Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes: Evaluation of Hepatic Fibrosis and Steatosis Using Fibroscan
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design: This Study Was A Cross-Sectional Analysis
2.2. Populations
2.2.1. Inclusion Criteria
2.2.2. Exclusion Criteria
2.3. Sample Size
2.4. Performance
2.4.1. Clinical Assessment
2.4.2. FibroScan Examination
2.5. Data Analysis
3. Results
3.1. Population Characteristic
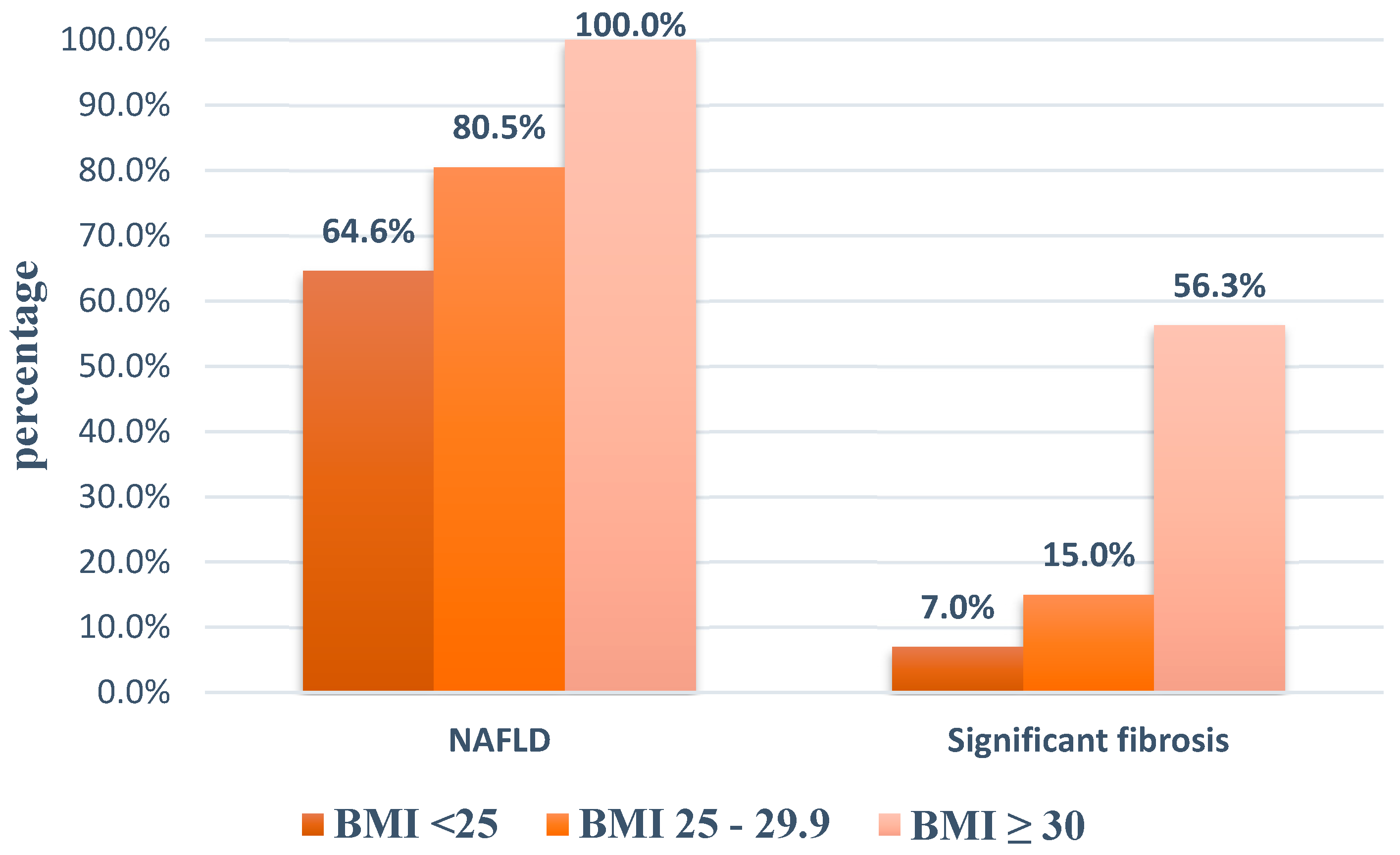
3.2. Prevalence of NAFLD in Type 2 Diabetic Patients
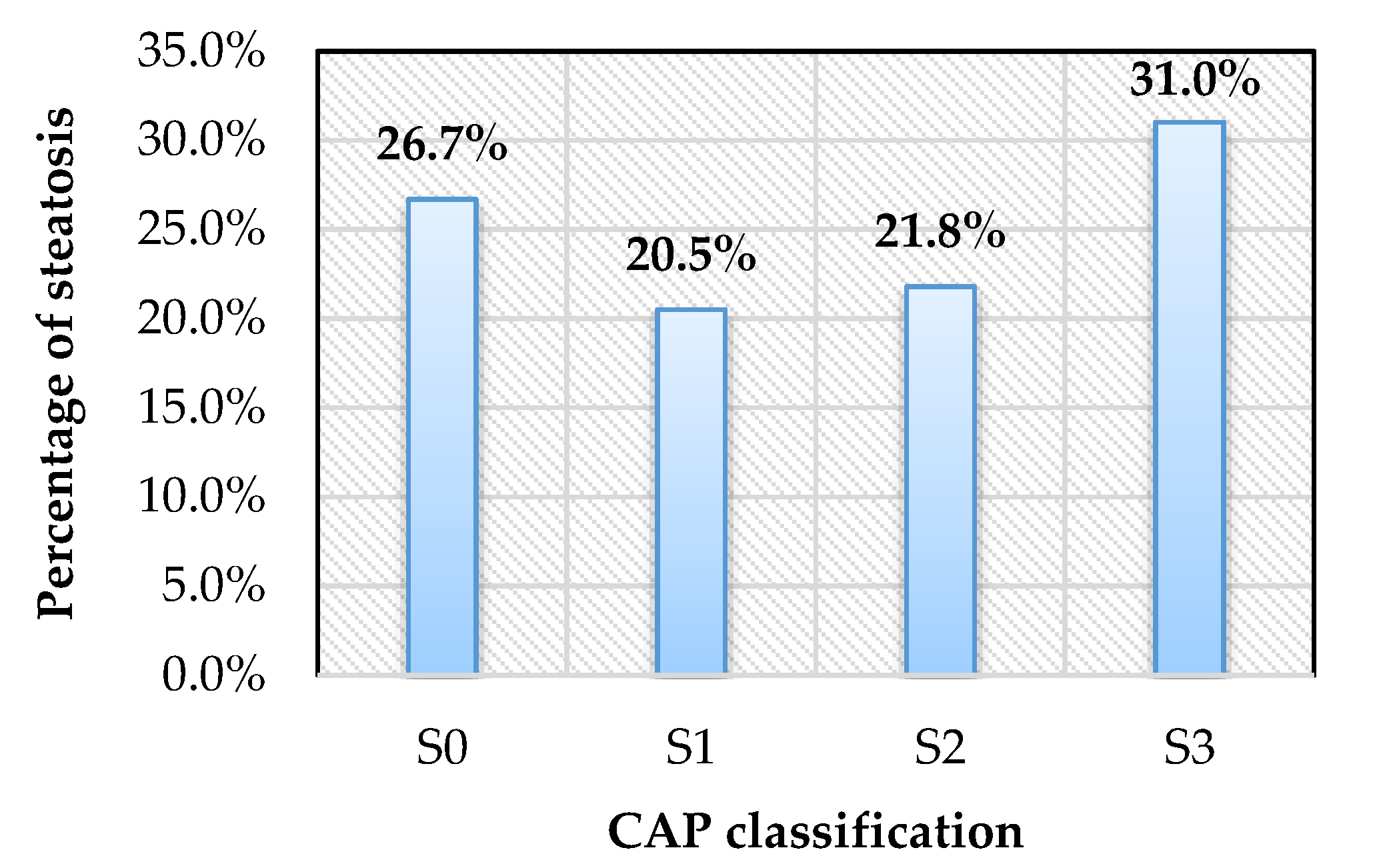
3.3. Prevalence of Hepatic Fibrosis Stages in Type 2 Diabetic Patients
3.4. NASH in Diabetic Patients
3.5. Factors Predicting Advanced Fibrosis in Type 2 Diabetic Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- LaBrecque, D.; Abass, Z.; Anania, F.; Ferenci, P. Nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. In World Gastroenterology Organisation Global Guidelines; WGO: Milwaukee, WI, USA, 2012. [Google Scholar]
- Ashtari, S.; Pourhoseingholi, M.; Zali, M. Non-alcohol fatty liver disease in Asia: Prevention and planning. World J. Hepatol. 2015, 7, 1788–1796. [Google Scholar] [CrossRef] [PubMed]
- Jian-Gao, F.; Seung-Up, K.; Vincent, W. New trends on obesity and NAFLD in Asia. J. Hepatol. 2017, 67, 862–873. [Google Scholar]
- Targher, G.; Byrne, C.; Lonardo, A.; Zoppini, G.; Barbui, C. Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: A meta-analysis. J. Hepatol. 2016, 65, 589–600. [Google Scholar] [CrossRef] [PubMed]
- Ekstedt, M.; Franzen, L.; Mathiesen, U.; Thorelius, L. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology 2006, 44, 865–873. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.; Gramlich, T.; Matteoni, C.; Boparai, N.; Mccullough, A. Nonalcoholic fatty liver disease in patients with type 2 diabetes. Clin. Gastroenterol. Hepatol. 2004, 2, 262–265. [Google Scholar] [CrossRef]
- Chalasani, N.; Younossi, Z.; Lavine, J.; Charlton, M.; Cusi, K.; Rinella, M.; Harrison, S.; Brunt, E.M.; Sanyal, A.J. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the study of liver diseases. Hepatology 2018, 67, 328–357. [Google Scholar] [CrossRef]
- EASL; EASD; EASO. EASL–EASD–EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J. Hepatol. 2016, 59, 1121–1140. [Google Scholar]
- Association, A.D. Classification and diagnosis of diabetes: Standards of medical care in diabetes 2018. In Standards of Medical Care in Diabetes—2018; Riddle, M., Ed.; American Diabetes Association: Arlington County, VA, USA, 2018; Volume 41, pp. 13–27. [Google Scholar]
- Kwok, R.; Choi, K.; Wong, G.; Zhang, Y. Screening diabetic patients for non-alcoholic fatty liver disease with controlled attenuation parameter and liver stiffness measurements: A prospective cohort study. Gut 2015, 65, 1359–1368. [Google Scholar] [CrossRef]
- Wong, V.; Vergniol, J.; Wong, G.; Foucher, J. Diagnosis of fibrosis and cirrhosis using liver stiffness measurement in nonalcoholic fatty liver disease. Hepatology 2010, 51, 454–462. [Google Scholar] [CrossRef]
- Karlas, T.; Petroff, D.; Garnov, N.; Bohm, S. Non-invasive assessment of hepatic steatosis in patients with NAFLD using controlled attenuation parameter and H-MR spectroscopy. PLoS ONE 2014, 9, e91987. [Google Scholar] [CrossRef]
- World Health Organization. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment; WHO: Geneva, Switzerland, 2000; pp. 18–20. [Google Scholar]
- International Diabetes Federation. The IDF Consensus Worldwide Definition of the Metabolic Syndrome; International Diabetes Federation: Brussels, Belgium, 2006. [Google Scholar]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- National, C.E.P.C.C. National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III); International Medical publishing, Inc.: Mclean, VA, USA, 2002; p. 106. [Google Scholar]
- Kwo, P.; Cohen, S.; Lim, J. ACG practice guideline: Evaluation of abnormal liver chemistries. Am. J. Gastroenterol. 2016, 112, 18–35. [Google Scholar] [CrossRef] [PubMed]
- Adams, L.; Feldstein, A. Non-invasive diagnosis of nonalcoholic fatty liver and nonalcoholic steatohepatitis. J. Dig. Dis. 2011, 12, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Lai, L.; Yusoff, W.; Vethakkan, S.; Mustapha, N. Screening for non-alcoholic fatty liver disease in patients with type 2 diabetes mellitus using transient elastography. J. Hepatol. 2019, 34, 1396–1403. [Google Scholar] [CrossRef]
- Wang, Y.; Fan, Q.; Wang, T.; Wen, J.; Wang, H.; Zhang, T. Controlled attenuation parameter for assessment of hepatic steatosis grades: A diagnostic meta-analysis. Int. J. Clin. Exp. Med. 2015, 8, 17654–17663. [Google Scholar] [PubMed]
- Bambha, K.; Belt, P.; Abraham, M.; Wilson, L.A. Ethnicity and nonalcoholic fatty liver disease. Hepatology 2012, 55, 769–780. [Google Scholar] [CrossRef]
- Rich, N.; Oji, S.; Mufti, A.; Browning, J.D.; Parikh, N.D.; Odewole, M.; Mayo, H.; Singal, A.G. Racial and ethnic disparities in nonalcoholic fatty liver disease prevalence, severity, and outcomes in the united states: A systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 2018, 16, 198–210.e2. [Google Scholar] [CrossRef] [PubMed]
- Ryan, C.; Johnson, L.; Germin, B.; Marcos, A. One hundred consecutive hepatic biopsies in the workup of living donors for right lobe liver transplantation. Liver Transplant. 2002, 8, 1114–1122. [Google Scholar] [CrossRef]
- Je´rome, B.; Paul, C. Controlled attenuation parameter (CAP): A new device for fast evaluation of liver fat? Liver Int. 2012, 32, 875–877. [Google Scholar]
- Wong, V.; Chan, W.; Chitturi, S.Y.C. Asia-Pacifc working party on non-alcoholic fatty liver disease guidelines 2017-Part 1: Definition, risk factors and assessment. J. Gastroenterol. Hepatol. 2018, 33, 70–85. [Google Scholar] [CrossRef]
- Wong, G.; Wong, V.; Chim, A.; Yiu, K. Factors associated with unreliable liver stiffness measurement and its failure with transient elastography in the Chinese population. Hepatology 2011, 26, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Sobhonslidsuk, A.; Pulsombat, A.; Kaewdoung, P.; Petraksa, S. Non-alcoholic fatty liver disease (nafld) and significant hepatic fibrosis defined by non-invasive assessment in patients with type 2 diabetes. Asian Pac. J. Cancer Prev. 2015, 16, 1789–1794. [Google Scholar] [CrossRef] [PubMed]
- Lédinghen, V.; Vergniol, J.; Gonzalez, C.; Foucher, J. Screening for liver fibrosis by using FibroScan® and FibroTest in patients with diabetes. Dig. Liver Dis. 2012, 44, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Hajiani, E.; Alavinejad, P.; Hashemi, S.; Masjedizadeh, A. Comparison of the transient elastography (fibroscan) results among diabetic and non-diabetic patients with non- alcoholic fatty liver disease. Gastroenterol. Hepatol. 2014, 1, 00021. [Google Scholar]
- Das, K.; Das, K.; Mukherjee, P.; Ghosh, A.; Ghosh, S. Nonobese population in a developing country has a high prevalence of nonalcoholic fatty liver and significant liver disease. Hepatology 2010, 51, 1593–1602. [Google Scholar] [CrossRef]
- Sookoian, S.; Pirola, C. Systematic review with meta-analysis: Risk factors for non-alcoholic fatty liver disease suggest a shared altered metabolic and cardiovascular profile between lean and obese patients. Aliment. Pharm. 2017, 46, 85–95. [Google Scholar] [CrossRef]
- Rej, R. Aspartate aminotransferase activity and isoenzyme proportions in human liver tissues. Clin. Chem. 1978, 24, 1971. [Google Scholar] [CrossRef]
- Wai, C.; Marrero, J.A.; Conjeevaram, H.S.; Lok, A.S.; Greenson, J.K.; Fontana, R.J.; Kalbfleisch, J.D. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology 2003, 38, 518–526. [Google Scholar] [CrossRef]
- Witters, P.; Freson, K.; Verslype, C.; Peerlinck, K. Review article: Blood platelet number and function in chronic liver disease and cirrhosis. Aliment. Pharm. Ther. 2008, 27, 1017–1029. [Google Scholar] [CrossRef]
| Patients with NAFLD (n = 225) | Patients without NAFLD (n = 82) | p | |
|---|---|---|---|
| Age (year) | 56.5 ± 10.5 | 57.6 ± 13.1 | 0.508 |
| Male (%) | 46.7 | 45.1 | 0.810 |
| Duration of DM (year) | 3 | 3 | 0.439 |
| SBP (mmHg) | 125.2 ± 13.9 | 122.7 ± 14.0 | 0.164 |
| DBP (mmHg) | 77.7 ± 9.0 | 74.7 ± 9.3 | 0.010 |
| Hypertension (%) | 65.8 | 52.4 | 0.033 |
| BMI (kg/m2) | 25.4 ± 2.8 | 23.4 ± 2.9 | <0.001 |
| Waist circumfenrence (cm) | 87.9 ± 9.3 | 80.5 ± 9.4 | <0.001 |
| Obesity (%) | 54.7 | 31.7 | <0.001 |
| Central obesity (%) | 72.4 | 39.0 | <0.001 |
| Dyslipidemia (%) | 93.8 | 73.2 | <0.001 |
| MS (%) | 68.9 | 36.6 | <0.001 |
| Glucose (mg/dL) | 136 (120–168) | 125 (112–153) | 0.016 |
| Cholesterol (mg/dL) | 186.7 ± 52.1 | 173.5 ± 51.6 | 0.050 |
| Triglyceride (mg/dL) | 199.1 (136.4–264) | 127.3 (87–193.2) | <0.001 |
| HDL (mg/dL) | 50.6 ± 13.0 | 56.6 ± 15.0 | 0.002 |
| LDL (mg/dL) | 114.2 ± 39.0 | 100.3 ± 41.5 | 0.009 |
| ALT (U/L) | 34 (23.4–54.1) | 20.8 (15.9–29.8) | <0.001 |
| AST (U/L) | 24.4 (20.1–33.9) | 20.2 (15.8–23.7) | <0.001 |
| GGT (U/L) | 46 (36.7–77.6) | 37.5 (21.4–46.8) | <0.001 |
| Platelet (K/μL) | 224 ± 53 | 229 ± 61 | 0.538 |
| Patients with Advanced Fibrosis (n = 18) | Patients without Advanced Fibrosis (n = 289) | p | |
|---|---|---|---|
| Age (year) | 58.7 ± 11.3 | 56.7 ± 11.2 | 0.725 |
| Male (%) | 38.9 | 46.7 | 0.518 |
| Duration of DM (year) | 6.5 (3–10) | 3 (2–6) | 0.056 |
| SBP (mmHg) | 123.3 ± 12.6 | 124.6 ± 14.0 | 0.690 |
| DBP (mmHg) | 76.7 ± 8.6 | 76.9 ± 9.2 | 0.920 |
| Hypertension (%) | 72.2 | 61.6 | 0.367 |
| BMI (kg/m2) | 26.3 ± 3.1 | 24.8 ± 2.9 | 0.039 |
| Waist circumference (cm) | 90.7 ± 9.0 | 85.6 ± 9.9 | 0.034 |
| Dyslipidemia (%) | 94.4 | 87.9 | 0.402 |
| Obesity (%) | 66.7 | 47.4 | 0.113 |
| Central obesity (%) | 88.9 | 61.9 | 0.021 |
| MS (%) | 88.9 | 58.5 | 0.011 |
| Glucose (mg/dL) | 147.5 (132–170) | 133 (117–165) | 0.113 |
| Cholesterol (mg/dL) | 174.5 ± 50.2 | 183.7 ± 52.4 | 0.469 |
| Triglyceride (mg/dL) | 177.1(142.3–244.9) | 182.2 (109.9–250.7) | 0.547 |
| HDL–C (mg/dL) | 48.9 ± 11.9 | 52.4 ± 13.9 | 0.248 |
| LDL–C (mg/dL) | 105.2 ± 41.2 | 110.8 ± 40.1 | 0.582 |
| ALT (U/L) | 60.6 (40.8–80.6) | 29.7 (19.5–42.2) | <0.001 |
| AST (U/L) | 45.3 (33.2–67.9) | 22.6 (18.2–29.2) | <0.001 |
| GGT (U/L) | 87.4 (62.4–173.9) | 46 (30.4–63.4) | <0.001 |
| Platelet (K/μL) | 186 ± 41 | 228 ± 55 | 0.005 |
| Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | Adjusted OR | 95% CI | p | |
| Age | 1.016 | 0.974–1.061 | 0.454 | |||
| Gender | 0.726 | 0.273–1.925 | 0.520 | |||
| Duration of DM | 1.092 | 1.000–1.193 | 0.050 | |||
| BMI | 1.191 | 1.006–1.411 | 0.043 | 1.152 | 0.837–1.586 | 0.385 |
| Obesity | 2.219 | 0.811–6.073 | 0.121 | |||
| Waist circumference | 1.055 | 1.004–1.110 | 0.036 | 0.964 | 0.870–1.069 | 0.486 |
| Central obesity | 4.916 | 1.109–21.792 | 0.036 | 3.220 | 0.460–22.527 | 0.239 |
| SBP | 0.993 | 0.959–1.029 | 0.713 | |||
| DBP | 0.997 | 0.947–1.051 | 0.924 | |||
| Hypertension | 1.621 | 0.563–4.672 | 0.371 | |||
| Cholesterol | 0.997 | 0.987–1.006 | 0.485 | |||
| HDL | 0.981 | 0.945–1.019 | 0.322 | |||
| LDL | 0.997 | 0.984–1.009 | 0.583 | |||
| Triglyceride | 0.999 | 0.996–1.003 | 0.771 | |||
| Glucose | 1.003 | 0.995–1.011 | 0.429 | |||
| ALT | 1.022 | 1.009–1.035 | 0.001 | 0.983 | 0.954–1.013 | 0.271 |
| AST | 1.055 | 1.032–1.077 | <0.001 | 1.067 | 1.017–1.119 | 0.008 |
| GGT | 1.007 | 1.003–1.010 | <0.001 | 0.999 | 0.995–1.005 | 0.933 |
| Platelet | 0.981 | 0.970–0.993 | 0.002 | 0.985 | 0.972–0.999 | 0.034 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tuong, T.T.K.; Tran, D.K.; Phu, P.Q.T.; Hong, T.N.D.; Chu Dinh, T.; Chu, D.T. Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes: Evaluation of Hepatic Fibrosis and Steatosis Using Fibroscan. Diagnostics 2020, 10, 159. https://doi.org/10.3390/diagnostics10030159
Tuong TTK, Tran DK, Phu PQT, Hong TND, Chu Dinh T, Chu DT. Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes: Evaluation of Hepatic Fibrosis and Steatosis Using Fibroscan. Diagnostics. 2020; 10(3):159. https://doi.org/10.3390/diagnostics10030159
Chicago/Turabian StyleTuong, Tran Thi Khanh, Dang Khoa Tran, Pham Quang Thien Phu, Tong Nguyen Diem Hong, Thien Chu Dinh, and Dinh Toi Chu. 2020. "Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes: Evaluation of Hepatic Fibrosis and Steatosis Using Fibroscan" Diagnostics 10, no. 3: 159. https://doi.org/10.3390/diagnostics10030159
APA StyleTuong, T. T. K., Tran, D. K., Phu, P. Q. T., Hong, T. N. D., Chu Dinh, T., & Chu, D. T. (2020). Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes: Evaluation of Hepatic Fibrosis and Steatosis Using Fibroscan. Diagnostics, 10(3), 159. https://doi.org/10.3390/diagnostics10030159






