Influencing Cardiovascular Outcomes through Heart Rate Variability Modulation: A Systematic Review
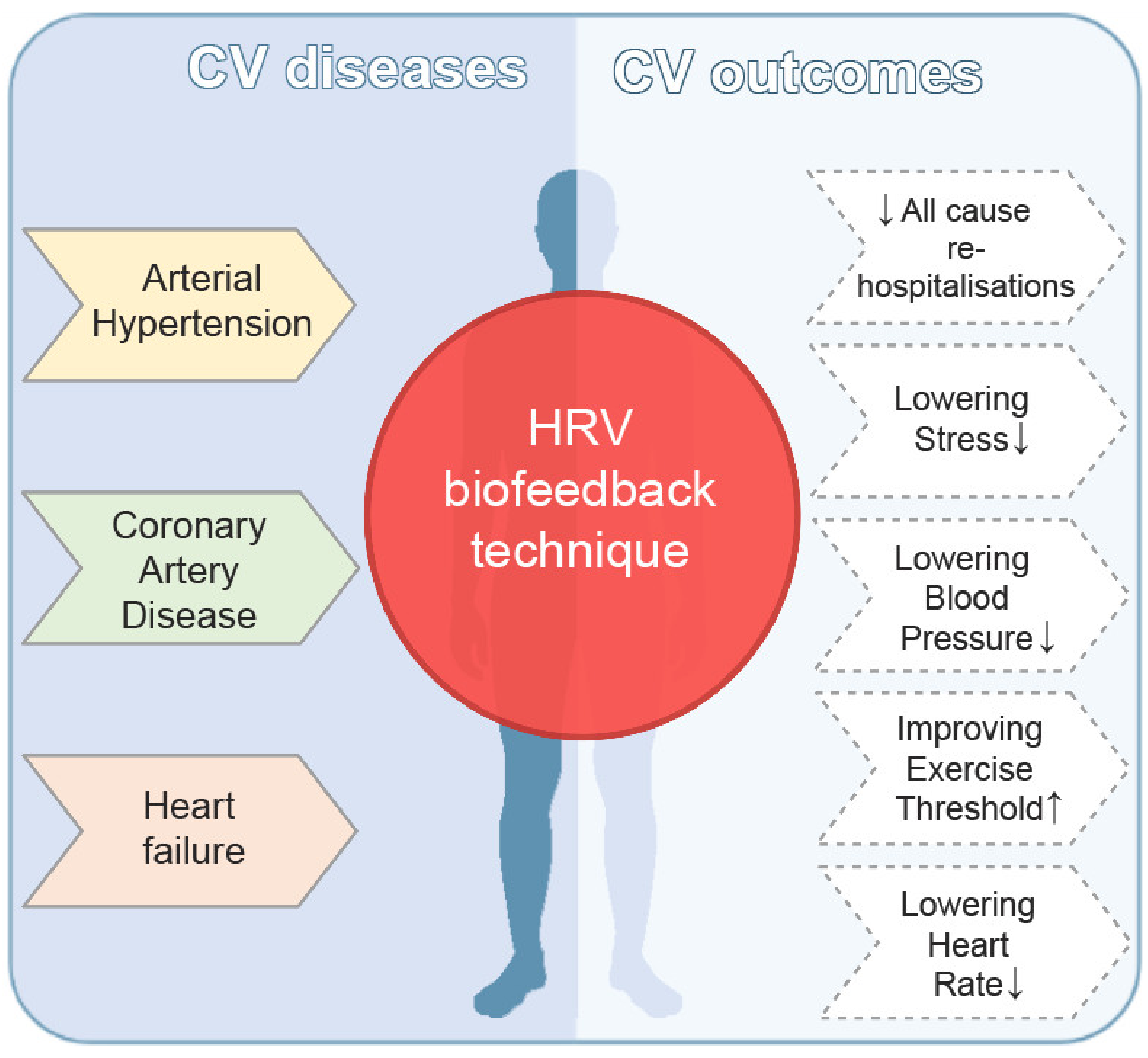
Abstract
1. Introduction
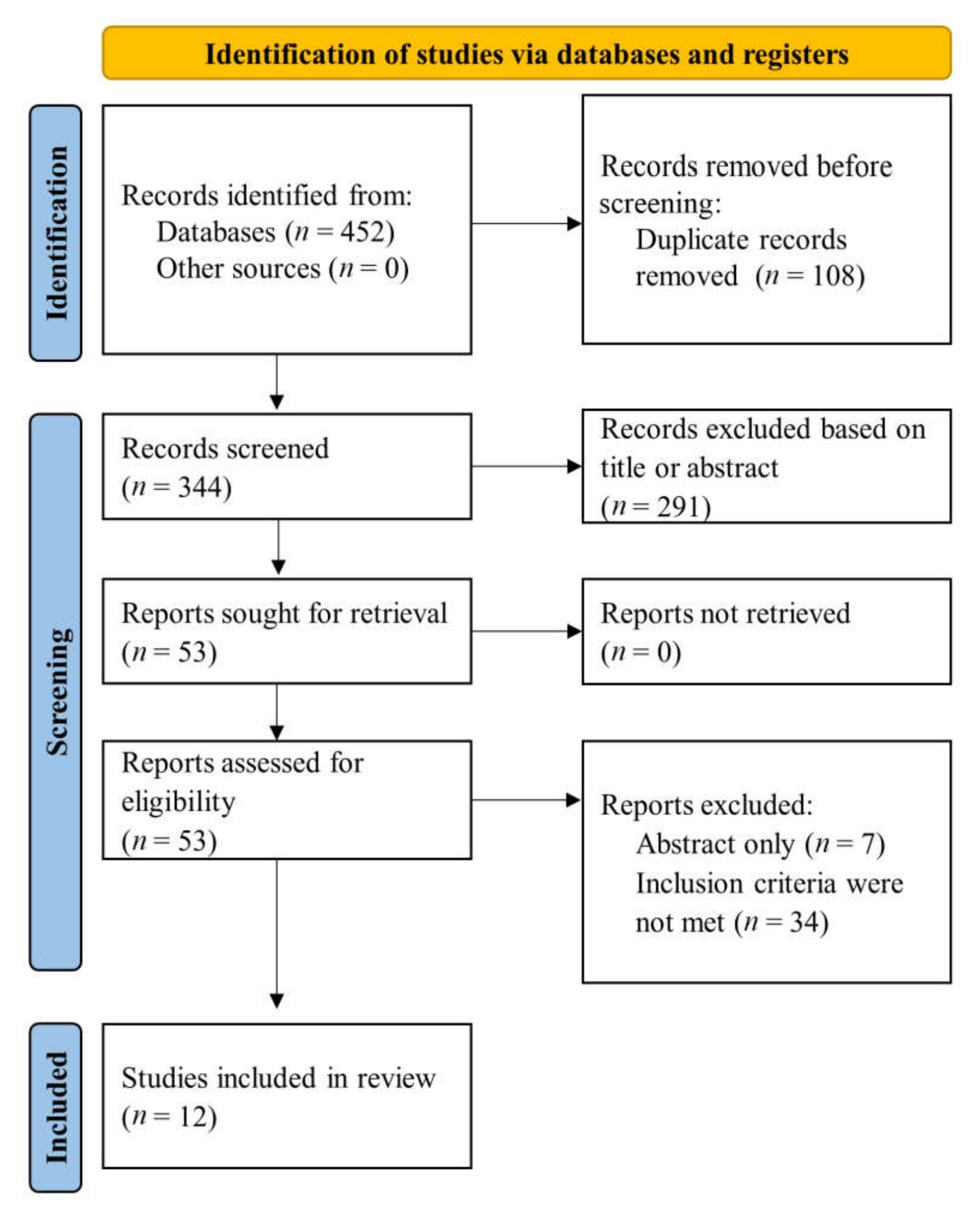
2. Materials and Methods
2.1. Data Sources and Search Strategy
2.2. Eligibility Criteria and Outcomes
2.3. Data Collection
2.4. Quality and Risk of Bias Assessment
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Ernst, G. Heart-Rate Variability—More than Heart Beats? Front. Public Health 2017, 5, 240. [Google Scholar] [CrossRef]
- Lee, H.; Jeon, S.-B.; Lee, K.-S. Continuous heart rate variability and electroencephalography monitoring in severe acute brain injury: A preliminary study. Acute Crit. Care 2021, 36, 151–161. [Google Scholar] [CrossRef]
- Blons, E.; Arsac, L.M.; Gilfriche, P.; McLeod, H.; Lespinet-Najib, V.; Grivel, E.; Deschodt-Arsac, V. Alterations in heart-brain interactions under mild stress during a cognitive task are reflected in entropy of heart rate dynamics. Sci. Rep. 2019, 9, 18190. [Google Scholar] [CrossRef]
- Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 1996, 93, 1043–1065. [CrossRef]
- Yang, L.; Zhao, Y.; Qiao, B.; Wang, Y.; Zhang, L.; Cui, T.; Fu, P. Heart Rate Variability and Prognosis in Hemodialysis Patients: A Meta-Analysis. Blood Purif. 2021, 50, 298–308. [Google Scholar] [CrossRef] [PubMed]
- Mather, M.; Thayer, J.F. How heart rate variability affects emotion regulation brain networks. Curr. Opin. Behav. Sci. 2018, 19, 98–104. [Google Scholar] [CrossRef]
- Kim, H.-G.; Cheon, E.-J.; Bai, D.-S.; Lee, Y.H.; Koo, B.-H. Stress and Heart Rate Variability: A Meta-Analysis and Review of the Literature. Psychiatry Investig. 2018, 15, 235–245. [Google Scholar] [CrossRef] [PubMed]
- Fang, S.-C.; Wu, Y.-L.; Tsai, P.-S. Heart Rate Variability and Risk of All-Cause Death and Cardiovascular Events in Patients with Cardiovascular Disease: A Meta-Analysis of Cohort Studies. Biol. Res. Nurs. 2020, 22, 45–56. [Google Scholar] [CrossRef]
- Qin, H.; Steenbergen, N.; Glos, M.; Wessel, N.; Kraemer, J.F.; Vaquerizo-Villar, F.; Penzel, T. The Different Facets of Heart Rate Variability in Obstructive Sleep Apnea. Front. Psychiatry 2021, 12, 1128. [Google Scholar] [CrossRef] [PubMed]
- Richardson, S.; Shaffer, J.A.; Falzon, L.; Krupka, D.; Davidson, K.W.; Edmondson, D. Meta-analysis of perceived stress and its association with incident coronary heart disease. Am. J. Cardiol. 2012, 110, 1711–1716. [Google Scholar] [CrossRef]
- Dar, T.; Radfar, A.; Abohashem, S.; Pitman, R.K.; Tawakol, A.; Osborne, M.T. Psychosocial Stress and Cardiovascular Disease. Curr. Treat. Options Cardiovasc. Med. 2019, 21, 23. [Google Scholar] [CrossRef]
- Fournié, C.; Chouchou, F.; Dalleau, G.; Caderby, T.; Cabrera, Q.; Verkindt, C. Heart rate variability biofeedback in chronic disease management: A systematic review. Complement. Ther. Med. 2021, 60, 102750. [Google Scholar] [CrossRef] [PubMed]
- Pizzoli, S.F.M.; Marzorati, C.; Gatti, D.; Monzani, D.; Mazzocco, K.; Pravettoni, G. A meta-analysis on heart rate variability biofeedback and depressive symptoms. Sci. Rep. 2021, 11, 6650. [Google Scholar] [CrossRef] [PubMed]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Goessl, V.C.; Curtiss, J.E.; Hofmann, S.G. The effect of heart rate variability biofeedback training on stress and anxiety: A meta-analysis. Psychol. Med. 2017, 47, 2578–2586. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.C.; Lin, I.M.; Fan, S.Y.; Chien, C.L.; Lin, T.H. One-Year Cardiovascular Prognosis of the Randomized, Controlled, Short-Term Heart Rate Variability Biofeedback among Patients with Coronary Artery Disease. Int. J. Behav. Med. 2018, 25, 271–282. [Google Scholar] [CrossRef]
- Swanson, K.S.; Gevirtz, R.N.; Brown, M.; Spira, J.; Guarneri, E.; Stoletniy, L. The effect of biofeedback on function in patients with heart failure. Appl. Psychophysiol. Biofeedback 2009, 34, 71–91. [Google Scholar] [CrossRef] [PubMed]
- Nolan, R.P.; Kamath, M.V.; Floras, J.S.; Stanley, J.; Pang, C.; Picton, P.; Young, Q.R. Heart rate variability biofeedback as a behavioral neurocardiac intervention to enhance vagal heart rate control. Am. Heart J. 2005, 149, 1137. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.; Xiang, Q.; Fu, X.; Wang, S.; Wang, S.; Chen, S.; Shao, L.; Zhao, Y.; Wang, T. Heart rate variability biofeedback decreases blood pressure in prehypertensive subjects by improving autonomic function and baroreflex. J. Altern. Complement. Med. 2012, 18, 143–152. [Google Scholar] [CrossRef]
- Jones, C.U.; Sangthong, B.; Pachirat, O. Slow breathing training reduces resting blood pressure and the pressure responses to exercise. Physiol. Res. 2015, 64, 673–682. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.U.; Sangthong, B.; Pachirat, O. An inspiratory load enhances the antihypertensive effects of home-based training with slow deep breathing: A randomised trial. J. Physiother. 2010, 56, 179–186. [Google Scholar] [CrossRef][Green Version]
- Climov, D.; Lysy, C.; Berteau, S.; Dutrannois, J.; Dereppe, H.; Brohet, C.; Melin, J. Biofeedback on heart rate variability in cardiac rehabilitation: Practical feasibility and psycho-physiological effects. Acta Cardiol. 2014, 69, 299–307. [Google Scholar] [CrossRef]
- Chen, S.; Sun, P.; Wang, S.; Lin, G.; Wang, T. Effects of heart rate variability biofeedback on cardiovascular responses and autonomic sympathovagal modulation following stressor tasks in prehypertensives. J. Hum. Hypertens. 2016, 30, 105–111. [Google Scholar] [CrossRef]
- Nolan, R.P.; Floras, J.S.; Harvey, P.J.; Kamath, M.V.; Picton, P.E.; Chessex, C.; Hiscock, N.; Powell, J.; Catt, M.; Hendrickx, H.; et al. Behavioral neurocardiac training in hypertension: A randomized, controlled trial. Hypertension 2010, 55, 1033–1039. [Google Scholar] [CrossRef]
- Bernardi, L.; Porta, C.; Spicuzza, L.; Bellwon, J.; Spadacini, G.; Frey, A.W.; Yeung, L.Y.; Sanderson, J.E.; Pedretti, R.; Tramarin, R. Slow breathing increases arterial baroreflex sensitivity in patients with chronic heart failure. Circulation 2002, 105, 143–145. [Google Scholar] [CrossRef]
- New York, B.S.D.A.C.; Nascimento, M.F.; de Moraes, A.A.; Leite, J.C.; de Souza, I.T.C.; Fernandes, A.T.D.N.S.F. Effect of device-guided paced breathing of biofeedback on blood pressure, stress and anxiety levels in hypertensives. Res. Soc. Dev. 2021, 10, e56110918525. [Google Scholar] [CrossRef]
- Joseph, C.N.; Porta, C.; Casucci, G.; Casiraghi, N.; Maffeis, M.; Rossi, M.; Bernardi, L. Slow breathing improves arterial baroreflex sensitivity and decreases blood pressure in essential hypertension. Hypertension 2005, 46, 714–718. [Google Scholar] [CrossRef]
- Schuurmans, A.A.T.; De Looff, P.; Nijhof, K.S.; Rosada, C.; Scholte, R.H.J.; Popma, A.; Otten, R. Validity of the Empatica E4 Wristband to Measure Heart Rate Variability (HRV) Parameters: A Comparison to Electrocardiography (ECG). J. Med. Syst. 2020, 44, 190. [Google Scholar] [CrossRef]
- Chorin, E.; Hochstadt, A.; Schwartz, A.L.; Matz, G.; Viskin, S.; Rosso, R. Continuous Heart Rate Monitoring for Automatic Detection of Life-Threatening Arrhythmias with Novel Bio-Sensing Technology. Front. Cardiovasc. Med. 2021, 8, 748. [Google Scholar] [CrossRef]
- Shaffer, F.; Meehan, Z.M. A Practical Guide to Resonance Frequency Assessment for Heart Rate Variability Biofeedback. Front. Neurosci. 2020, 14, 1055. [Google Scholar]
- Lehrer, P.M.; Vaschillo, B.; Zucker, T.; Graves, J.; Katsamanis, M.; Aviles, M.; Wamboldt, F.S. Protocol for Heart Rate Variability Biofeedback Training. Biofeedback 2013, 41, 98–109. [Google Scholar] [CrossRef]
- Lehrer, P.M.; Gevirtz, R. Heart rate variability biofeedback: How and why does it work? Front. Psychol. 2014, 5, 756. [Google Scholar] [CrossRef] [PubMed]
- Moravec, C.S. Biofeedback therapy in cardiovascular disease: Rationale and research overview. Clevel. Clin. J. Med. 2008, 75 (Suppl. S2), S35–S38. [Google Scholar] [CrossRef] [PubMed]
- Valensi, P. Autonomic nervous system activity changes in patients with hypertension and overweight: Role and therapeutic implications. Cardiovasc. Diabetol. 2021, 20, 170. [Google Scholar] [CrossRef] [PubMed]
- Carthy, E.R. Autonomic dysfunction in essential hypertension: A systematic review. Ann. Med. Surg. 2013, 3, 2–7. [Google Scholar] [CrossRef]
- van Bilsen, M.; Patel, H.C.; Bauersachs, J.; Böhm, M.; Borggrefe, M.; Brutsaert, D.; Coats, A.J.S.; de Boer, R.A.; de Keulenaer, G.W.; Filippatos, G.S.; et al. The autonomic nervous system as a therapeutic target in heart failure: A scientific position statement from the Translational Research Committee of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2017, 19, 1361–1378. [Google Scholar] [CrossRef] [PubMed]
| Author, Year | Design | Patients, No. | Age, Mean/ Median ± SD | Setting | Intervention and Comparator | Outcomes | Follow-Up |
|---|---|---|---|---|---|---|---|
| Yu et al., 2018 | Randomized, controlled, single-blinded, multicentre | 210 | 61.24—HRV-biofeedback group | Patients with coronary artery disease | HRV-biofeedback group (n = 105) versus control group (n = 105) which included 10 min of psychological education |
| 1 year |
| 60.31—control group | |||||||
| Swanson et al., 2009 | Randomized, controlled, single-blind, single centre | 29 | 54 ± 11—HRV-biofeedback group | Patients with NYHA class I–III heart failure | HRV-biofeedback (n = 15; once per week for 45 min at weeks 1–6) versus control group (n = 14) |
| 18 weeks |
| 56.4 ± 13.5—control group | |||||||
| Nolan et al., 2005 | Randomized, controlled, multicentre | 46 | 54.22 ± 1.04—HRV-biofeedback group | Patients with coronary heart disease (myocardial infarction, or positive diagnostic test) | HRV-biofeedback, 5 sessions, 6 breaths/minute (n = 27) versus active control group (n = 19) |
| 4 weeks |
| 54.95 ± 1.52—active control group | |||||||
| Lin et al., 2012 | Randomized, controlled, single centre | 43 | 22.3 | Asymptomatic patients with prehypertension (systolic blood pressure = 120-139 mmHg and/or diastolic blood pressure = 80–89 mmHg) | HRV-biofeedback group (n = 18, 10 sessions over 5 weeks), slow abdominal breathing group (n = 15) and control group (n = 10) |
| 3 months |
| Jones et al., 2015 | Randomized, controlled, single centre | 30 | 53.4 ± 4.3—no load training group | Patients with essential hypertension stage I–II | Slow breathing training for 8 weeks (n = 20, 10 with unloaded slow breathing and 10 against an inspiratory load of 20 cmH2O) or untrained controls (n = 10) | Systolic blood pressure and heart rate response to handgrip exercise | 10 weeks |
| 51.4 ± 5.3—loaded training group | |||||||
| 50.4 ± 5.4—control group | |||||||
| Jones et al., 2010 | Randomized, controlled, single centre | 30 | 53 ± 4—no load training group | Patients with essential hypertension stage I–II | Slow deep breathing at home, 30 min sessions, twice daily for 8 weeks (n = 20, 10 with unloaded breathing and 10 against an inspiratory load of 20 cm H2O) or control group (n = 10, normal daily life) | Resting blood pressure and heart rate (measured at home and in the laboratory) | 9 weeks |
| 51 ± 5—loaded training group | |||||||
| 50 ± 5— control group | |||||||
| Climov et al., 2014 | Randomized, controlled, single centre | 31 | 61.3 ± 6.2—HRV- biofeedback group | Patients with coronary artery disease | HRV-biofeedback group (10 sessions of 45–60 min in addition to rehabilitation programme) versus a control group in a cardiac rehabilitation centre setting |
| 6 weeks |
| 51.8 ± 9.7—control group | |||||||
| Chen et al., 2015 | Randomized, controlled, single centre | 32 | 21.5 ± 0.18 | Prehypertensive patients (systolic blood pressure = 120–139 mmHg and/or diastolic blood pressure = 80–89 mmHg) | HRV-biofeedback group (n = 12, 15 sessions), slow abdominal breathing group (n = 10) or control group (n = 10) |
| 3 months |
| Bernardi et al., 2002 | Observational | 102 | 58 ± 1—chronic heart failure group | Patients with stable chronic heart failure, NYHA classes I–IV | Slow breathing rate (4 min of controlled breathing 15/min and 4 min of controlled breathing 6/min) or spontaneous breathing |
| – |
| 55 ± 2— control group | |||||||
| Albuquerque Cacique et al., 2021 | Observational, single centre | 16 | 57.3 ± 14 | Patients with essential hypertension stage I–II | Biofeedback paced breathing, 8 sessions for 20 min |
| – |
| Nolan et al., 2010 | Randomized, controlled | 65 | 55.0 ± 1.2—HRV- biofeedback group | Patients with uncomplicated arterial hypertension | HRV-biofeedback (6 breaths/minute or active control (autogenic relaxation) —six 1 h sessions |
| 9 weeks |
| 55.9 ± 1.2— active control group | |||||||
| Joseph et al., 2005 | Observational | 46 | 56.4 ± 1.9— hypertensive patients | Patients with essential hypertension (n = 20) and healthy controls (n = 26) | Slow breathing (6 breaths/minute) or spontaneous breathing or faster breathing (15 breaths/minute) |
| – |
| 52.3 ± 1.4—healthy controls |
| Author, Year | Outcomes | Results | |
|---|---|---|---|
| Yu et al., 2018 | HRV-BF Group vs. Control Group | ||
| All-cause readmissions | 12.0% vs. 25.42% (RR = 0.31, 95% CI, 0.11–0.84) | p = 0.028 | |
| All-cause emergency visits | 13.33% vs. 35.59% (RR = 0.26, 95% CI, 0.11–0.63) | p = 0.001 | |
| All-cause and cardiac mortality | No deaths were reported | ||
| Swanson et al., 2009 | HRV-BF Group vs. Control Group | ||
| The 6 min walk test (Patients with LVEF ≥ 31%) | Baseline: 432 ± 77 m vs. 416 ± 166 m; Follow-up: 485 ± 109 m vs. 385 ± 160 m | p = 0.05 | |
| The 6 min walk test (Patients with LVEF ≤ 30%) | Baseline: 394 ± 73 m vs. 318 ± 113 m; Follow-up: 395 ± 87 m vs. 325 ± 115 m | ||
| LHFQ (patients with LVEF ≥ 31%) | Baseline: 33.0 ± 23.2 m vs. 33.7 ± 15.9 m; Follow-up: 38.0 ± 19.5 m vs. 22.2 ± 23.3 m (post-intervention) | p = 0.66 | |
| Nolan et al., 2005 | Stress—HRV-BF group (logHF) | Adjusted R2 = 0.86 | p = 0.022 |
| Depression—HRV-BF group (logHF) | Adjusted R2 = 0.81 | p = 0.033 | |
| Stress—active control group (logHF) | Adjusted R2 = 0.04 | p = 0.567 | |
| Depression—active control group (logHF) | Adjusted R2 = 0.13 | p = 0.946 | |
| Lin et al., 2012 | Blood pressure | Baseline: 131.7 ± 8.7/79.3 ± 4.7 mmHg After intervention: 118.9 ± 7.3/71.9 ± 4.9 mmHg 3 months: 118.9 ± 6.6/72.4 ± 5.6 mmHg | p < 0.01 |
| Systolic blood pressure | HRV-BF vs. Slow Abdominal Breathing | p < 0.05 | |
| Baroreflex sensitivity | Baseline: 7.0 ± 5.9 ms/mmHg After intervention: 15.8 ± 5.3 ms/mmHg | p < 0.01 | |
| Jones et al., 2015 | Systolic blood pressure in response to exercise | After slow breathing training, systolic blood pressure response was reduced by 10 mmHg (95% CI, −7 to −13) | p < 0.05 |
| Heart rate in response to exercise | After slow breathing training, heart rate response was reduced by 5 beats per minute (95% CI, −4 to −6) | p < 0.05 | |
| Jones et al., 2010 | Resting systolic blood pressure | Decreased with 7.0 mmHg (95% CI, 5.5–8.5) in unloaded breathing group and with 18.8 mmHg (95% CI, 16.1–21.5) in loaded breathing group compared to control group | p < 0.05 |
| Resting heart rate | Decreased with 8 beats/minute (95% CI, 6.5–10.3) in unloaded breathing group and with 9 beats/minute (95% CI, 5.6–12.2) in loaded breathing group | p < 0.05 | |
| Climov et al., 2014 | Systolic blood pressure | No statistically significant differences between the two groups | p = 0.64 |
| Diastolic blood pressure | p = 0.34 | ||
| Depression and anxiety | |||
| Chen et al., 2015 | Systolic blood pressure | Decreased from 131.58 ± 8.41 mmHg to 116.17 ± 9.25 mmHg in HRV-BF group vs. control group | p < 0.01 |
| Diastolic blood pressure | Decreased from 81.33 ± 3.06 mmHg to 71.17 ± 7.12 mmHg in HRV-BF vs. control group | ||
| Systolic and diastolic blood pressure | Decreased significantly in HRV-BF compared to slow abdominal breathing group at 3 months | p < 0.05 | |
| Bernardi et al., 2002 | Systolic blood pressure | Decreased from 117 ± 3 mmHg to 110 ± 4 mmHg | p = 0.009 |
| Diastolic blood pressure | Decreased from 62 ± 1 mmHg to 59 ± 1 mmHg | p = 0.02 | |
| Baroreflex sensitivity | Increased from 5.0 ± 0.3 ms/mmHg to 6.1 ± 0.5 ms/mmHg (in chronic heart failure patients) and from 9.4 ± 0.7 ms/mmHg to 13.8 ± 1.0 ms/mmHg (in healthy controls) | p < 0.0025 | |
| Albuquerque Cacique et al., 2021 | Systolic blood pressure | Decreased from 120 ± 16 mmHg to 111 ± 21 mmHg | p = 0.002 |
| Diastolic blood pressure | Decreased from 74.8 ± 9 mmHg to 72.1 ± 8 mmHg | p = 0.13 | |
| Anxiety (Hamilton anxiety rating scale) | Decreased from 17.2 ± 9 to 11 ± 7 | p = 0.0009 | |
| Stress (PSS) | Decreased from 15 ± 10 to 13 ± 5 | p = 0.37 | |
| Nolan et al., 2010 | Systolic blood pressure reduction | Daytime: −2.4 ± 0.9 mmHg 24 h: −2.1 ± 0.9 mmHg | p = 0.009 p = 0.03 |
| Pulse pressure reduction | Daytime: −1.7 ± 0.6 mmHg 24 h: −1.4 ± 0.6 mmHg | p = 0.004 p = 0.02 | |
| Diastolic blood pressure | Daytime and 24 h | p > 0.10 | |
| Uncontrolled blood pressure | Number of patients decreased from 17 (pre-treatment) to 12 after HRV-BF with a number needed to treat = 7 (95% CI, 4–57) | ||
| Joseph et al., 2005 | Systolic blood pressure | Decreased from 149.7 ± 3.7 mmHg to 141.1 ± 4 mmHg | p < 0.05 |
| Diastolic blood pressure | Decreased from 82.7 ± 3 mmHg to 77.8 ± 3.7 mmHg | p < 0.01 | |
| Baroreflex sensitivity | Increased from 5.8 ± 0.7 ms/mmHg to 10.3 ± 2.0 ms/mmHg | p < 0.01 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burlacu, A.; Brinza, C.; Popa, I.V.; Covic, A.; Floria, M. Influencing Cardiovascular Outcomes through Heart Rate Variability Modulation: A Systematic Review. Diagnostics 2021, 11, 2198. https://doi.org/10.3390/diagnostics11122198
Burlacu A, Brinza C, Popa IV, Covic A, Floria M. Influencing Cardiovascular Outcomes through Heart Rate Variability Modulation: A Systematic Review. Diagnostics. 2021; 11(12):2198. https://doi.org/10.3390/diagnostics11122198
Chicago/Turabian StyleBurlacu, Alexandru, Crischentian Brinza, Iolanda Valentina Popa, Adrian Covic, and Mariana Floria. 2021. "Influencing Cardiovascular Outcomes through Heart Rate Variability Modulation: A Systematic Review" Diagnostics 11, no. 12: 2198. https://doi.org/10.3390/diagnostics11122198
APA StyleBurlacu, A., Brinza, C., Popa, I. V., Covic, A., & Floria, M. (2021). Influencing Cardiovascular Outcomes through Heart Rate Variability Modulation: A Systematic Review. Diagnostics, 11(12), 2198. https://doi.org/10.3390/diagnostics11122198








