.org/10.3390/diagnostics9040141
Hagiwara Y, Saito Y, Ogura H, Yaguchi Y, Shimizu T, Hasegawa Y. Ultrasound-Guided Needle Aspiration of Peritonsillar Abscesses: Utility of Transoral Pharyngeal Ultrasonography. Diagnostics. 2019; 9(4):141. https://doi.org/10.3390/diagnostics9040141
Chicago/Turabian StyleHagiwara, Yuta, Yoshimitsu Saito, Hana Ogura, Yuichiro Yaguchi, Takahiro Shimizu, and Yasuhiro Hasegawa. 2019. "Ultrasound-Guided Needle Aspiration of Peritonsillar Abscesses: Utility of Transoral Pharyngeal Ultrasonography" Diagnostics 9, no. 4: 141. https://doi.org/10.3390/diagnostics9040141
APA StyleHagiwara, Y., Saito, Y., Ogura, H., Yaguchi, Y., Shimizu, T., & Hasegawa, Y. (2019). Ultrasound-Guided Needle Aspiration of Peritonsillar Abscesses: Utility of Transoral Pharyngeal Ultrasonography. Diagnostics, 9(4), 141. https://doi.org/10.3390/diagnostics9040141



