How to Perform Cardiac Contrast-Enhanced Ultrasound (cCEUS): Part II—Advanced Applications and Interpretation
Abstract
1. Introduction
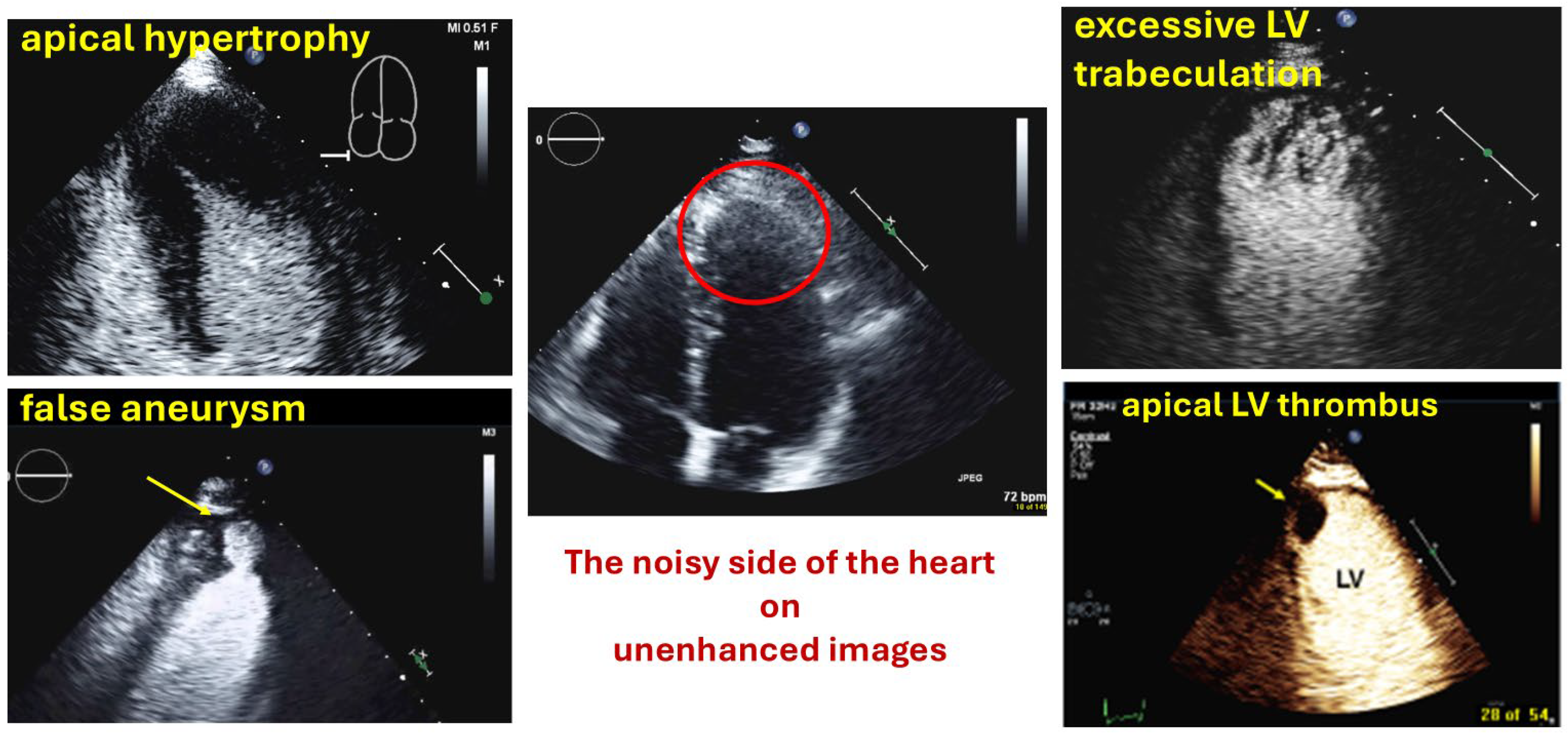
Echocardiography with UEAs for Assessment of Left Ventricular Aneurysm, Masses and Myocardial Disease
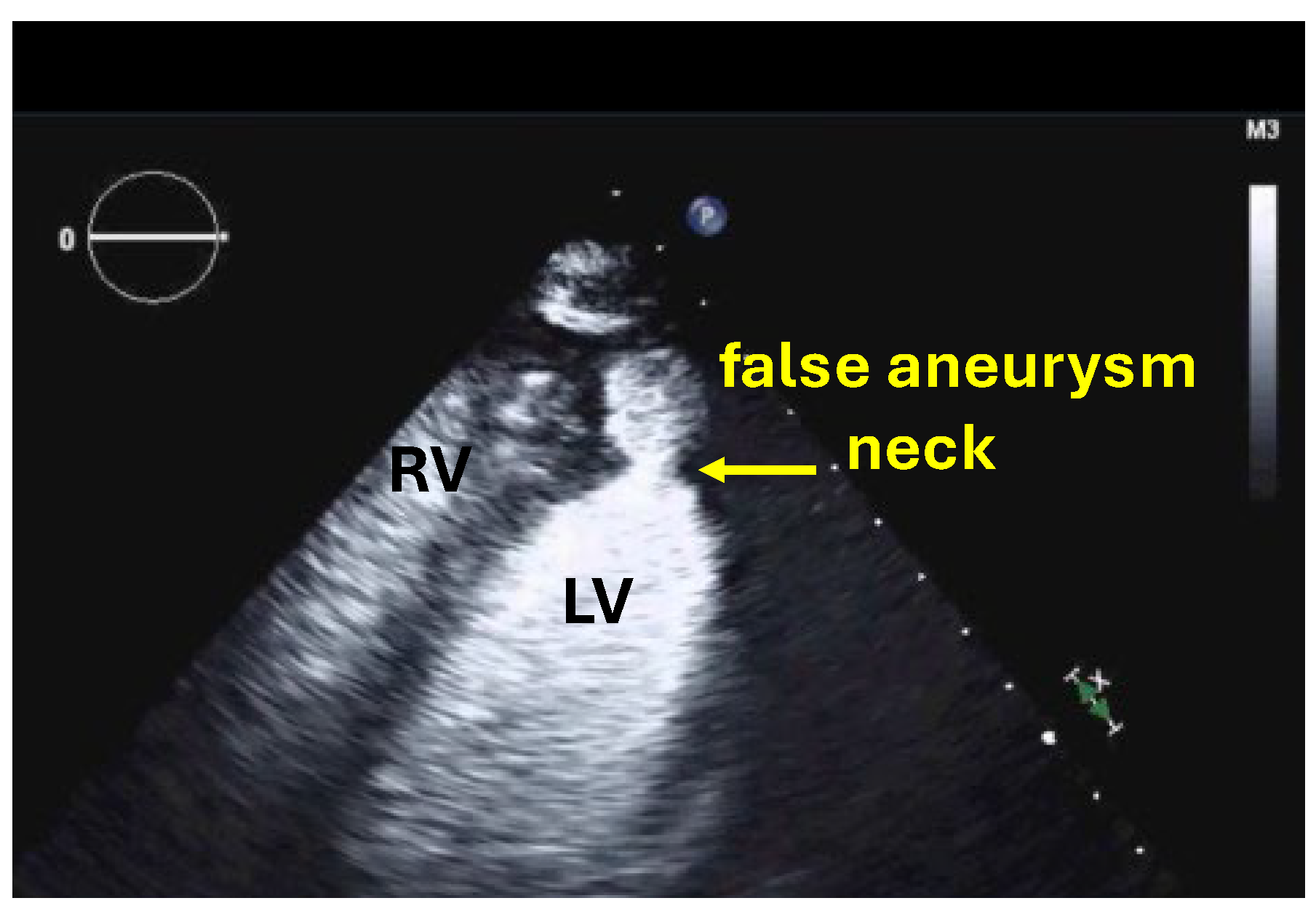
2. Left Ventricular Aneurysms
2.1. Background and Indications
2.2. Preparation and Performance
2.2.1. Technical Aspects, Settings
2.2.2. Pre-Assessment and Primary Scan Planes
2.2.3. CEUS Procedure
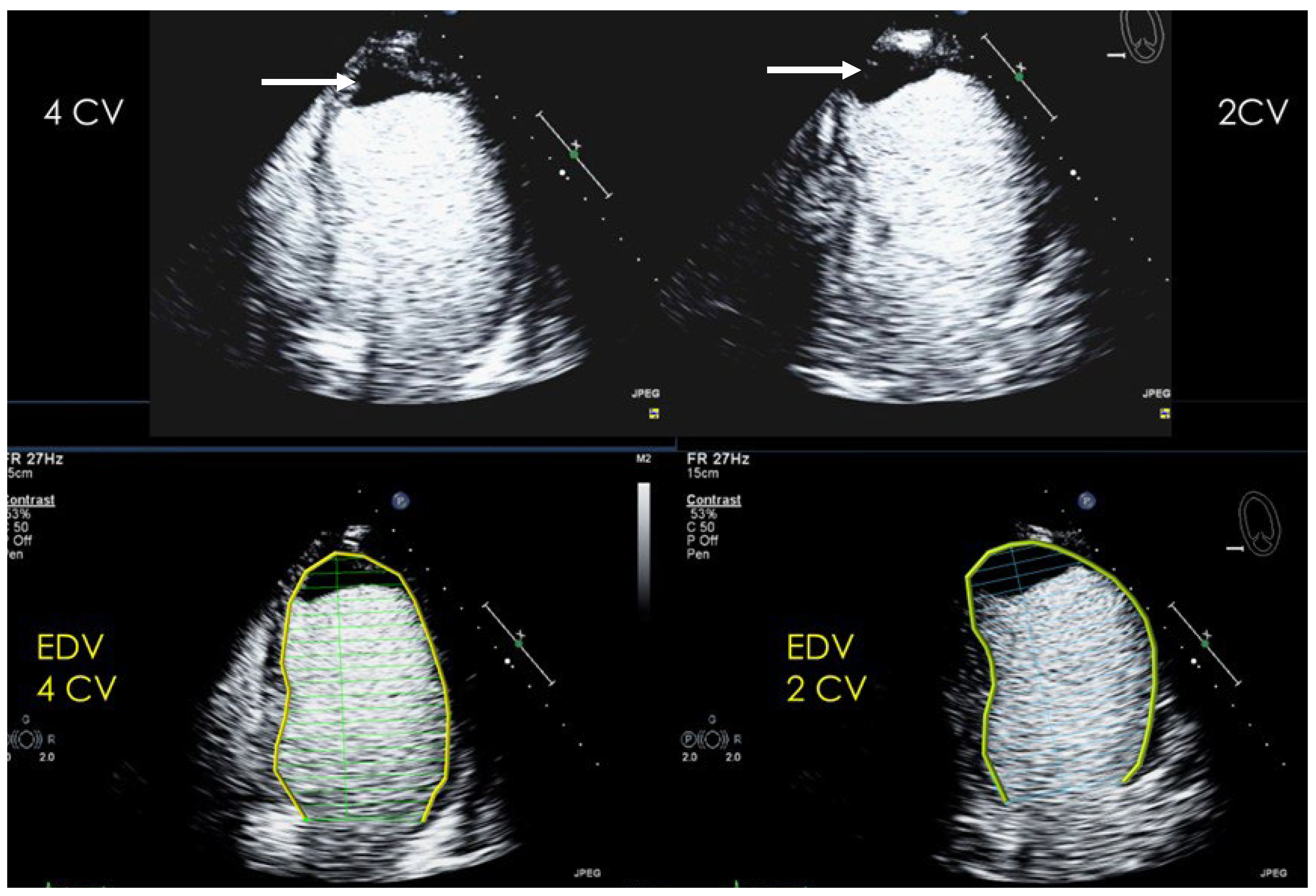
2.3. Interpretation and Reporting
2.4. Pitfalls
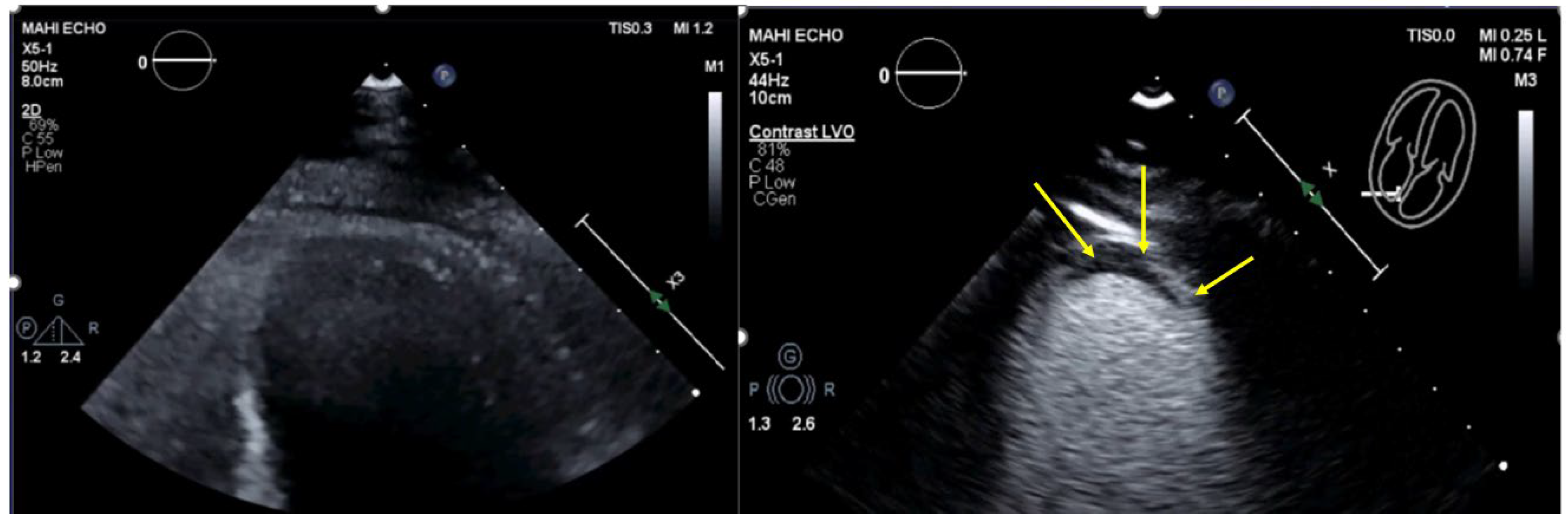
3. Left Ventricular Thrombi and Tumors
3.1. Background and Indications
3.2. Preparation and Performance
3.2.1. Technical Aspects, Settings for Echocardiography with UEAs
3.2.2. Pre-Assessment and Primary Scan Planes
3.2.3. CEUS Procedure
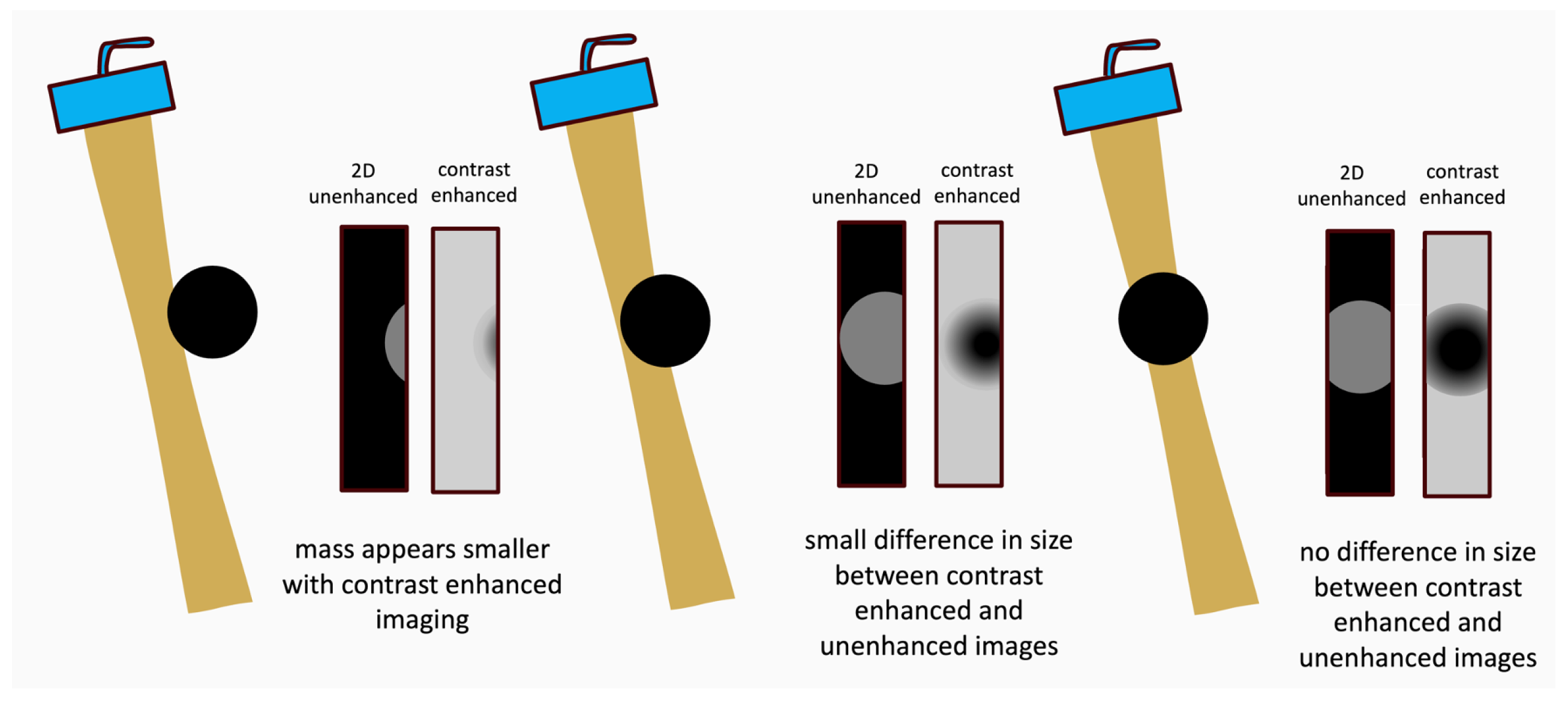
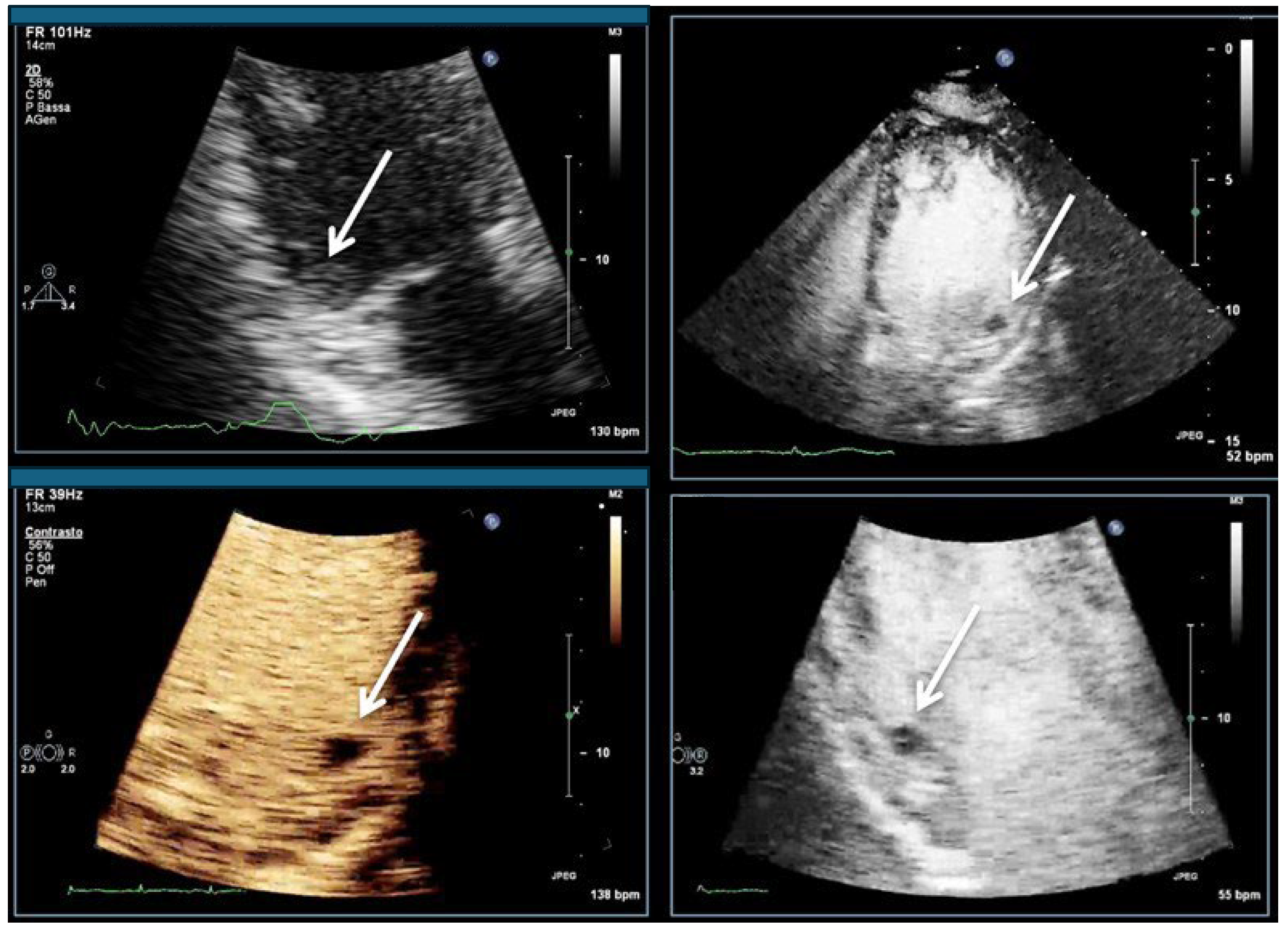
3.3. Interpretation and Reporting
3.4. Pitfalls
3.5. Alternative Imaging Methods
4. Hypertrophic Cardiomyopathy
4.1. Background and Indications
4.2. Preparation and Performance
4.2.1. Technical Aspects, Settings
4.2.2. Pre-Assessment and Primary Scan Planes
4.2.3. CEUS Procedure
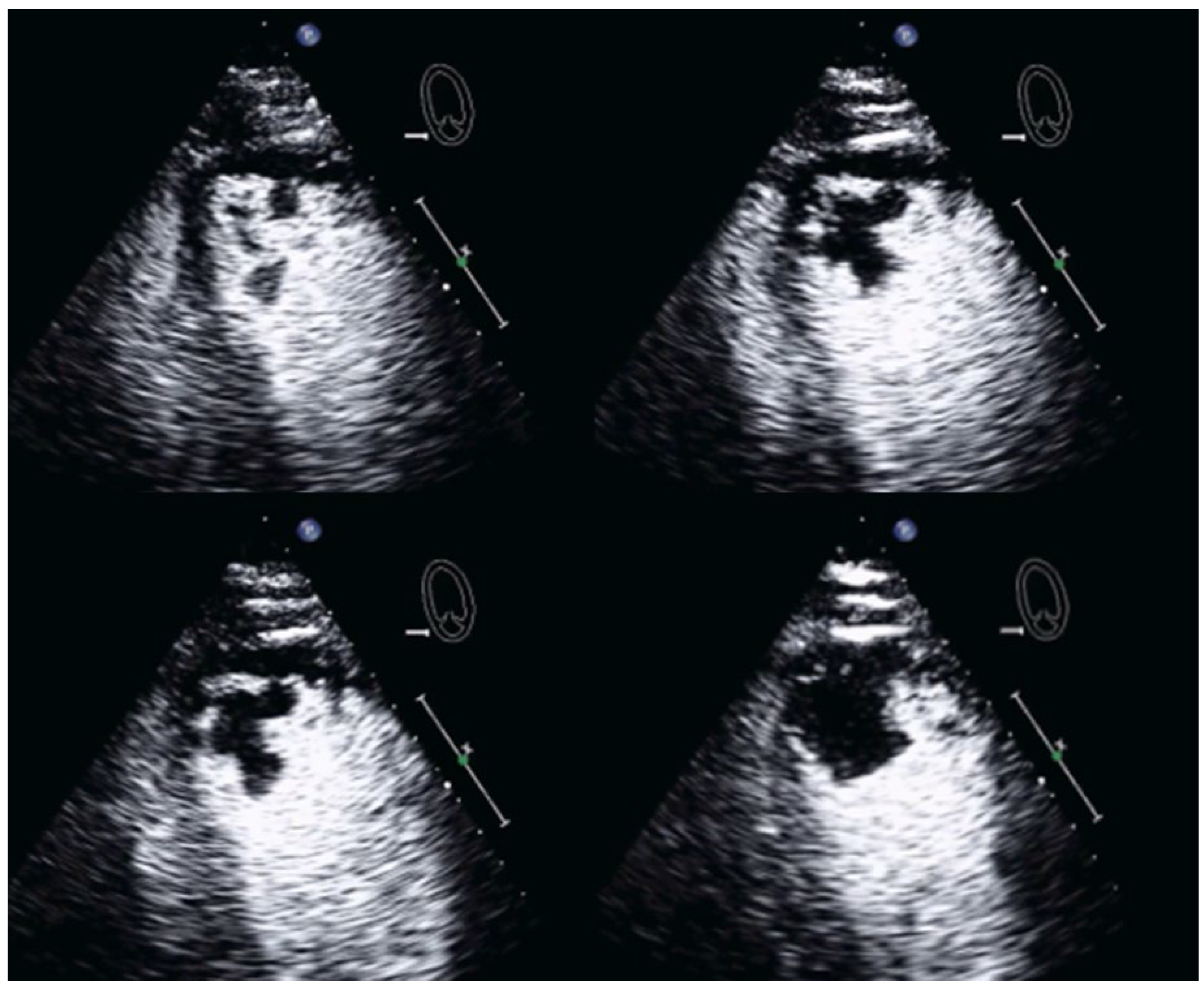
4.3. Interpretation and Reporting
4.4. Pitfalls
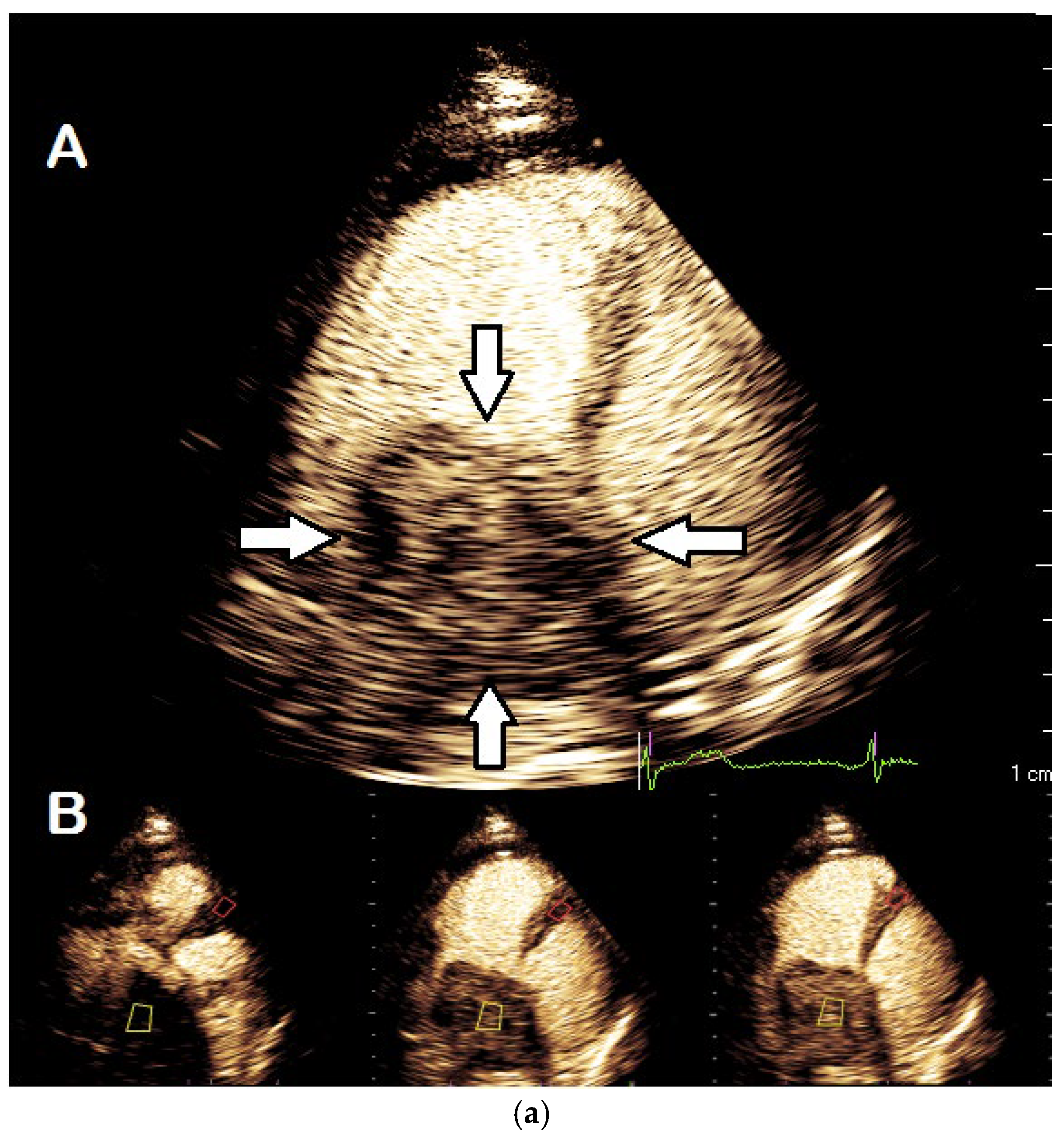
5. Excessive Trabeculation of the Left Ventricle
5.1. Background and Indications
5.2. Preparation and Performance
5.2.1. Technical Aspects, Settings
5.2.2. Pre-Assessment and Primary Scan Planes
5.2.3. CEUS Procedure
5.3. Interpretation and Reporting
5.4. Pitfalls
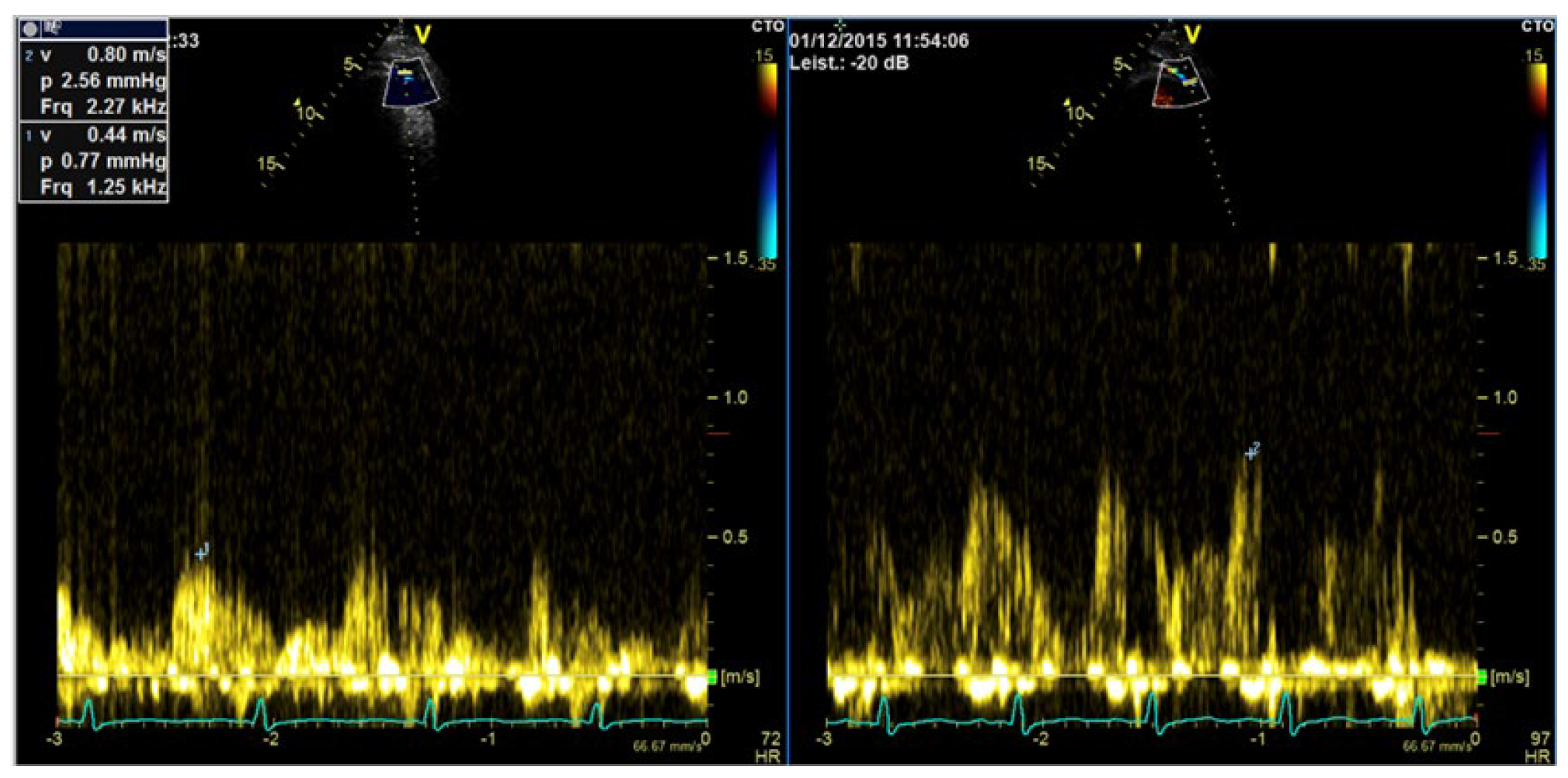
6. Enhancement of Doppler Signals
6.1. Background and Indications
6.2. How to Measure LAD Coronary Flow Velocity
6.3. Preparation and Performance for Enhancement of Valvular Flows
Technical Aspects, Settings
6.4. Velocity Measurements on Enhanced Doppler Recordings
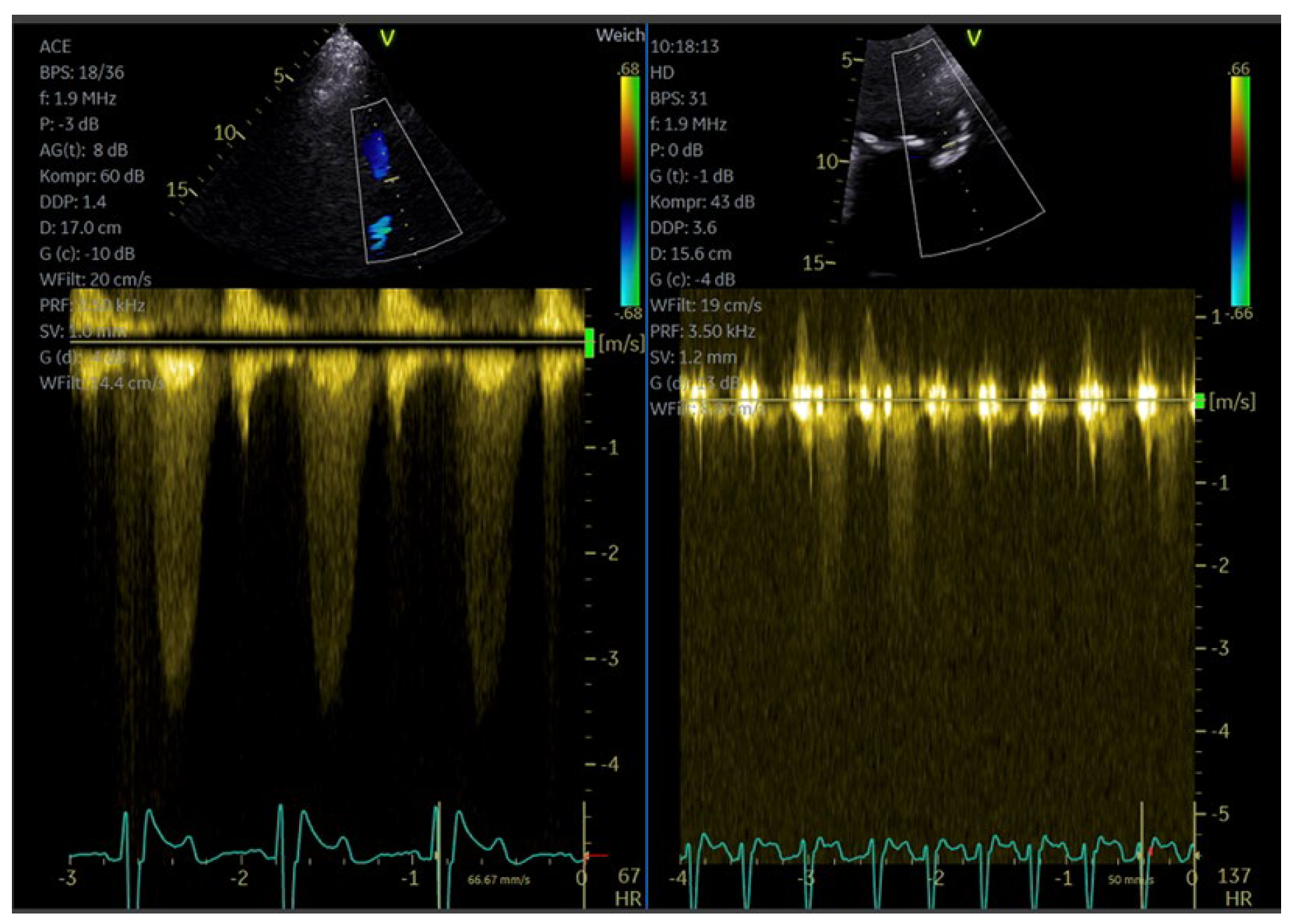
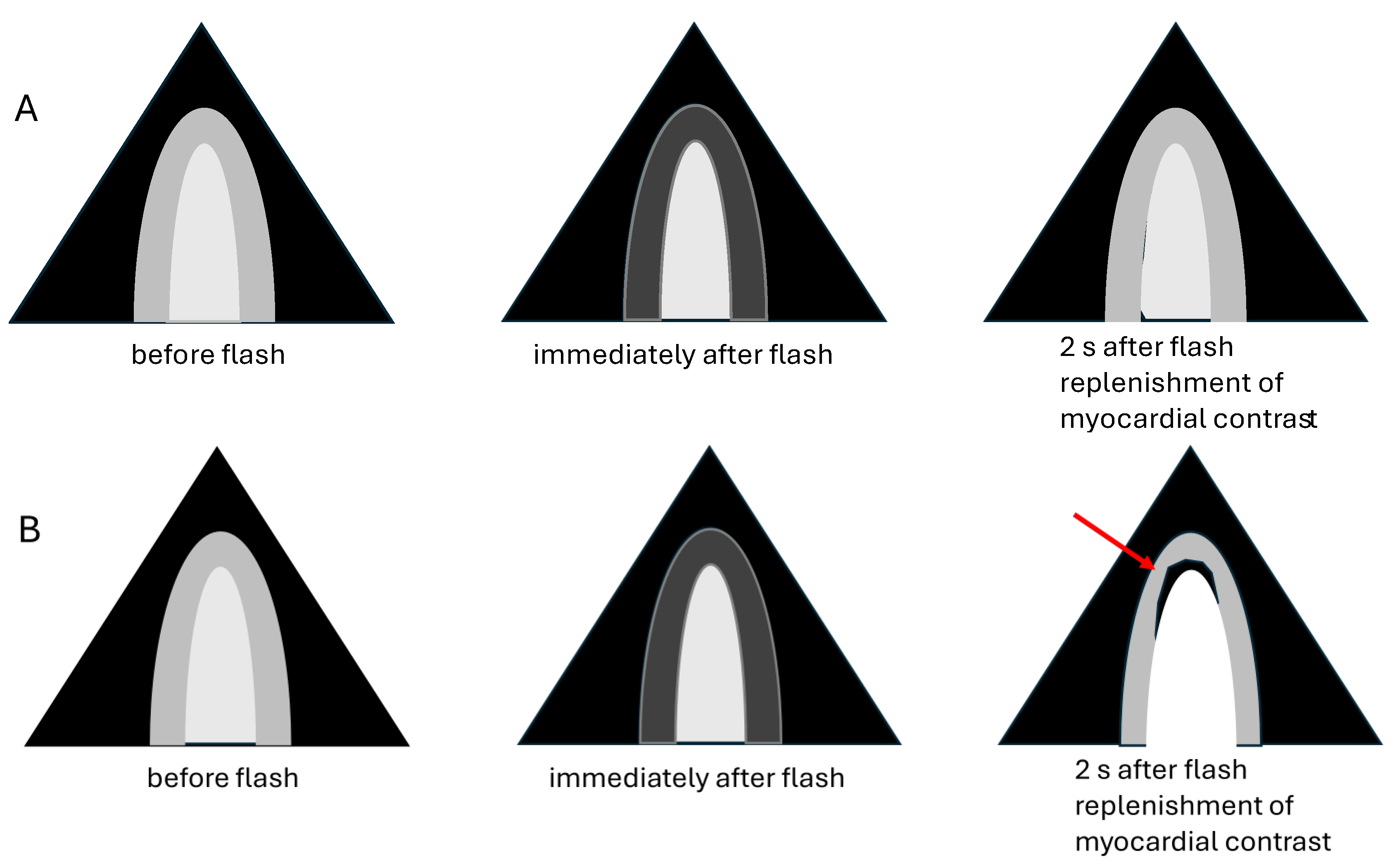
7. Myocardial Perfusion—Fundamentals and Practical Application
7.1. Background and Indications
7.2. Preparation and Performance
7.2.1. Technical Aspects, Settings
7.2.2. Pre-Assessment and Primary Scan Plane
7.2.3. CEUS Procedure
7.2.4. Pitfalls
7.3. Interpretation and Reporting
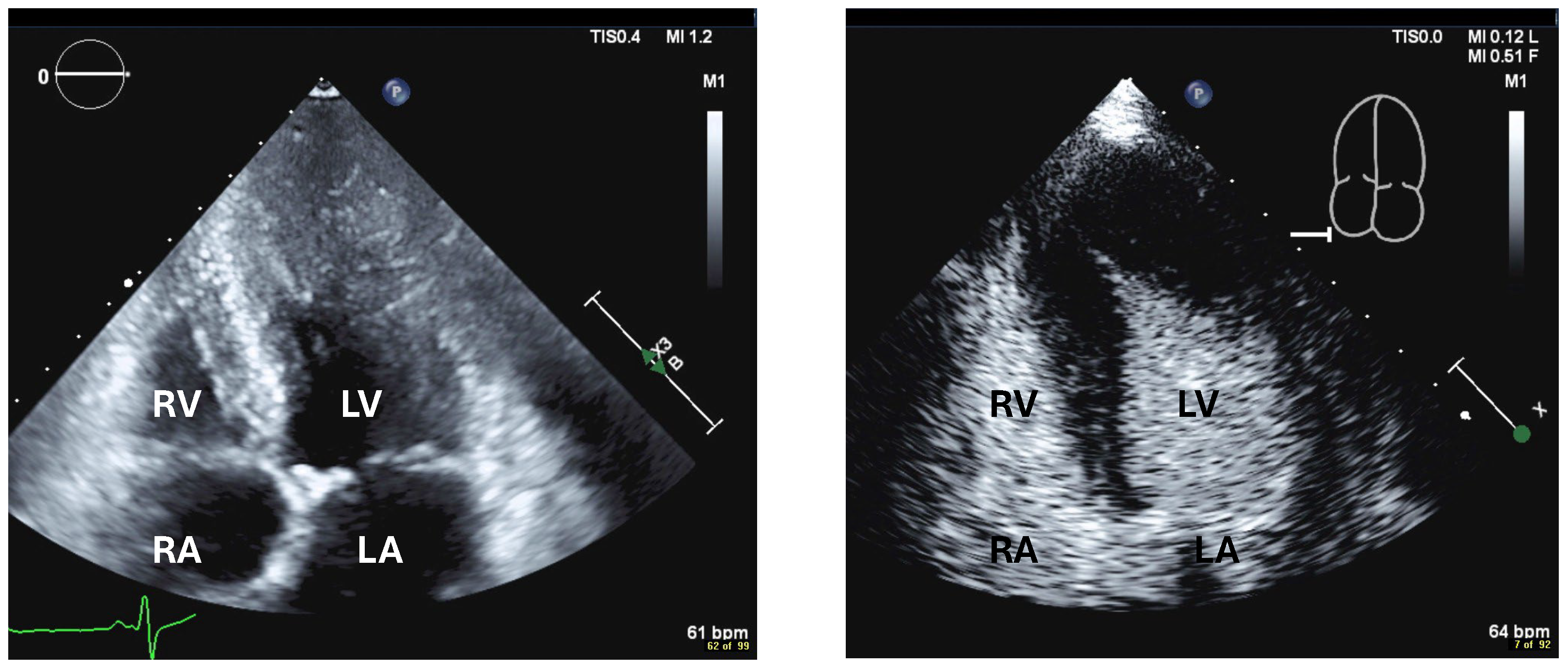
8. Echocardiography with UEA in Critically Ill Patients
9. Education, Qualification
9.1. Qualification and Clinical Practitioner Training
9.2. Quality Assurance and Control
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Igata, S.; Kraushaar, M.; Strachan, M.; Ma, J.I.; Nishimura, M.; Raisinghani, A.; Blanchard, D.G.; DeMaria, A.N. Systematic Assessment of the Impact of Ultrasound-Enhancing Agents upon Measurements of Cardiac Size and Function by Echocardiography. J. Am. Soc. Echocardiogr. 2020, 33, 313–321. [Google Scholar] [CrossRef]
- Nishimura, M.; Igata, S.; Wong, D.J.; Wettersten, N.; Kahn, A.M.; Raisinghani, A.; Blanchard, D.G.; Strachan, M.; DeMaria, A.N. Hypertrabeculation as a Noncompaction Phenotype in Dilated Cardiomyopathy Defined by Contrast Echocardiography. JACC Cardiovasc. Imaging 2019, 12, 1287–1288. [Google Scholar] [CrossRef]
- Mulvagh, S.L.; DeMaria, A.N.; Feinstein, S.B.; Burns, P.N.; Kaul, S.; Miller, J.G.; Monaghan, M.; Porter, T.R.; Shaw, L.J.; Villanueva, F.S. Contrast echocardiography: Current and future applications. J. Am. Soc. Echocardiogr. 2000, 13, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Becher, H.; Helfen, A.; Michels, G.; Gaibazzi, N.; Senior, R.; Dietrich, C.F. How to Perform Cardiac Contrast-Enhanced Ultrasound (cCEUS): Part I. Diagnostics 2025, 15, 1743. [Google Scholar] [CrossRef] [PubMed]
- Hoyland, K.; Mohamed Ali, A.; Vegsundvag, J.; Chambers, J.B.; Saeed, S. Echocardiographic features of left ventricular recess, cleft, diverticulum, and aneurysm: A systematic review. J. Clin. Ultrasound 2022, 50, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Porter, T.R.; Abdelmoneim, S.; Belcik, J.T.; McCulloch, M.L.; Mulvagh, S.L.; Olson, J.J.; Porcelli, C.; Tsutsui, J.M.; Wei, K. Guidelines for the cardiac sonographer in the performance of contrast echocardiography: A focused update from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2014, 27, 797–810. [Google Scholar] [CrossRef]
- Levine, G.N.; McEvoy, J.W.; Fang, J.C.; Ibeh, C.; McCarthy, C.P.; Misra, A.; Shah, Z.I.; Shenoy, C.; Spinler, S.A.; Vallurupalli, S.; et al. Management of Patients at Risk for and With Left Ventricular Thrombus: A Scientific Statement From the American Heart Association. Circulation 2022, 146, e205–e223. [Google Scholar] [CrossRef]
- Citro, R.; Lyon, A.R.; Meimoun, P.; Omerovic, E.; Redfors, B.; Buck, T.; Lerakis, S.; Parodi, G.; Silverio, A.; Eitel, I.; et al. Standard and advanced echocardiography in takotsubo (stress) cardiomyopathy: Clinical and prognostic implications. J. Am. Soc. Echocardiogr. 2015, 28, 57–74. [Google Scholar] [CrossRef]
- Siebelink, H.M.; Scholte, A.J.; Van de Veire, N.R.; Holman, E.R.; Nucifora, G.; van der Wall, E.E.; Bax, J.J. Value of contrast echocardiography for left ventricular thrombus detection postinfarction and impact on antithrombotic therapy. Coron. Artery Dis. 2009, 20, 462–466. [Google Scholar] [CrossRef]
- Aggeli, C.; Dimitroglou, Y.; Raftopoulos, L.; Sarri, G.; Mavrogeni, S.; Wong, J.; Tsiamis, E.; Tsioufis, C. Cardiac Masses: The Role of Cardiovascular Imaging in the Differential Diagnosis. Diagnostics 2020, 10, 1088. [Google Scholar] [CrossRef]
- Abdelmoneim, S.S.; Pellikka, P.A.; Mulvagh, S.L. Contrast echocardiography for assessment of left ventricular thrombi. J. Ultrasound Med. 2014, 33, 1337–1344. [Google Scholar] [CrossRef]
- Lee, D.Z.J.; Chan, R.H.; Montazeri, M.; Hoss, S.; Adler, A.; Nguyen, E.T.; Rakowski, H. Left Ventricular Apical Aneurysms in Hypertrophic Cardiomyopathy: Equivalent Detection by Magnetic Resonance Imaging and Contrast Echocardiography. J. Am. Soc. Echocardiogr. 2021, 34, 1262–1272. [Google Scholar] [CrossRef]
- Urbano-Moral, J.A.; Gonzalez-Gonzalez, A.M.; Maldonado, G.; Gutierrez-Garcia-Moreno, L.; Vivancos-Delgado, R.; De Mora-Martin, M.; Rodriguez-Palomares, J.F.; Evangelista-Masip, A. Contrast-Enhanced Echocardiographic Measurement of Left Ventricular Wall Thickness in Hypertrophic Cardiomyopathy: Comparison with Standard Echocardiography and Cardiac Magnetic Resonance. J. Am. Soc. Echocardiogr. 2020, 33, 1106–1115. [Google Scholar] [CrossRef]
- Adabifirouzjaei, F.; Igata, S.; DeMaria, A.N. Hypertrabeculation; a phenotype with Heterogeneous etiology. Prog. Cardiovasc. Dis. 2021, 68, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Petersen, S.E.; Jensen, B.; Aung, N.; Friedrich, M.G.; McMahon, C.J.; Mohiddin, S.A.; Pignatelli, R.H.; Ricci, F.; Anderson, R.H.; Bluemke, D.A. Excessive Trabeculation of the Left Ventricle: JACC: Cardiovascular Imaging Expert Panel Paper. JACC Cardiovasc. Imaging 2023, 16, 408–425. [Google Scholar] [CrossRef] [PubMed]
- Caiati, C.; Montaldo, C.; Zedda, N.; Bina, A.; Iliceto, S. New noninvasive method for coronary flow reserve assessment: Contrast-enhanced transthoracic second harmonic echo Doppler. Circulation 1999, 99, 771–778. [Google Scholar] [CrossRef]
- Terasawa, A.; Miyatake, K.; Nakatani, S.; Yamagishi, M.; Matsuda, H.; Beppu, S. Enhancement of Doppler flow signals in the left heart chambers by intravenous injection of sonicated albumin. J. Am. Coll. Cardiol. 1993, 21, 737–742. [Google Scholar] [CrossRef][Green Version]
- Cosyns, B.; Helfen, A.; Leong-Poi, H.; Senior, R. How to perform an ultrasound contrast myocardial perfusion examination? Eur. Heart J.—Cardiovasc. Imaging 2022, 23, 727–729. [Google Scholar] [CrossRef]
- Picano, E.; Pierard, L.; Peteiro, J.; Djordjevic-Dikic, A.; Sade, L.E.; Cortigiani, L.; Van De Heyning, C.M.; Celutkiene, J.; Gaibazzi, N.; Ciampi, Q.; et al. The clinical use of stress echocardiography in chronic coronary syndromes and beyond coronary artery disease: A clinical consensus statement from the European Association of Cardiovascular Imaging of the ESC. Eur. Heart J.—Cardiovasc. Imaging 2024, 25, e65–e90. [Google Scholar] [CrossRef]
- Michels, G.; Horn, R.; Helfen, A.; Hagendorff, A.; Jung, C.; Hoffmann, B.; Jaspers, N.; Kinkel, H.; Greim, C.A.; Knebel, F.; et al. Standardized contrast-enhanced ultrasound (CEUS) in clinical acute and emergency medicine and critical care (CEUS Acute): Consensus statement of DGIIN, DIVI, DGINA, DGAI, DGK, OGUM, SGUM and DEGUM. Med. Klin. Intensiv. Notfmed. 2022, 117, 1–23. [Google Scholar] [CrossRef]
- Filippone, A.; Kirchin, M.A.; Monteith, J.; Storto, M.L.; Spinazzi, A. Safety of Lumason(R) (SonoVue(R)) in special populations and critically ill patients. Front. Cardiovasc. Med. 2023, 10, 1225654. [Google Scholar] [CrossRef]
- Strom, J.B.; Appis, A.; Barr, R.G.; Chammas, M.C.; Clevert, D.A.; Darge, K.; Feinstein, L.; Feinstein, S.B.; Fowlkes, J.B.; Gorman, B.; et al. Multi-societal expert consensus statement on the safe administration of ultrasound contrast agents. Echo Res. Pract. 2025, 12, 4. [Google Scholar] [CrossRef]




| Myocardial disease and masses |
| Thrombi |
| Apical hypertrophy |
| Pseudoaneurysm |
| Myocardial rupture |
| LV diverticula |
| Excessive LV trabeculations |
| Imaging method | Low-MI-contrast-specific imaging and intermediate-MI-contrast-specific imaging |
| Imaging planes | Standard apical views, zoomed apical views and modified/zoomed views |
| Sector depth/width | First assessment of the global and regional function using low-MI method and display of the entire LV + 1/3 LA, then zoomed views to display the region of the aneurysm |
| Focus | At the depth of the aneurysm |
| Gain | Adjust to avoid obscuring the LV borders by intensive opacification of the cavity |
| Contrast application | Bolus injection |
| Typical findings | Clear demarcation from the normal myocardium Narrow neck of false aneurysms Search for associated thrombi and pericardial effusion (more likely near false aneurysms) |
| Alternative imaging | Cardiac MRI or cardiac CT in patients with contraindications to UEAs or inadequate recordings with UEAs |
| Number |
|---|
| Localization: attached to which segments |
| Size: diameter in two planes, document in which planes measurements were performed |
| Shape: laminar, protruding, pedunculated |
| Mobility: yes/no |
| Comparison with previous echocardiogram if available |
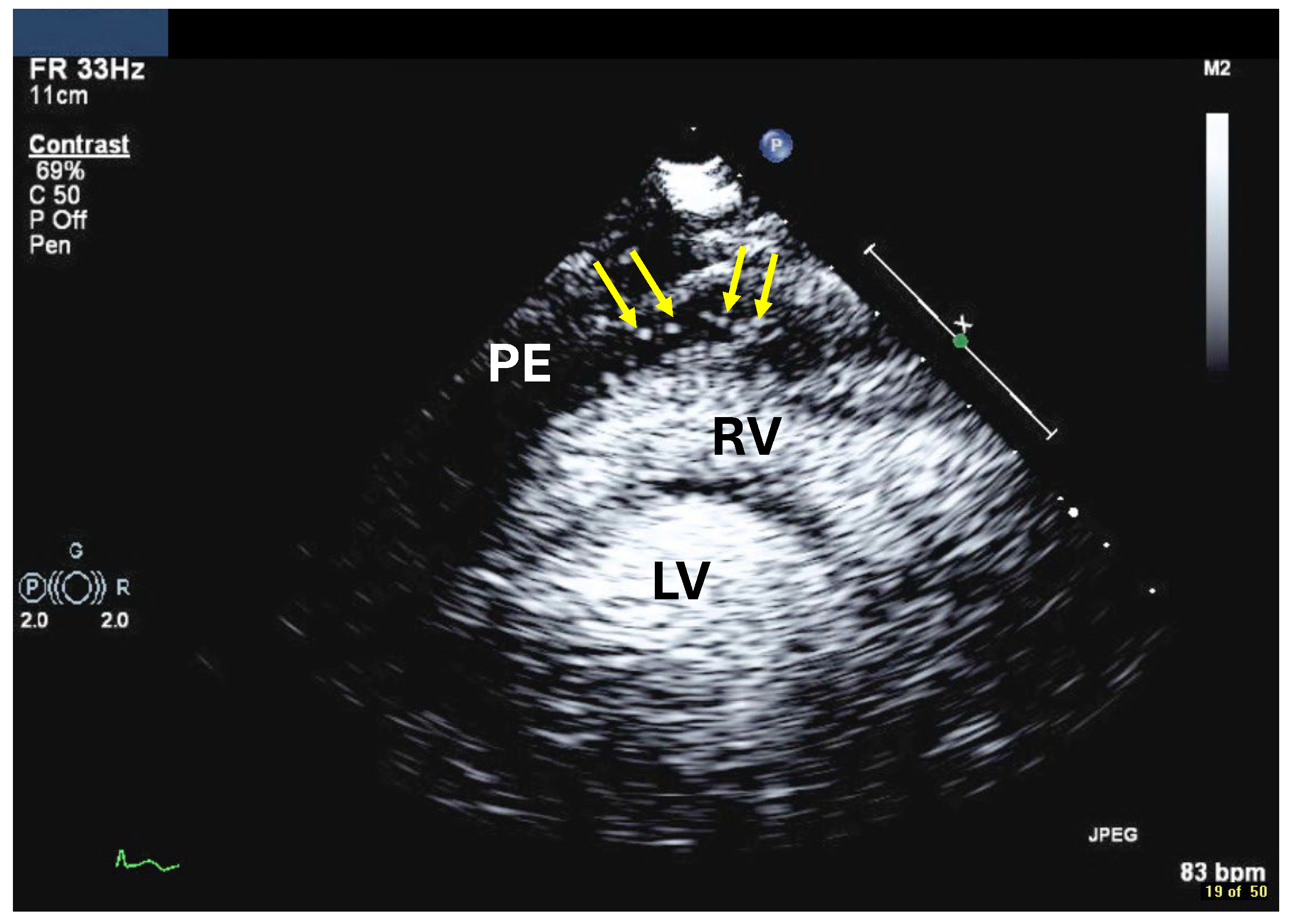
| Imaging method | Low-MI-contrast-specific imaging and intermediate-MI-contrast-specific imaging |
| Imaging planes | standard apical views additional zoomed views sweeps through the region of the suspected thrombus |
| Sector depth/width | Entire LV + 1/3 LA to assess global/regional LV function, zoomed views of the region with the suspected thrombus |
| Focus | At the depth of the suspected thrombus |
| Gain | Adjust to avoid obscuring the thrombus by intensive opacification of the cavity |
| Contrast application | bolus injections |
| Typical findings | 1. echofree mass 2. present in two different imaging planes 3. lump or laminar shape different from trabeculations’ documented size (two orthogonal diameters in at least one of the views), location, type (laminar vs. lump, single vs. multiple), surface (smooth vs. irregular) and mobility |
| DD tumor vs. thrombus | Opacified (vascularized) masses are suggestive of tumors; the vascularization can be demonstrated with myocardial perfusion imaging. CAVEAT: There are malignant tumors which appear avascular on CEUS. Tumors often are attached to normal myocardium. |
| Alternative imaging | Thrombi: Cardiac MRI when contrast echo is not possible or non-diagnostic, cardiac CT when cardiac MRI is not available Tumors: MRI provides tissue characterization and should be performed unless there is typical myxoma (attached to the interatrial septum) |
| Imaging method | Low-MI-contrast-specific imaging, additional intermediate-MI imaging in case of apical aneurysm for assessment of thrombus in the aneurysm |
| Imaging planes | Standard apical views and apical sweeps to assess the aneurysm for thrombi |
| Contrast application | Bolus injections |
| Typical finding | 1. Hourglass/ace-of-spades shape of apical LV cavity 2. Apical myocardium appears dark in late systole due to compression of the intramyocardial vessels 3. Apical aneurysms +/− thrombi in some patients |
| Alternative imaging | MRI useful for scar/fibrosis imaging and display of apical aneurysms CT in patients with contraindication for MRI and UEAs |
| Imaging method | start with low-MI-contrast-specific imaging for assessment of global and regional LV function then use intermediate-MI-contrast-specific imaging which provides better display of LV trabeculations |
| Imaging planes | standard apical views parasternal and apical short-axis view |
| Contrast application | bolus injection |
| Typical findings | trabeculated layer apical, lateral, and inferior: more than 3 trabeculations, ratio of trabeculated/compact myocardium >2 The number of trabeculations and the ratio of trabeculated/compact myocardium does not seem to impact clinical management |
| Alternative imaging | MRI for tissue characterization in dilated cardiomyopathy and risk assessment in hypertrophic cardiomyopathy, assessment of LV thrombi when CEUS recordings are non-diagnostic |
| Flow assessment in epicardial coronary arteries (Color and PW Doppler) |
| Aortic stenosis (CW Doppler) |
| Pulmonary venous flow (PW Doppler) mitral regurgitation |
| Tricuspid regurgitation (CW Doppler) for measurement of PA pressure * |
| Imaging method | CW Doppler for aortic stenosis/tricuspid regurgitation PW-Doppler: for pulmonary–venous flow |
| Imaging planes | Same as for non-contrast Doppler imaging, the enhanced color Doppler signals facilitate the alignment of the cursor for spectral Doppler measurements |
| Contrast application | Bolus injection, the recordings can be performed during the washout after recordings for assessment of LV function |
| Typical findings | Intensive Doppler spectra Consider reduction in gain or power. |
| Alternative imaging | TEE, cardiac MRI |
| Viability in chronic CAD |
| No reflow in acute MI |
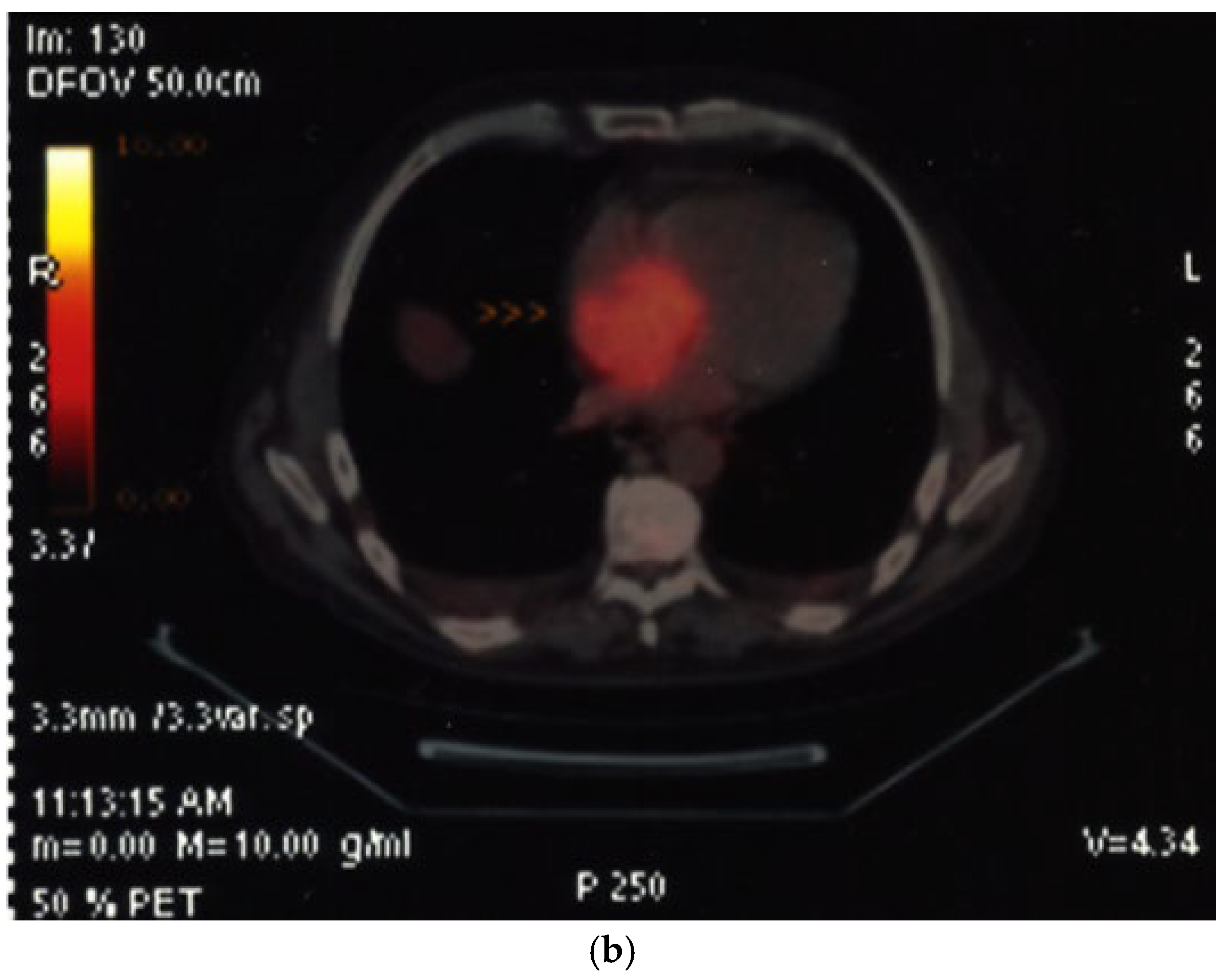
| Cardiac tumors |
| Assessment of myocardial ischemia/viability during stress echocardiography |
| Adequate Flash | Flash Too Intense | Flash Too Low |
|---|---|---|
| Clears the contrast signals across the entire myocardium | Clears the contrast signals across the entire myocardium | Incomplete disappearance of myocardial contrast |
| Entire LV cavity still opacified | Major destruction of LV cavity contrast | Opacification of the entire LV cavity |
| Reduce MI of the flash, e.g., 0.02 steps, or reduce the number of flash frames, e.g., 5 frames less | Increase MI of the flash, e.g., 0.02 steps, or reduce the number of flash frames, e.g., 5 frames more |
| Imaging method | Low-MI-contrast-specific imaging—Flash–Replenishment |
| Imaging planes | standard apical views additional modified views to optimize perfusion imaging in basal anterior/lateral segments or views to optimize the display of suspected tumors |
| Contrast application | Infusion bolus injection acceptable for demonstration of vascularization of a cardiac tumor |
| Typical findings | Normal myocardial perfusion: homogeneous opacification of the segment, contrast replenishment within 5 s after flash (2 s during stress) Abnormal perfusion: delayed contrast replenishment, perfusion defect, often combined with abnormal wall motion Tumors may show patchy opacification and include dark areas due to necrosis |
| Alternative imaging | Doppler velocity measurements (see above), nuclear imaging (SPECT, PET), cardiac MRI for assessment of myocardial perfusion and viability Tumors: MRI provides tissue characterization and should be performed unless there is typical myxoma (attached to the interatrial septum) |
| Imaging method | Low-MI-contrast-specific imaging, alternatively intermediate-MI-contrast-specific imaging |
| Imaging planes | First try subcostal view, then standard views |
| Contrast application | Bolus injection |
| Typical findings | Usually isolated bubbles in the pericardial fluid Review frame by frame! |
| Alternative imaging | Cardiac computed tomography with contrast |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Becher, H.; Helfen, A.; Michels, G.; Gaibazzi, N.; Senior, R.; Dietrich, C.F. How to Perform Cardiac Contrast-Enhanced Ultrasound (cCEUS): Part II—Advanced Applications and Interpretation. Diagnostics 2025, 15, 2371. https://doi.org/10.3390/diagnostics15182371
Becher H, Helfen A, Michels G, Gaibazzi N, Senior R, Dietrich CF. How to Perform Cardiac Contrast-Enhanced Ultrasound (cCEUS): Part II—Advanced Applications and Interpretation. Diagnostics. 2025; 15(18):2371. https://doi.org/10.3390/diagnostics15182371
Chicago/Turabian StyleBecher, Harald, Andreas Helfen, Guido Michels, Nicola Gaibazzi, Roxy Senior, and Christoph Frank Dietrich. 2025. "How to Perform Cardiac Contrast-Enhanced Ultrasound (cCEUS): Part II—Advanced Applications and Interpretation" Diagnostics 15, no. 18: 2371. https://doi.org/10.3390/diagnostics15182371
APA StyleBecher, H., Helfen, A., Michels, G., Gaibazzi, N., Senior, R., & Dietrich, C. F. (2025). How to Perform Cardiac Contrast-Enhanced Ultrasound (cCEUS): Part II—Advanced Applications and Interpretation. Diagnostics, 15(18), 2371. https://doi.org/10.3390/diagnostics15182371





