Trans-Olecranon Fracture-Dislocations of the Elbow: A Systematic Review
Abstract
:1. Introduction
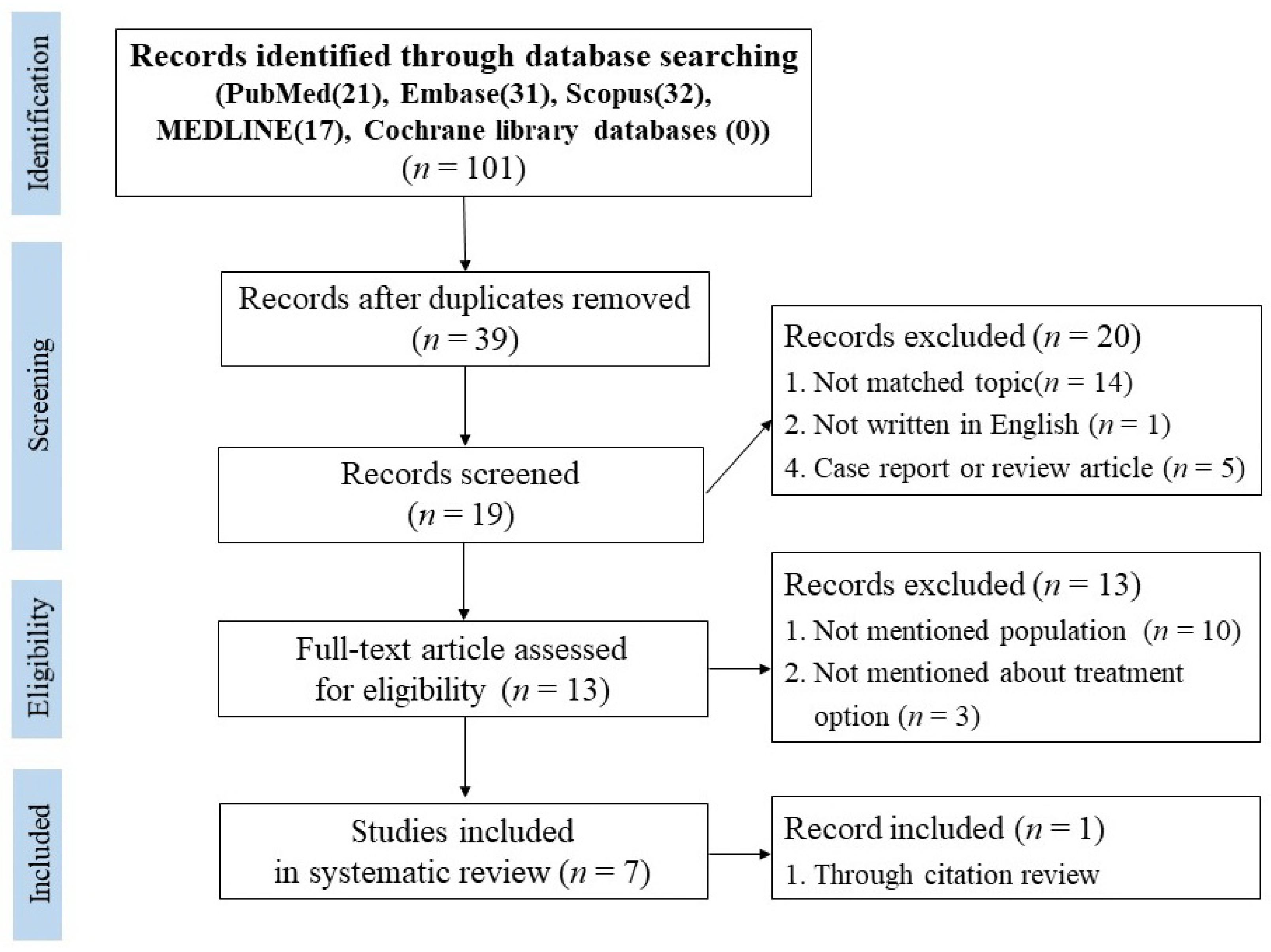
2. Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Data Extraction and Analysis
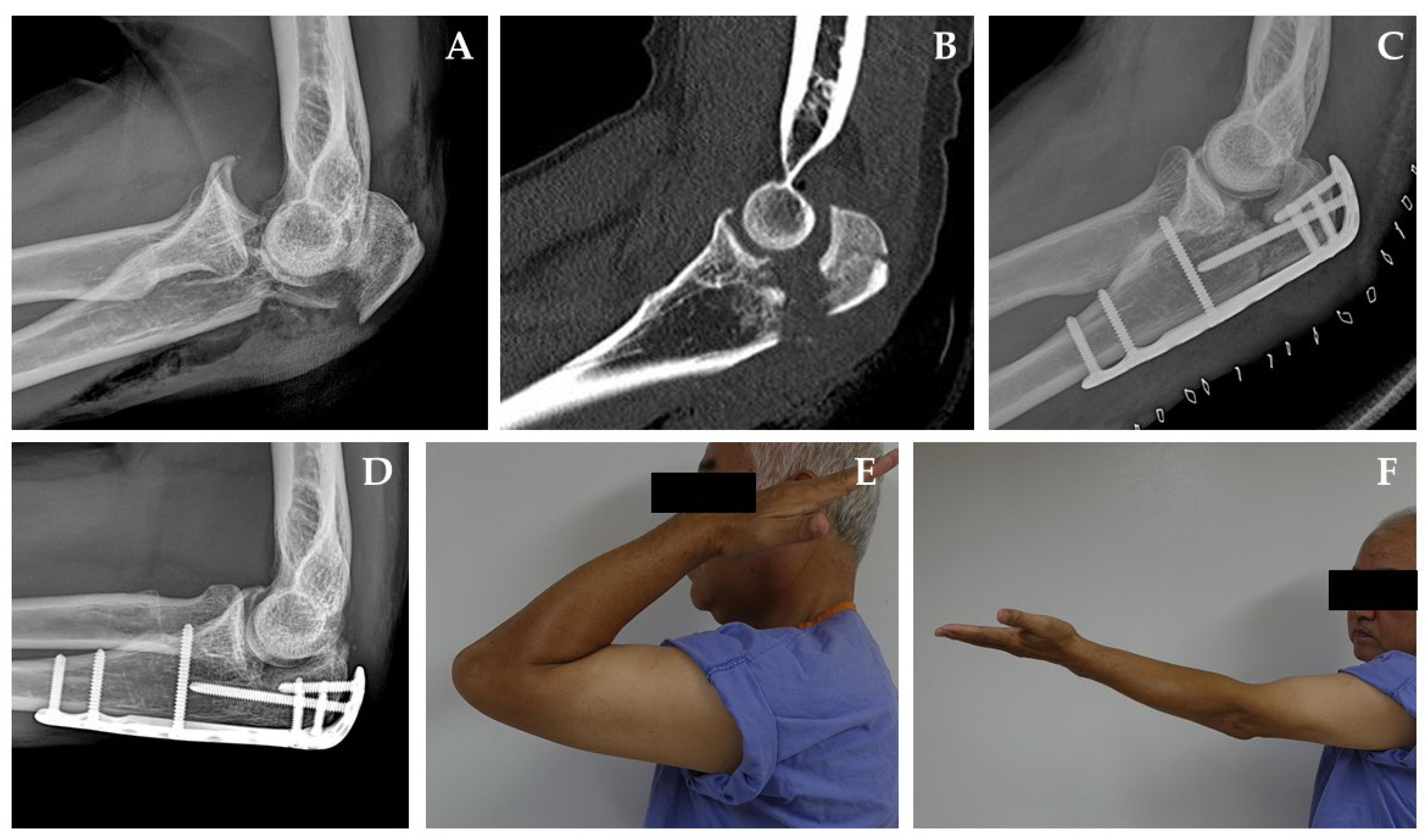
3. Results
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Scolaro, J.A.; Beingessner, D. Treatment of Monteggia and Transolecranon Fracture-Dislocations of the Elbow: A Critical Analysis Review. JBJS Rev. 2014, 2. [Google Scholar] [CrossRef] [PubMed]
- Ring, D.; Jupiter, J.B.; Sanders, R.W.; Mast, J.; Simpson, N.S. Transolecranon fracture-dislocation of the elbow. J. Orthop. Trauma 1997, 11, 545–550. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.; King, G.J.; Faber, K.J. Treatment of complex elbow fracture-dislocations. Curr. Rev. Musculoskelet. Med. 2016, 9, 185–189. [Google Scholar] [CrossRef] [PubMed]
- O’Driscoll, S.W.; Jupiter, J.B.; Cohen, M.S.; Ring, D.; McKee, M.D. Difficult elbow fractures: Pearls and pitfalls. Instr. Course Lect. 2003, 52, 113–134. [Google Scholar] [PubMed]
- Mortazavi, S.M.; Asadollahi, S.; Tahririan, M.A. Functional outcome following treatment of transolecranon fracture-dislocation of the elbow. Injury 2006, 37, 284–288. [Google Scholar] [CrossRef] [PubMed]
- Doornberg, J.; Ring, D.; Jupiter, J.B. Effective treatment of fracture-dislocations of the olecranon requires a stable trochlear notch. Clin. Orthop. Relat. Res. 2004, 292–300. [Google Scholar] [CrossRef] [PubMed]
- Biga, N.; Thomine, J.M. Trans-olecranal dislocations of the elbow. Rev. Chir. Orthop. Reparatrice Appar. Mot. 1974, 60, 557–567. [Google Scholar] [PubMed]
- Kamali, M. Monteggia fracture. Presentation of an unusual case. J. Bone Jt. Surg. Am. 1974, 56, 841–843. [Google Scholar] [CrossRef]
- Bruce, H.E.; Harvey, J.P.; Wilson, J.C., Jr. Monteggia fractures. J. Bone Jt. Surg. Am. 1974, 56, 1563–1576. [Google Scholar] [CrossRef]
- Haller, J.M.; Hulet, D.A.; Hannay, W.; Cardon, J.; Tashjian, R.; Beingessner, D. Patient Outcomes After Transolecranon Fracture-Dislocation. J. Am. Acad. Orthop. Surg. 2020. [Google Scholar] [CrossRef] [PubMed]
- Cha, Y.H.; Yoo, J.I.; Hwang, S.Y.; Kim, K.J.; Kim, H.Y.; Choy, W.S.; Hwang, S.C. Biomechanical Evaluation of Internal Fixation of Pauwels Type III Femoral Neck Fractures: A Systematic Review of Various Fixation Methods. Clin. Orthop. Surg. 2019, 11, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Cho, C.H.; Jung, J.W.; Na, S.S.; Bae, K.C.; Lee, K.J.; Kim, D.H. Is Acromial Fracture after Reverse Total Shoulder Arthroplasty a Negligible Complication? A Systematic Review. Clin. Orthop. Surg. 2019, 11, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Lindenhovius, A.L.; Brouwer, K.M.; Doornberg, J.N.; Ring, D.C.; Kloen, P. Long-term outcome of operatively treated fracture-dislocations of the olecranon. J. Orthop. Trauma 2008, 22, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Mouhsine, E.; Akiki, A.; Castagna, A.; Cikes, A.; Wettstein, M.; Borens, O.; Garofalo, R. Transolecranon anterior fracture dislocation. J. Should. Elbow Surg. 2007, 16, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Öztürkmen, Y.; Şükür, E.; Akman, Y.E.; Şenel, A.; Gürpınar, T. Clinical and radiological evaluation of surgical management in olecranon fracture-dislocations. Musculoskelet. Surg. 2019. [Google Scholar] [CrossRef] [PubMed]
- Morrey, B.F. Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid. Instr. Course Lect. 1995, 44, 175–185. [Google Scholar] [CrossRef] [PubMed]
| Authors | Number of Patients | Mean Age | Male | Female | Dominant Limb Ratio (%) | Mean Follow Up Period (month) |
|---|---|---|---|---|---|---|
| Ring et al. [2] | 17 | 38 | 14 | 3 | 41.2 | 25 |
| Doornberg et al. [6] | 10 | 49 | 7 | 3 | N/R | 79.2 |
| Moushine et al. [14] | 14 | 54 | 6 | 8 | 50 | 42 |
| Mortazavi et al. [5] | 8 | 35 | 7 | 1 | 25 | 37.4 |
| Haller et al. [10] | 35 | 45 | 25 | 10 | N/R | 28 |
| Lindenhovius et al. [13] | 10 | 30 | N/R | N/R | N/R | 235.2 |
| Öztürkmen et al. [15] | 11 | 44 | 7 | 4 | N/R | 34.9 |
| 105 | 42.1 | 66 | 29 | 41 | 68.8 |
| Authors | Ring et al. [2] | Doornberg et al. [6] | Moushine et al. [14] | Mortazavi et al. [5] | Haller et al. [10] | Lindenhovius et al. [13] | Öztürkmen et al. [15] |
|---|---|---|---|---|---|---|---|
| Number | 17 | 10 | 14 | 8 | 35 | 10 | 11 |
| Mechanism of injury | |||||||
| MVA * | 11 | 4 | 6 | 5 | 12 | N/R | 2 |
| Fall from height | 3 | 2 | 3 | 1 | 0 | N/R | 4 |
| Fall from standing height | 1 | 2 | 2 | 1 | 8 | N/R | 3 |
| Assault | 2 | 0 | 0 | 0 | N/R | N/R | 0 |
| Bicycle accident | 0 | 1 | 0 | 0 | N/R | N/R | 0 |
| Roller skating accident | 0 | 0 | 3 | 0 | N/R | N/R | 0 |
| Direct blow | 0 | 0 | 0 | 1 | N/R | N/R | 1 |
| Sports injury | 0 | 0 | 0 | 0 | N/R | N/R | 1 |
| Snow mobile accident | 0 | 1 | 0 | 0 | N/R | N/R | 0 |
| Fracture patterns | |||||||
| Simple, oblique | 3 | 1 | 1 | 1 | N/R | N/R | 1 |
| Simple, transverse | 0 | 0 | 3 | 0 | N/R | N/R | 0 |
| Complex, comminuted | 14 | 9 | 10 | 7 | N/R | N/R | 5 |
| Open fractures | |||||||
| Total | 5 | 3 | 6 | 1 | 12 | 1 | 1 |
| GA I | 0 | 0 | 0 | 1 | 3 | 1 | 1 |
| GA II | 2 | 2 | 4 | 0 | 7 | 0 | 0 |
| GA IIIA | 2 | 1 | 0 | 0 | 2 | 0 | 0 |
| GA IIIB | 1 | 0 | 2 | 0 | 0 | 0 | 0 |
| Coronoid process fractures | 8 | 5 | 5 | 4 | 23 | 5 | 6 |
| Radial head fractures | 2 | 1 | 1 | 2 | 9 | 0 | 3 |
| Accompanied injury | 7: segmental ulnar fx. * | 0 | N/R | 1: humerus neck fx. 1: calcaneus fx. | 2: capitellum fx. 1: lateral condylar fx. 1: compartment syndrome | N/R | N/R |
| Approach | Dorsal mid longitudinal | Dorsal mid longitudinal | Dorsal mid longitudinal | N/R | Dorsal mid longitudinal | N/R | Dorsal mid longitudinal |
| Surgical method | |||||||
| ORIF * c plate | |||||||
| 3.5 mm Limited contact DCP * | 9 | 5 | 0 | 0 | 0 | 0 | N/R |
| 3.5 mm DCP | 0 | 1 | 1 | 0 | 0 | 4 | N/R |
| 3.5 mm Recon plate | 2 | 0 | 4 | 7 | 0 | 0 | N/R |
| Semitubular plate | 2 | 0 | 0 | 0 | 0 | 0 | N/R |
| 1/3 tubular plate | 2 | 1 | 2 | 0 | 0 | 2 | N/R |
| 3.5 precontoured plate | 0 | 0 | 0 | 0 | 35 | 0 | N/R |
| ORIF c tension band | 2 | 2 | 7 | 1 | 0 | 3 | N/R |
| ORIF c tension suture | 0 | 1 | 0 | 0 | 0 | 0 | N/R |
| RC * transfixation c wire | 0 | 0 | 0 | 0 | 0 | 1 | N/R |
| Clinical Scores | |||||||
| Broberg/Morrey rating | Excellent: 7 Good: 8 Fair: 2 Poor: 0 | Excellent: 4 Good: 5 Fair: 0 Poor: 1 | Excellent: 4 Good: 6 Fair: 2 Poor: 2 | Excellent: 2 Good: 5 Fair: 1 Poor: 0 | N/R | Excellent: 5 Good: 3 Fair: 0 Poor: 2 | Excellent: 3 Good: 6 Fair: 2 Poor: 0 |
| ASES * | N/R | 89.2 | N/R | 89 | N/R | N/R | 87.8 |
| DASH * | N/R | N/R | N/R | N/R | 9 (28 patients) | 14.5 | N/R |
| MEPI * | N/R | N/R | N/R | N/R | N/R | Excellent: 5 Good: 3 Fair: 1 Poor: 1 | N/R |
| Average ROM * | |||||||
| Flexion | 127° | 130° | 125° (110–140°) | 115° (85–140°) | 123° (45–145°) | N/R | N/R |
| Extension | N/R | N/R | −22° (−40–0°) | N/R | 16° (0–80°) | N/R | N/R |
| Flexion–extension arc | N/R | 110° | N/R | N/R | 107° (10– 130°) | Early F/U *: 117° (70–140°) Long term F/U: 124° (50–145°) | 107.3° |
| Flexion contracture | 14° | 20° | N/R | 22° (0–45°) | N/R | N/R | N/R |
| Supination | Normal | 75° | 76° (60–90°) | 83° (80–85°) | 77° (20–85°) | N/R | 69.1° |
| Pronation | Normal | 80° | 68° (55–85°) | 75° (40–90°) | 65° (30–70°) | N/R | 79.1° |
| Supination-pronation arc | N/R | 155° | N/R | 157.5° (120–173°) | 137° (50–155°, 29 pt.) | Early F/U: 123° (0–180°) Long term F/U: 133° (0–170°) | 150° |
| Authors | No * | HO * | Arthrosis | Nerve Injury | Osteoarthritis | Radioulnar Synostosis | Persistent Pain | Loosening | Infection | Delayed Union | Nonunion | Limitation of Motion | UH * Instability | Malunion | Re-Operation |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ring D et al. [2] | 17 | 1 | 2 | 0 | N/R * | N/R | 3 | 2: 1/3 tubular | N/R | N/R | 0 | 1 | 0 | 0 | 2: 1/3 tubular plate loosening |
| Doornberg et al. [6] | 10 | 1 | 2 | 1 BPI *, 1 ulnar nerve | N/R | 4 | 1: tension band wire | N/R | N/R | N/R | 1 (MUA *) | 2 | 2 | 5: 1 failed tension band3: capsular release1: ulnar nonunion | |
| Moushine et al. [14] | 14 | 4 | N/R | 0 | 4 | N/R | N/R | N/R | 0 | 3 | 2 | N/R | 0 | N/R | 4: tension band wiring failed |
| Mortazavi et al. [5] | 8 | 1 | N/R | N/R | 0 | N/R | 1 | 1: tension band | N/R | N/R | 1 | 1 | N/R | N/R | 4: 1 failed tension band, 3: elective hardware removal |
| Haller et al. [10] | 35 | 15 | 13 | 6: ulnar nerve | 11 | 2 | 2 | N/R | 4 (I & D with IV * Anti-biotics) | N/R | N/R | N/R | N/R | N/R | 14: 4 devices remove |
| Lindenhovius et al. [13] | 10 | N/R | 5 | 7: ulnar nerve | N/R | N/R | N/R | N/R | N/R | N/R | N/R | N/R | N/R | N/R | 2: 1/3 tubular plate loosening |
| Öztürkmen et al. [15] | 11 | 1 | 5 | 1: ulnar nerve | N/R | N/R | N/R | N/R | N/R | N/R | N/R | N/R | N/R | N/R | N/R |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, C.-H.; Kim, D.-H.; Na, S.S.; Choi, B.-C.; Kim, B.-S. Trans-Olecranon Fracture-Dislocations of the Elbow: A Systematic Review. Diagnostics 2020, 10, 1058. https://doi.org/10.3390/diagnostics10121058
Cho C-H, Kim D-H, Na SS, Choi B-C, Kim B-S. Trans-Olecranon Fracture-Dislocations of the Elbow: A Systematic Review. Diagnostics. 2020; 10(12):1058. https://doi.org/10.3390/diagnostics10121058
Chicago/Turabian StyleCho, Chul-Hyun, Du-Han Kim, Sang Soo Na, Byung-Chan Choi, and Beom-Soo Kim. 2020. "Trans-Olecranon Fracture-Dislocations of the Elbow: A Systematic Review" Diagnostics 10, no. 12: 1058. https://doi.org/10.3390/diagnostics10121058
APA StyleCho, C.-H., Kim, D.-H., Na, S. S., Choi, B.-C., & Kim, B.-S. (2020). Trans-Olecranon Fracture-Dislocations of the Elbow: A Systematic Review. Diagnostics, 10(12), 1058. https://doi.org/10.3390/diagnostics10121058







