Depression, Functional Dependence, and Oral Health: Evidence from a Clinical Study of Older Spanish Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Questionnaire Data
2.4. Smoking and Alcohol Consumption
2.5. General Health Data
- Severely underweight: BMI < 16.5 kg/m2
- Underweight: BMI 16.5–18.4 kg/m2
- Normal weight: BMI 18.5–24.9 kg/m2
- Overweight: BMI 25–29.9 kg/m2
- Obese: BMI ≥ 30 kg/m2. This category was further subdivided into: (1) Class I obesity: BMI 30–34.9 kg/m2; (2) Class II obesity: BMI 35–39.9 kg/m2; (3) Class III obesity: BMI ≥ 40 kg/m2 (also known as severe, extreme, or morbid obesity).
2.6. Oral Health Data
2.7. Statistical Analysis
3. Results
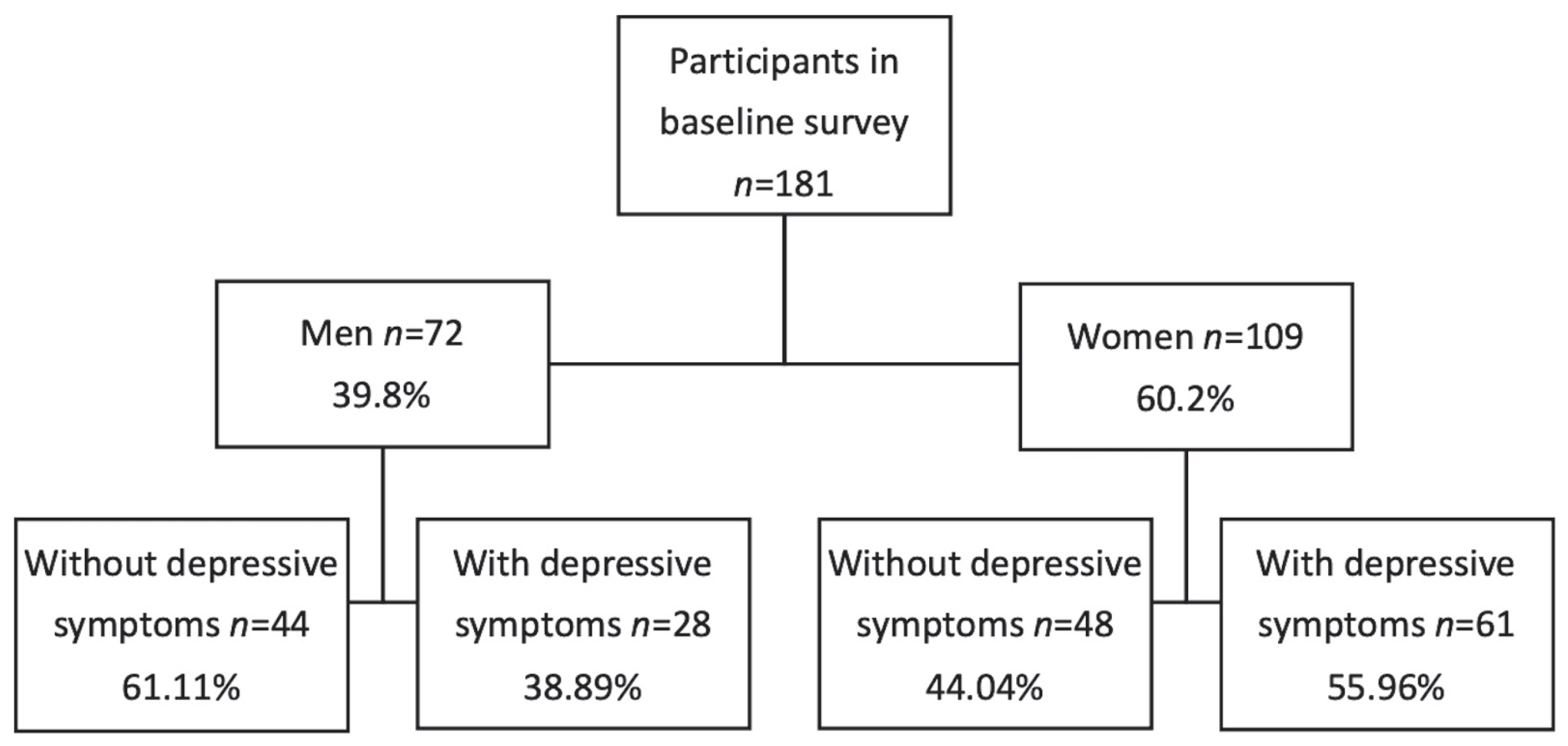
3.1. Sample Characteristics
3.2. GDS Questionnaire Results and Correlations with Other Variables
3.3. Barthel Index (Functional Dependence Status)
3.4. Oral Health Status
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| GDS | Geriatric Depression Scale |
| BMI | Body Mass Index |
| MMSE | Mini-Mental State Examination |
| AUDIT-C | Alcohol Use Disorders Identification Test–Short Form |
| MGI | Modified Gingival Index |
References
- World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates; World Health Organization: Geneva, Switzerland, 2017; Available online: https://www.who.int/publications/i/item/depression-global-health-estimates (accessed on 14 May 2025).
- Zhao, X.; Yuan, X.; Meng, D.; Liang, H.; Xiong, Y.; Li, Y.; Li, S.; He, M.; Cai, P. Prevalence and correlates of anxiety and depression among chronically ill older adults in Zunyi, China: A cross-sectional study. Front. Psychol. 2025, 16, 1560650. [Google Scholar] [CrossRef]
- Su, Z.; Wang, Y.; Chen, X.; Qian, D. Association of workforce participation with depression among US older adults: Results from NHANES 2005–2018. BMC Geriatr. 2025, 25, 77. [Google Scholar] [CrossRef]
- Trevisan, F.K.; Silva, R.H.D.; Reis, S.F.A.; Giehl, M.W.C. Prevalence of depressive symptoms and associated factors in Brazilian older adults: 2019 Brazilian National Health Survey. Cad. Saude Publica 2025, 40, e00006124. [Google Scholar] [CrossRef]
- Dickins, M.; Kelly, J.; Paxton, S.; Kwan, B.; Carveth, D.; Barker, A.; Smith, K.; Bhar, S.; Davison, T.E. The prevalence and correlates of depression and anxiety symptoms in older adults receiving in-home aged care: A cross-sectional survey. Australas. J. Ageing 2025, 44, e13396. [Google Scholar] [CrossRef]
- Oumer, B.; Abera, R.; Beshah, A.; Tesfaye, S.; Niguse, T.; Mohammed, B.; Yimer, A.A.; Sidamo, N.B. Prevalence of depressive symptoms and its associated factors among the aging population in Gamo zone, Southern Ethiopia: A community-based cross-sectional study. Front. Psychiatry 2024, 15, 1402622. [Google Scholar] [CrossRef]
- Melo, D.; Midão, L.; Mimoso, I.; Alcântara, L.; Figueiredo, T.; Carrilho, J.; Costa, E. Prevalence and Determinants of Depressive Symptoms in Older Adults Across Europe: Evidence from SHARE Wave 9. J. Clin. Med. 2025, 14, 5340. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Oral Health Status Report: Towards Universal Health Coverage for Oral Health by 2030; World Health Organization: Geneva, Switzerland, 2022; Available online: https://www.who.int/publications/i/item/9789240061484 (accessed on 18 May 2025).
- Zhao, B.; Jiang, X.; Kong, F.; Nam, E.W. Relationship between Cognition, Depression, and Oral health status in Older adults: A longitudinal cross-lagged analysis. J. Affect. Disord. 2023, 330, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Preethanath, R.S.; Ibraheem, W.I.; Meshni, A.A.; Dawood, T.; Alam, M.N.; Anil, S. The Impact of Psychological Factors on Periodontitis in the Elderly: A Systematic Review. Eur. J. Dent. 2025. Online ahead of print. [Google Scholar] [CrossRef]
- Cademartori, M.G.; Gastal, M.T.; Nascimento, G.G.; Demarco, F.F.; Corrêa, M.B. Is depression associated with oral health outcomes in adults and elders? A systematic review and meta-analysis. Clin. Oral Investig. 2018, 22, 2685–2702. [Google Scholar] [CrossRef]
- Huang, C.; Song, M.; Wei, X.; Wang, X.; Dai, H.; Gou, Z.; Chenwu, F.; Jiang, Y.; Wan, J.; Guo, Y.; et al. Modelling analysis of dietary behaviors and oral health status to assess the impact on the mental well-being of elderly individuals: A cross-sectional survey study. Front. Nutr. 2025, 12, 1486987. [Google Scholar] [CrossRef] [PubMed]
- Krause, L.; Seeling, S.; Schienkiewitz, A.; Fuchs, J.; Petrakakis, P. Chewing ability and associated factors in older adults in Germany. Results from GEDA 2019/2020-EHIS. BMC Oral Health 2023, 23, 988. [Google Scholar] [CrossRef] [PubMed]
- Yesavage, J.A.; Brink, T.L.; Rose, T.L.; Lum, O.; Huang, V.; Adey, M.; Leirer, V.O. Development and validation of a geriatric depression screening scale: A preliminary report. J. Psychiatr. Res. 1982, 17, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Lesher, E.L.; Berryhill, J.S. Validation of the Geriatric Depression Scale–Short Form among inpatients. J. Clin. Psychol. 1994, 50, 256–260. [Google Scholar] [CrossRef]
- Yamamoto, T.; Aida, J.; Kondo, K.; Fuchida, S.; Tani, Y.; Saito, M.; Sasaki, Y. Oral Health and Incident Depressive Symptoms: JAGES Project Longitudinal Study in Older Japanese. J. Am. Geriatr. Soc. 2017, 65, 1079–1084. [Google Scholar] [CrossRef] [PubMed]
- Wright, F.A.C.; Takehara, S.; Stanaway, F.F.; Naganathan, V.; Blyth, F.M.; Hirani, V.; Le Couteur, D.G.; Handelsman, D.J.; Waite, L.M.; Seibel, M.J.; et al. Associations between oral health and depressive symptoms: Findings from the Concord Health and Ageing in Men Project. Australas. J. Ageing 2020, 39, e306–e314. [Google Scholar] [CrossRef]
- Lobo, A.; Saz, P.; Marcos, G.; Día, J.L.; de la Cámara, C.; Ventura, T.; Morales Asín, F.; Fernando Pascual, L.; Montañés, J.A.; Aznar, S. Revalidation and standardization of the cognition mini-exam (first Spanish version of the Mini-Mental Status Examination) in the general geriatric population. Med. Clin. 1999, 112, 767–774. [Google Scholar]
- Viebranz, S.; Dederichs, M.; Kwetkat, A.; Schüler, I.M. Effectiveness of Individual Oral Health Care Training in Hospitalized Inpatients in Geriatric Wards. Int. J. Environ. Res. Public Health 2023, 20, 4275. [Google Scholar] [CrossRef]
- Ripoll Perelló, J.; Barrés Fernández, P.C.; Pick Martín, J. Study of correlation between different scales that measure smoking dependence. Aten. Primaria 2023, 55, 102581. [Google Scholar] [CrossRef]
- Villanueva-Blasco, V.J.; Mateu-Mollá, J.; Villanueva-Silvestre, V.; Vázquez-Martínez, A. Relationship Between Depression and Risky Alcohol Consumption in Women: The Mediating Role of Coping Styles and Age. Int. J. Ment. Health Addict. 2022. Online ahead of print. [Google Scholar] [CrossRef]
- Mabuchi, T.; Hosomi, K.; Yokoyama, S.; Takada, M. Polypharmacy in elderly patients in Japan: Analysis of Japanese real-world databases. J. Clin. Pharm. Ther. 2020, 45, 991–996. [Google Scholar] [CrossRef]
- Silverman, M.P. Perspective on the Body Mass Index (BMI) and Variability of Human Weight and Height. J. Biosci. Med. 2025, 13, 309–320. [Google Scholar] [CrossRef]
- Vandenbulcke, P.A.I.; de Almeida Mello, J.; Schoebrechts, E.; De Lepeleire, J.; Declercq, A.; Declerck, D.; Duyck, J. Oral health of nursing home residents in Flanders, Belgium, and its associated factors. Sci. Rep. 2025, 15, 5463. [Google Scholar] [CrossRef] [PubMed]
- Mirza, F.; Nelson, M.; Ambers, J.; Milleman, K.; Milleman, J.; Ward, M. A Randomized, Parallel Design Study to Compare the Effects of Different Interdental Cleaning Modalities on Gingivitis and Plaque After a 6-Week Period of Home Use. Compend. Contin. Educ. Dent. 2024, 45 (Suppl. S1), 14–17. [Google Scholar]
- Porumb Chifor, I.; Leucuta, D.C.; Nigoghossian, M.; Culic, B.; Lucaciu, P.O.; Culic, C.; Badea, I.C.; Leghezeu, A.N.; Nicoara, A.G.; Simu, M.R. Caries Lesion Assessment Using 3D Virtual Models by Examiners with Different Degrees of Clinical Experience. Medicina 2023, 59, 2157. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Assariparambil, A.R.; Noronha, J.A.; Kamath, A.; Adhikari, P.; Nayak, B.S.; Shankar, R.; George, A. Depression among older adults: A systematic review of South Asian countries. Psychogeriatrics 2021, 21, 201–219. [Google Scholar] [CrossRef] [PubMed]
- Hu, T.; Zhao, X.; Wu, M.; Li, Z.; Luo, L.; Yang, C.; Yang, F. Prevalence of depression in older adults: A systematic review and meta-analysis. Psychiatry Res. 2022, 311, 114511. [Google Scholar] [CrossRef]
- Sempértegui, G.A.; Baliatsas, C.; Knipscheer, J.W.; Bekker, M.H.J. Depression among Turkish and Moroccan immigrant populations in Northwestern Europe: A systematic review of prevalence and correlates. BMC Psychiatry 2023, 23, 402. [Google Scholar] [CrossRef]
- Albert, P.R. Why is depression more prevalent in women? J. Psychiatry Neurosci. 2015, 40, 219–221. [Google Scholar] [CrossRef]
- Van de Velde, S.; Bracke, P.; Levecque, K. Gender differences in depression in 23 European countries. Cross-national variation in the gender gap in depression. Soc. Sci. Med. 2010, 71, 305–313. [Google Scholar] [CrossRef]
- Piccinelli, M.; Wilkinson, G. Gender differences in depression: Critical review. Br. J. Psychiatry 2000, 177, 486–492. [Google Scholar] [CrossRef]
- Kiran, T.; Halder, P.; Sharma, D.; Mehra, A.; Goel, K.; Behera, A. Distribution and association of depression with tobacco consumption among middle-aged and elderly Indian population: Nested multilevel modelling analysis of nationally representative cross-sectional survey. J. Health Popul. Nutr. 2025, 44, 61. [Google Scholar] [CrossRef]
- Bakhshaie, J.; Zvolensky, M.J.; Goodwin, R.D. Cigarette smoking and the onset and persistence of depression among adults in the United States: 1994–2005. Compr. Psychiatry 2015, 60, 142–148. [Google Scholar] [CrossRef]
- Liu, Q.; Leng, P.; Gu, Y.; Shang, X.; Zhou, Y.; Zhang, H.; Zuo, L.; Mei, G.; Xiong, C.; Wu, T.; et al. The dose-effect relationships of cigarette and alcohol consumption with depressive symptoms: A multiple-center, cross-sectional study in 5965 Chinese middle-aged and elderly men. BMC Psychiatry 2022, 22, 657. [Google Scholar] [CrossRef] [PubMed]
- Verlinden, J.J.; Moloney, M.E.; Vsevolozhskaya, O.A.; Whitehurst, L.N.; Weafer, J. Indirect effects of perceived stress and depression on the relationship between insomnia symptoms and hazardous drinking. Alcohol 2025, 123, 1–9. [Google Scholar] [CrossRef]
- Cobb, C.L. Depression, Drinking to Cope, and Alcohol Use Severity Among Latinos Who Drink: The Moderating Role of Sex. J. Clin. Psychol. 2025, 81, 62–70. [Google Scholar] [CrossRef]
- Scott, R.G.; Wiener, C.H.; Paulson, D. The Benefit of Moderate Alcohol Use on Mood and Functional Ability in Later Life: Due to Beers or Frequent Cheers? Gerontologist 2020, 60, 80–88. [Google Scholar] [CrossRef]
- Gea, A.; Beunza, J.J.; Estruch, R.; Sánchez-Villegas, A.; Salas-Salvadó, J.; Buil-Cosiales, P.; Gómez-Gracia, E.; Covas, M.I.; Corella, D.; Fiol, M.; et al. Alcohol intake, wine consumption and the development of depression: The PREDIMED study. BMC Med. 2013, 11, 192. [Google Scholar] [CrossRef]
- Schrempft, S.; Jackowska, M.; Hamer, M.; Steptoe, A. Associations between social isolation, loneliness, and objective physical activity in older men and women. BMC Public Health 2019, 19, 74. [Google Scholar] [CrossRef] [PubMed]
- Bludau, D.C.; Pabst, A.; Bleck, F.; Weyerer, S.; Maier, W.; Gensichen, J.; Mergenthal, K.; Bickel, H.; Fuchs, A.; Schäfer, I.; et al. Overweight, Obesity, and Depression in Multimorbid Older Adults: Prevalence, Diagnostic Agreement, and Associated Factors in Primary Care-Results from a Multicenter Observational Study. Nutrients 2025, 17, 1394. [Google Scholar] [CrossRef] [PubMed]
- Qiao, Z.; Wang, Z.; Qiu, J.; Zhang, J.; Cao, W. Analysis of the effect of BMI on depression and anxiety among older adults in China: The mediating role of ADL and IADL. Front. Public Health 2024, 12, 1387550. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.M.; Hur, Y.I. Relationship between obesity and depression in Korean adults: Korea National Health and Nutrition Examination Survey 2014. Medicine 2017, 96, e9478. [Google Scholar] [CrossRef]
- Neumann-Podczaska, A.; Tobis, S.; Antimisiaris, D.; Mossakowska, M.; Puzianowska-Kuznicka, M.; Chudek, J.; Wierucki, L.; Merks, P.; Wizner, B.; Sobieszczanska, M.; et al. Polypharmacy in Polish Older Adult Population-A Cross-Sectional Study: Results of the PolSenior Project. Int. J. Environ. Res. Public Health 2022, 19, 1030. [Google Scholar] [CrossRef]
- Al-Azayzih, A.; Alamoori, R.; Altawalbeh, S.M. Potentially inappropriate medications prescribing according to Beers criteria among elderly outpatients in Jordan: A cross-sectional study. Pharm. Pract. Granada 2019, 17, 1439. [Google Scholar] [CrossRef] [PubMed]
- Eyigor, S.; Kutsal, Y.G.; Toraman, F.; Durmus, B.; Gokkaya, K.O.; Aydeniz, A.; Paker, N.; Borman, P. Polypharmacy, Physical and Nutritional Status, and Depression in the Elderly: Do Polypharmacy Deserve Some Credits in These Problems? Exp. Aging Res. 2021, 47, 79–91. [Google Scholar] [CrossRef]
- Chen, C.; Feng, Z.; Fu, Q.; Wang, J.; Zheng, Z.; Chen, H.; Feng, D. Predictors of Polypharmacy Among Elderly Patients in China: The Role of Decision Involvement, Depression, and Taking Chinese Medicine Behavior. Front. Pharmacol. 2021, 12, 745688. [Google Scholar] [CrossRef]
- Thomson, W.M.; Ferguson, C.A.; Janssens, B.E.; Kerse, N.M.; Ting, G.S.; Smith, M.B. Xerostomia and polypharmacy among dependent older New Zealanders: A national survey. Age Ageing 2021, 50, 248–251. [Google Scholar] [CrossRef]
- Topsakal, M.S.; Oğuz, Ö. How do aging, socioeconomic status, and gender affect verbal fluency, cognitive skills, depression, and daily living activities in older people? Appl. Neuropsychol. Adult 2025, 16, 1–17. [Google Scholar] [CrossRef]
- Zhang, F.; Yang, W. Interaction between activities of daily living and cognitive function on risk of depression. Front. Public Health 2024, 12, 1309401. [Google Scholar] [CrossRef] [PubMed]
- Jin, L.; Jing, F. Effects of activity participation and cognitive levels on depression in middle-aged and older adults with chronic illness: A national cross-sectional study. Front. Psychol. 2024, 15, 1415715. [Google Scholar] [CrossRef] [PubMed]
- Kisely, S.; Baghaie, H.; Lalloo, R.; Siskind, D.; Johnson, N.W. A systematic review and meta-analysis of the association between poor oral health and severe mental illness. Psychosom. Med. 2015, 77, 83–92. [Google Scholar] [CrossRef]
- Barbosa, A.C.D.S.; Pinho, R.C.M.; Vasconcelos, M.M.V.B.; Magalhães, B.G.; Dos Santos, M.T.B.R.; de França Caldas Júnior, A. Association between symptoms of depression and oral health conditions. Spec. Care Dentist. 2018, 38, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Kunrath, I.; Silva, A.E.R. Oral health and depressive symptoms among older adults: Longitudinal study. Aging Ment. Health 2021, 25, 2265–2271. [Google Scholar] [CrossRef]
- Lu, L.; Liu, X.; Wang, H.; Liu, Q.; Liu, H.; Xiang, W.; Gu, W. Oral frailty status and influencing factors in a community-based elderly population: A systematic review and meta-analysis. BMC Oral Health 2025, 25, 1565. [Google Scholar] [CrossRef]
- Jungo, S.; Smail-Faugeron, V.; Guez, D.; Hoertel, N.; Lemogne, C.; Carra, M.C. Cross-sectional analysis of role of socioeconomic status in the association between depression and periodontitis. J. Periodontol. 2025. [Google Scholar] [CrossRef]
- Palomer, T.; Ramírez, V.; Ortuño, D. Relationship between oral health and depression: Data from the National Health Survey 2016–2017. BMC Oral Health 2024, 24, 188. [Google Scholar] [PubMed]
- Cui, Y.; Yang, L.; Du, J.; Duan, Y.; Qi, Q.; Liu, H. Relationships among oral hygiene behavior, toothache, and depressive symptoms in Chinese older adults. Clin. Oral Investig. 2023, 27, 6147–6155. [Google Scholar] [CrossRef]
- Altalhi, A.M.; Alqahtani, N.S.; Alareefi, J.A.; Alamri, S.S.; Almutairi, K.S.; Bin Dous, R.A.; Albaqami, I.A. A Comparative Review of Water Flossers in Periodontal Therapy. Cureus 2023, 15, e50162. [Google Scholar] [CrossRef]
- Ren, X.; He, J.; Cheng, R.; Chen, Y.; Xiang, Y.; Zhang, Y.; Jiang, S.; Li, J.; Cheng, L.; Hu, T. The Efficacy and Safety of Oral Irrigator on the Control of Dental Plaque and Gingivitis: A Randomized, Single-Blind, Parallel-Group Clinical Trial. Int. J. Environ. Res. Public Health 2023, 20, 3726. [Google Scholar] [CrossRef] [PubMed]
| Item | Question | Yes | No |
|---|---|---|---|
| 1 | Are you basically satisfied with your life? | ||
| 2 | Do you continue to engage in your usual activities and interests? | ||
| 3 | Do you feel that your life is full and happy? | ||
| 4 | Do you find enjoyment in your daily activities? | ||
| 5 | Are you generally in good spirits most of the time? | ||
| 6 | Do you live your life without fear? | ||
| 7 | Are you content during the day? | ||
| 8 | Do you feel cared for or looked after? | ||
| 9 | Do you prefer going out of your home or room rather than staying in? | ||
| 10 | Is your memory satisfactory? | ||
| 11 | Do you think it’s great to be alive? | ||
| 12 | Do you feel useful as you are now? | ||
| 13 | Do you feel full of energy? | ||
| 14 | Do you believe your situation is not hopeless? | ||
| 15 | Do you think most people are worse off than you? | ||
| Total score | |||
| 0–5 = No depression 6–10 = Moderate depression 11–15 = Severe depression | |||
| Function | Score and Description |
|---|---|
| Feeding | 10 = Independent 5 = Needs help cutting food 0 = Dependent |
| Bathing | 5 = Independent 0 = Dependent |
| Grooming | 5 = Independent (face washing, hair, teeth, shaving) 0 = Dependent |
| Dressing | 10 = Independent 5 = Needs help 0 = Dependent |
| Bowel Control | 10 = Continent 5 = Occasional accident or needs help 0 = Incontinent |
| Bladder Control | 10 = Continent 5 = Occasional accident or needs help 0 = Incontinent |
| Toilet Use | 10 = Independent 5 = Needs some assistance 0 = Dependent |
| Transfers (bed to chair) | 15 = Independent 10 = Minimal help 5 = Major help 0 = Dependent |
| Mobility (walking/wheelchair) | 15 = Independent walking 10 = Needs supervision/help 5 = Independent in wheelchair 0 = Dependent |
| Stair Climbing | 10 = Independent 5 = Needs help 0 = Dependent |
| Levels of Dependence | |
| 100 = Independent 91–99 = Slight dependence 61–90 = Moderate dependence 21–60 = Severe dependence 0–20 = Total dependence | |
| GDS | No. Cases (n = 181) | Percentage |
|---|---|---|
| No depression | 92 | 50.83% |
| Moderate depression | 63 | 34.81% |
| Severe depression | 26 | 14.36% |
| No Depression (n = 92) | Moderate Depression (n = 63) | Severe Depression (n = 26) | p Value | |
|---|---|---|---|---|
| Average age (years) | 76.22 ± 9.41 | 83.40 ± 8.50 | 83.92 ± 7.29 | <0.001 * |
| Gender | ||||
| Women (n = 109) | 48 (44.0%) | 44 (40.4%) | 17 (15.6%) | 0.074 ** |
| Men (n = 72) | 44 (61.1%) | 19 (26.4%) | 9 (12.5%) | |
| Smoking habit | ||||
| Non-smoker (n = 63) | 28 (44.5%) | 22 (34.9%) | 13 (20.6%) | 0.191 ** |
| <10 cigarettes/day (n = 16) | 7 (43.75%) | 9 (56.25%) | 0 (0.0%) | |
| 10–20 cigarettes/day (n = 5) | 3 (60.0%) | 2 (40.0%) | 0 (0.0%) | |
| >20 cigarettes/day (n = 10) | 5 (50.0%) | 5 (50.0%) | 0 (0.0%) | |
| Former smoker (n = 87) | 49 (56.3%) | 25 (28.7%) | 13 (15.0%) | |
| Alcohol consumption | ||||
| (0) Teetotaller (n = 83) | 40 (48.2%) | 25 (30.1%) | 18 (21.7%) (+) | 0.012 ** |
| (1) Man = 30 g/day + Woman = 20 g/day (n = 18) | 6 (33.3%) | 11 (61.1%) (+) | 1 (5.6%) | |
| (2) Man = 30–50 g/day + Woman = 20–32 g/day (n = 20) | 13 (65.0%) | 6 (30.0%) | 1 (5.0%) | |
| (3) Man = 51–120 g/day + Woman = 33–80 g/day (n = 11) | 9 (81.8%) (+) | 2 (18.2%) | 0 (0.0%) | |
| (4) Man >120 g/day + Woman >80 g/day (n = 9) | 1 (11.1%) (−) | 6 (66.7%) (+) | 2 (22.2%) | |
| (5) Former drinker (n = 40) | 23 (57.5%) | 13 (32.5%) | 4 (10.0%) | |
| BMI | ||||
| Severe underweight (n = 0) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.016 ** |
| Underweight (n = 1) | 0 (0.0%) | 1 (100.0%) | 0 (0.0%) | |
| Normal weight (n = 68) | 38 (55.9%) | 22 (32.3%) | 8 (11.8%) | |
| Overweight (n = 46) | 14 (30.4%) (−) | 20 (43.5%) | 12 (26.1%) (+) | |
| Class I obesity (n = 41) | 29 (70.7%) (+) | 8 (19.5%) (−) | 4 (9.8%) | |
| Class II obesity (n = 12) | 6 (50.0%) | 6 (50.0%) | 0 (0.0%) | |
| Class III obesity (n = 13) | 5 (38.5%) | 6 (46.1%) | 2 (15.4%) | |
| Antidepressant use | ||||
| No (n = 58) | 48 (82.8%) (+) | 10 (17.2%) (−) | 0 (0.0%) (−) | <0.001 ** |
| Yes (n = 123) | 44 (35.8%) (−) | 53 (43.1%) (+) | 26 (21.1%) (+) | |
| Use of other medications | ||||
| <5 medications (n = 63) | 38 (60.3%) | 20 (31.8%) | 5 (7.9%) | 0.093 ** |
| ≥5 medications (n = 118) | 54 (45.8%) | 43 (36.4%) | 21 (17.8%) | |
| Dry mouth sensation | ||||
| No (n = 118) | 60 (50.8%) | 42 (35.6%) | 16 (13.6%) | 0.899 ** |
| Yes (n = 63) | 32 (50.8%) | 21 (33.3%) | 10 (15.9%) |
| No Depression (n = 92) | Moderate Depression (n = 63) | Severe Depression (n = 26) | p Value | |
|---|---|---|---|---|
| Total dependency Severe dependency Moderate dependency Low dependency Independent | 0 (0.0%) (−) 8 (20.5%) (−) 28 (44.4%) 9 (100.0%) (+) 47 (85.5%) (+) | 14 (50.0%) 26 (66.7%) (+) 15 (34.9%) 0 (0.0%) (−) 8 (14.5%) (−) | 14 (50.0%) (+) 5 (12.8%) 7 (20.6%) 0 (0.0%) 0 (0.0%) (−) | <0.001 ** |
| Average Barthel Index score and SD | 87.77 ± 18.29 | 54.44 ± 29.92 | 28.85 ± 28.99 | <0.001 * |
| No Depression (n = 92) | Moderate Depression (n = 63) | Severe Depression (n = 26) | p Value * | |
|---|---|---|---|---|
| Mean/SD | ||||
| Number of cavities | 3.13 ± 2.09 | 2.56 ± 2.76 | 1.85 ± 1.46 | 0.005 |
| Root caries | 2.21 ± 1.74 | 1.89 ± 2.11 | 2.19 ± 1.69 | 0.271 |
| Radicular remains | 1.42 ± 1.87 | 3.51 ± 3.83 | 6.69 ± 6.32 | <0.001 |
| No Depression (n = 92) | Moderate Depression (n = 63) | Severe Depression (n = 26) | p Value ** | |
|---|---|---|---|---|
| MGI/Gingivitis | ||||
| Absent-normal Mild Moderate Severe | 19 (86.4%) (+) 42 (85.7%) (+) 28 (39.4%) (−) 3 (7.7%) (−) | 1 (4.5%) (−) 7 (14.3%) (−) 36 (50.7%) (+) 19 (48.7%) (+) | 2 (9.1%) 0 (0.0%) (−) 7 (9.9%) 17 (43.6%) (+) | <0.001 |
| Brushing frequency | ||||
| None Once Twice 3 times | 17 (41.5%) 23 (46.0%) 17 (50.0%) 35 (62.5%) | 13 (31.7%) 19 (38.0%) 12 (35.3%) 19 (33.9%) | 11 (26.8%) 8 (16.0%) 5 (14.7%) 2 (3.6%) | 0.067 |
| Use of water jet | ||||
| No Yes | 74 (49.0%) 18 (60.0%) | 52 (34.4%) 11 (36.7%) | 25 (16.6%) 1 (3.3%) | 0.159 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abregú-Flores, C.E.; Ruiz-Sáenz, P.L.; Andrés-Veiga, M.; Fernández-Cáliz, F.; Meniz-García, C.; Martínez-Rodríguez, N. Depression, Functional Dependence, and Oral Health: Evidence from a Clinical Study of Older Spanish Adults. Diagnostics 2025, 15, 2934. https://doi.org/10.3390/diagnostics15222934
Abregú-Flores CE, Ruiz-Sáenz PL, Andrés-Veiga M, Fernández-Cáliz F, Meniz-García C, Martínez-Rodríguez N. Depression, Functional Dependence, and Oral Health: Evidence from a Clinical Study of Older Spanish Adults. Diagnostics. 2025; 15(22):2934. https://doi.org/10.3390/diagnostics15222934
Chicago/Turabian StyleAbregú-Flores, Carmen Esperanza, Pedro Luis Ruiz-Sáenz, María Andrés-Veiga, Fernando Fernández-Cáliz, Cristina Meniz-García, and Natalia Martínez-Rodríguez. 2025. "Depression, Functional Dependence, and Oral Health: Evidence from a Clinical Study of Older Spanish Adults" Diagnostics 15, no. 22: 2934. https://doi.org/10.3390/diagnostics15222934
APA StyleAbregú-Flores, C. E., Ruiz-Sáenz, P. L., Andrés-Veiga, M., Fernández-Cáliz, F., Meniz-García, C., & Martínez-Rodríguez, N. (2025). Depression, Functional Dependence, and Oral Health: Evidence from a Clinical Study of Older Spanish Adults. Diagnostics, 15(22), 2934. https://doi.org/10.3390/diagnostics15222934






