Diagnostic Assessment of Maxillary Sinus Membrane Thickening Associated with Dental Implant Perforation Using Cone-Beam Computed Tomography: A Retrospective Cross-Sectional Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Context and Participants
2.3. Clinical Data Collection
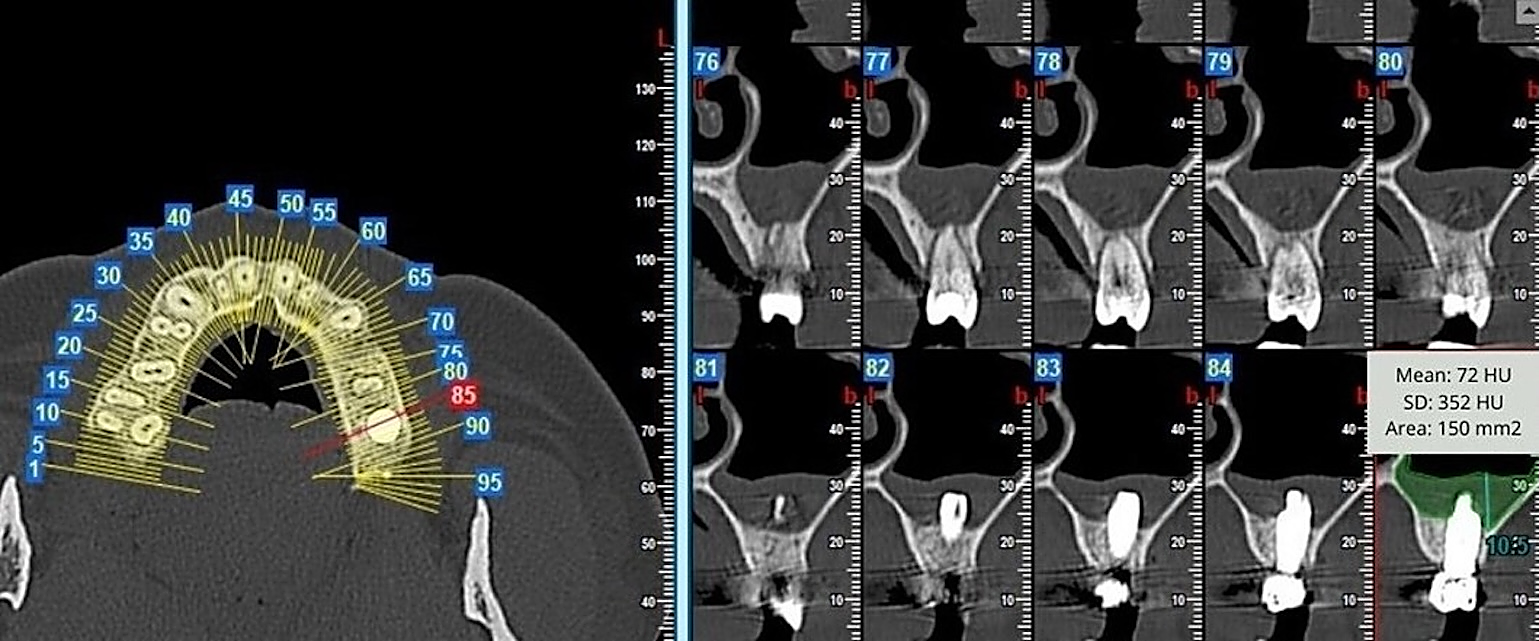
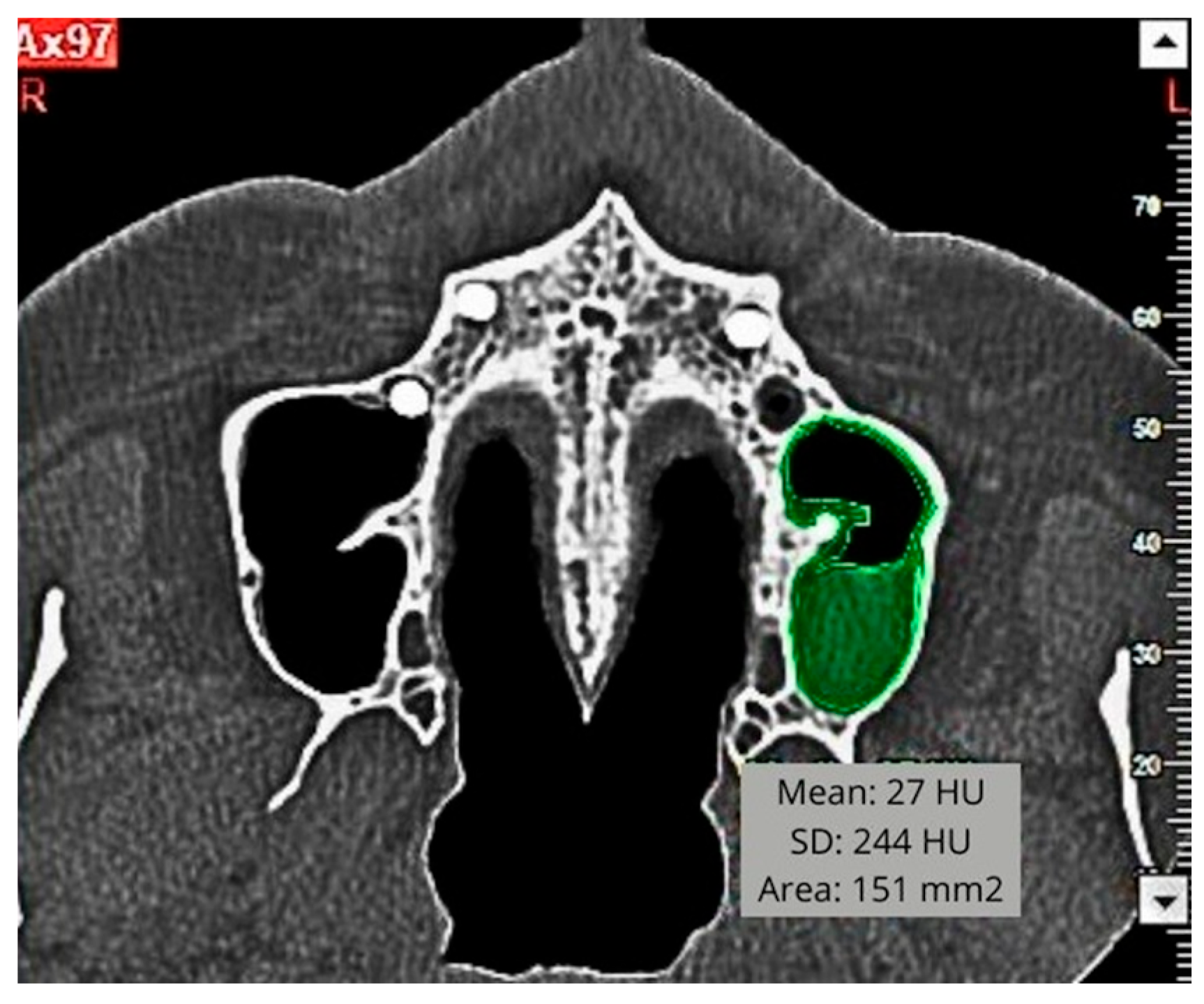
2.4. Radiological Data Assessment
2.5. Morphometric Measurements
2.6. Statistical Analysis
3. Results
3.1. Clinical Data Analysis
3.2. Radiological Data Analysis
4. Discussion
4.1. Interpretation
4.2. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CBCT | Cone Beam Computed Tomography |
| SMT | Sinus membrane thickening |
| HU | Hounsfield units |
References
- Bernardi, S.; Bianchi, S.; Gerardi, D.; Petrelli, P.; Rinaldi, F.; Piattelli, M.; Macchiarelli, G.; Varvara, G. Anatomy of Maxillary Sinus: Focus on Vascularization and Underwood Septa via 3D Imaging. Tomography 2024, 10, 444–458. [Google Scholar] [CrossRef]
- Rey-Martínez, M.H.; Ruiz-Sáenz, P.L.; Martínez-Rodríguez, N.; Barona-Dorado, C.; Meniz-García, C.; Cortés-Bretón Brinkmann, J.; Suárez-Quintanilla, J.A.; Martínez-González, J.M. Analysis of the Radiological Changes of the Sinus Membrane Using Cone Beam Computed Tomography and Its Relationship with Dental Treatments. A Retrospective Study. Biology 2022, 11, 165. [Google Scholar] [CrossRef]
- Scavia, S.; Audino, E.; Salgarello, S. Ridge Preservation Combined with Open Barrier Membrane Technique in Case of Postextractive Oroantral Communication: A Case Series Retrospective Study. J. Oral Implantol. 2024, 50, 141–152. [Google Scholar] [CrossRef]
- Jafer, M.A.; Salem, R.M.; Hakami, F.B.; Ageeli, R.E.; Alhazmi, T.A.; Bhandi, S.; Patil, S. Techniques for Extraction Socket Regeneration for Alveolar Ridge Preservation. J. Contemp. Dent. Pract. 2022, 23, 245–250. [Google Scholar]
- Molina, A.; Sanz-Sánchez, I.; Sanz-Martín, I.; Ortiz-Vigón, A.; Sanz, M. Complications in sinus lifting procedures: Classification and management. Periodontology 2000 2022, 88, 103–115. [Google Scholar] [CrossRef]
- Nooh, N. Effect of schneiderian membrane perforation on posterior maxillary implant survival. J. Int. Oral Health 2013, 5, 28–34. [Google Scholar] [PubMed]
- Ahmad, A.G.; Awadalkreem, F.; Osman, M.; Palka, L. Does the Protrusion of Corticobasal Implants in the Maxillary Sinuses Affect Sinus Health? A Retrospective Study. J. Contemp. Dent. Pract. 2023, 24, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Awadalkreem, F.; Ahmad, A.G.; Ihde, S.; Osman, M. Effects of Corticobasal Implant Protrusion inside the Nasal and Maxillary Sinus. Ann. Maxillofac. Surg. 2020, 10, 114–121. [Google Scholar] [CrossRef]
- Lazarov, A. A Prospective Cohort Study of Maxillary Sinus Complications in Relation to Treatments with Strategic Implants® Penetrating into the Sinus. Ann. Maxillofac. Surg. 2020, 10, 365–369. [Google Scholar] [CrossRef] [PubMed]
- Chaves, L.L.V.; Lopes Rosado, L.P.; Piccolo, S.M.; Ferreira, L.M.; Kamburoglu, K.; Junqueira, R.B.; Aquino de Castro, M.A.; Verner, F.S. Evaluation of the Maxillary Sinus of Patients with Maxillary Posterior Implants: A CBCT Cross-Sectional Study. Diagnostics 2022, 12, 3169. [Google Scholar] [CrossRef]
- Ragucci, G.M.; Elnayef, B.; Suárez-López Del Amo, F.; Wang, H.L.; Hernández-Alfaro, F.; Gargallo-Albiol, J. Influence of exposing dental implants into the sinus cavity on survival and complications rate: A systematic review. Int. J. Implant. Dent. 2019, 5, 6. [Google Scholar] [CrossRef]
- Oliveira-Santos, N.; Beersingh, A.H.; Felizardo, H.M.A.; Groppo, F.C.; Gaêta-Araujo, H. Association between maxillary sinus floor perforation by dental implants and mucosal thickening: A cone-beam computed tomography study. J. Dent. 2024, 144, 104963. [Google Scholar] [CrossRef]
- Brandstaetter, T.; Ziv, O.; Sagy, I.; Segal, N.; Schneider, S.; Givol, N.; Levin, L.; Zadik, Y.; Kordeluk, S. Perforating dental implants and maxillary sinus pathology. Oral Maxillofac. Surg. 2024, 28, 715–721. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- Maillet, M.; Bowles, W.R.; McClanahan, S.L.; John, M.T.; Ahmad, M. Cone-beam computed tomography evaluation of maxillary sinusitis. J. Endod. 2011, 37, 753–757. [Google Scholar] [CrossRef] [PubMed]
- Lupi, E.; Ciciarelli, G.; Bernardi, S.; Gerardi, D.; D’Armario, M.; Bianchi, S.; Giovannetti, F. The Bony Window Technique as a mini-invasive surgery to retrieve foreign bodies in the maxillary sinus: A technical note. Oper. Tech. Otolaryngol. 2024, 35, 242–248. [Google Scholar] [CrossRef]
- Chirilă, L.; Rotaru, C.; Filipov, I.; Săndulescu, M. Management of acute maxillary sinusitis after sinus bone grafting procedures with simultaneous dental implants placement—A retrospective study. BMC Infect. Dis. 2016, 16, 17–22. [Google Scholar] [CrossRef]
- Ueno, D.; Banba, N.; Hasuike, A.; Ueda, K.; Kodama, T.A. Sinus floor reaugmentation technique around an apically exposed implant into the maxillary sinus. J. Oral Implantol. 2019, 45, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Lascala, C.A.; Panella, J.; Marques, M.M. Analysis of the accuracy of linear measurements obtained by cone beam computed tomography (CBCT -NewTom). Dentomaxillofac. Radiol. 2004, 33, 291–294. [Google Scholar] [CrossRef]
- Chen, H.; van Eijnatten, M.; Wolff, J.; de Lange, J.; van der Stelt, P.F.; Lobbezoo, F.; Aarab, G. Reliability and accuracy of three imaging software packages used for 3D analysis of the upper airway on cone beam computed tomography images. Dentomaxillofac. Radiol. 2017, 46, 20170043. [Google Scholar] [CrossRef]
- Parks, E.T. Cone Beam Computed Tomography for the nasal cavity and paranasal sinuses. Dent. Clin. N. Am. 2014, 58, 627–651. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Filleul, O.; Costa de Araujo, P.; Hsieh, J.W.; Chantrain, G.; Saussez, S. Chronic maxillary rhinosinusitis of dental origin: A systematic review of 674 patient cases. Int. J. Otolaryngol. 2014, 2014, 465173. [Google Scholar] [CrossRef]
- Quirynen, M.; Lefever, D.; Hellings, P.; Jacobs, R. Transient swelling of the Schneiderian membrane after transversal sinus augmentation: A pilot study. Clin. Oral Implants Res. 2014, 25, 36–41. [Google Scholar] [CrossRef]
- Munakata, M.; Yamaguchi, K.; Sato, D.; Yajima, N.; Tachikawa, N. Factors influencing the sinus membrane thickness in edentulous regions: A cone-beam computed tomography study. Int. J. Implant Dent. 2021, 7, 16. [Google Scholar] [CrossRef]
- Ruhi, S.; Sunira, C.; Parvathi, D.; Neeraj, T.; Kunal, S.; Navdeep, K. Forensic importance of maxillary sinus in gender determination: A morphometric analysis from Western Uttar Pradesh, India. Eur. J. General Dent. 2014, 3, 53–56. [Google Scholar]
- Ritter, L.; Lutz, J.; Neugebauer, J.; Scheer, M.; Dreiseidler, T.; Zinser, M.J.; Rothamel, D.; Mischkowski, R.A. Prevalence of pathologic findings in the maxillary sinus in cone-beam computerized tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011, 111, 634–640. [Google Scholar] [CrossRef]
- Jung, J.H.; Choi, B.H.; Zhu, S.J.; Lee, S.H.; Huh, J.Y.; You, T.M.; Lee, H.J.; Li, J. The effects of exposing dental implants to the maxillary sinus cavity on sinus complications. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 102, 602–605. [Google Scholar] [CrossRef]
- Jung, J.H.; Choi, B.H.; Jeong, S.M.; Li, J.; Lee, S.H.; Lee, H.J. A retrospective study of the effects on sinus complications of exposing dental implants to the maxillary sinus cavity. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 103, 623–625. [Google Scholar] [CrossRef]
- Whyte, A.; Boeddinghaus, R. The maxillary sinus: Physiology, development and imaging anatomy. Dentomaxillofac. Radiol. 2019, 48, 20190205. [Google Scholar] [CrossRef]
- Tataryn, R.W.; Lewis, M.J.; Horalek, M.L.; Thompson, C.G.; Cha, B.Y.; Pokorny, A.T. Maxillary Sinusitis of Endodontic Origin. American Association of Endodontists Position Statement. American Association of Endodontists. 2018, pp. 1–18. Available online: https://www.aae.org/specialty/wp-content/uploads/sites/2/2018/04/AAE_PositionStatement_MaxillarySinusitis.pdf (accessed on 14 November 2024).
- Tabrizi, R.; Amid, R.; Özkan, B.T.; Khorshidi, H.; Langner, N.J. Effects of exposing dental implant to the maxillary sinus cavity. J. Craniofac. Surg. 2012, 23, 767–769. [Google Scholar] [CrossRef] [PubMed]
- Elhamrouni, L.M.; Marzook, H.A.; Ahmed, W.M.; Abdul-Rahman, M. Experimental study on penetration of dental implants into the maxillary sinus at different depths. Oral Maxillofac. Surg. 2016, 20, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Suomalainen, A.; Vehmas, T.; Kortesniemi, M.; Robinson, S.; Peltola, J. Accuracy of linear measurements using dental cone beam and conventional multislice computed tomography. Dentomaxillofac. Radiol. 2008, 37, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Soikkonen, K.; Ainamo, A. Radiographic maxillary sinus findings in the elderly. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1995, 80, 487–491. [Google Scholar] [CrossRef] [PubMed]
- Kato, S.; Omori, Y.; Kanayama, M.; Hirota, A.; Ferri, M.; Apaza Alccayhuaman, K.A.; Botticelli, D. Sinus Mucosa Thickness Changes and Ostium Involvement after Maxillary Sinus Floor Elevation in Sinus with Septa. A Cone Beam Computed Tomography Study. Dent. J. 2021, 9, 82. [Google Scholar] [CrossRef]
- Insua, A.; Monje, A.; Chan, H.L.; Zimmo, N.; Shaikh, L.; Wang, H.L. Accuracy of Schneiderian membrane thickness: A cone-beam computed tomography analysis with histological validation. Clin. Oral Implants Res. 2017, 28, 654–661. [Google Scholar] [CrossRef]
- Craig, J.R.; Tataryn, R.W.; Cha, B.Y.; Bhargava, P.; Pokorny, A.; Gray, S.T.; Mattos, J.L.; Poetker, D.M. Diagnosing odontogenic sinusitis of endodontic origin: A multidisciplinary literature review. Am. J. Otolaryngol. 2021, 42, 102925. [Google Scholar] [CrossRef]
- Crovetto-Martínez, R.; Martin-Arregui, F.J.; Zabala-López de Maturana, A.; Tudela-Cabello, K.; Crovetto-de la Torre, M.A. Frequency of the odontogenic maxillary sinusitis extended to the anterior ethmoid sinus and response to surgical treatment. Med. Oral Patol. Oral Cir. Bucal 2014, 19, e409–e413. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Female or male patients over 18 years old. | Patients restored with implants requiring bone regeneration procedures in the maxillary sinus area. |
| Patients with no sinus membrane alterations witnessed in the preoperative CBCT. | Patients with rhinosinusitis history. |
| Patients with implants perforating the maxillary sinus floor. | Patients under treatment with nebulizers or nasal decongestants. |
| Patients with >2 mm sinus mucosa thickening evaluated by CBCT after the intervention. |
| Patient | Age | Gender | NPI | Affected Side | IPL (mm) Panoramic | IPL (mm) Orthoradial |
|---|---|---|---|---|---|---|
| 1 | 45 | M | 1 | R | 0.6 | 0.6 |
| 2 | 61 | F | 2 | R | 6.3 | 4.1 |
| 3 | 76 | M | 2 | R | 2.4 | 2.1 |
| 4 | 69 | M | 1 | R | 1.5 | 2.1 |
| 5 | 68 | M | 1 | L | 4.8 | 4.5 |
| 6 | 78 | F | 1 | R | 1.5 | 2.1 |
| 7 | 81 | F | 2 | L | 0.9 | 0.6 |
| 8 | 51 | F | 1 | L | 2.7 | 5.1 |
| 9 | 85 | F | 1 | R | 2.7 | 2.1 |
| 10 | 77 | F | 1 | R | 2.1 | 1.5 |
| 11 | 88 | F | 2 | L | 2.4 | 3.3 |
| 12 | 69 | M | 1 | L | 0.6 | 0.3 |
| 13 | 78 | F | 1 | L | 1.8 | 5.1 |
| 14 | 77 | F | 1 | L | 2.5 | 1.2 |
| 15 | 69 | M | 2 | R | 2.4 | 3.3 |
| 16 | 49 | M | 1 | L | 1.5 | 1.2 |
| 17 | 75 | F | 2 | L | 5.1 | 1.2 |
| 18 | 74 | M | 1 | R | 4.2 | 2.4 |
| 19 | 76 | M | 1 | L | 1.5 | 1.5 |
| 20 | 88 | F | 2 | R | 1.2 | 0.9 |
| 21 | 43 | M | 2 | R | 2.7 | 2.2 |
| Patient | SMT Pattern | SMT Area (mm2) | SMT Density (HU) | SMT Max Height (mm) T1-T0 | |||||
|---|---|---|---|---|---|---|---|---|---|
| Pn | Ort | Ax | Pn | Ort | Ax | Pn | Ort | ||
| 1 | C | 221.94 | 153.36 | 280.98 | 242.4 | 63.4 | 287.1 | 17.1 | 16.7 |
| 2 | C | 160.9 | 118.26 | 141.03 | 74.2 | 306.8 | 461.3 | 11.9 | 13.1 |
| 3 | C | 117.45 | 57.15 | 172.8 | 261.8 | 353.9 | 558.6 | 3.1 | 2.1 |
| 4 | H | 201.33 | 50.4 | 191.43 | 119.2 | 343.3 | 205.1 | 11.2 | 2.7 |
| 5 | C | 348.39 | 119.07 | 209.61 | 165.3 | 81.2 | 307.5 | 19.2 | 11.7 |
| 6 | H | 321.66 | 129.42 | 236.52 | 86.1 | 35.8 | 247.1 | 11.4 | 9.2 |
| 7 | H | 114.12 | 70.74 | 111.78 | 152.2 | 430.8 | 256.3 | 17.7 | 6.0 |
| 8 | C | 289.35 | 207.9 | 364.32 | 196.5 | 107.7 | 165.0 | 19.7 | 19.5 |
| 9 | C | 506.34 | 153.09 | 310.14 | 166.3 | 113.2 | 197.4 | 18.0 | 14.9 |
| 10 | C | 116.73 | 72.75 | 109.53 | 145.0 | 108.3 | 365.9 | 15.9 | 2.3 |
| 11 | C | 411.12 | 209.88 | 317.16 | 128.0 | 91.4 | 219.4 | 21.3 | 23.6 |
| 12 | C | 169.11 | 96.39 | 99.36 | 23.7 | 179.5 | 480.0 | 16.7 | 3.6 |
| 13 | C | 112.32 | 58.95 | 82.26 | 96.1 | 41.8 | 247.3 | 2.4 | 3.0 |
| 14 | H | 199.89 | 111.33 | 404.37 | 21.8 | 186.6 | 343.3 | 9.9 | 13.2 |
| 15 | C | 234.54 | 85.5 | 269.73 | 71.2 | 428.5 | 178.8 | 9.3 | 9.8 |
| 16 | C | 78.84 | 17.55 | 60.12 | 366.2 | 404.8 | 271.0 | 4.2 | 2.8 |
| 17 | C | 219.24 | 105.39 | 189.63 | 179.9 | 703.4 | 327.3 | 8.1 | 4.5 |
| 18 | C | 173.52 | 97.74 | 233.73 | 248.2 | 188.7 | 320.5 | 5.1 | 12.4 |
| 19 | H | 136.26 | 36.63 | 120.87 | 72.5 | 218.4 | 584.0 | 3.0 | 3.2 |
| 20 | C | 223.74 | 154.71 | 290.88 | 335.7 | 115.5 | 395.6 | 3.7 | 10.5 |
| 21 | H | 238.32 | 83.97 | 89.73 | 295.1 | 278.1 | 582.0 | 4.5 | 3.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kemcha, N.; Andrés-Veiga, M.; Hurtado-Celotti, D.; Meniz-García, C.; Beca-Campoy, T.; Martínez-Rodríguez, N. Diagnostic Assessment of Maxillary Sinus Membrane Thickening Associated with Dental Implant Perforation Using Cone-Beam Computed Tomography: A Retrospective Cross-Sectional Pilot Study. Diagnostics 2025, 15, 2809. https://doi.org/10.3390/diagnostics15212809
Kemcha N, Andrés-Veiga M, Hurtado-Celotti D, Meniz-García C, Beca-Campoy T, Martínez-Rodríguez N. Diagnostic Assessment of Maxillary Sinus Membrane Thickening Associated with Dental Implant Perforation Using Cone-Beam Computed Tomography: A Retrospective Cross-Sectional Pilot Study. Diagnostics. 2025; 15(21):2809. https://doi.org/10.3390/diagnostics15212809
Chicago/Turabian StyleKemcha, Narjesse, María Andrés-Veiga, Dolores Hurtado-Celotti, Cristina Meniz-García, Tomás Beca-Campoy, and Natalia Martínez-Rodríguez. 2025. "Diagnostic Assessment of Maxillary Sinus Membrane Thickening Associated with Dental Implant Perforation Using Cone-Beam Computed Tomography: A Retrospective Cross-Sectional Pilot Study" Diagnostics 15, no. 21: 2809. https://doi.org/10.3390/diagnostics15212809
APA StyleKemcha, N., Andrés-Veiga, M., Hurtado-Celotti, D., Meniz-García, C., Beca-Campoy, T., & Martínez-Rodríguez, N. (2025). Diagnostic Assessment of Maxillary Sinus Membrane Thickening Associated with Dental Implant Perforation Using Cone-Beam Computed Tomography: A Retrospective Cross-Sectional Pilot Study. Diagnostics, 15(21), 2809. https://doi.org/10.3390/diagnostics15212809






