Incidence of Complicated Appendicitis during the COVID-19 Pandemic versus the Pre-Pandemic Period: A Systematic Review and Meta-Analysis of 2782 Pediatric Appendectomies
Abstract
:1. Introduction
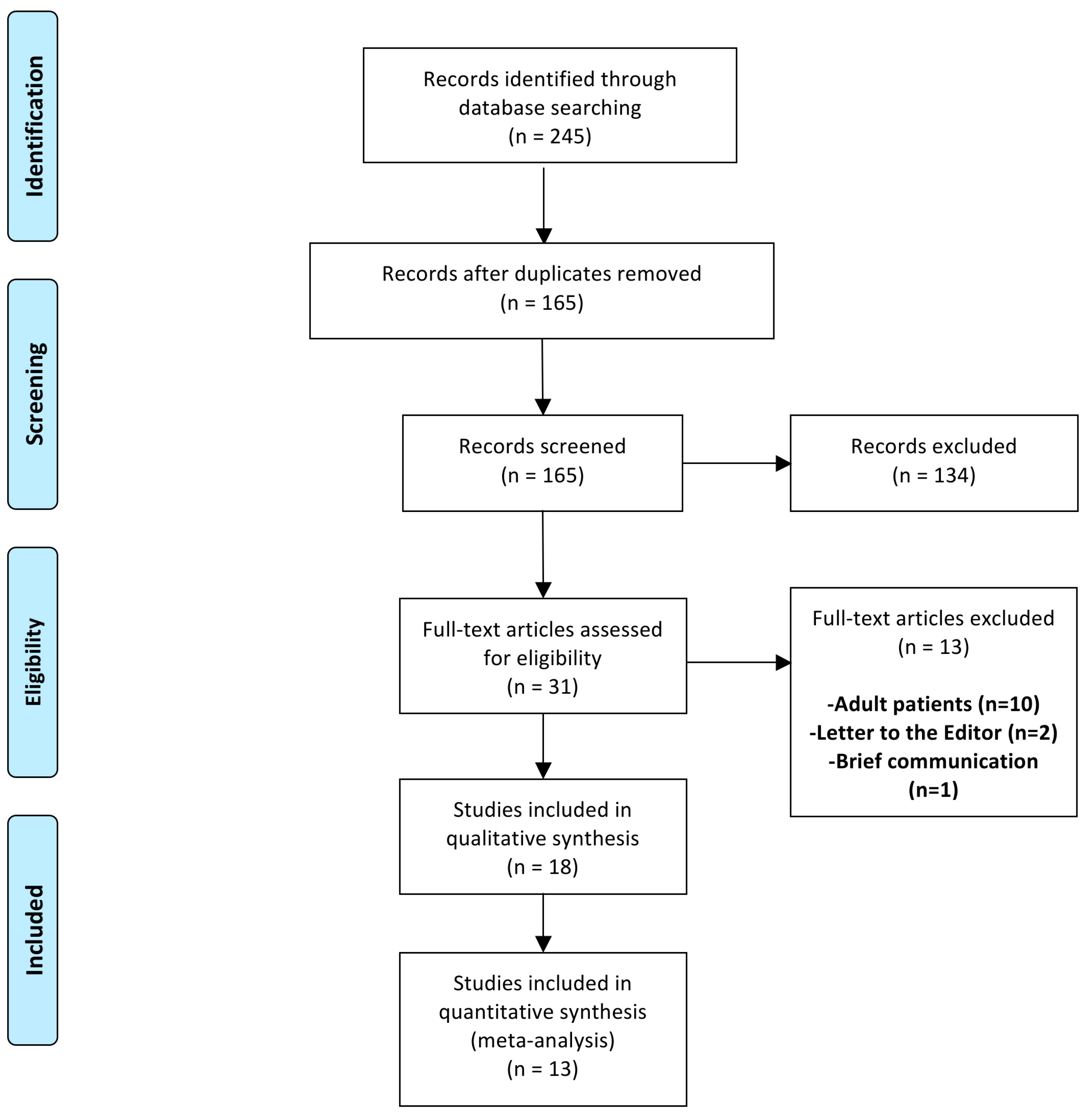
2. Materials and Methods
2.1. Systematic Search
2.2. Eligibility Criteria
2.3. Data Synthesis
2.4. Methodological Quality Assessment
2.5. Data Analysis
3. Results
3.1. Study Characteristics
3.2. Methodological Quality Assessment
3.3. Outcome Analysis
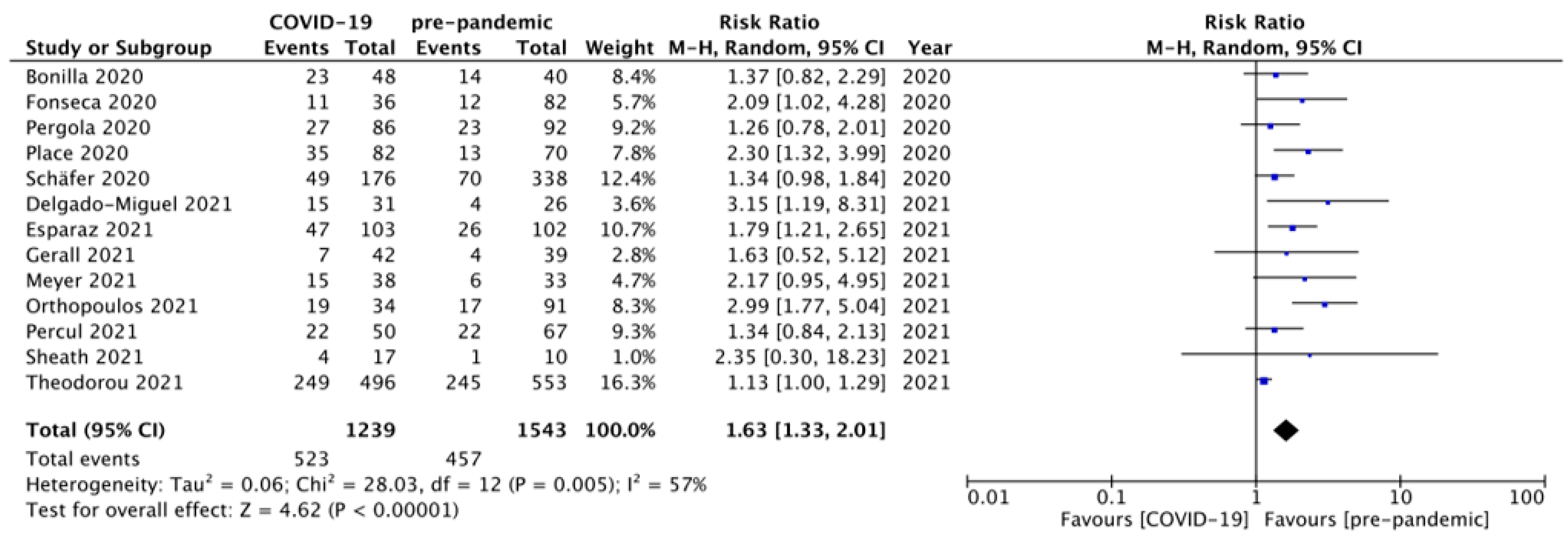
3.3.1. Proportion of Children with Complicated Appendicitis
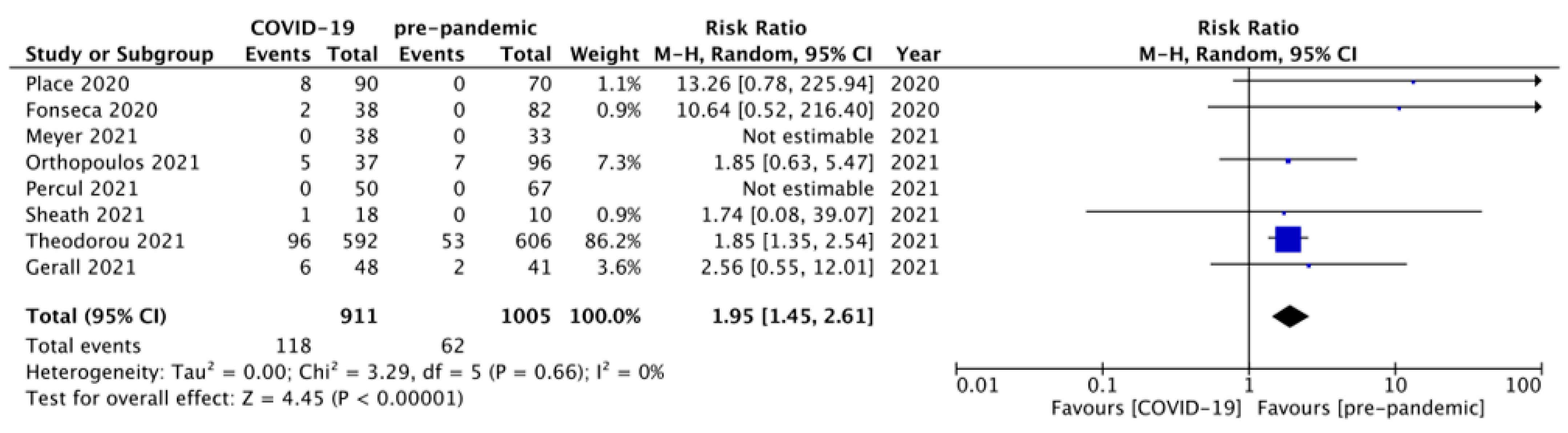
3.3.2. Proportion of Children Managed via the NOM
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Database | Studies |
|---|---|
| PubMed | 66 |
| EMBASE | 102 |
| Web of science | 54 |
| SCOPUS | 123 |
| Total | 345 |
| Duplications | 180 |
| After duplication removal | 165 |
References
- Stinger, M.D. Acute appendicitis. J. Paediatr. Child Health 2017, 53, 1071–1076. [Google Scholar] [CrossRef] [PubMed]
- Glass, C.C.; Rangel, S.J. Overview and diagnosis of acute appendicitis in children. Semin. Pediatr. Surg. 2016, 25, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Pogorelić, Z.; Mihanović, J.; Ninčević, S.; Lukšić, B.; Elezović Baleović, S.; Polašek, O. Validity of appendicitis inflammatory response score in distinguishing perforated from non-perforated appendicitis in children. Children 2021, 8, 309. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Rak, S.; Mrklić, I.; Jurić, I. Prospective validation of Alvarado score and pediatric appendicitis score for the diagnosis of acute appendicitis in children. Pediatr. Emerg. Care 2015, 31, 164–168. [Google Scholar] [CrossRef]
- Lounis, Y.; Hugo, J.; Demarche, M.; Seghaye, M.C. Influence of age on clinical presentation, diagnosis delay and outcome in pre-school children with acute appendicitis. BMC Pediatr. 2020, 20, 151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pogorelić, Z.; Domjanović, J.; Jukić, M.; Peričić, T.P. Acute appendicitis in children younger than five years of age: Diagnostic challenge for pediatric surgeons. Surg. Infect. 2020, 21, 239–245. [Google Scholar] [CrossRef]
- Miyauchi, H.; Okata, Y.; Hatakeyama, T.; Nakatani, T.; Nakai, Y.; Bitoh, Y. Analysis of predictive factors for perforated appendicitis in children. Pediatr. Int. 2020, 62, 711–715. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Lukšić, B.; Ninčević, S.; Lukšić, B.; Polašek, O. Hyponatremia as a predictor of perforated acute appendicitis in pediatric population: A prospective study. J. Pediatr. Surg. 2021, 56, 1816–1821. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Lukšić, A.M.; Mihanović, J.; Đikić, D.; Balta, V. Hyperbilirubinemia as an indicator of perforated acute appendicitis in pediatric population: A prospective study. Surg. Infect. 2021, 22, 1064–1071. [Google Scholar] [CrossRef]
- Chakraborty, I.; Maity, P. COVID-19 outbreak: Migration, effects on society, global environment and prevention. Sci. Total Environ. 2020, 728, 138882. [Google Scholar] [CrossRef]
- Dolić, M.; Antičević, V.; Dolić, K.; Pogorelić, Z. Questionnaire for assessing social contacts of nurses who worked with coronavirus patients during the first wave of the COVID-19 pandemic. Healthcare 2020, 9, 930. [Google Scholar] [CrossRef]
- COVID Surg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans. Br. J. Surg. 2020, 107, 1440–1449. [Google Scholar]
- Dong, C.T.; Liveris, A.; Lewis, E.R.; Mascharak, S.; Chao, E.; Reddy, S.H.; Teperman, S.H.; McNelis, J.; Stone, M.E., Jr. Do surgical emergencies stay at home? Observations from the first United States coronavirus epicenter. J. Trauma Acute Care Surg. 2021, 91, 241–246. [Google Scholar] [CrossRef]
- Garcia, S.; Albaghdadi, M.S.; Meraj, P.M.; Schmidt, C.; Garberich, R.; Jaffer, F.A.; Dixon, S.; Rade, J.J.; Tannenbaum, M.; Chambers, J.; et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J. Am. Coll. Cardiol. 2020, 75, 2871–2872. [Google Scholar] [CrossRef] [PubMed]
- Lange, S.J.; Ritchey, M.D.; Goodman, A.B.; Dias, T.; Twentyman, E.; Fuld, J.; Schieve, L.A.; Imperatore, G.; Benoit, S.R.; Kite-Powell, A.; et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions—United States, January–May 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 795–800. [Google Scholar] [CrossRef]
- De Filippo, O.; D’Ascenzo, F.; Angelini, F.; Bocchino, P.P.; Conrotto, F.; Saglietto, A.; Secco, G.G.; Campo, G.; Gallone, G.; Verardi, R.; et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in northern Italy. N. Engl. J. Med. 2020, 383, 88–89. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Milanović, K.; Veršić, A.B.; Pasini, M.; Divković, D.; Pavlović, O.; Lučev, J.; Žufić, V. Is there an increased incidence of orchiectomy in pediatric patients with acute testicular torsion during COVID-19 pandemic? A retrospective multicenter study. J. Pediatric Urol. 2021, 17, 479.e1–479.e6. [Google Scholar] [CrossRef]
- Dreifuss, N.H.; Schlottmann, F.; Sadava, E.E.; Rotholtz, N.A. Acute appendicitis does not quarantine: Surgical outcomes of laparoscopic appendectomy in COVID-19 times. Br. J. Surg. 2020, 107, 368–369. [Google Scholar] [CrossRef]
- Rosenthal, M.G.; Fakhry, S.M.; Morse, J.L.; Wyse, R.J.; Garland, J.M.; Duane, T.M.; Slivinski, A.; Wilson, N.Y.; Watts, D.D.; Shen, Y.; et al. Where did all the appendicitis go? Impact of the COVID-19 pandemic on volume, management, and outcomes of acute appendicitis in a nationwide, multicenter analysis. Ann. Surg. 2021, 2, e048. [Google Scholar] [CrossRef]
- Ganesh, R.; Lucoq, J.; Ekpete, N.O.; Ul Ain, N.; Lim, S.K.; Alwash, A. Management of appendicitis during COVID-19 pandemic; short-term outcomes. Scott. Med. J. 2020, 65, 144–148. [Google Scholar] [CrossRef]
- Maneck, M.; Günster, C.; Meyer, H.J.; Heidecke, C.D.; Rolle, U. Influence of COVID-19 confinement measures on appendectomies in Germany-a claims data analysis of 9797 patients. Langenbeck’s Arch. Surg. 2021, 406, 385–391. [Google Scholar] [CrossRef]
- Willms, A.G.; Oldhafer, K.J.; Conze, S.; Thasler, W.E.; von Schassen, C.; Hauer, T.; Huber, T.; Germer, C.T.; Günster, S.; Bulian, D.R.; et al. Appendicitis during the COVID-19 lockdown: Results of a multicenter analysis in Germany. Langenbeck’s Arch. Surg. 2021, 406, 367–375. [Google Scholar] [CrossRef]
- Emile, S.H.; Hamid, H.K.S.; Khan, S.M.; Davis, G.N. Rate of application and outcome of non-operative management of acute appendicitis in the setting of COVID-19: Systematic review and meta-analysis. J. Gastrointest. Surg. 2021, 25, 1905–1915. [Google Scholar] [CrossRef]
- Fadgyas, B.; Garai, G.I.; Ringwald, Z. How COVID-19 pandemic influences paediatric acute appendicitis cases? Orv. Hetil. 2021, 162, 608–610. [Google Scholar] [CrossRef]
- Pawelczyk, A.; Kowalska, M.; Tylicka, M.; Koper-Lenkiewicz, O.M.; Komarowska, M.D.; Hermanowicz, A.; Debek, W.; Matuszczak, E. Impact of the SARS-CoV-2 pandemic on the course and treatment of appendicitis in the pediatric population. Sci. Rep. 2021, 11, 23999. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [Green Version]
- Cochrane. Cochrane Handbook for Systematic Reviews of Interventions (Version 6.2). 2021. Available online: www.training.cochrane.org/handbook (accessed on 1 December 2021).
- Bonilla, L.; Gálvez, C.; Medrano, L.; Benito, J. Impact of COVID-19 on the presentation and evolution of acute appendicitis in pediatrics. An. Pediatr. 2021, 94, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, M.K.; Trindade, E.N.; Costa Filho, O.P.; Nácul, M.P.; Seabra, A.P. Impact of COVID-19 outbreak on the emergency presentation of acute appendicitis. Am. Surg. 2020, 86, 1508–1512. [Google Scholar] [CrossRef] [PubMed]
- La Pergola, E.; Sgrò, A.; Rebosio, F.; Vavassori, D.; Fava, G.; Codrich, D.; Montanaro, B.; Leva, E.; Schleef, J.; Cheli, M.; et al. Appendicitis in children in a large italian COVID-19 pandemic area. Front. Pediatr. 2020, 8, 600320. [Google Scholar] [CrossRef]
- Place, R.; Lee, J.; Howell, J. Rate of pediatric appendiceal perforation at a children’s hospital during the COVID-19 pandemic compared with the previous year. JAMA Netw. Open 2020, 3, e2027948. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, F.M.; Meyer, J.; Kellnar, S.; Warmbrunn, J.; Schuster, T.; Simon, S.; Meyer, T.; Platzer, J.; Hubertus, J.; Seitz, S.T.; et al. Increased incidence of perforated appendicitis in children during COVID-19 pandemic in a bavarian multi-center study. Front. Pediatr. 2021, 9, 683607. [Google Scholar] [CrossRef]
- Delgado-Miguel, C.; Muñoz-Serrano, A.J.; Miguel-Ferrero, M.; De Ceano-Vivas, M.; Calvo, C.; Martínez, L. Complicated acute appendicitis during COVID-19 pandemic: The hidden epidemic in children. Eur. J. Pediatr. Surg. 2021. [Google Scholar] [CrossRef]
- Esparaz, J.R.; Chen, M.K.; Beierle, E.A.; Anderson, S.A.; Martin, C.A.; Mortellaro, V.E.; Rogers, D.A.; Mathis, M.S.; Russell, R.T. Perforated appendicitis during a pandemic: The downstream effect of COVID-19 in children. J. Surg. Res. 2021, 268, 263–266. [Google Scholar] [CrossRef]
- Gerall, C.D.; DeFazio, J.R.; Kahan, A.M.; Fan, W.; Fallon, E.M.; Middlesworth, W.; Stylianos, S.; Zitsman, J.L.; Kadenhe-Chiweshe, A.V.; Spigland, N.A.; et al. Delayed presentation and sub-optimal outcomes of pediatric patients with acute appendicitis during the COVID-19 pandemic. J. Pediatr. Surg. 2021, 56, 905–910. [Google Scholar] [CrossRef] [PubMed]
- Meyer, T. Impact of the COVID-19 pandemic on appendicitis in COVID-19 negative children. Mon. Childcare 2021. [Google Scholar] [CrossRef]
- Orthopoulos, G.; Santone, E.; Izzo, F.; Tirabassi, M.; Pérez-Caraballo, A.M.; Corriveau, N.; Jabbour, N. Increasing incidence of complicated appendicitis during COVID-19 pandemic. Am. J. Surg. 2021, 221, 1056–1060. [Google Scholar] [CrossRef]
- Percul, C.; Cruz, M.; Curiel Meza, A.; González, G.; Lerendegui, L.; Malzone, M.C.; Liberto, D.; Lobos, P.; Imach, B.E.; Moldes, J.M.; et al. Impact of the COVID-19 pandemic on the pediatric population with acute appendicitis: Experience at a general, tertiary care hospital. Arch. Argent. Pediatr. 2021, 119, 224–229. [Google Scholar] [PubMed]
- Sheath, C.; Abdelrahman, M.; MacCormick, A.; Chan, D. Paediatric appendicitis during the COVID-19 pandemic. J. Paediatr. Child. Health 2021, 57, 986–989. [Google Scholar] [CrossRef]
- Theodorou, C.M.; Beres, A.L.; Nguyen, M.; Castle, S.L.; Faltermeier, C.; Shekherdimian, S.; Tung, C.; DeUgarte, D.A.; Brown, E.G. Statewide impact of the COVID pandemic on pediatric appendicitis in California: A multicenter study. J. Surg. Res. 2021, 267, 132–142. [Google Scholar] [CrossRef] [PubMed]
- Velayos, M.; Muñoz-Serrano, A.J.; Estefanía-Fernández, K.; Sarmiento Caldas, M.C.; Moratilla Lapeña, L.; López-Santamaría, M.; López-Gutiérrez, J.C. Influence of the coronavirus 2 (SARS-Cov-2) pandemic on acute appendicitis. An. Pediatr. 2020, 93, 118–122. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.C.; Tomita, S.S.; Ginsburg, H.B.; Gordon, A.; Walker, D.; Kuenzler, K.A. Increase in pediatric perforated appendicitis in the New York city metropolitan region at the epicenter of the COVID-19 outbreak. Ann. Surg. 2021, 273, 410–415. [Google Scholar] [CrossRef] [PubMed]
- Montalva, L.; Haffreingue, A.; Ali, L.; Clariot, S.; Julien-Marsollier, F.; Ghoneimi, A.E.; Peycelon, M.; Bonnard, A. The role of a pediatric tertiary care center in avoiding collateral damage for children with acute appendicitis during the COVID-19 outbreak. Pediatr. Surg. Int. 2020, 36, 1397–1405. [Google Scholar] [CrossRef] [PubMed]
- Demir, S.; Öztorun, C.; Kiriş, A.G.; Ertürk, A.; Erten, E.E.; Çalışkan, D.; Altınok, M.K.; Uzun, A.U.; Akkaya, F.; Yılmaz, Y.; et al. Is the COVID-19 pandemic causing delays in the diagnosis of appendicitis in children? Türkiye Çocuk Hast. Derg. 2021, 15, 155–161. [Google Scholar]
- Gaitero Tristán, J.; Souto Romero, H.; Escalada Pellitero, S.; Espiñera, C.R.; Andina Martín, D.; Espinosa Góngora, R.; Martín Diaz, M.J.; Leónidas Espinoza, M. Acute appendicitis in children during the COVID-19 pandemic: Neither delayed diagnosis nor worse outcomes. Pediatr. Emerg. Care 2021, 37, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Pham, X.D.; Sullins, V.F.; Kim, D.Y.; Range, B.; Kaji, A.H.; de Virgilio, C.M.; Lee, S.L. Factors predictive of complicated appendicitis in children. J. Surg. Res. 2016, 206, 62–66. [Google Scholar] [CrossRef]
- Reynolds, S.L. Missed appendicitis in a pediatric emergency department. Pediatr. Emerg. Care 1993, 9, 1–3. [Google Scholar] [CrossRef]
- Nelson, D.S.; Bateman, B.; Bolte, R.G. Appendiceal perforation in children diagnosed in a pediatric emergency department. Pediatr. Emerg. Care 2000, 16, 233–237. [Google Scholar] [CrossRef]
- Rothrock, S.G.; Skeoch, G.; Rush, J.J.; Johnson, N.E. Clinical features of misdiagnosed appendicitis in children. Ann. Emerg. Med. 1991, 20, 45–50. [Google Scholar] [CrossRef]
- Narsule, C.K.; Kahle, E.J.; Kim, D.S.; Anderson, A.C.; Luks, F.I. Effect of delay in presentation on rate of perforation in children with appendicitis. Am. J. Emerg. Med. 2011, 29, 890–893. [Google Scholar] [CrossRef] [PubMed]
- Bodnar, C.; Buss, R.; Somers, K.; Mokdad, A.; Van Arendonk, K.J. Association of neighborhood socioeconomic disadvantage with complicated appendicitis in children. J. Surg. Res. 2021, 265, 245–251. [Google Scholar] [CrossRef]
- O’Toole, S.J.; Karamanoukian, H.L.; Allen, J.E.; Caty, M.G.; O’Toole, D.; Azizkhan, R.G.; Glick, P.L. Insurance-related differences in the presentation of pediatric appendicitis. J. Pediatr. Surg. 1996, 31, 1032–1034. [Google Scholar] [CrossRef]
- Dhatt, S.; Sabhaney, V.; Bray, H.; Skarsgard, E.D. Improving the diagnostic accuracy of appendicitis using a multidisciplinary pathway. J. Pediatr. Surg. 2020, 55, 889–892. [Google Scholar] [CrossRef] [PubMed]
- Pogorelic, Z.; Buljubasic, M.; Susnjar, T.; Jukic, M.; Pericic, T.P.; Juric, I. Comparison of open and laparoscopic appendectomy in children: A 5-year single center experience. Indian Pediatr. 2019, 56, 299–303. [Google Scholar] [CrossRef] [PubMed]
- Jukić, M.; Antišić, J.; Pogorelić, Z. Incidence and causes of 30-day readmission rate from discharge as an indicator of quality care in pediatric surgery. Acta Chir. Belg. 2021. [Google Scholar] [CrossRef]
- Mihanović, J.; Šikić, N.L.; Mrklić, I.; Katušić, Z.; Karlo, R.; Jukić, M.; Jerončić, A.; Pogorelić, Z. Comparison of new versus reused Harmonic scalpel performance in laparoscopic appendectomy in patients with acute appendicitis-a randomized clinical trial. Langenbeck’s Arch. Surg. 2021, 406, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Perko, Z.; Bilan, K.; Pogorelić, Z.; Druzijanić, N.; Srsen, D.; Kraljević, D.; Juricić, J.; Krnić, D. Acute appendicitis and ileal perforation with a toothpick treated by laparoscopy. Coll. Antropol. 2008, 32, 307–309. [Google Scholar]
- Podda, M.; Gerardi, C.; Cillara, N.; Fearnhead, N.; Gomes, C.A.; Birindelli, A.; Mulliri, A.; Davies, R.J.; Di Saverio, S. Antibiotic treatment and appendectomy for uncomplicated acute appendicitis in adults and children: A systematic review and meta-analysis. Ann. Surg. 2019, 270, 1028–1040. [Google Scholar] [CrossRef]
- Umakanthan, S.; Sahu, P.; Ranade, A.V.; Bukelo, M.M.; Rao, J.S.; Abrahao-Machado, L.F.; Dahal, S.; Kumar, H.; Kv, D. Origin, transmission, diagnosis and management of coronavirus disease 2019 (COVID-19). Postgrad. Med. J. 2020, 96, 753–758. [Google Scholar] [PubMed]
- Westgard, B.C.; Morgan, M.W.; Vazquez-Benitez, G.; Erickson, L.O.; Zwank, M.D. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann. Emerg. Med. 2020, 76, 595–601. [Google Scholar] [CrossRef]
- Boserup, B.; McKenney, M.; Elkbuli, A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am. J. Emerg. Med. 2020, 38, 1732–1736. [Google Scholar] [CrossRef]
- Lazzerini, M.; Barbi, E.; Apicella, A.; Marchetti, F.; Cardinale, F.; Trobia, G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc. Health 2020, 4, e10–e11. [Google Scholar] [CrossRef]
- Kostopoulou, E.; Gkentzi, D.; Papasotiriou, M.; Fouzas, S.; Tagalaki, A.; Varvarigou, A.; Dimitriou, G. The impact of COVID-19 on paediatric emergency department visits. A one-year retrospective study. Pediatr. Res. 2021. [Google Scholar] [CrossRef]
- Holzman, S.A.; Ahn, J.J.; Baker, Z.; Chuang, K.W.; Copp, H.L.; Davidson, J.; Davis-Dao, C.A.; Ewing, E.; Ko, J.; Lee, V.; et al. A multicenter study of acute testicular torsion in the time of COVID-19. J. Pediatr. Urol. 2021, 17, 478.e1–478.e6. [Google Scholar] [CrossRef] [PubMed]
- Schirmer, C.M.; Ringer, A.J.; Arthur, A.S.; Binning, M.J.; Fox, W.C.; James, R.F.; Levitt, M.R.; Tawk, R.G.; Veznedaroglu, E.; Walker, M.; et al. Delayed presentation of acute ischemic strokes during the COVID-19 crisis. J. Neurointerv. Surg. 2020, 12, 639–642. [Google Scholar] [CrossRef]
- Balzora, S.; Issaka, R.B.; Anyane-Yeboa, A.; Gray, D.M., 2nd; May, F.P. Impact of COVID-19 on colorectal cancer disparities and the way forward. Gastrointest. Endosc. 2020, 92, 946–950. [Google Scholar] [CrossRef] [PubMed]
- Collard, M.; Lakkis, Z.; Loriau, J.; Mege, D.; Sabbagh, C.; Lefevre, J.H.; Maggiori, L. Antibiotics alone as an alternative to appendectomy for uncomplicated acute appendicitis in adults: Changes in treatment modalities related to the COVID-19 health crisis. J. Visc. Surg. 2020, 157, S33–S42. [Google Scholar] [CrossRef]
- Köhler, F.; Müller, S.; Hendricks, A.; Kastner, C.; Reese, L.; Boerner, K.; Flemming, S.; Lock, J.F.; Germer, C.T.; Wiegering, A. Changes in appendicitis treatment during the COVID-19 pandemic—A systematic review and meta-analysis. Int. J. Surg. 2021, 95, 106148. [Google Scholar] [CrossRef]
- Scott, C.; Lambert, A. Managing appendicitis during the COVID-19 pandemic in the UK. Br. J. Surg. 2020, 107, e271. [Google Scholar] [CrossRef]
- Veziant, J.; Bourdel, N.; Slim, K. Risks of viral contamination in healthcare professionals during laparoscopy in the Covid-19 pandemic. J. Visc. Surg. 2020, 157, S59–S62. [Google Scholar] [CrossRef] [PubMed]
- Parreira, J.G.; DE-Godoy, L.G.L.; DE-Campos, T.; Lucarelli-Antunes, P.S.; DE-Oliveira-E-Silva, L.G.; Santos, H.G.; Luna, R.A.; Portari Filho, P.E.; Assef, J.C. Management of acute appendicitis during the COVID-19 pandemic: Views of two Brazilian surgical societies. Rev. Colégio Bras. Cir. 2021, 48, e20202717. [Google Scholar] [CrossRef] [PubMed]
| Author | Study Design | Sample Size | Average (Mean/Median) Duration of Symptoms; Hours | Average (Mean/Median) LOS; Days | |||
|---|---|---|---|---|---|---|---|
| A | B | A | B | A | B | ||
| Bonilla et al., 2020 [30] | Retro | 49 | 41 | 40 (11–301) * | 30.5 (9–248) * | 5.3 (6.7) † | 4.2 (4.3) † |
| Fonseca et al., 2020 [31] | Retro | 38 | 82 | 40.6 (35.5) † | 28.2 (23.2) † | 2.2 (2.0) † | 2.4 (2.6) † |
| La Pergola et al., 2020 [32] | Retro | 86 | 92 | 1 (1–2) * days | 1 (1–2) * days | Not mentioned | |
| Place et al., 2020 [33] | Cross | 90 | 70 | Not mentioned | Not mentioned | ||
| Schäfer et al., 2020 [34] | Retro | 176 | 338 | Not mentioned | 5.3 (0.2) † | 4.9 (0.1) † | |
| Delgado-Miguel et al., 2021 [35] | Retro | 31 | 26 | 46.8 (13.5) † | 22.9 (11.5) † | 4.9 (3.2) † | 2.5 (1.4) † |
| Esparaz et al., 2021 [36] | Retro | 103 | 102 | Not mentioned | Not mentioned | ||
| Gerall et al., 2021 [37] | Retro | 48 | 41 | 2 (0.5–14) * days | 1 (0.5–14) * days | 2 (0.5–22) * | 1 (0.5–9) * |
| Meyer et al., 2021 [38] | Retro | 38 | 33 | 2 days * | 2 days * | 6 days * | 6 days * |
| Orthopoulos et al., 2021 [39] | Retro | 37 | 96 | Not mentioned | 2.5 (3.1) † | 1.8 (1.9) † | |
| Percul et al., 2021 [40] | Retro | 50 | 67 | 24 (3–120) * | 24 (4–96) * | 3 (2) † days | 3 (2) † days |
| Sheath et al., 2021 [41] | Retro | 18 | 10 | 4 (1–14) * days | 2 (1–10) * days | 1 (0–10) * | 1 (0–6) * |
| Theodorou et al., 2021 [42] | Retro | 592 | 606 | 2 (1–3) * days | 2 (1–3) * days | 3 (1–5) * | 2 (1–4) * |
| Study | Reporting | External Validity | Internal Validity-Bias | Internal Validity-Confounding | Power | Total Scores |
|---|---|---|---|---|---|---|
| Methodological assessment by Observer 1 | ||||||
| Orthopoulos, 2021 [39] | 9 | 3 | 5 | 2 | 0 | 19 |
| Bonilla, 2021 [30] | 8 | 3 | 5 | 2 | 0 | 18 |
| Gerall, 2021 [37] | 10 | 3 | 5 | 2 | 0 | 20 |
| Fonseca, 2020 [31] | 10 | 3 | 5 | 2 | 0 | 20 |
| Sheath, 2021 [41] | 9 | 3 | 5 | 2 | 0 | 19 |
| Place, 2020 [33] | 8 | 3 | 5 | 2 | 0 | 18 |
| Percul, 2021 [40] | 10 | 3 | 5 | 2 | 0 | 20 |
| Delgado-Miguel, 2021 [35] | 9 | 3 | 5 | 2 | 0 | 19 |
| Meyer, 2021 [38] | 8 | 3 | 5 | 2 | 0 | 18 |
| Esparaz, 2021 [36] | 8 | 3 | 5 | 2 | 0 | 18 |
| Pergola, 2020 [32] | 8 | 3 | 5 | 2 | 0 | 18 |
| Schafer, 2021 [34] | 8 | 3 | 5 | 2 | 0 | 18 |
| Theodorou, 2021 [42] | 11 | 3 | 5 | 2 | 4 | 25 |
| Methodological assessment by Observer 2 | ||||||
| Orthopoulos, 2021 [39] | 10 | 3 | 5 | 2 | 0 | 20 |
| Bonilla, 2021 [30] | 9 | 3 | 5 | 2 | 0 | 19 |
| Gerall, 2021 [37] | 10 | 3 | 5 | 2 | 0 | 20 |
| Fonseca, 2020 [31] | 9 | 3 | 5 | 2 | 0 | 19 |
| Sheath, 2021 [41] | 9 | 3 | 5 | 2 | 0 | 19 |
| Place, 2020 [33] | 7 | 3 | 5 | 2 | 0 | 17 |
| Percul, 2021 [40] | 10 | 3 | 5 | 2 | 0 | 20 |
| Delgado-Miguel, 2021 [35] | 10 | 3 | 5 | 2 | 0 | 20 |
| Meyer, 2021 [38] | 8 | 3 | 5 | 2 | 0 | 18 |
| Esparaz, 2021 [36] | 8 | 3 | 5 | 2 | 0 | 18 |
| Pergola, 2020 [32] | 9 | 3 | 5 | 2 | 0 | 19 |
| Schafer, 2021 [34] | 8 | 3 | 5 | 2 | 0 | 18 |
| Theodorou, 2021 [42] | 11 | 3 | 5 | 2 | 4 | 25 |
| Study | Rater 1 | Rater 2 | Mean | Kappa Value | p |
|---|---|---|---|---|---|
| Orthopoulos, 2021 [39] | 19 | 20 | 19.5 | 0.961 | <0.001 |
| Bonilla, 2021 [30] | 18 | 19 | 18.5 | ||
| Gerall, 2021 [37] | 20 | 20 | 20 | ||
| Fonseca, 2020 [31] | 20 | 19 | 19.5 | ||
| Sheath, 2021 [41] | 19 | 19 | 19 | ||
| Place, 2020 [33] | 18 | 17 | 17.5 | ||
| Percul, 2021 [40] | 20 | 20 | 20 | ||
| Delgado-Miguel, 2021 [35] | 19 | 20 | 19.5 | ||
| Meyer, 2021 [38] | 18 | 18 | 18 | ||
| Esparaz, 2021 [36] | 18 | 18 | 18 | ||
| Pergola, 2020 [32] | 18 | 19 | 18.5 | ||
| Schafer, 2021 [34] | 18 | 18 | 18 | ||
| Theodorou, 2021 [42] | 25 | 25 | 25 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pogorelić, Z.; Anand, S.; Žuvela, T.; Singh, A.; Križanac, Z.; Krishnan, N. Incidence of Complicated Appendicitis during the COVID-19 Pandemic versus the Pre-Pandemic Period: A Systematic Review and Meta-Analysis of 2782 Pediatric Appendectomies. Diagnostics 2022, 12, 127. https://doi.org/10.3390/diagnostics12010127
Pogorelić Z, Anand S, Žuvela T, Singh A, Križanac Z, Krishnan N. Incidence of Complicated Appendicitis during the COVID-19 Pandemic versus the Pre-Pandemic Period: A Systematic Review and Meta-Analysis of 2782 Pediatric Appendectomies. Diagnostics. 2022; 12(1):127. https://doi.org/10.3390/diagnostics12010127
Chicago/Turabian StylePogorelić, Zenon, Sachit Anand, Tomislav Žuvela, Apoorv Singh, Zvonimir Križanac, and Nellai Krishnan. 2022. "Incidence of Complicated Appendicitis during the COVID-19 Pandemic versus the Pre-Pandemic Period: A Systematic Review and Meta-Analysis of 2782 Pediatric Appendectomies" Diagnostics 12, no. 1: 127. https://doi.org/10.3390/diagnostics12010127
APA StylePogorelić, Z., Anand, S., Žuvela, T., Singh, A., Križanac, Z., & Krishnan, N. (2022). Incidence of Complicated Appendicitis during the COVID-19 Pandemic versus the Pre-Pandemic Period: A Systematic Review and Meta-Analysis of 2782 Pediatric Appendectomies. Diagnostics, 12(1), 127. https://doi.org/10.3390/diagnostics12010127








